
FDA approved for Opioid Use Disorder treatment in an office-
based setting.
For those with tolerance to opioids as a result of OUD,
buprenorphine is often a safe choice.
Buprenorphine acts as a partial mixed opioid agonist at the μ-
receptor and as an antagonist at the κ-receptor. It has a higher
affinity for the μ-receptor than other opioids, and it can
precipitate withdrawal symptoms in those actively using other
opioids.
It is dosed daily, has a long half-life, and prevents withdrawal in
opioid dependent patients.
Can be in tablet, sublingual film, or injectable formulations.
Many formulations contain naloxone to prevent injection
diversion. This formulation is the preferred treatment medication.
The buprenorphine only version is often used with pregnant
women to decrease potential fetal exposure to naloxone.
There is a “ceiling effect” in which further increases above 24mg in
dosage does not increase the effects on respiratory or
cardiovascular function.
Buprenorphine should be part of a comprehensive management
program that includes psychosocial support. Treatment should
not be withheld in the absence of psychosocial support.
Overdose with buprenorphine in adults is less common, and most
likely occurs in individuals without tolerance, or who are using co-
occurring substances like alcohol or benzodiazepines.
QUICK START GUIDE
Understand that
discontinuing
buprenorphine
increases risk of
overdose death upon
return to illicit
opioid use.
Know that use of
alcohol or
benzodiazepines
with buprenorphine
increases the risk of
overdose and death.
Understand the
importance of
informing providers
if they become
pregnant.
Tell providers if they
are having a
procedure that may
require pain
medication.
Specifically discuss
safety concerns:
A patient history
Ensure that the assessment includes a medical
and psychiatric history, a substance use
history, and an evaluation of family and
psychosocial supports.
Access the patient’s prescription drug use
history through the state’s Prescription Drug
Monitoring Program (PDMP), where available,
Your
assessment should include:
Facts About Buprenorphine
Assess the need for treatment
For persons diagnosed with an opioid use
disorder,* first determine the severity of
patient’s substance use disorder. Then identify
any underlying or co-occurring diseases or
conditions, the effect of opioid use on the
patient’s physical and psychological
functioning, and the outcomes of past
treatment episodes.

A physical examination that focuses on
physical findings related to addiction and
its complications.
Laboratory testing to assess recent opioid
use and to screen for use of other drugs.
Useful tests include a urine drug screen or
other toxicology screen, urine test for
alcohol (ethyl glucuronide), liver enzymes,
serum bilirubin, serum creatinine, as well
as tests for hepatitis B and C and HIV.
Providers should not delay treatment
initiation while awaiting lab results.
to detect unreported use of other
medications, such as sedative-hypnotics or
alcohol, that may interact adversely with
the treatment medications.
Educate the patient about how the medication
works and the associated risks and benefits;
obtain informed consent; and educate on
overdose prevention.
There is potential for relapse & overdose on
discontinuation of the medication. Patients
should be educated about the effects of using
opioids and other drugs while taking the
prescribed medication and the potential for
overdose if opioid use is resumed after tolerance
is lost.
Evaluate the need for medically managed
withdrawal from opioids
Those starting buprenorphine must be in a state
of withdrawal.
Address co-occurring disorders
All medications for the treatment of the opioid use
disorder may be prescribed as part of a
comprehensive individualized treatment plan that
includes counseling and other psychosocial
therapies, as well as social support through
participation in mutual-help programs.
Have an integrated treatment approach to meet
the substance use, medical and mental health, and
social needs of a patient.
Integrate pharmacologic and nonpharmacologic
therapies
Refer patients for higher levels of care, if
necessary
*See The Criteria from American Psychiatric Association (2013). Diagnostic
and Statistical Manual of Mental Disorders, Fifth Edition,. Washington, DC,
American Psychiatric Association, page 541.
Refer the patient for more intensive or specialized
services if office-based treatment with
buprenorphine or naltrexone is not effective, or the
clinician does not have the resources to meet a
particular patient’s needs. Providers can find
programs in their areas or throughout the United
States by using SAMHSA’s Behavioral Health
Treatment Services Locator at
www.findtreatment.samhsa.gov.
Long acting opioids, such as methadone, require at least 48-72 hours since last use
before initiating buprenorphine.
Short acting opioids (for example, heroin) require approximately 12 hours since last use
for sufficient withdrawal to occur in order to safely initiate treatment. Some opioid such
as fentanyl may require greater than 12 hours.
Clinical presentation should guide this decision as individual presentations will vary.
The
dose of buprenorphine depends on the severity of withdrawal symptoms, and the
history of last opioid use (see flowchart in appendix for dosing advice).
