
Overdose Prevention in New York City:
Supervised Injection as a Strategy to
Reduce Opioid Overdose and Public
Injection
1
TABLE OF CONTENTS
Executive Summary 03
Background 07
Overdose in New York City
HealingNYC 12
Expanding New York City’s Response to the Overdose Crisis
A Legacy of Public Health Innovation in New York City 17
Why Supervised Injection Facilities? 20
A Review of the Evidence
Would New Yorkers Support Supervised Injection Facilities? 23
Community Support for and Concerns about Supervised Injection
What Would New York City Gain from Supervised Injection Facilities? 33
Estimating the Health and Fiscal Impacts of Supervised Injection in New York City
How Could New York City Implement Supervised Injection Facilities? 36
Viable Legal Frameworks for Supervised Injection Facilities in New York City
Case Studies: Supervised Injection Facilities at the Municipal Level 40
Update from Seattle, San Francisco, and Philadelphia
Recommendations 43
Acknowledgments 48
References 51
Appendix A 55
Institutional Support for Supervised Injection
Appendix B 57
Statement of Support for Supervised Injection from the American Medical Association
Appendix C 59
Statement of Support for Supervised Injection from the American Public Health
Association
2
Appendix D 81
Letter of Support for Supervised Injection from amfAR, the Foundation for AIDS
Research to New York State Governor Andrew M. Cuomo
Appendix E 83
New York City Supervised Injection Facility Impact Report
Appendix F 127
Legal Challenges to and Avenues for Supervised Injection Facility Implementation in
New York City
3
EXECUTIVE SUMMARY
Overdose deaths in New York City have risen steadily over the past 15 years, growing to
the crisis we now face. In 2017, provisional data confirmed 1,441 overdose fatalities in
New York City—the deadliest year on record.
1
Someone dies from a drug overdose in New
York City every seven hours, and more people died from overdose in New York City in 2017
than from suicide, homicide, and motor vehicle accidents combined.
2
Since 2014, fentanyl,
an opioid 50 to 100 times more potent than morphine, has driven the dramatic increase in
overdose deaths.
The opioid overdose epidemic in New York City persists despite current efforts, which
include availability of treatment services, collaborative interventions between public
health and law enforcement, and increased access to the emergency overdose rescue
medicine naloxone. Recognizing that opioid-involved overdose deaths are preventable, the
City has redoubled its efforts with a broad, multi-agency cross-sector approach known as
HealingNYC. This comprehensive strategy aims to reduce opioid overdose deaths by 35%
by 2022. Key components of HealingNYC include: expanded access to effective treatment;
innovative methods of overdose prevention that reach individuals at high risk; education
aimed at clinicians and communities to prevent substance misuse before it starts; and
using new methods to reduce the supply of drugs.
3
As HealingNYC moves forward, the City
maintains its commitment to deploying strategies grounded in science and to considering
all evidence-based interventions that could prevent people from dying in the present
overdose crisis.
Supervised injection facilities (SIFs) are one public health strategy to reduce overdose
deaths, infectious disease transmission, and public drug use. Supervised injection facilities
offer hygienic spaces for people to inject drugs obtained offsite using sterile equipment
under medical supervision. There are 100 SIF locations worldwide, including a recent
expansion to three cities in Canada. In the United States, SIFs have not been implemented
but are under consideration in at least five cities. Through co-location or referral, SIFs also
provide people who inject drugs access to a range of health, substance use, and social
services. As such, SIFs serve as an early entry point along the continuum of care for people
with substance use disorders. Finally, SIFs have garnered support and endorsement from a
range of professional health bodies, including the American Medical Association,
4
the
American Public Health Association,
5
the International Drug Policy Consortium,
6
and the
European Monitoring Centre for Drugs and Drug Addiction.
7
To explore the potential impact of incorporating supervised injection into City’s opioid
response strategy, the New York City Council provided funding to the New York City
Department of Health and Mental Hygiene (DOHMH) to assess the feasibility of establishing
a SIF. DOHMH began with a literature review to summarize the international experience
with SIFs. Additionally, an Expert Advisory Panel comprised of national and international
drug policy experts, scientists, and advocates was assembled to guide the study. A list of the
Expert Advisory Panel members can be found in the Acknowledgments.

4
To explore the feasibility of SIFs in New York City, three key questions were addressed:
1. Would New Yorkers support supervised injection facilities?
The New York Academy of Medicine (NYAM) and DOHMH conducted structured
focus groups and individual interviews regarding perspectives on supervised
injection services with key community and institutional stakeholders. Participants
represented a range of constituencies: law enforcement, health care, social and
community services, faith traditions, business development, and harm reduction.
Input from elected officials serving in New York City and State offices also was
solicited.
2. What are the potential health and fiscal benefits of a supervised
injection facility to New York City?
Researchers at Weill Cornell Medical College projected the impact of a supervised
injection facility on opioid overdose deaths and direct health care expenditures in
New York City, looking at emergency medical service usage, emergency department
visits, and hospitalizations. A Technical Advisory Group composed of global leaders
in supervised injection with expertise in economics, policy analysis, and clinical and
behavioral sciences offered guidance and oversight to this study.
3. What are the viable legal frameworks within which New York City could
establish a supervised injection facility?
A legal scholar from Columbia Law School assessed the current legal barriers to the
establishment of a supervised injection facility in New York City to identify potential
avenues for implementation. This review assessed federal, state, and municipal
criminal and civil laws and regulations that could be relevant to the establishment of
a SIF in New York City, as well as examples and lessons learned from other
jurisdictions across the United States. The findings from this review support the
feasibility of supervised injection facilities.
Supervised injection is an evidence-based health intervention for people who
inject drugs
Scientific evidence suggests that SIFs—like methadone maintenance treatment and syringe
exchange programs established in response to the previous opioid and HIV/AIDS crises—
prevent overdose and reduce the harms associated with injection drug use, including HIV
and hepatitis C transmission. Supervised injection facilities provide support and
connections to health and social services to marginalized individuals, particularly shelter
residents, so people who inject drugs can reduce their risk of death and take positive steps
toward healthier lives. In addition to the individual benefits, research from other
jurisdictions shows that SIFs may lead to long-term reductions in individual-level drug use
and community-level drug-related crime in areas where they are located, and thus save
taxpayer dollars on health care and crime control.
5
Key community leaders recognize the benefits of and challenges to establishing
supervised injection as a strategy to prevent overdose and reduce crime
Findings from NYAM’s community assessment and DOHMH’s stakeholder interviews
suggest that supervised injection facilities have the support of many medical, harm
reduction, business, faith, community, and elected leaders. Stakeholders acknowledged the
seriousness of the overdose crisis, the need for new solutions, and the functional approach
of SIFs. Stakeholders particularly appreciated SIFs’ role in linking participants to needed
medical, social, and community services. Some stakeholders highlighted potential
community concerns that SIFs could convey that drug use was being condoned or create
geographic concentrations of people who inject drugs. These community concerns could
lead to challenges with SIF placement, although these challenges may be mitigated through
co-location within existing harm reduction services as part of the continuum of care.
Almost all leaders and community representatives interviewed, however, acknowledged
the public health and safety benefits of supervised injection. Stakeholders emphasized that
meaningful community engagement and education would be critical to the success of SIFs,
particularly in any neighborhoods that could be selected for SIF placement. Additional
engagement is needed to best capture all community perspectives, as current findings are
limited to those who agreed to participate at the time of the study.
Establishment of four supervised injection facilities could conservatively avert
up to 130 overdoses and save up to $7 million in public health care costs
annually
Results from the impact study conducted by Weill Cornell Medical College found that
locating SIFs in four New York City neighborhoods most severely affected by fatal drug
overdose could prevent up to 130 overdose deaths each year and reduce associated annual
costs to the City health care system by up to $7 million. The estimates generated by this
study are conservative, as they do not include reduction in crime or chronic disease
treatment costs associated with injection drug use. The cost-savings of a SIF would be
offset by the costs to operate a SIF. These costs would vary depending on the model and
hours of operation. On the low end, a SIF could be implemented for $250,000 annually; on
the upper end, a new, freestanding facility with long hours could cost between $2 and $3
million.
Legal establishment of supervised injection facilities in New York City is possible
Findings from the legal review suggest that, despite legal barriers, state and municipal
options exist to establish one or more SIFs in New York City. Any avenue would require
engaging diverse representatives from public health, public safety, law enforcement,
advocacy and community groups, and elected officials in the planning process.
Taken together, these findings have led to a series of recommendations regarding the
planning and implementation of a SIF to supplement New York City’s comprehensive
overdose prevention strategy. In particular, the recommendations presented in this report
aim to leverage New York City’s existing treatment and social service resources to integrate
SIFs within established networks of care. A wide range of stakeholders in New York City
support supervised injection as a strategy, but also acknowledge potential community

6
concerns in establishing supervised injection services. Our recommendations around SIFs
build on the legacies of methadone maintenance treatment and early grassroots adoption
of syringe exchange programs by health advocates, medical and social service
professionals, and scientists in New York City. Additionally, New York City has a strong
network of health and social service agencies, and productive collaboration between the
public health and public safety communities—all essential partners to launch SIFs.
What follows are detailed findings from the three commissioned studies, supplementary
data collected by DOHMH, and a comprehensive review of the existing body of scientific
evidence on supervised injection. Overdose affects all New Yorkers. To learn more about
overdose prevention, we invite readers to visit: www1.nyc.gov/site/doh/health/health-
topics/alcohol-and-drug-use-prevent-overdose.page.

7
BACKGROUND
Overdose in New York City
The United States is in the midst of a overdose epidemic, with over 63,000 deaths in 2016
due to overdose. The majority of these deaths (66%) are caused by opioids, a drug class
that includes prescription painkillers, heroin, and the highly potent synthetic compound
fentanyl.
8
The entire nation—East and West, North and South, urban and rural—has been
touched by this crisis, which has shown no signs of slowing down.
Like the rest of the country, New York City has experienced alarming increases in overdose
deaths over the last 15 years. The number of deaths from overdose in New York City have
more than doubled since 2000, with an increase of over 2.5 fold since 2010. In 2017,
provisional data shows that 1,441 overdose fatalities ocurred in New York City, the highest
number ever recorded. Over 80% of these deaths involved opioids.
9
Someone dies every
seven hours of overdose in New York City; there are more annual deaths from opioid
overdose than from car crashes, suicides, and homicides combined.
10
Figure 1: Number of unintentional drug poisoning (overdose) deaths by year,
New York City, 2000 – 2017
Source: New York City Department of Health and Mental Hygiene, Unintentional Drug Poisoning (Overdose) Deaths Quarters 1-4, 2017,
New York City, released April, 2018.
0
200
400
600
800
1000
1200
1400
1600
Number of overdose
deaths
1,441 overdose deaths
deaths

8
Figure 2: Number of deaths from unintentional drug poisoning (overdose) compared to intentional self-harm
(suicide), assault (homicide), and motor vehicle crashes in New York City, 2006 – 2017
Source: New York City Department of Health and Mental Hygiene, Unintentional Drug Poisoning (Overdose) Deaths Quarters 1-4, 2017,
New York City, released April, 2018.Li W, Sebek K, Huynh M, Castro A, Gurr D, Kelley D, Kennedy J, Maduro G, Lee E, Sun Y, Zheng P, and
Van Wye G. Summary of Vital Statistics, 2015. New York, NY: New York City Department of Health and Mental Hygiene, Bureau of Vital
Statistics, 2017.
Zimmerman R, Li W, Gambatese M, Madsen A, Lasner-Frater L, Van Wye G, Kelley D , Kennedy J, Maduro G, Sun Y. Summary of Vital
Statistics, 2012. New York, NY: New York City Department of Health and Mental Hygiene, Bureau of Vital Statistics, 2013.
Although prescription painkillers helped to drive the increase in the rate of overdose
deaths in New York City from 2010 to 2011, the proportion of overdose deaths involving
opioid analgesics had decreased to 18% by 2016, from a high of 35% in 2011.
11
Between
2011 and 2014, a rise in heroin-involved overdoses drove the increases in overdose deaths.
Beginning in 2015, New York City has experienced the emergence of fentanyl, which was
involved in nearly half (44%) of all overdose deaths by the end of 2016.
12
0
1000
2000
2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017
Number of deaths
Deaths From Overdose
Deaths From Suicide, Homicide, and Motor Vehicle Crashes
1,441 overdose deaths

9
Fentanyl: A public health crisis
Fentanyl is a highly potent synthetic opioid propelling drug overdose deaths to
record numbers. While fentanyl is a prescription medication used for cancer-related
pain or palliative care, non-pharmaceutical fentanyl has been introduced into illicit
drug markets in New York City and nationally in recent years. Typically, fentanyl
found in the illicit drug supply typically is not sourced from diverted prescriptions,
but rather is produced in illicit laboratories and used as a common adulterant to
heroin, cocaine, and counterfeit pills—including opioid analgesics, such as
oxycodone, and benzodiazepines, such as Xanax. The presence of fentanyl in illicit
drugs puts people who use them at enormously increased risk of overdose.
13
Fentanyl’s potency is such that a small amount can induce overdose; as a fast-acting
opioid, overdoses involving fentanyl can occur within minutes of ingestion.
14
Toxicology analyses indicate that fentanyl drove the increase in overdose deaths
from 2015 to 2016. Deaths involving fentanyl have increased nearly every quarter
since 2015, constituting almost half (44%) of all overdose deaths in 2016.
15
The acceleration of overdose deaths since the introduction of non-pharmaceutical
fentanyl in the New York City drug supply has brought a mutual recognition among
the public health and safety communities that new and different strategies must be
considered.
Many people who inject drugs in New York City are aware of the risks of fentanyl
and generally do not seek it out.
16
Typically fentanyl is introduced into illicit drug
mixes at the level of the supplier. As a result, people who use drugs and street-level
drug sellers are unlikely to know whether a certain product does or does not
contain fentanyl.
17, 18
Additionally, other non-pharmaceutical fentanyl analogues
may not yet be identifiable by existing laboratory tests.
Figure 3: Number of drug overdose deaths and percent of overdose deaths involving fentanyl in New York
City, by quarter, 2014-2016
Source: Paone D, Nolan ML, Tuazon E, Blachman-Forshay J. Unintentional Drug Poisoning (Overdose) Deaths in New York City, 2000–
2016. New York City Department of Health and Mental Hygiene: Epi Data Brief (89); June 2017.
0%
10%
20%
30%
40%
50%
60%
0
100
200
300
400
2014 2015 2016
Percent fentanyl
Number of
overdose deaths
Number of overdose deaths
Percent of overdose deaths involving fentanyl

10
Overdose affects all neighborhoods in New York City and cuts across lines of race, class,
age, and gender. However, certain populations and neighborhoods bear a disproportionate
burden of overdose deaths. Residents of both poor neighborhoods with endemic heroin-
related issues and affluent neighborhoods with more recent heroin- and fentanyl-related
issues experience some of the highest rates of opioid-involved overdose citywide. In 2016,
Staten Island and the Bronx experienced the highest rates of fatal overdose in New York
City in 2016 (31.8 and 28.1 per 100,000 residents, respectively), over two times higher
than residents of other boroughs. The largest numbers of deaths in 2016 occurred among
residents of the Bronx and Brooklyn, with 308 and 297 deaths, respectively. The breadth of
harm spans East Harlem in Manhattan, Hunts Point-Mott Haven in the Bronx, and South
Beach-Tottenville in Staten Island, as well as neighborhoods in other boroughs.
19
Taken
together, these numbers illustrate the widespread but unequal burden across the city.
Figure 4: Top five New York City neighborhoods: Rates of unintentional drug poisoning (overdose) involving
heroin and/or fentanyl by neighborhood of residence, 2016
Source: Paone D, Nolan ML, Tuazon E, Blachman-Forshay J. Unintentional Drug Poisoning (Overdose) Deaths in New York City, 2000–
2016. New York City Department of Health and Mental Hygiene: Epi Data Brief (89); June 2017.
Overdose death rates have increased dramatically among all racial groups from 2015 to
2016. In 2016, white New Yorkers experienced the highest rate (18.9 per 100,000) of
heroin- and/or fentanyl-related overdose death citywide, followed by Latino/a New
Yorkers (16.9 per 100,000); the rate among black New Yorkers was 12.3 per 100,000.
Rate of overdose deaths involving
heroin and/or fentanyl, 2016
0.0
10.0
20.0
30.0
(per 100,000 residents)

11
Although males experience rates of overdose from heroin and/or fentanyl over four times
that of females, both male and female New Yorkers experienced substantial fentanyl-driven
increases from 2015 to 2016.
Individuals who reside in shelters or are undomiciled are at increased risk of overdose.
These individuals represented 7% of the overdose deaths in New York City in 2016, despite
comprising less than 1% of the City population.
20
Overdose is now the leading cause of
death for this population, overtaking heart disease in FY 2014.
21
Furthermore, people who
inject drugs in public or semi-public locations, many of whom are homeless or unstably
housed, are at heightened risk of infectious disease transmission (HIV and hepatitis C) and
other harms associated with injection drug use.
22
,
23
2015 2016
White and Black race categories exclude Latino ethnicity.
Latino includes Hispanic or Latino of any race.
*Data for 2015 and 2016 are provisional and subject to change.
Source: Paone D, Nolan ML, Tuazon E, Blachman-Forshay J. Unintentional Drug Poisoning (Overdose) Deaths in New York City,
2000–2016. New York City Department of Health and Mental Hygiene: Epi Data Brief (89); June 2017
Number of overdose deaths
Figure 5: Increase in number of unintentional drug poisoning (overdose) deaths involving
heroin and/or fentanyl, by race/ethnicity, from 2015 to 2016*, New York City
9
.
Black
Latino
White
100
200
300
400
95
206
416
274
211
319

12
HealingNYC
Expanding New York City’s Response to the Overdose Crisis
In recent years, New York City has established itself as a national leader in addressing the
overdose epidemic through public health and public safety interventions. In March 2017,
the City committed an additional $38 million annually over five years to fight overdose
through HealingNYC, an innovative, multi-pronged agenda focused on four areas. In March
2018, the City expanded HealingNYC by an additional $22 million annually.
24
1. Prevent opioid overdose deaths
2009: DOHMH began to provide naloxone—a medication used to reverse the effects of an
opioid overdose—to syringe exchange programs and other registered opioid overdose
prevention programs for distribution to laypeople to carry and respond to overdose.
2013: The New York City Police Department (NYPD) equipped approximately 1,000 patrol
officers in the precincts with the highest rates of opioid-involved overdose with naloxone.
2014: The New York City Fire Department (FDNY) equipped emergency medical
technicians and certified first responder firefighters with naloxone. FDNY reported using
naloxone to reverse over 180 overdoses per month in the second half of 2016.
2014: Correctional Health Services, a division of New York City Health + Hospitals (H+H),
established one of the first jail-based naloxone distribution programs at the Rikers Island
Visitor Center. As of September 30, 2017, the program has distributed over 6,000 kits to
the families and friends of incarcerated persons, who are at elevated risk of overdose
following release from jail.
2015: The New York City Commissioner of Health authorized naloxone distribution by
pharmacists under a non-patient specific prescription (standing order), and the medication
is now available to laypeople without a personal prescription in over 725 pharmacies
citywide. Naloxone is now effectively available over the counter.
2016: The New York City Department of Social Services (DSS) trained all its shelter
providers in naloxone administration to ensure 24/7 overdose prevention coverage in the
City shelter system.
As part of HealingNYC, New York City committed to:
Distribute 65,000 naloxone kits in 100 services citywide, including, but not limited
to: treatment, detoxification, harm reduction, and other programs serving at-risk
New Yorkers and their families and loved ones
Equip all 23,000 NYPD patrol officers with naloxone and train all officers in
overdose response

13
Distribute 5,000 naloxone kits annually through the Rikers Island Visitor Center
program to directly target those individuals at increased risk
Increase the number of pharmacies offering naloxone without a prescription to
1,000
Distribute 6,500 kits in City shelters and continue to train Department of Social
Services shelter providers in naloxone administration
2. Prevent opioid misuse and addiction
2011: DOHMH developed New York City’s judicious opioid prescribing guidelines, which
served as the model for the guidelines issued by the Centers for Disease Control and
Prevention in March 2016. DOHMH’s guidelines subsequently were implemented in public
hospital emergency departments and private hospitals throughout the city.
2013: DOHMH employed public health detailing methods—delivering judicious
prescribing, overdose prevention, and door-to-door treatment messaging to health care
providers—to reach nearly 900 health care providers on Staten Island.
2015-2017: DOHMH expanded its door-to-door health care provider detailing efforts to
over 1,000 providers in the Bronx and nearly 1,000 providers in Brooklyn.
2016-2017: The City ran the “I Am Living Proof,” “Save a Life, Carry Naloxone,” and “I Saved
a Life” public awareness campaigns, its largest drug treatment and overdose prevention
public education campaigns to date.
2017: DOHMH launched Relay, a peer-based crisis intervention and overose prevention
service for individuals in emergency rooms following a nonfatal overdose event. At the
time of HealingNYC’s launch, the program was operational in four hospitals across the city.
As part of HealingNYC, New York City committed to:
Create mental health clinics in high-need schools to address youth substance use
and intervene early to prevent misuse and addiction before it starts
Deliver targeted prevention and treatment messaging in primary care settings to
communities at high risk of overdose
Train 1,500 clinicians annually in judicious opioid prescribing to reduce
overprescribing
Expand Relay to 15 emergency departments citywide

14
Public health detailing in New York City
Public health “detailing” campaigns deliver critical education and prevention
messaging directly to health care providers. Providers engage in one-on-one visits
with DOHMH representatives during which they receive educational messages
about the judicious prescription of opioid analgesic and benzodiazepine
medications and means to reduce patient risk of overdose. Judicious prescribing
messages recommend that prescribers utilize the lowest effective dose for the
shortest duration necessary to reduce the risk of overdose or other harms. Detailing
is a key component of the City’s prevention strategy, reaching providers to help
prevent substance misuse before it starts.
3. Connect New Yorkers to effective treatment
2007: Correctional Health Services, which operates the oldest jail-based methadone
maintenance treatment program in the nation (since 1987), first introduced
buprenorphine treatment to individuals detained at Rikers Island as part of a research
study. Rikers Island now offers access to both methadone and buprenorphine.
25
Like
methadone, buprenorphine is a medication that is highly effective in treating opioid use
disorder.
2016: DOHMH funded an innovative buprenorphine treatment model that supports nurse
care managers (NCM) in seven primary care organizations that run federally qualified
health centers. These NCM programs support primary care clinics and their clinicians to
provide comprehensive substance use care for patients with buprenorphine treatment.
As part of HealingNYC, New York City committed to:
Train an additional 1,500 health care providers in buprenorphine prescribing, with
a focus on engaging nurse practitioners and physician assistants, who are newly
eligible to prescribe buprenorphine under federal law
Expand the City’s nurse care manager for buprenorphine treatment model to
provide case management services and increased patient adherence to an additional
seven federally qualified health centers
Start addiction treatment and care management with buprenorphine prescribing in
all New York City H+H primary care clinics
Establish buprenorphine induction, the first phase of maintenance, in at least 10
New York City emergency departments
Embed buprenorphine maintenance treatment in up to seven harm reduction
programs
Transform the New York City H+H substance use care network into a system of
excellence in addressing harmful opioid use

15
Increase the daily number of patients in the New York City jail system receiving
methadone to 600 and buprenorphine to 150, and offer individualized treatment
plans and connections to care for these patients upon release
Engage health professional training programs and health systems leadership to
cultivate workforce readiness and optimize responses to treatment needs
Connect New Yorkers involved with the criminal justice system to substance use
services through the HOPE (Heroin Overdose Prevention and Education) Program
Connect New Yorkers with substance use and mental health problems to necessary
treatment services through by establishing Health Engagement and Assessment
Teams (HEAT)
4. Reduce the supply of dangerous opioids
2012: DOHMH and the New York/New Jersey High Intensity Drug Trafficking Area
launched New York City RxStat, a public health and safety working group comprised of
over 25 City, State, and federal agencies that share information about overdose and
strategize collaborative policies and interventions to reduce overdose death. RxStat has
been hailed as a leading national model by Former President Obama’s White House Office
of National Drug Control Policy and the United States Department of Justice.
2015: NYPD increased heroin seizures by 32% citywide.
2016: NYPD and the Staten Island District Attorney’s Office launched the Overdose
Response Initiative to investigate overdose deaths to rapidly identify dealers, dismantle
distribution operations, and provide assistance to families and friends of overdose victims.
As part of HealingNYC, NYC committed to:
Increase laboratory and technology capacity at the NYPD and Office of the Chief
Medical Examiner narcotics testing labs to identify new dangerous synthetic drugs
and target supply reduction operations
Expand the Overdose Response Initiative to more neighborhoods
Add NYPD personnel to New York City airports, highways, and ports to disrupt the
opioid supply at the level of trafficking

16
The continuum of care for people who use drugs
The identification, diagnosis, care, and treatment of substance misuse and substance
use disorders are part of a range of services available to people who use drugs.
Termed the continuum of care, these services span multiple health care settings,
from specific programs for substance use, like overdose prevention programs and
opioid treatment programs, to medical settings such as hospitals, emergency care,
and primary care that address individuals’ general health needs. Providing a range
of services with complementary goals and capabilities allows people who use drugs
to enter this continuum and receive care that matches their needs.
Primary care, emergency medical systems, and hospitals can effectively leverage their
high volumes of patient contact to identify substance use disorders and initiate
treatment—particularly medication for addiction treatment—among patients at
risk of overdose or other negative health outcomes. Practitioners in these settings
can treat the complications of substance use disorders and provide connections and
referrals to other parts of the continuum of care that would meet an individual
patient’s needs.
Treatment for opioid use disorder is most effective when it includes the use of
medication, termed medications for addiction treatment (MATs). The best-studied
medications are methadone and buprenorphine. Both medications have been shown
to decrease the risk of death from overdose and increase the likelihood of
individuals reducing or ceasing their drug use and improving their social and
economic lives. These medications can be used as long-term treatment depending
on individual need. Medications for addiction treatment also reduce the risk of
HIV/AIDS, chronic hepatitis C infection, other health problems, and even
engagement in criminal activity.
Harm reduction programs provide services and programing for people who use and
inject drugs. These programs may include but are not limited to syringe exchange
programs, support groups, and treatment services. Harm reduction programs aim to
serve people who use drugs by providing connections to support services, such as
housing, public benefits, education, or workforce programs.
Supervised injection facilities provide a space for people who use and inject drugs to
do so safely, in private settings with medical staff who can readily respond to an
overdose. SIFs reduce other risks associated with injection, such as bloodborne
disease transmission, and alleviate the threat of arrest and incarceration. On-site
medical, substance use treatment, and social services allow individuals to receive an
appropriate level of support.
17
A Legacy of Public Health Innovation
in New York City
The current opioid overdose epidemic is not the first drug-driven health epidemic to
necessitate an innovative public health response in New York City. New Yorkers have a
recognized history of national leadership in responding to substance use and associated
harms with scientifically grounded innovative approaches that protect public health.
1960s and 1970s
New York City experienced its first large-scale increase in injection heroin use in the
decades following World War II. By the 1960s, heroin-involved overdose was the leading
cause of death among New Yorkers between the ages of 15 and 35, with 75% of deaths in
this age group attributed to heroin overdose.
26
In response, the world’s first methadone
maintenance treatment program (MMTP) was established as a research pilot at Rockefeller
University in 1964. Methadone is a medication that prevents withdrawal symptoms and
reduces cravings for people with opioid use disorder. This groundbreaking pilot
demonstrated the efficacy and safety of methadone as a long-term maintenance therapy.
Over the next decade, MMTPs were institutionalized across the New York City health care
system and prescribed to approximately 34,000 patients. Scientific evidence and rigorous
evaluations indicating MMTPs’ association with decreases in overdose, drug-related crime,
and hepatitis transmission helped to push forward public and governmental acceptance
and propel the treatment toward wider use.
27
By the close of the 1970s, the heroin
overdose epidemic declined in large part due to the expansion of methadone maintenance
treatment.
28
While methadone maintenance is now widely accepted as the standard of care
for treating opioid use disorder, the intervention initially faced significant opposition.
However, the combined efforts of scientists, health care professionals, advocates, and
government led to the program that exists today. Approximately 30,000 people are
currently enrolled in methadone maintenance treatment in New York City.
1980s and 1990s
The second drug-driven epidemic New York City faced was the catastrophic rise of
HIV/AIDS in the 1980s and early 1990s. By 1984, an estimated 100,000 people who
injected drugs were infected with HIV in New York City, the highest disease concentration
among people who injected drugs in the United States.
29
Without access to sterile syringes,
HIV was spreading and people were dying at alarming rates, as sharing injection equipment
and paraphernalia greatly increases the risk of bloodborne disease transmission.
Advocates and health researchers identified lack of access to sterile syringes as a risk factor
in disease transmission and advocated for increased access to sterile syringes.
This collaboration resulted in the founding of syringe exchange programs (SEPs), now an
accepted public health intervention despite initially vehement opposition in the 1980s.
Opponents charged that syringe exchange programs condoned drug use and would lead to
increased drug use and crime in communities. However, evaluations of SEPs in Europe
18
indicated the contrary: SEPs led to reductions in community drug use and crime and, most
importantly, reductions in HIV transmission.
30
,
31
Despite the strength of this scientific
evidence, governmental opposition to syringe exchange continued in the United States.
Health advocates, unable to obtain licensure or approval to open a formalized service,
distributed syringes underground to quell the HIV epidemic.
32
By the early 1990s, the scientific evidence was overwhelming that syringe exchange
reduced HIV transmission. Proven effectiveness along with the mounting toll of AIDS,
which took so many lives, spurred government to action. In May 1992, after a decade of
advocacy by scientists and activists,
33
the New York State Department of Health adopted
emergency regulations to authorize the possession and distribution of syringes without a
prescription. This emergency regulation was adopted into law in October 1993, and the
first formal and legal syringe exchange pilot began in New York City, supported by a grant
from the Foundation for AIDS Research (amfAR). An evaluation confirmed the pilot’s
effectiveness in reducing risk behavior and HIV infection, with no documented increases in
injection drug use or negative impacts at the community level.
34
As evidence of the health
benefits of SEPs in New York City grew, more sites opened across the city and the scope of
SEPs expanded to offer a broad range of essential services, such as on-site medical care,
substance use treatment, and housing placements. By the late 1990s, these programs were
attributed with driving down the prevalence of HIV infection among people who inject
drugs, and further, reducing HIV transmission to sexual partners.
35
This momentum has
continued; in 2001 New York State implemented the expanded syringe access program to
make syringes available without a prescription in pharmacies and medical settings
statewide. Syringe exchange programs remain a significant contibutor to the overall
reduction in HIV cases in New York City.
36
Although syringe exchange has become institutionalized in New York City, the intervention
remains contested in some jurisdictions across the United States and to date remains illegal
in 23 states. Indiana—one state where syringe exchange is illegal—experienced an
outbreak of HIV infections in 2015 in rural communities of people who inject drugs.
Researchers quickly linked the outbreak directly to unsafe and unhygienic injection
practices. Deeply held opposition to syringe exchange among Indiana government officials
and national coverage of the outbreak reopened a public debate about the intervention.
Proponents urged state leaders to lift the ban on syringe exchange. Opponents eventually
permitted the practice temporarily on an emergency order from the governor. In the year
between detection of the outbreak and the opening of syringe exchange, nearly 200
individuals in Scott County tested positive for HIV, compared with only five HIV diagnoses
in the county between 2004 and 2013. Following the implementation of syringe exchange
in the affected counties, the pace of infection slowed and the outbreak was contained.
37
2000s and 2010s
The current opioid epidemic in the United States began more than 15 years ago, driven by
the aggressive marketing of opioid analgesic medications by the pharmaceutical industry.
The epidemic has escalated since 2010, particularly due to demand for heroin and more
recently the introduction of fentanyl into the illicit drug supply. As a result of fentanyl, drug
19
overdose deaths are at unprecedented levels nationally and in New York City. While new
health and safety resources have been devoted to overdose prevention at the local, state,
and federal levels, the sheer magnitude of this epidemic has compelled scientists, health
experts, professional societies, and advocates in the United States to reassess how to
address substance use. Among the range of additional strategies under discussion are SIFs,
which have been shown to reduce overdose deaths in people who are most vulnerable,
including people who are unstably housed.
38
Supervised injection facilities were established in Europe in 1992. This model has been
adopted widely in Europe—initially in Switzerland, Germany, and the Netherlands—as
well as more recently in Australia and Canada. Supervised injection facilities now operate
in more than 10 countries. Abundant scientific evidence supports the effectiveness of SIFs
to reduce deaths and other health consequences of injection drug use while facilitating
access to the continuum of care. At the same time, the data refutes concerns that SIFs
would cause increases in drug use or crime. Based on this information, many advocates and
professional health bodies publicly support the establishment of SIFs and ask that local and
state governments implement this strategy as a lifesaving measure. In response, legislation,
new policy, or studies are in progress in Colorado, Maryland, Maine, Massachusetts, New
York City and Ithaca, Philadelphia, San Francisco, and Seattle.

20
WHY SUPERVISED INJECTION
FACILITIES?
A Review of the Evidence
Supervised injection facilities are one of many overdose prevention strategies available to
public heath authorities. They have been shown to improve individual and community
health, increase public safety, and reduce the health and social consequences of injection
drug use through medically supervised use of injected substances. Supervised injection
facilities offer hygienic spaces where people who inject drugs can inject pre-obtained
substances with sterile equipment. Medically trained staff are on-site to respond to
potential overdose events, although these staff do not assist with injection. Most
established SIFs refer or provide access to a host of on-site health, mental health, substance
use, and social services that supplement existing harm reduction and syringe exchange
services through increased opportunities for engagement, education, and treatment.
Approximately 100 SIFs operate in 10 countries and 67 cities worldwide, with six
additional facilities scheduled to open across Europe and Canada over the next two years.
39
Although no SIFs exist in the United States, a number of jurisdictions have announced
intentions to open or explore the possibility of opening these facilities, including Colorado,
Maryland, Maine, Massachusetts, Seattle, San Francisco, and Ithaca, New York.
A growing body of scientific evidence, generated primarily though evaluations of existing
facilities, suggests the safety and effectiveness of SIFs. To date, no fatal overdose has been
documented in a SIF anywhere in the world.
40
,
41
Supervised injection facilities reduce overdose mortality and associated harms
Community impact studies conducted in Vancouver, Canada, have found reductions in fatal
overdose of up to 35% in communities where SIFs are located.
42
Evaluations of a SIF in
Sydney, Australia, have demonstrated reductions of up to 80% in overdose-related
emergency medical service calls in areas surrounding SIFs.
43
The safe and “low-threshold”
*
access to safer injection, overdose prevention, health care, and drug treatment services
provided by SIFs are associated with decreases in risk-taking behavior among consistent
SIF visitors and reductions in the harms associated with public injection.
44
Supervised injection facilities improve access to health care and social services
People who use drugs may face stigma that can create barriers to accessing medical and
mental health care and social services.
45
By offering on-site medical services, SIFs increase
access to routine primary care for people who inject drugs and facilitates linkages to
ancillary services.
46
,
47
Evaluation of Vancouver’s SIF found that on-site and referred
*
That is, minimal barriers to entry, free, and with few or no demands on the individual in exchange for the
service.
21
medical services provided to SIF visitors reduced the length of their hospital stays and
improved overall health.
48
Supervised injection facilities reduce injection-related health risks
By providing sterile injection equipment and a safe space to inject, SIFs can further reduce
transmission of bloodborne infections, including HIV and hepatitis C (HCV). Conservative
estimates from Vancouver suggest that a single SIF can prevent up to 35 new cases of HIV
per year.
49
,
50
Supervised injection facilities also have been shown to reduce bacterial
infections associated with non-sterile injection equipment.
51
Supervised injection facilities,
as well as syringe exchange programs, educate clients about safer injection techniques and
proper syringe disposal, which disseminate through networks of people who inject drugs
and can lead to increased community use of safe and hygiene techniques.
52
Research
indicates that individuals who inject in public or semi-public locations are at heightened
risk of injection-related health complications since their injection is often rushed out of fear
of being sighted, interrupted or arrested. Rushed injections increase risks of using non-
sterile equipment, developing and spreading infections, and overdosing. As the majority of
individuals who inject publicly are homeless or unstably housed,
53
,
54
SIFs are particularly
well-suited to meet the needs of this high-risk and underserved population.
Supervised injection facilities increase referrals to drug treatment
Supervised injection facilities, like other harm reduction services, have been shown to
increase referrals to and uptake of drug treatment and detoxification and, over time, are
associated with drug use cessation.
55
-
57
These findings serve as an important reminder that
SIFs, harm reduction, and treatment are all points along a continuum of care for people
who use drugs.
Supervised injection facilities provide outreach, engagement, and care to
marginalized populations
Supervised injection facilities function as spaces to engage and connect marginalized or
disconnected populations with health care, harm reduction, and other social services.
Research has demonstrated that SIFs may function as safe havens for women who inject
drugs, thereby reducing violence against women associated with street-based drug use.
58
Similar findings have shown increased engagement with homeless or unstably housed
young adults, a group at elevated risk of overdose and infectious disease transmission.
59
Supervised injection facilities reduce health care expenditures
Evaluations of SIF sites worldwide have demonstrated annual savings of up to $3.5 million
per site in averted HIV and HCV treatment costs.
60
Other estimates suggest savings of up to
$18 million over a 10-year period based on the number of averted overdose deaths.
61
Supervised injection facilities do not increase crime or drug use
A number of studies, reviewed below, have examined whether SIFs have negative effects on
communities, including increased crime, drug use, or concentrations of people who use
drugs in the neighborhood in which a SIF is located. The potential for SIFs to have negative
effects on communities is one of the most frequent concerns raised.
22
Some opponents of supervised injection have suggested that SIFs increase drug-related
crime in areas where they are located. While this may seem like an intuitive conclusion
given that drug use remains illegal in the United States, research from Vancouver, Canada,
observed decreases in a range of drug-related crimes following the establishment of a SIF,
including decreases in drug sales, drug solicitations, and public injection.
62
Research from
Sydney, Australia, demonstated decreases in public perception of public injection,
discarded syringes, and drug-related crime.
63
Other studies evaluating the effects of SIFs on
their surrounding communities in Sydney have shown declines in vehicle break-ins and
auto theft and neutral effects on levels of drug trafficking, assault, or robbery in
communities with SIFs.
64
,
65
Opponents of SIFs have also suggested that these services promote drug use and
discourage treatment. However, evidence from Vancouver, Canada, suggests that SIFs
reduce drug use in neighborhoods where they are located, by providing engagement and
connections to harm reduction and drug treatment services.
66
SIFs can serve as an entry
point into the continuum of care and lead to reductions in drug use and drug-related health
and social consequences.
67
As reported above, SIFs increase participation in drug
treatment and are associated with long-term drug use cessation.
68
,
69
Additionally, some opponents of supervised injection facilities have suggested that these
services may facilitate initiation into substance use or substance use injection, particularly
among youth. Like syringe exchange programs, most SIFs are not accessible to individuals
under age 18. Research has shown, however, that the majority of SIF clients are long-term
injectors, with an estimated average injecting history of 16 years.
70
Additionally, SIFs
reduce the number of publicly-discarded syringes in communities where they are located
and thus reduce community exposure to injection drug use.
71
,
72
This reduced community
exposure to drug use can function as a prevention measure, particularly as SIFs are often
situated in areas with high concentrations of public drug use, drug-related activity, and
crime.
Opponents of SIFs have expressed concerns that these services may draw large numbers of
people who use drugs into communities where they don’t live. However, research has
shown that the majority of individuals who use SIF services are not likely to travel more
than 20 minutes to a given facility.
73
-
76
Existing SIFs have been located in areas with high
densities of drug use and overdose and function as a targeted health intervention for these
communities. Furthermore, this same concern arose in reaction to the early
implementation of syringe exchange programs and was disproved through evaluation of
SEPs.
23
WOULD NEW YORKERS SUPPORT
SUPERVISED INJECTION FACILTIES?
Community Support for and Concerns about Supervised
Injection
To assess the opinions of key stakeholders regarding the feasibility of opening a supervised
injection facility in New York City, the New York Academy of Medicine (NYAM) and the
New York City Department of Health and Mental Hygiene (DOHMH) jointly conducted a
community assessment. The assessment included focus groups and interviews with a range
of key stakeholders across the city. Findings are limited to those who agreed to participate
in the focus groups and interviews; several key stakeholders who have been vocal critics of
supervised injection were unavailable at the time of the study. Additional engagement is
need to best capture all community perspectives. An Expert Advisory Panel comprised of
national and international experts in supervised injection—including leading
epidemiologic and economic researchers, experts in drug policy and law, and advocates—
drew on research and implementation exertise to help identify stakeholder groups and
provide input into the study design and interview materials. A list of Expert Advisory Panel
members can be found in the Acknowledgments.
The assessment occurred in two parts. First, focus groups were conducted with a total of 52
people who use drugs to investigate if and how a SIF could meet the needs of this unique
and at-risk population in New York City. These focus group participants were asked about
their willingness to use a SIF, preferences regarding the types of services offered,
suggestions about the operational components of a facility, and perceived benefits and
concerns about SIFs.
Second, focus groups and individual interviews were conducted with a range of
stakeholders across New York City, including:
Elected officials
Law enforcement officials
Health care providers
Community leaders
Faith leaders
Business community representatives
Harm reduction program staff and management
The interviews and focus groups with the above stakeholder groups—which captured the
perspectives of 71 individuals separate from the sample of people who use drugs—aimed
to solicit opinions regarding community need for supervised injection services, gather
concerns about possible health or safety consequences that may be associated with a SIF,
and identify operational components of a SIF that communities consider essential.

