
Frequently Asked Question's (FAQ's)
WHAT IS THIS PLAN ALL ABOUT
HDFC ERGO Sampoorna Suraksha is a one-stop shop for a multitude of insurance requirements. It offers policy buyers complete protection for a varied
range of services, including Health, Home, Travel and Cyber Security.
HDFC ERGO General Insurance Company Limited
This document is a summary of the benefits offered. The information mentioned above is illustrative and not exhaustive. Information must be read in conjunction with the policy wordings.
In case of any conflict between this document and the policy wordings, the terms and conditions mentioned in the policy wordings shall prevail.
Convenience at your fingertips
On the HELP section of our website, you can:
`
Get Policy Copy/
80D Tax Certificate
Make Changes on Policy
Track Claim Status
Update Contact Details
Ver.OCT19
my:health Mobile App
▪ Health Calculators
Features:
▪ Vaccination
▪ Blood Donations
▪ Physical Activities
▪ Reliable offers, discounts on services and consultation
▪ Complete data security
▪ Cashless OPD and reimbursement
▪ Improved interactions
Download the App now
WHAT ARE THE CHECKS TO BE DONE AFTER
RECEIVING THE POLICY?
¡ Correspondence Address (House number, Street name, Locality,
Check the correctness and completeness of below points in the
policy schedule:
¡ Insured’s Name or Proposer’s Name (Salutation, Gender, Spelling)
¡ Policy Period
¡ Coverage or Sum Insured Details
Pincode, City, Village, Landmark, etc.)
¡ Date of Birth of insured
¡ Mobile Number, Landline Number and Personal E-mail ID
WOULD I RECEIVE ANY CONFIRMATION ON THE CHANGES DONE IN MY POLICY?
You would receive an endorsed policy schedule reflecting the changes made in the policy details on your correspondence address as per policy. Same
would be captured in the policy under the section “List of endorsements”.
HOW DO I RENEW MY POLICY?
§ Visit our nearest branch or contact your agent
You can renew your policy through any of the below options:
§ Visit our website www.hdfcergo.com and go to the Instant Renewal section
§ Give us a missed call on 1800 315 7272 and get quick assistance from Renewal expert
§ Call us on 022 6234 6234 / 0120 6234 6234 and renew instantly
§ Courier the Cheque / Demand Draft in favour of “HDFC ERGO General Insurance Company Ltd” to our Customer service office
HOW TO CONTACT US?
HOW TO TRACK MY CLAIM STATUS?
You can track your claim status through any of the options below:
¡ Visit our website www.hdfcergo.com - > Help - > Track your claim section
¡ Download mobile app, link your policy and track real time status
¡ Visit Mobile App (IPO): Login into online insurance portfolio organizer (IPO) on the home page of our website www.hdfcergo.com
Kindly mention your claim number and/or policy/reference number in the correspondence
DO I GET INCOME TAX BENEFIT?
Yes, you can avail a Tax benefit under Section 80D of Income Tax Act 1961 (Subject to change in Income Tax law). Tax certificate is provided along with the
policy copy. You can mail the same on your registered Email Id through Insurance Portfolio Organiser , online .
WHAT IS THE CLAIM PROCEDURES?
1. DETAILS TO KEEP HANDY WHILE REGISTERING A CLAIM
¡ Policy Number
¡ Nature of disease/illness
¡ Brief history of diagnosis (first diagnosis date is mandatory)
2. HOW DO I FILE MY CLAIM?
¡ For Reimbursement claim intimation, customer should visit
www.hdfcergo.com > Help > Claim registration OR Send duly
signed claim form along with required documents to below address
HDFC ERGO General Insurance company Ltd, 5th floor, Tower 1,
Stellar IT Park, C-25, Sector-62, Noida, UP, India - 201301.
¡ For preauth claim write to us [email protected]
3. WHAT ARE THE BASIC DOCUMENTS REQUIRED IN CASE OF
A CLAIM?
¡ Duly filled and signed claim form (available on our website)
¡ Copy of Photo ID proof of insured and claimant
¡ Discharge card and original discharge summary
¡ Consultation note/ Relevant treatment papers
¡ All relevant medical reports along with supporting invoices and
doctors requisition advising the same
¡ Original and final hositalisation bills with detailed breakup
¡ Pharmacy bills along with prescriptions
Please note: This is not an exhaustive list. Additional docs may be
required on case to case basis.
For claim /Policy Related please calls us at 022 6234 6234 /0120 6234 6234 or Visit the Help Section on www.hdfcergo.com

1
HDFC ERGO General Insurance Company Limited
Policy Wordings
Sampoorna Suraksha
Insuring Clause
In consideration of payment of Premium by You and realized by Us, We
will provide insurance cover to the Insured Person(s) under this Policy
up to Sum Insured or limits mentioned on the Schedule of Coverage
in the Policy Schedule.
This Policy is subject to Your statements in respect of all the Insured
Persons in Proposal form, declaration and/or medical reports, payment
of premium and the terms and conditions of this Policy.
Denitions
Certain words used in the Coverage description have specic meanings
which are mentioned in Denitions and which impacts the Coverage. All
such words, where ever mentioned in this document are mentioned in
Bold to enable you to identify that particular word has a specic meaning
for which You need to refer Section II, Denitions.
I. Coverage
SECTION 1: MY:HEALTH SURAKSHA
Section I 1A: Hospitalization Cover
We will pay under below listed Covers On Medically Necessary
Hospitalization of an Insured Person due to Illness or Injury sustained
or contracted during the Policy Period. The payment is subject to Sum
Insured and limits including Cumulative Bonus if applicable as specied
on the Schedule of Coverage in the Policy Schedule. Subject to otherwise
terms and conditions of the Policy.
1. Medical Expenses
i. Room rent, boarding and Nursing charges
ii. Intensive Care Unit charges
iii. Consultation fees
iv. Anesthesia, blood, oxygen, operation theatre charges, surgical
appliances
v. Medicines, drugs and consumables
vi. Diagnostic procedures
vii. The Cost of prosthetic and other devices or equipment if implanted
internally during a Surgical Procedure.
Insured Person shall bear specied percentage of admissible Claim
amount under each and every Claim If Co-payment under Section
I1C-14 is opted and specied in the Schedule of Coverage in the
Policy Schedule
a) Mental Healthcare
If an Insured Person is hospitalized for any Mental Illness contracted
during the Policy period We will pay Medical Expenses under Section
I1 A in accordance with The Mental Health Care Act, 2017,subsequent
amendments and other applicable laws and Rules provided that;
i. The Hospitalization is prescribed by a Medical Practitioner for
Mental Illness
ii. The Hospitalization is done in Mental Health Establishment
2. Home Healthcare
Insured Person can avail Hospitalization at home under Home
Healthcare for Illnesses including but not limited to following Medically
Necessary Treatment, if prescribed by treating Medical Practitioner.
We will pay Medical Expenses under Section I1A-1 incurred for
treatment of such Illness where opted.
• Gastroenteritis
• Bronchopneumonia
• Respiratory tract infection
• Chemotherapy
• Pancreatitis
• Dengue
• COPD management
• Hepatitis
• Fever management
This Cover can be availed through Cashless Facility only as procedure
given under Claims Procedure - Section IV1.
Insured Person shall bear specied percentage of admissible Claim
amount under each and every Claim If Co-payment under Section I1
C-14 is opted and specied in the Schedule of Coverage in the Policy
Schedule
3. Domiciliary Hospitalization
We will pay the Medical Expenses incurred on Domiciliary
Hospitalization of the Insured Person provided that:
i. It has been prescribed by the treating Medical Practitioner
and
ii. the condition the Insured Person is such that he/she could not be
removed to a Hospital
or
iii. the Medical Necessary Treatment is taken at Home on account of
non-availability of room in Hospital
Expenses incurred on Domiciliary Hospitalization in respect to following
treatment are excluded under the Policy
a. Asthma, Bronchitis, Tonsillitis and Upper Respiratory Tract infection
including Laryngitis and Pharyngitis, Cough and Cold, Inuenza
b. Arthritis, Gout and Rheumatism
c. Chronic Nephritis and Nephritic Syndrome
d. Diarrhoea and all type of Dysenteries including Gastroenteritis,
e. Diabetes Mellitus and Insipidus,
f. Epilepsy,
g. Hypertension,
h. Psychiatric or Psychosomatic Disorders of all kinds,
i. Pyrexia of unknown Origin.
j. Post Hospitalization Expenses are excluded if Insured Person opts
for Domiciliary Hospitalization
Insured Person shall bear specied percentage of admissible Claim
amount under each and every ClaimIf Co-payment under Section I1C-14
is opted and specied in the Schedule of Coverage in the Policy Schedule
4. Pre-Hospitalization cover
We will pay for the Medical Expenses incurred during the 60 days
immediately before Hospitalization of an Insured Person, provided
that such Medical Expenses are incurred for the same Illness/Injury
for which subsequent Hospitalization was required and Claim under
Section I1A-1 or 1A- 6 is admissible under the Policy.
Where Insured Person has opted for Home Healthcare treatment under
Section I1 A-2, Pre-Hospitalization expenses are payable up to 60 days
prior to start of the Medical treatment.
Insured Person shall bear specied percentage of admissible Claim
amount under each and every Claim If Co-payment under Section

2
I1C-14 is opted and specied in the Schedule of Coverage in the
Policy Schedule
5. Post-Hospitalization cover
We will pay for the Medical Expenses incurred upto180 days from the
date Insured Person is discharged from Hospital provided that such
costs are incurred in respect of the same Illness/Injury for which the
earlier Hospitalization was required and Claim under Section I1A-1 or
1A6 is admissibleunder the Policy
Where Insured Person has opted for Home Healthcare treatment under
Section I1A-2, Post Hospitalization expenses are payable up to 180
days post completion of the medical treatment.
Insured Person shall bear specied percentage of admissible Claim
amount under each and every ClaimIf Co-payment under Section I1
C-14 is opted and specied in the Schedule of Coverage in the Policy
Schedule
6. Day Care Procedures
We will pay for the Medical Expenses under Section I1A-1 on
Hospitalization of Insured Person in Hospital or Day Care
CentreforDay Care Treatment.
Indicative list of Day Care Treatment is attached in Annexure I
Insured Person shall bear specied percentage of admissible Claim
amount under each and every ClaimIf Co-payment under Section I1
C-14 is opted and specied in the Schedule of Coverage in the Policy
Schedule
7. Road Ambulance
We will pay for expenses incurred on Road Ambulance Services if
Insured Person is required;
i. to be transferred to the nearest Hospital following an emergency
(namely a sudden, urgent, unexpected occurrence or event, bodily
alteration or occasion requiring immediate medical attention)
ii. or from one Hospital to another Hospital
iii. of from Hospital to Home (within same City) following Hospitalization
provided that Claim under Section I1 A1 and I1 A6 is admissible under
the Policy.
Insured Person shall bear specied percentage of admissible Claim
amount under each and every ClaimIf Co-payment under Section I1C-14
is opted and specied in the Schedule of Coverage in the Policy Schedule
8. Organ Donor Expenses
We will pay Medical Expenses as listed under Section I1A-1 towards
organ donor’s Hospitalization for harvesting of the donated organ where
an Insured Person is the recipient, provided that;
i. The organ donor is any person whose organ has been made available
in accordance and in compliance with The Transplantation of Human
Organ (amendment) Act, 2011,Transplantation of Human Organs and
Tissues Rules, 2014and other applicable laws and rules.
ii. Hospitalization Claim under Section I1 A-1 is admissible under
the Policy
iii. The Organ Donor’s Pre-Hospitalization and Post-Hospitalization
expenses are excluded under the Policy
iv. Any other Medical Expenses or Hospitalization consequent to the
harvesting is excluded under the Policy
Insured Person shall bear specied percentage of admissible Claim
amount under each and every ClaimIf Co-payment under Section I1
C-14 is opted and specied in the Schedule of Coverage in the Policy
Schedule
9. Alternative Treatments
We will pay Medical Expensesas listed under Section I1 A-1
on Hospitalization of Insured Person for following Alternative
Treatments prescribed by Medical Practitioner
• Ayurvedic
• Unani
• Siddha
• Homeopathy
provided that;
i. The procedure performed on the Insured Person cannot be carried
out on Outpatient basis
ii. The treatment has been undertaken in a government Hospital or in
any institute recognized by government and/or accredited by Quality
Council of India/National Accreditation Board on Health or authorised
medical council of the respective country/state as applicable
iii. In the event of admissible Claim under this Cover, no Claim shall
be admissible under SectionI1 A -1 for Allopathic treatment of same
Illness or Injury
Insured Person shall bear specied percentage of admissible Claim
amount under each and every ClaimIf Co-payment under Section I1
C-14 is opted and specied in the Schedule of Coverage in the Policy
Schedule
Section I 1 B: Renewal Benets
1. Preventive Health Check-Up
After every block ofevery four consecutive, continuous and Claim free
Policy Years with Us, We will pay towards cost of Preventive Health
Check- upto specied percentage (as mentioned on the Schedule of
Coverage) of Sum Insuredfor those Insured Persons who were Insured
under the previous 4 Policy years with Us.
Other terms and Conditions applicable to this Benet
• This benet will not be carried forward if not utilized.
• Eligibility to avail Health Check-up will be in accordance to lower of
expiring Policy Sum Insured or Renewed Policy Sum Insured.
• This cover is applicable only to Insured Person covered under all four
Policy Years and who continue to remain insured in the subsequent
Policy Year/Renewal.
• Availing of Claim under this Cover will not impact the Sum Insured or
the eligibility for Cumulative Bonus
2. Cumulative Bonus
On each Renewal of the Policy with Us, We will apply 5% of Basic
Sum Insured under expiring Policy as Cumulative Bonus in the Policy
provided that;
i. There has been no claim under the Policy in expiring year under
Section I1 A
ii. Cumulative Bonus will be reduced at the same rate as accrued in the
event of admissible Claim under Section I1 A of the Policy.
iii. Cumulative Bonus can be accumulated upto 50% of Basic Sum
Insured.
iv. Cumulative Bonus applied will be applicable only to Insured
Person covered under expiring Policy and who continue to remain
insured on Renewal.
v. In case of multiyear policies, Cumulative Bonus that has accrued
for the second and third Policy Year will be credited on Renewal.
Accrued Cumulative Bonus may be utilized in case of any Claim
during Policy tenure
3. my: Health Active
A. Fitness discount @ Renewal
Insured Person can avail discount on Renewal Premium by accumulating
Healthy Weeks as per table given below.
One Healthy Week can be accumulated by;
• Recording minimum 50,000 steps in a week subject to maximum 15,000
steps per day, tracked through Your wearable device linked to Our my:
health mobile app and Your Policy number
OR
• burning total of 900 calories upto maximum of 300 calories in one
exercise session per day, tracked Your wearable device linked to Our
my: health mobile app and Your Policy number
• Fitness discount @ Renewal is applicable for Adult Insured Persons
only. Any Person covered as Child Dependent, irrespective of the Age
is excluded.

3
Healthy Weeks Discounts
No. of Healthy Weeks
Accumulated
Discount on Renewal
Premium
1-4 0.50%
5-8 1.00%
9-12 2.00%
13-16 3.00%
17-26 6.00%
27-36 7.50%
Above 36 10.00%
Steps to accumulate Healthy Weeks
Step 1 - The my: Health mobile App must be downloaded on the mobile.
Step 2 - You can start accumulating Healthy Weeks by tracking physical
activity trough the Wearable device linked to Our my: health mobile
app and Your Policy number
We encourage and recognize all types of exercise/tness activities
by making use of wearable devices to track and record the activities
Insured Person engages in.
Application of Fitness discount @ Renewal
• Annual Policy: Discount amount accrued based on Number of
accumulated Healthy Weeks during the expiring PolicyYear will be
applied on the Renewal Premium for expiring Policy Sum Insured and
for Insured Person covered under expiring Policy
• Multi Year Policy:
o Fitness discount earned on yearly basis will be accumulated till
Policy End date.
o On Renewal of the Policy, total discount amount accrued each Policy
Year will be applied on Renewal Premium of subsequent year and for
Insured Person covered under expiring Policy
• For Policiescovering more than one Insured Person,Healthy Weeks
for each Insured Person will be tracked and accrued. Such discount
will be applicable on individual Renewal Premium for both Individual
and Floater Sum Insured basis Policies.
• Premium will be discounted to the extent applicable to coverage
corresponding to expiring Policy.
• In case of Increase in Sum Insured at Renewal, discount amount will be
applied on the premium corresponding to expiring Policy Sum Insured.
• Fitness discount @ Renewal will be applied only on Renewal of Policy
with Us and only if accrued.
B. Health Incentive
This Program encourages Insured Persons to maintain good health and
avail incentives as listed below.
Under this Program, Insured Person having Pre-Existing Diseases
or Obesity (BMI above 30) as listed under table A below, will be eligible
for reduction in Medical Underwriting Loading applied on rst inception
of the Policy with Us provided that;
i. Insured Person shall undergomedical tests and/or BMIcheck-upas
listed belowminimum 3 months prior to expiry of Policy Year (For
Multiyear Policies) or before Renewal (For Annual Policies).
ii. Medical test shall be done at Your own cost through our Network
Provider on Our my: health mobile App.
iii. If the test parameters are within normal limits, We will apply 50%
discount on the Medical Underwriting loading applied for corresponding
Pre-Existing Disease or Obesity as applicable on Renewal of the
Policy with Us.
iv. If the test parameters at subsequent Renewal are not within normal
limits or Medical test reports are not submitted in accordance with
i and ii above, the discount amount applied on Medical Underwriting
loading will be zero
Table A
Pre-existing Diseases Test
Diabetes HbA1c
Hypertension Blood Pressure reading
Hyperlipidemia Total Cholesterol
Cardiovascular Diseases ECG
Hypothyroidism Thyroid function tests
Obesity BMI
Application of Health Incentive
• Annual Policy: Discount amount accrued during the expiring Policy
year will be applied on the Renewal Premium corresponding to
expiring Policy Sum Insuredand for Insured Person covered under
expiring Policy
• Multi Year Policy:
o Discount amount earned on yearly basis will be accumulated till
Policy End date.
• On Renewal of the Policy, total discount amount accrued each year will
be applied on Renewal Premium of subsequent yearand for Insured
Person covered under expiring Policy
• For Policies covering more than one Insure Person, tests shall be done
for each Insured Person basis which such reduction in loading where
ever applicable will be applied on individual Renewal Premium for both
Individual and Floater Sum Insured basis Policies.
• Medical Underwriting loading will be discounted only on Renewal
of Policy with Us and only for Insured Person covered under such
expiring Policy
• Discount on Medical Underwriting loading under this cover is
applicable only on next Renewal and cannot be utilized if Policy not
renewed with us.
C. Wellness services:
The services listed below are available to all Insured Person through
Our Network Provider on Our my: health mobile app only. Availing
of services under this Section will not impact the Sum Insured or the
eligibility for Cumulative Bonus.
i. Health Coach:
An Insured Person will have access to Health Coaching services in
areas such as:
• Disease management
• Activity and tness
• Nutrition
• Weight management.
These services will be available through Our my: health mobile app
as a chat service or as a call back facility.
ii. Wellness services
• Discounts: on OPD, Pharmaceuticals, pharmacy, diagnostic centres.
• Customer Engagement: Monthly newsletters, Diet consultation,
health tips
• Specialized programs: like stress management, Pregnancy Care,
Work life balance management.
These services will be available through Our my: health mobile app
Disclaimer applicable to my: health Mobile app and associated
services
It is agreed and understood that Our my:health mobile app and Wellness
services intention is not to provide specic medical advice but rather
to provide users with information to better understand their health and
their diagnosed disorders. The information is not a substitute for
professional medical care by a qualied doctor or other health care
professional.

4
The information provided is general in nature and is not specic to you.
You must never rely on any information obtained using this app for any
medical diagnosis or recommendation for medical treatment or as an
alternative to medical advice from your physician or other professional
healthcare provider. If you think you may be suffering from any medical
condition you should seek immediate medical attention.
Reliance on any information on this App is solely at your own risk. HDFC
EGRO General Insurance Company Limited do not assume any liability
towards any loss or damage arising out of or in relation to any opinion,
actual or alleged errors, omissions and representations, any decision
made or action taken or not taken in reliance upon the information.
Section I 1 C: Optional Covers
Insuring Clause
In consideration of payment of additional Premium or reduction in the
Premium as applicable, it is hereby declared and agreed that We will
pay/restrict the expenses under below listed Covers subject to all other
terms, conditions, exclusions and waiting periods applicable to the Policy.
These Covers are optional and applicable only if opted for and upto
the Sum Insured or limits mentioned on the Schedule of Coverage in
the Policy Schedule.
1. Preventive Health Check-Up - Booster
On opting this Cover, Insured Person will be entitled for Health Check-up
after each Policy Year with Us irrespective of Claims made under the
Policy in accordance with options given below.
i. We will reimburse the cost of Preventive Health Check-upup to limits
mentioned on the Schedule of Coverage.
Or
ii. Insured Person shall have the option to undergo Health Check-Up
at our Network Service Provider in accordance to criteria given below.
Sum Insured Tests
Upto 2 Lacs Medical Examination Report, Complete Blood
Count Urine R, Fasting Blood Sugar, Serum
Creatinine, Lipid Prole, Electro Cardio Gram
3 Lac and above Chest X Ray , 2D echo/ Stress test, PSA
for Males, PAP smear for Females, Medical
Examination Report, Complete Blood Count
Urine R, Fasting Blood Sugar, Serum
Creatinine, Lipid Prole, Electro Cardio Gram
Other Terms and Conditions applicable to this Cover
• This benet will not be carried forward if not utilized within 60 days of
Policy Anniversary/Renewal date.
• On opting this Cover, Renewal Benet 1, Preventive Health Check-up
under Section I1 B stands deleted.
2. Parent and Child care Cover - Basic
We will pay to the Insured Personsubject to waiting period as mentioned
in the Schedule of Coverage on the Policy Schedule under Covers as
given below.
I. Parent Care
i. Medical Expenses under Section I1 A1 for Maternity Expenses
limited up to 2 deliveries or 1 delivery and 1 termination or 2 terminations
during the lifetime of the Insured Person
ii. OPD Treatment in Pre-natal and Post-natal period provided Claim
under Maternity Expenses is admissible under the Policy.
II. Child Care
We will pay/coverfollowing expenses towards Child Care for New Born
Babyunder this cover if Claim for Maternity Expensesis admissible
under the Policy.
i. We will pay Medical Expenseslisted under Section I1 A1 withinSum
Insured for Parent Caretowards treatment of a New Born Babyas per
limit mentioned on Schedule of Coverage.
ii. New Born Baby Cover–We will cover New Born Baby immediately
after the birth as per original terms of the Policy on receipt of completed
proposal form and Premium received within 90 days of birth of Baby and
subject to acceptance by Us.
If this Cover is opted, General exclusion III b 1. ix) under General
Exclusions, Section III a 1 iv, stands deleted.
Exclusions applicable to this Cover.
i. Pre-Hospitalization and post-Hospitalization expenses are not
payable under this cover
ii. We will not pay any expenses related to ectopic pregnancy under
this cover. Ectopic pregnancy will be covered as a part of expenses
under SectionI 1A1 only.
iii. Treatment for impotency, treatment to effect infertility, surrogate or
vicarious pregnancy, voluntary termination of pregnancy, procedures to
assist birth control, contraceptive supplies.
3. Parent and Child care Cover – Booster
We will pay to the Insured Person subject to waiting period and limits
as mentioned in the Schedule of Coverage on the Policy Schedule under
Covers as given below.
I. Parent Care
i. Maternity Expenses - Medical Expenses for a delivery (including
caesarean section) on Hospitalization or the lawful medical termination
of pregnancy during the Policy Period.
ii. OPD Treatment in Pre-natal and post-natal periodup to the limit of
this cover, provided Claim under i. Maternity Expenses is admissible
under the Policy
iii. Infertility Treatment:Medical Expenseslisted under Section I1 A1
incurred for infertility treatment, assisted reproductive treatments like IVF
undertaken on advice of a Medical Practitioner, up to 50% of Normal
Delivery Sum Insured under this Cover. This cover is applicable for both
Male and Female Insured Person
II. Child Care
We will pay following expenses towards Child Care for New Born
Baby under this cover if Claim for Maternity Expenses is admissible
under the Policy.
i) New Born baby cover:
We will pay Medical Expenses listed under Section I1 A1 towards
treatment of a New Born Baby within the limit of Sum Insured under this
Cover as mentioned in Schedule of Coverage on the Policy Schedule
ii) Vaccination Charges:
We will pay expenses incurred on vaccination for New Born Baby
as per National Immunization Schedule until New Born Baby completes
1 year of age subject to maximum of sub limit of Sum Insured under
this Cover.
If opted, this cover General exclusion Section III b 1 .ix), x), xx) under
General Exclusions, Section III and Optional Cover 2 “Parent and Child
Cover – Basic” under Section I 1C stands deleted.
III. Waiting Period modication Option
On availing this option, Waiting Period listed under Section –III a 1, iv,
will stand modied as mentioned in the Schedule of Coverage on the
Policy Schedule.
All other terms and conditions of the Parent & Child Care Cover - Booster
shall remain unaltered.
Exclusions applicable to this Cover.
i. Pre-Hospitalization and post-Hospitalization expenses are not payable
under this cover
ii. We will not pay any expenses related to ectopic pregnancy under
this cover. Ectopic pregnancy will be covered as a part of expenses
under Section I1 A1 only.
iii. Treatment for impotency, treatment to effect infertility, surrogate or
vicarious pregnancy, voluntary termination of pregnancy, procedures to
assist birth control, contraceptive supplies.

5
4. Air Ambulance Cover
We will pay for Air Ambulance transportation in an airplane or helicopter
for Emergency Care which requires immediate and rapid ambulance
transportation as prescribed by a Medical Practitioner, from the site
of rst occurrence of the Illness/Accident to the nearest Hospital,that
ground transportation cannot provide. Claim would be reimbursed up to
the actual expenses subject to a maximum of Sum Insured as specied
on theSchedule of Coverage in the Policy Schedule.
Exclusion:
We will not pay for return transportation to the Insured Person’s home
by air ambulance
5. Recovery Benet
We will pay Sum Insured as specied on the Schedule of Coverage
in the Policy Schedule upon Medically Necessary Hospitalization of
an Insured Person exceeding 10 consecutive and continuous days
and for which Claim is admissible under Section I1 A– Hospitalization
Cover.
This benet is not applicable ifMedical treatment is taken under Section
I1 A2 – Home Health care and 1A3 – Domiciliary Hospitalization
6. Sum Insured Rebound
We will add to the Sum Insured, an amount equivalent to the admissible
Claim amount, subject to maximum of Basic Sum Insured, on subsequent
Hospitalization of the Insured Person during Policy Year subject to;
i. Total of Basic Sum Inured under Hospitalization Cover, Cumulative/
Extended Cumulative Bonus (if applicable) earnedand Sum Insured
Rebound will be available to all Insured Persons for all claims under
Section I1A during the current Policy Year and subject to the condition
that a single claim in a Policy Year cannot exceed the sum of Basic
Sum Insured and the Cumulative/Extended Cumulative Bonus (if
opted) earned
ii. In case of treatment for Chemotherapy and Dialysis, Sum Insured
Rebound will be applicable only once in lifetime of Policy
i. This cover will be applicable annually for policies with term more
than one year.
ii. Any unutilized amount of Sum Insured Rebound cannot be carried
over to next Policy Year or Renewal Policy
iii. The Sum Insured Rebound can be utilized for Claims under Section
I1 A only.
Illustration 1
Time Claim No.
Sum Insured
available
Cumulative Bonus
available
Admissible
Claim amount
SI Rebound
Available
Total SI Rebound
till date
Payable
amount
3 months
1
3,00,000 30,000 2,50,000 0 0 2,50,000
5 months 50,000 30,000 1,40,000 0 0 80,000
9 months 2 0 0 2,50,000 3,00,000 3,00,000 2,50,000
11 months 4 0 0 70,000 50,000 3,00,000 50,000
Illustration 2
Time Claim No.
Sum Insured
available
Cumulative Bonus Admissible
Claim amount
SI Rebound
Total SI Rebound
till date
Payable
amount
3 months 1 3,00,000 30,000 2,50,000 0 0 2,50,000
6 months 2 50,000 30,000 1,40,000 2,50,000 2,50,000 1,40,000
9 months 3 0 0 2,50,000
=250,000-
60,000+50,000
3,00,000 2,40,000
=240,000
11 months 4 0 0 70,000 0 3,00,000 0
7. Outpatient Dental Treatment
After threeconsecutive and continuous Policy Years with Us, We will pay
50% of Medical Expenses incurred by Insured Person towards Dental
Treatment prescribed by Medical Practitioner up to the amount as
mentioned in the Schedule of Coverage on the Policy Schedule. Claim
under this Section can be availed only through our Network Provider.
The Cover is applicable only to Insured Person covered under three
consecutive and continuous Policy Years and who continue to remain
insured in the subsequent Policy Year/Renewal
The Coverage is applicable only towards cost of X-rays, extractions,
amalgam or composite llings, root canal treatments and prescribed
drugs for the same.
Claim under this Section will not affect Cumulative Bonus under
Section I1 B2, condition ii.
Exclusions specic to Outpatient Dental Treatment
i. Cosmetic surgery, dentures, dental prosthesis, dental implants,
orthodontics, orthognathic surgery, jaw alignment or treatment for the
temporomandibular (jaw) joint, or upper and lower jaw bone surgery and
surgery related to the temporomandibular (jaw) unless necessitated by
an acute traumatic injury due to an accident or cancer
8. External Medical Aids
After every twoconsecutive and continuous Policy Year with Us, We
will pay up to 50% of cost incurred towards following Medical Expenses
subject to maximum of Sum Insured as mentioned in the Schedule of
Coverage, on the Policy Schedule;
i. One pair of spectacles or one pair of contact lenses,
ii. A hearing aid
Other terms
• The Cover is applicable only to Insured Person covered under two
consecutive and continuous Policy Years and who continue to remain
insured in the subsequent Policy Year/Renewal
• Under a Family Floater Policy, Our liability shall be limited to either one
pair of spectacles or contact lenses or hearing aid per family.
• Medical Expenses incurred under this Cover shall be prescribed by
our Network Provider and is payable only once after block of every
two consecutive and continuous Policy Year with Us.
• Claim under this Section will not affect Cumulative Bonus under
Section I1 B2, condition ii
9. Major Illness Hospitalization Expenses
We will payfor Medical Expenses incurred and admissible under Section
I1 A1,up to additional Sum Insured equivalent to Basic Sum Insured,on
Medically necessary Hospitalization of Insured Person for Major
illnesseslisted below whose diagnosis rst commence/occursafter the
applicable waiting period from commencement of the rst Policy with
Us, subject to the following;
i. Waiting Period – The coverage is subject to Waiting Period as
mentioned on Schedule of Coverage on the Policy Schedule
ii. Claim for each Major Illnessis payable only once during the lifetime
of Policy with Us. However, Insured Person will continue to be covered
under this Section for other Major Illnesses.
iii. Claim under this Cover is admissible only when total of Basic Sum
Insuredis completely utilized.

6
iv. The additional Sum Insured under this Cover is exclusive and specic
for the treatment of the rst occurrence of the above Critical Illness
undertaken in a Hospital/Nursing Home as an in-patient and will not be
available for other illnesses/hospitalization.
Major Illness Covered
1 Cancer of specied
severity
6 Major Organ/Bone Marrow
Transplant
2 Open Chest CABG 7 Stroke resulting in permanent
symptoms
3 Myocardial Infarction
(First Heart Attack of
specic severity)
8 Surgery of Aorta
4 Kidney Failure requiring
regular dialysis
9 Primary (Idiopathic)
Pulmonary Hypertension
5 Multiple Sclerosis with
Persisting Symptoms
10. Non-Medical Expenses cover
We will pay for Non-Medical Expenses upto the limit mentioned in
Schedule of Coverage in the Policy Schedule on Medically necessary
Hospitalization of Insured Person for claims admissible under Section
I1A1, 2 and 3.
In view of this Cover, Exclusion xxi) of Section III b , shall stand covered
upto the extent mentioned above.
11. Waiting period Modication Option
On availing this option, Waiting Periods listed under Section III a 1 – i,
ii and iii will stand modied as mentioned in Schedule of Coverage on
the Policy Schedule for following Sections;
Section I1 A – Hospitalization Cover
Section I1C4 – Air Ambulance
Section I1C5 – Recovery Benet
Section I1C9 – Major Illness Hospitalization Expenses
Section I1C17 –Hospital Cash
Section I1C18 – Global Health Cover
All other terms and Conditions of the respective Section and Policy
shall remain unaltered.
12. Extended Cumulative Bonus
On availing this cover, Cumulative Bonus percentage mentioned under
Section I1 B2 – Cumulative Bonus will stand modied as mentioned in
Schedule of Coverage on the Policy Schedule subject to;
i. Once the Extended Cumulative Bonus benet is availed by the
Insured Person, it cannot be opted out at subsequent Renewal.
ii. All other terms and Conditions of Renewal Benets Section I1 B, ii
shall remain unaltered.
13. Room Rent Modication Option
On availing this option, limits specied under Section I1 A1 i and I1A ii
will stand modied as below.
i. Room Rent, boarding and Nursing – limit of 1% of the Basic Sum
Insured subject to maximum of Rs. 5,000 per day
ii. Intensive care unit – limit of 2% of the Basic Sum Insured subject
to maximum of Rs. 10,000 per day
Proportionate deduction:
In case expenses incurred on i and ii above exceed respective applicable
limits under the Policy, expenses incurred under Section I1 A1, iii and
iv , shall be paid in the same proportion as the admissible rate per day
bears to the actual rate per day of Room Rent charges
14. Co-Payment
On availing this option, Co-Payment as mentioned on the Schedule
of Coverage in the Policy Schedule will be applied on each and every
admissible claim after Deductible/Excess wherever applicable under the
Policy. Once the Co-Payment option is availed by the Insured Person,
it cannot be opted out of at subsequent Renewal.
15. Major Illness – Benet
If the eldest Insured Person covered under the Policy suffers from Major
Illness as listed below, whose diagnosis rst commence/occurs after the
applicable Waiting Period from commencement of rst Policy with Us,
We will pay Sum Insured as mentioned on the Schedule of Coverage.
The Coverage under this benet shall cease to exist upon occurrence
of any one Major Illness covered for which Claim is admitted by the
Company.
Major Illness Covered
1 Cancer of specied severity 7 Permanent Paralysis of
Limbs
2 Open Chest CABG 8 Stroke resulting in
Permanent Symptoms
3 Myocardial Infarction(First
Heart Attack of specic
severity)
9 Surgery of Aorta
4 Kidney Failure requiring
regular dialysis
10 Primary (Idiopathic)
Pulmonary Hypertension
5 Major Organ/Bone Marrow
Transplant
11 Open Heart Replacement
or Repair of Heart Valves
6 Multiple Sclerosis with
Persisting Symptoms
Survival Period
Claim under this Cover is payable only if Insured Person survives 30
days from the diagnosis, fulllment of the denition of the Major illness
covered and with conrmatory diagnosis of the conditions covered
while the Insured Person is alive (A claim would not be admitted if the
diagnosis is made post mortem)
16. E-Opinion
We will pay expenses incurred towards second Medical Opinion availed
from Medical Practitionerin respect of Major Illness covered and listed
below under the Policy through our Network Provider.
The Coverage under this benet shall cease to exist upon availing
Second Opinion for any one Major Illness as listed below.
Major Illness Covered
1 Cancer of specied
severity
7 Permanent Paralysis of Limbs
2 Open Chest CABG 8 Stroke resulting in Permanent
Symptoms
3 Myocardial Infarction(First
Heart Attack of specic
severity)
9 Surgery of Aorta
4 Kidney Failure requiring
regular dialysis
10 Primary (Idiopathic)
Pulmonary Hypertension
5 Major Organ/Bone
Marrow Transplant
11 Open Heart Replacement or
Repair of Heart Valves
6 Multiple Sclerosis with
Persisting Symptoms
Disclaimer - E- Opinion Services are being offered by Network
providers through its portal/mail/App or what so ever electronic form
to Policyholders/Insured of HDFC ERGO GENERAL INSURANCE
COMPANY LIMITED. In no event shall HDFC ERGO be liable for any
direct, indirect, punitive, incidental, special consequential damages or
any other damages whatsoever caused to the Policyholders/Insured
of HDFC ERGO while receiving the services from Network providers.
17. Hospital Cash
We will pay per day Sum Insured up to maximum Number of days
and in manner as specied in Schedule of Coverage on the Policy
Schedule,for each continuous and completed period of 24 hours of
Medically Necessary Hospitalization of an eldest Insured Personin
the Policyand for which Claim is admissible under SectionI1 A –
Hospitalization Cover.

7
18. Global Health Cover
On availing this Cover,We will paythe Expenses incurred outside India
under Sections and Covers given below.
Section I1A: Hospitalization Cover
A1 Medical Expenses A7 Road Ambulance
A4 Pre-Hospitalization cover A8 Organ Donor Expenses
A5 Post-Hospitalization cover A9 Alternative Treatments
A6 Day Care Procedures
Section I1C: Optional Covers
C1 Preventive Health Check-Up
- Booster
C10 Non-Medical Expenses
cover
C2 Parent and Child care Cover
- Basic
C3 Parent and Child care Cover
– Booster
C15 Major Illness – Benet
C4 Air Ambulance Cover C16 E-Opinion
C5 Recovery Benet C17 Hospital Cash
C6 Sum Insured Rebound
C7 Outpatient Dental Treatment
C8 External Medical Aids
C9 Major Illness Hospitalization
Expenses
Global Cover is applicable subject to following terms and conditions
i. Global coverage for expenses towards all the listed covers is applicable
and effective only if mentioned on the Schedule of Coverage in the
Policy Schedule.
ii. A Deductible of USD 100 will apply for expenses under all the
respective covers separately for each and every claim.
iii. Claims on Reimbursement basis will be payable in INR only.
iv. All other terms and conditions of the respective Section and Covers
under the policy shall remain unaltered.
SECTION 2: MY:HEALTH CRITICAL SURAKSHA PLUS
Section I.2.A. Base Covers
I. Critical Illnesses Cover
1. Cancer Cover
If Insured Person suffers from Critical illnessor undergoesSurgical
Procedure as listed below, whose diagnosis rst commence/occurs
after the applicable Waiting Period from commencement of rst Policy
with Us, We will pay Sum Insured or percentage of Sum Insured in
accordance with table below:
Critical illness /
Surgical Procedure
Stage
Percentage of
Sum Insured
Payable
Waiting
Period
Applicable
1 Malignant Cancer of
specied Sites
Major
100% of Sum
Insured
90 days
Specied Sites-
Female
Breast
Cervix
Uterus
Fallopian Tube
Ovary
Vagina/Vulva
Critical illness /
Surgical Procedure
Stage
Percentage of
Sum Insured
Payable
Waiting
Period
Applicable
Specied Sites- Male
Major
100% of Sum
Insured
90 days
Head and Neck
Lung
Stomach
Colorectum
Prostate
2 Cancer of specied
severity
Major 100% of Sum
Insured
90 days
3 Aplastic Anemia Major 100% of Sum
Insured
90 days
4 Major Organ
Transplant – Bone
Marrow
Major 100% of Sum
Insured
90 days
5 Early Stage Cancer Minor 25% of Sum
Insured
subject to
maximum of
Rs. 1,000,000
180 days
6 Carcinoma in situ Minor
2. Heart Cover
If Insured Person suffers fromCritical illnessor undergoesSurgical
Procedure as listed below, whose diagnosis rst commence/occurs
after the applicable Waiting Period from commencement of rst Policy
with Us, We will pay Sum Insured or percentage of Sum Insured in
accordance with table below:
Critical Ailments/
Procedures
Stage
Percentage
of Sum
Insured
Payable
Waiting
Period
Applicable
1 Open Chest CABG Major
100%
of Sum
Insured
90 days
2 Myocardial Infarction
(First Heart Attack of
specied severity)
Major
3 Open Heart Replacement
or Repair of Heart Valves
Major
4 Major Organ Transplant
– Heart
Major
5 Surgery of Aorta Major
6 Primary (Idiopathic)
Pulmonary Hypertension
Major
7 Other serious coronary
artery disease
Major
8 Dissecting Aortic
Aneurysm
Major
9 Cardiomyopathy Major
10 Eisenmenger’s
Syndrome
Major
11 Infective Endocarditis Major
12 Angioplasty Minor 25%
subject to
maximum
payout
of INR
1,000,000
180 days
13 Balloon Valvotomy or
Valvuloplasty
Minor
14 Insertion of Pacemaker Minor
3. Nervous System Cover
If Insured Personsuffers from Critical illnessor undergoes Surgical
Procedure listed belowafter the applicable Waiting Period from

8
commencement of rst Policy with Us, We will pay Sum Insuredin
accordance with table below:
Critical illness /
Surgical Procedure
Stage
Percentage
of Sum
Insured
Payable
Waiting
Period
Applicable
1 Multiple Sclerosis with
persisting symptoms
Major
100%
of Sum
Insured
90 days
2 Permanent Paralysis
of Limbs
Major
3 Stroke resulting in
permanent symptoms
Major
4 Benign Brain Tumour Major
5 Coma of specied
severity
Major
6 Parkinson’s Disease Major
7 Alzheimer’s Disease Major
8 Motor Neurone Disease
with permanent
symptoms
Major
9 Muscular Dystrophy Major
10 Apallic Syndrome Major
11 Bacterial Meningitis Major
12 Creutzfeldt-Jakob
Disease (CJD)
Major
13 Encephalitis Major
14 Major Head Trauma Major
15 Progressive
Supranuclear Palsy
Major
16 Brain Surgery Major
17 Loss of Speech Major
4. Other Major Organ Cover
If Insured Personsuffers from Critical illnessor undergoesSurgical
Procedure listed below after the applicable Waiting Period from
commencement of rstPolicy with Us, We will pay percentage of Sum
Insured in accordance with table below:
Critical illness /Surgical
Procedure
Stage
Percentage
of Sum
Insured
Payable
Waiting
Period
Applicable
1 Kidney failure requiring
regular dialysis
Major
100%
of Sum
Insured
90 days
2 Major Organ Transplant
– Kidney, Lung, Liver and
Pancreas
Major
3 End Stage Liver Failure Major
4 Medullary Cystic Disease Major
5 Systemic Lupus
Erythematous with Lupus
Nephritis
Major
6 End Stage Lung Failure Major
7 Fulminant Hepatitis Major
8 Chronic Adrenal
Insufciency (Addison’s
Disease)
Major
9 Progressive Scleroderma Major
10 Chronic Relapsing
Pancreatitis
Major
Critical illness /Surgical
Procedure
Stage
Percentage
of Sum
Insured
Payable
Waiting
Period
Applicable
11 Elephantiasis Major
100% days
of sum
insured
90 days
12 HIV due to blood
transfusion and
occupationally acquired
HIV
Major
13 Terminal Illness Major
14 Myelobrosis Major
15 Pheochromocytoma Major
16 Crohn’s Disease Major
17 Severe Rheumatoid
Arthritis
Major
18 Severe Ulcerative Colitis Major
19 Deafness Major
20 Blindness Major
21 Third Degree Burns Major
22 Severe Osteoporosis Minor 25%
subject to
maximum
payout
of INR
1,000,000
180 days
Covers and General Conditions applicable to Section I2AI, 1 to 4
1. Reduced Premium Benet
If Insured Person is diagnosed with any covered Minor condition
covered under this section and for which Claim is admissible under the
Policy, We will waive 50% of the applicable Annual RenewalPremium
on subsequent Renewal of Policy with Us subject to:
i. Premium will be waived for the Renewal of Insured Personfor whom
the claim has been made, to the extent applicable to Coverage, terms
and conditions corresponding to expiring yearPolicy.
ii. Premium will be waived for subsequent Renewal of 5 PolicyYearsonly.
2. Survival Period
Claim under Section I2AI, 1 to 4is payable only if Insured Person
survives 7 days from the diagnosis and fulllment of the denition of
theCriticalIllness or Surgical Procedurecovered.
The Claim is admissible only with conrmatory diagnosis of the conditions
covered while the Insured Person is alive (A claim would not be admitted
if the diagnosis is made post mortem)
3. Number of Claims and Benets payable
Only one claim is payable under each of the stages given below during
lifetime of the Policy under this Sectionsubject to maximum 100% of
Sum Insured mentioned on the Policy Schedule irrespective of Number
of Sections opted and Number of Policies held by the Insured Person.
Minor Stage - On the admissibility of Claim under Minor Stage condition
under the Policy, coverage for all other Minor stage Conditions shall
cease to exist. The Policy shall continue to Cover Major Stage condition
for the Balance Sum Insured.
Major Stage – On the admissibility of Claim under Major Stage condition,
coverage under this Policy shall cease to exist.
In the event where an Insured Person holds multiple Policies insuring
different Covers under this Section of this product, Claim will be
admissible under one Cover only and Total Sum Insured as applicable
under such Cover across all policies of this product will be paid by the
Company. Insurance for other Covers, if applicable, shall cease to exist.
II. Multipay Critical Illnesses Cover
1. Cancer Cover
If Insured Person suffers fromCritical illnessor undergoesSurgical

9
Procedure as listed below, whose diagnosis rst commence/occurs
after the applicable Waiting Period from commencement of rst Policy
with Us, We will pay Sum Insured or percentage of Sum Insured in
accordance with table below:
Sr.
No.
Critical illness /
Surgical Procedure
Stage
Percentage
of Sum
Insured
Payable
Waiting
Period
Applicable
1 Cancer of Specied
Severity
Major
100%
of Sum
Insured
90 days2 Aplastic Anemia Major
3 Major Organ Transplant
– Bone Marrow
Major
2. Heart Cover
If Insured Person suffers fromCritical illnessor undergoes Surgical
Procedure as listed below, whose diagnosis rst commence/occurs
after the applicable Waiting Period from commencement of rst Policy
with Us, We will pay Sum Insured or percentage of Sum Insured in
accordance with table below:
A
CriticalAilments /
Surgical Procedures
Stage
Percentage
of Sum
Insured
Payable
Waiting
Period
Applicable
1 Open Chest CABG Major
100% of Sum
Insured
90 days
2 Myocardial Infarction
(First Heart Attack of
specied severity)
Major
3 Open Heart
Replacement or Repair
of Heart Valves
Major
4 Major Organ Transplant
– Heart
Major
5 Surgery of Aorta Major
6 Primary (Idiopathic)
Pulmonary
Hypertension
Major
7 Other serious coronary
artery disease
Major
8 Dissecting Aortic
Aneurysm
Major
9 Cardiomyopathy Major
10 Eisenmenger’s
Syndrome
Major
11 Infective Endocarditis Major
B* Angioplasty Minor 25% subject
to maximum
payout of
INR1,000,000
180 days
*B - Angioplasty
We will pay 25% of Sum Insured subject to maximum of INR 10,00,000
if Insured Person undergoes Angioplasty,whose diagnosis and/or
manifestation rst commence/occurs more than 180 days after the
commencement of rst Policy with Us.
On the admissibility of Claim under Angioplasty, coverage for Angioplasty
shall cease to exist. The Policy shall continue to cover other Critical
illnessor Surgical Procedureunder this cover, for Balance Sum
Insuredin accordance with table above.
3. Nervous System Cover
If Insured Personsuffers from Critical illnessor undergoes Surgical
Procedure listed below after the applicable Waiting Period from
commencement of rst Policy with Us, We will pay percentage of Sum
Insured in accordance with table below:
Critical illness /Surgical
Procedure
Stage
Percentage
of Sum
Insured
Payable
Waiting
Period
Applicable
1 Multiple Sclerosis with
persisting symptoms
Major
100%
of Sum
Insured
90 days
2 Permanent Paralysis of
Limbs
Major
3 Stroke resulting in
permanent symptoms
Major
4 Benign Brain Tumour Major
5 Coma of specied
severity
Major
6 Parkinson’s Disease Major
7 Alzheimer’s Disease Major
8 Motor Neurone Disease
with permanent
symptoms
Major
9 Muscular Dystrophy Major
10 Apallic Syndrome Major
11 Bacterial Meningitis Major
12 Creutzfeldt-Jakob
Disease (CJD)
Major
13 Encephalitis Major
14 Major Head Trauma Major
15 Progressive Supranuclear
Palsy
Major
16 Brain Surgery Major
17 Loss of Speech Major
4. Other Major Organ Cover
If Insured Personsuffers from Critical illnessor undergoes Surgical
Procedure listed below after the applicable Waiting Period from
commencement of rst Policy with Us, We will pay percentage of Sum
Insured in accordance with table below:
Critical illness /Surgical
Procedure
Stage
Percentage
of Sum
Insured
Payable
Waiting
Period
Applicable
1 Kidney failure requiring
regular dialysis
Major
100%
of Sum
Insured
90 days
2 Major Organ Transplant
– Kidney, Lung, Liver and
Pancreas
Major
3 End Stage Liver Failure Major
4 Medullary Cystic Disease Major
5 Systemic Lupus
Erythematous with Lupus
Nephritis
Major
6 End Stage Lung Failure Major
7 Fulminant Hepatitis Major
8 Chronic Adrenal
Insufciency (Addison’s
Disease)
Major
9 Progressive Scleroderma Major
10 Chronic Relapsing
Pancreatitis
Major
11 Elephantiasis Major

10
Critical illness /Surgical
Procedure
Stage
Percentage
of Sum
Insured
Payable
Waiting
Period
Applicable
12 HIV due to blood
transfusion and
occupationally acquired
HIV
Major
100%
of Sum
Insured
90 days
13 Terminal Illness Major
14 Myelobrosis Major
15 Pheochromocytoma Major
16 Crohn’s Disease Major
17 Severe Rheumatoid
Arthritis
Major
18 Severe Ulcerative Colitis Major
19 Deafness Major
20 Blindness Major
21 Third Degree Burns Major
Covers and General Conditions applicable to Section I2 AII, 1 to 4
1. Reduced Premium Benet
If Insured Person is diagnosed with any coveredCriticalIllness
under any Cover from Section I 2AII, 1 to 4 and for which Claim is
admissible under the Policy, We will waive 50% of the applicable
Annual RenewalPremium on subsequent Renewal of Policysubject to:
i. Premium will be waived for the renewal of Insured person for whom
the claim has been made, to the extent applicable to Coverage, terms
and conditions corresponding to expiring Policy.
ii. Premium will be waived for subsequent Renewal of 5 Policy Years,
following every admissible claim under each Cover.
2. Survival Period
Each Claim under Section I2AII, 1 to 4 is payable only if Insured Person
survives 7 days from the diagnosis and fulllment of the denition of
theCritical Illness or Surgical Procedure covered.
The Claim is admissible only with conrmatory diagnosis of the conditions
covered while the Insured Person is alive (A claim would not be admitted
if the diagnosis is made post mortem)
3. Number of Claims and Waiting Period
Coverage under this Section shall cease to exist; once a Claim has
been admitted under each of the Covers as opted by the Insured Person
and maximum 100% of the Sum Insured is paid by the Company under
such Covers subject to 12 months waiting period between Claims under
any two Covers.
In the event where an Insured Person holds multiple Policies under
this Section of this product, Total Sum Insured under this section
across all policies of this product will be paid by the Company for each
admissible claimsubject to 12 months waiting period between Claims
under any two Covers.
For Example: If an Insured Person suffers a Stroke resulting in
permanent symptoms and at any time within 12 months also suffers
from Myocardial Infraction (First Heart Attack of specied severity)
thereby triggering claims under both Nervous System Cover and Cardiac
Cover, the Company will pay maximum 100% of Sum Insured under one
Cover only. However, if the two incidences were separated by more than
12 months’ time period, theCompany will pay maximum 100% of Sum
Insured under each Cover.
Section B. my: health Active
1. Fitness discount @ Renewal
Insured Person can avail discount on Renewal Premium by
accumulating Healthy Weeks as per table given below.
One Healthy Week can be accumulated by;
• Recording minimum 50,000 steps in a week subject to maximum 15,000
steps per day, tracked through Your wearable device linked to Ourmy:
health mobile app andYourPolicy number
OR
• burning total of 900 calories up to maximum of 300 calories in one
exercise session per day, tracked Your wearable device linked to Ourmy:
health mobile appendYourPolicy number
Healthy Weeks Discounts
No. of Healthy Weeks
Accumulated
Discount on Renewal
Premium
1-4 0.50%
5-8 1.00%
9-12 2.00%
13-16 3.00%
17-26 6.00%
27-36 7.50%
Above 36 10.00%
Steps to accumulate Healthy Weeks
Step 1 - The my: Health App must be downloaded on the mobile.
Step 2 - You can start accumulating Healthy Weeks by tracking physical
activity trough the Wearable device linkedtomy: Health App
We encourage and recognize all types of exercise/tness activities
by making use of wearable devices to track and record the activities
Insured Person engages in.
Application of Fitness discount @ Renewal
• Annual Policy: Discount amount accrued based on Number of
accumulated Healthy Weeks during the expiring Policy year will be
applied on the Renewal Premium for expiring Policy Sum Insured.
· Multi Year Policy:
o Fitness discount earned on yearly basis will be accumulated till
Policy End date.
o On Renewal of the Policy, total discount amount accrued each year
will be applied on Renewal Premium of subsequent year.
• For Policiescovering more than one Insured Person, Healthy Weeks
for each Insured Person will be tracked andaccumulated. Such
discount will be applicable on individual RenewalPremium.Premium
will be discounted to the extent applicable to coverage corresponding
to expiring Policy.
• In case of Increase in Sum Insured at Renewal, discountpercentage
will be applied on the Sum Insured applicable under expiring Policy.
• Fitness discount @ Renewal will be applied only on Renewal of
Policy with Us.
2. Health Incentive
This Program encourages Insured Person to maintain good health and
avail incentives as listed below.
Under this Program, Insured Person having Pre-Existing Diseases
orObesity (BMI above 30)as listed under table A below, will be eligible
for reduction in Medical Underwriting Loading applied at rst inception
of the Policy with Us provided that;
i. Insured Person shall undergo medical tests and/or BMI check-up
below minimum 3 months prior to expiry of Policy Year (For Multiyear
Policies) or before Renewal (For Annual Policies).
ii. Medical test shall be done at Your own cost through our Network
Providerthrough Our my: health mobile app App.
iii. If the test parameters are within normal limits, We will apply 50%
discount on the Medical Underwriting loading applied for corresponding
Obesityas applicableon Renewal of the Policy with Us.
iv. If the test parameters at subsequent renewal is not within normal
limits or Medical test reports are not submitted in accordance with i
and ii above, the discount amount applied on Medical Underwriting
loading will be zero.