The risk with initiating
buprenorphine too soon is
that buprenorphine has a
very high affinity for the mu
receptor and will displace
any other opioid on the
receptor, thereby causing
precipitated opioid
withdrawal.
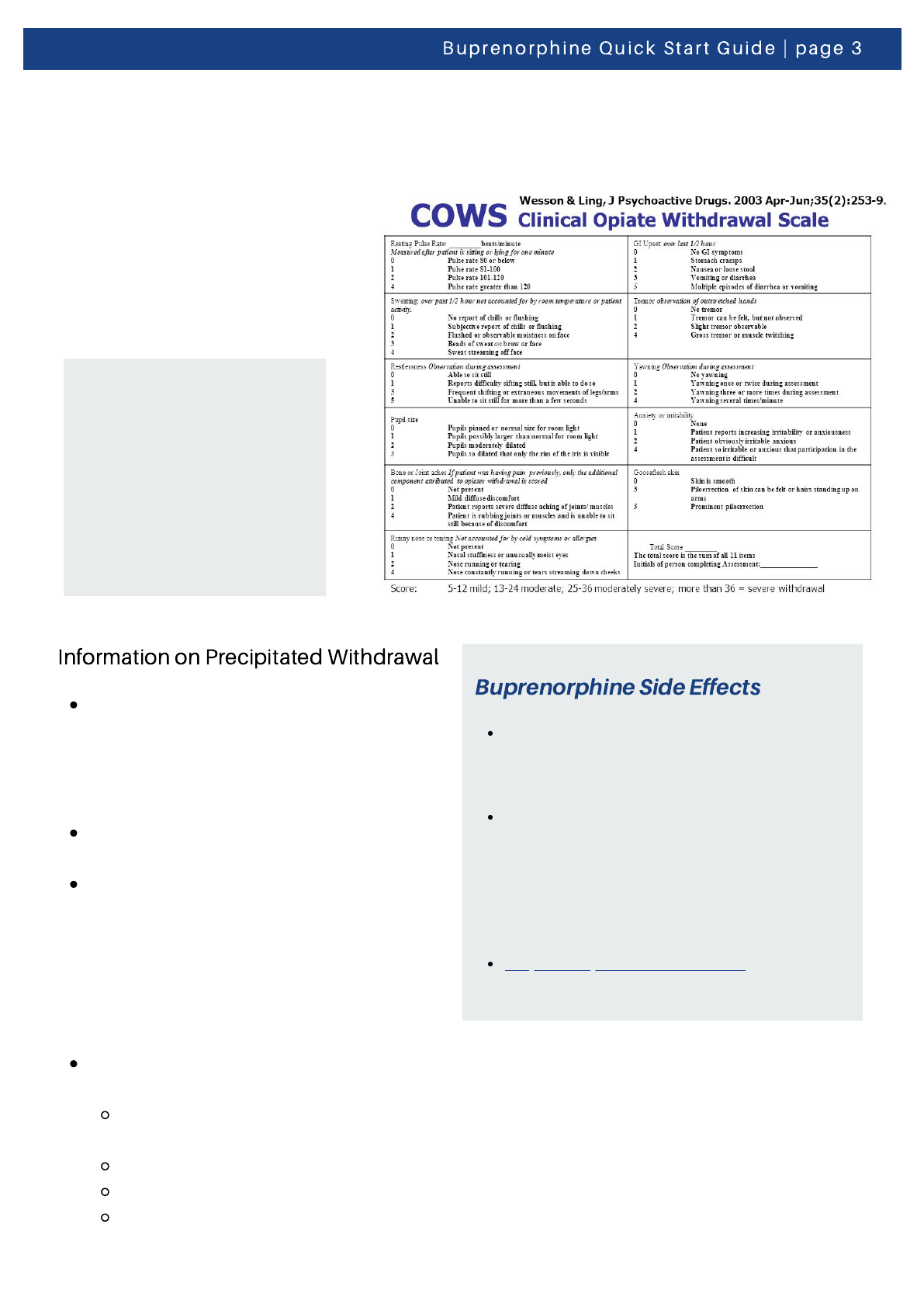
Precipitated withdrawal can occur due to
replacement of full opioid receptor
agonist (heroin, fentanyl, or morphine)
with a partial agonist that binds with a
higher affinity (Buprenorphine).
Symptoms are similar to opiate
withdrawal.
Avoid by ensuring adequate withdrawal
before induction (COWS > 12; Fentanyl
may require higher COWS score and
lower initial dosing), starting
Buprenorphine at a lower dose
(2.0mg/0.5 mg), and reassessing more
frequently.