24
Findings from both sets of focus groups and interviews are presented below.
People who use drugs: Perspectives on supervised injection
Between December 2016 and March 2017, researchers from NYAM conducted six focus
groups with a total of 52 people who use drugs. Participants were recruited from harm
reduction programs in the Bronx, Brooklyn, and Manhattan. Researchers obtained
informed consent from all individuals prior to participation. Focus groups were conducted
anonymously and confidentially; no identifying information was obtained. Focus groups
were audio-recorded and fully transcribed for analysis. Participants received a $25
honorarium for their time.
At the beginning of each focus group, participants completed a short written demographic
questionnaire—the results of which are presented in Figure 6. Following the demographic
survey, researchers provided an overview of SIFs, including photographs and/or videos of
existing facilities to demonstrate what SIFs look like in practice. Researchers utilized an
open-ended interview schedule to guide the remainder of the focus group. Interviews
broadly probed: participant perceptions on supervised injection facilities, including
individuals’ willingness to attend or consider attending such a facility; operational aspects
of supervised injection facilities, including facilitators and barriers to access; and perceived
benefits and concerns about SIFs that might affect people who use drugs.
Figure 6: People who use drugs, demographic characteristics (n=52)
Total
52
100%
Age
18-30
8
15%
31-40
14
27%
41-50
19
37%
51-60
8
15%
60 & older
3
6%
Gender
Male
35
67%
Female
15
29%
Transgender
1
2%
Gender non-conforming
1
2%
Race/Ethnicity
White
11
21%
Black/African American
7
14%
Latino/a
22
42%
Multi-racial
10
19%
Other
2
4%
Housing status
Own home
14
27%
Other’s home
13
25%
Unstably housed
*
17
33%
Street homeless
8
15%
*
Could include: shelter, single room occupancy (SRO) facility, drug treatment facilty, supportive/transitional/three-quarter housing, or
hospital

25
Figure 7: Supervised injection facility, Vancouver, Canada
Photo courtesy New York Academy of Medicine
Three themes emerged during analysis of the focus group data: health and safety benefits;
site design and service integration; and community stigma.
Health and safety benefits
A number of participants discussed the fear they experience while injecting in public: fears
of being seen, interrupted, or arrested; and notably the fear of death due to injection alone
or in a clandestine location. Many participants considered supervised injection a viable
means of alleviating that fear.
“You have staff there that’s going to look out for you and make sure that you don’t overdose.
In your own car, you can overdose and nobody is there.”
—Person who uses drugs
Participants also described SIFs as potential safe spaces for people at risk of victimization,
including women and homeless people. This function of SIFs was of particular importance,
as some participants had experienced victimization as a result of high-risk public use. The
covert nature of public injection demands that individuals rush the injection process, which
can lead to injury or further harm. Participants perceived supervised injection facilities as
one means to prevent rushed injection.
“I think supervised injection is excellent for people that are homeless don’t have nowhere to
go. They’re constantly going to bathrooms and going, you know, places where they’re not
welcome. People don’t make them welcome. People barging in, and sometimes it’ll hurt. There
are injuries to your arm or something.”
—Person who uses drugs

26
Additionally, participants emphasized that, contrary to popular perception, people who use
drugs care very much about their health and share information regarding health issues
within their drug-using social networks. Many participants framed SIFs as a means of
bringing together a community striving toward health.
“It gets very macabre and lonely to be alone and shooting up, drinking. . . Having a place to go
where there's others around me, it could be uplifting and not only save my life if I were to
overdose, but save my life in other ways.”
—Person who uses drugs
Service integration and site design
Participants overwhelmingly emphasized the need for any supervised injection facility to
offer on-site or linkages to health care and supportive social services. Noting that SIFs
would target people who inject drugs publicly, participants—many of whom were street
homeless or precariously sheltered—described access to housing and basic medical and
psychiatric services as a critical component of a SIF.
“Safe injection, safe needles, doctors, psychiatrists, case workers, housing. The SIF has to
incorporate those in, you know, to make things work.”
—Person who uses drugs
Regarding site design, participants discussed a need for consistent operational hours to
engage and build rapport with clients as well as encourage regular service use. Early
morning operating hours were presented as necessary to facilitate withdrawal
management for people who use opioids. Late night hours were suggested as preventive
safeguards against sexual assault and other forms of violence—particularly violence
against women—that may more likely occur at night.
77
“Being a female, I would personally prefer something with middle of the night hours, that
would be the ultimate safe place for me. I don’t know how strong it is what I’m using. I don’t
know how my body is going to react to that particular shot. I really would like to be
somewhere totally safe, specifically within the you know timeframe of like, you know, 12 to
five, 12 to four. “
—Person who uses drugs
Community stigma and resistance
Most participants anticipated opposition to supervised injection facilities within their
communities, with many individuals linking this perceived opposition to pervasive stigma
against people who use drugs. Most participants recounted personal experiences of stigma
associated with their drug use from family members, medical providers, community
members, or even strangers. The stigma these marginalized individuals described led them
to a reflexive assumption that the community would be opposed.
“Stigma is life. Stigma is real. We stigmatize each other and we don’t even realize it. And
that’s a shame, because we get enough from society, you know what I’m saying. We really

27
need to be very mindful about the words that we use and the way that we refer to somebody
who is just as human as the next person. Whether I use or not is irrelevant.”
—Person who uses drugs
New York City stakeholders: Perspectives on supervised injection
Between January and December of 2017, six focus groups and 39 individual interviews
were conducted with a total of 71 stakeholders representing the following disciplines,
backgrounds, and interests: State and local elected officials; law enforcement officials;
health care providers specializing in psychiatry, primary care, emergency medicine,
correctional health, addiction medicine, infectious disease, and pharmacy; faith leaders
representing the Buddhist, Christian, Islamic, and Jewish traditions; business leaders and
small business owners; harm reduction program staff and management; and local
community leaders. A breakdown of stakeholders by category is presented in Figure 8.
Figure 8: New York City stakeholders (n=71)
Business leaders and small business owners
8
Elected officials
8
Faith leaders
8
Harm reduction staff and management
23
Health care providers
7
Law enforcement officials
7
Local community leaders
10
Stakeholders were solicited for interviews by representatives from DOHMH and/or NYAM,
and all interviewees were assured of both organizational and personal confidentiality.
Focus groups and interviews were conducted using a structured interview guide that
probed perceived benefits and harms to communities and individuals that may result from
SIFs, as well as opinions on what features or services would be crucial to include in a
potential SIF. Consistent with the interviews with people who use drugs, at the start of the
interviews stakeholders were presented with background information about SIFs, which
included a fact sheet with results from studies and evaluations of SIFs worldwide and
photographs and/or videos of existing facilities. Audio recording was used at the
researchers’ discretion. At every interview, a designated scribe took detailed notes.
Demographic information was not collected at stakeholder interviews, and stakeholders
did not receive compensation.

28
Figure 9: Supervised injection facility, Sydney, Australia
Photo courtesy New York Academy of Medicine
Four themes emerged during analysis: health benefits; safety benefits; safety and
community concerns; and site design and community integration.
Health benefits
Across all stakeholders, there was broad agreement that reducing fatal overdose was a
critical need for their communities and New York City. Stakeholders generally
acknowledged the seriousness of the overdose crisis and the need for new solutions.
Regardless of whether stakeholders felt that SIFs were right for New York City, they nearly
all acknowledged that supervised injection is one evidence-based public health strategy
that could help avert overdose deaths.
“The idea of SIFs is creative but scary. A part of me says this is the wrong direction, but not
really, because there are so many people dying and in need.”
—Elected official
Some stakeholders—health care providers and harm reduction program staff, in
particular—viewed SIFs as an important step along the continuum of care for people who
use drugs and believed that engagement with these services could help individuals move
toward stability, health, and well-being. A number of health care providers considered SIFs
particularly important for individuals who might not be ready to fully curtail their drug use
and would otherwise be excluded from programs for which abstinence is a requirement.
Stakeholders who expressed this opinion generally viewed SIFs as an effective form of
overdose prevention and patient engagement—a way to keep people who use drugs alive
so that they may one day access treatment

29
“I think what people find the most challenging about caring for people who use drugs, is that
our [health care facility’s] model doesn't allow for continued drug use to be in care with us.
And so, we have to sometimes coerce or force a model onto a patient that isn't where they're
at in order for us to stay in a relationship.”
—Health care provider
Safety benefits
A number of stakeholders described a need for services that would reduce public injection
and publicly discarded syringes, which they viewed as hazards to public safety. Most
agreed that SIFs were one strategy to achieve these goals. The issue of community safety
was particularly salient among members of the business community, a number of whom
described some of the prior problems they had experienced with public injection and
public overdose in local places of business. These individuals were primarily interested in
whether SIFs would reduce high-risk drug use occurring in public and semi-public settings,
with many expressing the belief that moving public use into a private setting under medical
supervision would benefit both the community and the individual using the drugs.
“Often, a barista will be [at the café] by themselves at night, and [a person who injects drugs]
will use the bathroom, and then they'll sit down in the café and usually just be falling asleep or
nodding out. It's of concern because the staff isn't equipped to deal with that, and it's
upsetting to other customers, but it's also a concern to the person's health. I think that [a SIF]
is the best possible solution.”
—Small business owner
Some law enforcement officials viewed SIFs as potential cost-saving tools. When provided
with the evidence demonstrating localized decreases in both public drug use and
associated nuisance crimes following the establishment of a SIF, these stakeholders framed
the intervention in pragmatic, monetary terms. Even if they held reservations about
supervised injection, the possibility of reduced crime and criminal justice expenditures
functioned as a convincing argument for support.
“If SIFs give us less crime, less public drug use, and less vulnerability among drug users, police
will save enforcement resources. We need to enforce the law, but we also need to try things we
haven’t before.”
—Law enforcement official
“At the end of the day, it’s about serving the people. People who use drugs are real people with
real needs.”
—Elected official
Safety and community concerns
While concerns about SIFs were most frequently offered by law enforcement, all
stakeholders highlighted potential community concerns. First was the concern that
supervised injection could be perceived as condoning injection drug use, which remains
30
illegal in New York State. Some stakeholders framed the implementation of SIFs as
potentially negligent, given the increased overdose risks posed by fentanyl.
“I’m concerned that we’re arming people with the potential to kill themselves. The X factor is
what’s in the needle.”
—Law enforcement official
“We spend a lot of time trying to convince people that addiction is an illness. SIFs are almost a
bridge too far. It could have a terrible backlash.”
—Law enforcement official
Other stakeholders raised the concern that areas around a SIF might create new drug
markets in known locations and create geographic concentrations of people who inject
drugs. This perception could lead to challenges with SIF placement and generate pushback
from community members on the grounds that SIFs might bring new people who inject
drugs into their neighborhoods.
“Automatically you’ll have a fear issue. ‘Don’t you dare put that in my backyard.’ Needles?
They’ll say, ‘Oh my god, they’re bad people.’ Not that ‘people who use drugs are suffering.’”
—Local community leader
A handful of stakeholders raised the concern that their communities feel overburdened by
services for vulnerable populations and noted that community members were likely to
oppose a SIF on that basis. These stakeholders emphasized that their communities had
entrenched problems with regard to affordable housing, homelessness, workforce
development, and education that, for some individuals in their neighborhoods, might
supersede the needs of people who use drugs. Stakeholders emphasized that SIFs could
garner support in some communities by addressing some of these needs in addition to
offering overdose prevention and drug use services.
“It’s going to be hard to convince people that it works. We can’t even put supportive housing
in the neighborhood, because of the stigma surrounding the people who might occupy it.”
—Elected official
Some stakeholders, particularly more experienced elected officials and harm reduction
professionals, connected the current national debate about supervised injection with the
history of syringe exchange programs. These stakeholders recollected that similar concerns
were discussed widely in advance of the formal implementation of SEPs in the 1990s. They
noted that the political risk taken to implement SEPs ultimately benefitted the health and
safety of both individuals who use SEPs and their broader communities by reducing HIV
transmission.
“We don’t want to replicate the battle we fought about needle exchange. We need to educate
the public about the benefits: HIV reduction and overdose prevention.”
—Elected official

31
Site design and community integration
The majority of stakeholders suggested integrating supervised injection into established
harm reduction facilities rather than launching new facilities. They described a number of
perceived benefits of co-location within harm reduction programs: established credibility,
relationships, and trust with the surrounding communities and law enforcement; existing
on-site buprenorphine treatment services; existing on-site health and social services to
provide care and expedite and ease referrals; and existing expertise about injection drug
use and compassion for people who use drugs. Some stakeholders also suggested that
integration into harm reduction services could help assuage the concern that SIFs would
draw new people who use drugs to their neighborhood, as there is a substantial anticipated
overlap in use between syringe exchange and supervised injection.
“It’s a perfect idea to have the SIFs in the back and have the rest of the services out front.
Whatever people need they can just get.”
—Harm reduction professional
Stakeholders overwhelmingly agreed that a successful SIF ought to include co-located
health and social services. Individuals who are homeless and people who inject drugs in
public often are disconnected from health care, substance use treatment, housing, and
broader social services. Co-locating these services within SIFs would allow immediate
connections to be made. In particular, as SIFs sit at the early engagement end of the
continuum of care for people who use drugs, on-site or immediate access to drug treatment
services would allow individuals who feel ready to reduce or cease drug use to do so
immediately.
“We can’t just say over and over what a tragedy overdose is and do nothing about it. I like the
idea of a holistic approach to help people try to get better.”
—Law enforcement official
Nearly all stakeholders agreed that the success of a SIF was predicated on proactive
relationship-building between harm reduction program staff, medical providers, law
enforcement, and local community groups. This would involve preparatory outreach with
local police precincts to provide education on basic tenets of harm reduction and the
intended function and goals of the planned SIF. A successful model for this outreach exists
as part of the trust-building that has occurred between SEPs and local law enforcement.
Likewise, the SIF planning process must acknowledge, consider, and incorporate the needs
of police working with people who use drugs. A broad coalition of the stakeholders in this
assessment should be involved early in the planning and implementation processes for
establishing a SIF.
“I would welcome this in my district, but the community engagement piece is critical. You
need to start laying the groundwork now, because this will be contentious.”
—Elected official
32
“Are you going to find resistance? Yes. Are you going to need to educate? Absolutely. It will be
important to emphasize SIFs as one of many approaches to prevent overdose deaths.”
—Local community leader
33
WHAT WOULD NEW YORK CITY GAIN
FROM SUPERVISED INJECTION
FACILITIES?
Estimating the Health and Fiscal Impacts of Supervised
Injection in New York City
Weill Cornell Medical College conducted a study to estimate the overdose prevention and
public cost saving impacts of supervised injection in New York City. The study aimed to
develop neighborhood-specific estimates for overdose deaths prevented, given the wide
variation in mortality among different neighborhoods. Short-term cost savings estimates
were developed by identifying key areas of public health care expenditures that could
experience reductions from SIFs, including emergency medical services, emergency
departments, and inpatient hospitalizations. A brief review of the estimated impact is
presented below. Full text of the report prepared by Weill Cornell, including the methods
and results, can be found in Appendix B.
As part of the planning and execution of this impact analysis, a Technical Advisory Group of
five global experts in supervised injection provided guidance to Weill Cornell on methods,
analysis, and findings at key intervals across the life of the study between March and June
2017. Members of the Technical Advisory Group contributed a range of expertise across
economics, policy analysis, and the clinical and behavioral sciences. All members have
extensive experience in the evaluation of SIFs internationally.
To generate the the number of overdoses avoided, researchers developed a model that
accounted for the neighborhood-level number of death and the proportion of people who
inject drugs who are willing to travel to and use a SIF, drawn from the New York City
Injection Drug User Health Alliance Survey, 2013-2014 and 2014-2015. They used this
model to estimate the impact of up to four supervised injection facilities on opioid
overdose fatalities, assuming unrestricted hours of operation and capacity. Additionally,
researchers estimated the direct health care cost savings in New York City. Using New York
City data of emergency department visits and hospitalizations, and emergency services
costs, researchers developed a model of direct health care costs saved by implementation
of a SIF. Where data was unavailable, best estimates from the literature were used.
Findings from the study suggest that implementing supervised injection would contribute
to reductions in overdose mortality and savings in direct health care expenses.
34
Supervised injection facilities could prevent between 67 and 130 overdose
deaths annually in New York City
Conservative estimates indicate that establishing supervised injection services in four of
the neighborhoods with the highest rates of overdose death would prevent between 67 and
130 overdoses annually, dependent on the number and location of SIFs established.
Opening a single SIF in the neighborhood with the highest rate of overdose death citywide
is projected to prevent between 19 and 37 opioid overdoses annually. These lives saved
would represent a substantial reduction in the overall impact on citywide overdose. Given
that the estimates presented here are conservative, it is possible that reductions in
overdose will exceed these estimates.
Supervised injection facilities are designed to serve individuals most in need. Individuals
who are homeless or unstably housed may be most likely to inject in public or semi-public
settings. In New York City, people who are homeless die of overdose at a rate more than six
times that of the general population.
78
As SIFs directly target this group, it is likely that the
projected reductions in overdose would in large part benefit people who inject drugs, are
homeless, and are marginalized for other reasons.
Supervised injection facilities could save between $1 and $7 million annually in
New York City direct health care expenditures
Opioid overdose costs the New York City health care system an estimated $50 million
annually on emergency medical service calls, emergency department visits, and
hospitalizations. Establishing a single SIF in a neighborhood heavily affected by opioid
overdose could save the City $1 million annually in direct health care expenses.
Establishing four SIFs in the most impacted neighborhoods could save up to $7 million
annually in avoidable acute health care costs. Acute health care is short-term treatment of
severe or brief illnesses and injuries, as opposed to chronic care which involves long-term
treatment of ongoing conditions. Estimates suggest that SIFs could generate $4 to $6
million in annual net savings.

35
The above estimated cost savings to the health care system are conservative, as additional
areas of substantial anticipated cost saving were not included due to limitations in New
York City-specific health data. However, evaluations of SIFs from other jurisdictions have
shown additional savings drawn from the following public benefits:
Supervised injection facilities reduce HIV and HCV treatment costs by preventing
transmission through access to safe and sterile injection services.
79
Supervised injection facilities connect individuals to cost-effective addiction
treatments.
80
Treatment with methadone or buprenorphine has been demonstrated
to reduce overdose and the financial burden of overdose.
81
Supervised injection facilities reduce the high cost of treating skin and soft tissue
infections associated with unsafe injection practices. Skin and soft tissue infections
are prone to complications and often require lengthy and costly hospital admissions
to treat successfully.
82
The anticipated $1 to $7 million saved excludes the law enforcement and criminal justice
costs associated with overdose response.
Operating a supervised injection facility could cost a minimum of $250,000
annually
DOHMH estimated the operating costs of a supervised injection facility, considering
staffing, supplies, and siting. Locating a SIF within an existing harm reduction service
Up to
$7 million
Up to
130 overdose
deaths
36
would require substantially lower costs than a freestanding facility, given that this
configuration could eliminate the majority of new overhead and leverage existing and
funded on-site services, treatment, and referral networks. In this estimate, a SIF would
require annual costs between $250,000 and $500,000, depending on hours of operation,
and service and staffing models.
Opening a new, freestanding facility would demand substantially higher operating costs. In
this estimate, a SIF could require annual operating expenses of up to $2 to $3 million, most
of which are associated with infrastructure and capital costs.

37
HOW COULD NEW YORK CITY
IMPLEMENT SUPERVISED INJECTION
FACILITIES?
Viable Legal Frameworks for Supervised Injection Facilities
in New York City
To evaluate potential legal pathways and challenges to SIFs in New York City, Columbia
Law School Associate Professor Kristen Underhill conducted a review of relevant federal,
state, and municipal criminal and civil laws and regulations. A summary of legal issues
relevant to the establishment or operation of SIFs in New York City is presented below. Full
text of the legal review can found in Appendix C.
Despite the growing recognition and support in public health for the need for expanded
harm reduction services to help reverse the course of the opioid epidemic, federal and state
criminal laws present significant risks to the operators of SIFs. The clearest avenue for
establishing SIFs would be to changes federal law to allow SIFs to operate and provide SIF
clients, staff, and owners with exemptions from federal criminal law. Nevertheless, state
legislation or administrative action would also offer some protection, but still leave clients,
staff, operators and landlords of SIFs vulnerable to federal prosecution.
Existing Federal legislation
The Federal Controlled Substances Act (CSA) poses a number of constraints to operating a
SIF, including its prohibitions on individual drug possession and on organizations or spaces
that facilitate drug use (colloquially known as the “crack house statute”).
83
Supervised
injection facility clients, operators, and staff could be at risk of arrest and prosecution
under the CSA, although the enforcement of these statutes are at the discretion of federal
authorities. Penalties may include fines of up to $500,000 for individuals, $2 million for
institutions, and imprisonment. In addition, any property used to commit a CSA violation is
subject to forfeiture, that is, the property could be transferred to the U.S. Attorney General,
who may then sell it or transfer it. Professional staff licensed by the state are also at risk of
disciplinary proceedings if convicted of a federal or state felony. No federal prosecutions of
harm reduction facilities on the basis of participants’ on-site drug use have occurred under
the CSA to date.
A state or locally sanctioned program that explicitly supervises drug consumption would be
a legal first in the United States, and it is difficult to predict how federal prosecutors might
respond. Additionally, federal agencies and Congress have the authority to prevent the use
of federal funding to support SIFs, although no such restrictions exist currently.
84

38
State legislation
The New York State Legislature has the authority to authorize SIFs by statute, and could do
so either with a freestanding law, or with an extension to the current state law authorizing
SEPs.
†85
Although state legislation would not safeguard SIFs against the Federal CSA, the
state legislative pathway provides the greatest legal security with respect to state and local
law. Legislation authorizing a SIF could simultaneously amend or provide exemptions from
state laws on possession, paraphernalia, criminal injection, criminal nuisance, and
professional misconduct to protect SIF staff, owners, and clients from arrest, prosecution
and disciplinary proceedings in the state. Even if the authorizing legislation did not
explicitly amend existing criminal laws, statutory support for a SIF ought to deter arrest
and support strong defenses for SIF clients, personnel, and owners who might be criminally
charged.
86
Statutory authorization under state law could also provide some protection
from local efforts to declare SIFs a public nuisance, or to find SIF clients in violation of local
laws such as Administrative Code § 10-203.
Recognizing this potential, New York State Assembly bill A.8534 was introduced in June
2017 to authorize SIFs statewide.
87
The proposed legislation—currently under health
committee consideration—would permit local health authorities to set and maintain SIF
operating and reporting standards. In addition to New York, several other states have
considered or are considering legislation authorizing SIFs, including California,
88
Colorado,
89
Maryland,
90
Maine,
91
and Massachusetts.
92
No bill has passed both houses of
any state legislature to date.
State administrative action
The New York State Governor or New York State Commissioner of Health could establish
SIFs through executive authority. Provisions in New York State law grant administrative
authority to the Governor to direct funds for programming in the event of a disaster.
Similarly, the New York State Commissioner of Health holds the authority to provide
treatment, supplies, and services to residents in the event of a statewide medical
emergency.
93
The scope of the opioid overdose epidemic in New York and the recent
acceleration of mortality caused by the introduction of fentanyl likely would justify the
declaration of a disaster or state of emergency and initiate SIFs. There is historical
precendent for such an approach in New York State, as the State Department of Health used
such a emergency regulation in 1992 to successfully establish syringe exchange programs
in response to the HIV/AIDS crisis.
Executive or agency action would be open to the risk of challenge as contrary to state
criminal laws, and it is unknown how New York State and federal legislators and
prosecutors might respond to such an administrative directive. However, the emergency
health action taken by New York State to establish SEPs went unchallenged by federal
†
Although possession of controlled substances remains illegal in New York State, syringe
exchange program participants are allowed to possess trace amounts of illegal drugs in
used syringes, an exception to the law established to facilitate SEP use and reduce
transmission of HIV and other bloodborne diseases.

39
authorities in the 1990s; ultimately syringe exchange programs were authorized by state
law in 1993.
94
As with SEPs, State administrative action to establish SIFs may also go
unchallenged.
Local legislation or administrative action
The New York City Council could establish a SIF through City law.
95
A city law authorizing
SIFs may be found by the courts to conflict with state criminal laws leaving SIFs established
by it vulnerable to state prosecutions. The local law option would also leave providers
uncertain about professional disciplinary proceedings which are also governed by state
law.
Local legislative action would need to consider local nuisance codes that criminalize
individuals or organizations that “knowingly allow” drug use in a given location.
Enforcement of these codes is at the discretion of state prosecutors, and establishment of a
SIF through City ordinance may be vulnerable to challenge by state and federal law
enforcement. However, evidence from other jurisdictions indicates that SIFs reduce
nuisances associated with public injection and overdose, reducing the likelihood of
prosecution on nuisance grounds.
Additionally, the New York City Charter grants the New York City Mayor and DOHMH the
authority to establish emergency services during short-term crises.
96
Should the City define
the overdose epidemic in these terms, DOHMH could establish one or more SIFs.
Coordination with the New York State Deparment of Health would be essential so as not to
interfere with State health waivers authorizing SEPs. As with local legislative efforts, local
administrative actions may draw challenges under state law, depending on state
prosecutors’ enforcement decisions. Some other cities, including Baltimore, Philadelphia,
and San Francisco are using local authority to study SIF feasibility. Seattle and Ithaca, New
York have announced intentions or decisions to authorize the establishment of SIFs as part
of a larger strategy to reverse the opioid overdose epidemic. However, all are grappling
with the potential impact of state and federal criminal laws.
Research study with federal and state authorization
A supervised injection facility could be implemented as a research study, with the goal of
evaluating the acceptability and feasibility of a SIF in New York City. There are established
legal procedures for conducting research that involves the use of controlled substances,
which insulate researchers and participants from prosecution under federal and state drug
laws. Either the New York State Department of Health or DOHMH could establish a SIF as a
research pilot under a two-year state license. Although licensure can be granted by the
state, all research licenses of this nature would require review and approval from several
federal authorities, including the National Institute on Drug Abuse, the US Department of
Justice and the Drug Enforcement Administration.
To date, no American city has attempted to establish a SIF through a research program,
although successful SIFs in Vancouver, Canada and Sydney, Australia began as research
pilots. Federally approved research licenses provide several advantages, including
certainty on the part of SIF staff and clients that they are not violating federal or state laws.

40
The evidence generated from a pilot also may help garner public support for SIFs as a
prelude to New York State legislative or administrative efforts. However, sustaining
services beyond the two-year license is contingent on reapproval, which may be uncertain
in a given political climate, and, as experienced in both Sydney and Vancouver, expansion
from a demonstration pilot program has been restricted because of limitations in the
research license even after years of operation and proven program benefits.
Conclusion on legal challenges and opportunities
State legislative action offers the greatest certainty under state and local laws for a New
York City SIF. However, the risk of federal prosecution under the Controlled Substances
Act would not be diminished by state legislative action. In the absence of state legislation,
state administrative action would provide some security, but would not protect against
state or federal prosecution. The City could also use legislative power, executive power, or
both to authorize SIFs; however, SIFs so established would be vulnerable to possible
contravening powers of both the state and federal government. Regardless of the pathway
by which supervised injection is implemented, viability will depend on law enforcement
bodies recognizing SIFs as an extension of health services for individuals most vulnerable
to illness and death from opioid use.

41
CASE STUDIES: SUPERVISED
INJECTION FACILITIES AT THE
MUNICIPAL LEVEL
Update from Seattle, San Francisco, and Philadelphia
Although no supervised injection facilities exist currently in the United States, Seattle, San
Francisco, and Philadelphia are moving toward implementing SIFs as a strategy to respond
to increasing overdose deaths.
Seattle
In January 2017, the Seattle City Council and King County Board of Public Health approved
a measure to authorize two SIFs, slated to open in 2018.
‡
The proposal originated from the
formal recommendations of the King County Heroin and Prescription Opiate Addiction
Task Force, and formal approval followed two years of coalition building and sustained,
broad-based support.
97
In November 2017, the Seattle City Council voted to allocate $1.3
million to fund a community health engagement location (CHEL) that would include
supervised injection and post-consumption drop-in space in conjunction with syringe
exchange, overdose prevention, sexual health, peer education, and referrals to medical,
mental health, and social services.
Since the Task Force released its recommendations, the proposal to establish SIFs has
received public endorsement from King County Prosecutor Dan Satterberg. The
endorsement from Satterberg, in particular, was critical in shoring up support among the
law enforcement community. Satterberg has spoken publicly about his evolution from self-
professed “drug warrior” during the crack cocaine epidemic of the 1980s to his current
stance that drugs are an issue of public health. His support for supervised injection is
emblematic of the multidisciplinary nature of contemporary drug reform once
stakeholders examine the evidence and best practice options. In all jurisdictions with
operational SIFs, cooperation between law enforcement and health authorities has been
crucial to the advancement, establishment, and sustainability of SIFs.
However, there is opposition to supervised injection in Seattle. Washington State Senator
Mark Miloscia introduced a bill that effectively would ban SIFs in Washington State, shortly
after the measure was approved by the City Council and Board of Public Health.
98
The bill
passed the Washington State Senate in March 2017 but has not yet advanced in the State
House. Senator Miloscia also drafted an open letter to the United States Attorney General in
February 2017 requesting federal intervention to prevent the City of Seattle from opening
the scheduled SIF pilot sites.
99
While the US Department of Justice has not yet responded to
the letter, any federal movement to prohibit SIFs could collaterally affect New York City.
Finally, the community group Citizens for Safe King County introduced a public ballot
‡
Seattle is the county seat of King County.
42
initiative, Initiative 27, to ban supervised injection in King County. The initiative garnered
over 70,000 signatures and was scheduled for a February 2018 vote before the King County
Superior Court invalidated the initiative in October 2017 on the grounds that matters of
public health could not be voted on by referendum. King County intends to use public funds
toward the operation of supervised injection sites.
San Francisco
In April 2017, California State Assembly Member Susan Talamantes Eggman introduced a
bill to authorize eight California counties, including San Francisco, to open SIFs in response
to increased overdose and public injection across California.
100
While the bill passed the
Assembly and received broad public support, it ultimately was voted down in the State
Senate in September 2017.
Simultaneously, the San Francisco Board of Supervisors passed a resolution in April 2017
urging the San Francisco Department of Public Health to convene the San Francisco Safe
Injection Services Task Force. The Task Force was commissioned between April and
September 2017 and was composed of experts in public health, law enforcement, social
services, and drug policy, as well as community members representing the interests of
small businesses and people who use drugs. As part of the Task Force’s recommendations
development process, surveys and focus groups were conducted with small business
owners, neighborhood groups, people who inject drugs, and people engaged in treatment
for substance use disorder. Task Force meetings included sessions for public comment, and
feedback from the public about supervised injection was received and incorporated into
the recommendations.
In September 2017, the Task Force released its recommendations, which broadly endorsed
supervised injection as a public health intervention.
101
The recommendations detailed
suggestions for planning, implementation, and sustainability and were presented before
the Board of Supervisors’ Public Safety and Neighborhood Services Committee for
consideration in October 2017. In February 2018, the Director of the San Francisco
Department of Public Health announced that San Francisco would seek to pilot two
supervised injection sites as early as July 2018, funded through private sources. San
Francisco intends to co-locate supervised injection services within existing community-
based programs that provide syringe access and other health and social services to people
who use drugs.
Philadelphia
In January 2018, the Philadelphia Task Force to Combat the Opioid Epidemic released a
report recommending supervised injection as a strategy to reduce opioid overdose.
102
Shortly thereafter, Philadelphia Mayor Jim Kenney, District Attorney Larry Krasner, and
Health Commissioner Thomas Farley announced their joint public support for supervised
injection. The Kenney Administration intends to pilot “comprehensive drug user
engagement sites,” holistic health care, and social services for people who use drugs in
which supervised injection services would be available. While the details of these pilot
programs are in development, the City of Philadelphia has expressed that any supervised
43
injection pilots will operate with private funding in partnership with existing harm
reduction organizations to oversee site operations.
44
RECOMMENDATIONS
New York City has experienced a 166% increase in overdose death since 2010, reaching an
all-time high in 2017 with a provisional 1,441 confirmed fatalities. Over 80% of these
deaths involved opioids. Nearly half (44%) of all overdose deaths in 2016 involved non-
pharmaceutical fentanyl—a synthetic opioid 50 to 100 times more potent than morphine—
and the drug’s impact on overdose cannot be overstated. Non-pharmaceutical fentanyl
greatly increases the risk of overdose among people who inject drugs due to its potency,
short-acting effect, and inability to be detected by sight or smell. Projections suggest that
non-pharmaceutical fentanyl’s presence in the drug supply will continue to expand, thus
requiring that public health actors deploy new responses.
Like syringe exchange before it, supervised injection is an evidence-based public health
strategy to prevent and reduce overdose and overdose death, curtail the transmission of
bloodborne disease, and facilitate access to care, treatment, and health for individuals at
highest risk of overdose. Despite concerns about increases in drug-related crime or
substance misuse in communities following the establishment of a SIF, evidence indicates
that supervised injection facilities may be an effective measure to reduce crime and
prevent community exposure to harmful substance use.
Results from the three studies presented in this report, in conjunction with the broad
scientific evidence from other jurisdictions, suggest that supervised injection is one
possible intervention to combat opioid overdose in New York City in alignment with the
goals of HealingNYC and ThriveNYC. Supervised injection facilities can fit into New York
City’s comprehensive overdose prevention agenda as a targeted strategy to reduce the risk
of overdose and disease transmission among people who inject drugs, as well as offering
the community-wide benefit of decreasing public injection. Guided by this evidence, we
offer the following recommendations to address the planning and implementation of
supervised injection services in New York City.
Support the creation of supervised injection services in New York City
Our overarching recommendation is to support the piloting of four supervised
injection facilities in New York City, despite the risk of criminal prosecution for
clients, staff, and operators, as well as the risk of loss of licensure of clinical staff and
the forfeiture of property for facility operators and landlords. Supervised injection is
congruent with New York City’s comprehensive health and safety strategy to reduce
overdose. Establishing SIFs in neighborhoods highly affected by opioid overdose
death and in which public injection is a growing concern could maximize the
number of lives saved. Findings suggest that piloting four sites could prevent up to
130 overdose deaths and save up to $7 million annually while connecting
individuals at risk of overdose to a host of harm reduction, drug treatment, and
health care services.

45
Planning and implementation
Implement pilot supervised injection facilities by December 2018 in response to New York
City’s fentanyl-driven public health emergency
All available data demonstrate that the increases in overdose death—47% citywide
from 2015 to 2016—and the toxicity associated with non-pharmaceutical fentanyl
constitute a public health emergency in New York City. Non-pharmaceutical fentanyl
was identified in 44% of overdose decedents in 2016, indicating the tremendous
risk of overdose posed by the current drug supply. Individuals residing in shelters
represent less than 1% of the New York City population but account for 7% of all
overdose deaths. Supervised injection facilities would directly serve the population
of people who inject drugs publicly due to lack of housing or private space.
Supervised injection facilities also would link individuals to needed medical care,
drug treatment, and housing services.
Locate pilot supervised injection facilities within existing syringe exchange programs
Co-locating pilot SIFs within existing syringe exchange programs would leverage the
strong community relations and extensive on-site treatment and service referral
networks that SEPs have built over nearly three decades. Given the long-standing
history of collaboration and mutual respect between harm reduction services, law
enforcement, and local communities in New York City, locating SIF services within
an existing harm reduction facility will facilitate the acceptance of supervised
injection by law enforcement and local community members.
The concerns identified through the community assessment presented in this
report—such as the generation of concentrations of people who use drugs and
public injection—would be assuaged by the co-location of SIFs in SEPs. Evaluations
of existing SIFs suggest that, like SEPs, these services are highly localized; people
who use drugs generally do not travel more than 20 minutes to use either SIFs or
SEPs. Additionally, evaluations of existing SIFs have shown significant declines in
public injection and improperly discarded syringes in neighborhoods following the
opening of a SIF site.
Co-location of SIFs in SEPs would be cost-effective. It would eliminate the siting
expenses associated with developing a new facility, save startup and development
costs, and make co-location a fiscally responsible option.
Pilot sites should reflect where the burden of overdose is severe and the need for resources is
great
The burden of overdose is spread disproportionately across the city, with the
poorest neighborhoods—including Hunts Point-Mott Haven in the Bronx and East
Harlem in Manhattan—experiencing extremely high fentanyl-involved overdose
rates. In order to address endemic disparities in risk and harm, pilot SIFs should be
located in areas of New York City that have borne a disproportionate burden of
overdose deaths.
46
Support New York State administrative action as a realistic legal possibility in the absence of
legislation
While State legislative change could eliminate risk of prosecution under State law
and of loss of licensure and aid with defense in a federal criminal prosecution, State-
level administrative action may be more readily achievable. The current fentanyl
crisis and continued increases in overdose deaths constitute a public health
emergency, through which the New York State Department of Health could establish
a pilot SIF.
There is precedent for the New York State Department of Health to take progressive
administrative action. In response to the HIV/AIDS epidemic, the New York State
Department of Health used administrative action to issue an emergency health
waiver to authorize syringe exchange programming, which was being run
underground by activists at the time.
Build out and collaborate with coalitions of nongovernmental support to operate supervised
injection pilots
Widespread nongovernmental support exists for supervised injection, with 41
independent advocacy and community organizations endorsing the establishment of
supervised injection services nationally or in New York City. See Appendix A for the
full list of supporting organizations.
One organization in particular, amfAR, wrote an open letter to New York Governor
Andrew Cuomo in September 2017 urging him to take New York State
administrative action authorizing SIFs and offering to fund a pilot site, as the
organization did during the first NYS syringe exchange pilot in the 1990s. History
has proved the success of allowing scientific experts such as amfAR to operate high-
risk, high-reward pilot health programs. Without amfAR’s funding and operational
support, the institutionalization of syringe exchange in New York State would not
have been possible. See Appendix B for the full text of amfAR’s letter to Governor
Cuomo.
Ensure that supervised injection facilities are supportive and safe spaces for marginalized
communities at increased risk of overdose and associated harm
Supervised injection services can serve as targeted interventions to aid the city’s
most vulnerable populations. Shelter residents and undomiciled individuals
represent less than 1% of the New York City population, yet account for 7% of all
overdose deaths with an unprecedented mortality rate over six times that of the
general population. Women who use drugs are at heightened risk of experiencing
street-based violence. Supervised injection facilities can position themselves as
supportive and safe spaces for these and other groups at high risk of overdose to
access a variety of services and referrals given SIFs’ demonstrated ability to function
as holistic health care and social service centers.