11
Table A
Pre-existing Diseases Test
Diabetes HbA1c
Hypertension Blood Pressure reading
Hyperlipidemia Total Cholesterol
Hypothyroidism Thyroid function tests
Obesity BMI
Application of Health Incentive
• Annual Policy: Discount amount accrued during the expiring Policy
year will be applied on the Renewal Premium for expiring Policy Sum
Insured.
• Multi Year Policy:
o Discount amount earned on yearly basis will be accumulated till
Policy End date.
o On Renewal of the Policy, total discount amount accrued each year
will be applied on Renewal Premium of subsequent renewal.
• For Policiescovering more than one Insure Person,tests shall be done
for each Insured Person basis which such reduction in loading will be
applicable on individual Renewal Premium.
• Medical Underwriting loading will be discounted only on Renewal of
Policy with Us
• Discount on Medical Underwriting loading under this cover is applicable
only on next Renewal and cannot be utilized if Policyis not renewed
with Us.
3. Wellness services:
The services listed below are available to all Insured Person through
Our Network Provider on Ourmy: health mobile apponly.
i. Health Coach:
An Insured Person will have access to Health Coaching services in
areas such as:
• Disease management
• Activity and tness
• Nutrition
• Weight management.
These services will be available through Our my: health mobile app
as a chat service or as a call back facility.
ii. Wellness services
• Discounts: on OPD, Pharmaceuticals, pharmacy, diagnostic centers.
• Customer Engagement: Monthly newsletters, Diet consultation,
health tips
• Specialized programs: like stress management, Pregnancy Care,
Work life balance management
These services will be available through Our my: health mobile app
Disclaimer applicable to my: health Mobile app and associated
services
It is agreed and understood that Our my:health mobile app and Wellness
services are not providing and shall not be deemed to be providing any
Medical Advice, they shall only provide a suggestion for the Insured
Person’s consideration and it is the Insured Person’s sole and absolute
choice to follow the suggestion for any health related advice. We do
not assume any liability towards any loss or damage arising out of
or in relation to any opinion, actual or alleged errors, omissions and
representations suggested under this benet.
Section C. Renewal Benet
1. Preventive Health Check Up
Insured Person will be entitled for Preventive Health Check-up
onRenewal of the Policy with Us, at our Network Diagnostic centers
or hospitals in accordance to r list of tests, eligibility criteria and waiting
period as specied below:
Health Checkup- on each Policy Renewal
Age / Expiring
Policy Sum
Insured
1 Lac to
10Lacs
11 Lacs to
50 Lacs
Above
50 Lacs
18 to 40 Years Set 1 Set 1, Thyroid,
USG abdomen
and pelvis
Set 1, Thyroid , USG
abdomen and pelvis,
Lipid Prole, Renal
Prole
41 Yrs and
Above
Set 1,
Sr Creat
Set 1,SrCreat,
Thyroid, USG
abdomen and
pelvis
Set 1, Thyroid, USG
abdomen and pelvis,
Lipid Prole,Renal
prole, ECG
Set 1 -Comprises of, Complete Blood Count, Urine R,FBS,Sr Cholesterol
Health Checkup – Additional Tests
Age Gender Type of Test Waiting Period
Sum
Insured
Below
40 years
Female PAP Smear &
Mammography
Once in two
years
All Sum
Insured
Male PSA
Above
40 years
Female PAP Smear &
Mammography
Once in four
years
All Sum
Insured
Male PSA
Other terms and Conditions applicable to this Benet
• This benet will not be carried forward if not utilized within 60 days of
RenewalPolicy Inception date.
• Eligibility to avail Health Check-up will be in accordance to expiring
Policy Sum Insured.
• The test reports received under this benet shall not be utilized for
re-underwriting the Policy
Procedure for availing this benet
i. Insured personwill be intimated to undergo the health check-up at
our Network Provider, through Our my: health App.
ii. Test reports from our Network Provider will be made available to
You on Our my: health App
iii. You havethe option to avail this benet at our Network Provider
through Phone/Email or other modes of communication available
time to time.
Section D. Optional Covers
Insuring Clause
In consideration of payment of additional Premium by You, We will
provide insurance to the Insured Person(s)under below listed Covers,
up toSum Insuredor limits mentioned on the Schedule of Coverage
in the Policy Schedule.These Covers are optional and applicable
only if opted for.
1. Pre Diagnosis Cover
If a Claim is admissible under Section I2A I or I2A II as opted, We will pay
the expenses incurred towards diagnostic tests/ procedures incurred up
to 30 days priorto the diagnosis of such Critical Illness or Undergoing
of such Surgical Procedure.
Indicative list of Procedures covered
Sr.
No.
List of Diagnostic tests/ Procedures
1 Renal/Cardiac Angiogram.
2 Intravenous Pyelogram.
3 Ultrasonagraphy.
4 Ultrasound Guided FNAC.
5 Colour Doppler.
6 Mammography.

12
Sr.
No.
List of Diagnostic tests/ Procedures
7 CT Scan.
8 MRI Scan.
9 Treadmill Test ECHO.
10 Cardiogram.
11 Electrophysiology.
12 Endoscopic Procedures.
13 Special Radiological Procedures such as barium meal
investigations
14 Arthrogram, ERCP, Intravenous Urogram, Cystourethrogram,
15 Nephrostogram.
16 Special Blood Investigations such as Assay of Various Blood
Factors.
17 Virology Markers, Complete Coagulation Work up
2. Post Diagnosis Support
a. Second Medical Opinion
We will pay expenses incurred towards second Medical Opinion availed
from Medical Practitionerin respect of Critical Illness/Surgical
Procedurefor which Claim is admissible under the Policy.
b. Molecular Gene Expression Proling Test
We will pay the expenses incurred towards the expenses for Molecular
Gene Expression Proling Test for Treatment Guidance on diagnosis
of any Major stage Cancer for which Claim is admissible under Section
I2A I.1or I2A II.1, Cancer Cover as opted. The benet under this cover
can be availed only once during lifetime of the Policy.
c. Post Diagnosis Assistance
We will paySum Insuredtowardsoutpatient counseling required upon
diagnosis ofCritical Illnessesand Surgical Proceduresfor which Claim
is admissible under Section I2 A I or I2A II as opted. The Cover is subject
to maximum number of sessions as specied on Schedule of Coverage.
Applicability of Cover (Applicable to a. and c.)
Section I 2A I – if Base Coverage is opted under Section I2A I, the
Claim under this cover is admissible only once in life time of the Policy
Section I 2 A II – if Base Coverage is opted under Section I2A II, the
Claim under this cover is admissible after every admissible Claim
under the Policy
3. Loss of Job
We will pay Sum Insured if Insured Person suffers from Loss of Job
due to his/her Voluntary Resignation or Termination from the employment
within six months of diagnosis of any of the Major stage Critical Illnesses
or undergoing any of the Major stage Surgical Proceduresfor which
Claim is admissible under Section I2A I or I2A II of the Policy.
SECTION 3: MY:HEALTH MEDISURE SUPER TOP UP
INSURANCE
If during the PolicyPeriod, You suffer from any illness or accident which
requires Hospitalization as an inpatient, We will reimburse the amount
of such Medical Expenses as per the benets given below, in excess of
Aggregate Deductible and subject to a maximum of the Sum Insured
as stated in the Schedule.
1. In-patient Hospitalization Expenses:
If any Insured Person suffers an Illness or Accident during the Policy
Period requiring Inpatient Hospitalization, We will pay the Medical
Expenses incurred for
1.1 Room Rent/ Boarding & Nursing;
1.2 ICU Rent/Boarding & Nursing;
1.3 Fees of Surgeon, Anesthetist, Nurses and Specialists;
1.4 Cost of Operation Theatre, diagnostic tests, medicines, blood, oxygen
and cost of prosthetic and other devices or equipment if implanted
internally like pacemaker during a surgical procedure.
Occurrence of same illness after a lapse of 45 days will be considered
as fresh illness for the purpose of this Policy
2. Pre-Hospitalization Medical Expenses –
The Medical Expenses incurred in the 30 days immediately before You
were Hospitalized, provided that:
i. Such Medical Expenses were in fact incurred for the same condition
requiring subsequent Hospitalization, and;
ii. We have accepted the Claim under Scope of Cover 1 “In-patient
Hospitalization expenses”.
3. Post Hospitalization Medical Expenses –
The Medical Expenses incurred in the 60 days immediately after You
were discharged, provided that:
i. Such Medical Expenses were in fact incurred for the same condition
for which Your Hospitalization was required, and;
ii. We have accepted the Claim under Scope of Cover 1, “In-patient
Hospitalization expenses”.
3. Post Hospitalization Medical Expenses –
The Medical Expenses incurred in the 60 days immediately after You
were discharged, provided that:
i. Such Medical Expenses were in fact incurred for the same condition
for which Your Hospitalization was required, and;
ii. We have accepted the Claim under Scope of Cover 1, “In-patient
Hospitalization expenses”.
4. Day Care treatment –
The Medical Expenses for a day care treatment where the procedure
or surgery
- is undertaken is under General or Local Anaesthesia in a Hospital/
Day care centre for less than 24 hours because of technological
advancement, and
- which would have otherwise required hospitalization of more than
24 hours
- does not cover any treatment in an outpatient department or diagnostic
procedures.
Please refer annexure 1 at the end of this document for indicative list
of covered Day Care treatments
SECTION 4: MY:HEALTH HOSPITAL CASH BENEFIT
ADD ON
Section I. 4. A: Coverage
1. Hospital Cash Benet
We will pay Sum Insured on Medically NecessaryHospitalization
of an Insured Persondue to Illnessor Injurysustained or contracted
during the Policy Period. The payment is subject to per day benet Sum
Insuredas specied on the Schedule of Coverage in the Policy Schedule
for up to maximum of 30 days.
2. Companion Benet:
We will pay additional amount upto the limit specied on the Schedule of
Coverage in the Policy Schedule towards expenses of an accompanying
person during Hospitalizationfor up to maximum of 30 days.
Section I. 4 B: Optional Cover
Insuring Clause
In consideration of payment of additional Premium, it is hereby declared
and agreed that We will pay under below listed Cover subject to all other
terms, conditions, exclusions and waiting periods applicable to the add
on and Policy on which this add on is attached.
The Cover is optional and applicable only if opted for and up to the
Sum Insured or limits mentioned on the Schedule of Coverage in the
Policy Schedule.

13
1. Hospital Cash benet - Global
On availing this option, Wewill pay Sum Insured on Medically
NecessaryHospitalization of an Insured Personoutside India due
to Illnessor Injurysustained or contracted during the Policy Period.
2. Waiting period Modication Option
On availing this option, Waiting Periods listed under Section III
a 1: Waiting Periods will stand modied as mentioned in Schedule of
Coverage on the Policy Schedule.
All other terms and Conditions of the respective Section and Policy
shall remain unaltered.
Section C: Renewal Benets
A. Fitness discount @ Renewal
Insured Person can avail discount on Renewal Premium by accumulating
Healthy Weeks as per table given below.
One Healthy Week can be accumulated by;
• Recording minimum 50,000 steps in a week subject to maximum 15,000
steps per day, tracked through Your wearable device linked to Ourmy:
health mobile appandYourPolicy number
OR
• burning total of 900 calories upto maximum of 300 calories in one
exercise session per day, tracked Your wearable device linked to Ourmy:
health mobile appandYourPolicy number
• Fitness discount @ Renewal is applicable for Adult Insured Persons
only. Any Person covered as Child Dependent, irrespective of the Age
is excluded
Healthy Weeks Discounts
No. of Healthy Weeks
Accumulated
Discount on Renewal
Premium
01-04 0.50%
05-08 1.00%
09-12 2.00%
13-16 3.00%
17-26 6.00%
27-36 7.50%
Above 36 10.00%
Steps to accumulate Healthy Weeks
Step 1 - The my: Health App must be downloaded on the mobile.
• Step 2 - You can start accumulating Healthy Weeks by tracking physical
activity trough the Wearable device linkedto Ourmy: health mobile
appandYourPolicy number
We encourage and recognize all types of exercise/tness activities
by making use of wearable devices to track and record the activities
Insured Person engages in.
Application of Fitness discount @ Renewal
• Annual Policy: Discount amount accrued based on Number of
accumulated Healthy Weeks during the expiring Policy year will be
applied on the Renewal Premium for expiring Policy Sum Insured.
• Multi Year Policy:
o Fitness discount earned on yearly basis will be accumulated till
Policy End date.
o On Renewal of the Policy, total discount amount accrued each year
will be applied on Renewal Premium of subsequent year.
• For Policiescovering more than one Insure Person,Healthy Weeks for
each Insured Person will be tracked andaccumulated. Such discount
will be applicable on individual Renewal Premium for both Individual
and Floater Sum Insured basis Policies.
• Premium will be discounted to the extent applicable to terms
corresponding to expiring Policy.
• In case of Increase in Sum Insured at Renewal, discount amount
will be applied on the Sum Insured applicable under expiring Policy.
• Fitness discount @ Renewal will be applied only on Renewal of
Policy with Us.
B. Health Incentive
This Program encourages Insured Persons to maintain good health and
avail incentives as listed below.
Under this Program, Insured Personhaving Pre-Existing Diseasesor
Obesity (BMI above 30) as listed under table A below, will be eligible for
reduction in Medical Underwriting Loading applied from rst inception
of the Policy with Us provided that;
i. Insured Person shall undergomedical tests and/or BMIcheck-upas
listed belowminimum 3 months prior to expiry of Policy Year (For
Multiyear Policies) or before Renewal (For Annual Policies).
ii. Medical test shall be done at Your own cost through our Network
Provider on my:Health mobile App.
iii. If the test parameters are within normal limits, We will apply 50%
discount on the Medical Underwriting loading applied for corresponding
Pre-Existing Diseaseor Obesity as applicableon Renewal of the
Policy with Us.
iv. If the test parameters at subsequent renewal are not within normal
limits or Medical test reports are not submitted in accordance with i
and ii above, the discount amount applied on Medical Underwriting
loading will be zero
v. The test reports received to avail the health incentive benet shall not
be utilised for re underwriting the policy
Table A
Pre-existing Diseases Test
Diabetes HbA1c
Hypertension Blood Pressure reading
Hyperlipidemia Total Cholesterol
Cardiovascular Diseases ECG
Hypothyroidism Thyroid function tests
Obesity BMI
Application of Health Incentive
• Annual Policy: Discount amount accrued during the expiring Policy
year will be applied on the Renewal Premium for expiring Policy Sum
Insured.
• Multi Year Policy:
o Discount amount earned on yearly basis will be accumulated till
Policy End date.
o On Renewal of the Policy, total discount amount accrued each year
will be applied on Renewal Premium of subsequent year.
• For Policiescovering more than one Insure Person,testsshall be done
for each Insured Person basis which such reduction in loading will be
applicable on individual RenewalPremium for both Individual and Floater
Sum Insured basis Policies.
• Discount on Medical Underwriting loading under this cover is
applicable only on next Renewal and cannot be utilized if Policy not
renewed with us.
C. Wellness services:
The services listed below are available to all Insured persons through
Our Network Provider on Our mobile application only. Availing of
services under this Section will not impact the Sum Insured or the
eligibility for Cumulative Bonus.
i. Health Coach:
An Insured Person will have access to Health Coaching services in
areas such as:
• Disease management
• Activity and tness
• Nutrition
• Weight management.

14
These services will be available through Our mobile application as a
chat service or as a call back facility.
ii. Online Wellness services
• Discounts: on OPD, Pharmaceuticals,pharmacy, , diagnostic centres
etc.
• Customer Engagement: Monthly newsletters, Diet consultation,
health tips
• Specialized programs: like stress management, Pregnancy Care,
Work life balance management etc.
Disclaimer applicable to my: health Mobile app and associated
services
It is agreed and understood that Our my:health mobile app and Wellness
services are not providing and shall not be deemed to be providing any
Medical Advice, they shall only provide a suggestion for the Insured
Person’s consideration and it is the Insured Person’s sole and absolute
choice to follow the suggestion for any health related advice. We do
not assume any liability towards any loss or damage arising out of
or in relation to any opinion, actual or alleged errors, omissions and
representations suggested under this benet.
SECTION 5: PERSONAL ACCIDENT INSURANCE
1. Accidental Death
If during the Period of Insurance an Insured Person sustains Bodily
Injury which directly and independently of all other causes results
in Death within twelve (12) months of the Date of Loss, then the
Company agrees to pay to the Insured Person’s Beneciary or legal
representative the Compensation stated in the Schedule.
Specic Extensions
1) Disappearance: In the event of the disappearance of the Insured
Person, following a forced landing, stranding, sinking or wrecking of a
conveyance in which such Insured Person was known to have been
travelling as an occupant, it shall be deemed after twelve (12) months,
subject to all other terms and conditions of this Policy, that such Insured
Person shall have died as the result of an Accident. If at any time,
after the payment of the Accidental death benet, it is discovered that
the Insured Person is still alive; all payments shall be reimbursed in
full to the Company.
2) Exposure: Death as a direct result of exposure to the elements shall
be deemed to be Bodily Injury.
Specic Conditions
If applicable and if payment has been made under the Permanent
Disablement Section, any amounts paid under that Section would be
deducted from payment of a claim under this Section of the Policy.
2. Permanent Disablement
If during the Period of Insurance an Insured Person sustains Bodily
Injury which directly and independently of all other causes results in
disablement within twelve (12) months of the Date of Loss, then the
Company agrees to pay to the Insured Person the Compensation
stated in the specic Table of Benets below, which is shown as the Table
of Benets in the Schedule. The Deductible or Franchise, if applicable,
shall be deducted from the Compensation payable.
Specic Extensions
Exposure: Permanent disablement as a direct result of exposure to the
elements shall be deemed to be Bodily Injury.
Specic Provisions
1) Ankylosis of the ngers (other than thumb and forenger) and of the
toes (other than the big toe) shall be limited to fty percent (50%) of the
Compensation payable for the loss of the said members.
2) Any benet payable under item 23 of Table (C) shall be at the complete
discretion of the Company taking into consideration the nature of the
Bodily Injury in conjunction with the stated Compensation percentages
for more specic injuries shown in the Table of Benets.
Specic Conditions
1) The insurance shall terminate for an Insured Person under this
Section upon payment of a benet equal to the Total Sum Insured.
2) The total amount payable in respect of more than one disablement
due to the same Accident is arrived at by adding together the various
percentages shown in the Table of Benets, but shall not exceed the
Total Sum Insured.
3) The Deductible or Franchise, if applicable, shall apply to the total
amount payable, irrespective of the number of benets an Insured
Person is entitled to.
4) If an Insured Person dies as the result of the Bodily Injury any
amount claimed and paid to an Insured Person under the Permanent
Disablement Section will be deducted from any payment under the
Accidental Death Section.
Specic Denitions for all Tables of Benets
1) Limb means the hand above the wrist joint or foot above the ankle
joint.
2) Loss of Hearing means the total and irrecoverable Loss of Hearing.
3) Loss of Mastication means the total and irrecoverable loss of ability
to chew food.
4) Loss of Sight means the total and irrecoverable Loss of Sight. This
is considered to have occurred if the degree of sight remaining after
correction is 3 / 60 or less on the Snellen Scale.
5) Loss of Speech means the total and irrecoverable Loss of Speech.
Specic Denitions for Table (A)
Loss used with reference to Limb means the loss by physical severance
of such Limb.
Specic Denitions for Table (B)
Loss used with reference to Limb means the loss by physical severance
or the total and permanent loss of use of such Limb.
Specic Denitions for Table (C) and (D)
Loss used with reference to Limb and / or ngers, thumbs or toes,
means the loss by physical severance or the total and permanent loss
of use of said member.
TABLE OF BENEFITS – TABLE (A)
The Disablement
Compensation
Expressed as a
Percentage of Total
Sum Insured
1) Permanent Total Disablement 100%
2) Permanent and incurable insanity 100%
3) Permanent Total Loss of two Limbs 100%
4) Permanent Total Loss of Sight in
both eyes
100%
5) Permanent Total Loss of Sight of one
eye and one Limb
100%
6) Permanent Total Loss of Speech 100%
7) Complete removal of the lower jaw 100%
8) Permanent Total Loss of Mastication 100%
9) Permanent Total Loss of the central
nervous system or the thorax and
all abdominal organs resulting in the
complete inability to engage in any
job and the inability to carry out Daily
Activities essential to life without full
time assistance
100%
10) Permanent Total Loss of Hearing in
both ears
75%
11) Permanent Total Loss of one Limb 50%
12) Permanent Total Loss of Sight of
one eye
50%
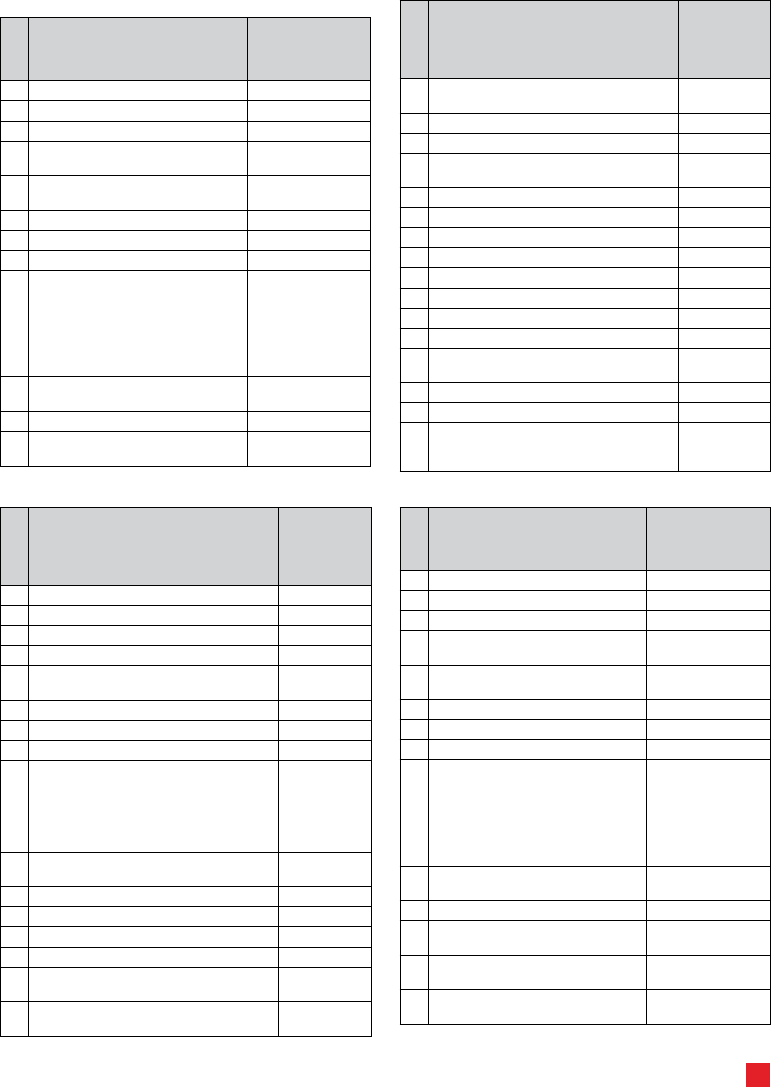
15
TABLE OF BENEFITS – TABLE (B)
The Disablement
Compensation
Expressed as a
Percentage of Total
Sum Insured
1) Permanent Total Disablement 100%
2) Permanent and incurable insanity 100%
3) Permanent Total Loss of two Limbs 100%
4) Permanent Total Loss of Sight in
both eyes
100%
5) Permanent Total Loss of Sight of one
eye and one Limb
100%
6) Permanent Total Loss of Speech 100%
7) Complete removal of the lower jaw 100%
8) Permanent Total Loss of Mastication 100%
9) Permanent Total Loss of the central
nervous system or the thorax and
all abdominal organs resulting in the
complete inability to engage in any
job and the inability to carry out Daily
Activities essential to life without full
time assistance
100%
10) Permanent Total Loss of Hearing in
both ears
75%
11) Permanent Total Loss of one Limb 50%
12) Permanent Total Loss of Sight of
one eye
50%
TABLE OF BENEFITS – TABLE (C)
The Disablement
Compensation
Expressed as
a Percentage
of Total Sum
Insured
1) Permanent Total Disablement 100%
2) Permanent and incurable insanity 100%
3) Permanent Total Loss of two Limbs 100%
4) Permanent Total Loss of Sight in both eyes 100%
5) Permanent Total Loss of Sight of one eye
and one Limb
100%
6) Permanent Total Loss of Speech 100%
7) Complete removal of the lower jaw 100%
8) Permanent Total Loss of Mastication 100%
9) Permanent Total Loss of the central nervous
system or the thorax and all abdominal
organs resulting in the complete inability to
engage in any job and the inability to carry
out Daily Activities essential to life without
full time assistance
100%
10) Permanent Total Loss of Hearing in both
ears
75%
11) Permanent Total Loss of one Limb 50%
12) Permanent Total Loss of Sight of one eye 50%
13) Permanent Total Loss of Hearing in one ear 15%
14) Permanent Total Loss of the lens in one eye 25%
15) Permanent Total Loss of use of four ngers
and thumb of either hand
40%
16) Permanent Total Loss of use of four ngers
of either hand
20%
The Disablement
Compensation
Expressed as
a Percentage
of Total Sum
Insured
17) Permanent Total Loss of use of one thumb
of either hand:
a) Both joints 20%
b) One joint 10%
18) Permanent Total Loss of one nger of either
hand:
a) Three joints 5%
b) Two joints 3.5%
c) One joint 2%
19) Permanent Total Loss of use of toes:
a) All – one foot 15%
b) Big – both joints 5%
c) Big – one joint 2%
d) Other than Big – each toe 2%
20) Established non-union of fractured leg or
kneecap
10%
21) Shortening of leg by at least 5 cms. 7.50%
22) Ankylosis of the elbow, hip or knee 20%
23) Permanent disablement not otherwise
provided for under Items 2-22 inclusive up to
a maximum of
75%
TABLE OF BENEFITS – TABLE (D)
The Disablement
Compensation
Expressed as a
Percentage of Total
Sum Insured
1) Permanent Total Disablement 100%
2) Permanent and incurable insanity 100%
3) Permanent Total Loss of two Limbs 100%
4) Permanent Total Loss of Sight in
both eyes
100%
5) Permanent Total Loss of Sight of one
eye and one Limb
100%
6) Permanent Total Loss of Speech 100%
7) Complete removal of the lower jaw 100%
8) Permanent Total Loss of Mastication 100%
9) Permanent Total Loss of the central
nervous system or the thorax and
all abdominal organs resulting in the
complete inability to engage in any
job and the inability to carry out Daily
Activities essential to life without full
time assistance
100%
10) Permanent Total Loss of Hearing in
both ears
75%
11) Permanent Total Loss of one Limb 50%
12) Permanent Total Loss of Sight of
one eye
50%
13) Permanent Total Loss of Hearing in
one ear
15%
14) Permanent Total Loss of the lens in
one eye
25%

16
The Disablement
Compensation
Expressed as a
Percentage of Total
Sum Insured
15) Permanent Total Loss of use of four
ngers and thumb of either hand
40%
16) Permanent Total Loss of use of four
ngers of either hand
20%
17) Permanent Total Loss of use of one
thumb of either hand:
a) Both joints 20%
b) One joint 10%
18) Permanent Total Loss of one nger of
either hand:
a) Three joints 5%
b) Two joints 3.5%
c) One joint 2%
19) Permanent Total Loss of use of toes:
a) All – one foot 15%
b) Big – both joints 5%
c) Big – one joint 2%
d) Other than Big – each toe 2%
20) Established non-union of fractured leg
or kneecap
10%
21) Shortening of leg by at least 5 cms. 7.50%
22) Ankylosis of the elbow, hip or knee 20%
3. In-Hospital Medical Expenses – Accident Only
If, during the Period of Insurance, an Insured Person sustains Bodily
Injury and is hospitalized as an in-patient for twenty-four (24) continuous
hours or more, then the Company will reimburse the Insured Person
the necessary Usual and Reasonable In-Hospital Medical Expenses,
incurred within twelve (12) months from the Date of Loss up to the
Total Sum Insured stated in the Schedule, subject to the Terms and
Conditions of this Policy. The Deductible or Franchise, if applicable,
shall be deducted from the Compensation payable.
Specic Conditions
1) Usual and Reasonable In-Hospital Medical Expenses shall include
and be limited to the following services:
a) charges for semi private Hospital room and board, use of the
operating room, emergency room, and Ambulatory Medical Centre
b) fees of Physicians.
c) charges for laboratory tests, ambulance service (to or from the
Hospital), prescription medicines or drugs, therapeutics, anaesthetics
(including administration of anaesthetics), transfusions, articial Limbs
or eyes (excluding repair or replacement of these items), x-rays,
prosthetic appliances.
d) charges for a registered nurse (R.N).
2) If an Insured Person has other insurance against a loss covered by
this Section, then the Company shall not be liable for a greater proportion
of the loss than the applicable benet under this Section bears to the
total applicable benet under all such insurance.
Specic Denitions
1) Ambulatory Medical Centre means a licensed facility providing
ambulatory surgical or medical treatment, other than a Hospital, clinic
or Physician’s ofce.
2) Usual and Reasonable In-Hospital Medical Expenses means
fees and prices generally charged in the locality where performed for
medically necessary services and supplies required for treatment of
cases of comparable severity and nature, but not to include charges
that would not have been made if no insurance existed.
Specic Exclusions
The Company shall not be liable to pay any benet in respect of any
Insured Person for:
1) Any Usual and Reasonable In-Hospital Medical Expenses before
the Period of Insurance.
2) any dental work.
3) any claim caused by or arising from or due to Sickness of any and
every kind.
4. Emergency Medical Expenses – Accident Only
If, during the Period of Insurance, an Insured Person sustains Bodily
Injury, then the Company will reimburse the Insured Person the
necessary Usual and Reasonable Medical Expenses, incurred within
twelve (12) months from the Date of Loss up to the Sum Insured stated
in the Schedule, subject to the Terms and Conditions of this Policy. The
Deductible or Franchise, if applicable, shall be deducted from the
Compensation payable.
Specic Conditions
1) Medical Expenses shall include and be limited to the following
services:
a) charges for semi-private Hospital room and board, use of the
operating room, emergency room, and Ambulatory Medical Centre.
b) fees of Physicians.
c) Medical Expenses, in or out of Hospital, including: laboratory tests,
ambulance service (to or from the Hospital), prescription medicines
or drugs, therapeutics, anaesthetics (including administration of
anaesthetics), transfusions, articial Limbs or eyes (excluding repair or
replacement of these items), x-rays, prosthetic appliances.
d) charges for a registered nurse (R.N).
2) If an Insured Person has other insurance against a loss covered by
this Section, then the Company shall not be liable for a greater proportion
of the loss than the applicable benet under this Section bears to the
total applicable benet under all such insurance.
Specic Denitions
1) Ambulatory Medical Centre means a licensed facility providing
ambulatory surgical or medical treatment, other than a Hospital, clinic
or Physician’ s ofce.
2) Usual and Reasonable Medical Expenses means fees and
prices generally charged in the locality where performed for medically
necessary services and supplies required for treatment of cases of
comparable severity and nature, but not to include charges that would
not have been made if no insurance existed.
Specic Exclusions
The Company shall not be liable to pay any benet in respect of any
Insured Person for:
1) AnyMedical Expenses incurred where an Insured Journey is
undertaken against the advice of a qualied licensed medical practitioner.
2) AnyMedical Expenses incurred when the specic purpose of a
journey is to receive medical treatment or advice.
3) AnyMedical Expenses incurred within the territorial limits that are
not stated in the Schedule.
4) any medical treatment, drugs or medicines, prescribed or applied,
before the Period of Insurance.
5) any dental work.
6) any claim caused by or arising from or due to Sickness of any and
every kind.
5. Emergency Medical Expenses
If, during the Period of Insurance, an Insured Person sustains
Bodily Injury or sudden unexpected Sickness, then the Company will
reimburse the Insured Person the necessary Usual and Reasonable
Medical Expenses, incurred within twelve (12) months from the Date
of Loss up to the Sum Insured stated in the Schedule. The Deductible
or Franchise, if applicable, shall be deducted from the Compensation
payable.

17
Specic Conditions
1) Medical Expenses shall include and be limited to the following
services:
a) charges for semi-private Hospital room and board, use of the
operating room, emergency room, and Ambulatory Medical Centre.
b) fees of Physicians.
c) Medical Expenses, in or out of Hospital, including: laboratory tests,
ambulance service (to or from the Hospital), prescription medicines
or drugs, therapeutics, anaesthetics (including administration of
anaesthetics), transfusions, articial Limbs or eyes (excluding repair or
replacement of these items), x-rays, prosthetic appliances.
d) charges for a registered nurse (R.N).
2) If an Insured Person has other insurance against a loss covered by
this Section, then the Company shall not be liable for a greater proportion
of the loss than the applicable benet under this Section bears to the
total applicable benet under all such insurance.
Specic Denitions
1) Ambulatory Medical Centre means a licensed facility providing
ambulatory surgical or medical treatment, other than a Hospital, clinic
or Physician’ s ofce.
2) Usual and Reasonable Medical Expenses means fees and
prices generally charged in the locality where performed for medically
necessary services and supplies required for treatment of cases of
comparable severity and nature, but not to include charges that would
not have been made if no insurance existed.
Specic Exclusions
The Company shall not be liable to pay any benet in respect of any
Insured Person for:
1) AnyMedical Expenses incurred where an Insured Journey is
undertaken against the advice of a qualied licensed medical practitioner.
2) AnyMedical Expenses incurred when the specic purpose of a
journey is to receive medical treatment or advice.
3) AnyMedical Expenses incurred within the territorial limits that are
not stated in the Schedule.
4) any medical treatment, drugs or medicines, prescribed or applied,
before the Period of Insurance.
any dental work.
6. Hospital Cash – Accident Only
If during the Period of Insurance an Insured Person sustains Bodily
Injury which directly and independently of all other causes results in
the Insured Person being in a Hospital as an inpatient within one (1)
calendar month of the Date of Loss, then the Company agrees to pay
to the Insured Person the Daily Benet stated in the Schedule. The
Deductible or Franchise, if applicable, shall be deducted from the
Compensation payable.
Specic Provisions
In case of successive Hospital stays with less than sixty (60) Days
between each one for a same cause, the Deductible or Franchise will
only apply once, as the Hospital stays will be deemed as one event.
Special Conditions
Once the Company has paid the Daily Benet up to the maximum
number of Days stated in the Schedule, cover under this Section will
cease for such Insured Person.
7. Hospital Cash & Home Convalescence – Accident Only
If during the Period of Insurance an Insured Person sustains Bodily
Injury which directly and independently of all other causes results in
the Insured Person being in a Hospital as an inpatient within one (1)
calendar month of the Date of Loss, then the Company agrees to pay
to the Insured Person the Daily Benet stated in the Schedule. In
addition, if the Insured Person is instructed by a Physician to complete
his/her recovery at home, then the Company will pay the Daily Home
Allowance stated in the Schedule. The Deductible or Franchise, if
applicable, shall be deducted from the Compensation payable.
Specic Provisions
In case of successive Hospital stays with less than sixty (60) Days
between each one for a same cause, the Deductible or Franchise will
only apply once, as the Hospital stays will be deemed as one event.
Specic Conditions
1) The Daily Home Allowance will be limited to the maximum number
of Days an Insured Person was in Hospital as an in-patient or the
maximum number of Days stated in the Schedule, whichever is the
lesser.
2) Once the Company has paid the Daily Benet and Daily Home
Allowance up to the maximum number of Days stated in the Schedule,
cover under this Section will cease for such Insured Person.
8. Hospital Cash – Accident & Sickness
If during the Period of Insurance an Insured Person sustains Bodily
Injury or Sickness which directly and independently of all other causes
results in the Insured Person being in a Hospital as an in-patient within
one (1) calendar month of the Date of Loss, then the Company agrees
to pay to the Insured Person the Daily Benet stated in the Schedule.
The Deductible or Franchise, if applicable, shall be deducted from the
Compensation payable.
Specic Provisions
In case of successive Hospital stays with less than sixty (60) Days
between each one for a same cause, the Deductible or Franchise will
only apply once, as the Hospital stays will be deemed as one event.
Specic Conditions
Once the Company has paid the daily benet up to the maximum number
of Days stated in the Schedule, cover under this Section will ease for
such Insured Person.
9. Hospital Cash & Home Convalescence – Accident & Sickness
If during the Period of Insurance an Insured Person sustains Bodily
Injury or Sickness which directly and independently of all other causes
results in the Insured Person being in a Hospital as an in-patient within
one (1) calendar month of the Date of Loss, then the Company agrees
to pay to the Insured Person the Daily Benet stated in the Schedule. In
addition, if the Insured Person is instructed by a Physician to complete
his/her recovery at home, then the Company will pay the Daily Home
Allowance stated in the Schedule. The Deductible or Franchise, if
applicable, shall be deducted from the Compensation payable.
Specic Provisions
In case of successive Hospital stays with less than sixty (60) Days
between each one for a same cause, the Deductible or Franchise will
only apply once, as the Hospital stays will be deemed as one event.
Specic Conditions
1) The Daily Home Allowance will be limited to the maximum number
of Days an Insured Person was in Hospital as an in-patient or the
maximum number of Days stated in the Schedule, whichever is the
lesser.
2) Once the Company has paid the Daily Benet and Daily Home
Allowance up to the maximum number of days stated in the Schedule,
cover under this Section will cease for such Insured Person.
10. Broken Bones
If during the Period of Insurance an Insured Person sustains Bodily
Injury which directly and independently of all other causes results in a
broken bone as specied in this Section, then the Company agrees to
pay to the Insured Person the Compensation stated in the Table of
Benets up to the Total Sum Insured in the Schedule. The Deductible
or Franchise, if applicable, shall be deducted from the Compensation
payable.

18
TABLE OF BENEFITS
Fracture
% of Sum
Insured
1) Fractures of the Skull:
a) Compound fracture with damage to the brain
tissue
100
b) Compound fracture without damage to the
brain tissue
75
c) All other fractures 50
2) Fractures of hip or pelvis (excluding thigh or
coccyx):
a) Multiple fractures (at least one compound &
one complete)
100
b) All other compound fractures 50
c) Multiple fractures, at least one complete 30
d) All other fractures 20
3) Fracture of thigh or heel:
a) Multiple fractures (at least one compound &
one complete)
50
b) All other compound fractures 40
c) Multiple fractures, at least one completed) 30
All other fractures 20
4) Fracture of Lower Leg, Clavicle, Ankle, Elbow,
Upper or Lower Arm (including wrist, but
excluding Colles-type fracture):
a) Multiple fractures (at least one compound &
one complete)
b) All other compound fractures
c) Multiple fractures, at least one complete
d) All other fractures 40302012
5) Fractures of Lower Jaw:
a) Multiple fractures (at least one compound &
one complete)
b) All other compound fractures
c) Multiple fractures, at least one complete
d) All other fractures 3020168
6) Fractures of Shoulder Blade, Kneecap, Sternum,
Hand (excluding ngers and wrist), Foot
(excluding toes and heel):
a) All compound fractures
b) All other fractures 2010
7) Colles type fracture to the Lower Arm:
a) Compound 20
b) Other 10
8) Fractures of Spinal Column (Vertebrae but
excluding coccyx):
a) All compression fractures 20
b) All spinous, transverse process or pedicle
fractures
20
c) All other vertebral fractures 10
9) Fractures of Rib or Ribs, Cheekbone, Coccyx,
Upper Jaw, Nose, Toe and toes, nger or ngers:
a) Multiple fractures (at least one compound &
one complete)
16
b) All other compound fractures 12
c) Multiple fractures, at least one complete 8
d) All other fractures 4
Specic Conditions
1) No benet will be paid before any fracture is recognized medically
and a Physician has established the extent and nature of the fracture.
2) The total amount payable under this Section, in respect of more
than one fracture due to the same Bodily Injury, will be calculated
by adding the various benets together, but shall not exceed the Total
Sum Insured.
3) In the event that an Insured Person has received a benet under this
Section, and the same Bodily Injury results in permanent disablement,
any benets paid under this Section will be deducted from the Permanent
Disablement benet
11. Burns
If during the Period of Insurance an Insured Person sustains Bodily
Injury whilst on a Common Carrier which directly and independently
of all other causes results in second or third degree burns, then the
Company agrees to pay to the Insured Person the Compensation
stated in the Table of Benets up to the Total Sum Insured in the
Schedule. The Deductible or Franchise, if applicable, shall be deducted
from the Compensation payable.
TABLE OF BENEFITS
Description
Percentage
of Total Sum
Insured
1) Head a) Third degree burns of 8% or
more of the total head surface
area
100%
b) Second degree burns of 8%
or more of the total head surface
area
50%
c) Third degree burns of 5% or
more, but less than 8% of the total
head surface area
80%
d) Second degree burns of 5% or
more, but less than 8% of the total
head surface area
40%
e) Third degree burns of 2% or
more, but less than 5% of the total
head surface area
60%
f) Second degree burns of 2% or
more, but less than 5% of the total
head surface area
30%
2) Rest of
Body
a) Third degree burns of 20% or
more of the total body surface
area
100%
b) Second degree burns of 20%
or more of the total body surface
area
50%
c) Third degree burns of 15% or
more, but less than 20% of the
total body surface area
80%
d) Second degree burns of 15%
or more, but less than 20% of the
total body surface area
40%
e) Third degree burns of 10% or
more, but less than 15% of the
total body surface area
60%
f) Second degree burns of 10%
or more, but less than 15% of the
total body surface area
30%
g) Third degree burns of 5% or
more, but less than 10% of the
total body surface area
20%
h) Second degree burns of 5%
or more, but less than 10% of the
total body surface area
10%

19
Specic Conditions
1) If the Bodily Injury results in more than one of the Descriptions
above, then the Company shall be liable for the largest Description only.
2) If an Insured Person dies or is permanently disabled as the result
of the Bodily Injury, then any amount claimed and paid to an Insured
Person under this Section will be deducted from any payment made
under Accidental Death or Permanent Disablement.
12. Last Rites Costs – Accident & Sickness
If during the Period of Insurance an Insured Person sustains Bodily
Injury or Sickness which directly and independently of all other causes
results within one (1) calendar month of the Date of Loss in death, then
the Company agrees to pay to the Insured Person’s Beneciary or
legal representative the Compensation stated in the Schedule towards
the cost of the last rites of the Insured Person.
13. In Hospital Surgery Benet
If during the Period of Insurance an Insured Person is hospitalised
as the result of Bodily Injury or Sickness and is charged for a surgical
procedure, performed by a Physician, then the Company agrees to
pay an amount equal to the costs of the surgical procedure or the
amount stated in the Table of Benets as a percentage of the Total
Sum Insured stated in the Schedule, whichever is the lesser. The
Deductible or Franchise, if applicable, shall be deducted from the
Compensation payable.
Specic Conditions
1) Should there be more than one surgical procedure performed during
the same operative sessions, the Company shall be liable for the
largest procedure only.
2) Any surgical procedure not mentioned in the Table of Benets shall
be compensated at the complete discretion of the Company taking
into consideration the nature of the surgical procedure in conjunction
with the stated Compensation percentages for more specic surgical
procedures shown in the Table of Benets.
Specic Denitions
1) In-Patient means a person who is conned in a Hospital as a
resident patient and who is charged at least one (1) Day’s room and
board in the Hospital.
2) Invasive Surgery means any surgery that involves entering the
specic body cavity shown in the Table of Benets.
Specic Exclusions
The Company shall not be liable to pay any benet in respect of any
Insured Person for:
1) congenital anomalies and conditions arising there from.
2) pregnancy, childbirth, miscarriage or abortion or any female organs
disease.
3) anyHospital, surgical treatment or surgical procedure as the result of
Sickness within ninety (90) Days of the Policy Effective Date.
4) cosmetic or plastic surgery, except as the result of an Accident.
5) any infection occurring during In-Patient care.
6) anyHospital, surgical treatment or surgical procedure on adenoids or
tonsils within one hundred eighty (180) Days of the Policy Effective Date.
Table Of Benets
Description of surgical procedure
The Benet
Expressed as
a % of Sum
Insured
1) Abdomen
a) Two or more surgical procedures
performed through the same abdominal
incision will be considered as one operation.
i) Appendectomy 50
ii) Resection of bowel 70
iii) Resection of stomach 70
Description of surgical procedure
The Benet
Expressed as
a % of Sum
Insured
iv) Gastro-enterostomy 60
v) Removal of gall-bladder 70
vi) Laparotomy for diagnostic or treatment
purposes or the removal of one or more
organs, unless herein provided
50
vii) Laparoscopy for diagnostic or treatment
purposes
50
2) Abscess
a) Incision of supercial abscess, boil or
furuncle, one or more
50
b) Treatment of carbuncle or abscess
requiring a Hospital stay, one or more
10
3) Amputation Of
a) one nger or one toe 10
b) hand, forearm or foot at ankle 20
c) leg, arm or thigh 40
d) thigh at hip 70
4) Breast
a) Mastectomy of one or both, radical with
resection into axilla
70
b) Mastectomy one or both, partial 40
5) Chest
a) Complete thoracoplasty 100
b) Removal of lung or portion of lung 70
c) Thoracoscopy for diagnostic, or treatment
purposes
20
d) Bronchoscopy – diagnostic 10
e) Bronchoscopy - operative, excluding
biopsy
20
f) Cardiac surgery involving valvular
replacement
100
g) Cardiac surgery involving bypass surgery 75
h) Cardiac surgery involving angioplasty 50
6) Ear
a) Myringotomy 5
b) Mastoidectomy – radical – one side 50
c) Mastoidectomy – radical – both sides 60
d) Fenestration, one or both sides 100
7) Esophagus
a) Operation for stricture 40
b) Gastroscopy 10
8) Eye
a) Detached retina – multiple fusions 100
b) Cataract 50
c) Glaucoma 30
d) Removal of eyeball 30
e) Removal of pterygium 20
f) Incision of sty or chalazion
9) Fractures treatment of simple
a) For compound fractures the benet is
increased by 50%, but will not exceed the
Total Sum Insured in the Schedule.