Should precipitated withdrawal occur,
treatment includes:
Providing support and information to
the patient
Management of acute symptoms
Avoid the use of benzodiazepines
Encourage the patient to try induction
again soon
Buprenorphine’s side effects may be
less intense than those of full
agonists. Otherwise, they resemble
those of other mu-opioid agonists.
Possible side effects include: Oral
numbness, constipation, tongue pain,
oral mucosal erythema, vomiting,
intoxication, disturbance in attention,
palpitations, insomnia, opioid
withdrawal syndrome, sweating, and
blurred vision
Buprenorphine FDA labels list all
potential side effects
Determine Withdrawal
Objective withdrawal signs help establish physical dependence
Co-prescribing of overdose reversal agents
such as Naloxone is also recommended

Check PDMP regularly to
ensure prescriptions are
filled, and to check other
prescriptions.
Order urine drug testing
(UDT) and consider
confirmatory testing for
unexpected results. UDT
can facilitate open
communication to change
behavior.
Assess for readiness for
extended take-home
dosing
Goal = once-daily dosing, no
withdrawal between doses.
Ideally, average dosing does
not exceed 16 mg/4 mg (See
flowchart in appendix)
Although people often
focus on the role of
medications in MAT,
counseling and
behavioral therapies that
address psychological
and social needs may also
be included in treatment.
To find treatment, please
consult
www.findtreatment.gov.
Diversion is defined as the
unauthorized rerouting or
misappropriation of
prescription medication to
someone other than for
whom it was intended
(including sharing or selling
a prescribed medication);
m i s u s e includes taking
medication in a manner, by
route or by dose, other than
prescribed.
Early in treatment patients should be seen often, and
less frequently only when the provider determines
they are doing well.
Providers should inquire about safe and locked
storage of medications to avoid theft or inadvertent
use, especially by children. Patients must agree to safe
storage of their medication. Counsel patients about
acquiring locked devices and avoiding storage in parts
of the home frequented by visitors.
Limit medication supply. Prescribe an appropriate
amount of medications until the next visit. Do not
routinely provide an additional supply “just in case.”
Use buprenorphine/naloxone combination products
when medically indicated. Reserve daily
buprenorphine monoproducts for pregnant patients
and/or patients who could not afford treatment if the
combination product were required.
Counsel patients on taking their medication as
instructed and not sharing medication.
Ensure that the patient understands the practice’s
treatment agreement and prescription policies.
Providers can utilize the sample treatment agreement
in SAMHSA’s
TIP 63, Page 3-78. A treatment agreement
and other documentation are clear about policies
regarding number of doses in each prescription, refills,
and rules on “lost” prescriptions.
Directly observe ingestion randomly when diversion is
suspected.
Providers should order random urine drug testing to
check for other drugs and for metabolites of
buprenorphine. Providers should also consider
periodic point of care testing.
Doctors should schedule unannounced pill/film
counts. Periodically ask patients to bring in their
medication containers for a pill/film count.
Providers should make inquiries with the Prescription
Drug Monitoring program in their state to ensure that
prescriptions are filled appropriately and to detect
prescriptions from other providers.
Early in treatment, providers can ask the patient to
sign a release of information for a trusted community
support individual, such as a family member or
spouse, for the purpose of communicating treatment
concerns including diversion.
How can providers minimize diversion risk?
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.

Misuse or diversion doesn’t mean automatic discharge from the practice.
Document and describe the misuse and diversion incident. Also document the clinical thinking
that supports the clinical response, which should be aimed at minimizing future risk of diversion
while still supporting the use of MAT.
Strongly consider smaller supplies of medication and supervised dosing.
Treatment structure may need to be altered, including more frequent appointments, supervised
administration, and increased psychosocial support.
When directly observed doses in the office are not practical, short prescription time spans can
be considered.
In situations where diversion is detected, open communication with the patient is critical.
Providers may consider injectable and implantable buprenorphine to reduce diversion, once
verified.
Disclaimer: Nothing in this document constitutes an indirect or direct endorsement by the Substance Abuse and Mental Health
Services Administration (SAMHSA) or the U.S. Department of Health and Human Services (HHS) of any non-federal entity’s
products, services, or policies and any reference to a non-federal entity’s products, services, or policies should not be construed
as such. No official support of or endorsement by SAMHSA or HHS for the opinions, resources, and medications described is
intended to be or should be inferred. The information presented in this document should not be considered medical advice and
is not a substitute for individualized patient or client care and treatment decisions.

Algorithm for In-Office Induction (for home induction prescriptions may be given)
Tablets/film may be split if
necessary
May take up to 10 min to
dissolve completely (no
talking, smoking, or
swallowing at this time)
Absorption better with
moistened mouth
samhsa.gov