47
Evaluate the health, safety, and fiscal impacts of a supervised injection pilot
While with clear proven value globally, given that no comparable services currently
exist in New York City or the United States, pilot supervised injection facilities in
New York City will be evaluated to assess their health, safety, and fiscal impacts. To
accomplish this, we recommend sustained engagement with the scientific
community coupled with ongoing quality improvement to ensure that pilot SIFs are
accountable and successful in meeting the aims for which they are established, and
contribute to the body of knowledge for use by other jurisdictions nationally and
internationally. As was the case with the first syringe exchange programs,
evaluation by independent academic experts should be conducted and required to
ensure that the highest possible scientific standards are met.
Public engagement and education
Leverage the support of county prosecutors to facilitate supervised injection pilot
implementation
The support of prosecutors has been integral to the success of drug reforms in New
York City and nationally. In Seattle, the public support for supervised injection of
King County District Attorney, Dan Satterberg, was a key link in building the
coalition between public health and law enforcement that has brought Seattle closer
to opening a SIF.
In New York City, prosecutors have been at the cutting edge of drug reform in the
law enforcement community. The late Brooklyn District Attorney, Kenneth
Thompson, ceased prosecuting low-level marijuana possession offenses in 2014,
which paved the way for the New York City Police Department to revise their
marijuana arrest policy. The Manhattan District Attorney, Cyrus Vance, Jr., is a
leader in restructuring drug diversion procedures, allowing the use of evidence-
based medications for addiction treatments in drug courts. The Staten Island
District Attorney, Michael McMahon, led the design and implementation of the HOPE
Program, a post-arrest drug diversion program. The Bronx District Attorney, Darcel
Clark, leads the Bronx Heroin Enforcement and Access to Treatment workgroup,
which aims to coordinate a comprehensive and collaborating public health and
safety response to increasing rates of opioid overdose in the Bronx. We recommend
engaging one or more New York City prosecutors in the planning and development
process of any supervised injection pilot to ensure that these front-line leaders in
law enforcement are able to provide their expertise and input into the development
of a SIF pilot.
Engage key perspectives as part of a collaborative planning process
Incorporating the complementary perspectives of public health, public safety, law
enforcement, social services, and local communities in the planning process is
critical to maximize the potential benefits of SIFs with respect to all groups.
Responsiveness to a range of interests will ensure that SIFs can most effectively help
the New Yorkers who need them most.
48
Hold public planning sessions for the communities most impacted by overdose
Public and community support are critical to the successful implementation of
supervised injection services. We recommend establishing planning consortiums of
key community stakeholders and advocates in target neighborhoods highly affected
by overdose mortality, with an anchor harm reduction provider in each. Planning
meetings would provide a structured space for members of the public to learn about
SIFs from recognized experts, provide feedback throughout the implementation
process, and raise concerns. An advisory committee comprised of health, safety,
community leaders, and advocates would guide the public discussion process in the
selected neighborhoods and ensure that public feedback is adequately incorporated
into the implementation plan. New Yorkers support the City’s ongoing mental health
and overdose prevention efforts. Sustained community engagement and procedural
transparency are essential to ensuring that SIFs are successfully integrated into the
existing landscape of harm reduction services. Including professional organizations
and expert bodies (e.g., the New York State Medical Society and New York State
Nursing Association) in the planning and feedback processes could garner support
and educate members who are New York City residents.
Work with law enforcement officials
Law enforcement agencies are key partners of the public health and social service
communities citywide and it is important that they remain engaged throughout the
planning and implementation processes of any pilot supervised injection facility.
Strengthening the coalition through NYC RxStat that exists in New York City
between public health, public safety, and community-based social services will
cultivate cooperation and accountability between groups, allow groups to identify
clear roles and responsibilities, and ensure that all voices are heard.
Develop public resources and education about supervised injection facilities to inform local
stakeholders about the continuum of care and discuss stigma toward people who use drugs
Opportunities for education about supervised injection and the substance use
continuum of care can be developed through collaboration between advocates,
public health professionals, and health care providers to both inform and receive
feedback from community stakeholders as part of a pilot implementation process.
Engaging community stakeholders early and often as part of a design and
implementation plan would help facilitate referrals between a pilot SIF and other
critical services—including housing, public benefits, re-entry, and victim services—
as well as address community drug use stigma. Additionally, advocates and health
professionals can offer training and education to public safety and law enforcement
professionals as part of pilot implementation to ensure collaboration between
multiple groups.
49
ACKNOWLEDGMENTS
Columbia Law School
Kristen Underhill, DPhil, JD
New York Academy of Medicine
Michele Calvo, MPH
Peter Schafer
New York City Department of Health and Mental Hygiene
Bennett Allen
Gary Belkin, MD, PhD, MPH
Stephanie Buhle
Holly Catania, JD
Cody Colon-Berezin, MPH
Rebecca Giglio, MPH
Alex Harocopos, PhD, MS
Amy Hecker, MPA
Maura Kennelly, MPH
Jacob Kraemer
Hillary Kunins, MD, MPH
Sam Miller, MPA
Michelle Nolan, MPH
Denise Paone, EdD
Maibe Ponet
Emily Winkelstein, MSW
Ricky Wong
Weill Cornell Medical College
Czarina Behrends, PhD, MPH
Bruce Schackman, PhD, MBA
Expert Advisory Panel
Ahmed Bayoumi, MD, MSc
Scientist at the Centre for Research on Inner City Health at the Li Ka Shing Knowledge Institute, general
internist and HIV physician at St. Michael's Hospital, and professor in the Department of Medicine at the
Institute of Health Policy, Management and Evaluation at the University of Toronto
Czarina N. Behrends, PhD, MPH
Postdoctoral Associate in the Division of Comparative Effectiveness and Outcomes Research in the
Department of Health care Policy and Research at Weill Cornell Medicine
Richard Elliott, LLM
Executive Director of the Canadian HIV/AIDS Legal Network
50
Liz Evans
Nurse, Co-founder of InSite, a supervised injection facility in Vancouver, founder and former director of PHS
Community Services Society, Executive Director of New York Harm Reduction Educators (NYHRE) and
Washington Heights Corner Project, and fellow with Open Society Foundation
Sarah Evans, MA
Senior Program Officer for the Open Society Foundation’s International Harm Reduction Development
Program
Brad Finegood, MA, LMHC
Assistant Division Director and Alcohol and Drug Treatment and Prevention Coordinator for the Behavioral
Health and Recovery Division of King County, Seattle and Co-Chair of the King County Heroin and Prescription
Opiate Task Force
Kassandra Frederique, MS
New York State Director at the Drug Policy Alliance, Co-author of Blueprint for a Public Health and Safety
Approach to Drug Policy and as Technical Advisor to Ithaca Mayor Svante Myrick’s The Ithaca Plan
Terrell Jones
Education and Advocacy Program Manager at New York Harm Reduction Educators
Thomas Kerr, PhD
Co-director of the Addiction and Urban Health Research Initiative at the British Columbia Centre for
Excellence in HIV/AIDS and professor in the Department of Medicine, University of British Columbia (Division
of AIDS)
Alex Kral, PhD, MS
Director of the Behavioral and Urban Health Program, San Francisco Regional Office of RTI International
Daniel Raymond
Policy Director at the Harm Reduction Coalition and member of the steering committee of the National Viral
Hepatitis Roundtable
Bruce Schackman, PhD, MBA
Professor of Health care Policy and Research, Weill Cornell Medical College.
Kristen Underhill, DPhil, JD
Associate Professor of Law at Columbia Law School
Technical Advisory Group
Ahmed Bayoumi, MD, MSc (Chair)
Scientist at the Centre for Research on Inner City Health at the Li Ka Shing Knowledge Institute, general
internist and HIV physician at St. Michael's Hospital, and professor in the Department of Medicine at the
Institute of Health Policy, Management and Evaluation at the University of Toronto
Eva Enns, PhD
Assistant Professor in the Division of Health Policy and Management at the School of Public Health, University
of Minnesota
51
Bohdan Nosyk, PhD, MA
Associate Professor and Endowed Chair of Economics of HIV/AIDS at the Faculty of Health Sciences, Simon
Fraser University and research scientist at the British Columbia Centre for Excellence in HIV/AIDS
Carol Strike, PhD, MSc
Division Head of Social & Behavioural Health Sciences at the Dalla Lana School of Public Health, University of
Toronto
Greg Zaric, PhD, MS, MASc
Professor and Chair in Management Science at Ivey Business School in Western University Canada
Report prepared by:
Bennett Allen
New York City Department of Health and Mental Hygiene

52
REFERENCES
1
New York City Department of Health and Mental Hygiene. Unintentional drug poisoning (overdose) deaths in
New York City, Quarters 1-3, 2017. Provisional Data Report. New York, NY: DOHMH; 2018.
2
DOHMH, 2018.
3
Blakeman D, Lewine E. HealingNYC: Preventing overdoses, saving lives. New York, NY: Office of the Mayor of
the City of New York; 2017.
4
AMA wants new approaches to combat synthetic and injectable drugs. American Medical Association
https://www.ama-assn.org/ama-wants-new-approaches-combat-synthetic-and-injectable-drugs. Accessed
July 18, 2017.
5
Defining and implementing a public health response to drug use and misuse. American Public Health
Association https://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-
database/2014/07/08/08/04/defining-and-implementing-a-public-health-response-to-drug-use-and-
misuse. Updated November 5, 2013. Accessed July 18, 2017.
6
Schatz E, Nougier M. Drug consumption rooms: Evidence and practice. IDPC Briefing Paper. London, UK:
International Drug Policy Consortium; 2012.
7
European Monitoring Centre for Drugs and Drug Addiction. Drug consumption rooms: An overview of
provision and evidence. EMCDDA Perspectives on Drugs. Lisbon, Portugal: EMCDDA; 2017.
8
Seth P, Scholl L, Rudd RA, Bacon S. Overdose Deaths Involving Opioids, Cocaine, and Psychostimulants —
United States, 2015–2016. MMWR Morb Mortal Wkly Rep 2018;67:349–358.
9
Paone et al., 2017.
10
Paone et al., 2017.
11
Paone D, Tuazon E, Nolan ML, Mantha S. Unintentional drug poisoning (overdose) deaths involving heroin
and/or fentanyl in New York City, 2000-2015. Epi Data Brief: 74. New York, NY: New York City Department of
Health and Mental Hygiene; 2016.
12
Paone et al., 2017.
13
Drug Enforcement Administration. 2016 National Drug Threat Assessment summary. Washington, DC: US
Department of Justice; 2016.
14
Drug Policy Alliance. Fact sheet: Fentanyl and synthetic opioids. New York, NY: Drug Policy Alliance; 2016.
15
Paone et al., 2017.
16
New York City Department of Health and Mental Hygiene. Unpublished data, 2016.
17
Carroll JJ, Marshall BDL, Rich JD, Green TC. Exposure to fentanyl-contaminated heroin and overdose risk
among illicit opioid users in Rhode Island: A mixed methods study. Int J Drug Policy. 2017.
18
Ciccarone D, Ondocsin J, Mars SG. Heroin uncertainties: Exploring users’ perceptions of fentanyl-
adulterated and –substituted ‘heroin’. Int J Drug Policy. 2017.
19
Paone et al., 2017.
20
Department of Homeless Services. Daily Report Census, October 2, 2017. Published October 3, 2017.
21
New York City Department of Health and Mental Hygiene. Unpublished data; 2017.
22
Kral AH, Bluthenthal RN, Booth RE, Watters JK. HIV seroprevalence among street-recruited injection drug
and crack cocaine users in 16 US municipalities. Am J Public Health. 1998;88(1):108-13.
23
Holtzman D, Barry V, Ouellet LJ, et al. The influence of needle exchange programs on injection risk
behaviors and infection with hepatitis C virus among young injection drug users in select cities in the United
States, 1994-2004. Prev Med. 2009;49(1):68-73.
24
Office of the Mayor of the City of New York. (2018, March 19). HealingNYC: Mayor and First Lady announce
$22 million expansion of City’s plan to combat opioid epidemic. [Press release]. Retrieved from:
http://www1.nyc.gov/office-of-the-mayor/news/143-18/healingnyc-mayor-first-lady-22-million-expansion-
city-s-plan-combat-opioid
25
Magura, S., Lee, J. D., Hershberger, J., Joseph, H., Marsch, L., Shropshire, C., & Rosenblum, A. (2009).
Buprenorphine and methadone maintenance in jail and post-release: a randomized clinical trial. Drug and
alcohol dependence, 99(1), 222-230.
26
Halpern M, Rho YM. Deaths from narcotism in New York City: Incidence, circumstances and postmortem
findings. NY State J Med 1966; 66(12):2391 – 2408.

53
27
Joseph H, Stancliff S, Langrod J. Methadone maintanence treatment (MMT): a review of historical and
clinical issues. Mt Sinai J Med. 2000;67(5-6): 347-64.
28
Joseph et al., 2000.
29
Des Jarlais DC, Friedman SR, Sotheran JL, et al. Continuity and change within an HIV epidemic. Injecting
drug users in New York City, 1984 through 1992. JAMA. 1994;271(2):121-7.
30
Stimson GV, Alldritt L, Dolan K, Donoghoe M. Syringe exchange schemes for drug users in England and
Scotland. Br Med J. 1988;296(6638):1717-9.
31
Tsai R, Goh EH, Webeck P, Mullins J. Prevention of human immunodeficiency virus infection among
intravenous drug users in New South Wales, Australia: the needles and syringes distribution programme
through retail pharmacies. Asia Pac J Public Health. 1988;2(4):245-51.
32
Anderson W. The New York Needle Trial: the politics of public health in the age of AIDS. Am J Public Health.
1991;81(11):1506-17.
33
Comprehensive Harm Reduction Reverses the Trend in New HIV Infections. New York State Department of
Health, AIDS Institute https://www.health.ny.gov/diseases/aids/providers/reports/docs/sep_report.pdf.
Updated 2014. Accessed October 15, 2017.
34
Paone D, Des jarlais DC, Gangloff R, Milliken J, Friedman SR. Syringe exchange: HIV prevention, key findings,
and future directions. Int J Addict. 1995;30(12):1647-83.
35
Des jarlais DC, Marmor M, Paone D, et al. HIV incidence among injecting drug users in New York City
syringe-exchange programmes. Lancet. 1996;348(9033):987-91.
36
Comprehensive Harm Reduction Reverses the Trend in New HIV Infections. New York State Department of
Health, AIDS Institute https://www.health.ny.gov/diseases/aids/providers/reports/docs/sep_report.pdf.
Updated 2014. Accessed October 15, 2017.
37
Peters PJ, Pontones P, Hoover KW, et al. HIV Infection Linked to Injection Use of Oxymorphone in Indiana,
2014-2015. N Engl J Med. 2016;375(3):229-39.
38
Hadland SE, DeBeck K, Kerr T, et al. Use of a medically supervised injection facility among street youth. J
Adolesc Health. 2014;55(5):684-9.
39
Drug Policy Alliance. Supervised consumption facilities. New York, NY: Drug Policy Alliance; 2017.
40
Potier C, Laprévote V, Dubois-arber F, Cottencin O, Rolland B. Supervised injection services: what has been
demonstrated? A systematic literature review. Drug Alcohol Depend. 2014;145:48-68.
41
Hedrich, D, Kerr T, Dubois-Arber F. 2010. “Drug Consumption Facilities in Europe and Beyond.” Chap. 11. In
Harm Reduction: Evidence, Impacts, and Challenges, edited by T. Rhodes and D. Hedrich, 305–331. Lisbon,
Portugal: European Monitoring Centre for Drugs and Drug Addiction.
42
Marshall BD, Milloy MJ, Wood E, Montaner JS, Kerr T. Reduction in overdose mortality after the opening of
North America's first medically supervised safer injecting facility: a retrospective population-based study.
Lancet. 2011;377(9775):1429-37.
43
Salmon AM, Van Beek I, Amin J, Kaldor J, Maher L. The impact of a supervised injecting facility on
ambulance call-outs in Sydney, Australia. Addiction. 2010;105(4):676-83.
44
Stoltz JA, Wood E, Small W, et al. Changes in injecting practices associated with the use of a medically
supervised safer injection facility. J Public Health. 2007;29(1):35-9.
45
Van Boekel LC, Brouwers EP, Van Weeghel J, Garretsen HF. Stigma among health professionals towards
patients with substance use disorders and its consequences for healthcare delivery: Systematic review. Drug
Alcohol Depend. 2013;131(1-2):23-35.
46
Small W, Van Borek N, Fairbairn N, Wood E, Kerr T. Access to health and social services for IDU: The impact
of a medically supervised injection facility. Drug Alcohol Rev. 2009;28(4):341-6.
47
Small W, Wood E, Lloyd-Smith E, Tyndall M, Kerr T. Accessing care for injection-related infections through a
medically supervised injecting facility: A qualitative study. Drug Alcohol Depend. 2008;98(1-2):159-62.
48
Lloyd-Smith E, Wood E, Zhang R, et al. Determinants of hospitalization for a cutaneous injection-related
infection among injection drug users: A cohort study. BMC Public Health. 2010;10:327.
49
Andresen MA, Boyd N. A cost-benefit and cost-effectiveness analysis of Vancouver's supervised injection
facility. Int J Drug Policy. 2010;21(1):70-6.
50
Milloy MJ, Wood E. Emerging role of supervised injecting facilities in human immunodeficiency virus
prevention. Addiction. 2009;104(4):620-1.
51
Bravo MJ, Royuela L, De La Fuente L, et al. Use of supervised injection facilities and injection risk
behaviours among young drug injectors. Addiction. 2009;104(4):614-9.
52
Stoltz et al., 2007.

54
53
Kral et al., 1998.
54
Holtzman et al., 2009.
55
Kimber J, Mattick RP, Kaldor J, Van Beek I, Gilmour S, Rance JA. Process and predictors of drug treatment
referral and referral uptake at the Sydney Medically Supervised Injecting Centre. Drug Alcohol Rev.
2008;27(6):602-12.
56
Wood E, Tyndall MW, Zhang R, et al. Attendance at supervised injecting facilities and use of detoxification
services. N Engl J Med. 2006;354(23):2512-4.
57
Debeck K, Kerr T, Bird L, et al. Injection drug use cessation and use of North America's first medically
supervised safer injecting facility. Drug Alcohol Depend. 2011;113(2-3):172-6.
58
Fairbairn N, Small W, Shannon K, Wood E, Kerr T. Seeking refuge from violence in street-based drug scenes:
Women's experiences in North America's first supervised injection facility. Soc Sci Med. 2008;67(5):817-23.
59
Hadland SE, DeBeck K, Kerr T, et al. Use of a medically supervised injection facility among street youth. J
Adolesc Health. 2014;55(5):684-9.
60
Andresen MA, Boyd N. A cost-benefit and cost-effectiveness analysis of Vancouver's supervised injection
facility. Int J Drug Policy. 2010;21(1):70-6.
61
Bayoumi AM, Zaric GS. The cost-effectiveness of Vancouver's supervised injection facility. CMAJ.
2008;179(11):1143-51.
62
Wood E, Tyndall MW, Lai C, Montaner JS, Kerr T. Impact of a medically supervised safer injecting facility on
drug dealing and other drug-related crime. Subst Abuse Treat Prev Policy. 2006;1:13.
63
Salmon AM, Thein HH, Kimber J, Kaldor JM, Maher L. Five years on: what are the community perceptions of
drug-related public amenity following the establishment of the Sydney Medically Supervised Injecting
Centre?. Int J Drug Policy. 2007;18(1):46-53
64
Freeman K, Jones CG, Weatherburn DJ, Rutter S, Spooner CJ, Donnelly N. The impact of the Sydney Medically
Supervised Injecting Centre (MSIC) on crime. Drug Alcohol Rev. 2005;24(2):173-84.
65
Snowball L, Burgess M, Price B. Trends in property and illicit drug-related crime in Kings Cross: An update.
Crime and Just Statistics. 2010;51:1-6.
66
Kerr T, Stoltz JA, Tyndall M, et al. Impact of a medically supervised safer injection facility on community
drug use patterns: A before and after study. BMJ. 2006;332(7535):220-2.
67
Tyndall MW, Kerr T, Zhang R, King E, Montaner JG, Wood E. Attendance, drug use patterns, and referrals
made from North America's first supervised injection facility. Drug Alcohol Depend. 2006;83(3):193-8.
68
Kimber et al., 2008.
69
Debeck et al., 2011.
70
Kerr T, Tyndall MW, Zhang R, Lai C, Montaner JS, Wood E. Circumstances of first injection among illicit drug
users accessing a medically supervised safer injection facility. Am J Public Health. 2007;97(7):1228-30.
71
Wood E, Kerr T, Small W, et al. Changes in public order after the opening of a medically supervised safer
injecting facility for illicit injection drug users. CMAJ. 2004;171(7):731-4.
72
Vecino C, Villalbí JR, Guitart A, et al. Safe injection rooms and police crackdowns in areas with heavy drug
dealing: Evaluation by counting discarded syringes collected from the public space. Adicciones.
2013;25(4):333-8.
73
Bayoumi AM, Strike C, Brandeau M, et al. Report of the Toronto and Ottawa Supervised Consumption
Assessment Study, 2012. Toronto, Ontario: St. Michael's Hospital and the Dalla Lana School of Public Health,
University of Toronto;2012.
74
Kral AH, Wenger L, Carpenter L, Wood E, Kerr T, Bourgois P. Acceptability of a Safer Injection Facility
among Injection Drug Users in San Francisco. Drug Alcohol Depend. 2010;110(1-2):160-163.
75
Fischer B, Allard C. Feasibility Study on ‘Supervised Drug Consumption’ Options in the City of Victoria Victoria,
British Columbia: Centre for Addictions Research of British Columbia, University of Victoria;2007.
76
Bouvier BA, Elston B, Hadland SE, Green TC, Marshall BDL. Willingness to use a supervised injection facility
among young adults who use prescription opioids non-medically: a cross-sectional study. Harm Reduct J.
2017;14:13.
77
Joshi M, Sorenson SB. Intimate partner violence at the scene: incident characteristics and implications for
public health surveillance. Eval Rev. 2010;34(2):116-36.
78
New York City Department of Health and Mental Hygiene. Unpublished data; 2017.
79
Milloy MJ, Wood E. Emerging role of supervised injecting facilities in human immunodeficiency virus
prevention. Addiction. 2009;104(4):620-1.

55
80
Kimber J, Mattick RP, Kaldor J, Van Beek I, Gilmour S, Rance JA. Process and predictors of drug treatment
referral and referral uptake at the Sydney Medically Supervised Injecting Centre. Drug Alcohol Rev.
2008;27(6):602-12.
81
Kenworthy J, Yi Y, Wright A, Brown J, Maria madrigal A, Dunlop WCN. Use of opioid substitution therapies
in the treatment of opioid use disorder: results of a UK cost-effectiveness modelling study. J Med Econ.
2017;20(7):740-748.
82
Irwin A, Jozaghi E, Weir BW, Allen ST, Lindsay A, Sherman SG. Mitigating the heroin crisis in Baltimore, MD,
USA: a cost-benefit analysis of a hypothetical supervised injection facility. Harm Reduct J. 2017;14(1):29.
83
21 U.S.C. §§ 801 et seq. (2017).
84
See Burris et al., supra note 18, at 1146-47 (noting that Congress could, in theory, limit federal funds to
programs or jurisdictions that operate SIFs, and describing an unsuccessful prior legislative effort to do so).
85
N.Y. Public Health Law § 3381 (2017).
86
See Roe v. City of New York, 232 F. Supp. 2d 240 (S.D.N.Y. 2002) (finding an exception to the law
criminalizing possession of trace amounts of drug in syringes, as applied to clients of legally authorized SEPs).
87
A.8534, 2017-2018 Reg. Sess. (N.Y. 2017) (introduced June 21, 2017, in the Committee on Health).
88
AB-186, 2017-2018 Reg. Sess. (Cal. 2017) (passed the House as of June 2017).
89
https://leg.colorado.gov/sites/default/files/summary_report_to_legislative_council_-
_opioid_and_other_substance_use_disorders.pdf
90
H.B. 519, 2017 Reg. Sess. (Md. 2017) (in the House as of June 2017).
91
L.D. 1375, 128th Legisl. (Me. 2017) (rejected in the House and Senate as of June 2017).
92
S.1081, 190th Gen. Court. (Mass. 2017) (in the Joint Committee on Mental Health, Substance Use and
Recovery as of June 2017).
93
NY Public Health Law § 201 (2017).
94
N.Y. Comp. Codes R. & Regs. 10, § 80.135
95
NY Constitution, art. IX § 2(c)(10).
96
New York City Charter § 556.
97
King County Heroin and Prescription Opiate Addiction Task Force. Final report and recommendations.
Seattle, WA: King County Department of Community and Human Services; 2016.
98
SB 5223, 65
th
Legisl. (Wfa. 2017).
99
Sessions, Jeff. Sen. Miloscia Letter to U.S Attorney General Jeff Sessions. Senate Republican Caucus. 2017.
100
AB-186, 2017-2018 Reg. Sess. (Cal. 2017)
101
San Francisco Safe Injection Services Task Force. (2017). 2017 final report. San Francisco, CA: San
Francisco Department of Public Health.
102
Mayor of Philadelphia’s Task Force to Combat the Opioid Epidemic. Final report and recommendations,
Philadelphia, PA: Philadelphia Department of Public Health; 2017.
56
APPENDIX A
Institutional Support for Supervised Injection
Supervised injection as a health strategy is supported by a wide range of professional
organizations, advocacy groups, community-based social services, and policy institutes.
Below is a list of local, national, and selected international organizations that have publicly
endorsed the establishment or pilot of supervised injection facilities.
New York City Organizations
ACT UP New York
After Hours Project
AIDS United
BOOM! Health
Bronx Defenders
Callen-Lorde Community Health Center
Community Access
Family Services Network of New York
Harlem United
Harm Reduction Coalition
Hepatitis C Mentor and Support Group
Hispanic Health Coalition
Housing Works
Injection Drug User Health Alliance
Lower East Side Harm Reduction Center
Metropolitan Community Church of New York
New York City Anti-Violence Project
New York Harm Reduction Educators
Peer Network of New York
Positive Health Project
St. Anne’s Corner of Harm Reduction
Sex Workers Project, Urban Justice Center
VOCAL New York
Washington Heights CORNER Project
National and International Policy and Advocacy Organizations
ACRIA
amfAR, the Foundation for AIDS Research
Center for Constitutional Rights
Clinton Foundation
Criminal Justice Policy Foundation
Drug Policy Alliance
European Monitoring Centre for Drugs and Drug Addiction
International Drug Policy Consortium
Katal Center for Health, Equity, and Justice
57
Latino Commission on AIDS
LatinoJustice PRLDEF (Puerto Rican Legal Defense and Education Fund)
Treatment Action Group
National and International Professional Organizations
American Medical Association
American Public Health Association
Australian Medical Association
Massachusetts Medical Society
National Association of State and Territorial AIDS Directors
New York Academy of Medicine

58
APPENDIX B
Statement of Support for Supervised Injection from the
American Medical Association
American Medical Association wants new approaches to combat synthetic and
injectable drugs
1
Responding to the health and safety threat posed by the abuse of new designer drugs that
are synthesized and marketed to circumvent drug laws, the American Medical Association
(AMA) today voted to support a comprehensive, multidisciplinary effort to close a gap in
the nation’s ability to identify, regulate, and mitigate the dangers posed by new
psychoactive substances.
New psychoactive substances – or NPS - mimic the effects of a wide range of substances,
including prescription opioids, cannabinoids, stimulants, hallucinogens, and central
nervous system depressants. NPS are sold as “legal highs” and alternatives to established
drugs of abuse. NPS have been increasingly associated with hospital emergencies, acute
adverse health consequences, and drug-induced death.
“Although Congress passed AMA-supported legislation in 2012 that placed 26 synthetic
drugs in Schedule 1 under the Controlled Substances Act (CSA), drug traffickers have
devised ways to circumvent federal drug laws by slightly altering the chemical structure of
their products and designing new synthetic drugs,” said Patrice A. Harris, MD, chair of the
AMA Board of Trustees and the AMA Task Force on Opioid Abuse. “These new products are
currently unregulated and are frequently marketed to young people as innocent products
like “bath salts,” plant food, or incense. They also include variations of the extremely
dangerous opioid fentanyl, which has been wreaking havoc across the country and
resulting in a sharp increase in drug overdoses and deaths due to such overdoses.”
Delegates at the AMA Annual Meeting voted to support multifaceted, collaborative
multiagency approach to combat NPS. Delegates also supported increased NPS surveillance
and early warning systems for more actionable information that can quickly aid law
enforcement, public health officials, emergency physicians, and vulnerable populations in
mitigating the growing NPS problem.
1
American Medical Association. AMA wants new approaches to combat synthetic and injectable drugs.
Available at: https://www.ama-assn.org/ama-wants-new-approaches-combat-synthetic-and-injectable-
drugs. Accessed December 29, 2017.

59
Public health approaches have been used to successfully address outbreaks of NPS
overdoses. When such approaches have been successful, pre-existing coordinated
relationships among multiple stakeholders have allowed for a rapid and comprehensive
response to a given outbreak.
In addition to the newly adopted policies for eliminating the NPS threat, the AMA is also
supporting the “Synthetic Drug Control Act of 2017” (H.R. 1732) that would require the
Attorney General of the United States to assign Schedule I classification to approximately
250 dangerous new synthetic substances identified by the Drug Enforcement
Administration since 2012.
In an effort to consider promising strategies that could reduce the health and societal
problems associated with injection drug use, the AMA today voted to support the
development of pilot facilities where people who use intravenous drugs can inject self-
provided drugs under medical supervision.
Studies from other countries have shown that supervised injection facilities reduce the
number of overdose deaths, reduce transmission rates of infectious disease, and increase
the number of individuals initiating treatment for substance use disorders without
increasing drug trafficking or crime in the areas where the facilities are located.
“State and local governments around the nation are currently involved in exploratory
efforts to create supervised injection facilities to help reduce public health and societal
impacts of illegal drug use,” said Dr. Harris. “Pilot facilities will help inform US
policymakers on the feasibility, effectiveness and legal aspects of supervised injection
facilities in reducing harms and health care costs associated with injection drug use.”
The examination of this issue by physicians at the AMA Annual Meeting was greatly
assisted by the Massachusetts Medical Society and its recently completed
comprehensive study of the literature associated with supervised injection facilities.
2
2
Fitzgerald TC, Abel B, Bates SR. Establishment of a pilot medically supervised injection facility in
Massachusetts: Report of the Task Force on Opioid Therapy and Physician Communication. Waltham, MA:
Massachusetts Medical Society; 2017.

60
APPENDIX C
Statement of Support for Supervised Injection from the
American Public Health Association
Defining and implementing a public health response to drug use and misuse
1
Problem Statement
As recognized in APHA policy 8817(PP), the current “war on drugs” is a “severely flawed”
approach based on “misplaced priorities and strategies.”
2
In the more than 40 years since
President Richard Nixon declared a war on drugs in 1971, the United States has spent an
estimated $1 trillion on drug war policies.
3
-
5
Yet national rates of drug use have remained
relatively stable, albeit with some minor fluctuations.
6
-
8
Meanwhile, drug-related harms,
such as the spread of bloodborne diseases and accidental overdose deaths, have grown
severely worse.
9
-
12
Overdose is second only to motor vehicle accidents as a leading cause of
injury-related death in the United States.
13
The war on drugs is a major driver of the HIV/AIDS pandemic among people who inject
drugs and their sexual partners. The criminalization of people who use illicit drugs, along
with the mass incarceration of people for nonviolent drug law violations, has restricted
1
American Public Health Association. Policy No. 201312. Available at: https://www.apha.org/policies-and-
advocacy/public-health-policy-statements/policy-database/2014/07/08/08/04/defining-and-
implementing-a-public-health-response-to-drug-use-and-misuse. Accessed December 29, 2017.
2
American Public Health Association. Policy No. 8817(PP). Available at:
http://www.apha.org/advocacy/policy/policysearch/default.htm?id=1179. Accessed December 12, 2013.
3
Lambert D. Drugs and receptors. Contin Educ Anaesth Crit Care Pain. 2004;4(6):181–184.
4
Ruiz P, Strain EC, eds. Substance Abuse: A Comprehensive Textbook. 5th ed. Philadelphia, PA: Wolters
Kluwer Health; 2011.
5
Mendoza M. US drug war has met none of its goals. Available at:
http://www.huffingtonpost.com/2010/05/13/us-war-on-drugs-has-met-n_n_575351.html#. Accessed
December 12, 2013.
6
Results from the 2011 National Survey on Drug Use and Health. Rockville, MD: Substance Abuse and Mental
Health Services Administration; 2012.
7
Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future, National Survey Results on
Drug Use, 1975–2012: Volume I, Secondary School Students. Ann Arbor, MI: Institute for Social Research,
University of Michigan; 2013.
8
World Drug Report 2013. New York, NY: United Nations; 2013.
9
The War on Drugs and HIV/AIDS: How the Criminalization of Drug Use Fuels the Global Pandemic. Rio de
Janeiro, Brazil: Global Commission on Drug Policy; 2012.
10
Compressed Mortality File 1999–2009. Atlanta, GA: Centers for Disease Control and Prevention; 2012.
11
Warner M, Chen LH, Makuc DM, Anderson RN, Miniño AM. Drug poisoning deaths in the United States,
1980–2008. NCHS Data Brief.2011;81:1–8.
12
US Department of Health and Human Services. Vital signs: overdoses of prescription opioid pain relievers—
United States, 1999–2008. MMWR Morb Mortal Wkly Rep. 2011;60(43):1487–1492.
13
Compressed Mortality—Underlying Cause of Death, ICD-10 Codes X40-44. Washington, DC: US Department
of Health and Human Services; 2010.

61
access to sterile syringes and opioid substitution treatments, and aggressive law
enforcement practices have promoted risky practices that facilitate the spread of HIV/AIDS
and other diseases while creating barriers to drug and HIV treatment.
Failure to adopt proven harm reduction measures has significantly increased the public
health harms of drug misuse. For example, legal and bureaucratic barriers still prevent
people who inject drugs from accessing sterile syringes in the United States, despite
decades of evidence proving that syringe access programs help to reduce the spread of
diseases.
14
-
18
In fact, the US Congress recently reinstated a federal ban on funding of sterile
syringe programs, after finally lifting the 2-decade-long ban just 3 years ago. The federal
ban is estimated to have cost thousands of lives and hundreds of millions of dollars.
19
Perhaps not surprisingly, fewer than one-third of people who inject drugs surveyed by the
Centers for Disease Control and Prevention (CDC) had been reached by an HIV
intervention.
20
Furthermore, while the United States has relatively high HIV prevalence
rates among people who inject drugs (at roughly 14%), countries that have consistently
and comprehensively provided harm reduction and effective treatment options, such as
syringe access and opioid substitution therapies, have rates that are far lower; in some of
these nations, HIV prevalence among people who inject drugs is 1% or lower.
21
Public funds are routinely prioritized for drug law enforcement instead of proven HIV
prevention strategies. While drug war budgets have generally increased, effective
treatment programs are chronically under resourced, and in the United States practically
no federal funds are invested in programs that will reduce harms related to injection drug
14
Effectiveness of Sterile Needle and Syringe Programming in Reducing HIV/AIDS Among Injecting Drug
Users. Geneva, Switzerland: World Health Organization; 2004.
15
Tilson H, Aramrattana A, Bozzette S, Celentano D, Falco M, Hammett T. Preventing HIV Infection Among
Injecting Drug Users in High-Risk Countries: An Assessment of the Evidence. Washington, DC: Institute of
Medicine; 2007.
16
International Guidelines on HIV/AIDS and Human Rights: 2006 Consolidated Version. Geneva, Switzerland:
Joint United Nations Programme on HIV/AIDS; 2006.
17
Hurley SF, Jolley DJ, Kaldor JM. Effectiveness of needle-exchange programmes for prevention of HIV
infection. Lancet. 1997;349(9068):1797–1800.
18
Uuskula A, Des Jarlais DC, Kals M, et al. Expanded syringe exchange programs and reduced HIV infection
among new injection drug users in Tallinn, Estonia. BMC Public Health. 2011;11:517.
19
Lurie P, Drucker E. An opportunity lost: HIV infections associated with lack of a national needle-exchange
programme in the USA. Lancet. 1997;349(9052):604–608.
20
Centers for Disease Control and Prevention. HIV-associated behaviors among injecting-drug users—23
cities, United States, May 2005–February 2006. MMWR Morb Mortal Wkly Rep. 2009;58(13):329–332.
21
Mathers BM, Degenhardt L, Ali H, et al. HIV prevention, treatment, and care services for people who inject
drugs: a systematic review of global, regional, and national coverage. Lancet. 2010;375(9719):1014–1028.