20
Description of surgical procedure
The Benet
Expressed as
a % of Sum
Insured
b) For fractures requiring an open operation
including bone grafting or bone splicing,
the benet is increased by 100%, but will
not exceed the Total Sum Insured in the
Schedule.
i) Collar bone, shoulder blade, or forearm,
one bone
15
ii) Coccyx, tarsals, metatarsals or Talar bone 10
iii) Thigh 40
iv) Upper arm or leg 25
v) Fingers or toes, each, or rib 5
vi) Forearm – two bones, knee cap, or pelvis
not requiring traction
20
vii) Leg, two bones 30
viii) Jaw, lower 20
ix) Carpals, metacarpals, nose, ribs (two or
more) or Sternum
10
x) Pelvis, requiring traction 30
xi) Vertebrae, transverse processes, each 5
xii) Vertebrae, compression fracture, one
or more
40
xiii) Wrist 10
10) Genito – Urinary Tract
a) Removal of kidney 70
b) Fixation of kidney 70
c) Laparotomy for diagnostic or treatment
purposes of tumours or stones in kidney,
urethra, or bladder by Invasive Surgery
60
d) Laparotomy for diagnostic or treatment
purposes or the removal of tumours or
stones in kidney, urethra, or bladder
by cauterisation, endoscopic means or
lithotripsy
20
e) Stricture or urethra – open operation 30
f) intra-urethral by Invasive Surgery 15
g) Prostrate entire removal of open
operation – complete procedure
70
h) Prostrate partial removal – by endoscopic
means
25
i) Prostrate by other cutting operation 50
j) Orchidectomy or epididymectomy 25
k) Hydrocele or variocele 10
l) Removal of broid tumours, without
abdominal approach
20
11) Thyroid
a) partial or total removal of thyroid,
including all stages of operative procedure
70
12) Hernia
a) Invasive Surgery – single hernia 20
b) Invasive Surgery – double hernia 25
c) Radical operation, including injection
treatment for cure of single hernia
40
d) Radical operation, including injection
treatment for cure of double hernia
50
Description of surgical procedure
The Benet
Expressed as
a % of Sum
Insured
13) Joints And Dislocations
a) For dislocations requiring an open
operation the benet is increased by 100%,
but will not exceed the Total Sum Insured in
the Schedule.
i) Incision into joint for disease or disorder,
except as herein otherwise provided and
except tapping
15
ii) Arthroscopy of shoulder, elbow, hip or
knee joint, tapping excepted
40
iii) Excision , open xation, disarticulation or
arthoplasty on shoulder, hip or spine
75
iv) Excision , open xation, disarticulation or
arthoplasty on knee, elbow, wrist or ankle
35
v) Dislocation of ngers or toes, each 5
vi) Dislocation of shoulder or elbow, wrist
or ankle
15
vii) Dislocation of lower jaw 5
viii) Dislocation of hip or knee, knee cap
excepted
20
ix) Dislocation of knee cap 5
14) Nose
a) Intranasal sinus operation 15
b) extra nasal sinus operation 35
c) polyps, removal one or more 5
d) submucous resection 25
e) turbinectomy 10
15) Paracentesis tapping of:
a) Abdomen 10
b) chest or bladder, catheterization excepted
c) ear drum, hydrocele, joints or spine 5
16) Rectum And Rectoscopy
a) radical resection for malignancy, all
stages including colostomy
100
b) haemorrhoids, external only, excision –
complete procedure
10
c) haemorrhoids internal or internal and
external including prolapsed rectum, total for
excision or complete injection treatment
20
d) stula in ano 15
e) ssure in ano 5
f) rectoscopy with or without biopsy 10
g) colonoscopy with or without biopsy 15
h) other cutting operations on rectum 20
17) Skull
a) Craniotomy for urgent removal of
hematoma
100
b) Craniotomy involving vascular surgery 75
c) Craniotomy for removal of tumours 75
18) Throat
a) Tonsillectomy or tonsillectomy and
adenoidectomy for adults and children 15
years of age and older
15

21
Description of surgical procedure
The Benet
Expressed as
a % of Sum
Insured
b) Tonsillectomy or tonsillectomy and
adenoidectomy for children under 15 years
of age
10
c) use of laryngoscope for diagnosis 5
19) Tumours– surgical removal of:
a) Malignant tumours except those of the
mucous membrane, skin and subcutaneous
tissue
50
b) Malignant tumours of the mucous
membrane, skin and subcutaneous tissue
25
c) Pilonidal sinus or cyst, cutting operation 25
d) benign tumours of the testicle or breast 20
e) ganglion 5
f) benign tumours, one or more, except as
otherwise herein provided
10
g) varicose – complete procedure on all
veins whether cutting operation or injection
treatment – one leg
20
h) varicose – complete procedure on all
veins whether cutting operation or injection
treatment – two legs
30
9. Temporary Total Disablement – Accident Only
If during the Period of Insurance an Insured Person sustains
Bodily Injury which directly and independently of all other causes
results (starting during the Period of Insurance) in Temporary Total
Disablement, then the Company agrees to pay to the Insured Person
the amount stated in the Schedule. The Deductible or Franchise, if
applicable, shall be deducted from the Compensation payable.
Specic Conditions
1) If Bodily Injury is sustained to or suffered in relation to the spine and
its muscular girdle, ligamentous system, cartilage, nervous system and
blood supply to the spine which is not detectable by means of radiological
scanning, imaging, or neurological fallout testing, then the Company
shall only be liable in respect of this Section for a maximum period of
ve (5) weeks, in excess of the Deductible or Franchise if applicable.
2) In the event of a dispute arising as to when Temporary Total
Disablement ceased, the date shall be nally determined by a Physician
commissioned by the Company who certies:
a) the date upon which the Insured Person recovered; or
b) the date upon which the Insured Person recovered as far as he/
she ever will; or
c) the date from which the Insured Person is declared to have suffered
Permanent Total Disablement;
3) The benet shall not in any event exceed the Total Sum Insured or
the Maximum Number of Weeks as stated in the Schedule.
4) If an Insured Person has other insurance against a loss covered by
this Section, then the Company shall not be liable for a greater proportion
of the loss than the applicable benet under this Section bears to the
total applicable benet under all such insurance.
Specic Denitions
Temporary Total Disablement means disablement which temporarily
and entirely prevents an Insured Person from engaging in or giving
attention to the Insured Person’s usual occupation.
Specic Exclusions
The Company shall not be liable to pay any benet in respect of any
Insured Person for any claim caused by or arising from or due to
Sickness of any and every kind.
10. Temporary Total Disablement– Accident And Sickness
If during the Period of Insurance an Insured Person sustains Bodily
Injury or Sickness (starting during the Period of Insurance) which
directly and independently of all other causes results in Temporary Total
Disablement, then the Company agrees to pay to the Insured Person
the amount stated in the Schedule. The Deductible or Franchise, if
applicable, shall be deducted from the Compensation payable.
Specic Conditions
1) If Bodily Injury or Sickness is sustained to or suffered in relation
to the spine and its muscular girdle, ligamentous system, cartilage,
nervous system and blood supply to the spine which is not detectable
by means of radiological scanning, imaging, or neurological fallout
testing, then the Company shall only be liable in respect of this Section
for a maximum period of ve (5) weeks, in excess of the Deductible or
Franchise if applicable.
2) In the event of a dispute arising as to when Temporary Total
Disablement ceased, the date shall be nally determined by a Physician
commissioned by the Company who certies:
a) the date upon which the Insured Person recovered; or
b) the date upon which the Insured Person recovered as far as he/
she ever will; or
c) the date from which the Insured Person is declared to have suffered
Permanent Total Disablement.
3) The benet shall not in any event exceed the Total Sum Insured or
the Maximum Number of Weeks as stated in the Schedule.
4) If an Insured Person has other insurance against a loss covered by
this Section, then the Company shall not be liable for a greater proportion
of the loss than the applicable benet under this Section bears to the
total applicable benet under all such insurance.
Specic Denitions
Temporary Total Disablement means disablement which temporarily
and entirely prevents an Insured Person from engaging in or giving
attention to the Insured Person’s usual occupation.
11. Hostage Release Fees
If during the Period of Insurance an Insured Person is Kidnapped,
then the Company agrees to pay the fees incurred for a professional
negotiation organisation appointed by the Company to secure the
release of the Insured Person up to the Total Sum Insured stated
in the Schedule:
1. The Insured Person agrees to reimburse the Company for any
payments made by the Company which are ultimately determined not
to be insured because of the application of the Specic Exclusions.
2. If an Insured Person has other insurance against a loss covered by
this Section, then the Company shall not be liable for a greater proportion
of the loss than the applicable benet under this Section bears to the
total applicable benet under all such insurance.
Specic Denitions
1. Informant means any person providing information solely in return for
monetary payment paid or promised by the Policyholder.
2. Insured Person: Specic to this Section and in addition to the Insured
Person(s) stated in the Schedule, an Insured Person shall also include:
a) Immediate Family Member of an Insured Person.
b) a person legally resident in the household of an Insured Person.
c) accompanying travel companion of the Insured Person.
3) Kidnap or Kidnapped means the wrongful abduction and holding
under duress or by fraudulent means of any Insured Persons by any
person or group making a Ransom demand or series of Ransom
demands for the release of such Insured Persons.
4) Ransom means the amount demanded by any person or group who
have Kidnapped the Insured Person, or the amount paid to a person
or group for the release of the Insured Person.
Specic Exclusions
The Company will not be liable for:

22
1) Any Ransomamount.
2) any amount paid to an Informant or Informants.
3) any fraudulent, dishonest, or criminal acts of the Insured Person.
4) AnInsured Person being Kidnappedby an Immediate Family
Member.
5) AnyKidnapoccurring in South America, Mexico or the Philippines.
12. Assault
If during the Period of Insurance an Insured Person sustains
Bodily Injury that results in death or permanent disablement, as a
result of or arising from Assault, then the Company agrees to pay
to the Insured Person or the Insured Person’s Beneciary or legal
representatives the increased percentage of the Accidental death or
permanent disablement Total Sum Insured stated under this Section
in the Schedule.
Specic Conditions
All Specic Extensions, Specic Provisions, Specic Conditions, Specic
Denitions, Specic Claims Provisions and Specic Exclusions shall also
apply to this Section for each benet to which it attaches.
Specic Denitions
Assault means any wilful or unlawful use of force inicted upon an
Insured Person that is a criminal offence in the jurisdiction in which
it occurs and which results in Bodily Injury to an Insured Person.
Specic Exclusions
The Company shall not be liable to pay any benet in respect of any
Insured Person for an act of Assault by an Immediate Family Member.
13. Mobility Extension
If during the Period of Insurance an Insured Person sustains Bodily
Injury which directly and independently of all other causes results in
Permanent Total Disablement of such a nature that such Insured
Person needs and can operate:
1) a self-powered, climbing wheelchair; and/or
2) his/her motor vehicle with the controls suitably adjusted; and/or
3) a lift, necessary ramps, railings and holds to usual place of residence,
then the Company agrees to pay for 95% of the costs of such equipment
and the installation thereof up to the Total Sum Insured stated in the
Schedule.
14. Ambulance Costs
If during the Period of Insurance, an Insured Person sustains Bodily
Injury which is life threatening, then the Company agrees to pay the
actual ground ambulance costs incurred by the Insured Person up to
the Total Sum Insured stated in the Schedule, for transportation to the
nearest Hospital where adequate care can be provided.
15. Concussion Extension
If during the Period of Insurance, an Insured Person sustains Bodily
Injury and is hospitalized as the result of concussion, then the Company
agrees to pay to the Insured Person the following percentages of the
Total Sum Insured stated in the Schedule: Length of Hospital stay
Length of Hospital stay
Compensation Expressed as a
Percentage of Total
Sum Insured
Percentage of sum insured
payable for 0 to 4 Days
0%
Percentage of sum insured
payable after 5 Days
25%
Percentage of sum insured
payable after 8 Days
Additional 25%
Percentage of sum insured
payable after 11 Days
Additional 25%
Percentage of sum insured
payable after 13 Days
Additional 25%
16. Animal Attack Extension
If during the Period of Insurance, an Insured Person sustains Bodily
Injury as the result of an attack by an Animal and is hospitalised for
seventy-two (72) continuous hours, then the Company agrees to pay
to the Insured Person the Total Sum Insured stated in the Schedule.
Specic Denition
Animal means any four (4) limbed animal that is not an insect or reptile.
17. Chauffeur Plan Benet
If during the Period of Insurance an Insured Person is partially
incapacitated and unable to attend to a substantial part of his / her
business commitments as a result of Bodily Injury, then the Company
agrees to pay the daily amount up to the Total Sum Insured stated in the
Schedule for the hire of a taxi or chauffeur driven car or other necessarily
incurred extra costs to maintain the Insured Person’s mobility to meet
his / her business commitments. The Deductible or Franchise, if
applicable, shall be deducted from the Compensation payable.
Specic Exclusions
The Company shall not be liable to pay any benet in respect of any
Insured Person if the Insured Person does not follow proper medical
advice from a Physician after sustaining the Bodily Injury.
18. Spouse Or Dependent Child Consolation Benet
If during the Period of Insurance an Insured Person’s Spouse
or Dependent Child sustains Bodily Injury which directly and
independently of all other causes results in Death within twelve (12)
months of the Date of Loss, then the Company agrees to pay to
the Insured Person the Compensation stated in the Schedule. The
Spouse or Dependent Child must be insured under this Policy for this
benet to be paid.
Specic Extensions
1) Disappearance: In the event of the disappearance of the Insured
Person’s Spouse or Dependent Child, following a forced landing,
stranding, sinking or wrecking of a conveyance in which such Insured
Person’s Spouse or Dependent Child was known to have been
travelling as an occupant, it shall be deemed after twelve (12) months,
subject to all other terms and conditions of this Policy, that such Insured
Person’s Spouse or Dependent Child shall have died as the result
of an Accident. If at any time, after the payment of a benet under
this Section, it is discovered that the Insured Person’s Spouse or
Dependent Child is still alive, then all payments shall be reimbursed
in full to the Company.
2) Exposure: Death as a direct result of exposure to the elements shall
be deemed to be Bodily Injury.
19. Insured Person’s Counselling Benet
If during the Period of Insurance an Insured Person’s Spouse
or Dependent Child sustains Bodily Injury which directly and
independently of all other causes results in Death within twelve (12)
months of the Date of Loss, then the Company agrees to pay the
actual costs for professional counselling for the Insured Person up to
the Compensation stated in the Schedule.
Specic Extensions
1) Disappearance: In the event of the disappearance of the Insured
Person’s Spouse or Dependent Child, following a forced landing,
stranding, sinking or wrecking of a conveyance in which such Insured
Person’s Spouse or Dependent Child was known to have been
travelling as an occupant, it shall be deemed after twelve (12) months,
subject to all other terms and conditions of this Policy, that such Insured
Person’s Spouse or Dependent Child shall have died as the result
of an Accident. If at any time, after the payment of a benet under
this Section, it is discovered that the Insured Person’s Spouse or
Dependent Child is still alive, then all payments shall be reimbursed
in full to the Company.
2) Exposure: Death as a direct result of exposure to the elements shall
be deemed to be Bodily Injury.
Specic Conditions
Solely with respect to the insurance provided in this Section, Item 16 of
Section 5, General Exclusions, is deleted in its entirety.

23
20. Family Counselling Benet
If during the Period of Insurance an Insured Person sustains Bodily
Injury which directly and independently of all other causes results
in Death within twelve (12) months of the Date of Loss, then the
Company agrees to pay the actual costs for professional counselling
for the Insured Person’s Spouse and Dependent Child up to the
Compensation stated in the Schedule.
Specic Extensions
1) Disappearance: In the event of the disappearance of the Insured
Person, following a forced landing, stranding, sinking or wrecking of a
conveyance in which such Insured Person was known to have been
travelling as an occupant, it shall be deemed after twelve (12) months,
subject to all other terms and conditions of this Policy, that such Insured
Person shall have died as the result of an Accident. If at any time,
after the payment of a benet under this Section, it is discovered that
the Insured Person is still alive, then all payments shall be reimbursed
in full to the Company.
2) Exposure: Death as a direct result of exposure to the elements shall
be deemed to be Bodily Injury.
Specic Conditions
1) The total Sum Insured is the total amount payable for the Spouse
and Dependent Child combined, not per person.
2) Solely with respect to the insurance provided in this Section, Item 16
of Section 5, General Exclusions, is deleted in its entirety.
21. Common Accident
If during the Period of Insurance an Insured Person and his or her
Spouse sustain Bodily Injury in the same Accident which, directly
and independently of all other causes, results in the death of both the
Insured Person and the Spouse within twelve (12) months after the
Date of Loss, then the Total Sum Insured payable for each of the
Insured Person and Spouse shall be either the Accidental Death
Total Sum Insured applicable to the Insured Person or the Accidental
Death Total Sum Insured applicable to the Spouse, whichever is greater.
This benet shall in no event exceed the Common Accident maximum
amount shown in the Schedule.
This benet applies only if:
1) the Insured Person has elected insurance under the Policy for a
Spouse; and
2) such insurance is in effect on the date of the Accident.
Specic Extensions
1) Disappearance: In the event of the disappearance of the Insured
Person, following a forced landing, stranding, sinking or wrecking of a
conveyance in which such Insured Person was known to have been
travelling as an occupant, it shall be deemed after twelve (12) months,
subject to all other terms and conditions of this Policy, that such Insured
Persons shall have died as the result of an Accident. If at any time,
after the payment of a benet under this Section, it is discovered that
an Insured Person is still alive, all payments shall be reimbursed in
full to the Company.
2) Exposure: Death as a direct result of exposure to the elements shall
be deemed to be Bodily Injury.
22. Evacuation Benet
If during the Period of Insurance an Insured Person is Evacuating
from the building that is the Primary Insured Person’s place of
employment and sustains Bodily Injury in the Evacuation which directly
and independently of all other causes results in death or disablement
within twelve (12) months of the Evacuation, then the Company agrees
to pay the Compensation stated in the Schedule.
Specic Denitions
Evacuating / Evacuation means an emergency exit due to a re, a
re alarm, a bomb scare (whether there is a bomb or not), or an armed
attack on the building or the people in the building.
23. Medical Insurance Premium Indemnity
If during the Period of Insurance an Insured Person sustains Bodily
Injury which directly and independently of all other causes results in
death within twelve (12) months of the Date of Loss,then the Company
agrees to pay the actual costs of the medical insurance premiums for
the Insured Person’s surviving Spouse and Dependent Child up to
the amount stated in the Schedule per year up to the number of years
stated in the Schedule.
Specic Extensions
1) Disappearance: In the event of the disappearance of an Insured
Person, following a forced landing, stranding, sinking or wrecking of a
conveyance in which such Insured Person was known to have been
travelling as an occupant, it shall be deemed after twelve (12) months,
subject to all other terms and conditions of this Policy, that such Insured
Person shall have died as the result of an Accident. If at any time,
after the payment of a benet under this Section, it is discovered that
an Insured Person is still alive, all payments shall be reimbursed in
full to the Company.
2) Exposure: Death as a direct result of exposure to the elements shall
be deemed to be Bodily Injury.
Specic Conditions
The total Sum Insured is the total amount payable for the Spouse and
Dependent Child combined, not per person.
24. Dependent Child Education Benet
If during the Period of Insurance an Insured Person sustains Bodily
Injury which directly and independently of all other causes results in
Death within twelve (12) months of the Date of Loss, then the Company
agrees to pay the education fees for the Insured Person’s surviving
Dependent Child up to the amount stated in the Schedule per year up
to the number of years stated in the Schedule.
Specic Conditions
1) To receive benets under this Section, the Dependent Child must
be in full time education at an accredited tertiary educational institution.
2) The Total Sum Insured is the total amount payable for all Dependent
Children combined, not per person.
Specic Extensions
1) Disappearance: In the event of the disappearance of an Insured
Person, following a forced landing, stranding, sinking or wrecking of a
conveyance in which such Insured Person was known to have been
travelling as an occupant, it shall be deemed after twelve (12) months,
subject to all other terms and conditions of this Policy, that such Insured
Person shall have died as the result of an Accident. If at any time,
after the payment of a benet under this Section, it is discovered that
an Insured Person is still alive, all payments shall be reimbursed in
full to the Company.
2) Exposure: Death as a direct result of exposure to the elements shall
be deemed to be Bodily Injury.
30. Comatose Benet – Accident Only
If during the Period of Insurance an Insured Person sustains Bodily
Injury which directly and independently of all other causes results in the
Insured Person being in a Hospital in a Comatose State, within one
(1) calendar month of the Date of Loss, then the Company agrees to
pay to the Insured Person the Compensation stated in the Schedule.
The Deductible or Franchise, if applicable, shall be deducted from the
Compensation payable.
Specic Provisions
In case of successive Comatose State with less than ten (10) Days
between each one for a same cause, the Deductible or Franchise
will only apply once, as the Comatose State will be deemed as one.
Specic Conditions
1) The Insured Person must be in the Hospital Intensive Care Unit
for the duration of the Comatose State for any benets to be payable.
2) The Comatose State must be for three (3) months or more for any
benets to be payable.
Specic Denitions
Comatose State means a state of profound unconsciousness,
characterised by the absence of spontaneous eye openings, response

24
to painful stimuli, and vocalisation.
31. Comatose Benet – Accident & Sickness
If during the Period of Insurance an Insured Person sustains Bodily
Injury or Sickness which directly and independently of all other causes
results in the Insured Person being in a Hospital in a Comatose State,
within one (1) calendar month of the Date of Loss, then the Company
agrees to pay to the Insured Person the Compensation stated in the
Schedule. The Deductible or Franchise, if applicable, shall be deducted
from the Compensation payable.
Specic Provisions
In case of successive Comatose State with less than ten (10) Days
between each one for a same cause, the Deductible or Franchise
will only apply once, as the Comatose State will be deemed as one.
Specic Conditions
1) The Insured Person must be in the Hospital Intensive Care Unit
for the duration of the Comatose State for any benets to be payable.
2) The Comatose State must be for three (3) months or more for any
benets to be payable.
Specic Denitions
Comatose State means a state of profound unconsciousness,
characterised by the absence of spontaneous eye openings, response
to painful stimuli, and vocalisation.
32. Home Tuition Benet
If during the Period of Insurance an insured Dependent Child sustains
Bodily Injury (starting during the Period of Insurance) which directly
and independently of all other causes results in Temporary Total
Disablement, then the Company agrees to pay Home Tuition Fees
per Day up to the amount stated in the Schedule, for up to the maximum
number of weeks stated in the Schedule. The Deductible or Franchise,
if applicable, shall be deducted from the Compensation payable.
Specic Conditions
1) In the event of a dispute arising as to when Temporary Total
Disablement ceased, the date shall be nally determined by a Physician
commissioned by the Company who certies:
a) the date upon which the Insured Person recovered; or
b) the date upon which the Insured Person recovered as far as he/
she ever will; or
c) the date from which the Insured Person is declared to have suffered
Permanent Total
Disablement;
2) The benet shall not in any event exceed the Total Sum Insured or
the Maximum Number of Weeks as stated in the Schedule.
3) If an Insured Person has other insurance against a loss covered by
this Section, then the Company shall not be liable for a greater proportion
of the loss than the applicable benet under this Section bears to the
total applicable benet under all such insurance.
Specic Denitions
1) Temporary Total Disablement means disablement which temporarily
and entirely prevents an Insured Person from attending full time
education at an accredited tertiary educational institution
2) Home Tuition Fees means the costs for a fully registered and licensed
teacher to continue the education of the Insured Person at home during
Temporary Total Disablement.
Specic Exclusions
The Company shall not be liable to pay any benet in respect of any
Insured Person for any claim caused by or arising from or due to
Sickness of any and every kind.
33. Rehabilitation Benet
If during the Period of Insurance an Insured Person sustains Bodily
Injury which requires Rehabilitation within three (3) weeks of the Date
of Loss, then the Company agrees to pay the actual costs of such
treatment up to the amount stated in the Schedule. The Deductible or
Franchise, if applicable, shall be deducted from the Compensation
payable.
Specic Denitions
Rehabilitation means:
1) treatment by a therapist licensed, registered, or certied to provide
such treatment; or
2) treatment in an institution which is licensed to provide such treatment,
when the treatment is intended to prepare the Insured Person for
work in any gainful occupation, including the Insured Person’s regular
occupation.
Specic Exclusions
The Company shall not be liable to pay any benet in respect of any
Insured Person for any treatment not performed by a fully registered
and licensed Physiotherapist.
34. Reconstructive Surgery Benet
If during the Period of Insurance an Insured Person sustains Bodily
Injury which requires Reconstructive Surgery within six (6) months of
the Date of Loss, then the Company agrees to pay the actual costs of
such Reconstructive Surgery up to the amount stated in the Schedule.
The Deductible or Franchise, if applicable, shall be deducted from the
Compensation payable.
Specic Denitions
Reconstructive Surgery means surgery to reconstruct cutaneous or
underlying tissue, prescribed as necessary by a Physician.
Specic Exclusions
The Company shall not be liable to pay any benet in respect of any
Insured Person for
1) AnyReconstructive Surgery not performed by a fully registered and
licensed Cosmetic Surgeon.
2) AnyReconstructive Surgery an Insured Person elects to have.
35. Parental Care Benet
If during the Period of Insurance an Insured Person sustains Bodily
Injury which directly and independently of all other causes results in
Death within twelve (12) months of the Date of Loss, then the Company
agrees to pay the Compensation shown in the Schedule in equal shares
to each Dependent Parent of the Insured Person.
Specic Denitions
Dependent Parent means the parents or grandparents of the Insured
Person or the Insured Person’s Spouse. A Dependent Parent is
eligible for this benet if he or she, at the time of the Bodily Injury, is
receiving support and care provided by the Insured Person or Spouse.
36. Dependent Child Wedding Benet
If during the Period of Insurance an Insured Person sustains Bodily
Injury which directly and independently of all other causes results in
Death within twelve (12) months of the Date of Loss, then the Company
agrees to pay the Compensation shown in the Schedule in equal shares
to each Dependent Child of the Insured Person.
SECTION 6: TRAVEL INSURANCE
1. Accidental Death
If during the Period of Insurance an Insured Person sustains Bodily
Injury which directly and independently of all other causes results
in Death within twelve (12) months of the Date of Loss, then the
Company agrees to pay to the Insured Person’s Beneciary or legal
representative the Compensation stated in the Schedule.
Specic Extensions
1) Disappearance: In the event of the disappearance of the Insured
Person, following a forced landing, stranding, sinking or wrecking of a
conveyance in which such Insured Person was known to have been
travelling as an occupant, it shall be deemed after twelve (12) months,
subject to all other terms and conditions of this Policy, that such Insured
Person shall have died as the result of an Accident. If at any time,
after the payment of the Accidental death benet, it is discovered that

25
the Insured Person is still alive, all payments shall be reimbursed in
full to the Company.
2) Exposure: Death as a direct result of exposure to the elements shall
be deemed to be Bodily Injury.
Specic Conditions
If applicable and if payment has been made under the Permanent
Disablement Section, any amounts paid under that Section would be
deducted from payment of a claim under this Section of the Policy.
2. Permanent Disablement
If during the Period of Insurance an Insured Person sustains Bodily
Injury which directly and independently of all other causes results in
disablement within twelve (12) months of the Date of Loss, then the
Company agrees to pay to the Insured Person the Compensation
stated in the specic Table of Benets below, which is shown as the Table
of Benets in the Schedule. The Deductible or Franchise, if applicable,
shall be deducted from the Compensation payable.
Specic Extensions
Exposure: Permanent disablement as a direct result of exposure to the
elements shall be deemed to be Bodily Injury.
Specic Provisions
1) Ankylosis of the ngers (other than thumb and forenger) and of the
toes (other than the big toe) shall be limited to fty percent (50%) of the
Compensation payable for the loss of the said members.
2) Any benet payable under item 23 of Table (C) shall be at the complete
discretion of the Company taking into consideration the nature of the
Bodily Injury in conjunction with the stated Compensation percentages
for more specic injuries shown in the Table of Benets.
Specic Conditions
1) The insurance shall terminate for an Insured Person under this
Section upon payment of a benet equal to the Total Sum Insured.
2) The total amount payable in respect of more than one disablement
due to the same Accident is arrived at by adding together the various
percentages shown in the Table of Benets, but shall not exceed the
Total Sum Insured.
3) The Deductible or Franchise, if applicable, shall apply to the total
amount payable, irrespective of the number of benets an Insured
Person is entitled to.
4) If an Insured Person dies as the result of the Bodily Injury any
amount claimed and paid to an Insured Person under the Permanent
Disablement Section will be deducted from any payment under the
Accidental Death Section.
Specic Denitions for all Tables of Benets
1) Limb means the hand above the wrist joint or foot above the ankle
joint.
2) Loss of Hearing means the total and irrecoverable Loss of Hearing.
3) Loss of Mastication means the total and irrecoverable loss of ability
to chew food.
4) Loss of Sight means the total and irrecoverable Loss of Sight. This
is considered to have occurred if the degree of sight remaining after
correction is 3/60 or less on the Snellen Scale.
5) Loss of Speech means the total and irrecoverable Loss of Speech.
Specic Denitions for Table (A)
Loss used with reference to Limb means the loss by physical severance
of such Limb.
Specic Denitions for Table (B)
Loss used with reference to Limb means the loss by physical severance
or the total and permanent loss of use of such Limb.
Specic Denitions for Table (C) & Table (D)
Loss used with reference to Limb and / or ngers, thumbs or toes,
means the loss by physical severance or the total and permanent loss
of use of said member.
Table Of Benets – Table (A)
The Disablement
Compensation
Expressed as a
Percentage of Total
Sum Insured
1) Permanent Total Disablement 100%
2) Permanent and incurable insanity 100%
3) Permanent Total Loss of two Limbs 100%
4) Permanent Total Loss of Sight in
both eyes
100%
5) Permanent Total Loss of Sight of one
eye and one Limb
100%
6) Permanent Total Loss of Speech 100%
7) Complete removal of the lower jaw 100%
8) Permanent Total Loss of Mastication 100%
9) Permanent Total Loss of the central
nervous system or the thorax and
all abdominal organs resulting in the
complete inability to engage in any
job and the inability to carry out Daily
Activities essential to life without full
time assistance
100%
10) Permanent Total Loss of Hearing in
both ears
75%
11) Permanent Total Loss of one Limb 50%
12) Permanent Total Loss of Sight of
one eye
50%
Table Of Benets – Table (B)
The Disablement Compensation
Expressed as a
Percentage of Total
Sum Insured
1) Permanent Total Disablement 100%
2) Permanent and incurable insanity 100%
3) Permanent Total Loss of two Limbs 100%
4) Permanent Total Loss of Sight in
both eyes
100%
5) Permanent Total Loss of Sight of one
eye and one Limb
100%
6) Permanent Total Loss of Speech 100%
7) Complete removal of the lower jaw 100%
8) Permanent Total Loss of Mastication 100%
9) Permanent Total Loss of the central
nervous system or the thorax and
all abdominal organs resulting in the
complete inability to engage in any
job and the inability to carry out Daily
Activities essential to life without full
time assistance
100%
10) Permanent Total Loss of Hearing in
both ears
75%
11) Permanent Total Loss of one Limb 50%
12) Permanent Total Loss of Sight of
one eye
50%

26
Table Of Benets – Table (C)
The Disablement
Compensation
Expressed as
a Percentage
of Total Sum
Insured
1) Permanent Total Disablement 100%
2) Permanent and incurable insanity 100%
3) Permanent Total Loss of two Limbs 100%
4) Permanent Total Loss of Sight in both eyes 100%
5) Permanent Total Loss of Sight of one eye
and one Limb
100%
6) Permanent Total Loss of Speech 100%
7) Complete removal of the lower jaw 100%
8) Permanent Total Loss of Mastication 100%
9) Permanent Total Loss of the central nervous
system or the thorax and all abdominal
organs resulting in the complete inability to
engage in any job and the inability to carry
out Daily Activities essential to life without
full time assistance
100%
10) Permanent Total Loss of Hearing in both
ears
75%
11) Permanent Total Loss of one Limb 50%
12) Permanent Total Loss of Sight of one eye 50%
13) Permanent Total Loss of Hearing in one ear 15%
14) Permanent Total Loss of the lens in one eye 25%
15) Permanent Total Loss of use of four ngers
and thumb of either hand
40%
16) Permanent Total Loss of use of four ngers
of either hand
20%
17) Permanent Total Loss of use of one thumb
of either hand:
a) Both joints 20%
b) One joint 10%
18) Permanent Total Loss of one nger of either
hand:
a) Three joints 5%
b) Two joints 3.5%
c) One joint 2%
19) Permanent Total Loss of use of toes:
a) All – one foot 15%
b) Big – both joints 5%
c) Big – one joint 2%
d) Other than Big – each toe 2%
20) Established non-union of fractured leg or
kneecap
10%
21) Shortening of leg by at least 5 cms. 7.50%
22) Ankylosis of the elbow, hip or knee 20%
23) Permanent disablement not otherwise
provided for under Items 2-22 inclusive up
to a maximum of
75%
Table Of Benets – Table (D)
The Disablement
Compensation
Expressed as a
Percentage of Total
Sum Insured
1) Permanent Total Disablement 100%
2) Permanent and incurable insanity 100%
3) Permanent Total Loss of two Limbs 100%
4) Permanent Total Loss of Sight in
both eyes
100%
5) Permanent Total Loss of Sight of one
eye and one Limb
100%
6) Permanent Total Loss of Speech 100%
7) Complete removal of the lower jaw 100%
8) Permanent Total Loss of Mastication 100%
9) Permanent Total Loss of the central
nervous system or the thorax and
all abdominal organs resulting in the
complete inability to engage in any
job and the inability to carry out Daily
Activities essential to life without full
time assistance
100%
10) Permanent Total Loss of Hearing in
both ears
75%
11) Permanent Total Loss of one Limb 50%
12) Permanent Total Loss of Sight of
one eye
50%
13) Permanent Total Loss of Hearing in
one ear
15%
14) Permanent Total Loss of the lens in
one eye
25%
15) Permanent Total Loss of use of four
ngers and thumb of either hand
40%
16) Permanent Total Loss of use of four
ngers of either hand
20%
17) Permanent Total Loss of use of one
thumb of either hand:
a) Both joints 20%
b) One joint 10%
18) Permanent Total Loss of one nger of
either hand:
a) Three joints 5%
b) Two joints 3.5%
c) One joint 2%
19) Permanent Total Loss of use of toes:
a) All – one foot 15%
b) Big – both joints 5%
c) Big – one joint 2%
d) Other than Big – each toe 2%
20) Established non-union of fractured leg
or kneecap
10%
21) Shortening of leg by at least 5 cms. 7.50%
22) Ankylosis of the elbow, hip or knee 20%
3. Emergency Medical Expenses
If, during the Period of Insurance, an Insured Person sustains
Bodily Injury or sudden unexpected Sickness, then the Company will
reimburse the Insured Person the necessary Usual and Reasonable
Medical Expenses, incurred within two (2) months from the Date of

27
Loss up to the Sum Insured stated in the Schedule. The Deductible
or Franchise, if applicable, shall be deducted from the Compensation
payable.
Specic Conditions
1) Medical Expenses shall include and be limited to the following
services:
a) charges for semi private Hospital room and board, use of the
operating room, emergency room, and Ambulatory Medical Centre.
b) fees of Physicians.
c) Medical Expenses, in or out of Hospital, including: laboratory tests,
ambulance service (to or from the Hospital), prescription medicines
or drugs, therapeutics, anaesthetics (including administration of
anaesthetics), transfusions, articial Limbs or eyes (excluding repair or
replacement of these items), x-rays, prosthetic appliances.
d) charges for a registered nurse (R.N).
2) If a Policyholder or Insured Person has other insurance against a
loss covered by this Section, then the Company shall not be liable for
a greater proportion of the loss than the applicable benet under this
Section bears to the total applicable benet under all such insurance.
Specic Denitions
1) Ambulatory Medical Centre means a licensed facility providing
ambulatory surgical or medical treatment, other than a Hospital, clinic
or Physician’ sofce.
2) Usual and Reasonable Medical Expenses means fees and
prices generally charged in the locality where performed for medically
necessary services and supplies required for treatment of cases of
comparable severity and nature, but not to include charges that would
not have been made if no insurance existed.
Specic Exclusions
The Company shall not be liable to pay any benet in respect of any
Insured Person for:
1) AnyMedical Expenses incurred where an Insured Journey is
undertaken against the advice of a qualied licensed medical practitioner.
2) AnyMedical Expenses incurred when the specic purpose of a
journey is to receive medical treatment or advice.
3) AnyMedical Expenses incurred within the territorial limits that are
not stated in the Schedule.
4) any medical treatment, drugs or medicines, prescribed or applied,
before the Period of Insurance.
5) any dental work.
4. Emergency Dental Treatment
If during the Period of Insurance an Insured Person sustains Bodily
Injury or Acute Pain which directly and independently of all other causes
results in necessary emergency dental work, then the Company agrees
to pay for such costs up to the Total Sum Insured stated in the Schedule.
The Deductible or Franchise, if applicable, shall be deducted from the
Compensation payable.
Specic Conditions
If a Policyholder or Insured Person has other insurance against a
loss covered by this Section, then the Company shall not be liable for
a greater proportion of the loss than the applicable benet under this
Section bears to the total applicable benet under all such insurance.
Specic Denitions
Acute Pain means unexpected and sudden pain that requires immediate
treatment.
Specic Exclusions
The Company shall not be liable to pay any benet in respect of any
Insured Person for permanent crowns or articial teeth.
5. Emergency Travel Benets
The benets below will only be insured as part of the Policy if the
Assistance Provider Services Section has been purchased and contact
has been made with the Assistance Provider. Contact must be made
prior to any arrangements being made for such benets.
1) Medical Repatriation: If the Insured Person is unable to continue
his/her journey after a Hospital stay or medical treatment due to Bodily
Injury or Sickness, then the Company agrees to pay the actual costs or
the Total Sum Insured stated in the Schedule, whichever is the lesser,
for the repatriation of the Insured Person back to the Insured Person’s
Country of Residence or Country of Citizenship (for Operative Times
within the country of residence, the Insured Person will be returned to
his / her home town). If the gravity of the situation so dictates, then the
Company will pay for appropriate medical authorities to accompany the
Insured Person during the return journey.
2) Body Repatriation: If during the Period of Insurance, an Insured
Person dies as the result of Bodily Injury or Sickness then the
Company agrees to pay the actual costs or the Total Sum Insured stated
in the Schedule, whichever is the lesser, for the repatriation of the corpse
of the Insured Person to his / her Country of Residence or Country of
Citizenship (for Operative Times within the country of residence, the
corpse will be returned to his / her home town).
Specic Conditions
1) The decision on the most appropriate means, timing and course of
action belongs to the Assistance Provider only.
2) If a Policyholder or Insured Person has other insurance against a
loss covered by this Section, then the Company shall not be liable for
a greater proportion of the loss than the applicable benet under this
Section bears to the total applicable benet under all such insurance.
Specic Exclusions
The Company shall not be liable to pay any benet in respect of any
Insured Person:
1) if an Insured Person or anyone acting on behalf of an Insured Person
has not contacted the Assistance Provider, prior to any arrangements
that may give rise to a claim under this Section.
2) AnyMedical Expenses incurred where an Insured Journey is
undertaken against the advice of a qualied licensed medical practitioner.
3) AnyMedical Expenses incurred when the specic purpose of a
journey is to receive medical treatment or advice.
6. Contingency Travel Benets
The benets below will only be insured as part of the Policy if the
Assistance Provider Services Section has been purchased and contact
has been made with the Assistance Provider. Contact must be made
prior to any arrangements being made for such benets.
Emergency Hotel Extension: If during the Period of Insurance an
Insured Person sustains Bodily Injury or Sickness which directly
and independently of all other causes results in a Hospital stay as an
in-patient for more than ve (5) Days and misses his / her scheduled
ight back to the country of residence, then the Company agrees to
pay for the costs of Hotel accommodation up to the Total Sum Insured
stated in the Schedule, or until a return ight becomes available,
whichever is the earlier.
Specic Conditions
1) The decision on the most appropriate means, timing and course of
action belongs to the Assistance Provider only.
2) If a Policyholder or Insured Person has other insurance against
a loss covered by this Section, then the Company shall not be liable
for a greater proportion of the loss than the applicable benet under
this Section bears to the total applicable benefit under all such
insurance.
Specic Exclusions
The Company shall not be liable to pay any benet in respect of any
Insured Person:
1) if an Insured Person or anyone acting on behalf of an Insured Person
has not contacted the Assistance Provider, prior to an event that may
give rise to a claim under this Section.
2) Any Medical Expenses incurred where an Insured Journey is
undertaken against the advice of a qualied licensed medical practitioner.
3) Any Medical Expenses incurred when the specic purpose of a
journey is to receive medical treatment or advice.

28
7. Accidental Death - Common Carrier
If during the Period of Insurance an Insured Person is riding as a
passenger in or on, boarding or alighting from a Common Carrier and
sustains Bodily Injury which directly and independently of all other
causes results within twelve (12) calendar months of the Accident
in death, then the Company agrees to pay to the Insured Person’s
Beneficiary or legal representative Compensation stated in the
Schedule.
Specic Conditions
If applicable and if payment has been made under the Permanent
Disablement or Permanent Disablement – Common Carrier Section,
any amounts paid under that Section would be deducted from payment
of a claim under this Section of the Policy.
8. Permanent Disablement – Common Carrier
If during the Period of Insurance an Insured Person is riding as a
passenger in or on, boarding or alighting from a Common Carrier and
sustains Bodily Injury which directly and independently of all other
causes results in disablement within twelve (12) months of the Date
of Loss, then the Company agrees to pay to the Insured Person the
Compensation stated in the specic Table of Benets below, which
is shown as the Table of Benets in the Schedule. The Deductible or
Franchise, if applicable, shall be deducted from the Compensation
payable.
Specic Conditions
1) This insurance shall terminate for an Insured Person under this
Section upon payment of a benet equal to the Total Sum Insured.
2) The total amount payable in respect of more than one disablement
due to the same Accident is arrived at by adding together the various
percentages shown in the Table of Benets, but shall not exceed the
Total Sum Insured.
3) The Deductible or Franchise, if applicable, shall apply to the total
amount payable, irrespective of the number of benets an Insured
Person is entitled to.
4) If an Insured Person dies as the result of the Bodily Injury any
amount claimed and paid to an Insured Person under the Permanent
Disablement or Permanent Disablement – Common Carrier Section will
be deducted from any payment under the Accidental Death – Common
Carrier Section.
Specic Provisions
Ankylosis of the ngers (other than thumb and forenger) and of the
toes (other than the big toe) shall be limited to fty percent (50%) of the
Compensation payable for the loss of the said members.
Specic Denitions for all Tables of Benets
1) Limb means the hand above the wrist joint or foot above the ankle
joint.
2) Loss of Hearing means the total and irrecoverable Loss of Hearing.
3) Loss of Mastication means the total and irrecoverable ability to
chew food.
4) Loss of Sight means the total and irrecoverable Loss of Sight. This
is considered to have occurred if the degree of sight remaining after
correction is 3/60 or less on the Snellen Scale.
5) Loss of Speech means the total and irrecoverable Loss of Speech.
Specic Denitions for Table (B)
Loss used with reference to Limb and / or ngers, thumbs or toes,
means the loss by physical severance or the total and permanent loss
of use of said member.
TABLE OF BENEFITS – TABLE (B)
The Disablement
Compensation
Expressed as a
Percentage of Total
Sum Insured
1) Permanent Total Disablement 100%
2) Permanent and incurable insanity 100%
The Disablement
Compensation
Expressed as a
Percentage of Total
Sum Insured
3) Permanent Total Loss of two Limbs 100%
4) Permanent Total Loss of Sight in
both eyes
100%
5) Permanent Total Loss of Sight of one
eye and one Limb
100%
6) Permanent Total Loss of Speech 100%
7) Complete removal of the lower jaw 100%
8) Permanent Total Loss of Mastication 100%
9) Permanent Total Loss of the central
nervous system or the thorax and
all abdominal organs resulting in the
complete inability to engage in any
job and the inability to carry out Daily
Activities essential to life without full
time assistance.
100%
10) Permanent Total Loss of Hearing in
both ears
75%
11) Permanent Total Loss of one Limb 50%
12) Permanent Total Loss of Sight of
one eye
50%
9. Hospital Cash – Accident & Sickness
If during the Period of Insurance an Insured Person sustains Bodily
Injury or Sickness which directly and independently of all other causes
results in the Insured Person being in a Hospital as an in-patient within
one (1) calendar month of the Date of Loss, then the Company agrees
to pay to the Insured Person the Daily Benet stated in the Schedule.
The Deductible or Franchise, if applicable, shall be deducted from the
Compensation payable.
Specic Provisions
In case of successive Hospital stays with less than sixty (60) Days
between each one for a same cause, the Deductible or Franchise will
only apply once, as the Hospital stays will be deemed as one event.
Specic Conditions
Once the Company has paid the Daily Benet up to the maximum
number of Days stated in the Schedule, cover under this Section will
cease for such Insured Person.
10. LOSS OF BAGGAGE & PERSONAL DOCUMENTS
If, during the Period of Insurance, the Baggage, Personal Documents
and/or Personal Effects owned by or in the custody of an Insured Person
are damaged or lost, then the Company will reimburse the Insured
Person the cost of replacement of the articles for any amount up to the
Total Sum Insured stated in the Schedule. The Deductible, if applicable,
shall be deducted from the Compensation payable.
Specic Conditions
1) Any valid claim involving a motor vehicle, and at all time subject to
Specic Exclusion (5), will be limited to a maximum of fty percent (50%)
of the Sum Insured stated in the Schedule.
2) All claims will be subject to the Company at its own discretion
assessing the value of the claim based on the age and estimated wear
and tear of the article that forms the basis of the claim.
3) If applicable and if payment has been made under the Baggage Delay
Section, any amounts paid would be deducted from payment of a claim
under this Section of the Policy.
4) If a Policyholder or Insured Person has other insurance against
a loss covered by this Section, then the Company shall not be liable
for a greater proportion of the loss than the applicable benet under
this Section bears to the total applicable benefit under all such
insurance.

29
Specic Denitions
Personal Documents means an Insured Person’s identity card (if
applicable), ration card, voter identity card, passport, driving licence
and car licence.
Specic Claims Provisions
In the event of a claim the Insured Person must:
1) give immediate written notice:
a) to the relevant Common Carrier in the event of loss or damage
in transit;
b) to the relevant police authority in the event of loss or theft;
2) submit a copy of the relevant Common Carrier or police report
when a claim is made;
3) obtain a Common Carrier or police report where the loss occurred;
4) in the event of loss by a Common Carrier, retain original tickets and
baggage slips and submit them when a claim is made;
5) submit original purchase receipts in the event of claims regarding
goods purchased during the Insured Journey; and
6) for claims involving jewellery, submit original or certied copies of
valuation certicates issued prior to the commencement of the Period
of Insurance, when a claim is made.
For purposes of any claim hereunder:
1) a pair of skis, ski boots and accessories shall be regarded as one item;
2) bottles of perfume, aftershave, and make up shall together be
regarded as one item;
3) the equipment and accessories of any sport that an Insured Person
takes on a trip shall be regarded as one item.
Specic Exclusions
The Company shall not be liable to pay any benet in respect of any
Insured
Person for:
1) loss of cash, bank or currency notes, cheques, debit or credit cards
or unauthorised use thereof, postal orders, travellers cheques, travel,
tickets, securities of any kind and petrol or other coupons.
2) mechanical or electrical breakdown or derangement or breakage of
fragile or brittle articles, or damage caused by such breakage unless
caused by re or by Accident to the conveying ehicle.
3) destruction or damage due to wear and tear, moth or vermin.
4) baggage, clothing and personal effects despatched as unaccompanied
baggage.
5) theft from a motor vehicle unless the property is securely locked
in the boot and entry to such vehicle is gained by visible, violent and
forcible means.
6) loss or damage to sports equipment whilst in use, contact lenses,
samples, tools.
7) for loss, destruction, or damage due to delay, conscation or detention
by order of any government or Public Authority.
8) for loss, destruction or damage directly occasioned by pressure
waves, caused by aircraft or other aerial devices travelling at sonic or
supersonic speeds.
9) for loss, destruction or damage caused by any process of cleaning,
dyeing, repairing or restoring.
10) for loss, destruction, or damage caused by atmospheric or climatic
conditions or any other gradually deteriorating cause.
11) a claim involving animals.
12) loss, including but not limited to loss by theft, or damage to vehicles
or other accessories.
13) for any loss that is not reported either to the appropriate police
authority or transport carrier within twenty four (24) hours of discovery
or if the carrier is an airline if a property irregularity report is not obtained.
14) baggage and/or personal effects sent under an airway-bill or bill
of lading.
15) computer equipment, cameras, musical instruments, radios and
portable radio /cassette/compact disc players.
16) contact lenses, glasses, hearing aids or bridges or dentures for a
tooth or teeth.
11. Loss Of Checked Baggage
If, during the Period of Insurance, the Baggage, Personal Documents
and/or Personal Effects that have been checked in on the same
Common Carrier as a travelling Insured Person, are damaged or
lost, then the Company will reimburse the Insured Person the cost of
replacement of the articles for any amount up to the Total Sum Insured
stated in the Schedule. The Deductible, if applicable, shall be deducted
from the Compensation payable.
Specic Conditions
1) All claims will be subject to the Company at its own discretion
assessing the value of the claim based on the age and estimated wear
and tear of the article that forms the basis of the claim.
2) If applicable and if payment has been made under the Baggage Delay
Section, any amounts paid would be deducted from payment of a claim
under this Section of the Policy.
3) If a Policyholder or Insured Person has other insurance against a
loss covered by this Section, then the Company shall not be liable for
a greater proportion of the loss than the applicable benet under this
Section bears to the total applicable benet under all such insurance.
Specic Denitions
Personal Documents means an Insured Person’s identity card (if
applicable), ration card, voter identity card, passport, driving licence
and car licence.
Specic Claims Provisions
In the event of a claim the Insured Person must:
1) give immediate written notice:
a) to the relevant Common Carrier in the event of loss or damage
in transit;
b) to the relevant police authority in the event of loss or theft;
2) submit a copy of the relevant Common Carrier or police report when
a claim is made;
3) obtain a Common Carrier or police report where the loss occurred;
4) in the event of loss by a carrier, retain original tickets and baggage
slips and submit them when a claim is made;
5) submit original purchase receipts in the event of claims regarding
goods purchased during the Insured Journey; and
6) for claims involving jewellery, submit original or certied copies of
valuation certicates issued prior to the commencement of the Period
of Insurance, when a claim is made.
For purposes of any claim hereunder:
1) a pair of skis, ski boots and accessories shall be regarded as one item;
2) bottles of perfume, aftershave, and make up shall together be
regarded as one item;
3) the equipment and accessories of any sport that an Insured Person
takes on a trip shall be regarded as one item.
Specic Exclusions
The Company shall not be liable to pay any benet in respect of any
Insured Personfor:
1) loss of cash, bank or currency notes, cheques, debit or credit cards
or unauthorised use thereof, postal orders, travellers cheques, travel,
tickets, securities of any kind and petrol or other coupons.
2) mechanical or electrical breakdown or derangement or breakage of
fragile or brittle articles, or damage caused by such breakage unless
caused by re or by Accident to the conveying vehicle.
3) destruction or damage due to wear and tear, moth or vermin.
4) baggage, clothing and personal effects despatched as unaccompanied
baggage.

30
5) theft from a motor vehicle unless the property is securely locked
in the boot and entry to such vehicle is gained by visible, violent and
forcible means.
6) loss or damage to sports equipment whilst in use, contact lenses,
samples, tools.
7) for loss, destruction, or damage due to delay, conscation or detention
by order of any government or Public Authority.
8) for loss, destruction or damage directly occasioned by pressure
waves, caused by aircraft or other aerial devices travelling at sonic or
supersonic speeds.
9) for loss, destruction or damage caused by any process of cleaning,
dyeing, repairing or restoring.
10) for loss, destruction, or damage caused by atmospheric or climatic
conditions or any other gradually deteriorating cause.
11) a claim involving animals.
12) loss, including but not limited to loss by theft, or damage to vehicles
or other accessories.
13) for any loss that is not reported either to the appropriate police
authority or transport carrier within twenty four (24) hours of discovery
or if the carrier is an airline if a property irregularity report is not obtained.
14) baggage and/or personal effects sent under an airway-bill or bill
of lading.
15) computer equipment, cameras, musical instruments, radios and
portable radio /cassette/compact disc players.
16) contact lenses, glasses, hearing aids or bridges or dentures for a
tooth or teeth.
12. Baggage Delay
If, during the Period of Insurance, the baggage and/or personal
effects owned by or in the custody of an Insured Person is delayed or
misdirected for more than the Deductible stated in the Schedule, then
the Company will reimburse the Insured Person the cost of necessary
personal effects up to the Sum Insured stated in the Schedule.
Specic Conditions
1) The baggage and/or personal effects must have been checked in
as registered baggage by the airline operating under a licence issued
by a governmental authority having jurisdiction for the transportation of
fare paying passengers on xed established routes, for any benet to
be payable under this Section.
2) If upon further investigation it is later determined that the baggage and/
or personal effects has been lost, then any amount claimed and paid to
an Insured Person under the Baggage Delay Section will be deducted
from any payment under the Baggage Loss Section.
3) An Insured Person shall exercise all reasonable measures and
precautions for the safety of, and recovery of, any property insured
hereunder. Notication of any apparent delay to baggage must be made
immediately to the airline concerned.
4) If a Policyholder or Insured Person has other insurance against a
loss covered by this Section, then the Company shall not be liable for
a greater proportion of the loss than the applicable benet under this
Section bears to the total applicable benet under all such insurance.
5) If the Insured Person receives any form of compensation from the
Common Carrier in the form of vouchers, tickets or coupons, then these
items will be surrendered to the Company.
Specic Exclusions
The Company will not indemnify the Insured Person for delayed
baggage as a result of the following:
1) chartered ights, unless such ights are registered in the International
Data System.
2) conscation of baggage by customs or any government authority.
3) purchases made after arriving in the nal destination mentioned on
the airline ticket.
4) baggage and/or personal effects sent under an airway-bill or bill
of lading.
5) delays due to a strike or industrial action existing or announced before
the start of the journey.
6) delays due to withdrawal of aircraft from service by any civil aviation
authority of which notice had been given before the start of the journey.
7) any delays of the return journey.
13. Flight Delay
If during the Period of Insurance, the ight on which an Insured
Person is due to travel is delayed in excess of the Deductible, then the
Company agrees to reimburse up to the amount stated in the Schedule
per hour, or up to the Total Sum Insured, whichever is the lesser, for
essential purchases, such as meals, refreshments or other related
expenses directly resulting from the:
1) delay or cancellation of the Insured Person’s booked and conrmed
ight.
2) late arrival of the Insured Person’s connecting ight causing the
Insured Person to miss his or her onward connection.
3) or a late arrival (of more than 1 hour) of public transport causing the
Insured Person to miss the ight.
Specic Conditions
1) If a Policyholder or Insured Person has other insurance against a
loss covered by this Section, then the Company shall not be liable for
a greater proportion of the loss than the applicable benet under this
Section bears to the total applicable benet under all such insurance.
2) If the Insured Person receives any form of compensation from the
Common Carrier in the form of vouchers, tickets or coupons, then these
items will be surrendered to the Company.
Specic Claims Provisions
All claims must be submitted in writing to the Company by the Insured
Person, or his/her legal representative and all information, documents,
and evidence required by the Company shall be furnished at no expense
to the Company and shall be in such form and of such nature as the
Company may prescribe. All claims must be reported to the Company
within twenty- one (21) Days of a delay occurring, and must contain:
a) the Policy number.
b) detailed circumstances of the delay.
c) a copy of declaration of delay made by the public transport company
(other than an airline).
d) all receipts, all invoices serving as proof of purchases made in
connection with the ight delay, as well as proof of the delay and the
ight number and place where the delay occurred.
Specic Exclusions
The Company shall not be liable for any claim:
1) arising or as the result of chartered ights, unless such ights are
registered in the International Data System.
2) if comparable alternative transport has been made available within
six (6) hours after scheduled departure time or within six (6) hours of
an actual connecting ight arrival time.
3) if an Insured Person fails to check-in according to the itinerary
supplied, unless it is due to a strike.
4) if the delay is due to a strike or industrial action existing or announced
before the start of the journey.
5) if the delay is due to withdrawal of aircraft from service by any civil
aviation authority of which notice had been given before the start of
the journey.
14. Hijacking
If during the Period of Insurance an Insured Person is travelling on
board a Common Carrier which is Hijacked, then the Company agrees
to pay to the Insured Person the Compensation stated in the Schedule
for every six (6) continuous hours in excess of the Deductible up to
the Total Sum Insured.
Specic Denitions
Hijacked means the unlawful seizure or wrongful exercise of control of
a Common Carrier, or the crew thereof.

31
Specic Exclusions
The Company shall not be liable to pay any benet in respect of any
Insured Person for any claim caused by civil authority.
15. Personal Liability
Property Damage
If while this Policy is in force a claim is made or a suit brought against
an Insured Person for Property Damage that occurred during the
Period of Insurance, then the Company agrees to pay to the Insured
Person the Compensation stated in the Schedule, up to the Total Sum
Insured, for the damages for which the Insured Person is legally liable.
Medical Payments to Others
If while this Policy is in force a claim is made or a suit brought against an
Insured Person for Medical Expenses as the result of an Accident that
occurred during the Period of Insurance caused by the Insured Person
and resulting in Bodily Injury to another person, then the Company
agrees to pay to the Insured Person the Compensation stated in the
Schedule, up to the Total Sum Insured, for the damages for which the
Insured Person is legally liable.
In no event with the Company pay more than the Total Sum Insured for
all Property Damage or Medical Expenses arising out of one event.
Specic Conditions
1) If a Policyholder or Insured Person has other insurance against a
loss covered by this Section, then the Company shall not be liable for
a greater proportion of the loss than the applicable benet under this
Section bears to the total applicable benet under all such insurance.
2) The Total Sum Insured is the total amount payable for Property
Damage and Medical Payments to Others combined, not for each one.
Specic Denitions
1) Medical Expenses means reasonable charges for medical, surgical,
X-ray, dental, ambulance, Hospital, professional nursing, prosthetic
devices and funeral services.
2) Property Damage means physical injury to, destruction of or loss of
use of tangible property.
Specic Exclusions
The Company will not be liable for any claims caused by or resulting
either directly or indirectly from:
1) liability which is expected or intended by an Insured Person.
2) liability arising out of or in connection with a business engaged in
by an Insured Person. This exclusion applies but is not limited to an
act or omission,
3) regardless of its nature or circumstance, involving a service or duty
rendered, promised, owed, or implied to be provided because of the
nature of the business.
4) liability arising out of the rental or holding for rental of any part of
any premises or a motor vehicle of any kind by an Insured Person.
5) liability arising out of the rendering of or failure to render professional
services.
6) liability arising out of a premises, watercraft or aircraft that is owned
by, rented to or rented by an Insured Person.
7) liability arising out of the ownership, maintenance, use, loading or
unloading of motor vehicles, all other motorised land conveyances,
water craft or aircraft.
8) liability arising out of the transmission of a communicable disease
by an Insured Person.
9) liability arising out of sexual molestation, corporal punishment, or
physical or mental abuse.
10) liability arising out of the use, sale, manufacture, delivery, transfer or
possession by any person of a controlled substance or contraband as
dened by the appropriate authority or government agency.
11) liability under any contract or agreement.
12) Property Damage to property owned by an Insured Person.
13) Property Damage to property rented to, occupied, or used by or in
the care of an Insured Person.
14) Bodily Injury to any person eligible to receive any benets voluntarily
provided or required to be provided by an Insured Person under any
worker’s compensation law, non occupational disablement law or
occupational diseases law.
15) any claims or suits arising from any Immediate Family Member,
Close Business Associate or an Immediate Family Member of a
Close Business Associate against an Insured Person.
16. Financial Emergency Assistance
The deductible excess in respect of this benet will be applicable for each
separate claim, and shall be of an amount as specied in the Schedule
of this Policy. For the purpose of this benet, ‘nancial emergency’ shall
mean a situation wherein theInsured loses all or a substantial amount
of his/her travel funds due to theft, robbery, mugging or dacoity, such
that there is a detrimental effect on his/her travel plans.
The Company shall have the sole discretion to determine whether a
‘nancial emergency’ has occurred in any instance.
This is an assistance provided by the company through service provider.
The assistance would be provided subject to the terms and conditions
of the service provider, as stated below.
Exclusions Applicable - Financial Emergency Assistance
The Company shall not be liable to make any payment under this benet
in connection with or in respect of any expenses whatsoever incurred
by the Insured in connection with or in respect of
1) A shortage or loss of funds due to currency uctuation, errors
omissions, exchange, loss or depreciation in value.
2) Any loss not reported to the police authorities having jurisdiction at
the place of loss within 24 hours of the occurrence of the incident and
a written report beingobtained for the same.
3) Any claim in respect of a loss of traveller’s cheques not immediately
reported to the local branches or agents of the issuing authority.
4) Loss of funds not kept in the personal custody of the Insured.
5) Any reimbursement under Financial Emergency Assistance is
excluded if the claim is put up after arrival of the Insured to the Republic
of India
Any exclusion mentioned in the ‘General Exclusions’ section of this
Policy.
SECTION 7: HOME INSURANCE – REVISION
Section I. 7. A. – Fire and Special Perils
The Company will indemnify the Insured in respect of loss or damage to
the building wherein the home of the Insured is situated and/or contents
which shall for purposes of this Section, mean and include items of
property in the Insured’s home and/or items of property there in for
which the Insured is accountable, due to:
1. Fire
Excluding destruction of or damage caused to the property insured by:
a. i.Its own fermentation, natural heating or spontaneous combustion;
ii. Its undergoing any heating or drying process.
b. Burning of property insured by order of any Public Authority.
2. Lightning
3. Explosion/Implosion
Excluding loss, destruction of or damage:
a. To boilers (other than domestic boilers), economisers or other vessels,
machinery or apparatus (in which steam is generated) or their contents
resulting from their own explosion/implosion;
b. Caused by centrifugal forces.
4. Aircraft Damage
Loss, destruction of or damage caused by aircraft, other aerial or space
devices and articles dropped there from excluding those caused by
pressure waves.
5. Riot, Strike and Malicious Damage
Loss or visible physical damage or destruction by external violent means

32
directly caused to the property insured but excluding those caused by:
a. Permanent or temporary dispossession resulting from conscation,
commandeering, requisition or destruction by order of the Government
or any lawfully constituted authority;
b. Permanent or temporary dispossession of any building resulting from
the unlawful occupation by any person of such building or prevention
of access to the same;
c. Burglary, housebreaking, theft, larceny or any such attempt or omission
of any kind by any person (whether or not such act is committed in the
course of a disturbance of public peace)by any malicious act.
6. Storm, Cyclone, Typhoon, Tempest, Hurricane, Tornado, Flood
and Inundation
Loss, destruction or damage directly caused by storm, cyclone, typhoon,
tempest, hurricane, tornado, ood or inundation.
7. Impact Damage
Loss or visible physical damage or destruction caused to the property
insured due to impact by any rail/road vehicle or animal by direct contact
not be longing to or ownedby
a. The Insured or any occupier of the property insured ;or
b. Their employees while acting in the course of their employment.
8. Subsidence and Land slide including Rockslide
Loss, destruction or damage directly caused by Subsidence of part of
the site on which the property stands or Landslide/Rockslide excluding:
a. The normal cracking, settlement or bedding down of new structures.
b. The settlement or movement of made up ground.
c. Coastal or river erosion.
d. Defective design or workmanship or use of defective materials.
e. Demolition, construction, structural alterations or repair of any property
or ground works or excavations.
9. Bursting and/or Over owing of Water Tanks, Apparatus &Pipes
10. Missile Testing Operations
11. Leakage from Automatic Sprinkler Installations
Excluding loss, destruction or damage caused by
a. Repairs or alterations to the buildings or premises.
b. Repairs, removal or extension of the sprinkler installation.
c. Defects in construction known to the Insured.
12. Bush Fire
Excluding loss, destruction or damage caused by forest re.
13. Earthquake, Volcanic Eruption & Other Convulsions of Nature
Loss, destruction or damage (including loss, destruction or damage
by re) to any of the property insured by this policy occasioned by or
through or inconsequence of earthquake including ood or overow
of the sea, lakes, reservoirs and rivers and/or Landslide/Rockslide
resulting there from.
Exclusions
This Section does not cover -
1. Loss, destruction or damage caused by war, invasion, act of foreign
enemy, hostilities or war like operations (whether war be declared or
not), civil war, mutiny or civil commotion assuming the proportions of
or amounting to a popular rising, military rising, rebellion, revolution,
insurrection or military or usurped power.
2. Loss, destruction or damage, directly or indirectly, caused to the
property insured by a) ionising, radiation or contamination by radioactivity
from any nuclear fuel or from any nuclear waste from the combustion of
nuclear fuel; b)radioactive toxic, explosives or other hazardous properties
of any explosive nuclear assembly or nuclear component thereof.
3. Loss, destruction or damage caused to the insured property by
pollution or contamination excluding a) pollution or contamination which
itself results from a peril hereby insured against; b) any peril hereby
insured against which itself results from pollution or contamination.
4. Loss, destruction or damage to manuscripts, plans, drawings,
securities, documents of any kind, stamps, coins, cash/paper money,
deeds, ATM cards, credit cards, charge cards, bonds, bills of exchange,
promissory notes, or any other negotiable instrument, books of accounts
or any other business books, and explosives.
5. Loss, destruction or damage to articles of consumable nature, livestock
and motor vehicles.
6. Loss, destruction or damage to Specied Items including jewellery,
curios, antiques, pictures and other works of art, guns, collection of
stamps, coins and medals for an amount collectively in excess of
Rs. 10,000 unless specically stated to the contrary in the Schedule.
7. Loss, destruction or damage to any electrical machine, apparatus,
xture or tting arising from or occasioned by over-running, excessive
pressure, short circuiting, arcing, self heating or leakage of electricity
from whatever cause (lightningincluded)provided that this exclusion
shall apply only to the particular electrical machine, apparatus, xture
or tting so affected and not to other machines, apparatus, xtures or
ttings which may be destroyed or damaged by re so setup.
8. Expenses necessarily incurred on (i) Architects, Surveyors and
Consulting Engineer’s Fees and (ii) debris removal by the Insured
following loss, destruction or damage to the property insured by any of the
insured perils in excess of 3% and 1% of the claim amount respectively.
9. Loss of earnings, or other consequential or indirect loss or damage
of any kind or description what so ever.
10. Loss by the ft during or after the occurrence of any of the insured
perils except as provided under riot, strike, and malicious damage cover
Terrorism Damage Exclusion Warranty
Notwithstanding any provision to the contrary within this insurance it is
agreed that this insurance excludes loss, damage cost or expense of
what so ever nature directly or indirectly caused by, resulting from or in
connection with any act of terrorism regardless of any other cause or
event contributing concurrently or in any other sequence to the loss. For
the purpose of this warranty, an act of terrorism means an act, including
but not limited to the use of force or violence and/or the threat thereof, of
any person or group (s) of persons whether acting alone or on behalf of
or in connection with any organisation(s) or government(s), committed for
political, religious, ideological or similar purpose including the intention
to inuence any government and/or to put the public, or any section of
the public in fear. The warranty also excludes loss, damage, cost or
expenses of whatsoever nature directly or indirectly caused by, resulting
from or in connection with any action taken in controlling, preventing,
suppressing or in any way relating to action taken in respect of any act
of terrorism. If the Company alleges that by reason of this exclusion,any
loss, damage, cost or expenses is not covered by this insurance the
burden of proving the contrary shall be upon the insured. In the event
any portion of this exclusion is found to be invalid or unenforceable, the
remainder shall remain in full force and effect
SUMINSURED
The basis of valuation shall be
i. Reinstatement value for buildings and all contents excepting personal
effects, and
ii. Market value for personal effects.
BASIS OF INDEMNITY
1. The indemnity shall be on the basis of reinstatement value or market
value as applicable and as stated above.
2. In the event of property insured being damaged by any of the insured
perils , the Company shall pay for the amount of damage or loss or at
its option replace or repair the damaged property.
3. If the property hereby insured shall, at the breaking out of any re or
at the commencement of any destruction of or damage to the property
by any of the insured perils be collectively of greater value than the
Sum Insured there on , then the Insured shall be considered as being
his own insurer for the difference and shall bear a rateable portion of
the loss accordingly. Provided, however, that if the Sum Insured here
by on the property insured shall at the breaking out of such re or at
the commencement of such destruction or damage be not less than

33
85% (eighty ve percent) of the collective value of the property insured,
clause 3 of Basis of Indemnity under this Section shall not apply, not with
standing anything to the contrary contained in the policy.
Section I 7. B. BURGLARY AND HOUSE BREAKING INCLUDING
LARCENY AND THEFT (AS DEFINDED IN INDIAN PENAL CODE)
What is covered
a. The Company will indemnify the Insured in respect of loss or damage
to contents ,by burglary and house breaking including larceny and theft.
b. The Company will further indemnify the Insured in respect of damage
to the Insured’s home and / or safe resulting from burglary and/or house
breaking or any attempt thereat subject to a maximum of 5% of the
Sum Insured under this Section. Provided however that no loss under
clauses a) and b) herein above, shall together exceed the Sum Insured
under this Section.
EXCLUSIONS
This Section does not cover loss, destruction or damage:
1. Caused by burglary and/or house breaking and/or theft and/or larceny
where any member of the Insured’s family is concerned as principal
or accessory.
2. To securities, documents of any kind, stamps, coins, cash/ paper
money, deeds, ATM cards, credit cards, charge cards, bonds, bills of
exchange, promissory notes, or any other negotiable instrument, books
of accounts or any other business books ,and explosives.
3. To articles of consumable nature ,live stock and motor vehicles.
4. To curios, antiques, pictures and other works of art, guns, collection
of stamps, coins and medals for an amount collectively in excess of
Rs. 10,000 unless specically stated to the contrary in the Schedule.
5. To jewellery and valuables in excess of Rs. 10,000 per single article
unless stated to the contrary in the Schedule.
SPECIAL CONDITION
1. Jewellery is covered subject to its being kept in locked safe within
the home premises.
2. Where any item insured hereunder consists of articles in pair or set
the Company’s liability in respect there of shall not exceed the value
of any article which may be lost or damaged without reference to any
special value which such article may have as part of such pair or set.
3. The cover under this section becomes inoperative if the premises
remain unoccupied for more than 60 consecutive days unless prior
written notice is sent to the Company and its consent obtained, subject to
fullment of terms and conditions that may be stipulated by the Company
for extending cover in such circumstances.
4. For Multi year policy-
Extends to cover the property of the insured up to policy period as
specied in the schedule provided that:
a. The policy shall be issued for a minimum period of 2 years.
b. Refund shall be allowed as per below rules.
1. No refund shall be allowed if there has been a claim under the policy.
2. If the policy is cancelled within 3 years of inception, the premium to
be retained shall be worked out as per normal rates applicable - that is
with out all owing any discount.
3. If the policy is cancelled after 3 years of inception, the discounts lab
shall be reworked for the number of years the policy was actually in
force .For this purpose fraction of a year shall be rounded to the next
higher year.
4. Refund, if any, shall be subject to the retention of minimum premium
of Rs.100/-
c. Mid-term inclusion of perils shall not be allowed.
d. Premium for entire policy period shall be collected in advance.
e. Mid-term increase in sum insured shall be allowed on prorate basis
for the balance period.
f. Mid-term reduction in Sum Insured is not allowed
g. Policy with long term extension can be issued to only to house/at
owners and not to others who do not own the house/at.
h. Discounts for Earthquake Cover for Long term policies cannot be
allowed.
i. All Other terms and conditions remain same as per Policy wording
SUM INSURED
The basis of valuation shall be
i. Reinstatement value for all contents excepting personal effects, and
ii. Market value for personal effects.
BASIS OF INDEMNITY
1. The indemnity shall be on the basis of reinstatement value or market
value as applicable and asstated above.
2. In the event of property insured being damaged by any of the insured
perils , the Company shall pay for the amount of damage or loss or at
its option replace or repair the damaged property.
If the property here by insured shall, at the commencement of any
destruction of or damage to the property by any of the insured perils be
collectively of greater value than the Sum Insured there on, then the
Insured shall be considered as being his own insurer for the difference
and shall be at a rateable portion of the loss accordingly. Provided,
however, that if the Sum Insured hereby on the property insured shall at
the breaking out of such re or at the commencement of such destruction
or damage be not less than 85% (eighty ve percent) of the collective
value of the property insured, clause 3 of Basis of Indemnity under this
Section 1. shall not apply, not withstanding anything to the contrary
contained in the policy.
SECTION 8: E@SECURE INSURANCE
1. Legal Protection
If You have a legal dispute over any of the Specified Events,
Wewillprovide Youthe necessary legal protection against the costs of
pursuing and defending legal actions maximum up to the amount of
the sub limit set forth under “Legal Protection” specied on the Policy
Schedule:
a) Professional Legal Advice
We will pay for the legal advice sought by You based on the laws of India.
b) Legal Costs
Wewill cover Yourlegal costs to:
• Pursue or defend any legal actions against or by the Third Party;
• Remove any criminal or civil judgments wrongly entered against You; or
• Challenge the accuracy or completeness of any information in a
credit report.
Provided that:
1. The Specied Eventoccurred on the internet during the Period of
Insurance;
2. Our prior written consent must be obtained before any costs are
incurred (which shall not be unreasonably withheld or delayed );
3. The legal action pursued / defended is within the jurisdiction of the
Indian courts.
B. SPECIFIED EVENTS
2. Damage to e-Reputation
If You suffer damage to Your personal reputation which arises directly
from a Harmful Publication (whether in the form of videos, photographs
or published statements) by any Third Party on the internet, We will
reimburse for the costs incurred by You:
a) For the services of an IT specialist to remove and / or Flood such
Harmful Publication from the internet maximum up to the amount of
the sub limit set forth under “Damage to e-Reputation’’ on the Policy
Schedule; and
For the Face – to – face consultation with a Psychologist / an accredited
Psychiatrist for post – traumatic stress disorder, suicidal tendencies,
self-harm, depression, anxiety disorder, insomnia, eating disorders

34
or similar serious medical condition that makes consultation Deemed
Necessary, maximum up to the amount of the sub limit set forth under
“Psychological counseling” on the Policy schedule. Any sub limit of
liability available for counseling service under this is part of, and not
in addition to, the sub limit of liability set forth under limit mentioned in
“Damage to e-reputation” on Policy Schedule; the payment by Us of
any such sub limit of liability erodes the sub limit of liability set forth in
“Damage to e-reputation” of the Policy Schedule.
Provided that:
1. This Specied Eventoccurred on the internet during the Period
of Insurance;
2. You lodge an FIR within Seventy – two (72) hours upon discovering
the Harmful Publication, giving details of the contents and specic
internet sites where the Harmful Publicationis published.
What We will not cover under this Section:
In addition to the General Exclusions, Wewillalso not pay any claim
in respect of:
1. Loss that occurs within the rst forty – ve (45) days of the inception
date of this insurance cover.
2. Any non-digital media (e.g. in print), radio and television broadcast
3. Damage caused by a Journalist.
4. Any legal proceedings (pending or settled) with a Third Party prior
to the commencement of this cover.
3. Identity Theft
If Your Personal Information is stolen over the internet, and a Third
Party knowingly and unlawfully uses it subsequently without Your
express consent to obtain money, goods or services, We will provide
for reimbursement of the costs / expenses that You incurred maximum
up to the amount of the sub limit set forth under “Identity Theft” on the
Policy Schedule for /to :
a) amend or rectify records regarding Your true name or identity,
including but not limited to:
• To notarize afdavits for nancial institutions or credit bureau agencies
to restore Your Bank Accounts and credit rating;
• To re-submit loan applications which were declined solely because the
lender received incorrect credit information; and
• Costs of telephone calls, postage and bank charges to resolve the
Identity Theft.
b) Any lost wages due to time taken off from work, not exceeding 7days
solely for the purpose of meeting with the relevant organizations and/
or authorities to amend or rectify records as a result of an Identity Theft
§ If You are self - employed, lost wages will be calculated based on Your
tax returns in the prior year and limited to wages lost within 12 months
upon discovery of the Identity Theft.
b) For the Face – to – face consultation with a Psychologist / an
accredited Psychiatrist for post – traumatic stress disorder, suicidal
tendencies, self-harm, depression, anxiety disorder, insomnia, eating
disorders or similar serious medical condition that makes consultation
Deemed Necessary, maximum up to the amount of the sub limit set
forth under “Psychological counseling” on the Policy schedule. Any sub
limit of liability available for counseling service under this is part of, and
not in addition to, the sub limit of liability set forth under limit mentioned
in “Identity Theft” on Policy Schedule; the payment by Us of any such
sub limit of liability erodes the sub limit of liability set forth in “Identity
Theft” of the Policy Schedule.
Provided that:
1. This Specied Event occurred on the internet during the Period
of Insurance;
2. You lodge an FIR detailing the Identify Theft within 72 hours upon
discovery of Identity Theft by You;
3. You notify Your bank or Credit / Debit Card issuer(s) of the Identity
Theft by You within 72 hours upon discovery of the Identity Theft by
You (if applicable).
4. You provide evidence of lost wages.
All losses resulting from the same, continuous, related or repeated acts
shall be treated as arising out of a single Identity Theft occurrence.
What We will not cover under this Section:
In addition to the General Exclusions, We will also not pay any claim
in respect of:
1. Expenses incurred (e.g. loan application fees, telephone charges
etc.) six (6) months after the expiry of the cover.
4. Unauthorized Online Transactions
If You suffer loss as a direct result of the fraudulent use of Your Bank
Account and / or Credit/Debit Cards and /or E-Wallets by a Third Party
for purchases made over the internet, We will indemnify You maximum
up to the amount of the sub limit set forth under “Unauthorized Online
Transaction” on the Policy Schedule for:
a) Any Unauthorized Online Transactions that are charged to Your
Credit/Debit Card or Bank Account or E-Wallets that are legally
unrecoverable from any other sources.
b) Any lost wages due to time taken off from work, not exceeding 7days
solely for the purpose of meeting with the relevant organizations and
authority to amend or rectify records regarding Your true name or identity
as a result of the Unauthorized Online Transactions.
• If You are self-employed, lost wages will be based onYour tax returns
in the prior year and limited to wages lost within 12 months upon
discovery of the theft.
c) Costs of telephone calls, postage and bank charges to resolve the
breach of payment.
Provided that:
1. This Specied Event occurred on the internet during the Period
of Insurance;
2. You lodge an FIR detailing the Unauthorized Online Transaction within
72 hours upon discovery of the breach by You;
3. You notify to the issuing bank and/or Credit/Debit Card and/or
E-Wallet provider within 72 hours upon discovery of the breach by You;
4. You provide evidence that the bank is not reimbursing You for the
fraudulent transactions;
5. You provide evidence of lost wages.
What We will not cover under this Section:
In addition to the General Exclusions, Wewill also not pay any claim
in respect of:
1. Reimbursement by the bank for the transaction.
2. Cash advances (or cash withdrawn through an ATM or Bank Account)
made through Your stolen Bank Accounts and/or Credit/Debit Cards.
5. E-Extortion
If Yousuffer nancial loss solely and directly as a result of Extortion
Threat, We will reimburse You or pay on Your behalf Extortion
Loss that You incur solely and directly as result of Extortion Threat
maximumup to the amount of the sub limit set forth under “E-Extortion”
on the Policy Schedule
Provided that:
1. This Specied Eventoccurred on the internet during the Period
of Insurance;
2. You lodge an FIR within seventy two (72) hours upon receiving the
Extortion Threat;
3. You shall use your best efforts at all times to ensure that knowledge
regarding the existence of the insurance for Extortion Loss afforded
by this policy is kept condential, unless disclosure to law enforcement
authorities is required.
4. You shall allow Us (or the our nominated representatives) to notify
the police or other responsible law enforcement authorities of any
Extortion Threat.
What We will not cover under this Section:
In addition to the General Exclusions, We will also not pay any claim
in respect of:

35
1. Loss that occurs within the rst forty ve (45) days of the inception
date of this insurance cover.
2. Any claim or legitimate demand or even conscation of the assets by
bonade governmental or judicial authority.
6. Cyber Bullying or Harassment
If You are the victim of Cyber Bullying or Harassment by a Third Party,
resulting in or possibly leading to lower self-esteem, increased suicidal
ideation, and a variety of emotional responses including retaliating,
being scared, frustrated, angry, and depressed as certied by a qualied
Psychologist / Psychiatrist being the direct result of Cyber Bullying
or Harassment, We will reimburse You maximumup to the amount of
the sub limit set forth under “ Cyber Bullying” on the Policy Schedule for
a) Face – to – face consultation with a Psychologist / an accredited
Psychiatrist for post – traumatic stress disorder, suicidal tendencies, self-
harm, depression, anxiety disorder, insomnia, eating disorders or similar
serious medical condition that makes consultation Deemed Necessary.
Provided that:
1. This Specied Event occurred on the internet during the Period
of Insurance;
2. You lodge an FIR detailing the perpetrators or in event of victim
being a minor, an FIR following a psychological consultation or a written
complaint to the school authorities.
In addition to the General Exclusions, Wewill also not pay any claim
in respect of:
1. Event that occurs within the rst 45(forty ve) days of the inception
date of this insurance cover.
2. Any non-digital media (e.g. in print, radio or television broadcast)
3. Any act of government or authority putting You under surveillance
or monitoring.
4. Any disciplinary act or related disciplinary action initiated by authorities
against You at work place, clubs, social forums or school.
5. Any legal proceedings (pending or settled) with a Third Party prior
to the commencement of this cover.
7. Phishing & Email Spoong
If Yousuffer nancial loss directly due to Phishing, wewill indemnify
You for the MoneyYou lost as a direct result of Phishing maximum
up to the amount of sub-limit set forth under “Phishing” on the Policy
Schedule. In the event, the Phishing is of the nature of Email Spoong
as dened, We will indemnify You for the Money You lost, maximum
up to the amount of sub-limit set forth under “Email Spoong” on the
Policy Schedule.
Provided that:
1. This Specied Eventoccurred on the internet during the Period
of Insurance;
2. You lodge an FIR detailing the loss within 72 hours upon discovery
of the loss by You
3. In event of Email Spoong, the onus is on You to prove and establish
that You had every reason to expect such email and You had the
requirement to make payment against same
What We will not cover under this Section:
In addition to the General Exclusions, Wewillalso not pay any claim
in respect of:
1. Any Illegal transactions e.g bribes, commissions or illegal gratications
2. Phishing resulting in revelation of personal information including
passwords
3. Any payments or charges towards lottery, unexpected bequeath of
wealth, or any other similar unsolicited promises or dishonest incentives
LIMIT OF COVER
(a) Limit of Liability: Our maximum limit of liability for any one Period
of Insurance is limited to the amount specied in the Policy Schedule.
Deductible: We shall be liable only in excess of the Deductible stated in
the Policy Schedule. The Deductible shall apply to all claims resulting
from one event (or a series of events) occurring at the same time or
from the same originating cause.
II Denitions
The terms dened below have the meanings asdescribed to them
wherever they appear in this Policy and, where appropriate, references
to the singular include references to the plural; references to the male
include the female and references to any statutory enactment include
subsequent changes to the same
Denitions Applicable to my:health Suraksha , my:health Critical
Suraksha Plus , my:health Medisure Super Top up Insurance ,
my:health Hospital cash Benet Add on , Personal Accident &
Travel Insurance
1. Accident or Accidental means a sudden, unforeseen and involuntary
event caused by external, visible and violent means.
2. Age or Aged means completed years as at the Policy Commencement
Date.
3. Any one illness means continuous period of Illness and includes
relapse within 45 daysfrom the date of last consultation with the Hospital/
Nursing Home where treatment was taken
4. Alternative treatments means forms of treatments other than
treatment “Allopathy” or “modern medicine” and includes Ayurveda,
Unani, Sidha and Homeopathy in the Indian context
5. Cashless Facilitymeans a facility extended by the insurer to the
insured where the payments, of the costs of treatment undergone by
the insured in accordance with the policy terms and conditions, are
directly made to the Network Provider by the insurer to the extent
pre-authorization is approved.
6. Commencement Date means the commencement date of the Policy
as specied in the Policy Schedule.
7. Condition Precedent means a policy term or condition upon which
the Insurer’s liability under the policy is conditional upon
8. Congenital Anomalymeans a condition(s) which is present since
birth, and which is abnormal with reference to form, structure or position.
a) Internal Congenital Anomaly:Congenital Anomaly which is not in
the visible and accessible parts of the body.
b) External Congenital Anomaly:Congenital Anomaly which is in the
visible and accessible parts of the body
9. Co-Paymentmeans a cost sharing requirement under a health
insurance policy that provides that the policyholder/insured will bear a
specied percentage of the admissible claims amount. A Co-Payment
does not reduce the Sum Insured
10. Cumulative Bonusmeans any increase or addition in the Sum
Insured granted by the Insurer without an associated increase in
premium.
11. Day care Centremeans any institution established for Day Care
Treatment of Illness and / or injuries or a medical set -up witha
Hospital and which has been registered with the local authorities,
wherever applicable, and is under the supervision of a registered
and qualied medical practitioner AND must comply with all minimum
criterionas under:-
I. has qualied nursing staff under its employment;
II. has qualied medical practitioner/s in charge;
III. has fully equipped operation theatre of its own where surgical
procedures are carried out;
IV. maintains daily records of patients and will make these accessible
to the insurance company’s authorized personnel
12. Day Care Treatment/ Proceduresmeans those medical treatment,
and/or surgical procedure which is
i. undertaken under General or Local Anaesthesia in a Hospital/
Day Care Centre in less than 24 hours because of technological
advancement, and
ii. which would have otherwise required Hospitalization of more than
24 hours,

36
Treatment normally taken on an Out-patient basis is not included in the
scope of this denition
13. Deductible means a costsharing requirement under a health
insurance policy that provides that the Insurer will not be liable for a
specied rupee amount in case of indemnity policies and for a specied
number of days/hours in case of Hospital cash policies, which will apply
before any benets are payable by the insurer. A Deductible does not
reduce the sum insured.
14. Dependents means only the family members listed below:
a) Your legally married spouse as long as she continues to be married
to You
b) Your children Aged between 91 days and 25 years if they are
unmarried, still nancially dependent on You and have not established
their own independent households;
c) Your natural parents or parents that have legally adopted You, and
Your parent in laws
15. Dental Treatmentmeans a treatment related to teeth or structures
supporting teeth including examinations, llings (where appropriate),
crowns, extractions and surgery
16. Disclosure of information norm means the policy shall be void
and all premiums paid hereon shall be forfeited to the Company, in
the event of misrepresentation, mis-description or non-disclosure of
any material fact.
17. Domiciliary Hospitalization means medical treatment for an
Illness/disease/Injury whichin the normal course would require care
and treatment at a Hospital but is actually takenwhile conned at home
under any of the following circumstances:
I. the condition of the patient is such that he/she is not in a condition to
be removed to a Hospital, or
II. the patient takes treatment at home on account of non-availability
of room in a Hospital
18. Emergency Care means management for an Illness or injury
which results in symptoms which occur suddenly and unexpectedly, and
requires immediate care by a Medical Practitioner to prevent death or
serious long term impairment of the insured person’s health.
19. Family Floater means a Policy described as such in the Policy
Schedule whereunder You and Your Dependents (Spouse, dependent
children, dependent parents/parents in laws) named in the Policy
Schedule are insured under this Policy as at the Commencement Date. .
20. Grace Period means the specied period of time immediately
following the premium due date during which a payment can be made to
renew or continue a policy in force without loss of continuity benets such
as waiting periods and coverage of pre –existingdiseases. Coverage is
not available for the period for which no premium is received.
21. Hospital means any institution established for In-patient Care and
Day Care Treatment ofIllness and/or injuries and which has been
registered as a Hospital with the local authorities under the clinical
Establishments (Registration and Regulation) Act, 2010 or under the
enactments specied under the Schedule of Section 56(1) of the said
Act OR complies with all minimum criteria as under:
• has at least 10 in-patient beds, in towns having a population of less
than 10,00,000 and 15 in-patient beds in all other places,
• has qualied nursing staff under its employment round the clock,
• has qualied Medical Practitioner(s) in charge round the clock,
• has a fully equipped operation theatre of its own where surgical
procedures are carried out,
· maintains daily records of patients and will make these accessible to
the insurance company’s authorized personnel.
22. Hospitalization means admission in a Hospital for a minimum
period of 24 consecutive ‘In-patient Care’ hours except for specied
procedures/ treatments, where such admission could be for a period of
less than 24 consecutive hours.
23. Illness/ Illnessesmeans a sickness or a disease or pathological
condition leading to the impairment of normal physiological function
which manifests itself during the Policy Period and requires medical
treatment
(a) Acute condition - Acute condition is a disease, Illness or Injury that
is likely to respond quickly to treatment which aims to return the person
to his or her state of health immediately before suffering the disease/
Illness/ Injury which leads to full recovery
(b) Chronic condition - A chronic condition is dened as a disease,
Illness, or Injury that has one or more of the following characteristics:
i. it needs ongoing or long-term monitoring through consultations,
examinations, check-ups, and /or tests
ii. it needs ongoing or long-term control or relief of symptoms
iii. it requires rehabilitation for the patient or for the patient to be specially
trained to cope with it
iv. it continues indenitely
v. it recurs or is likely to recur
24. Injury means Accidental physical bodily harm excluding Illness or
disease solely and directly caused by external, violent and visible and
evident means which is veried and certied by a Medical Practitioner.
25. In-patient Care means treatment for which the Insured Person
has to stay in a Hospital for more than 24 hours for a covered event.
26. Insured Person means the persons named in the Policy Schedule
and insured under the Policy.
27. Intensive Care Unit means an identied section, ward or wing of a
Hospital which is under the constant supervision of a dedicated Medical
Practitioner(s), and which is specially equipped for the continuous
monitoring and treatment of patients who are in a critical condition, or
require life support facilities and where the level of care and supervision
is considerably more sophisticated and intensive than in the ordinary
and other wards.
28. ICU (Intensive Care Unit)Chargesmeans the amount charged by
a Hospital towards ICU expenses which shall include the expenses
for ICU bed, general medical support services provided to any
ICU patient including monitoring devices, critical care nursing and
intensive charges
29. Maternity Expensesmeans
a. Medical treatment expenses traceable to childbirth (including
complicated deliveries and caesareansection incurred during
Hospitalization).
b. Expenses towards lawful medical termination of pregnancy during
the policy Period.
30. Major Illness means:
1. Cancer of specied severity
A malignant tumour characterized by the uncontrolled growth and spread
of malignant cells with invasion and destruction of normal tissues. This
diagnosis must be supported by histological evidence of malignancy. The
term cancer includes leukaemia, lymphoma and sarcoma.
The following are excluded:
i. All tumours which are histologically described as carcinoma in situ,
benign, pre-malignant, borderline malignant, low malignant potential,
neoplasm of unknown behaviour, or non-invasive, including but not
limited to: Carcinoma in situ of breasts, Cervical dysplasia CIN-1,
CIN - 2 and CIN-3.
ii. Any non-melanoma skin carcinoma unless there is evidence of
metastases to lymph nodes or beyond;
iii. Malignant melanoma that has not caused invasion beyond the
epidermis;
iv. All tumours of the prostate unless histologically classied as having
a Gleason score greater than 6 or having progressed to at least clinical
TNM classication T2N0M0
v. All Thyroid cancers histologically classified as T1N0M0 (TNM
Classication) or below;
vi. Chronic lymphocytic leukaemia less than RAI stage 3

37
vii. Non-invasive papillary cancer of the bladder histologically described
as TaN0M0 or of a lesser classication,
viii. All Gastro-Intestinal Stromal Tumours histologically classied as
T1N0M0 (TNM Classication) or below and with mitotic count of less
than or equal to 5/50 HPFs;
ix. All tumours in the presence of HIV infection.
2. Open Chest CABG
I. The actual undergoing of heart surgery to correct blockage or narrowing
in one or more coronary artery(s), by coronary artery bypass grafting
done via a sternotomy (cutting through the breast bone) or minimally
invasive keyhole coronary artery bypass procedures. The diagnosis must
be supported by a coronary angiography and the realization of surgery
has to be conrmed by a cardiologist.
II. The following are excluded:
a. Angioplasty and/or any other intra-arterial procedures
3. Myocardial Infarction (First Heart Attack of specied severity)
I. The rst occurrence of heart attack or myocardial infarction, which
means the death of a portion of the heart muscle as a result of inadequate
blood supply to the relevant area. The diagnosis for Myocardial Infarction
should be evidenced by all of the following criteria:
a. A history of typical clinical symptoms consistent with the diagnosis of
acute myocardial infarction (For e.g. typical chest pain)
b. New characteristic electrocardiogram changes
c. Elevation of infarction specic enzymes, Troponins or other specic
biochemical markers.
II. The following are excluded:
a. Other acute Coronary Syndromes
b. Any type of angina pectoris
c. A rise in cardiac biomarkers or Troponin T or I in absence of overt
ischemic heart disease OR following an intra-arterial cardiac procedure.
4. Kidney failure requiring regular dialysis
I. End stage renal disease presenting as chronic irreversible failure of
both kidneys to function, as a result of which either regular renal dialysis
(haemodialysis or peritoneal dialysis) is instituted or renal transplantation
is carried out. Diagnosis has to be conrmed by a specialist medical
practitioner.
5. Major Organ/Bone Marrow Transplant
The actual undergoing of a transplant of:
a. One of the following human organs: lung, liver, kidney, pancreas,
that resulted from irreversible end-stage failure of the relevant organ,
b. The undergoing of a transplant has to be conrmed by a specialist
medical practitioner.
The following are excluded:
a. Other stem-cell transplants
b. Where only islets of langerhans are transplanted
6. Multiple Sclerosis with persisting symptoms
I. The unequivocal diagnosis of Denite Multiple Sclerosis conrmed
and evidenced by all of the following:
a. investigations including typical MRI ndings which unequivocally
conrm the diagnosis to be multiple sclerosis and
b. there must be current clinical impairment of motor or sensory function,
which must have persisted for a continuous period of at least 6 months.
II. Other causes of neurological damage such as SLE and HIV are
excluded.
7. Permanent Paralysis of Limbs
I. Total and irreversible loss of use of two or more limbs as a
result of injury or disease of the brain or spinal cord. A specialist
medical practitioner must be of the opinion that the paralysis will be
permanent with no hope of recovery and must be present for more
than 3 months.
8. Stroke resulting in permanent symptoms
I. Any cerebrovascular incident producing permanent neurological
sequelae.
a. This includes infarction of brain tissue, thrombosis in an intracranial
vessel, haemorrhage and embolisation from an extracranial source.
b. Diagnosis has to be conrmed by a specialist medical practitioner
and evidenced by typical clinical symptoms as well as typical ndings
in CT Scan or MRI of the brain. Evidence of permanent neurological
decit lasting for at least 3 months has to be produced.
II. The following are excluded:
a. Transient ischemic attacks (TIA)
b. Traumatic injury of the brain
c. Vascular disease affecting only the eye or optic nerve or vestibular
functions.
9. Surgery of Aorta
The actual undergoing of medically necessary surgery for a disease of
the aorta needing excision and surgical replacement of the diseased
aorta with a graft. For the purpose of this denition aorta shall mean
the thoracic and abdominal aorta but not its branches. Traumatic injury
of the aorta is excluded.
10. Primary (Idiopathic) Pulmonary Hypertension
I. An unequivocal diagnosis of Primary (Idiopathic) Pulmonary
Hypertension by a Cardiologist or specialist in respiratory medicine
with evidence of right ventricular enlargement and the pulmonary
artery pressure above 30 mm of Hg on Cardiac Cauterization. There
must be permanent irreversible physical impairment to the degree of
at least Class IV of the New York Heart Association Classication of
cardiac impairment.
II. The NYHA Classication of Cardiac Impairment are as follows:
i. Class III: Marked limitation of physical activity. Comfortable at rest, but
less than ordinary activity causes symptoms.
ii. Class IV: Unable to engage in any physical activity without discomfort.
Symptoms may be present even at rest.
III. Pulmonary hypertension associated with lung disease, chronic
hypoventilation, pulmonary thromboembolic disease, drugs and toxins,
diseases of the left side of the heart, congenital heart disease and any
secondary cause are specically excluded.
11. Open Heart Replacement or Repair of Heart Valves
The actual undergoing of open-heart valve surgery is to replace or
repair one or more heart valves, as a consequence of defects in,
abnormalities of, or disease- affected cardiac valve(s). The diagnosis of
the valve abnormality must be supported by an echocardiography and
the realization of surgery has to be conrmed by a specialist medical
practitioner. Catheter based techniques including but not limited to,
balloon valvotomy/valvuloplasty are excluded.
31. Medical Advice means any consultation or advice from a
Medical Practitioner including the issue of any prescription or follow
upprescription.
32. Medical Expenses means those expenses that an Insured Person
has necessarily and actually incurred for medical treatment on account
of Illness or Accident on the advice of a Medical Practitioner, as long
as these are no more than would have been payable if the Insured
Person had not been insured and no more than other hospitals or
Medical practitioners in the same locality would have charged for the
same medical treatment.
33. Medically Necessary treatment means any treatment, test,
medication, or stay in Hospital or part of stay in Hospital which
• Is required for the medical management of the Illness or Injury suffered
by the Insured Person;
• Must not exceed the level of care necessary to provide safe, adequate
and appropriate medical care in scope, duration or intensity.
• Must have been prescribed by a Medical Practitioner.
• Must conform to the professional standards widely accepted in
international medical practice or by the medical community in India.