62
use.
22
The stigma associated with seeking and accessing drug treatment is also a barrier.
23
-
25
Criminalization of substance use further stigmatizes people who use drugs, making it more
difficult to engage people in health care and other services, a tendency that is often
compounded by sociocultural factors associated with problematic drug-using populations,
such as fear, lack of information and education, general physical and mental health
problems, homelessness, and incarceration.
26
-
28
Criminalization also exacerbates social
marginalization and encourages high-risk behaviors such as poly-drug use, binging, and
injecting in unhygienic, unsupervised environments.
29
Aggressive campaigns to arrest and
incarcerate people who use drugs only increase drug-related deaths, primarily because
people are too afraid to call 911 if they witness an overdose.
30
-
34
Harsh mandatory
minimum sentencing laws have also led to increased overdose deaths, because the illicit
drug market encourages the sale of more potent forms of prohibited drugs.
35
Drug law
enforcement has been shown to increase overdose mortality, while the provision of
medication-assisted treatment has been found to have the opposite effect.
36
Moreover,
aggressive drug law enforcement has been shown to increase levels of violence related to
22
Office of National Drug Control Policy. 2013 National Drug Control Strategy. Washington, DC: Executive
Office of the President; 2013.
23
Lloyd C. The stigmatization of problem drug users: a narrative literature review. Drugs Educ Prev Policy.
2013;20(2):85–95.
24
Semple SJ, Grant I, Patterson TL. Utilization of drug treatment programs by methamphetamine users: the
role of social stigma. Am J Addict. 2005;14(4):367–380.
25
Lloyd C. Sinning and Sinned Against: The Stigmatisation of Problem Drug Users. York, England: University
of York; 2010.
26
Corrigan PW, Kuwabara SA, O’Shaughnessy J. The public stigma of mental illness and drug addiction:
findings from a stratified random sample. J Soc Work. 2009;9(2):139–147.
27
White WL. Long-Term Strategies to Reduce the Stigma Attached to Addiction, Treatment, and Recovery
Within the City of Philadelphia (With Particular Reference to Medication-Assisted Treatment/Recovery).
Philadelphia, PA: Department of Behavioral Health and Mental Retardation Services; 2009.
28
Friedman SR, Cooper HL, Tempalski B, et al. Relationships of deterrence and law enforcement to drug-
related harms among drug injectors in US metropolitan areas. AIDS. 2006;20(1):93–99.
29
Hughes CE, Stevens A. What can we learn from the Portuguese decriminalization of illicit drugs? Br J
Criminol. 2010;50(6):999–1022.
30
Darke S, Ross J, Hall W. Overdose among heroin users in Sydney, Australia: II. Responses to overdose.
Addiction. 1996;91(3):413–417.
31
Davidson PJ, Ochoa KC, Hahn JA, Evans JL, Moss AR. Witnessing heroin-related overdoses: the experiences
of young injectors in San Francisco. Addiction. 2002;97(12):1511–1516.
32
Ochoa KC, Hahn JA, Seal KH, Moss AR. Overdosing among young injection drug users in San Francisco.
Addict Behav. 2001;26(3):453–460.
33
Pollini RA, McCall L, Mehta SH, Celentano DD, Vlahov D, Strathdee SA. Response to overdose among
injection drug users. Am J Prev Med. 2006;31(3):261–264.
34
Tracy M, Piper TM, Ompad D, et al. Circumstances of witnessed drug overdose in New York City:
implications for intervention. Drug Alcohol Depend. 2005;79(2):181–190.
35
Davies RB. Mandatory minimum sentencing, drug purity and overdose rates. Econ Soc Rev.
2010;41(4):429–457.
36
Nordt C, Stohler R. Combined effects of law enforcement and substitution treatment on heroin mortality.
Drug Alcohol Rev. 2010;29(5):540–545.

63
drug markets: a systematic review revealed that “contrary to the conventional wisdom that
increasing drug law enforcement will reduce violence, the existing scientific evidence
strongly suggests that drug prohibition likely contributes to drug market violence and
higher homicide rates.”
37
The domestic drug war has also been an engine of mass incarceration. With less than 5% of
the world’s population but nearly 25% of its incarcerated population, the United States
imprisons more people (and at a higher rate) than any other nation in the world, largely as
a result of the war on drugs.
38
More than 1.5 million drug arrests occurred in the United
States in 2011. The vast majority—more than 80%—were for possession only, and half
were for marijuana law violations.
39
Seventeen percent (17%) of people in state prisons
and nearly half (48%) of those in federal prisons were incarcerated for a drug law violation
in 2011.
40
Roughly 500,000 Americans are behind bars on any given night for a drug law
violation, 10 times the total in 1980.
41
-
43
Misguided drug laws and disproportionate sentencing requirements have produced grossly
unequal outcomes for communities of color. Although rates of drug use and selling are
comparable across racial and ethnic lines, Blacks and Latinos are far more likely to be
criminalized for drug law violations than Whites.
44
-
46
People of color experience
discrimination at every stage of the judicial system.
47
This is particularly the case for drug
law violations. Blacks make up 13% of the US population and are consistently documented
by the US government to use drugs at rates similar to those among people of other races.
48
However, Blacks account for nearly one-third of drug arrests
and roughly 45% of those
37
Werb D, Rowell G, Guyatt G, Kerr T, Montaner J, Wood E. Effect of drug law enforcement on drug market
violence: a systematic review. IntJ Drug Policy. 2011;22(2):87–94.
38
Walmsley R. World Population List. 9th ed. London, England: International Centre for Prison Studies; 2011.
39
Crime in the United States, 2011. Washington, DC: Federal Bureau of Investigation; 2012.
40
Carson EA, Sabol WJ. Prisoners in 2011. Washington, DC: US Department of Justice, Bureau of Justice
Statistics; 2012.
41
The Sentencing Project. Trends in US corrections: state and federal prison population, 1925–2011.
Available at: http://sentencingproject.org/doc/publications/inc_Trends_in_Corrections_Fact_sheet.pdf.
Accessed December 12, 2013.
42
Beck AJ, Gilliard DK. Prisoners in 1994. Washington, DC: US Department of Justice, Bureau of Justice
Statistics; 1995.
43
Mauer M, King RS. A 25-year quagmire: the war on drugs and its impact on American society. Available at:
http://www.sentencingproject.org/detail/publication.cfm?publication_id=170. Accessed December 12, 2013.
44
Fellner J, Vinck P. Targeting Blacks: Drug Law Enforcement and Race in the United States. New York, NY:
Human Rights Watch; 2008.
45
Nguyen H, Reuter P. How risky is marijuana possession? Considering the role of age, race, and gender.
Crime Delinquency. 2012;58(6):879–910.
46
Tonry M. Punishing Race: A Continuing American Dilemma. New York, NY: Oxford University Press; 2011.
47
Alexander M. The New Jim Crow: Mass Incarceration in the Age of Colorblindness. New York, NY: New
Press; 2012.
48
Rastogi S, Johnson TD, Hoeffel EM Jr. The Black Population: 2010. Washington, DC: US Department of
Commerce; 2011.

64
incarcerated in state and federal prisons for drug law violations.
49
From 1980 to 2007,
Blacks were arrested for drug law violations nationwide at rates 3 to nearly 6 times higher
than Whites.
50
A recent report by the American Civil Liberties Union, for example, showed
that Blacks were arrested for marijuana possession offenses at roughly 4 times the rate of
Whites, although rates of use are essentially no different.
51
Furthermore, Blacks and
Latinos tend to be arrested for crimes that hold more serious punishments, such as selling
drugs rather than just possessing them.
52
-
54
Mass incarceration resulting from the war on drugs has devastated many families and
communities. A 2012 national study published in the American Journal of Public Health
showed that Black youths were less likely than Whites to use or sell drugs but more likely
to be arrested; the researchers concluded that “[r]acial disparities in adolescent arrest
appear to result from differential treatment of minority youths and to have long-term
negative effects on the lives of affected African American youths.”
55
Approximately 2.7
million children are growing up in US households in which one or more parents are
incarcerated. One in 9 Black children have an incarcerated parent, as compared with one in
28 Latino children and one in 57 White children.
56
Punishment for a drug law violation is not only meted out by the US criminal justice system
but also perpetuated by policies denying child custody, voting rights, employment, business
loans, trade licensing, student aid, and public housing and other public assistance to people
with criminal convictions. In addition, criminal records are cited as justification for
deporting legal residents and barring other noncitizens from visiting the United States.
57
Even if a person does not face jail or prison time, a drug conviction record—particularly a
felony—often imposes a lifelong ban on many aspects of social, economic, and political life.
Such exclusions create a permanent second-class status for millions of people and, as with
drug war enforcement itself, fall disproportionately on people of color. According to a 2008
article published in the American Journal of Public Health, “the popular war on drugs
translates to a war on people of color in terms of their overall health and well-being….
49
US Department of Justice. Federal Justice Statistics Program. Available at: http://bjs.ojp.usdoj.gov/fjsrc/.
Accessed December 12, 2013.
50
Fellner J. Decades of Disparity: Drug Arrests and Race in the United States. New York, NY: Human Rights
Watch; 2009.
51
The War on Marijuana in Black and White. Washington, DC: American Civil Liberties Union; 2013.
52
Beckett K. Race, drugs, and law enforcement. Criminology Public Policy. 2012;11(4):641–653.
53
Fellner J. Race, drugs, and law enforcement in the United States. Stanford Law Policy Rev. 2009;20:257.
54
Helms R, Costanza S. Race, politics, and drug law enforcement: an analysis of civil asset forfeiture patterns
across US counties. Policing Soc. 2009;19(1):1–19.
55
Kakade M, Duarte CS, Liu X, et al. Adolescent substance use and other illegal behaviors and racial disparities
in criminal justice system involvement: findings from a US national survey. Am J Public Health.
2012;102(7):1307–1310.
56
Western B, Pettit B. Collateral Costs: Incarceration's Effect on Economic Mobility. Washington, DC: Pew
Charitable Trusts; 2010.
57
Chesney-Lind M, Mauer M. Invisible Punishment: The Collateral Consequences of Mass Imprisonment. New
York, NY: New Press; 2011.

65
Communities of color face an escalating public health problem created by our society’s
solution to imprison those arrested for nonviolent drug offenses.”
58
APHA recognizes that the United States leads the world in incarceration and that the war
on drugs is a major driver of mass incarceration, particularly among people of color. APHA
policy 9123 (Social Practice of Mass Imprisonment) states that APHA has “a long history of
concern and activity aimed at correcting inadequacies in health conditions in correctional
institutions, and is aware that prison health and community health are intimately related
elements of public health in the US with…millions of individuals released annually from
custody to community.” It notes that “APHA has long-defined drug abuse as a public health
problem rather than a criminal justice problem and called for drug treatment to be
available for all who request it.” It further “condemns the social practice that sanctions
mass imprisonment rather than defining and changing those conditions that engender and
accompany criminal behavior, including drug addiction,” and calls for alternatives to
incarceration.
In 2009, in the wake of the XVIII International AIDS Conference in Vienna, Austria, the
international scientific and public health community issued the Vienna Declaration, a
statement seeking to improve community health and safety by calling for the incorporation
of scientific evidence into illicit drug policies. The Vienna Declaration calls for an
acknowledgment of the limits and harms of drug prohibition, for ending the criminalization
of people who use drugs, and for drug policy reform to remove barriers to effective HIV
prevention, treatment, and care.
59
Since then, an increasing number of prominent figures in and sectors of society have raised
their voices against policies that criminalize people who use drugs, in favor of robust,
health-centered alternatives. In 2011, former presidents Fernando Henrique Cardoso
(Brazil), Cesar Gaviria (Colombia), and Ernesto Zedillo (Mexico) joined with former UN
secretary general Kofi Annan, former US secretary of state George Shultz, former Federal
Reserve Board chairman Paul Volcker, former Swiss president Ruth Dreifuss, and other
members of the Global Commission on Drug Policy (GCDP) to launch a landmark report
calling for fundamental reforms to national and global drug policies, including (1)
acknowledging the failure of the “war on drugs” and its disastrous impact on human rights,
violence, and corruption; (2) replacing the criminalization and punishment of people who
use drugs with the offer of health and treatment services to those who need them; and (3)
encouraging governments to experiment with models of legal regulation to undermine the
power of organized crime and safeguard people’s health and security.
60
In advance of the
58
Moore LD, Elkavich A. Who’s using and who’s doing time: incarceration, the war on drugs, and public
health. Am J Public Health. 2008;98(5):782–786.
59
The Vienna Declaration. Available at: http://www.viennadeclaration.com/. Accessed December 12, 2013.
60
Report of the Global Commission on Drug Policy. Rio de Janeiro, Brazil: Global Commission on Drug Policy;
2011.

66
International AIDS Conference in Washington, DC, the GCDP issued a second report in June
2012, The War on Drugs and HIV/AIDS, which was successful in exposing the causal links
between the HIV pandemic and the criminalization of drug use.
The GCDP has since been joined by former presidents Jorge Sampaio (Portugal), Alexander
Kwasniewski (Poland), and Ricardo Lagos (Chile). Former US presidents Jimmy Carter and
Bill Clinton have echoed most or all of the commission’s recommendations, as has former
president Vicente Fox of Mexico. In 2013, the GCDP issued a third report, The Negative
Impact of the War on Drugs on Public Health: The Hidden Hepatitis C Epidemic, which
again called for the decriminalization of drug use and the expansion of proven, science-
based solutions to reduce hepatitis C, including sterile syringe access, supervised injection
facilities, and heroin prescription programs.
61
Against this backdrop, the Organization of American States issued a groundbreaking, 2-part
report in May 2013 in which it critically examined the current war on drugs and considered
new approaches for the future, giving equal weight to options such as decriminalization
and harm reduction.
62
Among the report’s conclusions is the urgent need for a “public
health approach” to address drug problems, and it specifies that “the decriminalization of
drug use needs to be considered as a core element in any public health strategy.”
63
In June 2013, Human Rights Watch publicly condemned “[n]ational drug control policies
that impose criminal penalties for personal drug use” as a violation of human rights, stating
that the “criminalization of drug use has undermined the right to health” because “fear of
criminal penalties deters people who use drugs from using health services and treatment,
and increases their risk of violence, discrimination, and serious illness.” Its statement
continues, “Criminal prohibitions have also impeded the use of drugs for legitimate medical
research, and have prevented patients from accessing drugs for palliative care and pain
treatment,” a harm well documented in the literature.
64
It concludes by urging governments
to “rely instead on non-penal regulatory and public health policies.”
65
And in November
2012, Colorado and Washington became the first political jurisdictions in the world to vote
to permit the legal regulation of marijuana sales, cultivation, and distribution among adults
21 years of age and older within their borders, and both states are in the process of
61
The Negative Impact of the War on Drugs on Public Health: The Hidden Hepatitis C Epidemic. Rio de
Janeiro, Brazil: Global Commission on Drug Policy; 2013.
62
Scenarios for the Drug Problem in the Americas: 2013–2025. Washington, DC: Organization of American
States; 2013.
63
The Drug Problem in the Americas: Analytical Report. Washington, DC: Organization of American States;
2013.
64
Nickerson JW, Attaran A. The inadequate treatment of pain: collateral damage from the war on drugs. PLoS
Med. 2012;9(1):e1001153.
65
Human Rights Watch. Americas: decriminalize personal use of drugs; reform policies to curb violence,
abuse. Available at: http://www.hrw.org/news/2013/06/04/americas-decriminalize-personal-use-drugs.
Accessed December 12, 2013.

67
implementing their new laws in such a way as to strengthen public safety and health to the
maximum extent possible.
Joining those distinguished colleagues and peers, APHA agrees that the criminalization of
people who use illicit drugs is fueling the HIV epidemic and has resulted in overwhelmingly
negative health and social consequences, and that a full policy reorientation is needed.
Proposed Recommendations Statement
APHA policies 7121 and 8817(PP) call for a reorientation of current US drug policies, and
APHA also has adopted longstanding policies that support several aspects of a health-based
response to drug misuse. Policy 8817(PP) urges a “redirection of current War on Drugs
policies, which are seriously flawed and have little chance of alleviating the serious drug
problems facing our society today.”
The present policy statement identifies the following proposals as vital elements of the
redirection in US drug policy envisioned by APHA’s existing policy statements, toward the
adoption and implementation of a truly public health approach to reducing the harms of
drug misuse.
End the criminalization of drug possession and people who use drugs: APHA’s policies
7121 and 8817(PP) recommend the removal of criminal penalties for drug use.
Policy 7121
first expressed APHA’s belief that people who use drugs should not be criminalized:
“because substance abuse is viewed primarily as a public health problem, this Association
recommends that no punitive measures be taken against the users of alcohol, marijuana, or
other substances when no other illegal act has been committed.”
APHA reiterated its belief that drug misuse must be primarily addressed as a public health
issue, resolving in policy 8817(PP) that “[s]trict punitive measures should not take priority
over drug treatment and prevention goals…punitive measures have only a limited impact
on drug use and problem rates and, in many cases, have been shown to have an underlying
purpose to discriminate against disadvantaged groups.” Policy 8817(PP) further
recommends that US drug policy give “high priority to prevention, treatment and recovery”
and that “punitive measures should be used with caution and should play a secondary
role.… Particular attention should be given to the special needs of young people and
disenfranchised groups and caution must be exercised to avoid discriminatory policies.”
Countries that have ended the criminalization of drug use and possession have generally
been better able to cope with injection drug–related HIV/AIDS. Decriminalizing drug
possession and investing in treatment and harm reduction services can provide several
major benefits for public health, including reducing the number of people incarcerated;
increasing uptake into drug treatment; reducing criminal justice costs and redirecting
resources from criminal justice to health systems; redirecting law enforcement resources

68
to prevent serious and violent crime; addressing racial disparities in drug law enforcement,
incarceration, and related health characteristics and outcomes; minimizing stigma and
creating a social, cultural, and policy climate in which people who use drugs are less fearful
of seeking and accessing treatment, using harm reduction services, and receiving HIV/AIDS
services; and protecting people from the wide-ranging and debilitating consequences of a
criminal conviction.
Some countries particularly stand out. In 2001, Portuguese legislators enacted a
comprehensive form of decriminalization of low-level possession and consumption of all
illicit drugs and reclassified these activities as administrative violations.
A person caught
with personal-use amounts of any drug in Portugal is no longer arrested but, rather,
ordered to appear before a local “dissuasion commission” composed of 3 officials (one from
the legal arena and a pair from the health arena) who determine whether and to what
extent the person is addicted to drugs. On the basis of these findings, the commission can
order someone to attend a treatment program, complete other monitoring activities, pay a
fine, or submit to other administrative sanctions. Drug trafficking and non-drug offenses
remain illegal and are still processed through the criminal justice system.
The decriminalization policy was part of a comprehensive health-oriented approach to
addressing problematic drug use, especially unsafe injecting drug use, that also included a
major expansion of treatment and harm reduction services. New diagnoses of HIV and AIDS
among people who inject drugs have also declined in Portugal. Between 2000 and 2008, the
number of cases of HIV among people who inject drugs declined from 907 to 267, and the
number of AIDS cases decreased from 506 to 108. These highly significant declines are
largely attributable to the increased provision of harm reduction services and efforts made
possible by decriminalization.
66
In addition, research has shown no significant increases in overall illicit drug use among
adults in Portugal, and any slight increases in lifetime use of some drugs appear to be part
of a regional trend. More importantly, adolescent drug use, as well as problematic drug
use—defined as use by people deemed to be dependent or addicted and by people who
inject drugs—has decreased overall since 2003.
The number of people arrested and sent to
criminal courts for drug law violations declined by more than half after decriminalization.
The percentage of people in Portugal’s prison system as a result of drug-related offenses
also decreased by about half, from 44% in 1999 to 21% in 2008.
These positive outcomes cannot be attributed to decriminalization alone. Alongside its
decriminalization law, Portugal significantly expanded its treatment and harm reduction
services, including access to sterile syringes as well as methadone maintenance therapy
and other medication-assisted treatments. Between 1998 and 2008, the number of people
66
Domoslawski A, Siemaszko H. Drug Policy in Portugal: The Benefits of Decriminalizing Drug Use.
Washington, DC: Open Society Institute; 2011.

69
in drug treatment increased by more than 60% (from 23,654 to 38,532 people). The
percentage of drug-related deaths in which opiates were the primary substance involved
declined from 95% in 1999 to 59% in 2008.
On the basis of such evidence and APHA’s longstanding policies, eliminating criminal
penalties for personal drug use and possession is an essential feature of a public health
response to drugs and drug misuse, and APHA calls on state and federal governments to
remove such criminal penalties.
Expand access to harm reduction interventions: Harm reduction programs including sterile
syringe access, supervised injection facilities, and medication-assisted treatment should be
scaled up to eliminate HIV and hepatitis C transmission among people who inject drugs.
Interventions that have proven effective in other countries should be evaluated for
implementation in the United States, and legal and political barriers to programs with
evidence of effectiveness should be removed. Treatment providers, health professionals
(including primary care physicians), community health workers (CHWs), and other
stakeholders should receive professional preparation and training with respect to proven
treatment and harm reduction interventions. CHWs play a critical role in making contact
and building trust with hard-to-reach, drug-using populations at high risk and connecting
them to health services or delivering those services to them. To expand access to these
harm reduction and treatment services to every person in need, CHWs must be empowered
to deliver cost-effective interventions such as syringe access programs, secondary syringe
exchange services, low-threshold methadone maintenance, peer education programs, and
HIV/AIDS testing, education, and links to treatment. Criminalization, by contrast, makes the
essential harm reduction functions of CHWs more difficult or even impossible.
Restricting access to sterile syringes among people who inject drugs has been proven to
lead to syringe sharing, a major cause of HIV infections. According to the CDC, people who
inject drugs represented 9% (4,500) of all estimated new HIV infections in 2009, an annual
figure that has not changed significantly since 2006.
67
Such restrictions persist despite
conclusive evidence from more than 200 studies conducted in the United States and abroad
showing that expanding sterile syringe access—through syringe exchange programs and
non-prescription sales of syringes—is a cost-effective means of reducing the spread of HIV
and viral hepatitis and that these programs do not contribute to increased drug use, drug
67
Estimates of New HIV Infections in the United States, 2006–2009. Atlanta, GA: Centers for Disease Control
and Prevention; 2011.

70
injection, crime, or unsafe discarding of syringes.
68
-
75
According to a CDC-funded study
published in the Journal of the American Medical Association, syringe access has helped
reduce HIV incidence among people who inject drugs in the United States by 80% in the
past decade.
76
Current APHA policy in this regard recognizes “the critical importance of
access to sterile syringes to prevent disease spread, and the effectiveness of increasing
sterile syringe access in reducing risk behavior”; it “urges states that criminalize possession
of prescribed syringes for injection of illicit substances to modify their laws or policies to
permit such possession.”
Sterile syringe access programs are integral elements of a
comprehensive health response to problematic drug use, are necessary to reach the goal of
an AIDS-free generation, and should be funded at the local, state, and national levels toward
the goal of providing a sterile syringe for every injection.
Medically supervised injection facilities (SIFs) are controlled health care settings where
people who use drugs can more safely do so under clinical supervision and receive health
care, counseling, and referral to health and social services, including drug treatment. There
are currently 92 SIFs operating in 62 cities around the world, but none in the United States.
SIFs are proven to reduce unsafe injecting practices and the transmission of bloodborne
viruses; prevent overdose fatalities; increase access or referrals to treatment programs,
including medication-assisted treatment and detoxification services; decrease societal
costs associated with emergency room visits and crime; and reduce the social harms
68
Belani HK, Muennig PA. Cost-effectiveness of needle and syringe exchange for the prevention of HIV in New
York City. J HIV/AIDS Soc Serv. 2008;7(3):229–240.
69
Lurie P, Gorsky R, Jones TS, Shomphe L. An economic analysis of needle exchange and pharmacy-based
programs to increase sterile syringe availability for injection drug users. J Acquir Immune Defic Syndr Hum
Retrovirol. 1998;18(suppl 1):S126–S132.
70
Schackman BR, Gebo KA, Walensky RP, et al. The lifetime cost of current human immunodeficiency virus
care in the United States. Med Care. 2006;44(11):990–997.
71
Centers for Disease Control and Prevention. Syringe exchange programs—United States, 2008. MMWR
Morb Mortal Wkly Rep. 2010;59(45):1488–1491.
72
Lambert EY, Cesari HK, Stein JB. Principles of HIV Prevention in Drug-Using Populations: A Research-Based
Guide. Bethesda, MD: National Institute on Drug Abuse; 2002.
73
Marx MA, Crape B, Brookmeyer RS, et al. Trends in crime and the introduction of a needle exchange
program. Am J Public Health. 2000;90(12):1933–1936.
74
Palmateer N, Kimber J, Hickman M, Hutchinson S, Rhodes T, Goldberg D. Evidence for the effectiveness of
sterile injecting equipment provision in preventing hepatitis C and human immunodeficiency virus
transmission among injecting drug users: a review of reviews. Addiction. 2010;105(5):844–859.
75
Des Jarlais DC, Perlis T, Arasteh K, et al. Reductions in hepatitis C virus and HIV infections among injecting
drug users in New York City, 1990–2001. AIDS. 2005;19(suppl 3):S20–S25.
76
Hall HI, Song R, Rhodes P, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300(5):520–
529.

71
associated with injection drug use, such as public disorder, public intoxication, public
injecting, and publicly discarded syringes.
77
-
80
Medication-assisted treatments, most commonly opioid-substitution programs (also called
narcotic replacement therapies), have demonstrated success in improving the lives and the
health of people who use heroin and other opioids. Such therapies include methadone and
buprenorphine,
as well as pharmaceutical heroin treatment, and they have proven
successful in many countries.
81
-
83
Denial of these treatments can result in untreated
addiction, preventable HIV risk behaviors, and heightened vulnerability to fatal
overdose.
84
,
85
APHA took a leading position in 1970 when it supported “further experimentation with
organized maintenance programs using methadone and similar compounds, subject to
appropriate supervision and evaluation,” in policy 7015. One year earlier, policy 6907 had
resolved:
“The American Public Health Association believes that the illicit profit incentive involved in
the sale of drugs to drug addicts not only contributes to their misery but puts at risk entire
communities in the United States, unnecessarily submitting its citizens to muggings,
robberies, injuries and in some instances murder, while constantly contributing to the
profits of gangsters and Mafia-like organizations. APHA…declares that it will seek and
support state and federal legislation to eliminate the profit motive in the illicit sale of
drugs…by making medically approved drugs and regimens of the most suitable and
clinically evaluated methods readily available to known drug addicts at specially
designated health centers equipped with professional staffs competent to deal with the
comprehensive rehabilitation of the addict by means of: Medical care…psychological and
77
Kerr T, Wood E, Montaner J, Tyndall M. Findings from the Evaluation of Vancouver’s Pilot Medically
Supervised Safer Injection Facility—Insite. Vancouver, British Columbia, Canada: Centre for Excellence in
HIV/AIDS; 2009.
78
Schatz E, Nougier M. Drug Consumption Rooms: Evidence and Practice. London, England: International
Drug Policy Consortium; 2012.
79
Semaan S, Fleming P, Worrell C, Stolp H, Baack B, Miller M. Potential role of safer injection facilities in
reducing HIV and hepatitis C infections and overdose mortality in the United States. Drug Alcohol Depend.
2011;118(2–3):100–110.
80
Maher L, Salmon A. Supervised injecting facilities: how much evidence is enough? Drug Alcohol Rev.
2007;26(4):351–353.
81
Mattick RP, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement
therapy for opioid dependence. Cochrane Database Syst Rev. 2009;3:CD002209.
82
Gowing L, Farrell M, Bornemann R, Sullivan L, Ali R. Substitution treatment of injecting opioid users for
prevention of HIV infection. Cochrane Database Syst Rev. 2008;2:CD004145.
83
Gowing L, Ali R, White JM. Buprenorphine for the management of opioid withdrawal. Cochrane Database
Syst Rev. 2009;3:CD002025.
84
McKenzie M, Zaller N, Dickman SL, et al. A randomized trial of methadone initiation prior to release from
incarceration. Substance Abuse. 2011;33(1):19–29.
85
Substitution Maintenance Therapy in the Management of Opioid Dependence and HIV/AIDS Prevention.
Geneva, Switzerland: World Health Organization; 2004.

72
psychiatric counseling; social, economic, and welfare counseling aimed at increased
employability [and] provision of the necessary funding to enable states, communities, and
consumer action groups to give priority and coordinated action to implement
establishment of such centers.”
Since that time the CDC,
86
the Institute of Medicine,
87
the National Institutes of Health,
88
the
Substance Abuse and Mental Health Services Administration (SAMHSA),
89
the National
Institute on Drug Abuse,
90
,
91
the World Health Organization (WHO),
92
and more than 4
decades of government-funded, peer-reviewed medical research have unequivocally and
repeatedly proven that substitution therapies such as methadone maintenance are the
most effective treatments for opioid dependence.
93
-
98
Methadone, buprenorphine, and
other existing medication-assisted treatments should be expanded to serve all who need
them. Indeed, according to the National Institutes of Health, “all opiate-dependent persons
under legal supervision should have access to methadone maintenance therapy.” Yet, few
opioid-dependent people in the United States have access to these treatments; according to
SAMHSA, only 9% of substance abuse treatment facilities in the country offer specialized
treatment of opioid dependence with methadone or buprenorphine.
99
Publicly funded
treatment programs are far less likely than privately funded programs to offer opioid
replacement therapies.
100
86
Centers for Disease Control and Prevention. Methadone maintenance treatment. Available at:
http://www.cdc.gov/idu/facts/Methadone.htm. Accessed December 12, 2013.
87
Rettig RA, Yarmolinsky A. Federal Regulation of Methadone Treatment. Washington, DC: National Academy
Press; 1995.
88
Effective Medical Treatment of Opiate Addiction. Bethesda, MD: National Institutes of Health; 1997.
89
Medication-Assisted Treatment for Opioid Addiction in Opioid Treatment Programs. Rockville, MD: Center
for Substance Abuse Treatment; 2005.
90
National Institute on Drug Abuse. Research report: heroin abuse and addiction. Available at:
http://www.drugabuse.gov/ResearchReports/heroin/heroin.html. Accessed December 12, 2013.
91
Methadone Research Web Guide. Bethesda, MD: National Institute on Drug Abuse; 2007.
92
Substitution Maintenance Therapy in the Management of Opioid Dependence and HIV/AIDS Prevention.
Geneva, Switzerland: World Health Organization; 2004.
93
Ball JC, Ross A. The Effectiveness of Methadone Maintenance Treatment: Patients, Programs, Services, and
Outcome. New York, NY: Springer-Verlag; 1991.
94
Fiellin DA, O’Connor PG, Chawarski M, Pakes JP, Pantalon MV, Schottenfeld RS. Methadone maintenance in
primary care: a randomized controlled trial. JAMA. 2001;286(14):1724–1731.
95
Novick DM, Joseph H. Medical maintenance: the treatment of chronic opiate dependence in general medical
practice. J Subst Abuse Treat. 1991;8(4):233–239.
96
Hser YI, Hoffman V, Grella CE, Anglin MD. A 33-year follow-up of narcotics addicts. Arch Gen Psychiatry.
2001;58(5):503–508.
97
Ward J, Hall W, Mattick RP. Role of maintenance treatment in opioid dependence. Lancet.
1999;353(9148):221–226.
98
Catania H. About Methadone and Buprenorphine. Revised 2nd ed. New York, NY: Drug Policy Alliance;
2006.
99
National Survey of Substance Abuse Treatment Services: 2011 Data. Rockville, MD: Substance Abuse and
Mental Health Services Administration; 2013.
100
Abraham AJ, Knudsen HK, Rieckmann T, Roman PM. Disparities in access to physicians and medications
for the treatment of substance use disorders between publicly and privately funded treatment programs in
the United States. J Stud Alcohol Drugs. 2013;74(2):258.

73
Medication-assisted treatment models for opioid dependence using diacetylmorphine
(heroin) have been safely and successfully implemented in several countries and are now
well supported in the academic literature as one tool in an effective, health-based response
to problematic drug use, especially among those who have not responded to conventional
treatments.
101
-
115
A systematic review of all published studies to date on heroin-assisted
treatment (HAT) showed significant reductions in illicit drug use and crime and
improvements in the health of participants. An important article in the New England
Journal of Medicine on the success of the North American Opioid Medication Initiative in
Canada, which provided heroin by prescription to a select group of people who had not
responded to other forms of treatment, reported a two-thirds (67%) reduction in illicit
drug use and other illegal activity.
Similar reductions in illicit heroin use were reported
from HAT trials in the United Kingdom (72%) and Germany (69%). HAT is not only more
101
Blanken P, Hendriks VM, Koeter MW, van Ree JM, van den Brink W. Craving and illicit heroin use among
patients in heroin-assisted treatment. Drug Alcohol Depend. 2012;120(1–3):74–80.
102
Blanken P, van den Brink W, Hendriks VM, et al. Heroin-assisted treatment in the Netherlands: history,
findings, and international context. Eur Neuropsychopharmacol. 2010;20:S105–S158.
103
Ferri M, Davoli M, Perucci CA. Heroin maintenance for chronic heroin-dependent individuals. Cochrane
Database Syst Rev. 2011;12:CD003410.
104
Fischer B, Oviedo-Joekes E, Blanken P, et al. Heroin-assisted treatment (HAT) a decade later: a brief update
on science and politics. J Urban Health. 2007;84(4):552–562.
105
Haasen C, Verthein U, Degkwitz P, Berger J, Krausz M, Naber D. Heroin-assisted treatment for opioid
dependence: randomised controlled trial. Br J Psychiatry. 2007;191:55–62.
106
Oviedo-Joekes E, Brissette S, Marsh DC, et al. Diacetylmorphine versus methadone for the treatment of
opioid addiction. N Engl J Med. 2009;361(8):777–786.
107
Oviedo-Joekes E, March JC, Romero M, Perea-Milla E. The Andalusian trial on heroin-assisted treatment: a
2 year follow-up. Drug Alcohol Rev. 2010;29(1):75–80.
108
Petrushevska T. Heroin maintenance treatment—are further investigations needed? Macedonian J Med
Sci. 2012;5(4):453–461.
109
Strang J, Groshkova T, Metrebian N. New heroin-assisted treatment: recent evidence and current practices
of supervised injectable heroin treatment in Europe and beyond. Available at:
http://www.emcdda.europa.eu/attachements.cfm/att_154996_EN_Heroin%20Insight.pdf. Accessed
December 12, 2013.
110
Strang J, Metrebian N, Lintzeris N, et al. Supervised injectable heroin or injectable methadone versus
optimised oral methadone as treatment for chronic heroin addicts in England after persistent failure in
orthodox treatment (RIOTT): a randomised trial. Lancet. 2010;375(9729):1885–1895.
111
Uchtenhagen A. Heroin-assisted treatment in Switzerland: a case study in policy change. Addiction.
2010;105(1):29–37.
112
Killias M, Aebi MF, Jurist K. The impact of heroin prescription on heroin markets in Switzerland. Crime
Prev Stud. 2000;11:83–100.
113
Nordt C, Stohler R. Incidence of heroin use in Zurich, Switzerland: a treatment case register analysis.
Lancet. 2006;367(9525):1830–1834.
114
Verthein U, Bonorden-Kleij K, Degkwitz P, et al. Long-term effects of heroin-assisted treatment in
Germany. Addiction. 2008;103(6):960–966.
115
Reuter P. Can Heroin Maintenance Help Baltimore? Baltimore, MD: Abell Foundation; 2009.

74
effective in reducing street heroin (and other drug) use than methadone, but it has also
proven to be more cost-effective.
116
,
117
Emerging literature on treating stimulant dependence with the administration of agonists
or partial agonists, such as dextroamphetamine,
118
-
120
methylphenidate,
121
and
modafinil,
122
,
123
has shown favorable results. Such treatments utilizing opioid and
stimulant agonist and/or partial agonist substitution clearly merit research into their
feasibility in the United States and should be adopted as part of the US treatment response
if evaluations prove favorable.
124
Opposing Arguments/Evidence
Opponents of the health-based drug policies called for in the present policy statement often
claim that the criminalization of people who use drugs is effective in reducing drug use. As
a corollary, it is often argued that reducing or eliminating criminal penalties for drug
possession or expanding access to harm reduction services such as syringe exchanges,
supervised injection facilities, or medication-assisted treatments enables problematic drug
use; promotes the initiation of drug use; increases rates of drug misuse, crime, and related
problems; and worsens public health and public safety.
Yet, available evidence does not support these assertions. Not only has the dominant drug
war paradigm completely failed to curb drug use or supply, but the evidence consistently
shows that this approach has significantly amplified the harms of drug misuse and
addiction. A recent evaluation by the Government Accountability Office (GAO) issued in
March 2013 showed that the Office of National Drug Control Policy (ONDCP) and the
federal government “have not made progress toward achieving most of the goals
116
Verthein U, Haasen C, Reimer J. Switching from methadone to diamorphine: 2-year results of the German
heroin-assisted treatment trial. Subst Use Misuse. 2011;46(8):980–991.
117
Nosyk B, Guh DP, Bansback NJ, et al. Cost-effectiveness of diacetylmorphine versus methadone for chronic
opioid dependence refractory to treatment. CMAJ. 2012;184(6):E317–E328.
118
Longo M, Wickes W, Smout M, Harrison S, Cahill S, White JM. Randomized controlled trial of
dexamphetamine maintenance for the treatment of methamphetamine dependence. Addiction.
2010;105(1):146–154.
119
White R. Dexamphetamine substitution in the treatment of amphetamine abuse: an initial investigation.
Addiction. 2000;95(2):229–238.
120
Grabowski J, Rhoades H, Schmitz J, et al. Dextroamphetamine for cocaine-dependence treatment: a double-
blind randomized clinical trial. J Clin Psychopharmacol. 2001;21(5):522.
121
Vansickel AR, Fillmorex MT, Hays LR, Rush CR. Effects of potential agonist-replacement therapies for
stimulant dependence on inhibitory control in cocaine abusers. Am J Drug Alcohol Abuse. 2008;34(3):293–
305.
122
Dackis CA, Kampman KM, Lynch KG, Pettinati HM, O’Brien CP. A double-blind, placebo-controlled trial of
modafinil for cocaine dependence. Neuropsychopharmacology. 2005;30(1):205–211.
123
Hart CL, Haney M, Vosburg SK, Rubin E, Foltin RW. Smoked cocaine self-administration is decreased by
modafinil. Neuropsychopharmacology. 2008;33(4):761–768.
124
Reuter P. Can heroin maintenance help Baltimore? What Baltimore can learn from the experience of other
countries. Available at: http://www.abell.org/pubsitems/cja_HeroinMaintenance_0209.pdf Accessed
December 12, 2013.

75
articulated in the 2010 National Drug Control Strategy.” The GAO concluded that, in terms
of reducing youth drug use, overdose fatalities, and HIV caused by injection drug use, the
ONDCP not only has been unsuccessful but in fact has lost ground.
125
Aggressive drug law enforcement practices—and the resulting fear of arrest—drive many
people who inject drugs into environments where HIV risks are greatly elevated and away
from HIV testing, prevention, and other public health services.
126
,
127
Two studies published
in the American Journal of Public Health further demonstrate that aggressive drug law
enforcement exacerbates public health risks among people who use drugs. The first, a 2012
analysis of the relationship between arrest rates for heroin and cocaine offenses and the
prevalence of injection drug use from 1992 to 2002, revealed that “deterrence-based
approaches to reducing drug use seem not to reduce IDU prevalence” and that “alternative
approaches such as harm reduction, which prevents HIV transmission and increases
referrals to treatment, may be a better foundation for policy.”
128
The second, a 2005 study
of intense street-level enforcement near syringe exchange program sites in Philadelphia,
showed that utilization of such programs fell significantly as a result of increased drug law
enforcement.
129
After studying nearly a hundred metropolitan areas in the United States, researchers found
that repressive drug law enforcement was correlated with increased HIV prevalence
among people who inject drugs. The researchers concluded: “This may be because fear of
arrest and/or punishment leads drug injectors to avoid using syringe exchanges, or to
inject hurriedly or to inject in shooting galleries or other multi-person injection settings to
escape detection.” Criminalization also erects multiple barriers to both HIV and drug
treatment.
130
,
131
Research demonstrates that people who use drugs tend to have lower
rates of antiretroviral therapy utilization and higher rates of death due to HIV/AIDS. What
is more, these factors also seriously interfere with the front-line work of CHWs to reach out
to, engage, recruit, and retain hard-to-reach people in health programs, especially low-
threshold and secondary harm reduction services.
125
Office of National Drug Control Policy: Office Could Better Identify Opportunities to Increase Program
Coordination. Washington, DC: US Government Accountability Office; 2013.
126
Kerr T, Small W, Wood E. The public health and social impacts of drug market enforcement: a review of the
evidence. Int J Drug Policy. 2005;16(4):210–220.
127
Strathdee SA, Hallett TB, Bobrova N, et al. HIV and risk environment for injecting drug users: the past,
present, and future. Lancet. 2010;376(9737):268–284.
128
Friedman SR, Pouget ER, Chatterjee S, et al. Drug arrests and injection drug deterrence. Am J Public Health.
2011;101(2):344–349.
129
Davis CS, Burris S, Kraut-Becher J, Lynch KG, Metzger D. Effects of an intensive street-level police
intervention on syringe exchange program use in Philadelphia, Pa. Am J Public Health. 2005;95(2):233–236.
130
Wolfe D, Carrieri MP, Shepard D. Treatment and care for injecting drug users with HIV infection: a review
of barriers and ways forward. Lancet. 2010;376(9738):355–366.
131
Wood E, Kerr T, Tyndall MW, Montaner JS. A review of barriers and facilitators of HIV treatment among
injection drug users. AIDS. 2008;22(11):1247–1256.

76
Moreover, empirical evidence from jurisdictions around the world has demonstrated
rather conclusively that policies that eliminate criminal penalties for drug possession or
allow limited drug availability do not increase drug use to any appreciable degree.
Specifically, jurisdictions that have legalized medical marijuana, decriminalized possession
of marijuana and/or other drugs, or tolerated limited, retail sales (e.g., recreational
marijuana “coffee shops” in the Netherlands) have not experienced significant, if any,
increases in marijuana or other drug use.
132
-
143
A new study published in the American
Journal of Public Health, for instance, revealed that adolescent marijuana has not increased
in states with medical marijuana laws.
144
Empirical evidence from countries that have
adopted less punitive policies toward drug possession shows that these countries have not
experienced any significant increases in drug use, drug-related harm, or drug-related crime
relative to more punitive countries.
145
A WHO study of lifetime drug use rates among 17
countries showed that the United States had the highest drug use rates by a wide margin,
despite its punitive drug policies, noting that the US, which has been driving much of the
world’s drug research and drug policy agenda, stands out with higher levels of use of
alcohol, cocaine, and cannabis, despite more punitive illegal drug policies…than many
comparable developed countries. Clearly, by itself, a punitive policy towards possession
and use accounts for limited variation in nation-level rates of drug use.”
132
Degenhardt L, Chiu W-T, Sampson N, et al. Toward a global view of alcohol, tobacco, cannabis, and cocaine
use: findings from the WHO World Mental Health Surveys. PLoS Med. 2008;5(7):e141.
133
Room R. Cannabis Policy: Moving Beyond Stalemate. New York, NY: Oxford University Press; 2010.
134
Reinarman C, Cohen PDA, Kaal HL. The limited relevance of drug policy: cannabis in Amsterdam and in San
Francisco. Am J Public Health. 2004;94(5):836–842.
135
Harper S, Strumpf EC, Kaufman JS. Do medical marijuana laws increase marijuana use? Replication study
and extension. Ann Epidemiol. 2012;22(3):207–212.
136
Single EW. The impact of marijuana decriminalization: an update. J Public Health Policy. 1989;10(4):456–
466.
137
MacCoun RJ, Reuter P. Drug War Heresies: Learning From Other Vices, Times, and Places. Cambridge,
England: Cambridge University Press; 2001.
138
Reuter P. Marijuana Legalization: What Can Be Learned From Other Countries. Santa Monica, CA: RAND;
2010.
139
MacCoun RJ. What can we learn from the Dutch cannabis coffeeshop system? Addiction.
2011;106(11):1899–1910.
140
Vuolo M. National-level drug policy and young people’s illicit drug use: a multilevel analysis of the
European Union. Drug Alcohol Depend. 2013;131(1–2):149–156.
141
Joy JE, Watson SJ, Benson JA. Marijuana and Medicine: Assessing the Science Base. Washington, DC:
Institute of Medicine; 1999.
142
Gorman DM, Huber CJ Jr. Do medical cannabis laws encourage cannabis use? Int J Drug Policy.
2007;18(3):160–167.
143
O’Keefe K, Earleywine M. Marijuana Use by Young People: The Impact of State Medical Marijuana Laws.
Washington, DC: Marijuana Policy Project; 2011.
144
Lynne-Landsman SD, Livingston MD, Wagenaar AC. Effects of state medical marijuana laws on adolescent
marijuana use. Am J Public Health. 2013;103(8):1500–1506.
145
Johnston L, Bachman J, O’Malley P. Marijuana Decriminalization: The Impact on Youth 1975–1980. Ann
Arbor, MI: University of Michigan; 1981.

77
The Portuguese experience is particularly noteworthy; as described above, it has not
resulted in any significant increases in overall illicit drug use among adults.
In fact,
Portugal’s drug use rates remain below the European average and are far lower than those
in the United States.
Overall, evidence after 10 years shows that none of the fears of drug
war proponents have come to pass. According to the United Nations Office on Drugs and
Crime, “Portugal’s policy has reportedly not led to an increase in drug tourism. It also
appears that a number of drug-related problems have decreased.”
146
A new study of
European Union countries showed that countries such as Portugal that have decriminalized
the use and possession of all drugs have not experienced increases in rates of monthly drug
use and, in fact, have lower rates of use than countries with punitive policies.
Nor have harm reduction interventions such as syringe access, SIFs, and medication-
assisted treatments been shown to increase drug use. Syringe access programs, on the
contrary, have been proven not to contribute to increased drug use, drug injection, crime,
or unsafe discarding of syringes.
SIFs reduce the social harms associated with injection
drug use, such as public disorder, public intoxication, public injecting, and publicly
discarded syringes. Several dozen published articles in peer-reviewed journals have
confirmed the positive public health impact of SIFs, including 2 articles published in the
American Journal of Public Health showing that the SIF located in Vancouver, Canada, has
succeeded in attracting and retaining a population of injection drug users who are at
heightened risk for infectious disease and overdose without increasing initiation into
injection drug use.
147
,
148
The evidence is similarly (and uniformly) positive for HAT
programs: far from enabling drug use, these programs reduce illicit drug use and crime. In
fact, many HAT participants freely choose to move on to another form of treatment (such as
methadone) or to become abstinent, while others continue to receive HAT treatment on a
long-term basis, with lasting positive results.
149
,
150
Alternative Strategies
Some policymakers, academics, and commentators have suggested that, rather than
removing or reducing criminal penalties or investing in harm reduction services, US drug
policies should focus on delivering drug treatment through the criminal justice system,
146
World Drug Report 2009. Vienna, Austria: United Nations Office on Drugs and Crime; 2009.
147
Wood E, Tyndall MW, Qui Z, Zhang R, Montaner JSG, Kerr T. Service uptake and characteristics of injection
drug users utilizing North America’s first medically supervised safer injecting facility. Am J Public Health.
2006;96(5):770–773.
148
Kerr T, Tyndall MW, Zhang R, Lai C, Montaner JS, Wood E. Circumstances of first injection among illicit
drug users accessing a medically supervised safer injection facility. Am J Public Health. 2007;97(7):1228–
1230.
149
Rehm J, Gschwend P, Steffen T, Gutzwiller F, Dobler-Mikola A, Uchtenhagen A. Feasibility, safety, and
efficacy of injectable heroin prescription for refractory opioid addicts: a follow-up study. Lancet.
2001;358(9291):1417–1420.
150
Blanken P, Hendriks VM, van Ree JM, van den Brink W. Outcome of long-term heroin-assisted treatment
offered to chronic, treatment-resistant heroin addicts in the Netherlands. Addiction. 2010;105(2):300–308.

78
mainly in the form of an ever-growing number of drug court programs. The 2013 National
Drug Control Strategy, for example, “supports alternatives to incarceration such as drug
courts, diversion programs, enhanced probation and parole programs, and other
supervision strategies” and calls for an increase in the country’s already significant
investment in drug courts. Some evaluations have shown reductions in drug use and
recidivism for the duration of time that people are sentenced to drug court.
151
However, available evidence shows that coerced treatment programs, such as drug courts,
are costly, are no more effective than voluntary treatment, serve very few people, and often
deny proven treatment modalities such as methadone and buprenorphine.
152
-
156
A recent
survey of drug courts revealed that while nearly every drug court in the country serves
participants who are opioid dependent, fewer than half offer medication-assisted
treatments such as methadone. Most drug courts have not significantly reduced
participants’ chances of incarceration either.
In fact, one study showed that because of drug
courts’ nearly exclusive focus on low-level drug (especially marijuana) possession offenses,
their strict eligibility requirements, and underlying sentencing laws (e.g., mandatory
minimums) that render many individuals ineligible for any type of diversion, such
programs are highly unlikely to reduce the number of people incarcerated. That study also
suggested that drug courts may have a “net-widening” effect; that is, they may actually
increase the number of people incarcerated. Such criminal justice programs, moreover,
have absorbed scarce resources that could have been better spent on bolstering
demonstrated, health-centered approaches such as community-based treatment.
157
Finally, coerced treatment for any health condition, especially for mere drug possession,
raises serious ethical concerns; a recent commentary argued that coercive treatment for
people who use or possess drugs is unethical and runs counter to accepted health
principles; it is also “unlikely to have large effects on population levels of drug use and
crime.”
158
For these reasons, drug courts should be reserved for individuals charged with
151
Rossman SB, Roman J, Zweig JM. The Multisite Adult Drug Court Evaluation: The Impact of Drug Courts.
Washington, DC: Urban Institute; 2011.
152
Sevigny EL, Pollack HA, Reuter P. Can drug courts help to reduce prison and jail populations? Ann Am Acad
Polit Soc Sci. 2013;647(1):190–212.
153
Rossman SB, Roman JK, Zweig JM, et al. The Multi-Site Adult Drug Court Evaluation: Study Overview and
Design. Washington, DC: Urban Institute; 2011.
154
Pollack H, Sevigny E, Reuter P. If Drug Treatment Works So Well, Why Are So Many Drug Users
Incarcerated? Chicago, IL: University of Chicago Press; 2011.
155
Matusow H, Dickman SL, Rich JD, et al. Medication assisted treatment in US drug courts: results from a
nationwide survey of availability, barriers and attitudes. J Subst Abuse Treat. 2013;44(5):473–480.
156
Friedmann PD, Hoskinson R, Gordon M, et al. Medication-assisted treatment in criminal justice agencies
affiliated with the Criminal Justice-Drug Abuse Treatment Studies (CJ-DATS): availability, barriers, and
intentions. Subst Abuse. 2011;33(1):9–18.
157
Drug Courts Are Not the Answer: Toward a Health-Centered Approach to Drug Use. New York, NY: Drug
Policy Alliance; 2011.
158
Stevens A. The ethics and effectiveness of coerced treatment of people who use drugs. Hum Rights Drugs.
2012;2(1):7–16.

79
more serious (non-drug) offenses but whose behavior was motivated by an underlying
drug problem; they should never be used (as they currently are) for individuals charged
with mere drug possession offenses, who can be better served outside of the criminal
justice system. Coerced treatment is ethically unjustifiable, especially when voluntary
treatment can yield equal or more positive outcomes.
159
More alternative strategies are emerging in various localities. Seattle recently instituted a
pilot program known as “Law Enforcement Assisted Diversion,” or LEAD, the first pre-
booking diversion program; it aims to bypass the criminal justice system entirely. Instead
of arresting and booking people for certain drug law violations, including drug possession
and low-level sales, police in a pair of Seattle neighborhoods will immediately direct them
to drug treatment or other supportive services. LEAD allows law enforcement to focus on
serious crime but to still play a key role in linking people with certain drug law violations
to services before they enter the justice system.
160
-
162
In doing so, it has the potential to
reshape law enforcement practices and culture.
Seattle’s policy resembles aspects of the health focus that many European countries, as well
as Canada and others, have adopted: a public health policy orientation often termed a “4
pillars approach.” This comprehensive strategy is based on 4 principles—harm reduction,
prevention, treatment, and enforcement—and it has demonstrated dramatic reductions in
public drug consumption, overdose deaths, and HIV and hepatitis infection rates.
163
,
164
Programs such as LEAD, however, still rely on law enforcement as the primary point of
contact with people who misuse substances. To be most successful, local, state, and
national drug policies must empower health professionals to assess and deliver services to
each individual. CHWs, for example, should be enabled (and given adequate resources) to
serve as the point of contact, source of referrals and information, and service provider for
certain low-threshold services directly.
Ultimately, the removal of criminal sanctions in favor of optional, non-punitive,
proportionate, administrative sanctions—alongside a major expansion of proven,
evidence-based harm reduction, treatment, and prevention services—offers more promise
in achieving a health-centered approach to drug misuse. Some commentators hope that
159
Stevens A. The ethics and effectiveness of coerced treatment of people who use drugs. Hum Rights Drugs.
2012;2(1):7–16.
160
King County Government. Law Enforcement Assisted Diversion (LEAD) program. Available at:
http://leadkingcounty.org/. Accessed December 12, 2013.
161
Fan M. Street diversion and decarceration. Am Crim Law Rev. 2012;50:1.
162
Learning for Action Group L. LEAD program and evaluation plan narrative. Available at:
http://leadwa.squarespace.com/storage/LFA%20Evaluation%20Narrative%20-%20February%202012.pdf.
Accessed December 12, 2013.
163
Alexander BK. Beyond Vancouver’s “four pillars.” Int J Drug Policy. 2006;17(2):118–123.
164
Savary J-F, Hallam C, Bewley-Taylor D. The Swiss Four Pillars Policy: An Evolution From Local
Experimentation to Federal Law. Oxford, England: Beckley Foundation Drug Policy Programme; 2009.

80
various legislative changes—notably the Affordable Care Act of 2010—will expand
treatment availability and resources, potentially making it possible to deliver treatment
and harm reduction services through the health care, rather than the criminal justice,
system.
165
-
167
Action Steps
APHA believes that national and state governments and health agencies must reorient drug
policies to embrace health-centered, evidence-based approaches that reduce the individual
and community harms deriving from current policies and from illicit drug misuse, respect
the human rights of people who use drugs, and allow for the redirection of financial
resources toward where they are needed most. Therefore, APHA:
Urges Congress, the administration, and federal health agencies to convene relevant
experts and stakeholders in the fields of public health, drug treatment, medicine,
harm reduction, education and prevention, social work, and law enforcement, as
well as people who currently use (or formerly used) drugs and affected
communities, to critically review the effectiveness of current drug policies; to
examine the potential public health gains of a range of new drug policies, including
the decriminalization of personal drug possession and use; to open a public debate
about regulatory alternatives to drug prohibition in order to address the public
health and safety harms of illicit drug markets; and to produce a policy environment
that will be most conducive to significantly expanding US treatment, education, and
harm reduction programs.
Urges federal, state, and local elected officials and agency staff to implement
evidence-based and culturally appropriate prevention, regulatory, treatment, and
harm reduction interventions, including (but not limited to):
Expanding proven, life-saving public health interventions and harm
reduction and treatment programs, including medication-assisted treatment,
and strengthening professional preparation and training in these
interventions for health care providers, CHWs, and public health, allied
health, health education, and health communication professionals.
Investigating (and, if results are favorable, implementing) new innovative
agonist and partial agonist replacement treatments and medically supervised
165
Kilmer B, Caulkins JP, Pacula RL, Reuter PH. The US Drug Policy Landscape. Santa Monica, CA: RAND; 2012.
166
Croft B, Parish S. Care integration in the Patient Protection and Affordable Care Act: implications for
behavioral health. Adm Policy Ment Health. 2013;40(4):258–263.
167
Saloner B, Cook BL. Blacks and Hispanics are less likely than whites to complete addiction treatment,
largely due to socioeconomic factors. Health Aff. 2013;32(1):135–145.
81
injection facilities, which have demonstrated their safety and efficacy in
several countries around the world but have not yet been attempted in the
United States.
Increasing funding for existing treatment modalities and ensuring they are
available to all people who need them, including those who are incarcerated
or under criminal justice supervision.
Deprioritizing the use (and funding) of non-health agencies—such as drug
courts and other court-based diversion programs—to deal with people who
use drugs and redirecting resources from criminal justice programs toward
public health interventions to improve the health of such individuals.
Calls on Congress to permanently repeal the federal ban on syringe access funding,
to fund such programs to the maximum extent possible, and to remove other
detrimental barriers to proven interventions.
Encourages state governments to leverage resources potentially available through
the Affordable Care Act toward effective community-based drug treatment, harm
reduction, and physical and mental health services.
Urges Congress and state governments to eliminate federal and state criminal
penalties and collateral sanctions for personal drug use and possession offenses and
to avoid unduly harsh administrative penalties, such as civil asset forfeiture, and
acknowledges that proportionate criminal penalties may be appropriate—
consistent with principles of public health and human rights—for behavior that
occurs in conjunction with drug use if that behavior causes or seriously risks harm
to others, such as driving under the influence; however, such penalties should not be
imposed solely for personal drug possession and use.

82
APPENDIX D
Letter of Support for Supervised Injection from amfAR to
New York State Governor Andrew Cuomo

83

84
APPENDIX E
New York City Supervised Injection Facility Feasibility
Impact Report
Prepared by:
Czarina Behrends, PhD, MPH
Postdoctoral Associate, Weill Cornell Medical College
Bruce Schackman, PhD, MBA
Professor of Health Policy, Weill Cornell Medical College
Researchers from the Weill Cornell Medicine Department of Health care Policy and
Research analyzed the potential health impacts and health care cost impacts of
implementing supervised injection facility (SIFs) in New York City. SIFs provide a clean,
safe environment in which pre-obtained drugs can be consumed under clinical supervision
with purpose of quickly reversing overdoses, providing medical care, and connecting
people who inject drugs (PWID) with substance use treatment and care. This research was
done in collaboration with DOHMH and with input from a technical advisory group made
up of experts in SIF evaluation. We present a summary of the results below.
SIF Impact on preventing opioid overdose fatalities
Based on 2015-2016 NYC opioid overdose mortality data, implementing one SIF in
the neighborhood with the most opioid overdose fatalities could prevent 19 to
37 opioid overdose fatalities per year, assuming no operational constraints on
SIF hours or capacity.
Based on 2015-2016 data, up to 67 to 130 opioid overdose fatalities per year
could be saved if 4 SIFs were placed in four neighborhoods with the most
overdose fatalities.
The estimate of opioid overdose fatalities prevented in the highest priority
neighborhood is within the range of the estimated opioid overdose fatalities
prevented annually by Vancouver’s SIF (23 per year) and exceeds projected
annual opioid overdoses prevented for proposed SIFs in San Francisco and
Baltimore (0.24 and 5.9, respectively).
Because of the recent upward trend of overdose fatalities in NYC, increasing 46%
from 2015 to 2016, this forecast likely underestimates the impact of SIFs on
overdose mortality in 2017.
Short-term cost impact to the health care system
Opioid overdoses cost the NYC health care system an estimated $50 million per
year for EMS calls, ED visits, hospitalizations. Approximately $6 million of these
costs are associated with fatal opioid overdoses.

85
If one SIF was optimally placed, $1.0 million in health care system costs would
be saved if all onsite opioid overdoses were avoided in the base case scenario.
In an alternative scenario, $2.0 million in health care system costs would be
saved if all opioid overdoses were avoided. If overdoses continued to occur at SIFs
but EMS response and ED rates were at similar rates to those observed in Vancouver,
$860,600 in health care system costs would be avoided in the base case scenario.
If four SIFs were optimally placed, $3.6 million in health care system costs
would be saved ($905,000 per SIF) if all onsite opioid overdoses were avoided
in the base case scenario. If opioid overdoses continued to occur at SIFs but EMS
response and ED rates were at similar rates to those observed in Vancouver, $2.7
million in health care system costs would be avoided in the base case scenario.
Recommendations for future analyses to evaluate SIF impact on other health and cost
outcomes
Recommend additional analyses of fatal, non-fatal and averted opioid overdose
estimates that take into account fentanyl use trends and the potential impact of
synthetic opioids on opioid overdose estimates.
Recommend analyses of SIF impact on reducing hepatitis C infections, reducing
high cost medical care services (i.e., need for treatment of skin and soft tissue
infections and endocarditis), and increasing opioid agonist treatment and other
addiction treatment uptake.
Recommend economic analyses of cost-effectiveness and net monetary benefit of
SIFs that also consider non-health care economic impacts, including law
enforcement resource utilization and community impacts such as crime, public
injection, and public disposal of syringes
Background: Supervised injection facilities (SIFs) provide a clean, safe environment in
which pre-obtained drugs can be consumed under clinical supervision with purpose of
quickly reversing opioid overdoses, providing medical care, and connecting people who
inject drugs (PWID) with substance use treatment and care. Given the rising rates of
overdose fatalities in New York City reaching its all-time peak in 2016, SIFs may be one
strategy to reduce opioid overdose mortality in NYC, and the cost of implementing SIFs may
be offset in part by savings in health care system costs.
Purpose: Researchers from the Weill Cornell Medicine Department of Health care Policy &
Research, in collaboration with DOHMH, analyzed the potential opioid overdose-related
health and health care system cost impacts of implementing SIFs in New York City, with
input from a technical advisory group made up of experts in SIF evaluation.
Limitations: While our estimates are based on the best NYC data sources available, we
relied on the literature for several estimates. We received feedback on the face validity of
those assumptions and assistance in identifying additional relevant sources from the
technical advisory group and DOHMH. Base and alternate case estimates for fatal opioid
overdoses prevented under different scenarios were estimated. For costs, we provide a
range of estimates to account for different assumptions of SIF impact.
86
Summary of Findings:
1) SIF Impact on preventing opioid overdose fatalities
Based on 2015-2016 NYC opioid overdose mortality data, implementing one SIF in
the neighborhood with the most opioid overdose fatalities could prevent 19 to
37 opioid overdose fatalities per year, assuming no operational constraints on
SIF hours or capacity.
Based on 2015-2016 data, up to 67 to 130 opioid overdose fatalities per year
could be saved if 4 SIFs were placed in four neighborhoods with the highest
overdose fatalities.
The estimate of opioid overdose fatalities prevented in the highest priority
neighborhood is within the range of the estimated opioid overdose fatalities
prevented annually by Vancouver’s SIF (23 per year) and exceeds projected
annual opioid overdoses prevented for proposed SIFs in San Francisco and
Baltimore (0.24 and 5.9, respectively).
Because of the recent upward trend of overdose fatalities in NYC, increasing 46%
from 2015 to 2016, this forecast likely underestimates the impact of SIFs on
overdose mortality in 2017.
2) Short-term cost impact to the health care system
Opioid overdoses cost the NYC health care system an estimated $50 million per
year for EMS calls, ED visits, hospitalizations. Approximately $6 million of these
costs are associated with fatal opioid overdoses.
If one SIF was optimally placed, $1.0 million in health care system costs would
be saved if all onsite opioid overdoses were avoided in the base case scenario.
In an alternative scenario, $2.0 million in health care system costs would be
saved if all opioid overdoses were avoided. If overdoses continued to occur at SIFs
but EMS response and ED rates were at similar rates to those observed in Vancouver,
$860,600 in health care system costs would be avoided in the base case scenario.
If four SIFs were optimally placed, $3.6 million in health care system costs
would be saved ($905,000 per SIF) if all onsite opioid overdoses were avoided
in the base case scenario. If opioid
Overdoses continued to occur at SIFs but EMS response and ED rates were at similar
rates to those observed in Vancouver, $2.7 million in health care system costs would
be avoided in the base case scenario.
3) Recommendations for future analyses to evaluate SIF impact on other health and
cost outcomes
Recommend additional analyses of fatal, non-fatal and averted opioid overdose
estimates that take into account fentanyl use trends and the potential impact of
synthetic opioids on opioid overdose estimates.

87
Recommend analyses of SIF impact on reducing hepatitis C infections, reducing
high cost medical care services (i.e., need for treatment of skin and soft tissue
infections and endocarditis), and increasing opioid agonist treatment and other
addiction treatment uptake.
Recommend economic analyses of cost-effectiveness and net monetary benefit of
SIFs that also consider non-health care economic impacts, including law
enforcement resource utilization and community impacts such as crime, public
injection, and public disposal of syringes.
Benefits of current study: While there are limitations, this is one of few studies examining
the cost impact of SIF implementation in North America. Two recent studies have examined
the potential cost impact of establishing SIFs in two US cities: San Francisco and Baltimore.
In comparison to these studies, we took a narrower approach by focusing on opioid
overdose impact only, and we forecast greater overdose impact since we account for
greater geographical impact of overdoses in NYC and use local mortality data for estimates.
Supervised injection facilities (SIFs) provide a clean, safe environment in which pre-
obtained drugs can be consumed under clinical supervision with purpose of quickly
reversing opioid overdoses, providing medical care, and connecting people who inject
drugs (PWID) with substance use treatment and care. In North America, Vancouver was the
first city to implement a SIF in 2003 and most recently Montreal opened 3 SIFs in June
2017. To date, there is evidence that Vancouver’s SIF reduced opioid overdose mortality,
1
improved uptake of opioid use disorder treatment,
2
and reduced public injection drug use
and public syringe disposal.
3
Several studies have estimated the cost-effectiveness of SIFs
based on preventing HIV and HCV infections
4
,
5
,
6
,
7
and more recently two US studies have
examined the economic impact of implementing SIFs on a number of health outcomes
8
with
both of these studies indicating favorable economic impacts from SIF implementation.
Given the rising rates of overdose fatalities in New York City, reaching an all-time peak in
1
Marshall BDL, Milloy MJ, Wood E, Montaner JSG, Kerr T. Reduction in overdose mortality after the opening of
North America's first medically supervised safer injecting facility: a retrospective population-based study. The
Lancet. 2011;377(9775):1429-1437.
2
Wood E, Tyndall MW, Zhang R, Montaner JS, Kerr T. Rate of detoxification service use and its impact among
a cohort of supervised injecting facility users. Addiction. 2007;102(6):916-919.
3
Wood E, Kerr T, Small W, et al. Changes in public order after the opening of a medically supervised safer
injecting facility for illicit injection drug users. CMAJ : Canadian Medical Association Journal. 2004;171(7):731-
734.
4
Fischer B, Allard C. Feasibility Study on ‘Supervised Drug Consumption’ Options in the City of Victoria
Victoria, Centre for Addictions Research of British Columbia, University of Victoria.2007.
5
Jozaghi E, Reid AA, Andresen MA. A cost-benefit/cost-effectiveness analysis of proposed supervised
injection facilities in Montreal, Canada. Substance abuse treatment, prevention, and policy. 2013;8:25.
6
Jozaghi E, Reid AA, Andresen MA, Juneau A. A cost-benefit/cost-effectiveness analysis of proposed
supervised injection facilities in Ottawa, Canada. Substance abuse treatment, prevention, and policy. 2014;9:31.
7
Pinkerton SD. Is Vancouver Canada's supervised injection facility cost-saving? Addiction. 2010;105(8):1429-
1436.
8
Irwin A, Jozaghi E, Bluthenthal RN, Kral AH. A Cost-Benefit Analysis of a Potential Supervised Injection
Facility in San Francisco, California, USA. J Drug Issues. 2017;47(2):164-184.
88
2016, SIFs may be one strategy to reduce opioid overdose mortality in NYC with potential
economic benefits.
Researchers from the Weill Cornell Medicine Department of Health care Policy & Research,
in collaboration with DOHMH, analyzed the potential opioid overdose-related health
impacts and health care cost impacts of implementing SIFs in New York City, with input
from a technical advisory group made up of experts in SIF evaluation.
In this report, the data sources, methods, results and implications from the following three
aims are presented:
1. Develop scenario estimates of SIF impact on opioid overdose fatalities for NYC
neighborhoods
2. Estimate short-term cost impact on the health care system from opioid overdoses
prevented by SIFs
3. Recommend approaches for future analyses to evaluate SIF impact on other health
and cost outcomes
Aim #1: Develop scenario estimates of SIF impact on opioid overdose fatalities for NYC
neighborhoods
Data sources:
Opioid mortality Data: Estimates of fatal opioid overdoses were derived from a mortality
dataset provided by the NYC Office of the Chief Medical Examiner and the NYC DOHMH
Bureau of Vital Statistics for 2015 and 2016. Descriptive data are presented in Appendix I.
Type of information provided:
o type of location where the fatal opioid overdose occurred (e.g., deceased’s
own home, home of a friend or family member, public space),
o whether the opioid overdose was a result of heroin or other opioid use, and
o the zipcode where the opioid overdose occurred.
IDUHA (Injection Drug User Health Alliance) survey: The IDUHA survey collected
information from clients of all 14 syringe exchange programs in NYC with a sample size of
814 for the two combined years of data (June 2013-2014 and June 2014-2015).
Respondent demographics are described in Appendix I.
Type of information provided:
o Estimate of travel distance to a syringe exchange program (SEP) that serves
as a proxy for willingness to travel to a SIF in our modelProportion of people
who inject drugs (PWID) who do not primarily inject in their own home or
the home of a friend or family member (“public” injection).
Office of Alcoholism and Substance Abuse Services (OASAS) data set: OASAS collects
mandatory data on admissions and discharges from all certified chemical dependence
treatment programs in New York State.
89
Type of information provided: We estimated the average percentage of heroin
and non-heroin opioid users who inject among those who entered detoxification
(crisis admissions).
Literature Review: We conducted literature reviews to identify additional inputs for our
model, and to contextualize inputs from NYC data for face validity. We limited these
literature reviews to studies conducted in the USA and Canada because we felt the opioid
epidemics, substance use disorder treatment systems, and health care delivery systems in
other countries would not be generalizable to NYC.
Methods:
Geographical Distribution of Opioid Overdose Fatalities
NYC is made up of five boroughs (Bronx, Brooklyn, Manhattan, Queens, and Staten Island).
There are 42 United Hospital Fund neighborhoods (UHFs) designated to approximate NYC
community planning districts distributed across the boroughs (7 in the Bronx, 11 in
Brooklyn, 10 in Manhattan, 10 in Queens, and 4 in Staten Island). We selected UHF
neighborhoods as the main unit of geographical analysis for identifying opioid overdose
hotspots, with the advantages of being a measure frequently used by DOHMH for
evaluation and having zipcodes uniquely assigned to only one UHF (unlike boroughs or
precincts where zipcodes can cross several boundaries).
The combined numbers of fatal opioid overdoses for 2015 and 2016 were mapped at the
zipcode and UHF level. UHFs with a greater than average number of opioid overdose
fatalities were chosen for further analysis as potential sites for SIF placement, resulting in
16 of 42 UHFs being selected for further evaluation. These 16 UHFs accounted for 60.3 % of
the 1,852 fatal opioid overdoses recorded in 2015-2016.
All zipcodes within each UHF were ranked according to the number of 2015-2016 opioid
overdose fatalities. Optimal hypothetical SIF placement for each UHF was weighted by the
number of opioid overdose fatalities within each zipcode. Thus, SIFs were placed closer to
the geographic centers of zipcodes containing the most opioid overdose fatalities. SIF
placements were implemented in ArcGIS, version 10.2.1 and were not constrained by
actual geographical physical limitations such as highways or parks.
Projection of Opioid Overdose Fatalities Prevented
After placing a theoretical SIF within each UHF, the number of fatal opioid overdoses that
could have been avoided by establishing the SIF was estimated using the following
equation .
Potential fatal overdoses avoided (assuming all fatal overdoses are avoided in a SIF)
= Number of fatal overdoses
Proportion of IDU willing to travel to a SIF at a given distance from the theoretical SIF
Proportion of IDU willing to use a SIF

90
Proportion of fatal overdoses due to IDU
Proportion of IDU overdoses that occur outside the home
I. Number of Opioid overdoses/Willingness to travel:
For each SIF, the number of fatal opioid overdoses that may be prevented is partly
influenced by the number of PWID who would have traveled to the SIF location. We used
the IDUHA data set to estimate the distance between the address of the SEP used and the
center of the zipcode where the participant last slept. While there were PWID who
reported traveling further than 3 miles to the SEP, we assumed that PWID would not travel
more than 3 miles to a SIF because of more frequent expected use of a SIF versus an SEP. A
literature review (Appendix II) found that the median distance traveled to an SEP
calculated from IDUHA data is similar to that reported in the literature.
We established concentric rings around each hypothetical SIF at different distances (0.25,
0.5, 0.75, 1.0, 1.5, 2.0, 2.5, 3.0 miles) that represented different probabilities of traveling to
a SIF that were reduced as distances from the SIF increased. The proportions of PWID who
would travel to a SIF at each distance were estimated directly from the IDUHA data, and
applied as cumulative proportions (Figure 1).
Based on the distribution of willingness to travel at each distance from the SIF, the
proportion of PWID who experienced a fatal opioid overdose and would have traveled to a
SIF is then estimated for each SIF (Figure 2). In order to estimate the maximum potential
impact of each SIF, we include opioid overdoses in contiguous UHFs and do not consider
whether or not SIFs have been established in adjacent UHFs when calculating the potential
number of fatal opioid overdoses that may be reached by each SIF within a 3-mile radius.
100.0%
84.0%
71.6%
58.5%
46.3%
29.8%
18.5%
9.5%
0.0%
20.0%
40.0%
60.0%
80.0%
100.0%
0.25 0.5 0.75 1 1.5 2 2.5 3
Percentage of SEP clients
Miles traveled
Figure 1: Cumulative Proportion Estimated
Willing to travel to a SIF or SEP (Source: IDUHA
Survey)

91
II. Willingness to use a SIF:
We conducted a literature review regarding the willingness of PWID to use a SIF (Appendix
III) because we did not have any SIF-specific data from representative samples of PWID in
NYC. Since SIF knowledge and education has improved over time, we focused on the most
recent studies to estimate the percentage of PWID who would be willing to use a SIF.
9
,
10
III. Proportion of overdoses that result from injection drug use:
Because SIFs currently under consideration for NYC are spaces for PWID only, we limited
the potential number of fatal opioid overdoses avoided to those associated with injection
drug use. We estimate the proportion of heroin and non-heroin opioid users who inject
from the OASAS crisis admissions data set for NYC, and also conducted a literature review
in which we found results consistent with the estimates from the OASAS data (Appendix
IV).
IV. Proportion of overdoses that result from injection in public spaces (outside the
home)
In our base case scenario, we focused on individuals who primarily do not inject at home or
the home of friends or family (i.e., “public injectors”), assuming this population would be
most likely to use a SIF regularly for their injections. Given this assumption, we used
IDUHA data to determine the proportion of PWID who fit this definition. We also conducted
a literature review to assess the range of estimates for proportion of people who primarily
9
Low D. Interest in a Safe Injection Facility Among Injection Drug Users in King County, WA. Seattle, WA:
Department of Health Services, University of Washington. 2014.
10
Kral AH, Wenger L, Carpenter L, Wood E, Kerr T, Bourgois P. Acceptability of a Safer Injection Facility
among Injection Drug Users in San Francisco. Drug Alcohol Depend. 2010;110(1-2):160-163.

92
inject in public spaces, but found the definitions of “public injection” varied across studies
(Appendix V).
Analysis:
Base Case Scenario: Data for our base-case scenario were derived from both the
literature and NYC-specific data sources (Table 1), and we assumed SIF access
unconstrained by hours of operation or physical capacity. We make a conservative
assumption that people who primarily inject in their home or the home of a friend
or family member would not have an overdose averted in a SIF, as they would not
attend a SIF regularly for their injections.
Alternative Scenario: We include an alternative case where we assume some of
those PWID who primarily inject in private spaces would attend a SIF regularly,
using estimates of their willingness to attend a SIF from the literature, substantially
increasing the potential number of opioid overdoses avoided. We consider this an
upper range estimate of the potential impact on the number of fatal opioid
overdoses averted.
Vancouver comparison: We compare the results of the base and alternative cases
to a scenario in which our outcomes match those reported for the Vancouver, BC SIF
(INSITE), which was associated with a 35% reduction of overdose fatality rates in
one year within 500 meters of the SIF and no wider impact.
1
We applied this
assumption to a half mile radius (~800 meters) around each hypothetical SIF, with
no impact beyond this radius.
Table 1: Data for Base Case Scenario Estimates of Number of Opioid Overdoses
Prevented from Supervised Injection Facilities
Parameter
Base Case
Proportion
Source
Public Injection
0.39
IDUHA
Willingness to use SIF*
0.86
Seattle & SF study
11,12
Heroin use
0.735
NYC mortality data
Other opioid use
0.265
NYC mortality data
% heroin users who inject
0.485
OASAS, crisis data
% other opioid users
(non-heroin) who inject
0.015
OASAS, crisis data
*Applied to public injection; alternative scenario applies a public injector willingness to
use of 0.8 and non-public injector willingness to use of 0.56
11
Note: Public injection=outside own home or the home of a friend or family member;
IDU=injection drug use
11
DeBeck K, Kerr T, Lai C, Buxton J, Montaner J, Wood E. The validity of reporting willingness to use a
supervised injecting facility on subsequent program use among people who use injection drugs. Am J Drug
Alcohol Abuse. 2012;38(1):55-62.
93
Results (Table 2):
Using 2015-2016 mortality data, implementing one SIF in the neighborhood
with the most opioid overdose fatalities could prevent up to 19 opioid
overdose fatalities per year in the base case scenario and up to 37 opioid
overdose fatalities in the alternative scenario, assuming no operational constraints
on SIF hours or capacity.
For the highest priority neighborhood’s 3-mile radius, these estimates represent a
7% decrease in fatal opioid overdoses in the base case scenario and 14%
decrease for the alternative case scenario.
Based on 2015-2016 data, up to 67 to 130 opioid overdose fatalities per year
could be saved if 4 SIFs were placed in four neighborhoods with the most
overdose fatalities.
The estimate of 19-37 opioid overdose fatalities prevented with one SIF in the
highest priority neighborhood is within the range of the number opioid
overdose fatalities prevented by Vancouver’s SIF (23 per year) and exceeds the
projected number of opioid overdoses prevented annually by one SIF in San
Francisco and Baltimore (0.24 and 5.9, respectively). Estimates for each
neighborhood are also consistent with the comparison where we applied the
neighborhood impact observed in Vancouver to the half mile radius around each
hypothetical SIF in NYC.
Because overdose fatalities in NYC increased 46% from 2015 to 2016 in NYC due to
increased fatalities associated with fentanyl use, this forecast likely
underestimates the impact of SIFS on overdose mortality in 2017.