38
34. Medical Practitionermeans a person who holds a valid registration
from the Medical Council of any State or Medical Council of India
or Council for Indian Medicine or for Homeopathy set up by the
Government of India or a State Government and is thereby entitled to
practice medicine within its jurisdiction; and is acting within the scope
and jurisdiction of license.Medical Practitioner who is sharing the
same residence with the Insured person‘s and is a member of Insured
Person’s family are not considered as Medical Practitioner under the
scope of this Policy.
Medical practitioner for mental illnesses means a medical practitioner
possessing a post-graduate degree or diploma in psychiatry awarded
by an university recognised by the University Grants Commission
established under the University Grants Commission Act, 1956, or
awarded or recognised by the National Board of Examinations and
included in the First Schedule to the Indian Medical Council Act, 1956, or
recognised by the Medical Council of India, constituted under the Indian
Medical Council Act, 1956, and includes, in relation to any State, any
medical ofcer who having regard to his knowledge and experience in
psychiatry, has been declared by the Government of that State to be a
psychiatrist for the purposes of this Act;
Medical Practitioner (Denition applicable for the treatment taken
outside India)
Means a licensed medical practitioner acting within the scope of
hislicense and who holds a degree of a recognized institution and
isregistered by the Authorized Medical Council of the respectivecountry.
35. Mental illness means a substantial disorder of thinking, mood,
perception, orientation or memory that grossly impairs judgment,
behaviour, capacity to recognise reality or ability to meet the ordinary
demands of life, mental conditions associated with the abuse of alcohol
and drugs, but does not include mental retardation which is a condition
of arrested or incomplete development of mind of a person, specially
characterised by subnormality of intelligence;
36. Mental health establishment means any health establishment,
including Ayurveda, Yoga and Naturopathy, Unani, Siddha and
Homoeopathy establishment, by whatever name called, either wholly
or partly, meant for the care of persons with mental Illness, established,
owned, controlled or maintained by the appropriate Government, local
authority, trust, whether private or public, corporation, co-operative
society, organisation or any other entity or person, where persons with
mental Illness are admitted and reside at, or kept in, for care, treatment,
convalescence and rehabilitation, either temporarily or otherwise; and
includes any general Hospital or general nursing home established or
maintained by the appropriate Government, local authority, trust, whether
private or public, corporation, co-operative society, organisation or any
other entity or person; but does not include a family residential place
where a person with mental Illness resides with his relatives or friends;
37. my: Health Appis proprietary App of HDFC ERGO General
Insurance Company. With my: Health App you can:
o Access Your Policy Details
• Manage Your policy, download Your policy schedule and access to
Your e-card will always be at Your ngertips, 24 x 7.
o Policy Endorsement made easy
• By submitting a request to us through my:Health App, you can make
any modications in Your policy, for e.g. change in spelling of the name,
contact number etc.
o Effortless Claims Management
• Now you can Submit Your claims from the app for faster processing and
track the status at Your ngertips. You can also intimate a claim using the
app. You can also view Network hospitals in Your area with directions.
o Stay Active – Short Walks, Big Benets
• The App tracks Your steps, tness session and lets you earn incentive
on renewal discount on Your policy.
38. Newborn Baby means baby born during the Policy Period and is
Aged up to 90 days
39. Network Provider means Hospitals or health care providers enlisted
by an insurer, TPA or jointly by an Insurer and TPA to provide medical
services to an insured by a Cashless facility.
40. Non Network means any Hospital, Day Care Centre or other
provider that is not part of the Network
41. Non-Medical Expenses – Are expenses other than those dened
as Medical Expenses and which are listed on our website www.
hdfcergo.com
42. Notication of Claim means the process of intimating a claim to
the insurer or TPA through any of the recognized modes of
communication
43. OPD Treatment. OPD treatment means the one in which the Insured
visits a clinic / Hospital or associated facility like a consultation room for
diagnosis and treatment based on the advice of a Medical Practitioner.
The Insured is not admitted as a day care or in-patient.
44. Portabilitymeans transfer by an individual health insurance policy
holder (including family cover) of the credit gained for pre-existing
conditions and time bound exclusions if he/she chooses to switch from
one insurer to another.
45. Pre Existing Disease means any condition, ailment or Injury or
related condition(s) forwhich there were signs or symptoms, and / or
were diagnosed, and / or for which Medical Advice / treatment was
received within 48 months prior to the rst policy issued by the insurer
and renewed continuously thereafter
46. Preventive Health Check-up -Preventive Health Check-up means a
package of medical test(s) undertaken for general assessment of health
status, it does not include any diagnostic or investigative medical tests
for evaluation of illness or a disease.
47. Policy means Your statements in the proposal form (which are
the basis of this Policy), this policy wording (including endorsements,
if any), and the Policy Schedule (as the same may be amended from
time to time).
48. Policy Period means the period between the Commencement Date
and the Expiry Date specied in the Policy Schedule
49. Policy Holder means Person who has proposed the Policy and in
whose name the Policy is issued
50. Policy Schedule means Schedule attached to and forming part
of this Policy mentioning the details of the Insured Persons, the Sum
Insured, the period and the limits to which benets under the Policy
are subject to (Schedule of coverage), including any Annexures and/
or endorsements, made to or on it from time to time, and if more than
one, then the latest in time.
51. Policy Year means a year following the Commencement Date and
its subsequent annual anniversary.
52. Pre-hospitalization Medical Expenses means Medical Expenses
incurred during pre-dened number of days
preceding the Hospitalization of the Insured Person , provided that:
i. Such Medical Expenses are incurred for the same condition for which
the Insured Person’s Hospitalization was required, and
ii. The In-patient Hospitalization claim for such Hospitalization is
admissible by the Insurance Company
53. Post-hospitalization Medical Expenses means Medical Expenses
incurred during pre-dened number of days immediately after the insured
person is discharged from the Hospital provided that:
i. Such Medical Expenses are for the same condition for which the
insured person’s Hospitalization was required, and
ii. The inpatient Hospitalization claim for such Hospitalization is
admissible by the insurance company.
54. Qualied Nurse is a person who holds a valid registration from
the nursing council of India or the nursing council of any state in India
55. Renewal means the terms on which the contract of insurance can
be renewed on mutual consent with a provision of Grace Period for
treating the Renewal continuous for the purpose of gaining credit for Pre-
Existing Diseases, time-bound exclusions and for all waiting periods
56. Room Rent means the amount charged by a Hospital towards
Room and Boarding expenses and shall include the associated Medical
Expenses
57. Reasonable and Customary Charges means the charges for

39
services or supplies, which are the standard charges for a specic
provider and consistent with the prevailing charges in the geographical
area for identical or similar services ,taking into account the nature of
Illness/ Injury involved.
58. Sum Insuredmeans the sum shown in the Policy Schedule which
represents Our maximum liability for each Insured Person for any and
all benets claimed for during the Policy Year, and in relation to a Family
Floater represents Our maximum liability for any and all claims made by
You and all of Your Dependents during the Policy Year
59. Surgery or Surgical Proceduremeans manual and / or operative
procedure (s) required for treatment of an Illness or Injury, correction
of deformities and defects, diagnosis and cure of diseases, relief from
suffering and prolongation of life, performed in a Hospital or Day Care
Centre by a medical practitioner.
60. Unproven/Experimental Treatment is a treatment including drug
experimental therapy, which is based on established medical practice
in India, is a treatment experimental or unproven.
61. We/Our/Us means the HDFC ERGO General Insurance Company
Limited
62. You/Your/Policyholder means the person named in the Policy
Schedule who is insured under the Policy or has proposed and concluded
this Policywith Us.
Denitions Applicable to Section 2: my:health Critical Suraksha
Plus
1. Malignant Cancer of Specied sites (Female) – Breast, Cervix,
Uterus, Fallopian Tube, Ovary, Vagina/Vulva
A malignant tumour characterized by the uncontrolled growth and spread
of malignant cells with invasion and destruction of normal tissues. This
diagnosis must be supported by histological evidence of malignancy. The
term cancer includes leukaemia, lymphoma and sarcoma.
The following are excluded:
i. All tumours which are histologically described as carcinoma in situ,
benign, pre-malignant, borderline malignant, low malignant potential,
neoplasm of unknown behavior, or non-invasive, including but not
limited to: Carcinoma in situ of breasts, Cervical dysplasia CIN-1,
CIN - 2 and CIN-3.
ii. Any non-melanoma skin carcinoma unless there is evidence of
metastases to lymph nodes or beyond;
iii. Malignant melanoma that has not caused invasion beyond the
epidermis;
iv. All tumours of the prostate unless histologically classied as having
a Gleason score greater than 6 or having progressed to at least clinical
TNM classication T2N0M0
v. All Thyroid cancers histologically classified as T1N0M0 (TNM
Classication) or below;
vi. Chronic lymphocytic leukaemia less than RAI stage 3
vii. Non-invasive papillary cancer of the bladder histologically described
as TaN0M0 or of a lesser classication,
viii. All Gastro-Intestinal Stromal Tumours histologically classied as
T1N0M0 (TNM Classication) or below and with mitotic count of less
than or equal to 5/50 HPFs;
ix. All tumours in the presence of HIV infection.
x. Tumors of any other sites except Breast, Cervix, Uterus, Fallopian
Tube, Ovary, Vagina/Vulva
2. Malignant Cancer of Specied sites (Male)-Head and Neck, Lung,
Stomach, Colorectum, Prostate
A malignant tumour characterized by the uncontrolled growth and spread
of malignant cells with invasion and destruction of normal tissues. This
diagnosis must be supported by histological evidence of malignancy. The
term cancer includes leukaemia, lymphoma and sarcoma.
The following are excluded:
i. All tumours which are histologically described as carcinoma in situ,
benign, pre-malignant, borderline malignant, low malignant potential,
neoplasm of unknown behavior, or non-invasive, including but not
limited to: Carcinoma in situ of breasts, Cervical dysplasia CIN-1,
CIN - 2 and CIN-3.
ii. Any non-melanoma skin carcinoma unless there is evidence of
metastases to lymph nodes or beyond;
iii. Malignant melanoma that has not caused invasion beyond the
epidermis;
iv. All tumours of the prostate unless histologically classied as having
a Gleason score greater than 6 or having progressed to at least clinical
TNM classication T2N0M0
v. All Thyroid cancers histologically classified as T1N0M0 (TNM
Classication) or below;
vi. Chronic lymphocytic leukaemia less than RAI stage 3
vii. Non-invasive papillary cancer of the bladder histologically described
as TaN0M0 or of a lesser classication,
viii. All Gastro-Intestinal Stromal Tumours histologically classied as
T1N0M0 (TNM Classication) or below and with mitotic count of less
than or equal to 5/50 HPFs;
ix. All tumours in the presence of HIV infection.
x. Tumors of any other sites except Head and Neck, Lung, Stomach,
Colorectum, Prostate
3. Cancer of specied severity
A malignant tumour characterized by the uncontrolled growth and spread
of malignant cells with invasion and destruction of normal tissues. This
diagnosis must be supported by histological evidence of malignancy. The
term cancer includes leukaemia, lymphoma and sarcoma.
The following are excluded:
x. All tumours which are histologically described as carcinoma in situ,
benign, pre-malignant, borderline malignant, low malignant potential,
neoplasm of unknown behaviour, or non-invasive, including but not
limited to: Carcinoma in situ of breasts, Cervical dysplasia CIN-1,
CIN - 2 and CIN-3.
xi. Any non-melanoma skin carcinoma unless there is evidence of
metastases to lymph nodes or beyond;
xii. Malignant melanoma that has not caused invasion beyond the
epidermis;
xiii. All tumours of the prostate unless histologically classied as having
a Gleason score greater than 6 or having progressed to at least clinical
TNM classication T2N0M0
xiv. All Thyroid cancers histologically classied as T1N0M0 (TNM
Classication) or below;
xv. Chronic lymphocytic leukaemia less than RAI stage 3
xvi. Non-invasive papillary cancer of the bladder histologically described
as TaN0M0 or of a lesser classication,
xvii. All Gastro-Intestinal Stromal Tumours histologically classied as
T1N0M0 (TNM Classication) or below and with mitotic count of less
than or equal to 5/50 HPFs;
xviii. All tumours in the presence of HIV infection.
4. Carcinoma In Situ (CiS)
Carcinoma-in-situ shall mean rst ever histologically proven, localized
pre-invasion lesion where cancer cells have not yet penetrated the
basement membrane or invaded (in the sense of inltrating and / or
actively destroying) the surrounding tissues or stroma in any one of the
following covered organ groups, and subject to any classication stated:
i. Breast, where the tumour is classied as Tis according to the TNM
Staging method;
ii. Corpus uteri, vagina, vulva or fallopian tubes where the tumour
is classied as Tis according to the TNM Staging method or FIGO
(staging method of the Federation Internationale de Gynecologie et
d’Obstetrique) Stage 0;
iii. Cervix uteri, classied as cervical intraepithelial neoplasia grade
III (CIN III) or as Tis according to the TNM Staging method or FIGO
Stage 0;
iv. Ovary –include borderline ovarian tumours with intact capsule, no

40
tumour on the ovarian surface, classied as T1aN0M0, T1bN0M0 (TMN
Staging) or FIGO 1A, FIGO 1B
v. Colon and rectum; Penis; Testis; Lung; Liver; Stomach, Nasopharynx
and oesophagus;
vi. Urinary tract, for the purpose of in-situ cancers of the bladder, stage
Ta of papillary Carcinoma is included.
The diagnosis of the Carcinoma in situ must always be supported by a
histopathological report. Furthermore, the diagnosis of Carcinoma in situ
must always be positively diagnosed upon the basis of a microscopic
examination of the xed tissue, supported by a biopsy result. Clinical
diagnosis does not meet this standard.
5. Early Stage Cancer
Early stage Cancers shall mean rst ever presence of one of the following
malignant conditions:
i. Prostate Cancer that is histologically described using the TNM
Classication as T1N0M0 or Prostate cancers described using another
equivalent classication.
ii. Thyroid Cancer that is histologically described using the TNM
Classication as T1N0M0.
iii. Tumours of the Urinary Bladder histologically classied as T1N0M0
(TNM Classication).
iv. Chronic Lymphocytic Leukaemia (CLL) RAI Stage 1 or 2. CLL RAI
Stage 0 or lower is excluded.
v. Malignant melanoma that has not caused invasion beyond the
epidermis. Other skin carcinoma are excluded.
vi. Hodgkin’s lymphoma Stage I by the Cotswolds classication staging
system.
The Diagnosis must be based on histopathological features and
conrmed by a Pathologist.
6. Aplastic Anaemia
I. Chronic persistent bone marrow failure which results in anaemia,
neutropenia and thrombocytopenia requiring treatment with at least
one of the following:
a. Blood product transfusion;
b. Marrow stimulating agents;
c. Immunosuppressive agents; or
d. Bone marrow transplantation.
II. The diagnosis must be conrmed by a hematologist using relevant
laboratory investigations including Bone Marrow Biopsy resulting in
bone marrow cellularity of less than 25% which is evidenced by any
two of the following:
(a) Absolute neutrophil count of less than 500/mm³ or less
(b) Platelets count less than 20,000/mm³ or less
(c) Reticulocyte count of less than 20,000/mm³ or less
III. Temporary or reversible Aplastic Anaemia is excluded.
7. Major Organ Transplant – Bone Marrow
I. The actual undergoing of a transplant ofHuman bone marrow using
haematopoietic stem cells. The undergoing of a transplant has to be
conrmed by a specialist medical practitioner.
II. The following are excluded:
a. Other stem-cell transplants
b. Where only islets of langerhans are transplanted
8. Open Chest CABG
III. The actual undergoing of heart surgery to correct blockage or
narrowing in one or more coronary artery(s), by coronary artery bypass
grafting done via a sternotomy (cutting through the breast bone) or
minimally invasive keyhole coronary artery bypass procedures. The
diagnosis must be supported by a coronary angiography and the
realization of surgery has to be conrmed by a cardiologist.
IV. The following are excluded:
b. Angioplasty and/or any other intra-arterial procedures
9. Myocardial Infarction (First Heart Attack of specied severity)
III. The rst occurrence of heart attack or myocardial infarction, which
means the death of a portion of the heart muscle as a result of inadequate
blood supply to the relevant area. The diagnosis for Myocardial Infarction
should be evidenced by all of the following criteria:
d. A history of typical clinical symptoms consistent with the diagnosis of
acute myocardial infarction (For e.g. typical chest pain)
e. New characteristic electrocardiogram changes
f. Elevation of infarction specic enzymes, Troponins or other specic
biochemical markers.
IV. The following are excluded:
d. Other acute Coronary Syndromes
e. Any type of angina pectoris
f. A rise in cardiac biomarkers or Troponin T or I in absence of overt
ischemic heart disease OR following an intra-arterial cardiac procedure.
10. Open Heart Replacement or Repair of Heart Valves
The actual undergoing of open-heart valve surgery is to replace or
repair one or more heart valves, as a consequence of defects in,
abnormalities of, or disease- affected cardiac valve(s). The diagnosis of
the valve abnormality must be supported by an echocardiography and
the realization of surgery has to be conrmed by a specialist medical
practitioner. Catheter based techniques including but not limited to,
balloon valvotomy/valvuloplasty are excluded.
11. Major Organ Transplant – Heart
I. The actual undergoing of a transplant of heart, that resulted from
irreversible end-stage failure of the relevant organ,
a. The undergoing of a transplant has to be conrmed by a specialist
medical practitioner.
II. The following are excluded:
a. Other stem-cell transplants
b. Where only islets of langerhans are transplanted
12. Surgery of Aorta
The actual undergoing of medically necessary surgery for a disease of
the aorta needing excision and surgical replacement of the diseased
aorta with a graft. For the purpose of this denition aorta shall mean
the thoracic and abdominal aorta but not its branches. Traumatic injury
of the aorta is excluded.
13. Primary (Idiopathic) Pulmonary Hypertension
IV. An unequivocal diagnosis of Primary (Idiopathic) Pulmonary
Hypertension by a Cardiologist or specialist in respiratory medicine
with evidence of right ventricular enlargement and the pulmonary
artery pressure above 30 mm of Hg on Cardiac Cauterization. There
must be permanent irreversible physical impairment to the degree of
at least Class IV of the New York Heart Association Classication of
cardiac impairment.
V. The NYHA Classication of Cardiac Impairment are as follows:
iii. Class III: Marked limitation of physical activity. Comfortable at rest,
but less than ordinary activity causes symptoms.
iv. Class IV: Unable to engage in any physical activity without discomfort.
Symptoms may be present even at rest.
VI. Pulmonary hypertension associated with lung disease, chronic
hypoventilation, pulmonary thromboembolic disease, drugs and toxins,
diseases of the left side of the heart, congenital heart disease and any
secondary cause are specically excluded.
14. Other serious coronary artery disease
I. Severe coronary artery disease in which at least three (3) major
coronary arteries are individually occluded by a minimum of sixty percent
(60%) or more, as proven by coronary angiogram only (non-invasive
diagnostic procedures excluded).
II. For purposes of this denition, “major coronary artery” refers to any of
the left main stem artery, left anterior descending artery, circumex artery
and right coronary artery (but not including their branches).

41
15. Dissecting Aortic Aneurysm
I. A condition where the inner lining of the aorta (intima layer) is
interrupted so that blood enters the wall of the aorta and separates its
layers. For the purpose of this denition, aorta shall mean the thoracic
and abdominal aorta but not its branches. The diagnosis must be made
by a Registered Medical practitioner who is a specialist with computed
tomography (CT) scan, magnetic resonance imaging (MRI), magnetic
resonance angiograph (MRA) or angiogram. Emergency surgical repair
is required.
16. Cardiomyopathy
An impaired function of the heart muscle, unequivocally diagnosed
as Cardiomyopathy by a Registered Medical practitioner who is a
cardiologist, and which results in permanent physical impairment to
the degree of New York Heart Association Classication Class IV,
or its equivalent, for at least six (6) months based on the following
classication criteria:
i. Class IV – inability to carry out an activity without discomfort. Symptoms
of congestive cardiac failure are present even at rest. With any increase
in physical activity, discomfort will be experienced.
ii. The Diagnosis of Cardiomyopathy has to be supported by echographic
ndings of compromised ventricular performance.
iii. Irrespective of the above, Cardiomyopathy directly related to alcohol
or drug abuse is excluded.
17. Infective Endocarditis
Inammation of the inner lining of the heart caused by infectious
organisms, where all of the following criteria are met:
(a) Positive result of the blood culture proving presence of the infectious
organism(s);
(b) Presence of at least moderate heart valve incompetence (meaning
regurgitant fraction of 20% or above) or moderate heart valve stenosis
(resulting in heart valve area of 30% or less of normal value) attributable
to Infective Endocarditis; and
(c) The Diagnosis of Infective Endocarditis and the severity of valvular
impairment are conrmed by a Registered Medical practitioner who is
a cardiologist.
18. Eisenmenger’s Syndrome
Development of severe pulmonary hypertension and shunt reversal
resulting from heart condition. The diagnosis must be made by a
Registered Medical practitioner who is a specialist with echocardiography
and cardiac catheterization and supported by the following criteria:
1. Mean pulmonary artery pressure > 40 mm Hg;
2. Pulmonary vascular resistance > 3mm/L/min (Wood units); and
3. Normal pulmonary wedge pressure < 15 mm Hg.
19. Angioplasty
i. Coronary Angioplasty is dened as percutaneous coronary intervention
by way of balloon angioplasty with or without stenting for treatment of the
narrowing or blockage of minimum 50% of one or more major coronary
arteries. The intervention must be determined to be medically necessary
by a cardiologist and supported by a coronary angiogram (CAG).
ii. Coronary arteries herein refer to left main stem, left anterior
descending, circumex and right coronary artery.
iii. Diagnostic angiography or investigation procedures without
angioplasty/stent insertion are excluded.
20. Balloon Valvotomy or Valvuloplasty
An interventional procedure involving Percutaneous heart valve repair
by balloon valvotomy or valvuloplasty to repair narrowing of heart valves
using a catheter.
Payout will be based on the actual undergoing of surgery. The need
for surgery should be certied by a cardiologist and supported by an
echocardiography
21. Insertion of Pacemaker
Insertion of a permanent cardiac pacemaker that is required as a result
of life threatening cardiac arrhythmias, cardiomyopathy or any other
condition which cannot be treated via other means.
The insertion of the cardiac pacemaker must be certied to be absolutely
necessary by a specialist in the relevant eld.
22. Multiple Sclerosis with persisting symptoms
III. The unequivocal diagnosis of Denite Multiple Sclerosis conrmed
and evidenced by all of the following:
c. investigations including typical MRI ndings which unequivocally
conrm the diagnosis to be multiple sclerosis and
d. there must be current clinical impairment of motor or sensory function,
which must have persisted for a continuous period of at least 6 months.
IV. Other causes of neurological damage such as SLE and HIV are
excluded.
23. Permanent Paralysis of Limbs
a. Total and irreversible loss of use of two or more limbs as a result
of injury or disease of the brain or spinal cord. A specialist medical
practitioner must be of the opinion that the paralysis will be permanent
with no hope of recovery and must be present for more than 3 months.
24. Stroke resulting in permanent symptoms
III. Any cerebrovascular incident producing permanent neurological
sequelae.
a. This includes infarction of brain tissue, thrombosis in an intracranial
vessel, haemorrhage and embolisation from an extracranial source.
b. Diagnosis has to be conrmed by a specialist medical practitioner
and evidenced by typical clinical symptoms as well as typical ndings
in CT Scan or MRI of the brain. Evidence of permanent neurological
decit lasting for at least 3 months has to be produced.
IV. The following are excluded:
d. Transient ischemic attacks (TIA)
e. Traumatic injury of the brain
f. Vascular disease affecting only the eye or optic nerve or vestibular
functions.
25. Benign Brain Tumour
I. Benign brain tumor is dened as a life threatening, non-cancerous
tumor in the brain, cranial nerves or meninges within the skull. The
presence of the underlying tumor must be conrmed by imaging studies
such as CT scan or MRI.
II. This brain tumor must result in at least one of the following and must
be conrmed by the relevant medical specialist.
a. Permanent Neurological decit with persisting clinical symptoms for
a continuous period of at least 90 consecutive days or
b. Undergone surgical resection or radiation therapy to treat the brain
tumor.
III. The following conditions are excluded:
Cysts, Granulomas, malformations in the arteries or veins of the brain,
hematomas, abscesses, pituitary tumors, tumors of skull bones and
tumors of the spinal cord.
26. Coma of specied severity
I. A state of unconsciousness with no reaction or response to external
stimuli or internal needs. This diagnosis must be supported by evidence
of all of the following:
a. no response to external stimuli continuously for at least 96 hours;
b. life support measures are necessary to sustain life; and
c. permanent neurological decit which must be assessed at least 30
days after the onset of the coma.
II. The condition has to be conrmed by a specialist medical practitioner.
a. Coma resulting directly from alcohol or drug abuse is excluded.
27. Parkinson’s Disease
I. The occurrence of Parkinson’s Disease where there is an associated
Neurological Decit that results in Permanent Inability to perform
independently at least three of the activities of daily living as dened
below.

42
1. Transfer: Getting in and out of bed without requiring external physical
assistance
2. Mobility: The ability to move from one room to another without requiring
any external physical assistance
3. Dressing: Putting on and taking of all necessary items of clothing
without requiring any external physical assistance
4. Bathing/Washing: The ability to wash in the bath or shower (including
getting in and out of the bath or shower) or wash by other means
5. Eating: All tasks of getting food into the body once it has been prepared
II. Parkinson’s disease secondary to drug and/or alcohol abuse is
excluded.
28. Alzheimer’s Disease
Clinically established diagnosis of Alzheimer’s Disease (presenile
dementia) resulting in a permanent inability to perform independently
three or more activities of daily living – bathing, dressing/undressing,
getting to and using the toilet, transferring from bed to chair or chair to
bed, continence, eating/drinking and taking medication – or resulting
in need of supervision and permanent presence of care staff due to
the disease. These conditions have to be medically documented for
at least 3 months.
29. Motor Neurone Disease with permanent symptoms
Motor neuron disease diagnosed by a specialist medical practitioner
as spinal muscular atrophy, progressive bulbar palsy, amyotrophic
lateral sclerosis or primary lateral sclerosis. There must be progressive
degeneration of corticospinal tracts and anterior horn cells or bulbar
efferent neurons. There must be current signicant and permanent
functional neurological impairment with objective evidence of motor
dysfunction that has persisted for a continuous period of at least 3
months.
30. Muscular Dystrophy
A group of hereditary degenerative diseases of muscle characterised by
weakness and atrophy of muscle. The diagnosis of muscular dystrophy
must be unequivocal and made by a Registered Medical practitioner
who is a consultant neurologist. The condition must result in the inability
of the Insured to perform (whether aided or unaided) at least 3 of the 6
“Activities of Daily Living” for a continuous period of at least 6 months.
Activities of daily living:
a. Washing: the ability to wash in the bath or shower (including getting
into and out of the shower) or wash satisfactorily by other means and
maintain an adequate level of cleanliness and personal hygiene;
b. Dressing: the ability to put on, take off, secure and unfasten all
garments and, as appropriate, any braces, articial limbs or other
surgical appliances;
c. Transferring: The ability to move from a lying position in a bed to a
sitting position in an upright chair or wheel chair and vice versa;
d. Toileting: the ability to use the lavatory or otherwise manage bowel
and bladder functions so as to maintain a satisfactory level of personal
hygiene;
e. Feeding: the ability to feed oneself, food from a plate or bowl to the
mouth once food has been prepared and made available.
f. Mobility: The ability to move indoors from room to room on level
surfaces at the normal place of residence
31. Apallic Syndrome
Universal necrosis of the brain cortex with the brainstem remaining
intact. The diagnosis must be conrmed by a Neurologist acceptable
to Us and the condition must be documented for at least one month.
32. Bacterial Meningitis
I. Bacterial infection resulting in severe inammation of the membranes of
the brain or spinal cord resulting in signicant, irreversible and permanent
neurological decit. The neurological decit must persist for at least 6
weeks.This diagnosis must be conrmed by:
i. The presence of bacterial infection in cerebrospinal uid by lumbar
puncture; and
ii. A consultant neurologist.
II. Bacterial Meningitis in the presence of HIV infection is excluded.
33. Creutzfeldt-Jakob Disease (CJD)
Creutzfeldt-Jacob disease is an incurable brain infection that causes
rapidly progressive deterioration of mental function and movement. A
Registered Medical practitioner who is a neurologist must make a denite
diagnosis of Creutzfeldt-Jacob disease based on clinical assessment,
EEG and imaging. There must be objective neurological abnormalities
on exam along with severe progressive dementia.
34. Encephalitis
I. Severe inflammation of brain substance (cerebral hemisphere,
brainstem or cerebellum) caused by viral infection and resulting in
permanent neurological decit. This diagnosis must be certied by a
Registered Medical practitioner who is a consultant neurologist and the
permanent neurological decit must be documented for at least 6 weeks.
II. Encephalitis caused by HIV infection is excluded.
35. Major Head Trauma
I. Accidental head injury resulting in permanent Neurological decit to
be assessed no sooner than 3 months from the date of the accident.
This diagnosis must be supported by unequivocal ndings on Magnetic
Resonance Imaging, Computerized Tomography, or other reliable
imaging techniques. The accident must be caused solely and directly
by accidental, violent, external and visible means and independently
of all other causes.
II. The Accidental Head injury must result in an inability to perform at
least three (3) of the following Activities of Daily Living either with or
without the use of mechanical equipment, special devices or other aids
and adaptations in use for disabled persons. For the purpose of this
benet, the word “permanent” shall mean beyond the scope of recovery
with current medical knowledge and technology.
III. The Activities of Daily Living are:
i. Washing: the ability to wash in the bath or shower (including getting
into and out of the bath or shower) or wash satisfactorily by other means;
ii. Dressing: the ability to put on, take off, secure and unfasten all
garments and, as appropriate, any braces, articial limbs or other
surgical appliances;
iii. Transferring: the ability to move from a bed to an upright chair or
wheelchair and vice versa;
iv. Mobility: the ability to move indoors from room to room on level
surfaces;
v. Toileting: the ability to use the lavatory or otherwise manage bowel
and bladder functions so as to maintain a satisfactory level of personal
hygiene;
vi. Feeding: the ability to feed oneself once food has been prepared
and made available.
IV. The following are excluded:
i. Spinal cord injury;
36. Progressive Supranuclear Palsy
Conrmed by a Registered Medical practitioner who is a specialist in
neurology of a denite diagnosis of progressive supranuclear palsy.
There must be permanent clinical impairment of motor function, eye
movement disorder and postural instability.
37. Brain Surgery
The actual undergoing of surgery to the brain under general anaesthesia
during which a craniotomy is performed. Keyhole surgery is included
however, minimally invasive treatment where no surgical incision is
performed to expose the target, such as irradiation by gamma knife or
endovascular neuroradiological interventions such as embolizations,
thrombolysis and stereotactic biopsy are all excluded. Brain surgery
as a result of an Accident is also excluded. The procedure must be
considered medically necessary by a Registered Medical practitioner
who is a qualied specialist.
38. Loss of Speech
I. Total and irrecoverable loss of the ability to speak as a result of injury
or disease to the vocal cords. The inability to speak must be established

43
for a continuous period of 12 months. This diagnosis must be supported
by medical evidence furnished by an Ear, Nose, Throat (ENT) specialist.
II. All psychiatric related causes are excluded.
39. Kidney failure requiring regular dialysis
II. End stage renal disease presenting as chronic irreversible failure of
both kidneys to function, as a result of which either regular renal dialysis
(haemodialysis or peritoneal dialysis) is instituted or renal transplantation
is carried out. Diagnosis has to be conrmed by a specialist medical
practitioner.
40. Major Organ Transplant – Kidney, Lung, Liver and Pancreas
The actual undergoing of a transplant of:
c. One of the following human organs: lung, liver, kidney, pancreas,
that resulted from irreversible end-stage failure of the relevant organ,
d. The undergoing of a transplant has to be conrmed by a specialist
medical practitioner.
The following are excluded:
c. Other stem-cell transplants
d. Where only islets of langerhans are transplanted
41. End Stage Liver Failure
I. Permanent and irreversible failure of liver function that has resulted
in all three of the following:
a. Permanent jaundice; and
b. Ascites; and
c. Hepatic encephalopathy.
II. Liver failure secondary to drug or alcohol abuse is excluded.
42. Medullary Cystic Disease
I. Medullary Cystic Disease where the following criteria are met:
a. the presence in the kidney of multiple cysts in the renal medulla
accompanied by the presence of tubular atrophy and interstitial brosis;
b. clinical manifestations of anaemia, polyuria, and progressive
deterioration in kidney function; and
c. the Diagnosis of Medullary Cystic Disease is conrmed by renal biopsy.
II. Isolated or benign kidney cysts are specically excluded from this
benet.
43. Systemic Lupus Erythematous with LupusNephritis
i. A multi-system autoimmune disorder characterised by the development
of autoantibodies directed against various self-antigens. In respect of this
Policy, systemic lupus erythematosus will be restricted to those forms
of systemic lupus erythematosus which involve the kidneys (Class III to
Class V Lupus Nephritis, established by renal biopsy, and in accordance
with the WHO Classication). The nal diagnosis must be conrmed by
a Registered Doctor specialising in
Rheumatology and Immunology.
ii. The WHO Classication of Lupus Nephritis:
• Class I Minimal Change Lupus Glomerulonephritis
• Class II Mesangial Lupus Glomerulonephritis
• Class III Focal Segmental Proliferative Lupus Glomerulonephritis
• Class IV Diffuse Proliferative Lupus Glomerulonephritis
• Class V Membranous Lupus Glomerulonephritis
44. End Stage Lung Failure
I. End stage lung disease, causing chronic respiratory failure, as
conrmed and evidenced by all of the following:
a. FEV1 test results consistently less than 1 litre measured on 3
occasions 3 months apart; and
b. Requiring continuous permanent supplementary oxygen therapy for
hypoxemia; and
c. Arterial blood gas analysis with partial oxygen pressure of 55mmHg
or less (PaO2 < 5mmHg); and
d. Dyspnoea at rest.
45. Fulminant Hepatitis
I. A sub-massive to massive necrosis of the liver by the Hepatitis virus,
leading precipitously to liver failure. This diagnosis must be supported
by all of the following:
a. Rapid decreasing of liver size;
b. Necrosis involving entire lobules, leaving only a collapsed reticular
framework;
c. Rapid deterioration of liver function tests;
d. Deepening jaundice; and
e. Hepatic encephalopathy.
II. Acute Hepatitis infection or carrier status alone does not meet the
diagnostic criteria.
46. Chronic Adrenal Insufciency (Addison’s Disease)
I. An autoimmune disorder causing a gradual destruction of the adrenal
gland resulting in the need for life long glucocorticoid and mineral
corticoid replacement therapy. The disorder must be conrmed by a
Registered Medical practitioner who is a specialist in endocrinology
through one of the following:
1. ACTH simulation tests;
2. insulin-induced hypoglycemia test;
3. plasma ACTH level measurement;
4. Plasma Renin Activity (PRA) level measurement.
II. Only autoimmune cause of primary adrenal insufciency is included.
All other causes of adrenal insufciency are excluded.
47. Progressive Scleroderma
I. A systemic collagen-vascular disease causing progressive diffuse
brosis in the skin, blood vessels and visceral organs. This diagnosis
must be unequivocally supported by biopsy and serological evidence
and the disorder must have reached systemic proportions to involve
the heart, lungs or kidneys.
II. The following are excluded:
1. Localised scleroderma (linear scleroderma or morphea);
2. Eosinophilic fasciitis; and
3. CREST syndrome.
48. Chronic Relapsing Pancreatitis
I. An unequivocal diagnosis of Chronic Relapsing Pancreatitis, made by
a Registered Medical practitioner who is a specialist in gastroenterology
and conrmed as a continuing inammatory disease of the pancreas
characterised by irreversible morphological change and typically
causing pain and/or permanent impairment of function. The condition
must be conrmed by pancreatic function tests and radiographic and
imaging evidence.
II. Relapsing Pancreatitis caused directly or indirectly, wholly or partly,
by alcohol is excluded.
49. Elephantiasis
I. Massive swelling in the tissues of the body as a result of destroyed
regional lymphatic circulation by chronic filariasis infection. The
unequivocal diagnosis of elephantiasis must be confirmed by a
Registered Medical practitioner who is a specialist physician. There
must be clinical evidence of permanent massive swelling of legs, arms,
scrotum, vulva, or breasts. There must also be laboratory conrmation
of microlariae infection.
II. Swelling or lymphedema caused by infection with a sexually
transmitted disease, trauma, post-operative scarring, congestive heart
failure, or congenital lymphatic system abnormalities is excluded.
50. HIV due to blood transfusion and occupationally acquired HIV
I. Infection with the Human Immunodeciency Virus (HIV) through a
blood transfusion, provided that all of the following conditions are met:
a. The blood transfusion was medically necessary or given as part of
a medical treatment;
b. The blood transfusion was received in India after the Policy Date,
Date of endorsement , whichever is the later;

44
c. The source of the infection is established to be from the Institution
that provided the blood transfusion and the Institution is able to trace
the origin of the HIV tainted blood; and
d. The Insured does not suffer from Thalassaemia Major or Haemophilia.
II. Infection with the Human Immunodeciency Virus (HIV) which resulted
from an Accident occurring after the Policy inception Date, renewal dates,
whichever is the later whilst the Insured was carrying out the normal
professional duties of his or her occupation in India, provided that all of
the following are proven to the Company’s satisfaction:
1. Proof that the Accident involved a denite source of the HIV infected
uids;
2. Proof of sero-conversion from HIV negative to HIV positive occurring
during the 180 days after the documented Accident. This proof must
include a negative HIV antibody test conducted within 5 days of the
Accident; and
3. HIV infection resulting from any other means including sexual activity
and the use of intravenous drugs is excluded.
This benet is only payable when the occupation of the Insured is a
Registered Medical practitioner, housemen, medical student, registered
nurse, medical laboratory technician, dentist (surgeon and nurse) or
paramedical worker, working in medical centre or clinic in India. This
benet will not apply under either section a or b where a cure has become
available prior to the infection. “Cure” means any treatment that renders
the HIV inactive or non-infectious.
51. Terminal Illness
The conclusive diagnosis of an illness, which in the opinion of a Medical
Practitionerwho is an attending Consultant and agreed by our appointed
Registered Medical practitioner, life expectancy is no greater than twelve
(12) months from the date of notication of claim, regardless of any
treatment that might be undertaken.
52. Myelobrosis
A disorder which can cause brous tissue to replace the normal bone
marrow and results in anaemia, low levels of white blood cells and
platelets and enlargement of the spleen. The condition must have
progressed to the point that it is permanent and the severity is such
that the Insured requires a blood transfusion at least monthly. The
diagnosis of myelobrosis must be supported by bone marrow biopsy
and conrmed by a Registered Medical practitioner who is a specialist.
53. Pheochromocytoma
I. Presence of a neuroendocrine tumour of the adrenal or extra-
chromafn tissue that secretes excess catecholamines requiring the
actual undergoing of surgery to remove the tumour.
II. The Diagnosis of Pheochromocytoma must be conrmed by a
Registered Medical practitioner who is an endocrinologist.
54. Crohn’s Disease
I. Crohn’s Disease is a chronic, transmural inammatory disorder
of the bowel. To be considered as severe, there must be evidence
of continued inammation in spite of optimal therapy, with all of the
following having occurred:
5. Stricture formation causing intestinal obstruction requiring admission
to hospital, and
6. Fistula formation between loops of bowel, and
7. At least one bowel segment resection.
II. The diagnosis must be made by a Registered Medical practitioner
who is a specialist Gastroenterologist and be proven histologically on
a pathology report and/or the results of sigmoidoscopy or colonoscopy.
55. Severe Rheumatoid Arthritis
Unequivocal Diagnosis of systemic immune disorder of rheumatoid
arthritis where all of the following criteria are met:
i. Diagnostic criteria of the American College of Rheumatology for
Rheumatoid Arthritis;
ii. Permanent inability to perform at least two (2) “Activities of Daily
Living”;
iii. Widespread joint destruction and major clinical deformity of three (3)
or more of the following joint areas: hands, wrists, elbows, knees, hips,
ankle, cervical spine or feet; and
iv. The foregoing conditions have been present for at least six (6) months.
56. Severe Ulcerative Colitis
I. Acute fulminant ulcerative colitis with life threatening electrolyte
disturbances.
II. All of the following criteria must be met:
1. the entire colon is affected, with severe bloody diarrhoea; and
2. the necessary treatment is total colectomy and ileostomy; and
3. the diagnosis must be based on histopathological features and
conrmed by a Registered Medical practitioner who is a specialist in
gastroenterology.
57. Deafness
Total and irreversible loss of hearing in both ears as a result of illness
or accident. This diagnosis must be supported by pure tone audiogram
test and certied by an Ear, Nose and Throat (ENT) specialist. Total
means “the loss of hearing to the extent that the loss is greater than 90
decibels across all frequencies of hearing” in both ears.
58. Blindness
I. Total, permanent and irreversible loss of all vision in both eyes as a
result of illness or accident.
II. The Blindness is evidenced by:
a. corrected visual acuity being 3/60 or less in both eyes or;
b. the eld of vision being less than 10 degrees in both eyes.
III. The diagnosis of blindness must be conrmed and must not be
correctable by aids or surgical procedure.
59. Third Degree Burns
There must be third-degree burns with scarring that cover at least 20%
of the body’s surface area. The diagnosis must conrm the total area
involved using standardized, clinically accepted, body surface area
charts covering 20% of the body surface area.
Denitions applicable to Section 3: my:health Medisure Super
Top Up
1. For Super Top Up : Dependents: mean only the family members
listed below:
• Your legally married spouse ,
• Your dependent children – being your children (natural or legally
adopted) aged between 3 months and 23 years, who is/are nancially
dependent on the primary insured or proposer and does not have his /
her independent sources of income.
• Your parents or parents-in-law
2. Disease: means an alteration in the state of the body or of some of
its organs, interrupting or disturbing the performance of the functions,
and causing or threatening pain and weakness or physical or mental
disorder and certied by a Medical Practitioner to that effect.
3. Subrogation: Subrogation shall mean the right of the Insurer to
assume the rights of the Insured person to recover expenses paid out
under the Policy that may be recovered from any other source.
Denitions Applicable to Section 5 : Personal Accident Insurance
1. Daily Home Allowance means the amount payable for every
twenty-four (24) continuous hours an Insured Person is instructed by
a Physician to complete his/her recovery at home following a payment
of the Daily Benet.
2. Immediate Family / Immediate Family Member means an Insured
Person’sSpouse; children; children-in-law; siblings; siblings-in-law;
parents; parents-in-law; grandparents; grandchildren; legal guardian,
ward; step or adopted children; step-parents; aunts, uncles; nieces,
and nephews, who reside in the same country as the Insured Person.
3. Nominated Account means the account nominated by the
Policyholder in the Proposal Form, or as subsequently instructed by
the Policyholder in writing, to which premiums for this Policy are to

45
be debited/ charged.
Denitions Applicable to Section 6 : Travel Insurance
1. Insured Journey means a trip commencing during the Period of
Insurance. The Company agrees to continue the insurance for an
Insured Person who commences an Insured Journey before the Policy
Expiration Date, on the proviso that premium has been paid for such
Insured Journey and the return trip is within One hundred Eighty (180)
Days after the Insured Journey commences.
2. Medical Treatment means a Physician’s medical advice, treatment,
consultations, and prescribed or remedial attention
Denitions Applicable to Section 5 : Personal Accident Insurance
and Section 6:Travel Insurance
1. Accumulation Limit means the maximum amount payable by the
Company in respect of any one Accident, irrespective of the number
of Insured Persons involved in such Accident. In the event that an
Accident occurs which results in insurable losses under this Policy and
which ordinarily would mean that the Accumulation Limit is exceeded,
the Accumulation Limit amount will be distributed on a proportional
basis to all Insured Persons, taking into account the maximum Sums
Insured per Benet and per Insured Person
2. Any one illness means continuous Period of illness and it includes
relapse within 45 days from the date of last consultation with the Hospital/
Nursing Home where treatment may have been taken.
3. Assistance Provider means the assistance company with whom the
Company contracts, as an independent contractor, to provide travel-
related emergency assistance services.
4. Beneficiary: In case of death of the Insured Person, the
Beneciary means, unless stipulated otherwise by the Insured
Person, the surviving Spouse of the Insured Person, mentally capable
and not divorced, followed by the children recognized or adopted
followed by the Insured Person’s legal heirs or nominees. For all
other benets, the Beneciary means the Insured Person himself
unless stipulated otherwise.
5. Civil War means armed opposition, whether declared or not, between
two or more parties belonging to the same country where the opposing
parties are of different ethnic, religious or ideological groups. Included
in the denition: armed rebellion, revolution, sedition, insurrection, Coup
d’ Etat, the consequences of Martial law.
6. Close Business Associate means:
a. a business associate not a fellow employee of the Insured Person
where the business relationship with the Insured Person is continuous
and reliant on each other for the Insured Person’s business, or
b. a business companion who travels with the Insured Person for the
same business purpose, and whose presence is necessary for the
Insured Person’s business, or
c. a fellow employee of the Insured Person.
7. Common Carrier means any land, sea or air conveyance operated
under a licence issued by a governmental authority having jurisdiction,
for the transportation of fare paying passengers and which has xed,
established routes only.
8. Compensation means Sum Insured, Total Sum Insured or
percentage of the Sum Insured, as appropriate.
9. Daily Activities means activities such as, but not limited to, cooking
and/or taking of food, discharging of urine and/or faeces, getting
dressed or undressed, washing and taking a bath, walking and general
living activities.
10. Daily Benet means the amount payable for every twenty-four (24)
continuous hours an Insured Person is in Hospital as an in-patient up
to the maximum number of Days stated in the Schedule
11. Date of Loss:
o ForAccident means the date of the Accident.
o for all other benets means the date the event happened that leads
to an alleged claim.
o For Sickness means the rst date of diagnosis or the date the Insured
Person rst became aware of the Sickness.
12. Day means a continuous period of twenty-four (24) hours.
13. Family Accumulation Limit means the maximum amount payable
by the Company in respect of any one Accident, irrespective of the
number of Insured Persons from the same Immediate Family involved
in such Accident. In the event that an Accident occurs which results in
insurable losses under this Policy and which ordinarily would mean that
the Family Accumulation Limit is exceeded, the Family Accumulation
Limit amount will be distributed on a proportional basis to all Insured
Persons from the same Immediate Family, taking into account the
maximum Sums Insured per Benet and per Insured Person.
14. Foreign War means armed opposition, whether declared or not
between two countries.
15. Franchise means an amount stated in the Schedule as a percentage
or a xed amount for which the Company will not be responsible if the
claim falls below such percentage or xed amount, or a period of time
for which the Company will not be responsible unless the period of
time has expired.
16. Immediate Family / Immediate Family Member means an
Insured Person’s Spouse; children; children-in-law; siblings;
siblings-in-law; parents; parents-in-law; grandparents; grandchildren;
legal guardian, ward; step or adopted children; step-parents; aunts,
uncles; nieces, and nephews, who reside in the same country as the
Insured Person.
17. Operative Time means the time that the insurance is effective as
stated on the Schedule
18. Permanent Total Disablement means disablement, as the result
of a Bodily Injury, which:
o continues for a period of twelve (12) consecutive months, and
o is conrmed as total, continuous and permanent by a Physician after
the twelve (12) consecutive months, and
o entirely prevents an Insured Person from engaging in or giving
attention to gainful occupation of any and every kind for the remainder
of his/her life.
19. Primary Insured Person means the Insured Person who elects
insurance under the Policy and pays all the required premium for
the insurance elected
20. Salary means the total gross basic annual salary excluding
payments for overtime, commission or bonus payable by the
Policyholder to the Insured Person at the time of the Date of Loss.
For weekly paid Insured Persons, the Salary will be calculated by
taking the average gross weekly basic salary of the Insured Person
for the thirteen (13) weeks prior to the Date of Loss and multiplying
this amount by fty-two (52).
21. Serious Injury or Serious Sickness means Bodily Injury or
Sickness certied as being dangerous to life by a Physician.
22. Sickness means any fortuitous somatic illness or disease but
excluding any disease or illness which is, arises out of or is caused
by a condition or defect for which medical treatment was recognized,
advised, sought out, or should have reasonably sought out, or received
at any time before the Period of Insurance.
23. Spouse means an Insured Person’s husband or wife who is
recognized as such by the laws of the jurisdiction in which they reside.
24. Subrogation shall mean the right of the insurer to assume the rights
of the insured person to recover expenses paid out under the policy that
may be recovered from any other source.
25. Terrorism means activities against persons, organisations or
property of any nature:
1) that involve the following or preparation for the following:
a) use or threat of force or violence; or
b) commission or threat of a dangerous act; or
c) commission or threat of an act that interferes with or disrupts an
electronic, communication, information or mechanical system; and
2) when one or both of the following applies:

46
a) the effect is to intimidate or coerce a government or the civilian
population or any segment thereof, or to disrupt any segment of the
economy; or
b) it appears that the intent is to intimidate or coerce a government, or to
further political, ideological, religious, social or economic objectives or to
express (or express opposition to) a philosophy or ideology.
26. Total Number of Travel Days meansthe maximum number of days
insured under the Policy.
Denitions applicable forSection 7: Home Insurance - Revision
1. “Building” means structure (above plinth and foundation excluding
land) of standard construction unless specically mentioned. It shall
include connected utilities, sanitary ttings, xtures and ttings therein
belonging to the Insured and for which he is accountable.
2. “Contents” means all items/articles owned or held in trust by the
Insured and his/her family members residing in the same home for which
the Insured is accountable.
3. “Jewellery” means articles of precious stones, gold, silver or other
precious metals.
4. “Market Value” means Replacement Value less depreciation.
5. “Personal Effects” means clothing, spectacles, umbrellas, footwear,
etc.
6. “Reinstatement Value” means the cost of replacing or reinstating on
the same site, property of the same kind or type but not superior to or
more extensive than the insured property when new.
7 “Single Article” is dened as one distinct physical object having an
independent economic value.
8. “Specied Items” means jewellery, curios, antiques, pictures and
other works of art, collection of stamps, coins and medals.
9. “Standard Construction” means any construction with RCC/ RBC/
Tiles/ ACC roof and external walls of Burnt bricks/ Stone/ Concrete
blocks.
10. “Valuables” means carpets (other than normal wall to wall carpets),
telephone instruments, photographic equipment including still & video
cameras), clocks, binoculars, telescopes, musical instruments, audio
and video equipment, computers (including laptops) & other peripheral
equipment, watches, mobile phones, calculators, digital diaries and
palm tops.
Denitions applicable for Section 8:E@SECURE Insurance
1. Bank Account: YourBank Account details including personal
e-banking login name, passwords or Bank Account number that are
issued by banks operating in India.
2. Bank Rate: Means Bank rate xed by the Reserve Bank of India
(RBI) at the beginning of the nancial year in which claim has fallen due
3. Credit/Debit Card: Yourphysical Credit/Debit Card, Credit/Debit
Card details or Credit/Debit Card numbers that are issued by banks
operating in India.
4. Cyber Bullying or Harassment: Means an aggressive, intentional
act or behavior that is carried out by a group or an individual, using
electronic forms of contact, repeatedly and over time against a victim
who cannot easily defend himself or herself.
Cyber bullying or harassment includes any of the following but not
limited to: posting rumors about a person, sexual remarks, threats to
disclose victims’ personal information, or pejorative labels, internet
trolling and cyber stalking.
5. Computer System: Means Your electronic data storage or computing
devices including input and output support devices and excluding
calculators which are not programmable and capable of being used in
conjunction with external les, which contain ComputerProgrammes,
electronic instructions, input Data and output Data, that performs
logic, arithmetic, Data storage and retrieval, communication control
and other functions. Computer System shall include all kinds of digital
devices including but is not limited to mobile phones, laptops, personal
computers.
6. Endorsement: An authorized amendment to this Policy
7. Extortion Loss: means any:
i. monies paid by You with Our prior written consent to prevent or end
an Extortion Threat; or
ii. Professional Fees for independent advisors to conduct an
investigation to determine the cause of an Extortion Threat
8. Email Spoong: means forgery of an email header so that expected
and awaited message appears to have originated from a legitimate
source, instead was sent by someone from somewhere other than the
actual legitimate and/or trusted source
9. Extortion Threat: means any threat or connected series of threats,
for the purpose of demanding monies, communicated to You to prevent
or end a Security Threat
10. Flooding; Flood: The process of creating various e-contents (on blog
posts, social networking proles etc) to roll back the harmful information
in major search engines such as Google, Yahoo, MSN.
11. Harmful Publication: Published information on the internet
(including forums, blog postings, social media and any other websites)
that undermines Your reputation such that the information is:
a. Defamatory–an allegation of a fact that is false and injurious;
b. Insulting–an offensive expression of contempt or invectiveness;
orUnlawful disclosure of one’s private life.
12. Journalist: A person employed by traditional news media or
any professional medium or agency to regularly gather, process and
disseminate news and information to serve the public interest.
13. Money: Any circulating medium of exchange, including but not
limited to
a. coins & paper money,
b. gold, silver, or other metal in pieces of convenient form stamped by
public authority and issued as a medium of exchange and measure
of value
Any article or substance used as a medium of exchange, measure
of wealth, or means of payment, such as cheques on demand or
demand drafts.
14. Deemed Necessary: Means Psychiatric services needed to prevent,
diagnose, or treat a psychological illness, injury, condition, disease, or its
symptoms and that meet accepted standards of psychiatry.
15. Occupation: Yourfull-time or part-time gainful employment or any
other work for pay or prot.
16. Personal Information: Your private details (including any online
authentication information) relating to Your identity that will allow You
to be identied, such as:
• Full name
• Passport number
• Aadhaar ID number
• Mailing and/or home address
• Driving license number
• Telephone number(s) registered under Your name
• Online login ID and password
• Credit/Debit Card number
• Bank Account number
17. Period of Insurance The period of cover as stated in the Policy
Schedule.
18. Phishing: Fraudulent websites or emails, purporting to be from
reputable companies or institutions in order to induce individuals to
reveal personal information, such as usernames, passwords and credit
card numbers and internet banking details.