94
Table 2: Projected Maximum Number of Fatal Opioid Overdoses Avoided Annually by
Implementing a Supervised Injection Facility in Each of the Most Affected NYC
Neighborhoods
(Based on 2015-2016 Overdose Fatality Data)
UHF
Neighborhood
(Rank Order)
Base Case
Estimate
Alternative Case
Estimate
Comparison Based
on Vancouver BC
Outcomes*
1
19
37
24
2
18
35
31
3
15
29
37
4
15
29
46
5
15
28
16
6
11
21
18
7
10
20
26
8
10
20
14
9
10
19
20
10
8
15
10
11
7
13
21
12
6
12
21
13
5
10
7
14
4
9
9
15
4
8
10
16
4
7
3
* Represents the opioid overdoses prevented based on Vancouver’s percentage decrease in
opioid overdoses within 500 meters applied to a half mile radius of each theoretical SIF in
NYC. These numbers do not represent the actual number of overdoses prevented in
Vancouver, which were reported to be 23 per year.
1
Limitations:
Some model inputs are based on self-reported drug use behavior and willingness to
use a SIF.
Due to lack of data, SIF attendance assumptions in the base and alternate cases do
not include the proportion of daily injections that might occur at a SIF among
attendees. This may vary substantially depending on a variety of individual and SIF
characteristics, in addition to whether attendees primarily inject in public or private
spaces.
We used an estimate of the proportion of heroin and non-heroin users who inject
from the OASAS database, which reflect drug use behavior among substance use
treatment clients. People who inject drugs are more likely to experience a fatal
opioid overdose than non-injectors.
12
,
13
As a result, we may have underestimated
the proportion of fatal opioid overdoses attributable to injection drug use.
12
Galea S, Nandi A, Coffin PO, et al. Heroin and cocaine dependence and the risk of accidental non-fatal drug
overdose. J Addict Dis. 2006;25(3):79-87.
13
New York City Department of Health and Mental Hygiene. Unpublished Data. 2009.
95
The combined impact of implementing 4 SIFs may overstate their impact since the
potential number of opioid overdoses prevented by each theoretical SIF was
estimated assuming no other SIFs; there may be overlapping impact of SIFs
implemented within 3 miles of each other.
The impact of each SIF may be understated because there may be “spillover” effects
of a SIF in preventing overdoses for injections that occur outside of the facility due
to increased naloxone distribution and overdose prevention education that are not
accounted for in these estimates.
Our analysis used the average of 2015-2016 overdose data for each neighborhood in
order to ensure stable sample sizes. Given the increasing trend of overdoses
occurring in NYC between 2015 and 2016, if SIFs are implemented in 2017 their
impact may be greater and there may be some differences in impact by
neighborhood.
Aim #2: Short-term cost impact to health care system from opioid overdoses prevented
by a SIF
Data Sources:
Mortality Data: The number of fatal opioid overdoses was derived from the analysis of
2015-2016 data in Aim #1.
Types of information provided:
o Information about the number of opioid overdose fatalities that occur in the
hospital
Syndromic surveillance data set: The syndromic data set is emergency room surveillance
data that is reported to DOHMH.
Types of information provided:
o The relative frequency of non-fatal opioid overdoses was estimated using
syndromic data; DOHMH estimated that the total number of non-fatal opioid
overdoses in NYC is 10 times the number of fatal opioid overdoses.
o While the syndromic data set is an accurate count of total non-fatal opioid
overdoses, there is uncertainty around the geographical distribution of the
non-fatal opioid overdoses due to non-random missing information on the
location of where these overdoses occurred. We account for these limitations
in the data by using an estimated factor of 10 non-fatal opioid overdoses for
each identified fatal opioid overdose, so that the non-fatal opioid overdoses
were assumed to be distributed similarly to the fatal opioid overdoses by
geographic location.
o Use of EMS was estimated from the 2015 syndromic data set, which had
more consistent reporting of ambulance use.
Statewide Planning and Research Cooperative System (SPARCS): SPARCS is a
comprehensive all payer data reporting system that covers outpatient and inpatient

96
admissions, including ED visits. 2014 data is used because 2015 data were not available at
the time this analysis was conducted.
Types of information provided:
o We identified non-fatal and fatal opioid overdoses in this database
discharged from the ED or an inpatient setting from NYC hospitals. More
information on how opioid overdoses were defined in the SPARCS dataset is
available in Appendix VI.
o Health care utilization per fatal and non-fatal opioid overdose event was
estimated using this data and applied to the total fatal overdoses and non-
fatal overdose estimates.
o Based on information from a chart review of emergency department (ED)
opioid overdoses conducted by NYC DOHMH and the literature, the ED data
in SPARCS was determined to be underreported for non-fatal opioid
overdoses. In place of the SPARCS estimates for non-fatal ED utilization and
ED to inpatient transfers, we used percentages from the chart review (28%
ED to inpatient admissions). The remaining estimates of health care services
utilization comes directly from SPARCS, including direct inpatient admissions
and fatal opioid overdose health care services utilization.
Methods:
Health care Services Utilization: A decision analytic framework was used to assign
utilization of EMS, ED, and inpatient services, taking into consideration fatal and non-fatal
opioid overdoses (Figure 3).
Figure 3: Decision Tree of Health care Services Utilization from Opioid Overdoses
97
Health care services utilization per opioid overdose event for EMS services, ED discharges,
and inpatient discharges are described in Table 3. Among non-fatal opioid overdoses that
were treated at a hospital, most resulted from an EMS call and almost three quarters were
discharged after an ED visit. Among all fatal opioid overdoses, one quarter died in the
hospital with the majority dying in an inpatient setting. We assume that among all fatal
opioid overdoses an EMS call occurred 90% of the time, with the response for the other
10% coming directly from the Office of the Medical Examiner.
Table 3: Utilization of health care services by non-fatal and fatal opioid overdoses in NYC for
2014
% of non-
fatal
opioid
overdoses
treated at
the
hospital
% of all
fatal
opioid
overdoses
Emergency Medical Service Calls
Emergency Medical Services (EMS) called for hospital
transport
90%
90%*
Other transportation used to hospital or morgue
10%
10%
Total transportation utilization
100%
100%
Hospital Service Utilization
Fatal opioid overdose outside of hospital setting
0%
74%
Discharged from emergency department (ED) or died in
ED
72%
2%
Discharged from inpatient stay or died in inpatient
setting
28%
24%
Total hospital service utilization
100%
100%
*EMS is assumed to be 90% for fatal opioid overdoses. Assumption that 10% of 911 calls
for fatal opioid overdoses results in the office of medical examiner directly transporting to
morgue
Cost Measures:
Costs were assigned to each outcome from the perspective of the NYC health care system.
We used NYC area Medicare fee-for-service payment estimates as proxies for provider
costs, because these payments are designed to reimburse providers for the resources that
would be used to treat a typical patient with a given condition and are adjusted for a
number of relevant factors that are unique to the patient or provider. Costs are understated
in that they do not include physician costs that are billed separately to patients or insurers,
but this approach is consistent with several studies where physician costs are not included

98
or reported separately.
1415
All costs are reported in 2016 US dollars; cost sources from
earlier years were converted to 2016 US dollars using the NYC-area medical-care
Consumer Price Index.
16
Emergency medical services (EMS) unit cost. The mean cost of an ambulance call was
estimated using Medicare urban ground adjusted base rates for basic and advanced life
support rides in NYC.
17
The mean basic and advanced life support rates were weighted by
the proportion of observed rides reported nationally by the Department of Health and
Human Services, Office of Inspector General,
18
because no relevant local data were
available.
Emergency department (ED) unit cost. Medicare reimburses ED visits using ambulatory
payment classification (APC) codes. However, these codes were not available for many of
the opioid overdose patients discharged from the ED in the SPARCS database; therefore, we
calculated the mean Medicare reimbursement rate for an ED visit using data from the
Medical Expenditure Panel Survey (MEPS).
19
Through MEPS we were able to calculate a
nationally-representative mean Medicare payment for an ED visit.
Inpatient unit cost. Medicare reimburses for inpatient stays according to the patient’s
assigned diagnosis-related group (DRG).
20
Each DRG represents a clinically similar group of
patients that, on average, would be expected to utilize the same quantity of resources.
Generally, the amount that Medicare reimburses for each DRG is a function of the base rate
(i.e., the mean operating cost for a typical inpatient stay), the DRG weight that reflects the
resources used relative to the base case, local wage rates, hospital teaching and
disproportionate-share status, and outlier costs for cases that are exceptionally resource-
intensive. Four DRG codes accounted for approximately 85% of all opioid overdose
inpatient stays in SPARCS. Costs differences among these DRGs are consistent with
differences in the average length of stay and proportion with intensive care unit stays; fatal
opioid overdoses were also more likely to be assigned higher cost DRGs (see Appendix VII
for inpatient cost calculations).
14
Inocencio TJ, Carroll NV, Read EJ, Holdford DA. The Economic Burden of Opioid-Related Poisoning in the
United States. Pain Medicine. 2013;14(10):1534-1547.
15
Tak CR, Malheiro MC, Bennett HKW, Crouch BI. The value of a poison control center in preventing
unnecessary ED visits and hospital charges: A multi-year analysis. The American Journal of Emergency
Medicine. 2017;35(3):438-443.
16
Bureau of Labor Statistics. Consumer Price Index. https://www.bls.gov/cpi/. Accessed May 19, 2017.
17
Centers for Medicare and Medicaid Services. Ambulance Fee Schedule.
https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AmbulanceFeeSchedule/index.html.
Accessed May 19, 2017.
18
Wright S. Memorandum Report: Utilization of Medicare Ambulance Transports, 2002-2011. Washington,
DC: Department of Health and Human Services, Office of Inspector General. 2013.
19
Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey.
https://meps.ahrq.gov/mepsweb/index.jsp. Accessed May 19, 2017.
20
Centers for Medicare and Medicaid Services. Acute Inpatient PPS.
https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteinpatientPPS/index.html.
Accessed May 18, 2017.

99
Table 4: Costs for Emergency Medical Services, Emergency Department, and
Inpatient Services ($2016 USD)
Health care Service
Average Payment
Sources
Emergency Medical Services
$392
Centers for Medicare and
Medicaid Services
(NYC)
19
, Dept. of Health
and Human Services
(National)
20
Emergency Department
$684
MEPS (National)
21
Inpatient: non-fatal*
$14,267
SPARCS DRG codes (NYC)
Inpatient: fatal*
$25,159
SPARCS DRG codes (NYC)
*Assumption that those initially admitted through the ED have costs accounted for in
average inpatient payment. See Appendix VII for further information on calculation of the
average inpatient payment.
Cost Calculations:
Health care services utilization and the cost measures described above were used to
determine:
Current costs to the health care system from opioid overdoses
Cost savings from implementing 1 SIF assuming all opioid overdoses that occur at the
SIF are avoided or required no health care service utilization outside of the SIF
Cost savings from implementing 4 SIFs assuming all opioid overdoses that occur at
the SIF are avoided or required no health care service utilization outside of the SIF
Cost savings from implementing 1 SIF and 4 SIFs assuming that 39% of opioid
overdoses that occurred on site resulted in an ambulance call and 28% of those
overdoses resulted in a transfer to the hospital as was observed at the Vancouver SIF,
INSITE.
21
Results:
Current Health care Costs:
Opioid overdoses cost the NYC health care system an estimated $50 million per
year for EMS calls, ED visits, hospitalizations. Approximately $6 million of these
costs are associated with fatal opioid overdoses (See Appendix VIII for cost
estimate tables).
The average cost per opioid overdose was approximately $4,900 ($4,800 per
non-fatal overdose and $6,500 per fatal overdose)
Cost Savings from SIF Implementation:
If one SIF was optimally placed, $1.0 million in health care system costs would
be saved if all onsite opioid overdoses were avoided in the base case scenario.
21
Kerr T, Tyndall MW, Lai C, Montaner JSG, Wood E. Drug-related overdoses within a medically supervised
safer injection facility. International Journal of Drug Policy. 2006;17(5):436-441.
100
In an alternative scenario, $2.0 million in health care system costs would be
saved if all opioid overdoses were avoided. If overdoses continued to occur at SIFs
but EMS response and ED rates were at similar rates to those observed in Vancouver,
$860,600 in health care system costs would be avoided in the base case scenario.
If four SIFs were optimally placed, $3.6 million in health care system costs
would be saved ($905,000 per SIF) if all onsite opioid overdoses were avoided
in the base case scenario. If opioid overdoses continued to occur at SIFs but EMS
response and ED rates were at similar rates to those observed in Vancouver, $2.7
million in health care system costs would be avoided in the base case scenario.
Cost savings are derived primarily from avoided hospitalizations (84% of
savings), followed by avoided ED visits without hospitalizations (9%) and avoided
EMS transports (7%). Approximately 88% of savings are from non-fatal opioid
overdoses and 12% of savings are from fatal opioid overdoses.
Limitations
The health care service utilization data derived from SPARCS may not be
representative of all opioid overdoses in NYC; the total number of opioid overdose
cases identified in the SPARCS data set are substantially lower than the number of
ED admissions estimated from the syndromic data. While we accounted for the fact
that the ED data was underreported in SPARCS, we assumed that fatal opioid
overdoses and inpatient stays were more consistently reported in SPARCS.
A national ED cost was estimated instead of a NYC-specific cost for opioid
overdoses, which may underestimate actual ED costs for NYC
We were unable to identify NYC-specific data on EMS reimbursement codes
regarding the use of life support when responding to opioid overdoses, resulting in
applying national basic and advanced life support utilization to NYC-specific EMS
costs for a weighted mean cost.
In our sensitivity analysis we used the experience at INSITE in Vancouver to
estimate health care utilization for responding to opioid overdoses occurring at a
SIF; however, the NYC local practice may differ regarding whether or not to call EMS
for opioid overdoses occurring at a SIF. If EMS is more likely to be called in NYC the
estimated cost savings may be lower, although opioid overdoses transported from a
SIF may be less likely to result in a high cost inpatient admission.
Health care savings from other improved outcomes such as preventing hepatitis C,
providing onsite wound care, and substance use treatment referrals (see Aim #3)
and estimates of the costs of operating a SIF would be essential for providing an
accurate estimate of the net economic impact of SIFs on the health care system.
Aim #3: Recommend approaches for future analyses to evaluate SIF impact on other
health and societal cost outcomes
The implementation of a SIF provides benefits beyond reversing opioid overdoses;
therefore, we recommend that further analyses be conducted to better understand the total
impact that a SIF would have on health and other related outcomes. Further analyses in

101
these areas would also allow for more in depth economic impact analyses of cost-
effectiveness and net monetary benefit of establishing SIFs. Further areas of analysis are
described below.
Impact of Synthetic Opioids on Estimates
Rationale/Recommendation: The rates of opioid-related fatalities are increasing in the
northeast United States due to the increasing amount of synthetic opioids such as fentanyl
in the heroin and cocaine supply.
22
,
23
Fentanyl is a synthetic opioid that is 50 to 100 times
more potent than morphine. SIFs may be more effective at reversing fentanyl-induced
overdoses since these overdoses typically require multiple naloxone doses that exceed the
amount that people may have at home. Use of local neighborhood data on synthetic opioid
use as it relates to overdose fatalities is recommended to develop additional SIF impact
scenarios; otherwise a multiplier for recent overall trends could be applied to the existing
estimates.
Criminal Justice and Community Impact:
Rationale/Recommendation: Evidence from Vancouver’s SIF shows that there was no
significant increase in crime after opening
24
, but public injection and disposal of used
syringes in public spaces significantly decreased.
25
Thus, while the impact on the criminal
justice system is not expected to increase from opening a SIF, a SIF could potentially reduce
police responses to 911 calls for opioid overdoses thereby improving law enforcement
resource utilization. We recommend estimating this potential impact on police response
using law enforcement data from the NYC police department. Because there is evidence of
potential improvement in public injection and public disposal of needles, estimating the
potential economic impact on neighborhoods in terms of societal benefit is also
recommended.
HIV
Rationale/Recommendation: In contrast to studies that have examined the impact of SIFs
on HIV in Canada,
7,
26
,
27
the very low incidence of HIV among PWID in NYC (0.14 new
22
NYC Health. Health Department Warns New Yorkers About Cocaine Laced With Fentanyl; Occasional Users
At High Risk Of Overdose. https://www1.nyc.gov/site/doh/about/press/pr2017/pr043-17.page. 2017.
23
Paone D, Tuazon E, Nolan M, Mantha S. Unintentional Drug Poisoning (Overdose) Deaths involving Heroin
and/or Fentanyl in New York City, 2000-2015. Epi Data Brief. 2016(74).
24
Wood E, Tyndall MW, Lai C, Montaner JS, Kerr T. Impact of a medically supervised safer injecting facility on
drug dealing and other drug-related crime. Substance abuse treatment, prevention, and policy. 2006;1:13.
25
Wood E, Kerr T, Small W, et al. Changes in public order after the opening of a medically supervised safer
injecting facility for illicit injection drug users. CMAJ. 2004;171(7):731-734.
26
Andresen MA, Boyd N. A cost-benefit and cost-effectiveness analysis of Vancouver's supervised injection
facility. Int J Drug Policy. 2010;21(1):70-76.
27
Bayoumi AM, Zaric GS. The cost-effectiveness of Vancouver's supervised injection facility. CMAJ.
2008;179(11):1143-1151.

102
diagnoses per 100 person year)
28
suggests that unless incidence patterns change HIV
prevention can reasonably be excluded from future analyses of SIF impact for NYC.
Hepatitis C
Rationale: The cost-effectiveness of SIFs in Canada has been previously modeled taking
into account impact on Hepatitis C (HCV) prevention,
5,6,29,
29
but to date, no such cost-
effectiveness analysis has been conducted in the United States. Because of the high
prevalence (60%) and incidence of hepatitis C among PWID in NYC and high cost of
treatment,
30
determining the potential impact of SIFs on HCV transmission is important for
understanding the full impact of SIFs on health outcomes.
Recommendations: We recommend conducting a NYC-specific modeling study of the
impact of SIF implementation in NYC on HCV transmission, similar to a study recently
published for Toronto and Ottawa.
31
The model used in that study incorporated geographic
location and the combined impact of multiple SIFs, which would be amenable to the
situation in NYC where substance use is geographically dispersed. Potential data to use as
inputs to this model would include HCV and mortality data from DOHMH, as well as needle
and equipment sharing behavior data from IDUHA.
Medical care services
Rationale:
Skin and soft tissue infections (SSTIs) are prevalent among PWID due to muscle or skin
injection and are one of the most common causes for ED and hospital admissions for this
group.
31
,
32
The two recent studies that examined net monetary benefits of SIFs in San
Francisco and Baltimore both considered SSTIs, but acknowledged limitations of lack of
data on both rates of infection and costs.
8,9
Nevertheless, estimating the impact of
providing wound care services at SIFs, and the resulting savings to the health care system
would be valuable.
28
Des Jarlais DC, Arasteh K, McKnight C, et al. Consistent Estimates of Very Low HIV Incidence Among People
Who Inject Drugs: New York City, 2005-2014. Am J Public Health. 2016;106(3):503-508.
29
Enns EA, Zaric GS, Strike CJ, Jairam JA, Kolla G, Bayoumi AM. Potential cost-effectiveness of supervised
injection facilities in Toronto and Ottawa, Canada. Addiction. 2016;111(3):475-489.
30
Jordan AE, Des Jarlais DC, Arasteh K, McKnight C, Nash D, Perlman DC. Incidence and prevalence of hepatitis
c virus infection among persons who inject drugs in New York City: 2006–2013. Drug Alcohol Depend.
2015;152:194-200.
31
Kievlan DR, Gukasyan M, Gesch J, Rodriguez RM. Clinical profile of injection drug users presenting to the
ED. The American Journal of Emergency Medicine. 2015;33(5):674-676.
32
Binswanger IA, Takahashi TA, Bradley K, Dellit TH, Benton KL, Merrill JO. Drug Users Seeking Emergency
Care for Soft Tissue Infection at High Risk for Subsequent Hospitalization and Death. Journal of Studies on
Alcohol and Drugs. 2008;69(6):924-932.

103
Endocarditis: Safer injection practice can also reduce the risk of endocarditis, a heart
infection, more common among PWID who use used syringes for injection.
33
,
34
,
35
,
36
,
37
No
other studies have projected the impact of SIFs on reducing the risk of endocarditis and
associated health care costs, but endocarditis is a very expensive health condition that
often requires hospitalization or expensive outpatient treatment,
37
and we recommend
taking it into consideration.
Recommendations:
Data from SPARCS could be used to identify DRGs most frequently associated with SSTI and
endocarditis admissions. The proportion of clients receiving these medical care services
and the likelihood that these clients might have been treated at a hospital in the absence of
onsite care may be estimated from the literature and interviews with NYC SEP programs
providing these services. Projections of the potential cost savings to the health care sector
from improved wound care should be conducted in the context of defining SIF delivery
models, such as whether the SIF would be located at site that already provides wound care
services to PWID, would provide these services on-site de novo, or would provide medical
referrals for this care.
38
,
39
Projections should also take into account current medical
service delivery capacity (providers and hours) and potential increased demand from new
SIF clients versus existing clients newly accessing SIF services.
Substance use disorder and addiction treatment
Rationale: Offering substance use disorder treatment, particularly opioid agonist
treatment (OAT), is crucial to helping PWID mitigate and potentially eliminate illicit drug
use. The studies in San Francisco and Baltimore
8,9
that examined the economic benefit
projected increased uptake of OAT based on data from a SIF in Sydney, Australia that
provided OAT referrals.
40
Examining the impact of OAT and addiction treatment uptake is
an important outcome, as SIFs provide an opportunity for regular contact with health care
33
Axelsson A, Soholm H, Dalsgaard M, et al. Echocardiographic findings suggestive of infective endocarditis in
asymptomatic Danish injection drug users attending urban injection facilities. The American journal of
cardiology. 2014;114(1):100-104.
34
Cooper HL, Brady JE, Ciccarone D, Tempalski B, Gostnell K, Friedman SR. Nationwide increase in the
number of hospitalizations for illicit injection drug use-related infective endocarditis. Clinical infectious
diseases : an official publication of the Infectious Diseases Society of America. 2007;45(9):1200-1203.
35
Fleischauer AT, Ruhl L, Rhea S, Barnes E. Hospitalizations for Endocarditis and Associated Health Care
Costs Among Persons with Diagnosed Drug Dependence - North Carolina, 2010-2015. MMWR Morb Mortal
Wkly Rep. 2017;66(22):569-573.
36
Miro JM, del Rio A, Mestres CA. Infective endocarditis in intravenous drug abusers and HIV-1 infected
patients. Infectious disease clinics of North America. 2002;16(2):273-295, vii-viii.
37
Wurcel AG, Anderson JE, Chui KK, et al. Increasing Infectious Endocarditis Admissions Among Young People
Who Inject Drugs. Open forum infectious diseases. 2016;3(3):ofw157.
38
Small W, Van Borek N, Fairbairn N, Wood E, Kerr T. Access to health and social services for IDU: the impact
of a medically supervised injection facility. Drug Alcohol Rev. 2009;28(4):341-346.
39
Small W, Wood E, Lloyd-Smith E, Tyndall M, Kerr T. Accessing care for injection-related infections through a
medically supervised injecting facility: A qualitative study. Drug Alcohol Depend. 2008;98(1–2):159-162.
40
Final report of the evaluation of the Sydney Medically Supervised Injection Centre. MSIC Evaluation
Committee Sydney, Australia. 2003.

104
professionals able to connect PWIDs with the appropriate treatment resources when they
are ready.
Recommendations: For NYC, estimates for OAT treatment referrals should take into
account location and referral patterns of possible SIF delivery models. For example, if a SIF
were to be co-located at an SEP, the OAT referral history for the types of SEPs being
considered should be used in making these estimates, taking into account how much the
SEP will be serving new SIF clients versus existing clients newly accessing SIF services.
Once referral rate estimates are determined, existing literature and potentially data from
OASAS can be used to project the impact of OAT enrollment on health care system and
societal costs.
41
41
Murphy SM, Polsky D. Economic Evaluations of Opioid Use Disorder Interventions. Pharmacoeconomics.
2016;34(9):863-887.

105
Injection Drug User Health Alliance (IDUHA) survey respondents
compared to NYC Bureau of Vital Statistics/Office of the Chief Medical
Examiner overdose mortality data
Descriptive
Category
Group
IDUHA 2013/2014
& 2014/2015
Opioid Overdose
Mortality Data 2014 &
2015
Gender
Male
66.8%
74.1%
Female
31.3%
25.9%
Transgender
2.0%
0.0%
Age
15-24
4.0%
8.2%
25-34
13.5%
22.6%
35-44
23.1%
20.8%
45-54
37.5%
27.2%
55-64
19.0%
17.5%
65-84
2.8%
3.6%
Race/Ethnicity
Black, NH
29.0%
16.6%
White, NH
15.4%
30.1%
Hispanic
49.0%
49.5%
Other
6.7%
0.0%
Borough of
Residence or of
Death
Bronx
40.9%
25.3%
Brooklyn
21.7%
27.5%
Manhattan
23.7%
17.1%
Queens
8.2%
16.1%
Staten Island
5.5%
8.8%
Location Injection
or Death*
Public
38.4%
19.5%
Private
61.6%
80.5%
Drug of Injection or
Death (not
mutually
exclusive)**
Heroin
37.6%
73.5%
Fentanyl
---
12.8%
Other Opioids
17.0%
22.0%
* For injection location, IDUHA survey respondents were classified as “private” if they responded
that they had injected in their own home or the home of a friend’s or family member’s in the past 3
months. For the NYC Bureau of Vital Statistics/Office of the Chief Medical Examiner, overdose death
location was similarly classified as private if it occurred in the home of the deceased or a friend or
family of the deceased.
**For drug of injection, IDUHA survey respondents were asked if they used heroin, other opioids,
and a number of other drugs in the past 30 days. For the NYC Bureau of Vital Statistics/Office of the
Chief Medical Examiner heroin, fentanyl, and other opioids could all be present in an overdose.
Overdoses with opioids present but without the presence of heroin or fentanyl were classified as
other overdoses.

106
Literature Review Appendix
Willingness to Travel to a SIF
The following table details the findings from a literature review of peer-reviewed studies on the distance that people who use
drugs would travel to use a supervised injection facility. The value in the “% Willing to Travel” column represents the
percentage of respondents who selected the most popular response for distance willing to travel in the previous column.
Study
Most Common
Distance
Willing to
Travel (miles)
(% willing to
travel)
Distribution of
distance travel
Estimated
distance
(miles)*
Weighte
d
Average
distance
traveled
(miles)
Locatio
n
Sampl
e
Notes
Willingness to travel: by foot
Bayoumi
et al.
(2012)
1
0.12- 0.29 mi
(29%)
<= 1 block (3%),
2-5 blocks
(29%),
6-10 blocks
(19%),
1 km (20%),
>1km (28%)
0.06 mi (3%);
0.12- 0.29 mi
(29%);
0.35-0.59
(19%);
0.62 (20%);
>0.62 (28%)
0.85
Toronto
202
Respondents asked how far they
would be willing to travel to a SIF. Of
200, 47% would be willing to take
public transport, 26% would be
willing to take public transport but
can't afford it, 28% would not be
willing even if they could afford to.
Source: 2006 Toronto I-Track
survey.
1
Bayoumi AM, Strike C, Brandeau M, et al. Report of the Toronto and Ottawa Supervised Consumption Assessment Study, 2012. Toronto, Ontario: St.
Michael's Hospital and the Dalla Lana School of Public Health, University of Toronto.2012.
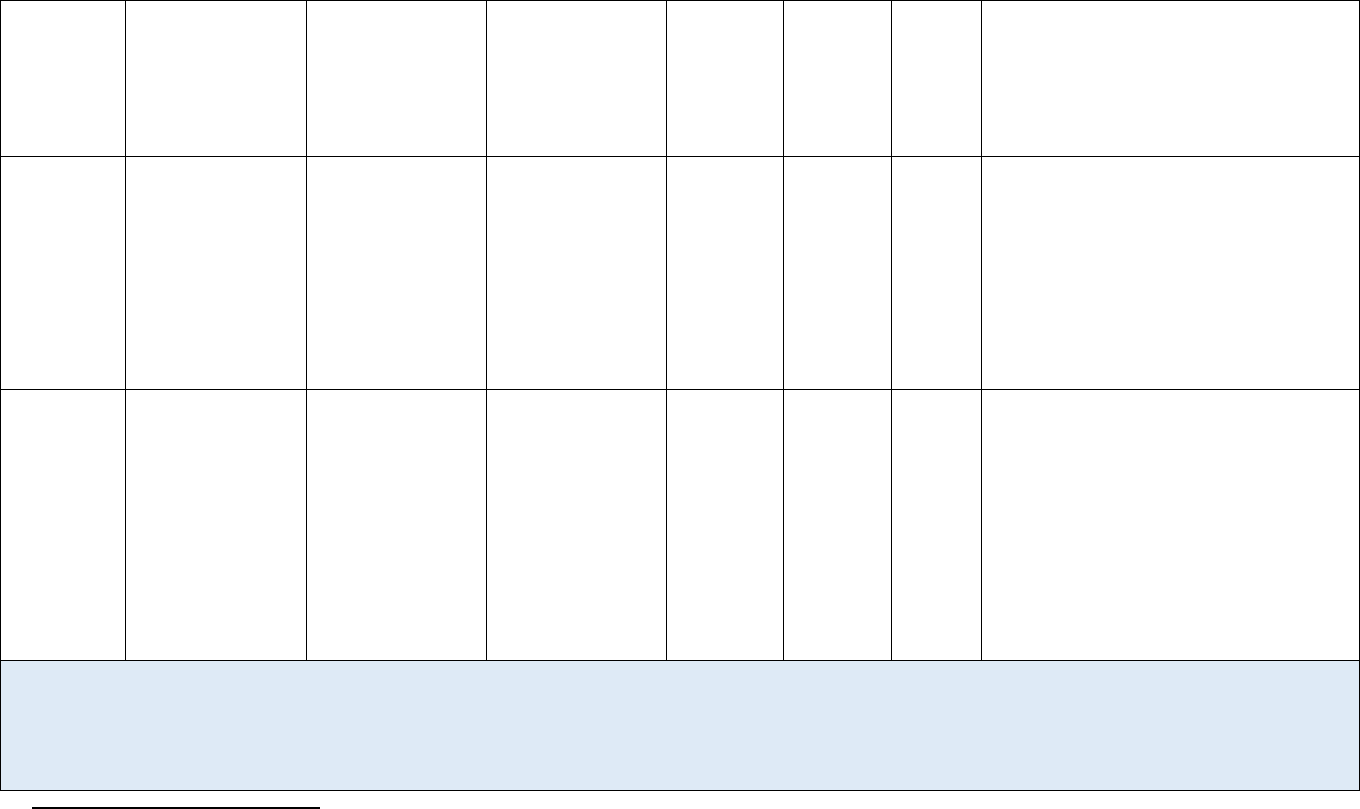
107
Bayoumi
et al.
(2012)
2
0.54 mi (30%)
Not willing
(12%), 10 min
(30%),
20 min (22%),
30 min (14%),
40 min (22%)
Not willing
(12%);
0.54 mi (30%);
1.08 mi (22%);
1.62 (14%); 2.16
(22%)
1.77
Ottawa
249
Respondents were asked how far
they would be willing to walk to a SIF.
Source: Leonard, DeRubeis, & Strike
(2008)
Kral et al.
(2010)
3
0.59-1.08 miles
(33%)
1-5 min (17%),
6-10 min (22%),
11-20 min
(33%), 21-30
min (16%), >30
min (12%)
0.05-0.27
(17%);
0.32-0.54 mi
(22%);
0.59-1.08 mi
(33%);
1.14-1.62 mi
(16%);
>1.62 mi (12%)
1.36
San
Francisc
o
513
Respondents would be willing to
walk 11-20 minutes (33%) to SIF.
82% respondents willing to take bus
to SIF. Source: Data from 2008.
Fischer &
Allard
(2007)
4
0.29 mi-0.59mi
(28.5%)
5 blocks or less
(28.5%);
10 blocks or less
(25.7%);
>1 km (22.3%);
1 km or less
(20.1%);
one block or less
(3.4%)
0.29 mi or less
(28.5%);
0.59 mi or less
(25.7%);
>0.62 mi
(22.3%);
0.62 mi or less
(20.1%);
0.06 mi or less
(3.4%)
0.63
Victoria
250
Stakeholder interviews found that on
average, drug users reported they
would travel 3-5 blocks to use a SCS.
Source: I-Track Phase 2 (2005-
2008).
2
Bayoumi et al;2012.
3
Kral AH, Wenger L, Carpenter L, Wood E, Kerr T, Bourgois P. Acceptability of a Safer Injection Facility among Injection Drug Users in San Francisco.
Drug Alcohol Depend. 2010;110(1-2):160-163.
4
Fischer B, Allard C. Feasibility Study on ‘Supervised Drug Consumption’ Options in the City of Victoria Victoria, Centre for Addictions Research of British
Columbia, University of Victoria.2007.

108
Willingness to travel: youth
Bouvier et
al. (2017)
5
0.59-1.08 miles
(35.3%)
1-10 min
(17.7%), 11-20
min (35.3%),
21-30 min
(23.5%),
>30 min
(17.7%), Don't
Know (5.9%)
0.05-0.54 mi
(17.7%);
0.59-1.08 mi
(35.3%);
1.14-1.62 mi
(23.6%);
>1.62 mi
(17.7%); don't
know (5.9%)
1.62
Rhode
Island
54
Among 34 respondents who were
willing to use SIF, 12 (35.3%)
indicated 11-20 min would be longest
time willing to travel to SIF.
Source: Rhode Island Young Adult
Prescription Drug Study (RAPiDs)
Sample: Youth aged 18-29 who have
reported NMPO, recruited from
January 2015 to February 2016. This
study's population restricts to those
who have ever injected drugs, have a
sex partner who injects drugs, or
have at least one close friend who
injects drugs.
5
Bouvier BA, Elston B, Hadland SE, Green TC, Marshall BDL. Willingness to use a supervised injection facility among young adults who use prescription
opioids non-medically: a cross-sectional study. Harm Reduct J. 2017;14:13.

109
Willingness to Use a SIF
The following table details the findings from a literature review of peer-reviewed studies on the willingness to use a SIF among
people who use drugs. For completeness we looked at willingness to use a SIF in different settings and among different
populations, but did not include these values in our estimates.
Study
Willing to use
SIF
Sample
Sample
Descriptio
n
Location
Notes
Willingness to use a SIF
(general)
Shaw et al.
(2015)
6
75.2%
270
PWID who
injected in
past 12
months
Ottawa
50.7% of those who want a SIF reported they would use
it daily. 45.8% of those who responded in favor of a SIF
injected heroin in previous year, 46.3% reported
injecting opiates a few times a week or more. 80% of this
SIF group were homeless in past 12 months and 60% per
unstably housed. 82.7% injects in public and 83.5%
overdosed in past 12 months.
Sample: Street based recruitment from PROUD trial in
2013.
6
Shaw A, Lazarus L, Pantalone T, et al. Risk environments facing potential users of a supervised injection site in Ottawa, Canada. Harm Reduct J.
2015;12:49.

110
Leonard,
DeRubeis,
& Strike
(2008)
7
64.0%
250
PWID who
injected in
past 6
months
Ottawa
64% reported would use a SIF; 14% reported they might
use a SIF. 86% reported they would use the SIF if located
in a convenient location. Among these respondents, 45%
women and 32% men said they would always use a SIF to
inject. 58% of both women and men indicated they would
use a SIF if it was located in a pre-existing service they
already used. 93% of women and 82% of men indicated
they would be willing to use standalone SIF. 23% of
respondents reported at least one non-fatal OD in prior 6
months. 24 respondents reported last OD occurred in
public space.
Sample: Recruitment in 2005. 180 men and 70 women
were surveyed. Top 3 drugs injected were cocaine, crack
cocaine, & morphine. Top 3 reasons for both men &
women were the ability to get clean sterile injection
equipment, ability to inject in private vs. public, & to be
safe from police.
Green et al.
(2004)
8
76.0%
251
PWID who
injected in
public or
semi-public
in the past 6
months
Montreal
Public injectors with histories of cocaine or heroin
overdose and injection drug use who injected at least
weekly were significantly more likely to be willing to use
SIF. 83% who are willing to use SIF have ever
experienced an overdose.
Drug of Choice: Most willing to use SIF were cocaine
users (78%), but that is because injection drug use in
Montreal is cocaine centered.
Sample: SurvUDI study (surveillance project) on PWID in
past 6 months. Sampled from 12 recruiting sites from
April 2001 to February 2002, but most of the sample
came from downtown SEP (93.6%).
7
Leonard L, DeRubeis E, Strike C. Needs Assessment for a Safer Injecting Facility in Ottawa, Canada. Ottawa, Ontario: University of Ottawa.2008.
8
Green TC, Hankins CA, Palmer D, Boivin J-F, Platt R. My Place, Your Place, or a Safer Place: The Intention Among Montréal Injecting Drug Users to Use
Supervised Injecting Facilities. Can J Public Health. 2004;95(2):110-114.

111
Fischer &
Allard
(2007)
9
72.3%
250
PWID who
injected in
the past 6
months
Victoria
Stakeholder interviews found that on average, drug users
reported they would travel 3-5 blocks to use a SIS. 40%
had injected daily in past 6 months; 76% had injected in
street over past 6 months; 30% of PWIDs reported that
the street was where the most injected in past 6 months;
over 50% reported they would use a SIF for 75-100% of
injections. Reasons were provided why they would use.
Willingness to cover included.
Source: I-Track Phase 2 (2005-2008).
DeBeck et
al. (2012)
10
54% report
willingness pre-
SIF; 65% (of both
who said yes and
no pre-SIF)
actually attended
a SIF
442
PWID who
injected in
the past
month
Vancouver
Study assessed whether reports of willingness to use a
SIF before the program opened were associated with
subsequent self-reported attendance at the SIF. Sampled
from street outreach or self-referral. Pre-SIF opening
willingness measured from December 2001 to May 2003.
Post-SIF opening attendance measured December 2003
to November 2005.
Pre-SIF: 54% (344 out of 600) reported willingness to
use SIF, 6% unsure (40/600). Of those who were unsure,
18 (62% of 29) used the SIF.
Post-SIF: 442 respondents were followed up from pre-
SIF period. Of the 274 who reported initial willingness to
use SIF, 198 (72%) later attended the SIF. 91 (54% of
198) of those who were initially unwilling later reported
attending the SIF.
Wood et al.
(2003)
11
36.6% of PWIDs,
52% of public
injectors
expressed
willingness to
attend a SIF
587
PWID who
injected at
least once in
past month
Vancouver
Public Injection: Public injection was asked for the past
6 months. 29.3% of those who said they were willing to
use a SIF were public injectors.
Heroin use: 42.3% of those who are willing to attend a
SIF injected heroin greater than once per day
9
Fischer et al;2007.
10
DeBeck K, Kerr T, Lai C, Buxton J, Montaner J, Wood E. The validity of reporting willingness to use a supervised injecting facility on subsequent
program use among people who use injection drugs. Am J Drug Alcohol Abuse. 2012;38(1):55-62.
11
Wood E, Kerr T, Spittal PM, et al. The potential public health and community impacts of safer injecting facilities: evidence from a cohort of injection
drug users. J Acquir Immune Defic Syndr. 2003;32(1):2-8.

112
Sample/Source: Surveyed active PWID enrolled in the
Vancouver Injection Drug User Study (VIDUS): June
2001-June 2002.
Kerr et al.
(2003)
12
92% (assuming 0
restrictions);
64% willing to
use SIF if no drug
sharing; 62%
willing to use if
no assisted
injection; 54%
willing to use if
required client
registration; 31%
will use if all
three restrictions
in place
458
Active PWID
Vancouver
25.8% of those willing to use a SIF injected heroin at least
once a day; 69.7% of those willing to use a SIF injects in
public; 38% of cocaine users were willing to attend
Sample: Active PWID were informed of study via street-
based recruitment and "snowballing" in 2003.
Respondents must provide evidence of track marks.
Sampled from 1 of 3 locations: rented storefront, Life
Skills Centre, and SEP.
Low
(2014)
13
87.0%
420
Syringe
exchange
clients
King County
Master's thesis with Caleb Banta-Green as part of
committee.
IDU: 91% who muscled were interested in SIF; 98%
femoral were interested in SIF
OD: 93% who had an overdose interested in SIF
Naloxone: 93% who have naloxone in past 3 months
were interested in SIF
Sample: Street intercept survey at SEPs for 2 weeks in
2013 at syringe exchanges
12
Kerr T, Wood E, Small D, Palepu A, Tyndall MW. Potential use of safer injecting facilities among injection drug users in Vancouver's Downtown
Eastside. CMAJ. 2003;169(8):759-763.
13
Low D. Interest in a Safe Injection Facility Among Injection Drug Users in King County, WA. Seattle, WA: Department of Health Services, University of
Washington; 2014.

113
Kral et al.
(2010)
14
85.0%
602
PWID who
injected
within the
past 30 days
San
Francisco
513 (85%) respondents said they would use a SIF should
it be convenient for them. Most respondents would be
willing to walk 11-20 minutes (33%) to SIF. Only 28%
would attend a SIF if it took more than 20 mins to walk
there. 82% respondents willing to take bus to SIF.
Public injection: 71% inject in public settings in past 6
months
SIF use: of those who would use SIF, 50% expected to
use it daily, 26% would use it 3-6 days/week, 12% 1-2
days/week, 11% would use it less than weekly.
Sample: represents 3.5% of all PWIDs in SF; Used
targeted sampling methods in community settings in
2008
Eligibility: IDU in past 30 days (check for venipuncture)
Characteristics: Majority of sample were homeless (69%)
Willingness to use a SIF in a hospital
Ti et al.
(2015)
15
68.2%
732
PWID who
injected at
least once in
past month
or HIV
positive &
injected illicit
drugs
Vancouver
Those who said they would use a SIF in hospital (47.7%)
said they have used illicit drugs in hospital (ever). The
most common reasons for using a SIF in hospital: 45.9%
to be able to stay in hospital, 37.9% to reduce their drug-
related risks, 19.4% to reduce stress with being kicked
out of hospital because they were using.
Source: Willingness to access an in-hospital SIF if
hospitalized people were measured from subjects
recruited from VIDUS and AIDS Care Cohort to evaluate
Exposure to Survival Services (ACCESS) in 2013.
14
Kral et al;2010.
15
Ti L, Buxton J, Harrison S, et al. Willingness to access an in-hospital supervised injection facility among hospitalized people who use illicit drugs. J Hosp
Med. 2015;10(5):301-306.

114
Willingness to use a SIF in a SEP
Broadhead
et al.
(2003)
16
79.0%
158
Needle
exchange
clients
NYC
28% injected in public place last month. 93% of 44 public
injectors were willing to use SIF. 71% of 114 nonpublic
injectors were willing to use SIF.
SIF knowledge: only 36 out of 158 respondents had
heard of SIFs before survey, and those that had heard of
SIFs before had less favorable view of them than people
who never heard of them before survey
Sample: Sampled every 3rd client from NEP clients at
Positive Health Project in midtown Manhattan over 8
weeks in 2002. Many co-located services at this program.
Drug of choice: 44% injects cocaine most frequently
IDU: 36% injects daily
Willingness to use a SIF among youth
Hadland et
al. (2014)
17
42.3%
414
Youth who
used an illicit
drug in past
30 days
Vancouver
Percentage is respondent’s reported use of SIF at least
once; SIF-using youth were more likely to inject in public
(AOR = 2.08). 51.4% went to SIF at least weekly, 44.5%
used it for at least 1/4 of all injections.
Sample: Recruited from At-Risk Youth Study, aged 14-
26, from September 2005 to May 2012.
16
Broadhead RS, Borch CA, Hulst Yv, Farrell J, Villemez WJ, Altice FL. Safer Injection Sites in New York City: A Utilization Survey of Injection Drug Users.
J Drug Issues. 2003;33(3):733-750.
17
Hadland SE, DeBeck K, Kerr T, et al. Use of a medically supervised injection facility among street youth. J Adolesc Health. 2014;55(5):684-689.

115
Bouvier et
al. (2017)
18
63.0%
54
Youth
reporting
NMPO who
ever injected
drugs, have a
sex partner
who injects
drugs, or
have at least
1 close friend
who injects
drugs
Rhode
Island
40 respondents (74.1%) thought their friends/other
people they knew would use a SIF. Among 34
respondents who were willing to use SIF, 12 (35.3%)
indicated 11-20 min would be longest time willing to
travel to SIF. Among 31 respondents reporting IDU in last
6 months, 27 (87.1%) reported willingness to use a SIF.
Among those who inject daily, all 12 (100%) reported
willingness to use SIF.
Sample/Source: Data from Rhode Island Young Adult
Prescription Drug Study, which canvasses youth aged 18-
29 who have reported NMPO. Respondents were
recruited from January 2015 to February 2016.
18
Bouvier et al;2017.

116
Injection Drug Use among Heroin and Prescription Opioid Misusers
The following table details the findings from a literature review of peer-reviewed studies on the percentage of heroin users
who inject and the percentage of prescription opioid misusers who inject.
Study
% of users
who inject
Type of
Sample
Sample
Location
Notes
Percentage of heroin users who inject
NASATS
(2006)
19
62.8%
Heroin
265,895
US
Table 3.4 Admissions by primary substance of abuse and usual
route of administration from the SAHMSA TEDS 2004.
NASATS
(2016)
20
71.7%
Heroin
357,293
US
Table 2.4a (12 & older) Admissions by primary substance of
abuse & usual route of administration from the SAHMSA TEDS
2014.
Rosenblum
et al.
(2007)
21
78.0%
Heroin
2,988
US
Data collected from 72 MMTPs located in 33 states in 2005.
2988 out of 5663 reported heroin as primary drug. Percentage
is lifetime injection of heroin among primary heroin abusers.
Novak &
Kral
(2011)
22
44.2%
Heroin
459
US
Repeated cross-sectional data (2005-2007) from the National
Survey on Drug Use and Health (NSDUH). Covers usage in the
past year. NSDUH sampling excludes people with no fixed
household address (homeless and/or transient people not in
shelters), active duty military, residents of institutional group
quarters (correctional facilities, nursing homes, mental
institutions, and long term hospitals).
19
Treatment Episode Data Set (TEDS) 1994-2004: National Admission to Substance Abuse Treatment Services. Substance Abuse and Mental Health
Services Administration, Office of Applied Studies. Rockville, MD 2006.
20
Treatment Episode Data Set (TEDS): 2004-2014. National Admissions to Substance Abuse Treatment Services. Substance Abuse and Mental Health
Services Administration, Center for Behavioral Health Statistics and Quality. Rockville, MD 2016.
21
Rosenblum A, Parrino M, Schnoll SH, et al. Prescription opioid abuse among enrollees into methadone maintenance treatment. Drug Alcohol Depend.
2007;90(1):64-71.
22
Novak SP, Kral AH. Comparing Injection and Non-Injection Routes of Administration for Heroin, Methamphetamine, and Cocaine Uses in the United
States. J Addict Dis. 2011;30(3):248-257.

117
Galea et al.
(2006)
23
65.8%
Heroin in
past year
1,059
NYC
Sampled habitual drug users via street based outreach (Harlem
and Bronx) from November 2001 through May 2004.
Used heroin, crack, or cocaine at least once in 2 months prior to
interview.
Studies on injection of prescription opioids or non-heroin opiates (used non-medically)
Surrat,
Kurtz, &
Cicero
(2011)
24
23.8%
Prescription
opioids
791
South
Florida
(Broward,
Lee, Miami-
Dade, Palm
Beach
counties)
Eligibility: 18 years or older who reported abuse of
psychoactive prescription drugs at least 5 times in past 90 days.
Sample: Recruited from treatment programs, street drug users,
and MSM who reported current illicit stimulant use. 18-24 year
olds had significantly higher odds of employing alternate route
of administration. Could choose multiple routes of
administration. Only participants who reported at least one
occasion of prescription opioid abuse in the past 90 days were
included.
Zule et al.
(2016)
25
17.4%
Prescription
opioids
393
North
Carolina
1,985 participants (drugs users & MSM, and their sex partners
(don't need to be drug users)) were recruited in 2 rural & 2
urban NC counties from 2005 to 2008. 393 reported
nonmedical use of prescription opioids. Of the 393, 17.4%
injected prescription opioids in last 30 days.
Sampling: RDS sampling method from the different Sexual
Acquisition and Transmission of HIV Cooperative Agreement
Project (SATHCAP) program sites
23
Galea S, Nandi A, Coffin PO, et al. Heroin and cocaine dependence and the risk of accidental non-fatal drug overdose. J Addict Dis. 2006;25(3):79-87.
24
Surratt H, Kurtz SP, Cicero TJ. Alternate Routes of Administration and Risk for HIV among Prescription Opioid Abusers. J Addict Dis. 2011;30(4):334-
341.
25
Zule WA, Oramasionwu C, Evon D, et al. Event-level analyses of sex-risk and injection-risk behaviors among nonmedical prescription opioid users. Am
J Drug Alcohol Abuse. 2016;42(6):689-697.

118
Davis &
Johnson
(2008)
26
4.4%
Prescription
opioids
501
NYC
Sampling: Project ethnographers approached street drug users
in public settings from 2004 to 2006. This street-recruitment
strategy likely under-sampled street drug users among working
persons and methadone clients who comply with medication
schedules. It likely oversampled persons who were
unemployed, homeless, engaged in illegal hustles, & spent most
of their time in public settings. Those recruited are very likely
to participate actively (as consumers or sellers) in street
markets for heroin, medication diversion, & prescription opioid
or other pill transfers.
Of 586 street drug users, 501 reported having nonmedically
used prescription opioids. Of those, 4.4% report injecting Rx
opioids.
NASATS
(2006)
27
11.8%
Other non-
heroin
opiates
63,243
US
Table 3.4 Admissions by primary substance of abuse and usual
route of administration from the SAHMSA TEDS 2004.
Sample: from substance use treatment programs in US.
Opiates include: methadone, buprenorphine, codeine,
hydrocodone, hydromorphone, meperidine, morphine, opium,
oxycodone, pantazocine, propoxyphene, tramadol, and other
drug with morphine-like effects.
NASATS
(2016)
28
17.5%
Other non-
heroin
opiates
132,387
US
Table 2.4a Admissions by primary substance of abuse & usual
route of administration from the SAHMSA TEDS 2014.
Opiates include: methadone, buprenorphine, codeine,
hydrocodone, hydromorphone, meperidine, morphine, opium,
oxycodone, pantazocine, propoxyphene, tramadol, and other
drug with morphine-like effects.
Katz et al.
(2011)
29
10.0%
Prescription
opioids
San Diego
This paper itself is a literature review on route of
administration of people who abuse prescription opioids.
26
Davis WR, Johnson BD. Prescription Opioid Use, Misuse, and Diversion among Street Drug Users in New York City. Drug Alcohol Depend. 2008;92(1-
3):267-276
27
National Admission to Substance Abuse Treatment Services;2006.
28
National Admission to Substance Abuse Treatment Services;2016.
29
Katz N, Dart RC, Bailey E, Trudeau J, Osgood E, Paillard F. Tampering with prescription opioids: nature and extent of the problem, health
consequences, and solutions. Am J Drug Alcohol Abuse. 2011;37(4):205-217

119
Source: Percentage derived from 2007 NIDA Community
Epidemiology Work Group.
Sample: Persons admitted to substance abuse treatment.
Katz et al.
(2011)
30
3% NYC;
5%
Baltimore
& St. Louis
(each); 7%
Phoenix;
10%
Denver;
14%
Chicago
Prescription
opioids
US
This paper itself is a literature review on route of
administration of people who abuse prescription opioids.
Source: Percentage derived from 2007 NIDA Community
Epidemiology Work Group.
Sample: Subjects were persons admitted to substance abuse
treatment and primarily addicted to "other opiates" in 2006.
Rosenblum
et al.
(2007)
31
32.9%
Prescription
opioids
2,174
US
Data from 72 MMTPs located in 33 states in 2005. Of the 5663
respondents, 38% (N=2174) indicated a Rx opioid as primary
drug. 32.9% of primary Rx opioid abusers reported that they
had a lifetime history of injecting their primary drug
Havens,
Walker, &
Leukefeld
(2007)
32
35.3%
Prescription
opioids
184
Rural
Appalachian
Kentucky
Percentage indicates ever injecting opioid analgesics.
Eligibility: using Oxycontin at least once in prior 3 years and
reported having used any Rx opioid in past 30 days. Entire
sample are using opioids non-medically.
Sampling: For the purposes of the current study, participants
who were initially recruited via flyers or from community key
informants and agreed to participate in the study were asked to
refer additional participants. Those who were referred were
also asked to refer additional participants and so on. Data were
collected from November 2004 to September 2005.
30
Katz et al;2011.
31
Rosenblum et al;2007.
32
Havens JR, Walker R, Leukefeld CG. Prevalence of opioid analgesic injection among rural nonmedical opioid analgesic users. Drug Alcohol Depend.
2007;87(1):98-102.

120
Public Injection
The following table details the findings from a literature review of peer-reviewed studies on the percentage of people who
inject drugs who primarily injects in public or semi-public settings. For completeness we looked at different time frames and
frequencies of public injecting, but did not include those values in our estimates.
Study
Public Injection
Sample
Location
Notes
Public or semi-public spaces is most common place for injecting
Fischer & Allard
(2007)
33
30% street was where injected most
in past 6 months; 76% had injected
in street in past 6 months
250
Victoria
Source: I-Track Phase 2 (2005-2008).
40% of respondents had injected daily in
past 6 months.
Leonard, DeRubeis, &
Strike (2008)
34
1/5 reported that they ONLY inject
in public places; 2/3 reported public
injection
250
Ottawa
Recruitment occurred in 2005. 180 men
and 70 women were surveyed. 23% of
respondents reported at least one non-
fatal OD in prior 6 months. 24 respondents
reported last OD occurred in public space.
No information on sampling. Had to have
injected drugs in past 6 months. Top 3
drugs injected were cocaine, crack
cocaine, and morphine.
DeBeck et al. (2009)
35
22.9% usually or always injecting in
public in past 6 months
620
Vancouver
Source: Vancouver IDU study (2003-
2005)
33
Fischer & Allard;2007.
34
Leonard et al;2008.
35
DeBeck K, Small W, Wood E, Li K, Montaner J, Kerr T. Public injecting among a cohort of injecting drug users in Vancouver, Canada. J Epidemiol
Community Health. 2009;63(1):81-86.

121
Public Injection (engage in public injection, but time frame unclear)
Leonard, DeRubeis, &
Strike (2008)
36
2/3 reported public injection; 1/5
reported that they ONLY inject in
public places
250
Ottawa
Recruitment occurred in 2005. 180 men
and 70 women were surveyed. 23% of
respondents reported at least one non-
fatal OD in prior 6 months. 24 respondents
reported last OD occurred in public space.
No information on sampling. Had to have
injected drugs in past 6 months. Top 3
drugs injected were cocaine, crack
cocaine, and morphine.
Kerr et al. (2003)
37
21.8% injects in public
458
Vancouver
Active PWID were informed of study
through street-based recruitment and
"snowballing" in 2003. Respondents must
provide evidence of track marks. Sampled
from 1 of 3 locations: rented storefront,
Life Skills Centre, and SEP
Public Injection in past 6 months
DeBeck et al. (2012)
38
40.3% of all respondents (N=442)
reported public injecting in the past
6 months
442
Vancouver
Pre-SIF opening willingness measured
from December 2001 to May 2003. Post-
SIF opening attendance measured
December 2003 to November 2005.
Fischer & Allard
(2007)
39
76% had injected in street in past 6
months; 30% street was where
injected most in past 6 months
250
Victoria
Source: I-Track Phase 2 (2005-2008).
40% of respondents had injected daily in
past 6 months.
36
Leonard et al;2008.
37
Kral et al;2003.
38
DeBeck et al;2012.
39
Fischer & Allard;2007.

122
Wood et al. (2003)
409
20.6% inject in public in the last 6
months at time of interview
587
Vancouver
Surveyed active IDU enrolled in the
Vancouver Injection Drug User Study
(VIDUS): June 2001-June 2002.
Sample: Had to have injected at least once
in past month.
Public Injection: Public injection was
asked for the past 6 months. 29.3% of
those who said they were willing to use a
SIF were public injectors.
Kral et al. (2010)
41
71 % inject in public settings in last
6 months
602
San
Francisco
513 (85%) respondents said they would
use a SIF should it be convenient for them.
Most respondents would be willing to
walk 11-20 minutes (33%) to SIF. Only
28% would attend a SIF if it took more
than 20 mins to walk there. 82%
respondents willing to take bus to SIF.
Sample: represents 3.5% of all IDUs in SF;
Used targeted sampling methods in
community settings in 2008.
Eligibility: IDU in past 30 days (check for
venipuncture)
Characteristics: Majority of sample were
homeless (69%)
Public injection: public injection defined
as street, alley, public bathroom, or park
40
Wood et al;2003.
41
Kral et al;2010.

123
Public Injection in past month
Broadhead et al.
(2003)
42
28% of men inject in public space in
last month; 72% of women inject in
public space last month
158
New York
28% injected in public place last month.
93% of 44 public injectors were willing to
use SIF. 71% of 114 nonpublic injectors
were willing to use SIF.
Sampling: Sampled every third client
from needle exchange clients at Positive
Health Project in midtown Manhattan over
8 weeks in 2002. Lots of co-located
services at this program.
42
Broadhead et al;2003.

124
Definition of Overdose in SPARCS
We defined opioid overdoses using ICD9 code 965.0x, poisoning by opiates and related narcotics, and also included 967.xx, 969.xx, and
970.xx, representing any other drug poisonings that was accompanied by codes 304.0x, 304.7x, 305.5x, representing opioid use disorder.
Defining opioid overdoses is a challenge that has been identified in the literature
26-29
, and we chose to use codes that would most
accurately identify opioid overdoses (high sensitivity), recognizing that the data would not capture all overdose admissions (low
specificity).
Appendix VI, Table 1: Health care Utilization by Leading DRGs in SPARCS, 2014.
ED to Inpatient
Direct Inpatient
DRG (%)
918 - POISONING & TOXIC EFFECTS OF DRUGS
W/O MCC
49.3%
43.0%
917 - POISONING & TOXIC EFFECTS OF DRUGS
W MCC
34.0%
26.0%
871 - SEPTICEMIA OR SEVERE SEPSIS W/O MV
96+ HOURS W MCC
1.7%
1.9%
004 - TRACH W MV 96+ HRS OR PDX EXC FACE,
MOUTH & NECK W/O MAJ O.R.
0.8%
0.6%
*Note: the 4 DRGs were chosen as either the top DRGs used or because the DRG was expensive (even if occurrence is rare).

125
Inpatient Unit Cost by Overdose Fatality
The following tables show the weighted average cost for inpatient care when considering the leading or most expensive DRGs identified in
SPARCS based on utilization by people with an opioid overdose.
Appendix VII, Table 1: NON-FATAL Inpatient
Utilization and Average Medicare Payment Rates
DRG
Non-Fatal
Utilization
Non-Fatal
Proportion
Average
Payment
0004
9
0.007
$851
871
25
0.020
$472
917
475
0.382
$6,869
918
734
0.591
$6,074
TOTAL
1243
1
$14,267
Appendix VII, Table 2: FATAL Inpatient Utilization and
Average Medicare Payment Rates
DRG
Fatal
Utilization
Fatal
Proportion
Average
Payment
0004
3
0.081
$9,531
871
1
0.027
$635
917
28
0.757
$13,603
918
5
0.135
$1,390
TOTAL
37
1
$25,159

126
Cost Estimate Tables
The following are tables that detail the base case and alternative case costs under different assumptions. See main report to get further
information about the base case and alternative case scenario descriptions.
Table 1: Base Case Costs to the Health care System per Year: Current Costs and Projected Costs with one SIF
Health care
Services
Current Costs
Costs with 1 SIF, avoiding all health
care costs from overdoses occurring in
SIFs
Costs with 1 SIF with some health
care utilization costs for overdoses
occurring in SIFs
Non-Fatal
Fatal
Total
Non-Fatal
Fatal
Total
Non-Fatal
Fatal
Total
Ambulance
$3,271,600
$322,000
$3,593,600
$3,204,500
$315,400
$3,519,900
$3,226,200
$317,500
$3,543,700
ED Visit
$4,599,500
$4,600
$4,604,100
$4,505,200
$4,500
$4,509,700
$4,515,500
$4,500
$4,520,000
Inpatient
Discharge
$36,171,300
$5,660,000
$41,831,300
$35,429,100
$5,543,900
$40,973,000
$35,510,200
$5,594,600
$41,104,800
Total Cost
per year
$44,042,500
$5,986,600
$50,029,100
$43,138,800
$5,863,700
$49,002,500
$43,251,800
$5,916,600
$49,168,400
Cost
Savings per
year
-
-
-
$903,700
$122,800
$1,026,500
$790,600
$70,000
$860,600
*Assumes that 19 overdose fatalities prevented and 190 non-fatal overdoses prevented per year

127
Table 2: Base Case Costs to the Health care System per Year with four SIFs
Health care Services
Costs with 4 SIFs, avoiding all health care costs
from overdoses occurring in SIFs
Costs with 4 SIFs with some health care utilization
costs for overdoses occurring in SIFs
Non-Fatal
Fatal
Total
Non-Fatal
Fatal
Total
Ambulance
$3,034,900
$298,700
$3,333,600
$3,111,400
$306,000
$3,417,400
ED Visit
$4,266,700
$4,200
$4,270,900
$4,599,300
$4,400
$4,603,700
Inpatient Discharge
$33,554,200
$5,250,500
$38,804,700
$33,839,800
$5,429,500
$39,269,300
Total Cost per year
$40,855,800
$5,553,400
$46,409,200
$41,550,600
$5,739,900
$47,290,500
Cost Savings per year
$3,186,700
$433,200
$3,619,900
$2,491,900
$246,700
$2,738,600
Annual Cost Savings per
SIF
$796,700
$108,300
$905,000
$623,000
$61,700
$684,700
*Assumes that 67 overdose fatalities prevented and 670 non-fatal overdoses prevented per year

128
Table 3: Alternative Case Costs to the Health care System per Year: Current Costs and Projected Costs with one SIF
Health care
Services
Current Costs
Costs with 1 SIF, avoiding all health care costs
from overdoses occurring in SIFs
Costs with 1 SIF with some health
care utilization costs for overdoses
occurring in SIFs
Non-Fatal
Fatal
Total
Non-Fatal
Fatal
Total
Non-Fatal
Fatal
Total
Ambulance
$3,271,600
$322,000
$3,593,600
$3,140,900
$309,100
$3,450,000
$3,183,100
$313,200
$3,496,300
ED Visit
$4,599,500
$4,600
$4,604,100
$4,415,700
$4,400
$4,420,100
$4,435,800
$4,500
$4,440,300
Inpatient
Discharge
$36,171,300
$5,660,000
$41,831,300
$34,726,000
$5,433,900
$40,159,900
$34,883,900
$5,532,700
$40,416,600
Total Cost
per year
$44,042,500
$5,986,600
$50,029,100
$42,282,700
$5,747,400
$48,030,100
$42,502,800
$5,850,300
$48,353,100
Cost
Savings per
year
-
-
-
$1,759,800
$239,200
$1,999,000
$1,539,700
$136,200
$1,675,900
*Assumes that 37 overdose fatalities prevented and 370 non-fatal overdoses prevented per year
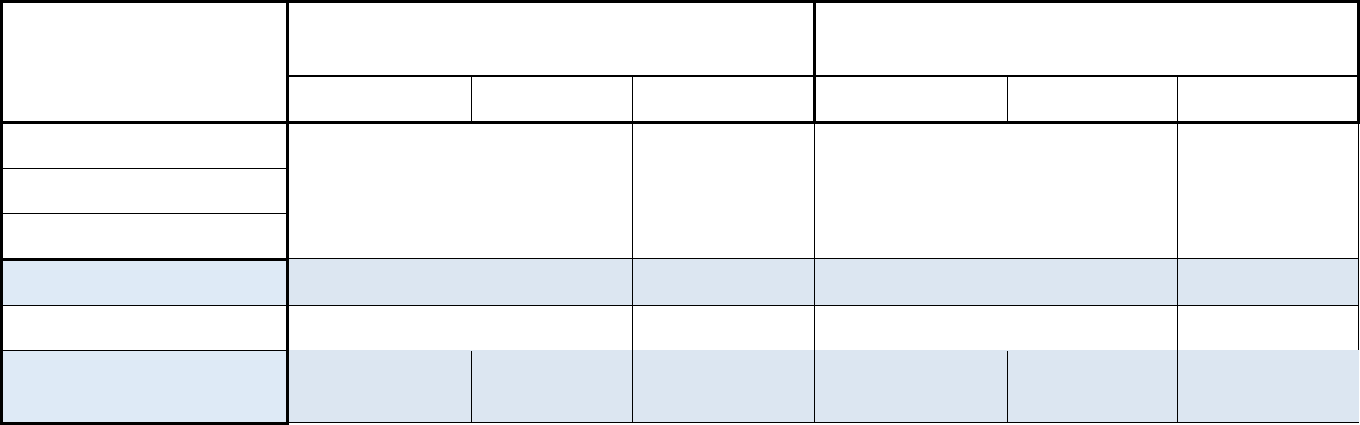
129
Table 4: Alternative Case Costs to the Health care System per Year with four SIFs
Health care Services
Costs with 4 SIFs, avoiding all health care costs
from overdoses occurring in SIFs
Costs with 4 SIFs with some health care utilization
costs for overdoses occurring in SIFs
Non-Fatal
Fatal
Total
Non-Fatal
Fatal
Total
Ambulance
$2,812,300
$276,800
$3,089,100
$2,960,800
$290,900
$3,251,700
ED Visit
$3,953,800
$3,900
$3,957,700
$4,599,500
$4,500
$4,604,000
Inpatient Discharge
$31,093,300
$4,865,400
$35,958,700
$31,647,500
$5,597,600
$37,245,100
Total Cost per year
$37,859,400
$5,146,100
$43,005,500
$39,207,800
$5,893,000
$45,100,800
Cost Savings per year
$6,183,100
$840,400
$7,023,500
$4,834,700
$93,500
$4,928,200
Annual Cost Savings per
SIF
$1,545,800
$210,100
$1,755,900
$1,208,700
$23,400
$1,232,100
*Assumes that 130 overdose fatalities prevented and 1,300 non-fatal overdoses prevented per year.

130
APPENDIX F
Legal Challenges to and Avenues for Supervised Injection
Facility Implementation in New York City
Prepared by:
Kristen Underhill, DPhil, JD
Associate Professor of Law, Columbia Law School
Establishing a supervised injection facility (SIF) or safe consumption site (SCS) in any
United States jurisdiction raises questions of federal, state, and local law. This brief
memorandum will evaluate potential legal challenges to operating a SIF in New York City,
as well as several legal pathways for establishing a local SIF. This memorandum will outline
challenges for SIF clients, criminal and civil law issues for SIF staff and property owners,
specific concerns for licensed health care providers who practice at SIFs, and potential
avenues for SIF implementation in New York City.
I. Federal, State, and Local Law Challenges for a New York City SIF
A. Legal Challenges for SIF Clients
The federal Controlled Substances Act (CSA)
1
poses potential legal difficulties for SIF
clients in any state. Clients of the SIF who bring controlled substances on the premises
would violate § 844 of the CSA, which penalizes persons for “knowingly or intentionally
possess[ing] a controlled substance.”
2
Penalties for an initial violation include a minimum
fine of $1,000 and/or imprisonment up to one year, with larger penalties for subsequent
offenses. Where users possess drugs with an intention to distribute them to other people, §
841 levies steep additional penalties, depending on the type and amount of the substance.
3
People who use drugs run the risk of arrest in any location where they possess controlled
substances, but a SIF could present a known location for enforcement efforts.
Clients’ possession of controlled substances and paraphernalia would also violate several
state criminal laws, principally N.Y. Penal Law § 220.03, which criminalizes the possession
of small amounts of controlled substances as a misdemeanor.
4
Prosecutions for possessing
extremely small amounts of controlled substances, including residue, are within the letter
1
21 U.S.C. §§ 801 et seq. (2017).
2
21 U.S.C. § 844 (2017). This section exempts persons who possess a controlled substance with a “valid
prescription” from a practitioner acting in the scope of professional practice, but clients with nonprescription
substances will violate the statute.
3
21 U.S.C. § 841 (2017).
4
N.Y. Penal Law § 220.03 (2017). A separate section criminalizes the possession of marijuana, which may be
relevant for some SIF clients, N.Y. Penal Law § 221.05 (2017). Possession of small quantities is a
misdemeanor; larger quantities incur felony charges.

131
of the federal CSA.
5
N.Y. Penal Law § 220.03, however, explicitly permits syringe exchange
program (SEP) clients to possess trace amounts of controlled substances in used syringes,
in order to facilitate SEP use.
6
It is useful to note that this exemption was initially
established in federal court as a logical extension of the New York state law enabling SEP
program operation.
7
A revision to the statute in 2010 subsequently codified the SEP
participant exception for trace amounts. If SIFs are authorized by state law, similar
reasoning may allow courts to find that this state statute impliedly exempts SIF clients
from possession laws for the purposes of using a SIF. N.Y. Penal Law § 220.45 similarly
criminalizes the possession of “hypodermic instruments,” including syringes and needles,
but provides a parallel exemption for SEP clients and program personnel.
8
A separate
section of the penal code, § 220.50, also criminalizes the possession of certain drug
paraphernalia, including “dilutants or adulterants” for preparing drugs.
9
(There is no SEP
client exemption for these materials, which are more likely to be used in manufacturing.)
In addition to extending the exemptions available to SEP clients, SIF clients may also
benefit from N.Y. Penal Law § 220.78, also known as the state’s “Good Samaritan” law. Like
the majority of state legislatures that passed such laws, the New York State Legislature
enacted this law primarily to promote access to emergency services for people
experiencing drug overdoses.
10
Under this statute, anyone “who, in good faith, seeks health
care for someone who is experiencing a drug overdose or other life threatening medical
emergency” is exempt from being charged or prosecuted for drug possession,
paraphernalia, or possession of alcohol by a minor.
11
This exemption extends to any
possession or paraphernalia that is discovered “as a result of such seeking or receiving
health care,” and it extends to both the victim and those who seek care on their behalf.
12
Seeking medical care for an overdose or other medical emergency may also be an
affirmative defense to some criminal sales of controlled substances, depending on prior
convictions.
13
This may provide some protection for SIF clients and staff who come in
5
See, e.g., U.S. v. Jones, 531 F.3d 163 (2d Cir. 2008).
6
Roe v. City of New York, 232 F. Supp. 2d 240 (S.D.N.Y. 2002) (interpreting an earlier version N.Y. Penal L. §
220.03, and noting that “[i[t would be bizarre to conclude that the Legislative intent was to permit the
creation of needle exchange programs in order to remove dirty needles, while at the same time frustrating
that goal by making the essential steps of participation criminal”). The current statute specifically exempts
residual amounts “in or on a hypodermic syringe . . . obtained and possessed” through a syringe exchange
program. N.Y. Penal Law § 220.03 (2017).
7
Id.
8
See also N.Y. Public Health Law § 3381, which echoes the criminal prohibition on possession or provision of
hypodermic syringes, but provides for the authorization of syringe exchange programs (SEPs) that qualify for
exemption from this law.
9
The remainder of this provision is more tailored to paraphernalia used for “manufacturing, packaging, or
dispensing,” such as scales and vials; there are no exemptions for SEPs.
10
See National Conference of State Legislatures, Drug Overdose Immunity and Good Samaritan Laws,
http://www.ncsl.org/research/civil-and-criminal-justice/drug-overdose-immunity-good-samaritan-
laws.aspx (noting that as of now, 40 states maintain Good Samaritan drug immunity laws). June 5, 2017.
11
N.Y. Penal Law § 220.78 (2017); see also N.Y. Penal Law § 220.03 (2017) (providing for this exemption).
12
N.Y. Penal Law § 220.78 (2017)
13
N.Y. Penal Law § 220.78(4) (2017).

132
contact with law enforcement during overdose responses. Indeed, there may be an
argument that this blanket exemption extends to all SIF clients and personnel, since using a
SIF may be viewed as a preventive form of seeking emergency care for overdose.
Importantly, however, this law can only extend exemptions for state drug offenses, rather
than federal offenses under the CSA.
Additional liabilities for SIF clients may depend on specific activities or substances used
within the SIF. For example, should SIF clients offer one another direct assistance with
injecting, they may violate N.Y. Penal Law § 220.46, which criminalizes injecting “a narcotic
drug” into another person’s body with that person’s consent, as a class E felony.
14
Sharing
drugs in the SIF may also qualify as “sales” under state law
15
or “distribution” under federal
law,
16
which would expose clients to additional charges in the event of arrest. New York
City’s local laws may also present challenges, particularly Administrative Code § 10-203,
which imposes criminal and civil penalties for the “manufacture, distribution, or sale” of
synthetic cannabinoids or phenethylamine, including possession with an intent to sell.
(These “designer drugs” evolve quickly to evade listing on controlled substances schedules,
which has prompted a response through local law while awaiting the inclusion of these
drugs in state and federal statutes.)
B. Legal Challenges for SIF Staff and Property Owners
This section will consider criminal law challenges arising under federal, state, and local law,
followed by questions regarding civil liability.
1. Criminal Law
Like SIF clients, SIF staff and owners will face some uncertainty under federal, state, and
local law. Most significantly, § 856 of the federal CSA—often cited as the “Crack House”
statute—imposes criminal penalties on persons who “knowingly open, lease, rent, use, or
maintain any place . . . for the purpose of . . . using any controlled substance,” or who
“manage or control any place . . . and knowingly and intentionally . . . make [it] available for
use . . . for the purpose of unlawfully . . . using a controlled substance.”
17
These provisions
may extend to the activities of SIF staff, as well as the owners of properties that house SIFs.
Penalties may include fines of up to $500,000 for individuals, $2,000,000 for institutions,
and imprisonment. SIF staff and owners may also be vulnerable to claims that they
14
N.Y. Penal Law § 220.46 (2017). Prosecutions under this statute require that the injector “unlawfully
possess” the drug. If a court or the legislature found an exemption to possession laws under § 220.03 to
enable SEP operation, the element of “unlawful possession” would be absent.
15
Sales are defined under New York law to include gifts and exchanges. See N.Y. Penal Law § 220.00(1)
(2017).
16
21 U.S.C. § 802 (2017).
17
21 U.S.C. § 856 (2017).

133
“possess” the drugs on site under § 844 or § 841(a)(1), although this is a weaker theory
compared to the § 856 violation.
18
In the event that a SIF is prosecuted and found liable for a § 856 violation, SIF owners may
also experience additional penalties under § 881 of the CSA.
19
This section extinguishes
private property rights in any property used to commit a CSA violation, including
controlled substances, vehicles, books and records, money, and real property, including
buildings and land.
20
This property would be transferred to the federal government under
custody of the U.S. Attorney General, who may then sell it or transfer it to the state for
public use.
21
The case law under § 856 does not include any prosecutions of harm reduction facilities on
the basis of clients’ drug use on the premises, and this may be a low priority for federal
drug enforcement and prosecution. But a SIF that explicitly supervises drug consumption
would be a legal first in the United States, and it is difficult to predict how federal
prosecutors may respond. There has been at least one public effort to encourage the
Attorney General to enforce § 856 against a potential SIF in Washington state, should one
successfully open.
22
At an extreme, federal agencies could also attempt to withhold federal
grants from jurisdictions that are viewed as noncompliant with a requirement of federal
law, such as § 856.
23
If the legislative branch were to oppose SIF implementation by states,
Congress could impose similarly restrictive conditions on receipt of all federal funding, or it
could specify that federal funds may not be used to operate a SIF.
24
Statutory or agency authorization of a SIF in New York would also invoke questions about
federal preemption of state or local initiatives. The federal CSA recognizes that states
independently regulate the use of controlled substances. Section 903 specifically notes that
the federal law does not “exclude[e] any State law on the same subject matter which would
otherwise be within the authority of the State, unless there is a positive conflict . . . so that
the two cannot consistently stand together.”
25
Where there is a conflict between a state and
federal law, however, the Supremacy clause of the U.S. Constitution requires that federal
18
See Scott Burris et al., Federalism, Policy Learning, and Local Innovation in Public Health: The Case of the
Supervised Injection Facility, 53 ST. LOUIS U. L.J. 1089, 1115-16 (2009).
19
21 U.S.C. § 881(a)(7) (2017).
20
21 U.S.C. § 881(a)(7) (2017).
21
21 U.S.C. §§ 881(e)(1)(B), 881(e)(4)(B) (2017).
22
Letter from Mark Miloscia, State Senator, Washington to Jeff Sessions, Attorney General (Feb. 14, 2017),
available at http://markmiloscia.src.wastateleg.org/sen-miloscia-letter-u-s-attorney-general-jeff-sessions/.
23
See, e.g., Memorandum from Jeff Sessions, Attorney General, to All Department Grant-Making Components,
May 22, 2017, available at https://www.justice.gov/opa/pr/attorney-general-jeff-sessions-issues-
memorandum-implementation-executive-order-13768 (announcing that “sanctuary jurisdictions”—those
that do not certify compliance with a named section of federal immigration law—are no longer eligible for
certain federal grants through the Department of Justice or the Department of Homeland Security); see also
County of Santa Clara v. Trump, 2017 WL 1459081 (N.D. Cal. 2017) (issuing a nationwide preliminary
injunction against an executive order limiting federal grants for sanctuary jurisdictions).
24
See Burris et al., supra note 18, at 1146-47 (noting that Congress could, in theory, limit federal funds to
programs or jurisdictions that operate SIFs, and describing an unsuccessful prior legislative effort to do so).
25
21 U.S.C. § 903 (2017)

134
law control.
26
Given the potential conflict between § 856 of the federal CSA and a state law
authorizing the operation of a SIF, it is an open legal question of whether § 856 preempts
state law in this field. There may be persuasive legal defenses for SIFs and jurisdictions that
attempt to authorize SIFs, including the argument that the CSA drafters did not intend for
the statute to reach harm reduction programming.
27
SIFs may also be within the scope of
“ethical medical practice” contemplated by the CSA, which establishes processes for
registered providers to prescribe and administer controlled substances in practice and
research.
28
These providers follow state laws regulating the practice of medicine; if SIFs are
within the usual scope of practice, there may be a colorable claim that SIFs are outside the
boundaries of activity proscribed by the CSA statute. In Gonzales v. Oregon, the Supreme
Court held that the CSA merely “bars doctors from . . . illicit drug dealing and trafficking as
conventionally understood,” but does not “regulate the practice of medicine generally.”
29
The regulation of medical practice is instead within the states’ police powers to provide for
their citizens’ health, safety, and welfare.
30
If SIFs are considered part of medical practice,
31
or if supervising injections is viewed as within providers’ existing authority,
32
SIFs may
succeed in a courtroom challenge under § 856. It is nevertheless difficult to predict how a
court would decide the question.
33
A broad reading of state and local law may also result in penalties for SIF staff and property
owners. If SIF clients commit state law felonies through possession or sale of drugs or
paraphernalia, SIF owners or staff may be engaging in “criminal facilitation”—“provid[ing] .
. . means or opportunity” to commit a crime.
34
If SIF owners are convicted of violating any
felony drug laws under N.Y. Penal Law § 220—which include the possession,
paraphernalia, sale, and injection laws outlined above—they may be subject under state
law to civil forfeiture of any property that is an “instrumentality of the crime,” including
real property.
35
Where the forfeiture is “disproportionate to the defendant’s gain from or
26
U.S. Const. art. VI, cl. 2.
27
See Burris et al., supra note 18, at 1120-45.
28
See Burris et al., supra note 18, at 1128 (quoting 21 U.S.C. § 801a(3))
29
Gonzales v. Oregon, 546 U.S. 243, 270 (2006) (striking down Attorney General’s interpretive rule that
would prohibit doctors from prescribing drugs for physician-assisted suicide, as permitted by Oregon state
law).
30
Id.
31
This may be increasingly true; see infra section II.C for the associations of medical professionals that have
endorsed SIF implementation or study in the United States.
32
Providers who are registered to prescribe controlled substances may do so “in the usual course of [their]
professional practice.” 21 C.F.R. § 1306.04 (2016); see also 21 U.S.C. § 822(b) (2017) (authorizing registered
providers to distribute controlled substances). If SIF activities can be considered part of usual medical
practice, there may be a claim that these activities are already authorized as a lesser entailment of
prescription authority, at least for registered providers.
33
Courts have divided on whether states may authorize the prescription of marijuana, although the Supreme
Court has found that federal CSA prosecutions of growers and users are still proper despite state laws. See
Preemption of State Regulation of Controlled Substances by Federal Controlled Substances Act, 60 A.L.R.6TH
175 (2010); Gonzales v. Raich, 545 U.S. 1 (2005).
34
N.Y. Penal Law § 115.00 (2017).
35
N.Y. Penal Law § 480.05 (2017).