47
19. Policyholder : The name stated in the Policy Schedule.
20. Specied Event: An occurrence of one or more of these covered
events which arises out of the use of the internet and that is attributed
to the conduct of a Third Party and is not due to Your fault:
• Damage to E-reputation
• Identity Theft
• Unauthorized Online Transactions
• E-Extortion
• Cyber Bullying
• Phishing and E-mail Spoong
21. Security Threat: means any threat conveyed over internet to
demand money or goods or services from You by threatening to inict
harm to Your person, Your reputation, or Your property by making public,
Your Personal Information/ data stored in your Computer System
while still in your physical possession and custody or by denying You
the access to data or information in such Computer Systems.
22. Third Party: Any person or entity who deals at arm’s length with
You and which neither controls nor is controlled by You. Third Party
shall not be:
• Any person covered under this Policy; or
• Any person or entity who is in an employer-employee relationship
with You; or
• Any member of YourFamily (regardless residing with You or not) and/
or their authorized representatives.
23. We/Us/Our HDFC ERGO General Insurance Company Limited
24.You/Your/Yourself The name stated in the Policy Schedule.
III Waiting Periods and Exclusions
a. Waiting Periods
1. Waiting Periods applicable to Section 1: my:health Suraksha
2. my:health Hospital Cash Benet Add on
Claims under the Policy are covered subject to waiting Period as
specied below.
i) General waiting period:claim arising due to condition for which
appearance of signs/symptoms, consultation, investigation, treatment
or admission started within 30 days from Policy Commencement Date,
except for the claims arising due to an Accident.
ii) Waiting Period for listed illnesses and Procedures: 24 months for
all Illnesses and Surgical Procedures listed below however this waiting
period will not be applicable where the underlying cause is cancer(s).
a. Illnesses
Internal Congenital diseases Non infective Arthritis
Diseases of gall bladder
including cholecystitis
Urogenital system
e.g.Kidneystone,Urinary Bladder
Stone
Pancreatitis Ulcer and erosion of stomach
and duodenum
All forms of Cirrhosis Gastro Esophageal Reux
Disorder (GERD)
Perineal Abscesses Perianal Abscesses
Cataract Fissure/stula in anus,
Haemorrhoids including
Pilonidal sinus Gout and rheumatism
Benign tumors, cysts, nodules,
polyps including breast lumps
Osteoarthritis and osteoporosis
Polycystic ovarian diseases Fibroids ( bromyoma)
Sinusitis, Rhinitis Tonsillitis
Skin tumors Benign Hyperplasia of Prostate
b. Surgical Procedures
Adenoidectomy,
tonsillectomy
Tympanoplasty, Mastoidectomy
Dilatation and curettage
(D&C)
Nasal concha resection
Myomectomy for broids Surgery of Genito urinary system
Surgery on prostate Cholecystectomy
Hernia Hydrocele/Rectocele
Surgery for prolapsed
inter vertebral disc
Joint replacement surgeries
Surgery for varicose
veins and varicose ulcers
Surgery for Nasal septum deviation
Surgery for Perianal
Abscesses
Fissurectomy, Haemorrhoidectomy,
Fistulectomy, ENT surgeries
iii) Waiting Period for Pre-existing conditions:
A waiting period of 48 months shall apply for all Pre-existing Conditions
declared and/or accepted at the time of applying rst policy with us.
iv) Waiting Period for Parent and Child Care Cover- Basic/Parent
Child Cover - Booster (SectionI 1 C,2 and 3)
A waiting period of 48 months shall apply for all Claims under Parent and
Child Care Cover – Basic/Parent and Child Cover – Booster
Waiting period for parent & child care cover –Basic / Booster is applicable
only for my:health Suraksha
2. Waiting Periods applicable to Section 3: my:health Medisure
Super Top Up Insurance
i) General waiting period: claim arising due to condition for which
appearance of signs/symptoms, consultation, investigation, treatment
or admission started within 30 days from Policy Commencement Date,
except for the claims arising due to an Accident.
This Exclusion doesn’t apply for those having any health insurance
indemnity policy in India at least for 1 year prior to taking this Policy as
well as for subsequent renewals with Us without a break
ii) Waiting Period for listed illnesses and Procedures: 24 months for
all Illnesses and Surgical Procedures listed below however this waiting
period will not be applicable where the underlying cause is cancer(s).
• Cataract
• Hysterectomy other than for malignancy
• Uterine prolapse including any condition requiring Hysterectomy
• Polycystic Ovarian Diseases, Myomectomy for Fibroids
• Knee Replacement Surgery (other than caused by an accident)
• Osteoarthritis and Osteoporosis
• Arthritis, Arthroscopic Surgery, Rheumatism, Joint Replacement
Surgery (other than caused by accident), Prolapse of Intervertibral
discs(other than caused by accident)
• Varicose Veins and Varicose Ulcers, Hernia, Stones in the urinary,
uro-genital and biliary systems, Benign Prostate Hypertrophy, Hydrocele
• Congenital internal anomaly
• Fistula in anus, Piles, Fissures
• Fibroids, Dilatation & Curettage for treatment purposes, Pilonidal sinus,
Chronic Suppurative Otitis Media (CSOM)
• Deviated Nasal Septum, Sinusitis and related disorders
• Surgery on tonsils/Adenoids
• Gastric and duodenal ulcer, any type of Cysts/Nodules/Polyps, and
any type of Breast lumps, benign ear, Nose and Throat disorders and
surgeries Chronic Nephritis and Nephropathy (Kidney diseases).
• Hypertension, Diabetes and related complications
iii) Waiting Period for Pre-existing conditions:
A waiting period of 36 months shall apply for all Pre-existing Conditions
declared and/or accepted at the time of applying rst policy with us.

48
b. General Exclusions
1. General Exclusions applicable for Section I1: my:health
Suraksha,
We will not make any payment for any claim in respect of any Insured
Person directly or indirectly for, caused by, arising from or in any way
attributable to any of the following unless expressly stated to the
contrary in this Policy:
i). War or any act of war, invasion, act of foreign enemy, war like
operations (whether war be declared or not or caused during service
in the armed forces of any country), civil war, public defence, rebellion,
revolution, insurrection, military or usurped acts, nuclear weapons/
materials, chemical and biological weapons, radiation of any kind.
ii). Any Insured Person committing or attempting to commit a breach of
law with criminal intent, or intentional self-injury or attempted suicide or
suicide while mentally sound or unsound.
iii). Any Insured Person’s participation or involvement in naval, military
or air force operation, racing, diving, aviation, scuba diving, parachuting,
hang-gliding, rock or mountain climbing of a professional or semi-
professional nature.
iv). The abuse or the consequences of the abuse of tobacco, intoxicants
or hallucinogenic substances such as drugs and alcohol, including
smoking cessation programs and the treatment of nicotine addiction
or alcohol addiction programs, any other substance abuse treatment
or services, or supplies.
v). Treatment of Obesity and any weight control program.
vi). sleep-apnoea, Parkinson and Alzheimer’s disease, general debility
or exhaustion (“run-down condition”).
vii). Congenital external diseases, defects or anomalies,
viii). Stem cell harvesting, or growth hormone therapy. Venereal disease,
sexually transmitted disease or Illness;
ix). Pregnancy (including voluntary termination), miscarriage (except as a
result of an Accident or Illness), maternity or birth (including caesarean
section) except in the case of ectopic pregnancy.
x). treatment to treat infertility any fertility, sub-fertility or assisted
conception procedure,
xi). Sterility, treatment whether to affect infertility, surrogate or vicarious
pregnancy, birth control, contraceptive supplies or services including
complications arising due to supplying services.
xii). Dental Treatment and surgery of any kind, unless requiring
Hospitalization.
xiii). Treatment and supplies for analysis and adjustments of spinal
subluxation, diagnosis and treatment by manipulation of the skeletal
structure or for muscle stimulation by any means except treatment of
fractures ( excluding hairline fractures) and dislocations of the mandible
and extremities).
xiv). Circumcisions (unless necessitated by Illness or Injury an forming
part of treatment); treatment for correction of vision due to refractive
error, aesthetic or change-of-life treatments of any description such as
sex transformation operations.
xv). Plastic surgery or cosmetic surgery or treatments to change
appearance unless necessary as a part of Medically Necessary
Treatment certified by the attending Medical Practitioner for
reconstruction following an Accident, cancer or burns.
xvi). Experimental, investigational or Unproventreatments, devices
and pharmacological regimens.
xvii). Admission primarily for diagnostic purposes not related to Illness
for which Hospitalization has been done and Conditions for which In
patient Hospitalization is not warranted.
xviii). Any Convalescence, cure, rest cure, sanatorium treatment,
rehabilitation measures, private duty nursing, respite care, long-term
nursing care or custodial care.
xix). Preventive care, any physical, psychiatric or psychological
examinations or testing if doesn’t required Hospitalization; enteral
feedings (infusion formulas via a tube into the upper gastrointestinal tract)
and other nutritional and electrolyte supplements, unless certied to be
required by the attending Medical Practitioner as a direct consequence
of an otherwise covered claim.
xx). vaccination including inoculation and immunisations (Except post
bite treatment),
xxi). Non-Medical expenses such as charges for admission, discharge,
registration, Items of personal comfort and convenience including but
not limited to television ( wherever specically charged for) , charges for
access to telephone and telephone calls ( wherever specically charged
for) , foodstuffs( except patient‘s diet) , cosmetics, hygiene articles,
body care products and bath additive, barber or beauty service,guest
service as well as similar incidental services and supplies, and medical
supplies including elastic stockings, diabetic test strips, Charges related
to a Hospital stay not expressly mentioned as being covered, including
but not limited to, administration, documentation and ling. Full list of
Non-Medical expenses is available at www.hdfcergo.com.
xxii). vitamins and tonics unless vitamins and tonics are certied to be
required by the attending Medical Practitioner as a direct consequence
of an otherwise covered claim.
xxiii). Treatment rendered by a Medical Practitioner which isoutside his
discipline or the discipline for which he is licensed; treatments rendered
by a Medical Practitioner who is a member of an Insured Person’s family,
or stays with him,
xxiv). Treatment taken on Outpatient basis
xxv). The provision or tting of hearing aids, spectacles or contact lenses.
xxvi). any treatment and associated expenses for alopecia, baldness,
wigs, or toupees, and similar products.optometric therapy.
xxvii). Any treatment or part of a treatment that is not of a Reasonable
and Customary charge, not Medically Necessary; treatments or drugs
not supported by a prescription.
xxviii). Expenses for Articial limbs, crutches or any other external
appliance and/or device used for diagnosis or treatment (except when
used intra-operatively).
xxix). Any Claim arising due to Non-disclosure of Pre-existing Illness or
Material fact as sought to be declared on the Proposal form
2. General Exclusions applicable for Section I2: my:health Critical
Illness Plus
1. General Exclusions applicable to all Covers
i. A waiting period of 48 months shall apply for all Pre-existing Conditions
declared and/or accepted at the time of applying rst Policy with us.
ii. Treatment directly or indirectly arising from or consequent upon war
or any act of war, invasion, act of foreign enemy, war like operations
(whether war be declared or not or caused during service in the armed
forces of any country), civil war, public defense, rebellion, revolution,
insurrection, military or usurped acts, nuclear weapons/materials,
chemical and biological weapons, radiation of any kind.
iii. Any Illness, sickness or disease other than those opted and specied
as Critical Illnesses or Surgical Procedure underthis Policy;
iv. Any claim with respect to any Critical Illness diagnosed or which
manifested prior toPolicy Inception Date
v. Any condition directly or indirectly caused by or associated with
any sexuallytransmitted disease, including Genital Warts, Syphilus,
Gonorrhoea, Genital Herpes,Chalmydia, Pubic Lice and Trichomoniasis,
whether or not arising out of any Pre-existing diseases.
vi. Any Critical Illness arising out of use, abuse or consequence or
inuence of anysubstance, intoxicant, drug, alcohol or hallucinogen;
vii. Narcotics used by the Insured Person unless taken as prescribed
by a registeredMedical Practitioner,
viii. Any Claim directly or indirectly caused due to intentional self-injury,
suicideor attempted suicide; whether the person is medically sane or
insane
ix. Any Critical Illness directly or indirectly, caused by or arising from
or attributable to aforeign invasion, act of foreign enemies, hostilities,
warlike operations (whether warbe declared or not or while performing

49
duties in the armed forces of any countryduring war or at peace time),
civil war, public defense, rebellion, revolution,insurrection, military or
usurped power;
x. Any claim caused by ionizing radiation or contamination by radioactivity
fromany nuclear fuel (explosive or hazardous form) or from any
nuclear waste from thecombustion of nuclear fuel, nuclear, chemical
or biological attack.
xi. Working in underground mines, tunneling or involving electrical
installations with hightension supply, or as jockeys or circus personnel;
xii. Congenital External Anomalies or any complications or conditions
arising therefromincluding any developmental conditions of the Insured;
xiii. Insured Persons whilst engaging in a speed contest or racing of
any kind (other thanon foot), bungee jumping, parasailing, ballooning,
parachuting, skydiving, paragliding,hang gliding, mountain or rock
climbing necessitating the use of guides or ropes,potholing, abseiling,
deep sea diving using hard helmet and breathing apparatus,polo, snow
and ice sports in so far as they involve the training for or participation
incompetitions or professional sports, or involving a naval, military or
air forceoperation;
xiv. Participation by the Insured Person in any ying activity, except
as a bona de, farepayingpassenger of a recognized airline on regular
routes and on a scheduledtimetable.
2. General Exclusions applicable to Loss of Job:
i. Loss of job due to retirement whether voluntary or otherwise
ii. Resignation due to non-conrmation of employment after or during
such period under which the Insured was under probation
3. Applicable for Section I3: my:health Medisure Super Top Up
Insurance
i). Domiciliary hospitalization expenses
ii). Co-payment: All person(s) named in the Schedule to this Policy above
the age of 80 years (age last birthday) shall bear a co-pay of 10% for
each and every claim.
iii). Aggregate Deductible: We are not liable for Claims/Claim amount
falling within Aggregate Deductible limit as opted and mentioned on
the Schedule
iv). Any treatment arising from or traceable to pregnancy, childbirth
including caesarean section. However, this exclusion will not apply to
Ectopic Pregnancy proved by diagnostic means.
v). Circumcision unless necessary for treatment of a illness or injury not
excluded hereunder or due to an accident.
vi). Ambulance charges.
vii). Genetic disorder and stem cell implantation/surgery.
viii). Dental treatment or surgery of any kind unless necessitated due
to an accident and requiring minimum 24 hours Hospitalization or
treatment of irreversible bone disease involving the jaw which cannot
be treated in any other way, but not if it is related to gum disease or
tooth disease or damage.
ix). Birth control procedures, hormone replacement therapy and
voluntary termination of pregnancy during the rst 12 weeks from the
date of conception.
x). Routine medical, eye and ear examinations, cost of spectacles, laser
surgery for cosmetic purposes or corrective surgeries, contact lenses or
hearing aids, vaccinations except post-bite treatment, issue of medical
certicates and examinations as to suitability for employment or travel.
xi). All expenses arising out of any condition directly or indirectly caused
due to or associated with human T-call Lymph tropic virus type III (HTLV-
III) or Lymphadinopathy Associated Virus (LAV) or Acquired Immune
Deciency Syndrome (AIDS), AIDS related complex syndrome (ARCS)
and all diseases / illness / injury caused by and/or related to HIV and
sexually transmitted diseases.
xii). Vitamins and tonics unless forming part of treatment for illness or
injury and prescribed by a Medical Practitioner.
xiii). Instrument used in treatment of Sleep Apnoea Syndrome (C.P.A.P.)
and Continuous Peritoneal Ambulatory Dialysis (C.P.A.D.) and Oxygen
Concentrator for Bronchial Asthmatic condition, Infusion pump or any
other external devices used during or after treatment.
xiv). Treatment for developmental problems including learning
difculties eg. Dyslexia, behavioural problems including attention decit
hyperactivity disorder (ADHD).
xv). Treatment for general debility, ageing, convalescence, run down
condition or rest cure, Congenital external anomaly/ies or defects,
sterility, infertility including IVF, impotency, venereal disease, puberty
or menopause.
xvi). Committing or attempting to commit a criminal or illegal act, or
intentional self injury or attempted suicide while sane or insane.
xvii). Certication / Diagnosis / Treatment by a family member or from
persons not registered as Medical Practitioners under the respective
Medical Councils, or any diagnosis or treatment that is not scientically
recognized or experimental or unproven.
xviii). Ailment requiring treatment due to use, abuse or a consequence
of an abuse of any substance, intoxicant, drug, alcohol or hallucinogen
and treatment for de-addiction, or rehabilitation.
xix). Any illness or hospitalization arising or resulting from You or any of
Your family members committing any breach of law with criminal intent.
xx). Any treatment received in convalescent homes, convalescent
hospitals, health hydros, nature cure clinics or similar establishments.
xxi). Prostheses, corrective devices and medical appliances, which
are not required intra-operatively for the illness/ injury for which You
were hospitalised.
xxii). Any stay in Hospital/Nursing Home without undertaking any
treatment or where there is no active line of treatment by the Medical
Practitioner.
xxiii). Treatment of any mental illness or sickness including a psychiatric
condition, disorganization of personality or mind, or emotions or behavior,
Parkinson’s or Alzheimer’s disease even if caused or aggravated by
or related to an accident or illness or general debility or exhaustion
(“run-down condition”).
xxiv). Any cosmetic surgery unless forming part of treatment for cancer
or burns, surgery for sex change or treatment of obesity/morbid obesity
or treatment/surgery /complications/illness arising as a consequence
thereof.
xxv). Charges incurred primarily for diagnostic, X-ray or laboratory
examinations or other diagnostic studies not consistent with or incidental
to the diagnosis and treatment even if the same requires connement
at a Hospital/Nursing Home.
xxvi). Costs of donor screening and organ.
xxvii). Costs incurred on Alternative treatments.
xxviii). whilst You are engaging in speed contest or racing of any
kind (other than on foot), bungee jumping, parasailing, ballooning,
parachuting, skydiving, paragliding, hang gliding, mountain or rock
climbing necessitating the use of guides or ropes, potholing, abseiling,
deep sea diving using hard helmet and breathing apparatus, polo,
snow and ice sports or involving a naval military or air force operation.
xxix). Whilst You are ying or taking part in aerial activities (including
cabin crew) except as a fare-paying passenger in a regular Scheduled
airline or air Charter Company.
xxx). All expenses caused by ionizing radiation or contamination by
radioactivity from any nuclear fuel or from any nuclear waste from the
combustion of nuclear fuel.
xxxi). All expenses directly or indirectly, caused by or arising from or
attributable to foreign invasion, act of foreign enemies, hostilities, warlike
operations (whether war be declared or not or while performing duties
in the armed forces of any country), civil war, public defense, rebellion,
revolution, insurrection, military or usurped power. .
xxxii). All non-medical expenses as per annexure 2 attached.
xxxiii). Any condition after the point at which it is certied by the attending
Medical Practitioner to be of such a nature that further medical treatment
may serve to stabilize or maintain it but it is unlikely to result in a material
improvement within a reasonable time.

50
xxxiv). Service charges or any other charges levied by the Hospital/
Nursing Home, except registration/admission charges.
4. Applicable for Section I 4: my:health Hospital Cash Add on
i). War or any act of war, invasion, act of foreign enemy, war like
operations (whether war be declared or not or caused during service
in the armed forces of any country), civil war, public defence, rebellion,
revolution, insurrection, military or usurped acts, nuclear weapons/
materials, chemical and biological weapons, radiation of any kind.
ii). Any Insured Person committing or attempting to commit a breach of
law with criminal intent, or intentional self-injury or attempted suicide or
suicide while mentally sound or unsound.
iii). Any Insured Person’s participation or involvement in naval, military
or air force operation, racing, diving, aviation, scuba diving, parachuting,
hang-gliding, rock or mountain climbing of a professional or semi-
professional nature.
iv). The abuse or the consequences of the abuse of tobacco, intoxicants
or hallucinogenic substances such as drugs and alcohol, including
smoking cessation programs and the treatment of nicotine addiction
or alcohol addiction programs, any other substance abuse treatment
or services, or supplies.
v). Treatment of Obesity and any weight control program.
vi). sleep-apnoea, Parkinson and Alzheimer’s disease, general debility
or exhaustion (“run-down condition”).
vii). Congenital external diseases, defects or anomalies,
viii). Stem cell harvesting, or growth hormone therapy. Venereal disease,
sexually transmitted disease or Illness; Pregnancy (including voluntary
termination), miscarriage (except as a result of an Accident or Illness),
maternity or birth (including caesarean section) except in the case of
ectopic pregnancy.
ix). treatment to treat infertility any fertility, sub-fertility or assisted
conception procedure,
x). Sterility, treatment whether to affect infertility, surrogate or vicarious
pregnancy, birth control, contraceptive supplies or services including
complications arising due to supplying services.
xi). Dental Treatment and surgery of any kind, unless requiring
Hospitalization.
xii). Treatment and supplies for analysis and adjustments of spinal
subluxation, diagnosis and treatment by manipulation of the skeletal
structure or for muscle stimulation by any means except treatment of
fractures ( excluding hairline fractures) and dislocations of the mandible
and extremities).
xiii). Circumcisions (unless necessitated by Illness or Injuryan forming
part of treatment); treatment for correction of vision due to refractive
error, aesthetic or change-of-life treatments of any description such as
sex transformation operations.
xiv). Plastic surgery or cosmetic surgery or treatments to change
appearance unless necessary as a part of Medically Necessary
Treatment certified by the attending Medical Practitioner for
reconstruction following an Accident, cancer or burns.
xv). Experimental, investigational or Unproven treatments, devices
and pharmacological regimens.
xvi). Admission primarily for diagnostic purposes not related to Illness
for which Hospitalization has been done and Conditions for which In
patient Hospitalization is not warranted.
xvii). Any Convalescence, cure, rest cure, sanatorium treatment,
rehabilitation measures, private duty nursing, respite care, long-term
nursing care or custodial care.
xviii). Preventive care, any physical, psychiatric or psychological
examinations or testing if doesn’t required Hospitalization; enteral
feedings (infusion formulas via a tube into the upper gastrointestinal tract)
and other nutritional and electrolyte supplements, unless certied to be
required by the attending Medical Practitioner as a direct consequence
of an otherwise covered claim.
xix). vaccination including inoculation and immunisations (Except post
bite treatment),
xx). Charges related to a Hospital stay not expressly mentioned as being
covered, including but not limited to, administration, , documentation
and ling.
xxi). charges for admission, discharge, registration, Items of personal
comfort and convenience including but not limited to television (wherever
specically charged for) , charges for access to telephone and telephone
calls (wherever specically charged for), foodstuffs (except patient‘s
diet), cosmetics, hygiene articles, body care products and bath additive,
barber or beauty service, guest service as well as similar incidental
services and supplies, and medical supplies including elastic stockings,
diabetic test strips,
xxii). Vitamins and tonics unless vitamins and tonics are certied to be
required by the attending Medical Practitioner as a direct consequence
of an otherwise covered claim.
xxiii). Treatment rendered by a Medical Practitioner which is outside his
discipline or the discipline for which he is licensed; treatments rendered
by a Medical Practitioner who is a member of an Insured Person’s family,
or stays with him,
xxiv). Treatment taken on Outpatient basis
xxv). The provision or tting of hearing aids, spectacles or contact lenses.
xxvi). Any treatment and associated expenses for alopecia, baldness,
wigs, or toupees, and similar products. Optometric therapy.
xxvii). Any treatment or part of a treatment that is not of a Reasonable
and Customary charge, not Medically Necessary; treatments or drugs
not supported by a prescription.
xxviii). Expenses for Articial limbs, crutches or any other external
appliance and/or device used for diagnosis or treatment (except when
used intra-operatively).
xxix). Any Claim arising due to Non-disclosure of Pre-existing Illness or
Material fact as sought to be declared on the Proposal form
5. Applicable for Section I5: Personal Accident Insurance and
section I6: Travel Insurance
The Company shall not be liable to pay any benet in respect of any
Insured Person:
1) ForBodily Injury or Sickness occasioned by Civil War or Foreign
War.
2) For Bodily Injury or Sickness caused or provoked intentionally by
the Insured Person.
3) for Bodily Injury or Sickness due to wilful or deliberate exposure
to danger, (except in an attempt to save human life), intentional self-
inicted injury, suicide or attempt thereat, or arising out of non-adherence
to Medical Advice.
4) For Bodily Injury or Sickness sustained or suffered whilst the
Insured Person is or as a result of the Insured Person being under
the inuence of alcohol or drugs or narcotics unless professionally
administered by a Physician or unless professionally prescribed by and
taken in accordance with the directions of a Physician.
5) ForBodily Injury due to a gradually operating cause.
6) For Bodily Injury sustained whilst or as a result of participating in
any sport as a professional player.
7) for Bodily Injury sustained whilst or as a result of participating in
any competition involving the utilisation of a motorised land, water or
air vehicle.
8) for Bodily Injury sustained whilst or as a result of riding or driving a
motorcycle or motor scooter over one hundred fty (150) cc.
9) for Bodily Injury whilst the Insured Person is travelling by air other
than as a fare paying passenger on an aircraft registered to an airline
company for the transport of paying passengers on regular and published
scheduled routes.
10) for Bodily Injury sustained whilst or as a result of participating in
any criminal act.
11) for Bodily Injury or Sickness resulting from pregnancy within
twenty-six (26) weeks of the expected date of birth.
12) for Bodily Injury or Sickness caused by or arising from the

51
conditions commonly known as Acquired Immunodeciency Syndrome
(AIDS) or Human Immunodeciency Virus (HIV) and/or any related
illness or condition including derivatives or variations thereof howsoever
acquired or caused. The onus shall always be upon the Insured Person
to show that Bodily Injury or Sickness was not caused by or did not
arise through AIDS or HIV.
13) For Bodily Injury or Sickness caused by or arising from or due to
venereal or venereal related disease.
14) For Bodily Injury sustained whilst or as a result of active
participation in any violent labour disturbance, riot or civil commotion
or public disorder.
15) for Bodily Injury sustained whilst on service or on duty with
or undergoing training with any military or police force, or militia or
paramilitary organisation, notwithstanding that the Bodily Injury
occurred whilst the Insured Person was on leave or not in uniform.
16) for treatments for nervous or mental problems, whatever their
classication, psychiatric or psychotic conditions, depression of any
kind, or mental insanity.
17) any pathological fracture.
18) for cures of any kind and all stays in long term care institutions
(retirement homes, convalescence centres, centres of detoxication
etc.).
19) for investigations, operations or treatment of a purely cosmetic
nature; or for obesity; or undertaken to facilitate pregnancy or to cure
impotence or to improve potency.
20) for Bodily Injury sustained whilst or as a result of engaging in,
practicing for, or taking part in training peculiar to any kind of hazardous
sport such as parachuting, hangliding, parasailing, off-piste skiing or
bungee jumping.
21) Any Medical Expenses incurred, the need of which arises out of a
Pre-existing Condition
22) For Bodily Injury caused by or arising from or as a result of
Terrorism.
6. Applicable for Section 8: E@Secure Insurance
1) Your failure to take due care and precaution to safe guard Your
Personal Information, Bank Accounts and/or Credit/Debit Cards
information and internet communication.
2) Deliberate, fraudulent, Illegal or malicious acts or failure to act by
You or intentional or knowing violation of any duty, obligation, contract,
law or regulation by You.
3) Facts or circumstances existing prior to the commencement of this
cover, which You knew or ought to have reasonably known to be facts
or circumstances likely to give rise to a claim.
4) Your business activities (including but not limited to e-trading and
blogging where You receive remuneration or benets in any form),
Occupation or political afliations.
5) Loss that You have directly or indirectly and intentionally created or
endorsed by You.
6) Any unexplained loss or mysterious disappearance.
7) Any loss or damage caused by the order of any government authority.
8) Consequential loss or damage of any kind including loss suffered
by any Third Party.
9) Any claim in connection with the ownership, driving or use of a
motor vehicle.
10) Fees and costs incurred before acceptance of a claim.
11) Any claims made in connection: failure or interruption, caused by
whatsoever reason, of access to a Third Party infrastructure or service
provider, including telecommunications, internet service, satellite, cable,
electricity, gas, water or other utility service providers.
12) Losses arising from the theft, disappearance, loss of value or
inaccessibility of any cryptocurrency”
13) Any claim reported to Us more than six (6) months after the
occurrence of the Specied Event.
14) Any damage to or destruction of any tangible property, including
loss of use thereof.
15) Any liability under any contract, agreement, guarantee or warranty
assumed or accepted by except to the extent that such liability would
have attached to You in the absence of such contract, agreement,
guarantee or warranty.
16) Any actual or alleged plagiarism or infringement of any Trade Secrets,
patents, trademarks, trade names, copyrights, licenses or any other
form of intellectual property.
17) War, Terrorism, looting and Governmental Acts.
18) Any losses or liabilities connected with any inherent product defect/
wear and tear or any types of purchase or sale transactions or other
dealing in securities, commodities, derivatives, foreign or Federal Funds,
currencies, foreign exchange, and the like.
19) Any distribution of unsolicited correspondence or communications
(whether in physical or electronic form), wire tapping, audio or video
recordings or telephone marketing.
SECTION F: CLAIMS PROCEDURE
Procedure
Cashless Hospitalization Cashless claims for
Hospitalizations outside India
Reimbursement
Claims
Home Healthcare Claims
Emergencies Planned
Claim
Intimation
You shall intimate the Claims to us through any available mode of communication as specied in the Policy, Health Card or our Website
Claim
Intimation
Timelines
Within 24 hours
of the Emergency
Hospitalization
At least 72 hours
prior to the planned
Hospitalization
Within 24 hours of the Emergency
Hospitalization At least 72 hours prior
to the planned Hospitalization
Within 48 hours of
admission or before
discharge from the
Hospital, whichever
is earlier
Immediately on diagnosis
of Illness
Particulars to
be provided to
Us for Claim
notication
i. The health card issued by Us, ii. KYC documents, iii. The Policy Number, iv. Name of the Policyholder, v.
Name and address of Insured Person in respect of whom the request is being made, vi. Nature of the Illness/
Injury and the treatment/Surgery required, vii. Name and address of the attending Medical Practitioner, viii.
Hospital where treatment/Surgery is proposed to be taken or /Hospital where the Insured person is admitted,
ix. Proposed /Actual Date of admission
Following particulars in addition to
those listed under Hospitalization
Claim: i. Treatment details, ii.
Preferred date and time for initial
assessment
Particulars to
be provided
for pre-
authorization
i. Policy Number, ii. Name of the Insured person(s) named in the Policy schedule availing
treatment, iii. Nature of disease/Illness/Injury, iv. Name and address of the attending
Medical Practitioner/Hospital, v. Date of admission & probable date of discharge,
vi. Approximate Claim Expenses, vii. Any other relevant information as required
Not Applicable
Following particulars in addition to
those listed under Hospitalization
Claim: Probable date of start of
treatment

52
Procedure
Cashless Hospitalization Cashless claims for
Hospitalizations outside India
Reimbursement
Claims
Home Healthcare Claims
Emergencies Planned
Process for
obtaining Pre-
Authorization
i. If the particulars are not provided in full or
are insufcient for Us to consider the request,
We will request additional information or
documentation
ii. On receipt of duly lled pre authorization
form from the Network Provider along with
other sufcient details to assess the request,
We may;·
• Issue the authorization letter specifying the
sanctioned amount any specic limitation
on the claim and non-payable items, if
applicable or
• Reject the request for pre-authorization
specifying reasons for the rejection.
i. We shall send Release Of Informa
-
tion form to the Insured Person for
signature and consent.
ii. After receiving the signed Release
Of Information form, We will retrieve
hospitalization documents along
with invoices.
iii. If these details are not provided
in full or are insufficient for Us
to consider the request, We will
request additional information or
documentation
iv. On receipt of the complete
documents We may·
• issue the guarantee of payment
specifying the sanctioned amount,
any specic limitation on the claim
and non-payable items, if applicable or
• reject the request for pre-
authorization specifying reasons for
the rejection
On receipt of duly filled pre
authorization form with other sufcient
details to assess the request, We
will inform our Home Healthcare
service provider who will follow the
following process:
i. Meet the treating medical
practitioner and verify the requirement
along with the prescription/discharge
summary (if applicable) and the
condition of the patient
ii. Verify the past medical history of
the patient
iii. Complete physical examination
of the patient
iv. Check if the patient requires any
equipment, devices etc
v. Share the care plan and treatment
cost estimation with Us.
vi. On receipt of the complete
documents We may;
• issue the authorization letter
specifying the sanctioned amount,
any specic limitation on the claim
and non-payable items, if applicable or
• reject the request for pre-
authorization specifying reasons for
the rejection.
List of Claim
documents
Not Applicable As enlisted below Not Applicable
List of Documents for Reimbursement Claims:
i. Duly signed, stamped and completed Claim Form
ii. Photo ID & Age Proof
iii. Copy of claim intimation letter / reference of Claim Intimation Number
in the absence of main claim documents
iv. Copy of the Network Provider’s Registration Certicate / Hospital
registration no in case of Hospitalization
v. Original Discharge Card / Day Care Summary / Transfer Summary
vi. Original nal Hospital Bill with all original deposit and nal payment
receipt
vii. Original invoice with payment receipt and implant stickers for all
implants used during surgeries e.g. lens sticker and invoice in cataract
Surgery, stent invoice and sticker in Angioplasty Surgery.
viii. All previous consultation papers indicating history and treatment
details for current Illness
ix. All original diagnostic reports (including imaging and laboratory) along
with prescription by Medical Practitioner and invoice / bill with receipt
from diagnostic center
x. All original medicine / pharmacy bills along with prescription by
Medical Practitioner
xi. MLC / FIR Copy – in Accidental cases only
xii. Copy of Death Summary and copy of Death Certicate (in death
claims only)
xiii. Pre and Post-Operative Imaging reports
xiv. Copy of indoor case papers with nursing sheet detailing medical
history of the patient, treatment details, and patient’s progress
xv. Original invoice for Vaccination and payment receipt
xvi. KYC documents
Conditions for obtaining Cashless facility:
i. Cashless facility can be availed only at Our Network Provider. The
complete list of Network Providers and empanelled Service Providers
is available on Our website and can be obtained by contacting Us.
ii. We reserve the right to modify, add or restrict any Network Provider
for Cashless Facilities at Our sole discretion. The same shall be duly
updated on Our website. You shall check the updated list of Network
Providers before applying for Cashless Claim.
iii. Pre-authorization is valid for 15 days from date of issuance and if all
the details of the Hospitalization/treatment, including dates, Hospital
and locations match with the details as per Cashless authorized.
iv. We will make payment for the Cashless authorized amount directly
to the Network Provider.
v. If the claim is not notied to Us within the specied time limits, then We
shall be provided the reasons for the delay in writing. We will condone
such delay on merits where the delay has been proved to be for reasons
beyond the claimant’s control
2) Applicable for Section 2 my:health Critical Suraksha Plus
On the occurrence of any Critical Illness or undergoing Surgical
Procedure that may give rise to a Claim under this Policy, the Procedure
set out below shall be followed.
Claim
Intimation
You shall intimate the Claims to us through any
available mode of communication as specied in
the Policy, Health Card or our Website
Claim
Intimation
Timelines
Within 14 days of the diagnosis of CriticalIllness
or undergoing Surgical Procedure
Particulars to
be provided to
Us for Claim
notication
• Policy Number,
• Name of the Insured Person(s) named in the
Policy Schedule availing treatment,
• Nature of disease/illness/injury,

53
• Name and address of the attending Medical
Practitioner/Hospital
• Date of admission & probable date of discharge
• Date and time of event if applicable
• Date of admission if applicable
Claims
documents
for Critical
Illnesses Cover
and Multipay
Critical Illness
Cover
• Claim Form duly signed
• Copy of Discharge Summary / Discharge
Certicate;
• First consultation letter from treating Medical
Practitioner
• Medical certicate conrming diagnosis, and the
treatment from Medical Practitioner
• certicate from treating Medical Practitioner,
specifying the duration and etiology
• OT Notes in case of Surgery
• Medical certificate from treating Medical
Practitioner specifying the diagnosis and need
for the surgery
• MLC/FIR copy/ certicate regarding abuse of
Alcohol/intoxicating agent if applicable
• All pathological/Histopathological and radiological
Investigation Reports
• NEFT details & cancelled chequeProvide KYC (
Know your customer ) form along with photocopy
of any one of following KYC documents for all
claims amounting to Rs 1 lakh and above (Aadhaar
Card, Passport, Driving Licence Voter ID, etc)
We may require the Insured Person to undergo
medical examination by Medical Practitioner
authorized by Us to obtain an independent
medical opinion for the processing of the claim.
Any cost towards such medical examination will
be borne by Us.
Claims
documents
and process
for Second
Expert medical
Opinion
• Duly lled claim form along with the copy of all
medical reports including investigation reports
and discharge summary (if any)Consultation fees
payment Receipt / invoice
• For availing Second Expert medical Opinion
from Network Service Provider
• Select Our network Medical Practitioner from
whom you would prefer to take the second opinion.
(Please refer our Website or call at 24X 7 toll free
line to obtain the list of Our panel doctors).
• On receipt of the complete set of documents,
We will forward the same to the concerned doctor.
• The Second Opinion shall be forwarded to the
member within 15 working days of receipt of the
complete set of documents.
Claims
documents for
loss of Job
• Duly Completed Claim Form signed by Insured
Person;
• Form 16A
• Termination letter/Resignation Letter/ Resignation
Acceptance letter
• NEFT details & cancelled cheque
Condonation
of delay
If the claim is not notied/ or submitted to Us
within the specied time limits, then We shall be
provided the reasons for the delay in writing. We
will condone such delay on merits where the delay
has been proved to be for reasons beyond the
claimant’s control
3) Applicable for Section 3 my:health Medisure Super Top Up
Insurance
Notication of Claim
Give immediate notice to the Company named in this Policy/Health Card,
by calling the Help Line number as specied in the Policy/Health Card, or
in writing to the address shown in the Schedule with particulars as below:
• Policy Number,
• Name of the person(s) named in the Schedule to this Policy availing
treatment,
• Nature of disease/illness/injury,
• Name and address of the attending Medical Practitioner/Hospital
• Date of admission & probable date of discharge
• Approximate Claim Expenses
• Any other relevant information
Intimation of claim must be done at least 72 hours prior to Hospitalization
in case of planned Hospitalization and within 24 hours of Hospitalization
in case of an emergency Hospitalization.
In case where initial covered Medical expenses were not expected to
exceed the deductible but subsequently found to be exceeding the opted
deductible, notication must be done immediately along with the copy
of intimation made to other Insurer.
2. Cashless Facility for Hospitalization
i) We may provide Cashless facility for Hospitalization expenses either
directly or through the Third Party Administrator (TPA) if treatment is
undergone at a Network Hospital by issue of pre-authorization by
Us or the TPA.
ii) For the purpose of considering pre-authorization and Cashless facility,
You shall submit to the TPA complete information of the illness or injury
requiring treatment along with necessary certication from the Medical
Practitioner and/or Hospital.
iii) If claim for treatment appears admissible, We or TPA shall issue pre-
authorization to the Hospital concerned for Cashless facility whereby
Hospitalization expenses shall be paid directly by Us directly or through
the TPA as conrmed in the pre-authorization.
iv) Cashless facility for Hospitalization will not be available for treatment
in Non-Network Hospital and may be declined even for treatment at
Network Hospital where the information available does not conclusively
establish that a claim in respect of the treatment would be admissible.
In such a case, You shall bear the expenses and claim reimbursement,
immediately after discharge from Hospital/Nursing Home in accordance
with the stipulations herein.
v) Cashless facility for Hospitalization benet shall be limited exclusively
to Hospitalization Expenses incurred for treatment at a Network Hospital
for illness or injury which are covered under the Policy and shall be
extended only for Coverage mentioned under Scope of cover(A)
“Inpatient Hospitalization expenses” and Scope of cover (B) “Day care
Procedures”
3. Claims Processing for Reimbursement
i) After intimation as aforesaid, further submit following documents to
the TPA at Your own expense within 30 days of discharge from the
Hospital, the following:-
• Claim Form Duly lled with requisite information and signed by Insured
& Hospital
• Copy of the claim intimation
• Original Hospital Main Bill
• Original Hospital Bill break up (Where issued by the Hospital)
• Original Hospital Bill Payment Receipt
• Hospital Discharge Card/Summary
• Original Pharmacy Bill with supporting prescriptions
• Medical Investigation report: ECG/X-Ray/USG/CT/MRI/Histopathology/
pathological and all other medical investigation report in support of
diagnosis as advised by the treating doctor.

54
• All Doctor’s consultation note: conrming provisional & nal diagnosis/
advise for admission/medical complication/proposed line of treatment/
past medical history
• Original bills and receipts for claiming Ambulance charges (if any)
• By signing the claim form you are authorizing us to collect the following
documents from the Hospital. If you have obtained these documents,
then please submit the same
• Operation Theatre Notes in surgical cases
• Bar code sticker & Invoice for implants and prosthesis (if used)
• In case of Accidental Injuries, Medico Legal Certificate and/ or
First information Report, where applicable and self statement giving
description of the incident
• Indoor case papers
Pre and Post hospitalization Claims documents
• Duly lled claim form(s) (If claimed Separately)
• Pharmacy Bills with supporting prescriptions
• Medical investigation test reports and payment receipts with doctor’s
advice note for such investigations.
• All Doctor’s consultation note with original bills and receipts for claiming
Doctors fees,
ii) Documents pertaining to the Post-Hospitalization claim shall be
submitted to the TPA within 15 days from the date of expiry of Post-
Hospitalisation coverage period.
iii) At any time You may be required to authorize and permit the TPA and/
or Us or anyone deputed by Us or TPA to obtain any further information
or records from the Hospital, Medical Practitioner, Lab or other agency,
in connection with the treatment relating to the claim.
iv) You should under go medical examination by Medical Practitioner
designated by Us or the TPA and the cost of such medical examination
will be borne by Us.
We may carry out verication/investigation on a case to case basis
to ascertain the facts/collect additional information/documents of the
case to determine the assessment of loss. Verication carried out, if
any, will be done by individuals or entities authorized by Us to carry
out such verication/investigation(s) and the costs for such verication/
investigation shall be borne by Us.
For determining the amount of admissible claim, applicable taxes
prevailing at the time of the claim will be considered as part of claim
amount and Our aggregate liability, including any payment towards such
Taxes shall in no case exceed the Sum Insured.
4. TPA to Pay or Reject
The TPA where appointed, shall process and communicate rejection, if
a claim is found to be not admissible under this Policy as authorized by
Us. However all decisions shall be Our responsibility.
5. Representation against Rejection
Where rejection is communicated, You, may if so desired, represent to
Us within 15 days for reconsideration of the decision.
6. Condition Precedent
Completed claim forms and documents must be furnished to Us within
the stipulated timelines. Failure to furnish such evidence within the
time required shall not invalidate nor reduce any claim, if You can
satisfy Us that it was not reasonably possible for You to submit/give
proof within such time.
The due intimation, submission of documents and compliance with
requirements by You as mentioned above shall be essential, failing
which We/TPA shall not be bound to entertain a claim.
7. Claims Service Assurance
1) If You notify a cashless facility request by sending the pre-
authorization form duly lled in and signed through email, fax to Us or
Our representative, then within 6 hours of the actual receipt of such a
request, We will respond with:
a) Approval, or
b) Rejection.
If such request has been notied during ofce hours (9 am to 9 pm)
on Monday to Saturday and We fail to either approve or reject or seek
further information after the expiry of 6 hours from the actual receipt
of the request then, We shall be liable to pay You for the delay in the
following manner:
i) For delay beyond 6 hours: Rs.1,000/-
ii) The maximum amount that We shall be liable to pay to You for any
delay, in respect of a single Hospitalization, shall at no time exceed
Rs.1,000/-.
If such request has been notied after ofce hours on a working day or
at any time during a holiday and We fail to either approve or reject after
the expiry of 8 hours from the actual receipt of the request, then We shall
be liable to pay You for the delay in the following manner:
iii) For delay beyond 8 hours: Rs.1,000/-
iv) The maximum amount that We shall be liable to pay You for any delay,
in respect of a single Hospitalization, shall at no time exceed Rs.1,000/-.
2) In case of reimbursement claims, We shall communicate our decision
on payment within 6 working days after You submit the complete details,
information and document requirements in respect of the claim. If
You have provided such information and documents as required by
Us and We fail to communicate our decision, then We shall pay You
Rs. 1,000/- for a delay beyond 6 days. The maximum amount that
We shall be liable to pay You for any delay, in respect of a single
Hospitalization, shall at no time exceed Rs.1,000/-.
3) We will not be liable to make any payments under Clauses 1 and
2 above in case of any natural event or manmade disturbance which
impedes Our ability to make a decision or to communicate such
decision to You.
4) Any amounts paid under this Clause will not affect the Sum Insured
as specied in the Schedule. Our liability to make payments under
this Clause shall at all times be restricted to the amounts specied
in Clause 1 and 2 above including the maximum amount specied
therein and You shall not be entitled to any sum whatsoever, in excess
of those amounts. Any payment made under this Clause by Us will not
amount to any admission of liability for a claim notied by You. Service
Assurance is applicable only to the rst response on a single claim and
to no subsequent correspondence.
The above compensation shall be paid to You notwithstanding Our
obligation to pay interest at a rate which is 2% above the bank rate
prevalent at the beginning of the nancial year in which the claim is
reviewed by the Company in cases of delay in settlement of claims,
as per Reg. 9(6) of IRDA (Protection of Policy Holder’s Interests)
Regulations 2002
8. Claim Settlement
Wherever a claim has not been settled within the stipulations of the
Claims Service Assurance Clause above, We will settle the Claim within
a period of 30 days from receipt of nal completed set of documents/
investigation reports (if applicable)
In the event that We decide to reject a claim made under this Policy, We
shall intimate the same to you within a period of 30 days of receipt of the
nal completed set of documents/investigation reports (if applicable),
in accordance with the provisions of IRDA (Protection of Policyholder’s
Interests) Regulations, 2002.
4) Applicable for Section 4. my:health Hospital Cash Benet Add on
On the occurrence of any Injury Illness or that may give rise to a
Claim under this Policy, the Claims Procedure set out below shall be
followed.
Claim Intimation You shall intimate the Claims to us through any
available mode of communication as specied in
the Policy, Health Card or our Website
Claim Intimation
Timelines
Within 24 hours of the Emergency
HospitalizationAt least 72 hours prior to the
planned Hospitalization

55
Particulars to
be provided to
Us for Claim
notication
a. Policy Number,
b. Name of the Insured person(s) named in the
Policy schedule availing treatment,
c. Nature of disease/illness/injury,
d. Name and address of the attending Medical
Practitioner/Hospital
e. Date of admission & probable date of discharge
Claims
documents
Claim Form duly signed by the insured;Copy of
Discharge Summary / Discharge Certicate;First
consultation letter from treating Medical
Practitionercertificate from treating Medical
Practitioner’s specifying the diagnosis,
duration and etiologyMLC/FIR copy/ certicate
regarding abuse of Alcohol/intoxicating agent
if applicableNEFT details & cancelled cheque
Condonation of
delay
If the claim is not notied/ or submitted to Us
within the specied time limits, then We shall
be provided the reasons for the delay in writing.
We will condone such delay on merits where the
delay has been proved to be for reasons beyond
the claimant’s control
5) Claims process applicable for Section 5: Personal Accident
Insurance
Claims documents for under Section 5: Personal Accident
Insurance
1) Written notice of any occurrence which may give rise to a claim under
this Policy must be given to the Company as soon as practicable and in
any case within thirty (30) Days after such occurrence. Written Notice
of Claim must be given to the Company immediately in the case of
death, or within thirty (30) Days after the Date of Loss in all other cases.
2) All certicates, information and evidence required by the Company
shall be furnished at no expense to the Company and shall be in such
form and of such nature as the Company may prescribe. When required
by the Company, at its own expense, the Insured Person shall submit
to medical examination in respect of any alleged claim that may give
rise to a benet being paid.
3) Complete, written proof of loss must be given to the Company
within sixty (60) Days after the Date of Loss, or as soon as reasonably
possible. Such proof of loss must contain:
i) the Policy Number, and
ii) the preliminary medical report describing the nature and extent of all
injuries or Sicknesses, and providing a precise diagnosis, and
iii) all invoices, bills, prescriptions, Hospital certicates which will permit
the Company to accurately determine the total amount of Medical
Expenses (if applicable) incurred by the Insured Person, and
iv) in the case where another party was involved (e.g. a car collision),
the names, contact details and if possible insurance details of the
other party, and
v) in the case of death, an ofcial death certicate, succession certicate
pursuant to the Indian Succession Act 1925, as amended, and any other
legal documents establishing the identity of any and all beneciaries, and
vi) proof of age, where applicable, and
vii) such other information as the Company may require to handle
the claim.
a) If an Accident:
i) detailed circumstances of the Accident and the names of any
witnesses, and
ii) any police reports concerning the Accident, and
iii) the date a Physician was seen due to the Bodily Injury, and
iv) the Physician’s contact details, or
b) If a Sickness:
i) the date symptoms of the Sickness began, and
ii) the date a Physician was seen due to the Sickness, and
iii) the Physician’s contact details.
The Company shall base its assessment of the claim on the complete,
written proof of loss.
4) The Company at its own expense shall have the right and opportunity
to examine the
Insured Person whose Bodily Injury or Sickness is the basis of a
claim and as often as it may be reasonably required during the pendency
of the claim and to make an autopsy in case of death, where it is not
forbidden by law.
5) In respect of any disablement claim, no benet shall be payable
before any disablement is recognized as denitive and permanent by a
Physician appointed by the Company.
6) Medical advice of a Physician shall be sought and followed promptly
on the occurrence of any Bodily Injury or Sickness and the Company
shall not be liable for any part of any claim which in the opinion of a
Physician appointed by the Company arises from the unreasonable
or willful neglect or failure of an Insured Person to seek and remain
under the care of a Physician.
7) No claim may be brought under this Policy, nor may any legal action
be brought against the Company to recover under such claim:
1) in cases of Accidental death, more than three (3) years after the date
of death or the date the claim is denied in whole or in part, whichever
is later; or
2) in all other cases, more than three (3) years after the Date of Loss or
date the claim is denied in whole or in part, whichever is later.
No such legal action may be brought against the Company unless there
has been full compliance with all the terms and conditions of this Policy.
In the event of any failure to timely submit any claim or commence legal
action with respect to any claim, all benets under this Policy in respect
of such claim shall be forfeited.
8) If any difference shall arise as to the amount to be paid under this
Policy (liability being otherwise admitted) such difference shall be
referred to arbitration in accordance with the Indian Arbitration and
Conciliation Act 1996, as amended, and the making of an award shall
be a condition precedent to any liability for the Company to make any
payment under this Policy.
9) The Company will effect payment of covered claims subject to: i) the
Company having received complete, written proof of loss and such other
information as the Company may require to handle the claim; and ii) the
premium for the Policy having been paid. In such cases, the Company
shall effect payment within 7 days.
10) No benet shall be payable in respect of an Insured Person
under more than one of the following insurances: Accidental death or
Accidental disablement.
11) No sum payable under this Policy shall carry interest.
12) Where amounts recoverable from the Company are delayed
pending nalisation of any claim, payments on account may be made
to the Insured Person at the Company’s discretion, on receipt by the
Company of certication by a Physician appointed by the Company.
13) An Insured Person has the right to designate a beneciary. All
beneciary designations shall be in writing, led with the Company. by
the Policyholder, and provided to the Company at the time of claim
and such other time as the Company may require.
The Insured Person, and no one else, unless there is an irrevocable
assignment, has the right to change the beneciary. The Insured Person
does not need the consent of anyone to do so. Changes must be in
writing, led with the Company by the Policyholder and provided to
the Company at the time of claim and such other time as the Company
may require. The Company does not assume any responsibility for the
validity of these changes.
The Insured Person’s rights under this Policy may be assigned by
giving the Company prior written notice. The assignment may be made
irrevocable. However, the Company will only recognise an assignment
if the Insured Person has given the Company prior written notice
and has the Company’s written acknowledgement of the assignment.