135
participation in the offense,” however, the owner may only be required to forfeit “a
portion” of his or her property.
36
This is likely to be true of a SIF owner, for whom the loss
of property would greatly outweigh any personal gain from using the property as a SIF.
SIF staff and owners may also fall under an expansive reading of the state criminal
nuisance law, which penalizes persons who “knowingly . . . maintain any premises, place, or
resort where persons gather for purposes of engaging in unlawful conduct.”
37
Past cases
have upheld New York’s criminal nuisance law against individuals who knowingly allow
their homes to be used for smoking marijuana, noting that “knowledge coupled with
acquiescence” is sufficient for conviction.
38
A SIF could be found to meet these standards,
39
although prosecuting SIFs may not be a high priority for state prosecutors. Several
defenses under state law may also be persuasive.
40
The New York City code barring public
nuisances may also penalize SIFs, depending on the discretion of the city corporation
counsel.
41
Public nuisances include “any building, erection or place” where there is a
criminal nuisance as defined by state law,
42
or where there are three or more violations per
year of state drug laws (with the exception of simple possession) or the city’s synthetic
marijuana code.
43
Where a building violates these codes, counsel for the city may sue to
enjoin the nuisance, including requesting a permanent injunction to seize or close the
premises.
If health care providers at the SIF provide direct assistance with injecting or other modes of
consumption, additional provisions of the CSA may apply. Injecting drugs into a person, or
otherwise applying drugs to a person’s body, qualifies as “administering” controlled
36
Id.
37
N.Y. Penal Law § 240.45 (2017). New York has additional statutes defining public nuisances on other
grounds, including public health grounds. See, e.g., N.Y. Pub. Health Law § 2320 (2017) (defining public
nuisances to include buildings “used for the purpose of lewdness, assignation, or prostitution” ); N.Y. Pub.
Health Law § 1300 et seq. (2017) (giving local departments of public health authority to examine and order
the abatement of public nuisances that are detrimental to public health). In general, public nuisance claims
require plaintiffs to prove a substantial interference with a right that is common to the public, which offends
public morals, interferes with the use of a public place, or endangers or injures the property, health, safety, or
comfort of “a considerable number” of persons. See, e.g., 532 Madison Ave. Gourmet Foods, Inc. v. Finlandia
Ctr. Inc., 96 N.Y.2d 280 (N.Y. 2001). A state prosecutor or city counsel may sue to enjoin the operation of a SIF
on this basis, and the success of such a claim would depend on the court’s interpretation of these terms. This
would be a novel use of public nuisance law.
38
People v. Schriber, 310 N.Y.S. 2d 551 (N.Y. App. Div., 3d Dep’t 1970) (aff’d 29 N.Y.2d 780 (1971)).
39
Notably, however, if state law were to exempt SIF clients from most § 220 possession laws—as has been
done for syringe and residue possession by SEP clients, and for possession by individuals who witness
overdoses—the “unlawful conduct” element would no longer apply.
40
For example, a SIF may defend on the basis of justification due to medical necessity. Years before SEPs were
authorized by statute in New York, a group of early SEP implementers used this defense successfully against
hypodermic needle possession charges, on the grounds that the danger of HIV transmission outweighed the
legal harm of possession. People v. Bordowitz, 588 N.Y.S.2d 507 (N.Y. Crim. Ct. 1991). A similar defense may
be successful against state criminal law charges for a SIF.
41
New York City Administrative Code § 7-703 (2017).
42
Id., at § 7-703(l) (2017).
43
Id., at § 7-703(g) (2017).

136
substances under the CSA.
44
Section 841(a)(1) prohibits “dispens[ing]” a controlled
substance, with penalties including imprisonment and fines, and administering a client’s
drug through direct injection may qualify.
45
As discussed above, the New York state law
prohibiting injecting another person with drugs would also apply to SIF staff who inject
clients in need of injection assistance.
46
2. Civil Liability
In general, SIF staff and owners will be subject to the same statutory and common-law civil
liabilities as other health care facilities that serve the general public, such as hospitals,
clinics, or SEPs. Like staff and owners of all health care facilities, SIF personnel must use
ordinary care to provide a safe facility and to deliver non-negligent services, and they will
be liable in tort for negligence resulting in injury. This memorandum is not intended to
provide a comprehensive list of potential liabilities, but the nature of services provided at a
SIF raises several potentially novel questions.
The prior section described criminal nuisance law on the theory of public nuisance, as well
as the capacity for both state prosecutors and New York City counsel to make public
nuisance claims.
47
New York state law also allows tort suits by private parties alleging
nuisance claims. Private nuisance claims in New York face a fairly demanding and fact-
specific test—the claimant must show an interference with the use or enjoyment of land,
and the interference must be “substantial in nature,” intentional, unreasonable, and caused
by the defendant’s actions or failure to act.
48
Private parties who oppose a SIF may allege
that a SIF interferes with the use and enjoyment of surrounding property. These parties
would be required to show injuries that are “certain and substantial,” rather than “fanciful”
or speculative, and the reasonable person standard would apply.
49
In this instance, a SIF
may be analogous to a homeless shelter. Several prior actions have alleged that homeless
shelters, including a homeless shelter providing alcohol crisis services, are nuisances due
44
21 U.S.C. § 802(2) (defining “administer[ing]” as “the direct application of a controlled substance to the
body of a patient or research subject”); 21 U.S.C. § 10 (“‘dispense’ means to deliver a controlled substance to
an ultimate user or research subject . . . including the prescribing and administering of a controlled
substance”). “Administering” may thus bring SIF staff within the prohibition of § 841.
45
21 U.S.C. § 841 (2017).
46
N.Y. Penal Law § 220.46 (2017).
47
Private parties may bring public nuisance claims in New York, but they must show an injury that is
“different in kind” from that suffered by the general public, not merely different in degree. This is difficult to
satisfy. See, e.g., N.A.A.C.P. v. AcuSport, Inc., 271 F. Supp. 2d 435 (2003) (finding that the N.A.A.C.P. did not
allege an injury “different in kind” from the injury experienced by “the community at large” from the lax sales
and distribution practices of handgun manufacturers, importers, and distributors).
48
See, e.g., Copart Indus., Inc. v. Consolidated Edison Co. of New York, Inc., 41 N.Y.2d 564 (N.Y. 1977); Taggart
v. Constabile, 14 N.Y.S.3d 388 (N.Y. App. Div., 2d Dep’t 2015). If the nuisance is based on criminal conduct, it is
a nuisance per se, meaning that plaintiffs need not show that the interference is intentional or negligent. See
State v. Fermenta ASC Corp., 656 N.Y.S.2d 342 (N.Y. App. Div., 2d Dep’t 1997).
49
See Matteliano v. Skitkzi, 925 N.Y.S.2d 276 (N.Y. App. Div., 4th Dep’t 2011).

137
to the presence of “violent or unstable” clientele.
50
Courts have found that these facilities
are public necessities, that “apprehensions” alone do not support nuisance allegations
against them, and that the burdens these services impose on public rights are neither
substantial nor unreasonable.
51
Professionals who work at a SIF will be subject to the same medical malpractice standards
as health care professionals in other settings in New York: claimants must show a deviation
from accepted standards of practice, and that deviation must have proximately caused
injury.
52
New York legislation provides for “Good Samaritan” immunity from malpractice
claims for health care providers who respond to accidents or emergencies outside “the
normal and ordinary course” of practice, without expecting monetary compensation, in
locations other than places “having proper and necessary medical equipment,” with the
exception of claims arising from gross negligence.
53
Although overdoses in SIFs would
certainly qualify as accidents or emergencies, providers at a SIF likely will not qualify for
this reduced standard of liability. SIF services will be part of the ordinary course of these
providers’ practice, providers may work at SIFs for compensation, and SIFs are likely have
“proper and necessary medical equipment” to treat overdoses. Ordinary medical
malpractice standards will thus likely apply to the duties of SIF providers, even when
responding to overdoses.
Available reports reflect no record of a client dying on the premises of a SIF, despite the use
of SIFs in a number of countries. Should a SIF client die from an overdose, however, the
client’s decedents may seek to make a claim against SIF staff and owners for wrongful
death. These claims are structured by statute in New York, which allows a decedent’s
personal representatives to recover damages for wrongful death due to “a wrongful act,
neglect or default which caused the decedent’s death.”
54
Wrongful death actions may allege
simple negligence (i.e., negligence that is easily discerned by a jury without expert
testimony) or malpractice by health care personnel; claims alleging medical malpractice
will require expert testimony regarding standards of practice.
55
If SIF staff and owners
operate the facility with ordinary care, and if SIF professionals practice according to
accepted standards, plaintiffs in a wrongful death suit are unlikely to prevail.
56
SIFs are
50
See Spring-Gar Community Civic Ass’n, Inc., v. Homes for the Homeless, Inc., 516 N.Y.S.2d 399 (N.Y. Sup. Ct.,
Queens Cty., 1987); DeStefano v. Emergency Housing Group, Inc., 722 N.Y.S.2d 35 (N.Y. App. Div., 1st Dep’t
2001).
51
Spring-Gar, 516 N.Y.S.2d 399 (Sup. Ct., Queens Cty. 1987); DeStefano, 722 N.Y.S.2d 35 (N.Y. App. Div., 1st
Dep’t 2001). The practice of a church of allowing homeless persons to sleep outside on church property has
also been found not to be a public nuisance under New York law. Fifth Avenue Presbyterian Church v. City of
New York, 2004 WL 2471406 (S.D.N.Y. 2004).
52
Gillespie v. New York Hosp. Queens, 947 N.Y.S.2d 148 (N.Y. App. Div., 2d Dep’t 2012); Arkin v. Gittleson, 32
F.3d 658 (2d Cir. 1994) (applying New York law).
53
See N.Y. Educ. Law § 6527(2) (2017) (for physicians); N.Y. Educ. Law § 6909(1) (2017) (for nurses); N.Y.
Educ. Law § 6545 (2017) (for physician assistants).
54
N.Y. Estates, Powers & Trusts Law § 5-4.1 (2017)
55
See Coursen v. New York Hosp. Cornell Med. Ctr., 499 N.Y.S.2d 52 (N.Y. App. Div., 1st Dep’t 1986).
56
Defining the standard of care for SIF owners and staff may require looking to how SIFs are operated in
other countries, given that no SIF is yet in operation in the United States.

138
thus similar to other health care facilities providing emergency services—although death
on the premises is possible, non-negligent operation of the SIF will be a defense against
wrongful death claims.
A final and somewhat unique question for SIFs is the application of “dram shop” liability
and its analogues, which take effect when intoxicated or impaired persons cause injury or
death to third parties (e.g., by driving under the influence). In the case of intoxication due
to alcohol use, New York’s Dram Shop Act (N.Y. General Obligations Law § 11-101)
provides a cause of action for these injured individuals, who may bring suit against anyone
who, “by unlawful selling or unlawfully assisting in procuring liquor [,] . . . [has] caused or
contributed to such intoxication.”
57
The intoxicated person himself or herself may not bring
claims, although any dependents may sue for loss of “means of support” in the event of the
intoxicated person’s death.
58
A complementary statute in New York (§ 11-103) applies
when injury is inflicted by someone “impaired by the use of a controlled substance” other
than alcohol.
59
Injured persons may then recover damages from “any person who caused or
contributed to such impairment by unlawfully selling to or unlawfully assisting in
procuring a controlled substance for such person.”
60
If SIF clients leave the SIF in a state of impairment or intoxication and subsequently cause
harm, injured parties may seek to recover damages from the SIF under the dram shop laws.
These actions, however, are unlikely to succeed under current judicial interpretations of §§
11-101 and 11-103. Courts examining the action of “assisting” in § 11-101 have generally
required actions related to sale, such as contributing funds or actually purchasing alcohol
for someone’s consumption.
61
Nonsellers, social hosts, and companions of impaired or
intoxicated people are not liable under § 11-101.
62
Although courts interpreting § 11-103
have noted that money need not change hands for the transfer of a controlled substance
(e.g., marijuana) to constitute a “sale,”
63
SIFs will not be the source of substances used by
SIF clients. A physician who prescribes controlled substances has also been found not liable
57
N.Y. Gen. Oblig. Law 11-101 (2017).
58
See Searley v. Wegmans Food Markets, Inc., 807 N.Y.S.2d 768 (N.Y. App. Div., 4th Dep’t 2005).
59
N.Y. Gen. Oblig. Law 11-103 (2017).
60
Id.
61
See Bregartner v. Southland Corp., 683 N.Y.S.2d 286 (2d Dep’t 1999)
62
See Martino v. Stolzman, 902 N.Y.S.2d 731 (N.Y. App. Div., 4th Dep’t 2010) (finding that social hosts that
provided alcohol at a party had “no expectation of pecuniary gain,” and therefore were not liable under the
Dram Shop Act; this finding on Dram Shop Act liability was later affirmed by Martino v. Stolzman, 18 N.Y.3d
905 (N.Y. 2012)); Casselberry v. Dominick, 533 N.Y.S.2d 31 (N.Y. App. Div., 4th Dep’t 1988) (finding that a
union that provided beer to union members was not engaged in commercial sale and therefore not liable);
D’Amico v. Christie, 71 N.Y.2d 76 (N.Y. 1987) (finding that an employees’ association that provided beer
without charge at a picnic was not liable, as they had “no recognizable expectation of pecuniary gain”); French
v. Cliff’s Place Ltd., 508 N.Y.S.2d 577 (N.Y. App. Div., 2d Dep’t 1986) (finding that “drinking companions” are
not liable). If SIFs are legally authorized in New York, claims under § 11-101 and § 11-103 may also fail on the
“unlawful” element of the claim. See infra section II.A.
63
Terrigino v. Zaleski, 544 N.Y.S.2d 283 (Sup. Ct. 1989) (finding a cause of action against someone who
supplied marijuana to a driver who subsequently injured other drivers, even without receiving “something in
return” for the transfer).

139
under § 11-103, where the complaint does not allege that the physician has “the authority
or ability” to control the drug user, and where there is no other relationship between the
physician and the injured party.
64
SIFs will not have any involvement in the purchase or
sale of controlled substances, and because all clients will bring their own substances, SIFs
will have less of a direct connection to the substances than social hosts. Accordingly,
although any injured parties may seek to bring suit against a SIF under these laws, the
success of these claims is far from certain, and they would be a novel extension of the state
statutes.
C. Legal Challenges for Professionals at SIFs
Additional legal issues may arise for health care professionals who practice at SIFs. If
licensed nurses, physicians, or other allied health personnel who staff SIFs are held to
violate federal, state, or local laws—such as § 856 of the federal CSA, or N.Y. Penal Law §
240.45 on criminal nuisance—they may face professional penalties in New York. New York
state law regulates the practices of medicine, nursing, and other allied health professions.
Under the state’s general professional misconduct statute,
65
as well as the specific statute
governing misconduct for physicians and physician assistants,
66
conviction of a crime
under New York or federal law is misconduct per se, even when the crime is unrelated to
the profession. The case law on these offenses does not show any disciplinary proceedings
arising from involvement in harm reduction activities. The Office of Professional Medical
Conduct in the New York Department of Health handles disciplinary proceedings for
physicians and physician assistants, while the New York State Education Department Office
of the Professions addresses complaints arising in other professions, including nursing.
Without a criminal conviction, disciplinary proceedings for practice “beyond [the]
authorized scope” of the profession (for physicians) or “committing unprofessional
conduct” (for other professions) may be broad enough to encompass some SIF activities,
depending on whether the professional offices recognize harm reduction as part of medical
practice. To this end, the views of national and regional professional societies may be
instructive. In June 2017, the American Medical Association—the nation’s largest physician
group and publisher of JAMA—voted to endorse pilot SIF projects in the United States as a
promising strategy to diminish overdose deaths, to reduce infectious disease associated
with injection, and to advance access to treatment.
67
In its press release announcing this
position, the AMA noted that it also consulted the recent deliberations and findings of the
Massachusetts Medical Society—publisher of the preeminent New England Journal of
64
Ferguson v. Laffer, 53 N.Y.S.3d 89 (N.Y. App. Div., 2d Dep’t 2017).
65
N.Y. Educ. Law § 6509 (2017).
66
N.Y. Educ. Law § 6530 (2017).
67
American Medical Ass’n, AMA Wants New Approaches to Combat Synthetic and Injectable
Drugshttps://www.ama-assn.org/ama-wants-new-approaches-combat-synthetic-and-injectable-drugs.
Updated June 12, 2017.

140
Medicine—endorsing SIFs.
68
The American Public Health Association has called for study
and implementation of SIFs in the US,
69
and the Medical Society of the State of New York
has also advocated a comprehensive study.
70
Several other groups have not yet weighed in
specifically on SIFs, but have previously supported harm reduction strategies for
responding to substance use: the AMA, American Nurses Association, American Society of
Addiction Medicine, and APHA have encouraged SEPs for decades.
71
This history of
commitment to harm reduction and interest in SIFs suggests that a provider facing
professional discipline for involvement in a New York SIF may persuasively argue that SIF
services are part of ethical medical practice.
II. Legal Avenues for Establishing a SIF in New York City
In light of these legal challenges, states and cities may choose among several pathways for
implementing a SIF. Of course, the clearest avenue for establishing a legal SIF would be a
federal statute that authorizes SIF operation and provides SIF clients, staff, and owners
with exemptions from federal criminal laws. The following analysis, however, assumes that
there will be no change in federal law.
A. State Legislation
The New York State Legislature has the authority to authorize SIFs by statute, and could do
so either with a freestanding law, or with an extension to the current state law authorizing
SEPs.
72
The Tenth Amendment to the U.S. Constitution provides that any powers that are
not specifically delegated to the federal government are “reserved to the states,” giving
states broad authority to regulate for the health, safety, and welfare of their residents.
Known as the “police power,” this authority extends to “health laws of every
description”
73
—as long as those state laws are not preempted by a federal statute within
the federal government’s authority.
On June 21, 2017, Linda B. Rosenthal, a Manhattan representative in the 150-member New
York Assembly, introduced bill A.8534 (the “Safer Consumption Services Act”) to authorize
the establishment of SIFs statewide.
74
This bill would provide a new section of the state
public health law, which would allow local health departments to approve SIFs
68
Massachusetts Medical Society, Massachusetts Medical Society Expands Advocacy on Opioid Crisis,
http://www.massmed.org/News-and-Publications/MMS-News-Releases/Massachusetts-Medical-Society-
Expands-Advocacy-on-Opioid-Crisis/#.WTTrB-vytXQ. Updated on May 1, 2017,
69
Defining and Implementing a Public Health Response to Drug Use and Misuse. American Public Health
Association. Updated Nov 5 2013.
70
Medical Society of the State of New York, Supervised Injection Facilities, Resolution 2017-160 (2017).
71
Normand et al. eds. Preventing HIV Transmission: The Role of Sterile Needles and Bleach.. The National
Academies Press. 1995.
72
N.Y. Public Health Law § 3381 (2017).
73
Gibbons v. Ogden, 22 U.S. 1, 78 (1824)
74
A.8534, 2017-2018 Reg. Sess. (N.Y. 2017) (introduced June 21, 2017, in the Committee on Health), available
at
http://nyassembly.gov/leg/?default_fld=&leg_video=&bn=A08534&term=2017&Summary=Y&Actions=Y&Co
mmittee%26nbspVotes=Y&Floor%26nbspVotes=Y&Memo=Y&Text=Y.

141
implemented by community-based organizations, hospitals, medical clinics or offices,
health centers, nursing care facilities, mental health facilities or “other similar entit[ies]
that provid[e] medical care.” The legislation permits local departments of health to set
standards for program approval and training, and it sets forth required program activities
and reporting requirements. All programs would also be designated as SEPs, and the
statute specifically provides that SIF clients, staff, and owners will be immune from arrest,
criminal charges, prosecution, and civil or administrative penalties (including civil
forfeiture and professional licensing sanctions) associated with “participation or
involvement” in an approved SIF. Immunity would not extend to activities “not permitted
or approved” under the SIF implementing legislation. The bill is currently under
consideration in the Committee on Health.
In addition to New York, several other states have considered legislation either authorizing
or prohibiting SIFs, including California,
75
Maryland,
76
Maine,
77
Massachusetts,
78
and
Washington (to prevent SIFs, as a response to a local Board of Health decision to establish
to SIFs in Seattle),
79
as of now, no bill has yet passed both houses of a state legislature. As of
June 2, 2017, the California State Assembly passed AB-186, which would authorize SIFs for
a period of five years in several state counties, including Alameda, Fresno, Humboldt, Los
Angeles, Mendocino, San Francisco, San Joaquin, and Santa Cruz.
80
The statute provides for
required program services, the development of operating procedures and policies to
address neighborhood concerns, and immunity from arrest, charge, or prosecution from
specific drug laws.
81
The bill is currently in committee in the state Senate Committees on
Health and Public Safety.
There are several advantages to establishing a SIF by state statute in New York. Any
legislation authorizing a SIF could simultaneously amend or provide exemptions from state
laws on possession, paraphernalia, criminal injection, criminal nuisance, and professional
misconduct to protect SIF staff, owners, and clients from arrest, prosecution and
disciplinary proceedings in the state. Even if the statute and implementing regulations do
not explicitly amend these criminal laws, statutory support for a SIF may deter arrest and
provide persuasive defenses for SIF clients, personnel, and owners faced with unexpected
75
AB-186, 2017-2018 Reg. Sess. (Cal. 2017) (passed the House as of June 2017).
76
H.B. 519, 2017 Reg. Sess. (Md. 2017) (in the House as of June 2017).
77
L.D. 1375, 128th Legisl. (Me. 2017) (rejected in the House and Senate as of June 2017).
78
S.1081, 190th Gen. Court. (Mass. 2017) (in the Joint Committee on Mental Health, Substance Use and
Recovery as of June 2017).
79
S.B. 5223, 2017-18 Sess. (Wash. 2017) (passed the Senate, referred by the House back to the Senate Rules
Committee as of June 2017).
80
Like many other U.S. cities considering SIF implementation, the San Francisco Department of Public Health
currently has a task force considering the feasibility of a local SIF. San Francisco Department of Public Health,
Safe Injection Services Task Force, https://www.sfdph.org/dph/comupg/knowlcol/SISTaskForce/ (last
visited June 30, 2017).
81
Assembly Bill 186, January 19, 2017.

142
criminal charges.
82
Statutory authorization under state law could also provide some
protection from local efforts to declare SIFs a public nuisance, or to find SIF clients in
violation of local laws such as Administrative Code § 10-203.
Although this pathway provides the greatest legal certainty with respect to state and local
law, it may not safeguard SIFs against federal efforts to enforce the CSA.
83
States have
authority to enact laws that appear to present conflicts with the CSA, as evidenced by laws
enabling SEPs, medical marijuana, legalization of recreational marijuana, and physician aid
in dying.
84
Questions remain, however, about how a state law establishing SIFs would fare
in a federal preemption challenge, or whether state law protections would insulate SIF
personnel in a federal prosecution under the CSA.
85
Under any legal pathway with the
current CSA, the operation of a SIF would depend on the discretion of federal prosecutors
and the reasoning of courts that would hear these challenges.
B. State Administrative Action
In the absence of state legislation, a state agency or the state governor could also establish
a SIF through executive authority. New York Public Health Law § 201 accords the state
Department of Health the authority to “promote or provide diagnostic and therapeutic
services for . . . communicable disease, medical rehabilitation . . . and other conditions and
diseases affecting public health;”
86
the department may also “receive and expend funds
made available for public health purposes pursuant to law.”
87
The commissioner of the
state Department of Health may authorize people to obtain and possess hypodermic
needles to enable the operation of SEPs.
88
The state governor has executive power to “take
care that the laws are faithfully executed,” and may issue executive orders within state
constitutional limits.
89
The governor may also declare a state of disaster in response to
“natural or man-made causes” that threaten “wide spread or severe damage, loss of life or
82
See Roe v. City of New York, 232 F. Supp. 2d 240 (S.D.N.Y. 2002) (finding an exception to the law
criminalizing possession of trace amounts of drug in syringes, as applied to clients of legally authorized SEPs).
83
See Burris et al., supra note 18, at 1112.
84
See id., at 1107. Some states have taken these actions directly through citizen ballot referenda, but New
York State law does not provide for direct referendum or initiative options for new legislation.
85
See id.; see also Leo Beletsky et al., The Law (and Politics) of Safe Injection Facilities in the United States, 98
AM. J. PUB. HEALTH 231 (2008). Congress has included language in several consecutive budget appropriations
to prevent the Department of Justice from spending federal funds to prosecute activities that are completely
authorized by state laws providing for medical marijuana use. See, e.g., Consolidated Appropriations Act 2016,
Pub. L. No. 114-113, § 542, 129 Stat. 2242, 2332-33 (2015); U.S. v. McIntosh, 833 F.3d 1163 (9th Cir. 2016).
SIFs lack this protection at present, but Congress could choose to enact parallel language to insulate state-
authorized SIF activities from federal prosecution under the CSA.
86
N.Y. Public Health Law § 201(1)(h) (2017).
87
N.Y. Public Health Law § 201(1)(p) (2017).
88
N.Y. Public Health Law §§ 3381(1)(b), 3381(4) (2017).
89
N.Y. Const., art. IV § 3.

143
property,”
90
and where local governments are unable to respond adequately.
91
Where there
is a disaster, the governor may direct state agencies to assist in a response.
92
The state Department of Health or governor could seek to establish a SIF through one of
these avenues, such as direct service provision and funding by the department,
authorization by the commissioner, executive order, or a governor’s declaration of disaster.
Any of these executive or agency actions, however, may be challenged as contrary to state
criminal laws, assuming that these laws remain unchanged. In 2004, the governor of New
Jersey authorized SEPs by executive order, citing the threat of HIV and hepatitis C
transmission. A group of state senators challenged the order as exceeding the governor’s
executive authority,
93
and an advisory opinion by the New Jersey State Legislature Office of
Legislative Services supported the senators’ position.
94
It is unclear how state lawmakers
and prosecutors would respond to a similar effort in New York State.
Although perhaps preferable to local authorization of a SIF, establishing a SIF through a
state agency or the governor’s authorization will leave substantial legal uncertainty about
conflicts with the federal CSA, state prosecution under state criminal laws, challenges from
state legislators citing separation-of-powers concerns (as in New Jersey), and professional
discipline for SIF providers. These issues are matters of prosecutorial discretion and/or
courts’ reasoning. A SIF established on this basis may prevail in court, or it may go
unchallenged; if so, the program may be durable despite the lack of supportive state
statutes.
95
C. Local Legislation or Administrative Action
New York City also has the authority to establish SIF services through a city ordinance. The
New York State Constitution
96
and New York Municipal Home Rule Law
97
allow cities to
“enact and amend local laws” for the “safety, health, and well-being” of their residents,
provided that city ordinances are not inconsistent with state laws. Like the state
legislature, New York City could exercise this power to authorize SIFs under city law. A SIF
established by city ordinance may be vulnerable, however, to challenge by state
prosecutors enforcing state criminal law, such as N.Y. Penal Code § 220.03 (possession) or
§ 240.45 (criminal nuisance). SIF providers may also remain uncertain about professional
90
N.Y. Exec. Law § 20 (2017).
91
N.Y. Exec. Law § 28 (2017).
92
N.Y. Exec. Law § 29 (2017).
93
State v. City of Atlantic City, 379 N.J. Super. 515, n.1 (N.J. Super. Ct. App. Div. 2005); Playing AIDS Games in
New Jersey, THE N.Y. TIMES, June 30, 2005.
94
See Letter from Albert Porroni & Pamela H. Espenshade, New Jersey State Legislature, Office of Legislative
Services, to Joseph Pennachio, Assemblyman, New Jersey, Nov. 15, 2004, available at
http://njlegallib.rutgers.edu/ols/ols20041115.html. See also Beletsky et al., supra note 85, at 233.
95
See Burris et al., supra note 18, at 111.
96
N.Y. Constitution, art. IX § 2(c)(10) (“[E]very local government shall have power to adopt and amend local
laws not inconsistent with the provisions of this constitution or any general law relating to . . . the
government, protection, order, conduct, safety, health and well-being of persons or property therein.”).
97
New York Municipal Home Rule Law § 10(1)(ii)(a)(12) (2017) (similar language as above).

144
disciplinary proceedings, and local endorsement of a SIF may be less persuasive than a
state statute for disciplinary purposes.
If state prosecutors choose to oppose a locally authorized SIF, a New York court could find
a city ordinance or agency action authorizing SIFs to be inconsistent with state criminal
laws. The case of SEPs in Atlantic City provides an instructive example; after state
legislative efforts to authorize SEPs stalled, the city established a SEP under local law to
address the local hepatitis C and HIV epidemic.
98
A state court subsequently struck down
the ordinance as inconsistent with state criminal laws, citing the failure of state-level SEP
bills as additional evidence of inconsistency.
99
New York may be distinguished from this
case, as the state does not have adverse precedent in the legislature rejecting SIFs.
100
Moreover, prosecution would remain a matter of state prosecutorial discretion. Cities in
other states have implemented SEPs successfully without state-level prosecution, including
cities in Pennsylvania, Ohio, and California.
101
Action by a city agency or city executive branch is another pathway by which New York
City could establish a SIF. Pursuant to the New York City Charter § 556, the New York
Department of Health and Mental Hygiene is empowered “to regulate all matters affecting
health in the city of New York and to perform all those functions and operations performed
by the city that relate to the health of people of the city, including . . . substance abuse-
related needs of the people of the city.”
102
This authority also entails the power to
“maintain and operate public health centers and clinics,” to “promote or provide for
programs for the prevention and control of disease,” to “provide or promote diagnostic and
therapeutic services for . . . communicable disease, medical rehabilitation, and other
diseases and conditions affecting public health,” and to “promote or provide medical and
health services for . . . the ambulant sick and needy persons of the city.”
103
The Board of
Health, as part of the department, may also amend the City Health Code.
104
City agencies
may adopt rules without notice and comment on a temporary basis if “necessary to address
an imminent threat to health,” but such rules may remain in effect for only 60 days.
105
Local
chief executives—here, the city mayor—also have authority to declare a local state of
emergency and to enact ordinances pursuant to that authority, but this power lasts only 30
days.
106
98
State v. City of Atlantic City, 379 N.J. Super. 515 (N.J. Super. Ct. App. Div. 2005); Beletsky et al., supra note
85, at 233.
99
City of Atlantic City, 379 N.J. Super., at 526.
100
The state legislature has yet to consider bill A. 8534, which was recently introduced. Moreover, unlike in
the state of Washington, there has been no legislative effort to prohibit SIFs in New York. See supra note 79.
101
Beletsky et al., supra note 85, at 233.
102
New York City Charter § 556.
103
New York City Charter § 556(d).
104
New York City Charter § 558(b)-(c).
105
New York City Charter § 1043(h).
106
N.Y. Exec. Law § 24 (2017).

145
The New York City Department of Health and Mental Hygiene could use these powers to
implement a SIF, as could the city mayor. But like local legislative efforts, these executive
and agency actions may draw challenges under state law, depending on state prosecutors’
enforcement decisions. Like New York City, other cities including Baltimore, Philadelphia,
and San Francisco are using local authority to study SIFs, and a few cities have publicized
intentions or decisions to implement SIFs. The King County Board of Health in Seattle has
voted to establish two SIFs, and although they have not been challenged by state
prosecutors, a state legislative effort to block SIFs statewide is ongoing.
107
Ithaca, NY, has
publicized the “Ithaca Plan” approach to address drug overdoses, which includes
establishing a SIF, but the plan has not yet taken effect.
108
D. State or Local Pilot Research Study with Federal and State Authorization
A final avenue for establishing a SIF is to run the program as a research study, with the
research goal of pilot-testing the acceptability and feasibility of a SIF in New York City.
There are established legal procedures for conducting research that involves the use of
controlled substances, which insulate researchers and participants from prosecution under
federal and state drug laws. The New York City Charter grants the city Department of
Mental Health and Hygiene the authority to “engage in or promote health research for the
purpose of improving the quality of medical and health care.”
109
New York Public Health
Law § 201 grants the state Department of Health similar research authority.
110
This
suggests that either department could establish a SIF on a research basis, or could contract
out to a local institution to implement the pilot program.
In order to operate a SIF program on a research basis, researchers must first obtain
institutional review board (IRB) approval for conducting human subjects research with SIF
clients as participants.
111
They would then apply for a research license under New York
State law, pursuant to N.Y. Public Health § 3324, to carry out “scientific research” with
controlled substances.
112
The commissioner of the New York State Department of Health
has statutory authority to issue these licenses for a period of two years,
113
and they are
managed by the Department of Health Bureau of Narcotic Enforcement.
114
After obtaining
the state license, researchers must then apply for a federal license to gain an exemption
from the federal CSA.
115
Registrations are reviewed by the U.S. Department of Justice Drug
107
See supra note 79 and accompanying text.
108
See GWEN WILKINSON & LILLIAN FAN, MUNICIPAL DRUG POLICY COMMITTEE, THE ITHACA PLAN (2016).
109
New York City Charter § 556(d)(2).
110
N.Y. Public Health Law § 201(1)(d) (2017).
111
45 C.F.R. § 46 (2017); see also N.Y. Public Health Law § 2444 (2017).
112
N.Y. Public Health § 3324 (2017).
113
Id.
114
New York State Department of Health, Dear Researcher Licensee Letter, available at
https://www.health.ny.gov/professionals/narcotic/licensing_and_certification/2008-08-
01_controlled_substance_license.htm. Aug. 1, 2008.
115
21 U.S.C. § 822(b) (2017).

146
Enforcement Agency (DEA), and the DEA will require proof of the state registration before
issuing the federal license.
Federal protocol review and approval will depend on the priorities of the Drug
Enforcement Agency and the Attorney General. The Attorney General has authority to
promulgate rules regarding registration, including research licenses.
116
By statute, the AG
considers at least five factors in granting research licenses: (1) recommendation by the
state licensing board, (2) the researchers’ experience in research with controlled
substances, (3) researchers’ conviction records under federal and state controlled
substance laws, (4) compliance with “applicable state, federal or local laws,” and (5) threats
to public health and safety.
117
Controls against the potential diversion of drugs “from
legitimate medical or scientific use” may also be part of the review.
118
The protocol for a SIF
will likely differ from the typical research protocol for the study of controlled substances.
Unlike research studies that supply controlled substances for research participants, a SIF
protocol would permit participants to bring their own (sometimes unknown) substances
for use on site. Controls against diversion may be inapposite for a protocol that aims to
measure the harm-reduction benefits of a SIF for recreational drug use. Approval of a
research exemption would be at the discretion of the state Department of Health and
federal Attorney General.
Implementing a SIF as a pilot research study has several advantages, and this was the initial
means by which Vancouver, Canada and Sydney, Australia first established local SIFs. By
opening a SIF with both federal and state licenses, SIF staff and owners would have some
certainty that they are not violating federal or state laws. The experimental period may
help the SIF gain public support, which may bolster subsequent state legislative or agency
efforts to establish a SIF for service, rather than research purposes. The New South Wales
Parliament, for example, legislatively authorized the Sydney SIF to continue in operation
after a nine-year trial period.
119
The drawbacks of establishing a SIF for research include
the uncertainty of success in licensing at both federal and state levels, the need for
reapproval and continued adherence to research protocol over time (at least every two
years for state authorization), concerns about sustainability, and the potential for drug
inventory recordkeeping requirements if the Attorney General does not waive them for a
116
21 U.S.C. § 821 (2017).
117
21 U.S.C. § 823(f) (2017).
118
Id.
119
Uniting, The MISC Story, https://uniting.org/who-we-help/for-adults/sydney-medically-supervised-
injecting-centre/our-story (last visited June 4, 2017). The first Vancouver SIF, Insite, operated as a pilot
program with an exemption from federal and provincial drug laws from 2003 through 2007. Insite’s
operators then sued the Canadian Attorney General, asking British Columbia courts to declare that attempts
to close the site violated clients’ rights to life, liberty, and security of the person, under the Canadian Charter
of Rights and Freedoms. Insite succeeded in this claim before the Supreme Court of Canada in 2011, and now
operates as a service rather than a pilot project. See PHS, The History of Insite,
https://www.phs.ca/index.php/project/the-history-of-insite/ (last visited June 4, 2017); Canada v. PHS
Community Services Soc’y, [2011] S.C.R. 3 (Can.).

147
protocol of this type.
120
There may also be disadvantages to delivering services in the
context of a researcher-subject relationship rather than a provider-client relationship.
Additionally, operating a SIF through a research protocol may require the creation and
storage of more identifiable information about individual clients, which could limit
program usage by clients who wish to stay anonymous.
III. Conclusions
As prior analyses have suggested,
121
U.S. jurisdictions—including New York State and New
York City—have legal authority to establish a SIF through several different pathways.
Assuming that federal laws do not change, enacting a SIF through state legislation provides
greatest legal certainty on a long-term basis for SIF clients, staff, and property owners, at
least with respect to state criminal law and professional licensure. (Creating a SIF through
a research waiver would provide greater legal certainty on a short-term basis, if the state
and federal research licenses were granted. A research SIF, however, would end with the
conclusion of the pilot or the expiration of either license.)
Although state legislative authorization may provide greatest certainty for a New York City
SIF, this pathway nonetheless leaves open questions about the federal response under the
Controlled Substances Act, particularly 21 U.S.C. § 856 (the “Crack House” statute). Legal
challenges to a SIF on the basis of the CSA will depend on enforcement priorities and
prosecutorial discretion. Federal Attorney General involvement (or forbearance) will
therefore matter for implementing a SIF by any pathway, including state legislation, state
administrative action, local ordinance or administrative action, or a research exemption to
federal and state laws.
120
See, e.g., 21 U.S.C. § 827 (2017).
121
See Beletsky et al., supra note 85; Burris et al., supra note 18.