56
The Company does not assume any responsibility for the validity of
an assignment.
Benefit shall be payable only to the Insured Person, his or her
Beneciary, or the Insured Person’s legal personal representatives,
or assignee if applicable, whose receipt shall effectively discharge the
Company
14) In the event of a claim under this Policy, the Policyholder, the
Insured Person and the Beneciary, if applicable, must fully cooperate
with the Company in its handling of the claim including, but not limited
to, the timely submission of all medical and other reports, and full
cooperation with all physical examinations and autopsies that the
Company may require.
15) The Company shall not be bound or be affected by any notice of
any trust, charge, lien, or other dealing with or in relation to this Policy.
Claims Procedure Applicable for Section 6: Travel Insurance
1) Written notice of any occurrence which may give rise to a claim under
this Policy must be given to the Company as soon as practicable and in
any case within thirty (30) Days after such occurrence. Written Notice of
Claim must be given to the Company immediately in the case of death,
or within thirty (30) Days after the Date of Loss in all other cases.
2) All certicates, information and evidence required by the Company
shall be furnished at no expense to the Company and shall be in such
form and of such nature as the Company may prescribe. When required
by the Company, at its own expense, the Insured Person shall submit
to medical examination in respect of any alleged claim that may give
rise to a benet being paid.
3) Complete, written proof of loss must be given to the Company
within sixty (60) Days after the Date of Loss, or as soon as reasonably
possible. Such proof of loss must contain:
I. the Policy Number, and
II. the preliminary medical report describing the nature and extent of all
injuries or Sicknesses, and providing a precise diagnosis, and
III. all invoices, bills, prescriptions, Hospital certicates which will permit
the Company to accurately determine the total amount of Medical
Expenses (if applicable) incurred by the Insured Person, and
IV. in the case where another party was involved (e.g. a car collision),
the names, contact details and if possible insurance details of the
other party, and
V. in the case of death, an ofcial death certicate, succession certicate
pursuant to the Indian Succession Act 1925, as amended, and any other
legal documents establishing the identity of any and all beneciaries, and
VI. proof of age, where applicable, and
VII. such other information as the Company may require to handle
the claim.
a) If an Accident:
I. detailed circumstances of the Accident and the names of any
witnesses, and
II. any police reports concerning the Accident, and
III. the date a Physician was seen due to the Bodily Injury, and
IV. the Physician’s contact details, or
b) If a Sickness:
I. the date symptoms of the Sickness began, and
II. the date a Physician was seen due to the Sickness, and
III. the Physician’s contact details.
The Company shall base its assessment of the claim on the complete,
written proof of loss.
4) The Company at its own expense shall have the right and opportunity
to examine the Insured Person whose Bodily Injury or Sickness is the
basis of a claim and as often as it may be reasonably required during
the pendancy of the claim and to make an autopsy in case of death,
where it is not forbidden by law.
5) In respect of any disablement claim, no benet shall be payable
before any disablement is recognised as denitive and permanent by a
Physician appointed by the Company.
6) Medical advice of a Physician shall be sought and followed promptly
on the occurrence of any Bodily Injury or Sickness and the Company
shall not be liable for any part of any claim which in the opinion of a
Physician appointed by the Company arises from the unreasonable
or willful neglect or failure of an Insured Person to seek and remain
under the care of a Physician.
7) No claim may be brought under this Policy, nor may any legal action
be brought against the Company to recover under such claim:
a) in cases of Accidental death, more than three (3) years after the date
of death or the date the claim is denied in whole or in part, whichever
is later; or
b) in all other cases, more than three (3) years after the Date of Loss or
date the claim is denied in whole or in part, whichever is later.
No such legal action may be brought against the Company unless there
has been full compliance with all the terms and conditions of this Policy.
In the event of any failure to timely submit any claim or commence legal
action with respect to any claim, all benets under this Policy in respect
of such claim shall be forfeited.
8) If any difference shall arise as to the amount to be paid under this
Policy (liability being otherwise admitted) such difference shall be
referred to arbitration in accordance with the Indian Arbitration and
Conciliation Act 1996, as amended, and the making of an award shall
be a condition precedent to any liability for the Company to make any
payment under this Policy.
9) The Company will effect payment of covered claims subject to: i) the
Company having received complete, written proof of loss and such other
information as the Company may require to handle the claim; and ii) the
premium for the Policy having been paid. In such cases, the Company
shall effect payment within 7days.
10) No benet shall be payable in respect of an Insured Person
under more than one of the following insurances: Accidental death or
Accidental disablement.
11) No sum payable under this Policy shall carry interest.
12) Where amounts recoverable from the Company are delayed
pending nalisation of any claim, payments on account may be made
to the Insured Person at the Company’s discretion, on receipt by the
Company of certication by a Physician appointed by the Company.
13) An Insured Person has the right to designate a beneciary. All
beneciary designations shall be in writing, led with the Policyholder,
and provided to the Company at the time of claim and such other time
as the Company may require.
The Insured Person, and no one else, unless there is an irrevocable
assignment, has the right to change the beneciary. The Insured
Person does not need the consent of anyone to do so. Changes must
be in writing, led with the Policyholder and provided to the Company
at the time of claim and such other time as the Company may require.
The Company does not assume any responsibility for the validity of
these changes.
The Insured Person’s rights under this Policy may be assigned by
giving the Company prior written notice. The assignment may be made
irrevocable. However, the Company will only recognise an assignment
if the Insured Person has given the Company prior written notice
and has the Company’s written acknowledgement of the assignment.
The Company does not assume any responsibility for the validity of
an assignment.
Benefit shall be payable only to the Insured Person, his or her
Beneciary, or the Insured Person’s legal personal representatives
or assignee if applicable, whose receipt shall effectively discharge the
Company.
14) In the event of a claim under this Policy, the Policyholder,
the Insured Person and the Beneciary, if applicable, must fully
cooperate with the Company in its handling of the claim including, but
not limited to, the timely submission of all medical and other reports,
and full Cupertino with all physical examinations and autopsies that the
Company may require.
15) The Company shall not be bound or be affected by any notice of

57
any trust, charge, lien, or other dealing with or in relation to this Policy.
Claims Procedure Applicable for Section 7: Home Insurance
revision
The Insured shall upon the occurrence of any event giving rise or likely
to give rise to a claim under this policy:
a. In the event of theft lodge forthwith a complaint with the Police and
take all practicable steps to apprehend the guilty person or persons and
to recover the property lost.
b. Give immediate notice there of to the Company and shall within
fourteen (14) days thereafter furnish to the Company at his own expense
detailed particulars of the amount of the loss or damage together
with such explanations and evidence to substantiate the claim as the
Company may reasonablyrequire.
c. Tender to the Company all reasonable information, assistance and
proof in connectionwithanyclaim.
Claims Procedure applicable for Section 8: E@Secure Insurance
I. In the event of a claim, and to report a claim upon discovery of an
occurrence of a Specied Event,You must give written notice to Us
along with duly lled claim form at the address mentioned in the Policy
Schedule with full details thereof, within 7days after such claim is rst
made. Such notice shall be effective on the date of receipt by Usat
such address.
a. It is the duty of the Insured to defend Claims and arrange for legal
representation, hearing, investigation and experts. We shall have
the right to effectively associate with You in respect of conductand
management of the Claim to which Policy may apply, and may, at Our
option, elect to assume conduct of Your defense and /or investigation
of any such claim.
b. The payment of claims is dependent on You providing all necessary
information. Upon learning of any circumstances likely to give rise to a
claim, You must provide all relevant documents including receipts, bills
and other records in support of Your claim.
c. You must make no admission or settlement and must not enter into
any correspondence or exchange of communications about the claim
without Our prior written authorization.
d. All claims are paid in Indian Rupee. If You suffer a loss which is in
a foreign currency, the amount will be converted into Indian Rupee at
cash rate of exchange published in the currency conversion website,
of Reserve Bank of India or, if it has ceased to be current, a currency
conversion website selected by Us, on the date of the loss.
II. On receipt of all required information/documents that can be
considered relevant and necessary for the claim, We shall, with in a
period of 30 days offer a settlement of the claim to You. If, for any
reasons to be recorded in writing and communicated to You, We decide
to reject a claim under the policy, it shall be within a period of 30 days
from the receipt of all required information/documents that are relevant
and necessary for the claim.
III. In the event the claim is not settled within 30 days as stipulated above,
We shall be liable to pay interest at a rate, which is 2% above the Bank
Rate from the date of receipt of last relevant and necessary document
from You by Us till the date of actual payment.
All benets are only payable when approved byUs.
* Note – We may condone delay in claim intimation/ document
submission on merit, where it is proved that delay in reporting of claim
or submission of claim documents, is due to reasons beyond the control
of the Insured.
Notwithstanding the above, delay in claim intimation or submission of
claim documents due to reasons beyond the control of the Insured
shall not be condoned where such claims would have otherwise been
rejected even if reported in time.
In the event of a claim, and to report a claim upon discovery of an
occurrence of a Specied Event, You must give Us such information
and co-operation as it may reasonably require including but not limited to:
(a) Submission of fully completed and signed claim form
(b) Copy of FIR lodged with Police Authorities / Cyber cell
(c) Copies of legal notice received from any affected person/entity
(d) Copies of summon received from any court in respect of a suit led
by an affected party/entity
(e) Copies of invoices for expenses You incurred for the services of
IT specialist
(f) Copies of invoices for expenses You incurred in amending / rectifying
Your Personal Information
(g) Evidence of Your consultation with Psychologist / Psychiatrist
(h) Evidence of unpaid wages
(i) Copy of Your last drawn monthly salary.
(j) Evidence of expenses incurred by You in rectifying records regarding
your identity
(k) Copies of correspondence with bank evidencing that bank is not
reimbursing You
V. General Conditions
A) General Conditions Applicable to Section I.
1: my:healthSuraksha,
1. Free Look period
A period of 15 days from the date of receipt of the Policy document is
available to review the terms and conditions of this Policy. You have the
option of cancelling the Policy stating the reasons for cancellation, if You
have any objections to any of the terms and conditions.
• We shall refund the premium paid after adjusting the amounts spent
on stamp duty charges, Medical examination (wherever applicable) and
proportionate premium (If Policy has already commenced).
• Cancellation will be allowed only if there are no admissible claims
under the Policy as on date of Cancellation.
• Free Look period is not applicable on Renewal
2. Other Insurance / Contribution
If Insured Person has two or more policies to indemnify treatment cost,
which also covers any claim (in part or in whole) being made under this
Policy, then the Policy holderhas the right to require a settlement of
claim under terms and conditions of any of his/herPolicies.
3. Non Disclosure or Misrepresentation
If at the time of issuance of Policy or during continuation of the Policy,
the information provided to Us in the proposal form or otherwise, by You
or the Insured Person or anyone acting on behalf of You or an Insured
Person, is found to be incorrect, incomplete, suppressed or not disclosed,
willfully or otherwise, the Policy shall be:
• cancelled ab initio from the inception date or the Renewal date (as
the case may be), or the Policy may be modied by Us at Our sole
discretion, upon 30 day notice by sending an endorsement to Your
address shown in the Schedule and
• the claim under such Policy if any, shall be prejudiced.
4. Fraudulent claim
If any Claim made or utilization of Covers under the Policy is found
to be fraudulent, or is supported by any fraudulent means, devices or
software by Insured Person or anyone acting on their behalf to obtain
any benet under this Policy;
• The policy shall be cancelled ab-initio from the inception date or the
Renewal date (as the case may be),
• All benets payable, if any, under such Policy shall be forfeited with
respect to such claim
5. Geography
This Policy only covers Medical Treatment taken within India, except
under the policies with Global Health Cover as may be specied in the
on the Schedule of Coverage in the policy Schedule.
6. Loadings
i. We may apply Medical Underwriting loading on the premium, based on
the declarations made in the proposal form and the health status, habits
and lifestyle, past medical records, and the results of the Pre-Policy
medical examination of the persons proposed for insurance.

58
ii. The maximum Medical Underwriting loading shall not exceed 35%
for each diagnosis / medical condition and a total of 100% for each
Insured Person
iii. Medical Underwriting loadings will be applied from Commencement
date of the Policy including subsequent Renewal(s) with Us or on
increased Sum Insured. We will not apply any additional loading
on Your policy premium at Renewal based on claim experience
in Your Policy. However increase or decrease of discount in
Medical Underwriting loading is subject to terms mentioned under
Section 3B – Health Incentives
iv. We will inform You about the applicable Medical underwriting loading
with time bound exclusion (if any) through a counter offer letter and will
issue the Policy only on Your acceptance within 15 days of the receipt
of such counter offer letter. In case, you neither accept the counter offer
nor revert to Us within 15 days, We shall cancel Your application and
refund the premium paid within next 7 days.
7. Renewal:
i. This policy is ordinarily renewable for lifetime except on grounds of
fraud, non-disclosure of material facts or misrepresentation as sought
to be declared in the proposal form or non-cooperation by the insured
ii. We are not under any obligation to send renewal notice or reminders.
iii. For dependent children, Policy is renewable up to 25 years. After the
completion of maximum Renewal age of dependent children, a separate
proposal form should be submitted to us at the time of Renewal. Credit
of continuity/waiting periods, earnedCumulative Bonus and Healthy
Weeks discount accrued for all the previous Policy Years would be
extended in the Renewal under new Policy.
iv. You can apply for enhancement of Sum Insured or change in plan at
the time of Renewal by submitting a fresh proposal form to Us. All waiting
periods as dened in the Policy shall apply afresh for the enhanced Sum
Insured from the effective date of enhancement.
v. Premium payable on Renewal and on subsequent continuation of
cover are subject to the provisions under condition 10
8. Grace Period
i. A Grace Period of 30 days is available for Renewal of the Policy. Any
Illness, disease or condition contracted during Grace Period will not be
covered and will be treated as Pre-existing diseases.
ii. Policies for which Premium is received after the Grace Period shall
be considered as a fresh policy.
9. Portability
Health Insurance portability can be availed under this Policy if;
i. The proposed Insured Person was continuously covered under
anysimilar health insurance policy with any other Insurance company
ii. The proposed Insured Person was insured continuously and without
a break under another retail or Group health insurance policy with Us.
Procedure to avail Portability:
a. The Portabilityof Policy can be availed of by submitting the completed
Proposal form, portability annexure along with previous policy documents
and Renewal notice of expiring policy, at least 45 days in advance,
but not earlier than 60 days, from the expiry of the existing health
insurance policy.
b. Policy can be ported on at the time of Renewal of the existing health
insurance policy.
c. Waiting period credits shall be extended to Pre-Existing Diseases
and time bound exclusions/waiting periods.
d. If the proposed Sum Insured is higher than the Sum insured under
the expiring policy, all waiting periods under Section E shall be applicable
on the increased Sum Insured.
e. Portability shall be applicable to the Sum Insured under previous Policy
and to the Cumulative Bonus acquired under that Policy
f. We will process Portability application within 15 days of receiving the
completeproposal form and Portability Form.
10. Endorsements
The following endorsements are permissible during the Policy Period:
1.1 Non-Financial Endorsements – which do not affect the premium
a. Minor rectication/correction in name of the Proposer / Insured Person
(and not the complete name change)
b. Rectication in gender of the Insured Person (if this does not impact
the premium)*
c. Rectication in relationship of the Insured Person with the Proposer
d. Rectication of date of birth of the Insured Person (if this does not
impact the premium)*
e. Change in the correspondence address of the Proposer(if this does
not impact the premium)*
f. Change in Nominee Details
g. Change in Height, weight, marital status (if this does not impact the
premium) *
h. Change in bank details
i. Any other non-nancial endorsement
1.2 Financial Endorsements – which result in alteration in premium
a. Change in Age/date of birth
b. Change in Height, weight
c. Addition of Insured Person (New Born Baby or newly wedded spouse)
d. Deletion of Insured Person on death or Marital separation
e. Any other nancial endorsement
The Policyholder shallapply in a proposal form along with birthCerticate
/ marriage certicate as the case may be for addition of Insured person.
11. Cancellation (Other than free look Period)
You may cancel this Policy at any time by giving Us written notice. The
cancellation shall be from the date of receipt of such written notice. In
case of any claim made during Policy Year, no premium will be refunded
for that Policy Year.
For Policies where instalment option is not availed and no claim has
been made under the Policy, We will refund premium in accordance
with the table below:
Month
Policy Tenure
1 Year
Policy Tenure
2 Year
Policy Tenure
3 Year
Up to 1 Month 85.0% 92.5% 95.0%
Up to 3 Month 70.0% 85.0% 90.0%
Up to 6 Month 45.0% 70.0% 80.0%
Up to 12 Month 0.0% 45.0% 60.0%
Up to 15 Month NA 30.0% 50.0%
Up to 18 Month NA 20.0% 45.0%
Up to 24 Month NA 0.0% 30.0%
Up to 27 Month NA NA 20.0%
Up to 30 Month NA NA 12.5%
Up to 36 Month NA NA 0.0%
For Policies where Premium is paid by instalment, additional
conditions as given below will be applicable.
i. When yearly payment option is chosen, cancellation grid as per 1-Year
Tenure policies will be applicable
ii. For all other options, 50% of current instalment premium will be
refunded when the current period is less than 6 months in to the policy
year. For instalment after 6 months, no refund will be payable.
iii. In case of admissible claim under the Policy, future instalments for the
current policy year will be adjusted in the claim amount and no refund
of any premium will be applicable during policy year
12. Premium Tier :
For the purpose of policy issuance, the premium will be computed basis
the city of residence provided by the Insured Person in the proposal
form. Classication of cities would be as under:
• Tier 1a: Delhi and NCR region
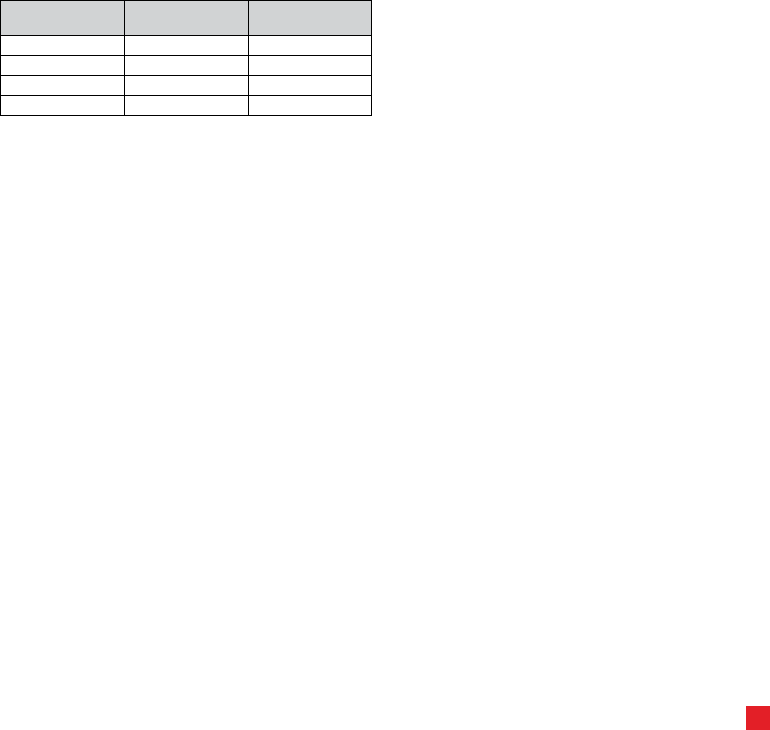
59
• Tier 1b: Mumbai, Mumbai Suburban and Navi Mumbai, Pune, Surat,
Ahmedabad, Varodara
• Tier 2: Rest of India
Conditions:
i. On payment of Tier 1a premiums, anInsured Person can avail
treatment all over India without any co-payment.
ii. On payment of Tier 1b premium, an Insured Person can avail
treatment at Tier1b cities and Tier 2 cities without any Co-Payment.
However if an Insured Person avails a treatment in Tier 1a cities , 20%
Co-Payment shall be applicable on admissible claim amount.
iii. On payment of Tier 2 premium, an Insured Person can avail treatment
at Tier 2 cities without any Co-Payment. However if an Insured Person
avails a treatment in Tier 1a or Tier1b cities, 20% Co-Payment shall be
applicable on admissible claim amount.
iv. Co-Payment under ii and iii above will not be applied If an Insured
Person opts for Hospitalization with Room Rent up to Rs 2,500 per
day or on Hospitalization for Medically Necessary treatment following
an Accident
13. Premium Payment Option
i. Insured Person has the option to pay total premium at the
commencement of policy or in instalments as per options below
Options
Installment
Premium Option
Grace Period
applicable
Option 1 Yearly 30 days
Option 2 Half Yearly 30 days
Option 3 Quarterly 30 days
Option 4 Monthly 15 days
ii. No Additional charges are levied if Premium is paid in Instalments.
iii. Grace Period shall be applicable as mentioned in the table above.
Diagnosis of Critical Illness, Undergoing of Surgical Procedure or
any Illness contracted during the Grace Period will not be admissible
under the Policy.
iv. If case of non-receipt of Instalment Premium before expiry of the
Grace Period, the policy shall stand cancelled and the Premium for
unexpired period will be refunded as below
a. When yearly payment option is chosen, cancellation grid as per 1
Year Tenure policies will be applicable
b. For all other Premium Payment options, 50% of current instalment
premium will be refunded, when the current period is less than 6 months
in to the policy year. For policy period after 6 months, no refund will
be payable.
c. No refund of Premium in case anyclaim is paid or payable during
the Policy Year.
14. Revision/ Modication of the product
We may revise the Renewal premium payable under the Policy or
the terms of cover, with the prior approval fromInsurance Regulatory
and Development Authority of India. We will intimate You of any such
changes at least 3 months prior to date of such revision or modication
15. Withdrawal of the Product
i. We may withdraw this product with the prior approval from Insurance
Regulatory and Development Authority of India.
ii. We will intimate You of any such changes at least 3 months prior to
date of such revision or modication.
iii. In such an event of withdrawal of this product, You can choose to
renew this policy under any of Our similar Health insurance products.
iv. Credit of continuity/waiting periods for all the previous policy years
would be extended in the new policy on Renewal with Us
16. Payment of Claim
i. If there are any deciencies in the necessary claim documents which
are not met or are partially met, We will send a maximum of 3 (three)
reminders following which We will send a closure letter or make a part-
payment if We have not received the deciency documents after 45 days
from the date of the initial request for such documents
ii. On receipt of all the documents and on being satised with regard to
the admissibility of the claim as per policy terms and conditions, We shall
offer within a period of 30 days a settlement of the claim to the insured.
iii. Upon acceptance of an offer of settlement by the Insured person,
the payment of the amount due shall be made within 7 days from the
date of acceptance of the offer by the insured. In the cases of delay
in the payment We shall be liable to pay interest at a rate which is 2%
above the bank rate prevalent at the beginning of the nancial year in
which the claim is reviewed by it.
iv. However, where the circumstances of a claim warrant an investigation,
We will initiate and complete such investigation at the earliest, in any
case not later than 30 days from the date of receipt of last necessary
document. In such cases, We will settle the claim within 45 days from
the date of receipt of last necessary document. In case of delay beyond
stipulated 45 days, the Company will be liable to pay interest at a rate
which is 2% above the bank rate from the date of receipt of last necessary
document to the date of payment of claim.
v. If We, for any reason decide to reject the claim the reasons regarding
the rejection shall be communicated to You in writing within 30 days of
the receipt of documents.
vi. If requested by Us and at Ourcost, the Insured Person must submit
to medical examination by Our Medical Practitioner as often as We
consider reasonable and necessary and We/Our representatives
must be permitted to inspect the medical and Hospitalization records
pertaining to the Insured Person’s treatment and to investigate the
circumstances pertaining to the claim.
vii. We and Our representatives must be given all reasonable co-
operation in investigating the claim in order to assess Our liability and
quantum in respect of the claim
B) Conditions Applicable for Section I.
2: my:health Critical Suraksha Plus
1. Fraudulent claim
• If any claim made under the Policy is found to be fraudulent, or is
supported by any fraudulent means or devices or software by Insured
Person or anyone acting on their behalf to obtain any benet under this
Policy then The policy shall be cancelled ab-initio from the inception date
or the renewal date (as the case may be),
• All benets payable, if any, under such Policy shall be forfeited with
respect to such claim
2. Geography
The policy provides worldwide coverage, there is no territorial limit
3. Free Look period
You have a period of 15 days from the date of receipt of the rst Policy
to review the terms and conditions of this Policy. If You have any
objections to any of the terms and conditions, You have the option to
cancel the Policy stating the reasons for cancellation. If you have not
made any claim during the Free look period, you shall be entitled to
refund of premium subject to,
• a deduction of the expenses incurred by Us on Your medical
examination, stamp duty charges, if the risk has not commenced,
• a deduction of the stamp duty charges, medical examination charges
& proportionate risk premium for period on cover, If the risk has
commenced
• a deduction of such proportionate risk premium commensuration
with the risk covered during such period ,where only a part of risk has
commenced
• Free Look period is not applicable for renewed policies
4. Grace Period
i. A grace period of 30 days for Renewals is permissible and the Policy
will be considered as continuous for the purpose of all waiting periods.
However, any treatment availed for an Illness contracted during the
grace period will not be admissible under the Policy.

60
ii. For Renewalreceived after completion of 30 days grace period,
the Policy would be considered as a fresh policy. All the discounts,
modications of loading earned on the previous policies shall not be
extended in the fresh Policy
iii. All eligible claims reported in the installment grace period would be
payable if otherwise admissible as per terms and conditions of the Policy
5. Renewal:
i. The Policy is ordinarily renewable for life except on grounds of fraud,
moral hazard or non-disclosure of any material facts or misrepresentation
or non-cooperation by the Insured Person (Subject to policy is renewed
annually with us within the Grace period of 30 days from the date of
Expiry)
6. Portability
An Insured Person can avail Health Insurance portability under this
Policy if;
i. The proposed Insured Person was continuously covered under any
similar health insurance Policy with any other Insurance company
ii. The proposed Insured Person was insured continuously and without
a break under another Similar retail or Group health insurance Policy
with Us.
Procedure to avail Portability:
a. The Portability benet, can be availed of by applying to Us with the
completed Proposal form and portability annexure along with previous
policy documents and renewal notice of existing policy, at least 45 days
before, but not earlier than 60 days, from the expiry of the existing
health insurance policy.
b. This benet is available only at the time of Renewal of the existing
health insurance policy.
c. If the proposed Sum Insured is higher than the Sum insured under
the expiring policy, then all waiting periods would be applied on the
increased Sum Insured.
d. Waiting period credits shall be extended to Pre-Existing Diseases
and time bound exclusions/waiting periods.
e. We will processPortabilityapplication within 15 days of receiving the
completed proposal form and Portability Form.
7. Endorsements
The following endorsements are permissible during the Policy Period:
1.3 Non-Financial Endorsements – which do not affect the premium
a. Minor rectication/correction in name of the Proposer / Insured
Person (and not the complete name change)
b. Rectication in gender of the Insured Person (if this does not impact
the premium)*
c. Rectication in relationship of the Insured Person with the Proposer
d. Rectication of date of birth of the Insured Person (if this does not
impact the premium)*
e. Change in the correspondence address of the Proposer
f. Change in Nominee Details
g. Change in Height, weight, marital status (if this does not impact
the premium)
h. Change in bank details
i. Any other non-nancial endorsement
1.4 Financial Endorsements – which result in alteration in premium
a. Change in Age/date of birth/ Gender
b. Change in Height, weight
c. Deletion of Insured Person on death or Marital separation
d. Any other nancial endorsement
e. Enhancement of Sum Insured – Enhancement of Sum Insured is
subject to Medical Underwriting
• Endorsements, a and b above shall be effective from the date of
receipt of premium withUsand weshall be effective from Date of
Commencement/Renewal of the Policy.
• The Policyholder should provide a fresh application in a proposal form
for addition of Insured person.
8. Cancellation
i. You may terminate this Policy at any time by giving Us written notice.
The cancellation shall be from the date of receipt of such written notice. In
case of any claim made during Policy Year, no premium will be refunded
on cancellation. If no claim has been made under the Policy, then We
will refund premium in accordance with the table below:
Month 1 Year 2 Year 3 Year
Up to 1 Month 85.0% 92.5% 95.0%
Up to 3 Month 70.0% 85.0% 90.0%
Up to 6 Month 45.0% 70.0% 80.0%
Up to 12 Month 0.0% 45.0% 60.0%
Up to 15 Month NA 30.0% 50.0%
Up to 18 Month NA 20.0% 45.0%
Up to 24 Month NA 0.0% 30.0%
Up to 27 Month NA NA 20.0%
Up to 30 Month NA NA 12.5%
Up to 36 Month NA NA 0.0%
ii. We may cancel on grounds of misrepresentation, fraud, non-disclosure
of material facts as sought to be in proposal form or non-cooperation
by any Insured Person. Cancelled ab initio from the inception date
or the renewal date (as the case may be), at our sole discretion upon
giving 30 days’ notice
9. Premium Payment Option
i. Insured Person shall have the option to pay Policy premium in total
at the inception of Policy or in installments as per options as below
Options Installment Premium Option
Option 1 Yearly
Option 2 Half Yearly
Option 3 Quarterly
Option 4 Monthly
ii. No Additional charges, on the existing premium are applicable
irrespective of the Installment Option selected.
iii. Grace Period of 15 days in case of Monthly premium payment option
and 30 days for half yearly and Quarterly premium payment option shall
be applicable.Diagnosis of Critical Illness, Undergoing of Surgical
Procedure or any Illness contracted during the Grace Period will not
be admissible under the Policy.
iv. If case of non-receipt of Installment Premium on the Installment due
date or before expiry of the grace period, the Policyshall stand cancelled
and the Premium for unexpired period will be refunded as below
v. Cancellation
a. When yearly payment option is chosen, cancellation grid as per 1
Year Tenure policies will be applicable
b. For all other Premium Payment options, 50% of current installment
premium will be refunded when the current period is less than 6 months
in to the Policy Year. For installment after 6 months, no refund will
be payable.
c. No refund of any premium in case of any claim during Policy Year.
10. Revision/ Modication of the product
We may revise the Renewal premium payable under the Policy or
the terms of cover, with the prior approval from Insurance Regulatory
and Development Authority of India. We will intimate You of any such
changes at least 3 months prior to date of such revision or modication.
11. Withdrawal of the Product
i. We may withdraw this product with the prior approval from Insurance
Regulatory and Development Authority of India.
ii. We will intimate You of any such changes at least 3 months prior to
date of such revision or modication.

61
iii. In the event of withdrawal of this product, You can choose to renew
this Policy under Our available similar and closely similar Health
Insurance Products.
iv. However benets payable shall be subject to the terms contained
in such other Productas approved by Insurance Regulatory and
Development Authority of India
v. Suitable credit of continuity/waiting periods for all the previous Policy
Yearshall be extended in the new Policy, provided the Policy has been
maintained without a break.
12. Payment of Claim
i. If there are any deciencies in the necessary claim documents which
are not met or are partially met, We will send a maximum of 3 (three)
reminders following which We will send a closure letter or make a part-
payment if We have not received the deciency documents after 45 days
from the date of the initial request for such documents
ii. On receipt of all the documents and on being satised with regard to
the admissibility of the claim as per Policy terms and conditions, We
shall offer within a period of 30 days a settlement of the claim to the
Insured person.
iii. Upon acceptance of an offer of settlement by the Insured person,
the payment of the amount due shall be made within 7 days from the
date of acceptance of the offer by the Insured Person. In the cases of
delay in the payment We shall be liable to pay interest at a rate which
is 2% above the bank rate prevalent at the beginning of the nancial
year in which the claim is reviewed by it.
iv. However, where the circumstances of a claim warrant an investigation,
We will initiate and complete such investigation at the earliest, in any
case not later than 30 days from the date of receipt of last necessary
document. In such cases, We will settle the claim within 45 days from
the date of receipt of last necessary document. In case of delay beyond
stipulated 45 days, the Company will be liable to pay interest at a rate
which is 2% above the bank rate from the date of receipt of last necessary
document to the date of payment of claim.
v. If We, for any reason decide to reject the claim the reasons regarding
the rejection shall be communicated to You in writing within 30 days of
the receipt of documents.
vi. If requested by Us and at Our cost, the Insured Person must submit
to medical examination by Our Medical Practitioner as often as We
consider reasonable and necessary and We/Our representatives must
be permitted to inspect the medical and Hospitalization records pertaining
to the treatment of Insured Personand to investigate the circumstances
pertaining to the claim.
vii. We and Our representatives must be given all reasonable co-
operation in investigating the claim in order to assess Our liability and
quantum in respect of the claim
C) General Conditions Applicable for Section I. 3: my:health
Medisure Super Top Up Insurance
1. Duty of Disclosure
The Policy shall be null and void and no benet shall be payable in the
event of the following:
• In case of any untrue or incorrect statements or misrepresentation, mis-
description or non-disclosure or suppression of any material particulars
as sought to be declared on the Proposal Form
• if any material information has been withheld in the Proposal Form,
personal statement, declaration or other documents,
• if a claim is found to be fraudulent or any fraudulent means or device
is used by You or any one acting on Your behalf to obtain a benet
under this Policy.
Material information to be disclosed includes every matter that You know,
or could reasonably be expected to know, that relates to questions in the
Proposal Form and which is relevant to Our decision to accept the risk
of insurance and if so on those terms. You must exercise the same duty
to disclose those matters to Us before the renewal, extension, variation,
endorsement or reinstatement of the Policy.
2. Observance of Terms and Conditions
The due observance and fulfilment of the terms, conditions and
endorsements of this Policy insofar as they relate to anything to be done
or complied with You shall be a condition precedent to any liability on
Us to make any payment under this Policy.
3. Reasonable Care
You shall take all reasonable steps to safeguard against any accident or
illnesses that may give rise to any claim under this Policy.
4. Notice of Charge
We shall not be bound to take notice or be affected by any notice of
any trust, charge, lien, assignment or other dealing with or relating to
this Policy, but Our payment to You or Your nominees or Your legal
representative or to the Hospital/Nursing Home, as the case may be,
of any benet under the Policy shall in all cases be a full, valid and an
effectual discharge by Us.
5. Electronic Transactions
You agree to adhere to and comply with all such terms and conditions
as We may prescribe from time to time, and hereby agree and conrm
that all transactions effected by or through facilities for conducting
remote transactions including the Internet, World Wide Web, electronic
data interchange, call centers, tele-service operations (whether
voice, video, data or combination thereof) or by means of electronic,
computer, automated machines network or through other means
of telecommunication, established by or on behalf of Us, for and in
respect of this Policy or its terms, or Our other products and services,
shall constitute legally binding and valid transactions when done in
adherence to and in compliance with Our terms and conditions for
such facilities, as may be prescribed from time to time. Sales through
such electronic transactions shall ensure that all conditions of Section
41 of the Insurance Act, 1938 prescribed for the proposal form and all
necessary disclosures on terms and conditions and exclusions are made
known to the Insured. A voice recording in case of tele-sales or other
evidence for sales through the World Wide Web shall be maintained
and such consent will be subsequently valix‘x‘dated/conrmed by You.
6. Subrogation
In the event of payment under this Policy, We shall be subrogated to
Your rights of recovery thereof against any person or organization, and
You shall execute and deliver instruments and papers necessary to
secure such rights. You and any claimant under this Policy shall at Our
expense do and concur in doing and permit to be done, all such acts
and things as may be necessary or required by Us, before or after Your
indemnication, in enforcing or endorsing any rights or remedies, or of
obtaining relief or indemnity, to which We shall be or would become
entitled or subrogated. This clause does not apply to coverage provided
on benet basis.
7. Contribution
If there shall be existing any other insurance covering the same Insured/
Insured Person whether effected by the Insured/Insured Person or not
and If the Claim amount exceeds the Sum Insured under the Policy after
considering the deductible or Co-pay, the Company shall not be liable to
pay or contribute more than its ratable proportion of Claim. This clause
does not apply where Claim amount is not exceeding the Sum Insured
and/or to benet sections under this Policy. Insured Person has the right
to choose the Insurer by who Claim to be settled.
8. Fraudulent Claims
If any claim is in any respect fraudulent, or if any false statement, or
declaration is made or used in support thereof, or if any fraudulent
means or devices are used by You or anyone acting on Your behalf to
obtain any benet under this Policy then this Policy shall be void and all
claims being processed shall be forfeited for all person(s) named in the
Schedule to this Policy, all sums paid under this Policy shall be repaid
to Us by all person(s) named in the Schedule to this Policy who shall
be jointly liable for such repayment.
9. Cancellation/Termination
We reserve the right and may at any time, cancel Your Policy, on grounds
of misrepresentation, fraud, non disclosure or suppression of material
facts as sought to be declared on the Proposal form or non co-operation,

62
by giving 15 days notice in writing by Registered Post Acknowledgment
Due to You at Your last known address in which case, We shall not be
liable to repay the premium for the unexpired term.
You may also give 15 days notice in writing, to Us, for the cancellation
of this Policy, in which case We shall from the date of receipt of notice
cancel the Policy and retain the premium for the period this Policy has
been in force at Our short period scales as under:
Period On Risk Rate of Premium Refunded
Up to 1 month 75% of annual Premium
Up to 3 months 50% of annual Premium
Up to 6 months 25% of annual Premium
Exceeding six months upto
365 days
Nil
In case of 2 year Policy;
If cancellation done before completion of 1 year: same grid as given
above is applicable on rst year Premium and second year Premium
will be completely refunded.
If cancellation is done after completion of 1 year: same grid as given
above is applicable however retention Premium on second year premium
will be calculated on Annual Premium without long term Policy discount.
An individual policy with a single person named in the Schedule to this
Policy shall automatically terminate in case of death of the Policyholder.
In case of an individual Policy with multiple persons named in the
Schedule to this Policy and incase of a oater, the Policy shall continue
to be in force for the remaining members of the family upto the expiry
of current Policy Period. The Policy may be renewed on an application
by another adult person named in the Schedule to this Policy, whenever
such is due.
However, in case of a valid claim having been paid or reported under
this Policy, there would be no refund of premium.
Minimum premium of Rs 250 per Policy will be retained by Us towards
administrative charges.
10. Free-look Period
A period of 15 days from the date of receipt of the Policy document is
available to review the terms and conditions of this Policy. You have
the option of cancelling the Policy stating the reasons for cancellation,
if You have any objections to any of the terms and conditions. We shall
refund the premium paid after adjusting the amounts spent on stamp duty
charges, Medical examination (wherever applicable) and proportionate
risk premium (If Policy has already commenced). Cancellation will be
allowed only if there are no claims paid or reported under the Policy.
Minimum premium shall not apply for free look cancellations.
11. Place/Currency: No claim shall be payable under this Policy for any
treatment or expenses incurred outside India. All claims shall be payable
in India and in Indian Rupees only.
12. Income Tax benet: Premium paid under the Policy shall be eligible
for benets under the Income Tax laws prevailing from time to time.
13. Law Applicable: Laws of the Republic of India shall govern the
validity, construction, interpretation and effect of this Policy or any
claim there under.
14. If a claim is rejected or partially settled and is not the subject matter
of any pending suit or other proceeding or arbitration, as the case may
be, within twelve months from the date of such rejection or settlement,
the claim shall be deemed to have been abandoned and Our liability
extinguished and shall not be recoverable thereafter.
15. Renewal
i. We shall not be bound to give notice that renewal is due.
ii. If You desire renewal, You shall apply to Us for the same prior to expiry
of the Policy Period of Insurance.
iii. Renewals are deemed to be continuous when received within a period
of 30 days from the date of expiry of last policy, subject to however, to
the effective policy inception date being reckoned from such period when
the renewal premium is received by Us.
iv. Policy will be considered as a fresh policy if there is a break of 30
or more days between the previous policy expiry date and current
policy start date.
v. We will not be liable to pay hospitalization expenses incurred during
break period. Any disease/ condition contracted in the break in period
will not be covered and will be treated as Pre-existing condition.
vi. Any enhanced Sum Insured during subsequent policy renewals will not
be available for an illness, injury already contracted under the preceding
policy periods. All Waiting periods as dened in the Policy shall apply
for this enhanced limit from the effective date of enhancement of such
Sum Insured considering such Policy Period as the rst Policy with Us.
Sum Insured enhancement will be subject to Underwriting approval.
vii. Where an individual is added to this Policy, either by way of
endorsement or at the time of renewal, the pre-existing disease clause,
exclusions and waiting periods will be applicable considering such Policy
Year as the rst year of Policy with Us.
viii. In case of oater Policies, where dependent child crosses age 23
years, renewal can be done in a separate Policy under the same Product
or any other available Products with continuity benets.
ix. A Policy shall be ordinarily renewable for lifetime unless:
a. any fraud, misrepresentation or suppression of material facts as
sought to be declared on the Proposal form by You or on Your behalf is
found either in obtaining insurance or subsequently in relation thereto or,
b. We have discontinued issuance of Policy under this Product , in which
event You will have the option of renewal under any similar Policy being
issued by Us; provided however, benets payable shall be subject to
the terms contained in such other Policy. Such modication or revision
of the terms and conditions of the Product shall be intimated to you 3
months in advance along with reasons of modication and revision.
• Based on the experience of the Product, Premium, Terms and
Conditions may be revised subject to prior approval of Insurance
Regulatory and Development Authority. Such revision shall be intimated
to you 3 months in advance with an option of renewal under any similar
Policy being issued by Us. However, benets payable shall be subject
to the terms contained in such other Policy. Individual Claims experience
loading is not applicable under the Policy.
16. Continuity Benets
For Portability Policies, continuity benefits shall be offered to all
in accordance with the Portability Guidelines issued by Insurance
Regulatory and Development Authority from time to time. Portability
benefits are not automatically applicable under the Policy unless
application for portability has been specically made and subsequently
accepted by the Company. Application for portability must be made 45
days before expiry of the Policy.
Where the product is discontinued or offered to the customers of a
specic institution, with which We have a tie up, continuity of benets
will be provided under the same or similar policies available with Us
during such period in the event that such tie-up has been discontinued
or Product is withdrawn.
17. Pre-acceptance Medical Test Requirement
a. All Individuals upto 55 years (age last birthday as at Policy inception
date) - The Company will rely on the declarations made on the Proposal
Form. In case the declaration reveals any medical adversity, the
Company may require the individual to undergo appropriate medical
tests.
b. For age group 56-65 years (age last birthday as at Policy inception
date)- The Individuals would be required to undergo pre-acceptance
medical tests as follows-Medical Examination Report, Treadmill Test/
ECG, Lipid Prole, HbA1C, Serum Creatinine, Complete Blood Count,
Urinalysis.
The Company reserves its right to require any individual to undergo such
medical tests or where required any further additional tests, at the sole
discretion of the Company to determine the acceptance of a Proposal.
The Health checkup and subsequent Medical reports are valid upto 30
days from date of Health Checkup.
In case of accepted proposals,
A 50% reimbursement of the medical test costs will be applicable for

63
accepted proposals (on our pre agreed rates with the network provider).
18. Medical Underwriting
Proposers above 55 years of age and those having medical history are
subject to Medical Underwriting by the Company. We reserve the right to
accept such proposals on standard terms/Decline/Accept with exclusion
or Premium loading (up to maximum of 100% on basic Premium).These
loadings are applied from Commencement Date of the Policy including
subsequent renewal(s) with Us.
19. Endorsements: Following type of endorsement are permissible
under the Policy.
Premium Bearing
• Increase in Sum Insured – Subject to medical underwriting permissible
at Renewal
• Decrease in Sum Insured – Permissible at Renewal unless Policy
wrongly issued by us
• Addition of member – Newly married spouse or New born baby
permissible at Renewal
• Policy cancellation
Non Premium Bearing
• Address change
• Corrections – Names, address etc
• Change of Occupation
Above list is indicative.
D) General Conditions Applicable for Section I. 4: my :hospital
Cash Benet Add on
1. Free Look period
A period of 15 days from the date of receipt of the Policy document is
available to review the terms and conditions of this Policy. You have the
option of cancelling the Policy stating the reasons for cancellation, if You
have any objections to any of the terms and conditions.
• We shall refund the premium paid after adjusting the amounts spent
on stamp duty charges, Medical examination (wherever applicable) and
proportionate premium (If Policy has already commenced).
• Cancellation will be allowed only if there are no claims paid or
reported under the Policy. Minimum premium shall not apply for free
look cancellations.
• Free Look period is not applicable for renewed policies
2. Non-Disclosure or Misrepresentation
If at the time of issuance of Policy or during continuation of the Policy,
the information provided to Us in the proposal form or otherwise, by You
or the Insured Person or anyone acting on behalf of You or an Insured
Person is found to be incorrect, incomplete, suppressed or not disclosed,
wilfully or otherwise, the Policy shall be:
• cancelled ab initio from the inception date or the Renewal date (as
the case may be), or the Policy may be modied by Us, at Our sole
discretion, upon 30 day notice by sending an endorsement to Your
address shown in the Schedule and
• the claim under such Policy if any, shall be rejected/repudiated forthwith.
3. Fraudulent claim
If any Claim made or utilization of Covers under the Policy is found
to be fraudulent, or is supported by any fraudulent means, devices or
software by Insured Person or anyone acting on their behalf to obtain
any benet under this Policy;
• The policy shall be cancelled ab-initio from the inception date or the
Renewal date (as the case may be),
• All benets payable, if any, under such Policy shall be forfeited with
respect to such claim
4. Geography
This Policy only covers medical treatment taken within India, except
under the policies with Global Cover as may be specied in the on the
Schedule of Coverage in the policy Schedule.
5. Renewal:
i. This policy is ordinarily renewable for lifetime except on grounds of
fraud, non-disclosure of material facts or misrepresentation as sought
to be declared in the proposal form or non-cooperation by the insured
ii. For dependent children, Policy is renewable up to 25 years. After the
completion of maximum Renewal age of dependent children, a separate
proposal form should be submitted to us at the time of Renewal. Suitable
credit of continuity/waiting periods and Cumulative Bonus for all the
previous policy years would be extended in the new policy, provided the
policy has been maintained without a break.
iii. You can apply for enhancement of Sum Insured or change in plan at
the time of Renewal by submitting a fresh proposal form to Us. All waiting
periods as dened in the Policy shall apply afresh for the enhanced Sum
Insured limit from the effective date of enhancement.
iv. Premium payable on Renewal and on subsequent continuation of
cover are subject to the provisions under condition 9
6. Grace Period
i. A Grace Period of 30 days for Renewals is permissible and the Policy
will be considered as continuous for the purpose of all waiting periods.
However, we shall not be liable for any treatment availed for an Illness
or Accident during the Grace Period
ii. For Renewals received after completion of 30 days Grace Period,
the policy would be considered as a fresh policy and all Waiting Periods
including those mentioned under Section E will start afresh. All the
Renewal benets earned on the previous Policy will lapse.
iii. All eligible claims reported in the grace period would be payable if
otherwise admissible as per terms and conditions of the policy.
7. Portability
An Insured person can avail Health Insurance portability under this
policy, if
i. The proposed Insured Person was continuously covered under
any similar health insurance policy with any other Insurance company
ii. The proposed Insured Person was insured continuously and without
a break under another retail or Group health insurance policy with Us.
Procedure to avail Portability:
a. The Portability benet, can be availed of by applying to Us with the
completed Proposal form and portability annexure along with previous
policy documents and Renewal notice of existing policy, at least 45
days before, but not earlier than 60 days, from the expiry of the existing
health insurance policy.
b. This benet is available only at the time of Renewal of the existing
health insurance policy.
c. If the proposed Sum Insured is higher than the Sum insured under
the expiring policy, then all waiting periods would be applied on the
increased Sum Insured.
d. Waiting period credits shall be extended to Pre-Existing Diseases
and time bound exclusions/waiting periods.
e. We will processPortabilityapplication within 15 days of receiving the
completeproposal form and Portability Form.
8. Endorsements
The following endorsements are permissible during the Policy Period:
1.5 Non-Financial Endorsements – which do not affect the premium
a. Minor rectication/correction in name of the Proposer / Insured Person
(and not the complete name change)
b. Rectication in gender of the Insured Person (if this does not impact
the premium)*
c. Rectication in relationship of the Insured Person with the Proposer
d. Rectication of date of birth of the Insured Person (if this does not
impact the premium)*
e. Change in the correspondence address of the Proposer(if this does
not impact the premium)*
f. Change in Nominee Details

64
g. Change in Height, weight, marital status (if this does not impact the
premium) *
h. Change in bank details
i. Any other non-nancial endorsement
1.6 Financial Endorsements – which result in alteration in premium
a. Change in Age/date of birth
b. Change in Height, weight
c. Addition of Insured Person (New Born Baby or newly wedded spouse)
d. Deletion of Insured Person on death or Marital separation
e. Any other nancial endorsement
The Policyholder shall apply in a proposal form along with birth Certicate
/ marriage certicate as the case may be for addition of Insured person.
9. Cancellation
• We may cancel on grounds of misrepresentation, fraud, non-disclosure
of material facts as sought to be in proposal form or non-cooperation
by any Insured Person. Cancelled ab initio from the inception date or
the renewal date (as the case may be), at our sole discretion upon
giving 30 days’ notice
• You may cancel this Policy at any time by giving Us written notice. The
cancellation shall be from the date of receipt of such written notice. In
case of any claim made during Policy Year, no premium will be refunded.
If no claim has been made under the Policy, We will refund premium in
accordance with the table below:
Month
Policy Tenure
1 Year
Policy Tenure
2 Year
Policy Tenure
3 Year
Up to 1 Month 85.0% 92.5% 95.0%
Up to 3 Month 70.0% 85.0% 90.0%
Up to 6 Month 45.0% 70.0% 80.0%
Up to 12 Month 0.0% 45.0% 60.0%
Up to 15 Month NA 30.0% 50.0%
Up to 18 Month NA 20.0% 45.0%
Up to 24 Month NA 0.0% 30.0%
Up to 27 Month NA NA 20.0%
Up to 30 Month NA NA 12.5%
Up to 36 Month NA NA 0.0%
10. Premium Payment Option
i. Insured Person shall have the option to pay premium in total at the
commencement of policy or in installments as per options below
Options Installment Premium Option
Option 1 Yearly
Option 2 Half Yearly
Option 3 Quarterly
Option 4 Monthly
ii. No Additional charges, on the existing premium are applicable
irrespective of the Installment Option selected.
iii. Grace Period of 15 days in case of Monthly premium payment option
and 30 days for half yearly, Quarterly and Yearly premium payment
option shall be applicable.
iv. If case of non-receipt of Installment Premium before expiry of the
Grace Period, the policy shall stand cancelled and the Premium for
unexpired period will be refunded as below
d. When yearly payment option is chosen, cancellation grid as per 1
Year Tenure policies will be applicable
e. For all other Premium Payment options, 50% of current installment
premium will be refunded, when the current period is less than 6 months
in to the policy year. For policy period after 6 months, no refund will
be payable.
f. No refund of any premium in case of any claim is paid during policy year
11. Revision/ Modication of the product
We may revise the Renewal premium payable under the Policy or
the terms of cover, with the prior approval from Insurance Regulatory
and Development Authority of India. We will intimate You of any such
changes at least 3 months prior to date of such revision or modication
12. Withdrawal of the Product
i. We may withdraw this product with the prior approval from Insurance
Regulatory and Development Authority of India.
ii. We will intimate You of any such changes at least 3 months prior to
date of such revision or modication.
iii. In such an event of withdrawal of this product, You can choose to
renew this policy under any of Our similar Health insurance products.
iv. Credit of continuity/waiting periods for all the previous policy years
would be extended in the new policy, provided the policy has been
continuously renewed with Us
13. Payment of Claim
i. If there are any deciencies in the necessary claim documents which
are not met or are partially met, We will send a maximum of 3 (three)
reminders following which We will send a closure letter or make a part-
payment if We have not received the deciency documents after 45 days
from the date of the initial request for such documents
ii. On receipt of all the documents and on being satised with regard to
the admissibility of the claim as per policy terms and conditions, We shall
offer within a period of 30 days a settlement of the claim to the insured.
iii. All claim payments shall be on reimbursement basis
iv. All claims payment will be made by Us in Indian rupees and into
Indian Bank accounts only
v. Upon acceptance of an offer of settlement by the Insured person, the
payment of the amount due shall be made within 7 days from the date
of acceptance of the offer by the insured. In the cases of delay in the
payment We shall be liable to pay interest at a rate which is 2% above
the bank rate prevalent at the beginning of the nancial year in which
the claim is reviewed by it.
vi. However, where the circumstances of a claim warrant an investigation,
We will initiate and complete such investigation at the earliest, in any
case not later than 30 days from the date of receipt of last necessary
document. In such cases, We will settle the claim within 45 days from
the date of receipt of last necessary document. In case of delay beyond
stipulated 45 days, the Company will be liable to pay interest at a rate
which is 2% above the bank rate from the date of receipt of last necessary
document to the date of payment of claim.
vii. If We, for any reason decide to reject the claim the reasons regarding
the rejection shall be communicated to You in writing within 30 days of
the receipt of documents.
viii. If requested by Us and at Ourcost, the Insured Person must
submit to medical examination by Our Medical Practitioner as often
as We consider reasonable and necessary and We/Our representatives
must be permitted to inspect the medical and Hospitalization records
pertaining to the Insured Person’s treatment and to investigate the
circumstances pertaining to the claim.
ix. We and Our representatives must be given all reasonable co-
operation in investigating the claim in order to assess Our liability and
quantum in respect of the claim
E) General Conditions Applicable to Section 5: Personal Accident
1. This Policy shall be governed by the laws of India and, except as
otherwise provided in Section4 (8) of this Policy, the Indian courts alone
shall have jurisdiction in any dispute arising hereunder.
2. This Policy shall be voidable in the event of misrepresentation, mis-
description or nondisclosure by any or on behalf of the Insured Person
of any material particular.
3. Insured Persons shall take all reasonable precautions to prevent
Accidents and to avoid Sickness and shall comply with all statutory
requirements, as a condition precedent to the Company’s liability
hereunder.

65
4. Where the Insured Person is required in Terms of this Policy to
perform any act or comply with any obligation timely performance or
compliance shall be a condition precedent to the Company’s liability
hereunder.
5. Insurance in respect of an Insured Person will begin under this Policy
from 00.00 a.m. on the Day after (or a future date that has been agreed
upon by the Insured Person and the Company) of the month after the
date all of the following are true:
a. the Insured Person is eligible to be insured;
b. the required premium has been paid to the Company; and
c. the Company has approved the Insured Person’s proposal for
this insurance.
6. This Policy may be cancelled at the request of the Policyholder by
thirty (30) Days notice given in writing to the Company and the premium
paid shall be adjusted on the basis of the Company retaining a minimum
of twenty-ve percent (25%) of the annual premium or earned premium
calculated pro-rata, whichever is the higher. No refund will be made for
such Insured Person for whom a claim has been paid or admitted by
the Company. This Policy may also be cancelled by the Company by
thirty (30) Days notice given in writing to the Policyholder at their last
known address on grounds of misrepresentation, fraud, non-disclosure
of material facts or non-cooperation and the premium paid shall be
adjusted on the basis of the Company retaining earned premium
calculated pro-rata.
7. Insurance in respect of an Insured Person shall immediately terminate
on the earliest of the following dates:
a. the date that the Policy is terminated;
b. the date that the Total Sum Insured is paid for covered loss under
Section 6 (Accidental Death), Section 7 (Permanent Disablement) or
any of the Hospital Cash sections of the Policy; or
c. in respect of Immediate Family, the date that such Insured Person
ceases to be the Insured Person’s Immediate Family Member.
8. In the event that the initial premium payable is not paid and realised,
this Policy shall be deemed to be void from the intended Policy Effective
Date stated in the Schedule. If one or more premiums payable under
this Policy has been paid, then the non-payment or non realisation of
any subsequent premium shall terminate this Policy as of the due date
of such unpaid or unrealised premium.
9. The Policyholder and Insured Person understand that if a proposal
has been completed for this insurance, then all statements and all
particulars provided in such proposal, and any attachments thereto,
are material to the Company’s decision to provide this insurance.
The Policyholder and Insured Person further understand that the
Company has issued this Policy in reliance upon the truth of such
statements and particulars.
10. Renewal denes the terms on which the contract of insurance can
be renewed on mutual consent with a provision of grace period for
treating the renewal continuous for the purpose of all waiting periods.
11. Free Look Period: The Policyholder have a period of 15 days
from the date of receipt of the Policy document to review the terms
and conditions of this Policy. If the policyholder has any objections to
any of the terms and conditions, then the policyholder has the option
of cancelling the Policy stating the reasons for cancellation and will be
refunded the premium paid after adjusting the amounts spent on any
medical check-up, stamp duty charges and proportionate risk premium.
The policyholder can cancel the Policy only if no claims have been
made under the Policy. All the policyholder’s rights under this Policy
will immediately stand extinguished on the free look cancellation of the
Policy. Free look provision is not applicable and available at the time
of renewal of the Policy.
12. Fraud warning:
i. Any person who, knowingly and with intent to defraud the company
or Other person, files a proposal for insurance containing any
falseInformation, or conceals for the purpose of misleading, information
ii. Concerning any fact material thereto, commits a fraudulentInsurance
act which will render the policy voidable at the company’s Sole discretion
and result in a denial of insurance benets.
iii. If a claim is in any respect fraudulent, or if any fraudulent or falsePlan,
specication, estimate, deed, book, account entry, voucher,Invoice or
other document, proof or explanation is produced, or ifAny fraudulent
means or devices are used by the insured person, Policyholder,
beneciary, claimant or by anyone acting on theirBehalf to obtain any
benet under this policy, or if any falseStatutory declaration is made
or used in support thereof, or if loss isOccasioned by or through the
procurement or with the knowledge or
iv. Connivance of the insured person, policyholder, beneciary,
claimantOr other person, then all benets under this policy are forfeited.
13. The titles of the various paragraphs of this Policy and any
endorsements attached to this Policy are inserted solely for convenience
of reference and do not limit or affect in any way the provisions to
which they relate
14. The Policyholder shown in Item 1 of the Schedule is responsible for
the collection and remittance of all premiums. Premiums are due on or
prior to the Policy Effective Date shown in Item 2 of the Schedule and,
in the case of a multi-year Policy, on or before the annual anniversary
of such Policy Effective Date. Timely payment of all premium due in full
is a condition precedent to the Company’s liability under this Policy.
15. Notices: Notices to the Company under this Policy shall be given in
writing addressed to the address shown in the preamble of this Policy.
Such notices shall be effective on the date of receipt by the Company
at such address.
16. Valuation and Foreign Currency: All premiums, benet amounts,
loss, Sums Insured and other amounts under this Policy are expressed
and payable in Indian currency. If judgement is rendered, settlement is
denominated or any benet, Sum Insured or element of loss is stated
in a currency other than Indian Rupees, then payment under this Policy
shall be made in Indian Rupees at the rate of exchange published by
the Reserve Bank of India on the date the nal judgement is entered,
the amount of settlement is agreed upon or any benet, Sum Insured
or element of loss is due, respectively.
17. Subject to the terms and conditions of this Policy, payment of the
renewal premium when due, will automatically renew this Policy. Renewal
documents will not be issued as the existing Policy is evidence of cover,
unless otherwise notied or terminated.
18. Any general increase or decrease in premium will be advised by
providing 30 days notication to the Insured Person’s last known
address.
F) General Conditions Applicable for Section 6: Travel Insurance
1) This Policy shall be governed by the laws of India and, except as
otherwise provided in Section 4(8) of this Policy, the Indian courts alone
shall have jurisdiction in any dispute arising hereunder.
2) This Policy shall be voidable in the event of misrepresentation,
misdescription or non-disclosure by any or on behalf of the Insured
Person of any material particular.
3) Insured Persons shall take all reasonable precautions to prevent
Accidents and to avoid Sickness and shall comply with all statutory
requirements, as a condition precedent to the Company’s liability
hereunder.
4) Where the Insured Person is required in Terms of this Policy to perform
any act or comply with any obligation timely performance or compliance
shall be a condition precedent to the Company’s liability hereunder.
5) Insurance in respect of an Insured Person will begin under this Policy
on the rst Day of the Insured Journey (except the Trip Cancellation
and Frequent Flyer Cancellation Sections) after the date all of the
following are true:
a) this Policy is in force;
b) the Insured Person is eligible to be insured;
c) the required premium has been paid to the Company; and
d) theCompany has approved the Insured Person’s proposal for this
insurance.
6) This Policy may be cancelled at the request of the Policyholder by
thirty (30) Days notice given in writing to the Company and the premium
paid shall be adjusted on the basis of the Company retaining a minimum

66
of Rs 251 (two fty one only). Refund of premium on cancellation will
be made under the Policy subject to no claims being paid or admitted
by the Company.
The Company reserves the right to cancel this Policy at any time by
sending thirty (30) days notice in writing to the Insured. In the event of
such cancellation refund of premium shall be on pro-rata basis.
The Company also reserves the right to cancel this Policy from inception
immediately upon becoming aware of any mis-representation, fraud,
non-disclosure of material facts or non-cooperation by or on behalf
of the Insured. No refund of premium shall be allowed in such cases.
Notice of cancellation will be mailed to the Insured at an address set forth
in the Policy Schedule, and will indicate the date of termination. If notice
of cancellation is mailed, proof of mailing will be sufcient proof of notice.
7) Insurance in respect of an Insured Person shall immediately terminate
on the earliest of the following dates:
a) the date that the Policy is terminated,
b) the date that the Total Sum Insured is paid for covered loss under
Section 6 (Accidental Death), Section 7 (Permanent Disablement) of
the Policy;
c) in respect of Immediate Family, the date that such person ceases to
be the Insured Person’s Immediate Family Member; or
d) the date when the actual number of travel days exceeds the Total
Number of Travel Days mentioned under Item 6 of the Schedule.
8) The Policyholder and Insured Person understand that if a proposal has
been completed for this insurance, then all statements and all particulars
provided in such proposal, and any attachments thereto, are material
to the Company’s decision to provide this insurance. The Policyholder
and Insured Person further understand that the Company has
issued this Policy in reliance upon the truth of such statements and
particulars.
Fraud warning:
Any person who, knowingly and with intent to defraud the company
or other person, les a proposal for insurance containing any false
information, or conceals for the purpose of misleading, information
concerning any fact material thereto, commits a fraudulent insurance
act which will render the policy voidable at the company’s sole discretion
and result in a denial of insurance benets.
if a claim is in any respect fraudulent, or if any fraudulent or false plan,
specication, estimate, deed, book, account entry, voucher, invoice or
other document, proof or explanation is produced, or if any fraudulent
means or devices are used by the insured person, policyholder,
beneciary, claimant or by anyone acting on their behalf to obtain any
benet under this policy, or if any false statutory declaration is made
or used in support thereof, or if loss is occasioned by or through the
procurement or with the knowledge or connivance of the insured person,
policyholder, beneciary, claimant or other person, then all benets under
this policy are forfeited.
9) The titles of the various paragraphs of this Policy and any
endorsements attached to this Policy are inserted solely for convenience
of reference and do not limit or affect in any way the provisions to which
they relate.
10) The Policyholder shown in Item 1 of the Schedule is responsible for
the collection and remittance of all premiums. Premiums are due on or
prior to the Policy effective Date shown in Item 2 of the Schedule and,
in the case of a multiyear Policy, on or before the annual anniversary
of such Policy Effective Date. Timely payment of all premium due in full
is a condition precedent to the Company’s liability under this Policy.
11) Notices: Notices to the Company under this Policy shall be given in
writing to the address shown in the preamble of this Policy. Such notices
shall be effective on the date of receipt by the Company at such address.
12) Valuation and Foreign Currency: All premiums, benet amounts,
loss, and other amounts under this Policy are expressed and payable
in Indian currency. If judgement is rendered, settlement is denominated
or any benet, Sum Insured or element of loss is stated in a currency
other than Indian Rupees, then payment under this Policy shall be made
in Indian Rupees at the rate of exchange published by the Reserve
Bank of India on the date the nal judgement is entered, the amount of
settlement is agreed upon or any benet, Sum Insured or element of
loss is due, respectively.
INTERNATIONAL SOS ASSISTANCE COMPANY
International SOS operates a twenty-four (24) hour, seven (7) Days a
week, toll-free emergency telephone assistance service. To access the
emergency assistance services while travelling, please call one of the
following emergency telephone numbers:
Telephone numbers:
Land line: 011-41898872
Fax: 011-41898801
Email: [email protected]
Toll Free No. 1866 202 4700 (For USA Only)
In the event of a travel-related emergency, International SOS will provide
the following assistance services:
1) Pre-Departure Services
a) Banking Facilities: - information on currencies, banking procedures
and bank hours in the country of destination.
b) Car rental Agency Referral & Limousine Arrangements - a referral
to car rental companies in foreign countries.
c) Destination Information - general information on the destination,
normally via fax.
d) Foreign Exchange Information Services - information concerning
exchange rates of major foreign currencies.
e) Hotel Accommodation Referral - the names, addresses, contact
numbers of hotels in major foreign cities world-wide.
f) Inoculation Information Services - information concerning
inoculation requirements for foreign countries.
g) Travel Advisory Services - information concerning foreign ministry
health and security advisories and circulars.
h) Visa Information Service - information concerning Visa requirements
for foreign countries.
i) Weather Information Services - weather forecasts and temperatures
of foreign countries.
2) Travel Assistance Services
a) Arrangement of a Bail Bond – the arrangement of a bail bond in
the event that an Insured Person has been arrested following a car
Accident. The Assistance Provider will only arrange the nancial
guarantee if payment has been secured through an Insured Person’s
credit card or personal assets.
b) Arranging an Emergency Cash Advance: assistance and will handle
liaisons with banks to arrange a cash advance (s) to the Insured Person,
subject to suitable guarantees.
c) Arranging for Replacement of Lost Passports - assistance in
contacting with consular authorities in case of the loss or theft of an
Insured Person’s passport, and arranging its replacement.
d) Arranging for Replacement of Lost Travel Documents – assistance
in replacing travel documents or tickets in the event of a theft or loss
or emergency.
e) Car Rental – arrangement of a rented car in the event of an
emergency. Payment is for the account of the Insured Person.
f) Claims Assistance - details to an Insured Person on how to correctly
le a claim to the Company.
g) Embassy Referral- the address, contact numbers, and ofce hours
for appropriate embassies and consulates in an emergency.
h) Emergency Travel Services – assistance in new travel arrangements
and reservations in the event of pre-departure cancellation or
interruption, curtailment or delay during the trip, or following a Hospital
stay of the Insured Person.
i) Interpreter Referral - the name, address, contact numbers and ofce
hours for interpreters world-wide.
j) Interpreting Assistance - an interpretation service over the telephone.
k) Legal Referral - the name, address, contact numbers, and ofce hours
of lawyers or legal practitioners where and when necessary.

67
l) Lost Luggage Assistance – assistance for an Insured Person who
has lost his or her luggage while travelling by contacting the appropriate
authorities involved and advising the Insured Person who they should
contact to recover their lost luggage.
m) Lost Travel Documents / Credit Card Assistance - directions on
reporting the loss and requesting replacement in the event an Insured
Person loses a travel document or credit card whilst abroad.
n) Restaurant Referral – a referral to restaurants in major foreign cities.
o) Secretarial Services & Business Centres Referral - wherever
possible, a referral to secretarial services and business centres
world-wide.
3) Emergency Medical and Related Services
a) Medical Advice Over the Phone - medical advice over the telephone.
b) Medical Service Provider Referral - information regarding
Physicians, Hospitals, Clinics, Dentists when and where the Insured
Person needs treatment.
c) Arrangement of Doctors Appointments – assistance in arranging
appointments for an Insured Person with medical service providers
if necessary.
d) Replacement of Essential Medicine - arrangement for the
replacement of essential medicines, subject to local regulations.
e) Arrangement of Hospital Admission – arrangements for Hospital
admission when the medical condition of the Insured Person requires
such action.
f) Guarantee of Medical Expenses Incurred During a Hospital
stay – a guarantee for the medical treatment necessary during an
Insured Person’s Hospital stay. The guarantees will only be arranged
if the Assistance Provider has secured payment through an Insured
Person’s credit card or through the Insured Person’s assets or the
insurance Policy.
g) Monitoring of Medical Condition during a Hospital stay – Constant
monitoring of the Insured Person’s medical condition with the attending
Physician if an Insured Person is hospitalised.
h) Emergency Message Transmission – a messenger service to
transmit messages or medical information, upon the Insured Person’s
request and consent, to the Insured Person’s family, friends and / or
business associates following a medical emergency.
i) Arranging Emergency Medical Evacuation – arrangement
of air / surface transportation, medical care during transportation,
communications and all usual ancillary services when moving an
Insured Person to the nearest Hospital where appropriate treatment
can be received.
j) Arrangement of Medical Repatriation – arrangement of air /
surface transportation, necessary medical care during transportation,
communications and all usual ancillary services when moving an Insured
Person to his/her country of residence following an emergency medical
evacuation for subsequent in-Hospital treatment.
k) Arrangement of Repatriation of Mortal Remains - the transportation
of the Insured Person’s mortal remains from the place of death to
his /her home country or arrange for local burial at the place of death.
l) Arrangement of Compassionate Visit - the return airfare for an
Immediate Family Member of the Insured Person to visit the Insured
Person when outside their normal country of residence.
m) Arrangement of Return of a Dependent Child - a one-way airfare
for the return of a Dependent Child to his or her home country, if such
Dependent Child is left unattended due to an Insured Person being
hospitalised or expecting to be hospitalised for more than ve (5) Days.
n) Arrangement of Hotel Accommodation - hotel arrangements for
a visiting family member or a Replacement Business Colleague if an
Insured Person is hospitalised or is expected to be hospitalised for
ve (5) or more Days.
Specic Conditions
The decision on the most appropriate means and timing belongs to The
Assistance Provider.
G) General Conditions Applicable for Section 7: Home Insurance
Revision
1. This policy shall be voidable in the event of mis-representation, mis-
description or non-disclosure of any material particular.
2. All insurances under this policy shall cease on expiry of seven days
from the date of fall or displacement of any building or part thereof the
whole or any part of anyrange of buildings or any of which such building
forms part. Provided such a fall or displacement is not caused by insured
perils, loss or damage which is covered by this policy or would be covered
if such building, range of buildings structure were insured under this
policy. Notwithstanding the above, the Company subject to an express
notice being given as soon as possible but not later than seven days
of any such fall or displacement may agree to continue the insurance
subject to revised rates, terms and conditions as may be decided by it
and conrmed in writing to this effect.
3. Under any of the following circumstances the insurance ceases to
attach as regards the property affected unless the insured, before the
occurrence of any loss or damage, obtains the sanction of the Company
signied by endorsement upon the policy by or on behalf of the Company:
i. If the interest in the property passes from the insured otherwise than
by will or operation of law.
4. This insurance may be terminated at any time at the request of the
insured, in which case the Company will retain the premium at customary
short period ratefor the time the policy has been in force. This insurance
may also at any time be terminated at the option of the Company, on 15
days notice to that effect beinggiven to the insured, in case of any fraud,
misrepresentation, non-disclosure of material fact or non-cooperation
of the insured as per Regulation 7(n) of IRDA(Protection on Policy
Holders interests) Regulations, 2002 in which case the Company shall
be liable to repay on demand a rateable proportion of the premium for
the unexpired term from the date of cancellation.
TABLE OF SHORT PERIOD SCALES
Period of Risk Premium to be retained
(%of the Annual Rate)
Not exceeding 15 days 10%
Not exceeding 1 Month 15%
Not exceeding 2 Months 30%
Not exceeding 3 Months 40%
Not exceeding 4 Months 50%
Not exceeding 5 Months 60%
Not exceeding 6 Months 70%
Not exceeding 7 Months 75%
Not exceeding 8 Months 80%
Not exceeding 9 Months 85%
Exceeding 9 Months Full Annual Premium
5. On the happening of any loss or damage the insured shall forthwith
give notice there of to the Company and shall within 15 days after the
loss or damage, or such further time as the Company may in writing
allow in that behalf , deliver to the Company
i. A claim in writing for the loss or damage containing as particular an
account as may be reasonably practicable of all the several articles or
items or property damaged or destroyed ,and of the amount of the loss
or damage thereto respectively, having regard to their value at the time
of the loss or damage not including prot of any kind.
ii. Particulars of all other insurances ,if any.
The Insured shall also at all the times at his own expense produce ,procure
and give to the Company all such further particulars, plans, specication
books, vouchers, invoices, duplicates or copies thereof, documents,
investigationreports(internal/external),proofsandinformationwithrespect
to the claim and the origin and cause of the loss and the circumstances
under which the loss or damage occurred, and any matter touching
the liability or the amount of the liability of the Company as may be
reasonably required by or on behalf of the Company together with a
declaration on oath in other legal form of the truth of the claim and of

68
any matters connected therewith. No claim under this policy shall be
payable unless the terms of this condition have been complied with.
II. In no case whatsoever shall the Company be liable for any loss or damage
after the expiry of 12 months from the happening of the loss or damage
unless the claim is the subject of pending action or arbitration; it being
expresslyagreedanddeclaredthatiftheCompanyshalldisclaimliabilityfor
any claim hereunder and such claim shall not within 12 (twelve)
calendar months from the date of the disclaimer have been made
the subject matter of a suit in a court of law then the claim shall for all
purposes be deemed to have been abandoned and shall not thereafter
be recoverable hereunder.
6. On the happening of loss or damage to any property insured under
this policy, the Company may
a. Enter and take keep possession of the building or premises where
the loss or damage has happened.
b. Take the possession of or require to be delivered to it any property
of the insured in the building or on the premises at the time of the loss
or damage.
c. Keep possession of any such property and examine, sort arrange
remove otherwise deal with the same.
d. Sell any such property or dispose of the same for account of whom it may
concern.Thepowersconferredbythisconditionshallbeexercisablebythe
Company at anytime until notice in writing is given by the insured that
he makes no claim under the policy, or if any claim is made, until such
claim is nally determined or withdrawn, and the Company shall not
by any act done in the exercise or purported exercise of its powers
hereunder, incur any liability to the Insured or diminish its rights to rely
upon any of the conditions of this policy in answer to any claim.If the
insured or any person on his behalf shall not comply with requirements
of the Company or shall hinder or obstruct the Company, in the exercise
of its powers hereunder, all benets under this policy shall be forfeited.
The Insured shall not in any case be entitled to abandon any property
to the Company whether taken possession of by the Company or not
7. Any person who, knowingly and with intent to defraud the insurance
company or other persons, les a proposal for insurance containing any
false information, or conceals for the purpose of misleading, information
concerning any fact material thereto, commits a fraudulent insurance act
which will render the policy voidable at the insurance company’s sole
discretion and result in a denial of insurance benets. If a claim is in
any respect fraudulent, or if any fraudulent or false plan, specication,
estimate, deed, book, account entry, voucher, invoice or other document,
proof or explanation is produced, or any fraudulent means or devices
are used by the insured, policyholder, beneciary, claimant or by anyone
acting on their behalf to obtain any benet under this policy, or if any
false statutory declaration is made or used in support .Thereof, or if loss
is occasioned by or through the procurement or with the knowledge or
connivance of the insured, policyholder, beneciary, claimant or other
person, then all benets under this policy are forfeited
8. If the Company at its option, reinstates or replaces the property
damaged or destroyed, or any part thereof, instead of paying the amount
of the loss or damage, or join with any other Company or Insurer(s)
in so doing, the Company shall not be bound to reinstate exactly or
completely but only as circumstances permit and in reasonably sufcient
manner, and in no case shall the Company be bound to expend more
in reinstatement than it would have cost to reinstate such property as it
was at the Company thereon. If the Company so elects to reinstate or
replace any property the insured shall at his own expense furnish the
Company with such plans, specications, measurements, quantities and
such other particulars as the Company may with a view to reinstatement
or replacement shall be deemed an election by the Company to reinstate
or replace. If in any case the Company shall be unable to reinstate or
repair the property hereby insured, because of any municipal or other
regulations in force affecting the alignment of streets or the construction
of buildings or otherwise, the Company shall, in every such case, only be
liable to pay such sum as would be requisite to reinstate or repair such
property if the same could lawfully be reinstated to its former condition.
9. Reinstatement Value Clause
The insurance in respect of building and all contents except Personal
Effects will be subject to the following provision:
“It is hereby declared and agreed that in the event of the building and/or
any content other than Personal Effects insured under this Policy being
lost, destroyed or damaged, the basis upon which the amount payable
under the policy is to be calculated shall be cost of replacing or reinstating
on the same site or any other site with property of the same kind or type
but not superior to or more extensive than the insured property when
new as on date of the loss, subject to the following Special Provisions
and subject also to the terms and conditions of the policy except in so
far as the same may be varied hereby.” Special Provisions:
a. The work of replacement or reinstatement (which may be carried
out upon another site and in any manner suitable to the requirements
of the insured subject to the liability of the Company not being thereby
increased) must be commenced and carried out with reasonable dispatch
and in any case must be completed within twelve (12) months after the
date of loss, destruction or damage or within such further time as the
Company may in writing allow, otherwise no payment beyond the amount
which would have been payable under the policy if this Reinstatement
Value Clause had not been incorporated there in shall be made.
b. Until expenditure has been incurred by the Insured in replacing or
reinstating the property lost, destroyed or damaged the Company shall
not be liable for any payment in excess of the amount which would have
been payable under the policy if this Reinstatement Value Clause had
not been incorporated therein.
c. If at the time of replacement or reinstatement the sum representing the
cost which would have been incurred in replacement or reinstatement
if the whole of the property covered had been destroyed, exceeds the
Sum Insured thereon or at the commencement of any loss, destruction
or damage to such property by any of the perils insured against by the
policy, then the insured shall be considered as being his own insurer for
the excess and shall bear a rateable proportion of the loss accordingly.
d. This Reinstatement Value Clause shall be without force or effect if:
1. The Insured fails to intimate to the Company within six (6) months
after the date of loss, destruction or damage or such further time as the
Company may in writing allow his intention to replace or reinstate the
property lost destroyed or damaged; or
2. The Insured is unable or unwilling to replace or reinstate the property
lost, destroyed or damaged on the same or another site.
10. If at the time of any loss or damage happening to any property hereby
insuredthere be any other subsisting insurance or insurances, whether
effected by the Insured or by any other person or persons covering the
same property, this Company shall not be liable to pay or contribute
more than its rateable proportion of such loss or damage.
11. The Insured shall at the expense of the Company do and concur in
doing, permit to be done, all such acts and things as may be necessary
or reasonably required by the Company for the purpose of enforcing any
rights and remedies or of obtaining relief or indemnity from other parties
to which the Company shall be or would become entitled or subrogated,
upon its paying for or making good any loss or damage under this policy,
whether such acts and things shall be or become necessary or required
before or after his indemnication by the Company.
12. If any dispute or difference shall arise as to the quantum to be paid
under this policy (liability being otherwise admitted) such difference
shall independently of all other questions be referred to the decision
of a sole arbitrator to be appointed in writing by the parties to or if they
cannot agree upon a single arbitrator to be within 30 days of any party
invoking arbitration, the same shall be referred to a panel of three
arbitrators, comprising of two arbitrators, one to be appointed by such
two arbitrators shall be conducted under and in accordance with the
provisions of the Arbitration and Conciliation Act, 1996, as amended. It
is clearly agreed and understood that no difference or dispute shall be
referable to arbitration as hereinbefore provided, if the Company has
disputed liability under or in respect of this policy. It is hereby expressly
stipulated and declared that it shall be a condition precedent to any right
of action or suit upon this policy that the award by such arbitrators of the
amount of the loss or damage shall be rst obtained.
13. Every notice and other communication to the Company required by
these conditions must be written and be addressed to the Company at
its corporate ofce address as follows:

69
HDFC ERGO General Insurance Company Limited
Registered & Corporate Office: 1st Floor, 165 - 166 Backbay
Reclamation, H. T. Parekh Marg, Churchgate, Mumbai – 400 020.
Customer Service Address: 6th Floor, Leela Business Park, Andheri
Kurla Road, Andheri (E), Mumbai – 400 059.
14. At all times during the period of insurance of this policy the insurance
cover will be maintained to the full extent of the respective Sum Insured
in consideration of which upon settlement of any loss under this policy,
pro-rata premium for the unexpired period from the date of such loss to
the expiry of period of insurance for the amount of such loss shall be
payable by the insured to the Company.
The additional premium referred above shall be deducted from the
net claim amount payable under the policy. This continuous cover to
the full extent will be available not withstanding any previous loss for
which the Company may have paid hereunder and irrespective of the
fact whether the additional premium as mentioned above has been
actually paid or not following such loss. The intention of this condition is
to ensure continuity of the cover to the insured subject only to the right
of the Company for deduction from the claim amount, when settled, of
pro-rata premium to be calculated from the date of loss till expiry of the
policy. Notwithstanding what is stated above, the Sum Insured shall
stand reduced by the amount of loss in case the insured immediately
on occurrence of the loss exercises his option not to reinstate the Sum
Insured as above.
15. The Insured shall take all reasonable steps to safeguard the property
insured against any loss or damage.
16. Observation of Terms and Conditions:
The due observance and fulfillment of the terms, conditions and
endorsements of this policy insofar as they relate to anything to be
done or complied with by the Insured shall be a condition precedent
to any liability of the Company to make any payment under this policy.
General Exceptions
The Company shall not be liable in respect of:
1.Loss or damage, whether director indirect occasioned by happening
through or arising from any consequencesofwar,invasion, act of foreign
enemy, hostilities (whether war be declared or not), civil war, rebellion,
revolution, insurrection military or usurped power or civil commotion or
loot or pillage in connection therewith.
2. Loss or damage caused by depreciation or wear and tear.
3. Consequentiallossofanykindordescription.
4. Loss or damage, directly or indirectly, caused by or arising from or in
consequence of or contributed to by
• Nuclear weaponsmaterial.
• Ionising radiations or contamination by radio activity from any nuclear
fuel or any nuclear waste from the combustion of nuclear fuel For this
purposeonly combustion shall include any self-sustaining process of
nuclear ssion.
4) General Conditions applicable for section 8: E@SecureInsurance
1. Triggering Multiple Specied Event
Where one loss occurrence triggering multiple Specied Events, in
such case Specied Events having highest sub limit will be payable.
2. Changes in Your circumstances
You must notify Us as soon as possible in writing of any change in Your
circumstances which may affect this insurance cover. Wewilladvise You
if there is any additional premium payable by You.
3. Taking Reasonable Precautions
You must take due care and reasonable precautions to safeguard Your
Personal Information, details of Your Bank Accounts and/or Credit/
Debit Cards and internet communications. You should also take all
practical measures to minimize claims. Such measures include but are
not limited to not sharing sensitive account information, regular data
backup, logins, PIN/TAN and Personal Information with Third Parties,
securing physical access to devices, only installing legal software from
trusted sources such as manufacturer app-stores and maintaining an
updated and secure state of their software and operating systems
as recommended by the manufacturer. You have to keep Yourself
informed of further recommendations and alerts made from time to
time by Us, Your Bank, Social Networks, other service providers or
software manufacturers, as well as relevant authorities such as the
police, CERT-IN and RBI.”
4. Fraud
You must not act in a fraudulent manner. If You, or anyone acting for You:
• Make a claim under the Policy knowing the claim to be false or
fraudulently inated;
• Cause any loss or damage by Your willful act or with Your knowledge;
• Send Us a document to support a claim knowing the document to be
forged or false in anyway; or
• Make a statement to support a claim knowing the statement to be
false in anyway,
We will not pay the claim and all cover under the Policy will be forfeited
and would render the policy void at Our sole discretion and which would
result in denial of insurance benets under this policy. We also reserve
the right to recover from You the amount of any claim We have already
paid under the Policy.
5. Cancellation
This policy will terminate at the expiration of the period for which premium
has been paid or on the expiration date shown in the policy Schedule.
You may cancel this Policy at any time by sending fteen (15) days notice
in writing to Us or by returning the Policy and stating when thereafter
cancellation is to take effect. In the event of such cancellation we will
retain the premium for the period that this Policy has been in force and
calculated in accordance with the short period rate table, provided there
is no claim under this Policy during the Period of Insurance.
We reserve the right to cancel this Policy from inception immediately
upon becoming aware of any mis-representation, mis-declaration, fraud,
non-disclosure of material facts or non-cooperation by You or on Your
behalf. No refund of premium shall be allowed in such cases.
Notice of cancellation will be mailed to You at Your address set forth
in the Policy Schedule, and will indicate the date on which coverage is
terminated. If notice of cancellation is mailed, proof of mailing will be
sufcient proof of notice.
In case of any claim under this Policy or any of its individual coverage
no refund of premium shall be allowed.
Table of Short ‘Period Scales
Period of Risk (Not exceeding) Annual Premium Rate (%)
1 month 15% of the Annual rate
2 months 30% of the Annual rate
3 months 40% of the Annual rate
4 months 50% of the Annual rate
5 months 60% of the Annual rate
6 months 70% of the Annual rate
7 months 75% of the Annual rate
8 months 80% of the Annual rate
9 months 85% of the Annual rate
For a period exceeding 9 months The full Annual rate.
6. Other Insurances
In the event of an incident which results in a claim under this Policy
and You have other insurance covering the same loss, We will not pay
more than Our share, subject to the maximum Limit of Cover granted
under this Policy.
7. Subrogation
We shall at any time be entitled to take proceedings in Your name (at
Our expense) to recover, for Our benet, the amount of any payment
made by Us under this Policy and in which case, You must cooperate
fully with Us in this respect and must not do anything to prejudice
Our rights.

70
8. Arbitration
Any and all disputes concerning the interpretation or difference of the
terms, exclusions or conditions contained herein is understood and
agreed to by both the parties are subject to Indian law.
If any difference arises as to the amount to be paid under this Policy
(liability being otherwise admitted) or the interpretation of a clause
under this Policy (including the Schedule and Endorsements), such
difference shall be referred to arbitration, in accordance with the [Indian]
Arbitration and Conciliation Act 1996, as amended, and the making of
an award shall be a condition precedent to any liability for Us to make
any payment under this Policy. Such arbitration panel shall consist of
one arbitrator selected by You, one arbitrator selected by Us, and a third
independent arbitrator selected by the rst two arbitrators in accordance
with the provisions of the [Indian] Arbitration and Conciliation Act, 1996
(as amended). The arbitration shall be governed by Indian Law and the
venue of arbitration shall be within India.
(i) All proceedings in any arbitration shall be conducted in English and
a daily transcript in English of such proceedings shall be prepared.
(ii) The cost of arbitration undertaken in accordance with this section shall
be borne by the parties associated with the arbitration and shall share
equally in the costs of the arbitration proceedings and presiding arbitrator.
(iii) It is clearly agreed and understood that no reference to arbitration
can be made if We have either not admitted or have disputed liability in
respect of any claim under or in respect of this Policy.
(iv) In the event that these arbitration provisions shall be held to be invalid
then all such disputes or differences shall be referred to the exclusive
jurisdiction of the Indian Courts.
It is further expressly agreed and declared that if We shall disclaim
liability in respect of any claim and is not within 12 calendar months
from the date of such disclaimer be made the subject matter of a suit
or proceeding before a Court of law or any other forum, it shall for all
purposes be deemed to have been abandoned and shall not thereafter
be recoverable hereunder.
9. Indian Contract Act 1872
A person or any entity who is not a party to this Policy shall have no
rights under the Contracts (Rights of Third Parties) Act 2001 or any
similar act, common law or any provision of law in any other jurisdiction
to enforce any of its terms.
10. Premium Payment
It is hereby agreed that, as a condition precedent to any liability under
this Policy, any premium due must be paid and actually realised by Usin
full. In the event of non-realisation of the premium, the Policy shall be
treated as void-ab-initio
11. Clerical Error
A clerical error by Us shall not invalidate the insurance cover otherwise
validly in force, nor continue the insurance cover otherwise not validly
in force.
12. Governing Law
This Policy shall be governed by the laws of India.
13. Assignment
No assignment of interest under this Policy shall be binding upon Us.
We do not assume any responsibility for the validity of an assignment.
14. Sanctions/Embargoes
We shall not be deemed to provide cover and provide any benet
hereunder to the extent that the provision of such cover, payment of
such loss or claim or provision of such benet would expose Us to any
sanction, prohibition or restriction under United Nations resolutions or
the trade or economic sanctions, law or regulations of the European
Union, United States of America and/or any other applicable national
economic or trade sanction law or regulations.
15. Territorial scope
Where legally permissible by the law of this policy and the jurisdiction in
which the payment is to be made and subject to all terms and conditions
of this policy, this policy shall apply to any Loss incurred or claims made
in India, unless otherwise stated in the schedule.
16. Jurisdiction
Subject to the provisions of Clause 9, this policy is subject to the exclusive
jurisdiction of the Courts of India.
17. The Proposal Form
In issuing this policy, We have relied on the statements and particulars
in the proposal form which shall form the basis of this policy and are
considered as being incorporated therein. You shall not conceal or
misrepresent or wrongfully declare any material fact or circumstance
when making any representation.
18. No Third party Rights
Notwithstanding what is stated in any Law, this policy is not intended to
confer any rights or benets on and or enforceable by any Third Party
other than You and accordingly no Third Party shall acquire any rights
in relation to or under this policy nor can enforce any benets or claim
under term of this contract against You.
19. Policy Renewal
We shall be under no obligation to renew the policy on expiry of the
period for which premium has been paid. We reserves the right to offer
revised rates, terms and conditions at renewal based on claim experience
and a fresh assessment of the risk. This policy may be renewed only by
mutual consent and subject to payment in advance of the total premium
at the rate in force at the time of renewal. We, however, shall not be
bound to give notice that the policy is due for renewal or to accept
any renewal premium. Unless renewed as herein provided, this policy
shall automatically terminate at the expiry of the Period of Insurance.
Contact Us
within India Outside India
Claim
Intimation:
Customer Service No :
022-62346234 /
0120-62346234
Phone (UAN) :
1860 2000 700 ( Local
charges applicable )
Fax (UAN) :
1860 2000 600 ( Local
charges applicable )
Email:healthclaims@
hdfcergo.com
Toll Free No:
800 08250825
Global Toll Free No:
+800 08250825
(accessible from
locations outside India
only)
Landline no
(Chargeable) :
0120-4507250
Emailtravelclaims@
hdfcergo.com
Claim
document
submission
at address
HDFC ERGO General
Insurance Co. Ltd.
Stellar IT Park,
Tower-15th Floor,
C - 25, Sector 62
Noida – 0120 398 8360
HDFC ERGO General
Insurance Co Ltd
6th Floor, Leela
Business Park,
AndheriKurla Road,
Andheri East,
Mumbai-400059,
Ph-022 66383600

71
Grievance Redressal Procedure
i.If You have a grievance that You wish Us to redress, You may contact Us with the details of Your grievance as given below:
Contact Points First Contact Point Escalation level 1 Escalation level 2
Contacts us at https://www.hdfcergo.com/
customer-care/grievances
Call - 022-62346234 / 0120-62346234
https://www.hdfcergo.com/
customecare/ grievances/escalation
level 1
Call - 022-62346234 / 0120-62346234
https://www.hdfcergo.com/
customer-care/grievances/escalation
level 2
Call - 022-62346234 / 0120-62346234
Write to us at Grievance cell of any of our
Branch ofce
The Grievance Cell, HDFC ERGO
General Insurance Company Ltd
6ht Floor, Leela Business Park,
AndheriKurla Road, Andheri,
Mumbai – 400059
Chief Grievance Ofcer, HDFC ERGO
General Insurance Company Ltd.,
D-301, 3rd Floor, Eastern Business
District (Magnet Mall), LBS Marg,
Bhandup (West) Mumbai-400078
ii.If You are not satised with Our redressal of Your grievance through one of the above methods, You may approach the nearest Insurance
Ombudsman for resolution of Your grievance. The contact details of Ombudsman ofces are mentioned below:
NAMES OF OMBUDSMAN AND ADDRESSES OF OMBUDSMAN CENTRES
Ofce Details Jurisdiction of Ofce Union Territory, District
AHMEDABAD
Ofce of the Insurance Ombudsman,
Jeevan Prakash Building, 6th oor, Tilak Marg, Relief Road, Ahmedabad – 380 001.
Tel.: 079 - 25501201/02/05/06
Email: [email protected]
Gujarat, Dadra & Nagar Haveli, Daman and Diu.
BENGALURU
Ofce of the Insurance Ombudsman,
Jeevan Soudha Building, PID No. 57-27-N-19
Ground Floor, 19/19, 24th Main Road, JP Nagar, 1st Phase, Bengaluru – 560 078.
Tel.: 080 - 26652048 / 26652049
Email: [email protected]
Karnataka
BHOPAL
Ofce of the Insurance Ombudsman,
Janak Vihar Complex, 2nd Floor,
6, Malviya Nagar, Opp. Airtel Ofce, Near New Market, Bhopal – 462 003.
Tel.: 0755 - 2769201 / 2769202, Fax: 0755 - 2769203
Email: [email protected]
Madhya Pradesh, Chattisgarh
BHUBANESHWAR
Ofce of the Insurance Ombudsman,
62, Forest park, Bhubneshwar – 751 009.
Tel.: 0674 - 2596461 /2596455, Fax: 0674 - 2596429
Email: [email protected]
Orissa
CHANDIGARH
Ofce of the Insurance Ombudsman,
S.C.O. No. 101, 102 & 103, 2nd Floor, Batra Building, Sector 17 – D,
Chandigarh – 160 017.
Tel.: 0172 - 2706196 / 2706468, Fax: 0172 - 2708274
Email: [email protected]
Punjab, Haryana, Himachal Pradesh, Jammu & Kashmir, Chandigarh.
CHENNAI
Ofce of the Insurance Ombudsman,
Fatima Akhtar Court, 4th Floor, 453, Anna Salai, Teynampet,
CHENNAI – 600 018.
Tel.: 044 - 24333668 / 24335284, Fax: 044 - 24333664
Email: [email protected]
Tamil Nadu, Pondicherry Town and Karaikal (which are part of
Pondicherry).
DELHI
Ofce of the Insurance Ombudsman,
2/2 A, Universal Insurance Building, Asaf Ali Road, New Delhi – 110 002.
Tel.: 011 - 23232481/23213504
Email: [email protected]
Delhi
GUWAHATI
Ofce of the Insurance Ombudsman,
Jeevan Nivesh, 5th Floor, Nr. Panbazar over bridge, S.S. Road,
Guwahati – 781001 (ASSAM).
Tel.: 0361 - 2632204 / 2602205
Email: [email protected]
Assam, Meghalaya, Manipur, Mizoram, Arunachal Pradesh,
Nagaland and Tripura.
HYDERABAD
Ofce of the Insurance Ombudsman,
6-2-46, 1st oor, “Moin Court”, Lane Opp. Saleem Function Palace,
A. C. Guards, Lakdi-Ka-Pool, Hyderabad - 500 004.
Tel.: 040 - 67504123 / 23312122, Fax: 040 - 23376599
Email: [email protected]
Andhra Pradesh, Telangana, Yanam and
part of Territory of Pondicherry.

72
HDFC ERGO General Insurance Company Limited. IRDAI Reg. No.146. CIN: U66030MH2007PLC177117. Registered & Corporate Ofce: 1st Floor, HDFC House,
165-166 Backbay Reclamation, H. T. Parekh Marg, Churchgate, Mumbai – 400 020. Trade Logo displayed above belongs to HDFC Ltd and ERGO International AG
and used by the Company under license. UIN: Sampoorna Suraksha - HDFHLIP20070V011920.
NAMES OF OMBUDSMAN AND ADDRESSES OF OMBUDSMAN CENTRES
Ofce Details Jurisdiction of Ofce Union Territory, District
JAIPUR
Ofce of the Insurance Ombudsman,
Jeevan Nidhi – II Bldg., Gr. Floor, Bhawani Singh Marg, Jaipur - 302 005.
Tel.: 0141 - 2740363
Email: [email protected]
Rajasthan.
ERNAKULAM
Ofce of the Insurance Ombudsman,
2nd Floor, Pulinat Bldg., Opp. Cochin Shipyard, M. G. Road, Ernakulam - 682 015.
Tel.: 0484 - 2358759 / 2359338, Fax: 0484 - 2359336
Email: [email protected]
Kerala, Lakshadweep, Mahe-a part of Pondicherry.
KOLKATA
Ofce of the Insurance Ombudsman,
Hindustan Bldg. Annexe, 4th Floor, 4, C.R. Avenue, KOLKATA - 700 072.
Tel.: 033 - 22124339 / 22124340, Fax : 033 - 22124341
Email: [email protected]
West Bengal, Sikkim, Andaman & Nicobar Islands.
LUCKNOW
Ofce of the Insurance Ombudsman,
6th Floor, Jeevan Bhawan, Phase-II, Nawal Kishore Road, Hazratganj,
Lucknow - 226 001.
Tel.: 0522 - 2231330 / 2231331, Fax: 0522 - 2231310
Email: [email protected]
Districts of Uttar Pradesh : Laitpur, Jhansi, Mahoba, Hamirpur, Banda,
Chitrakoot, Allahabad, Mirzapur, Sonbhabdra, Fatehpur, Pratapgarh,
Jaunpur,Varanasi, Gazipur, Jalaun, Kanpur, Lucknow, Unnao, Sitapur,
Lakhimpur, Bahraich, Barabanki, Raebareli, Sravasti, Gonda, Faizabad,
Amethi, Kaushambi, Balrampur, Basti, Ambedkarnagar, Sultanpur,
Maharajgang, Santkabirnagar, Azamgarh, Kushinagar, Gorkhpur,
Deoria, Mau, Ghazipur, Chandauli, Ballia, Sidharathnagar.
MUMBAI
Ofce of the Insurance Ombudsman,
3rd Floor, Jeevan Seva Annexe, S. V. Road, Santacruz (W), Mumbai - 400 054.
Tel.: 022 - 26106552 / 26106960, Fax: 022 - 26106052
Email: [email protected]
Goa, Mumbai Metropolitan Region excluding Navi Mumbai & Thane.
NOIDA
Ofce of the Insurance Ombudsman,
Bhagwan Sahai Palace 4th Floor, Main Road, Naya Bans, Sector 15,
Distt: Gautam Buddh Nagar, U.P-201301.
Tel.: 0120-2514250 / 2514252 / 2514253
Email: [email protected]
State of Uttaranchal and the following Districts of Uttar Pradesh:
Agra, Aligarh, Bagpat, Bareilly, Bijnor, Budaun, Bulandshehar, Etah,
Kanooj, Mainpuri, Mathura, Meerut, Moradabad, Muzaffarnagar,
Oraiyya, Pilibhit, Etawah, Farrukhabad, Firozbad, Gautambodhanagar,
Ghaziabad, Hardoi, Shahjahanpur, Hapur, Shamli, Rampur, Kashganj,
Sambhal, Amroha, Hathras, Kanshiramnagar, Saharanpur.
PATNA
Ofce of the Insurance Ombudsman,
1st Floor,Kalpana Arcade Building, Bazar Samiti Road, Bahadurpur, Patna 800 006.
Tel.: 0612-2680952
Email: [email protected]
Bihar, Jharkhand.
PUNE
Ofce of the Insurance Ombudsman,
Jeevan Darshan Bldg., 3rd Floor,
C.T.S. No.s. 195 to 198, N.C. Kelkar Road, Narayan Peth, Pune – 411 030.
Tel.: 020-41312555
Email: [email protected]
Maharashtra, Area of Navi Mumbai and Thane
excluding Mumbai Metropolitan Region.
