
All reasonable precautions have been taken by the World Health Organization to verify the information contained in this document. However, the published material is being distributed without warranty of any kind, either expressed
or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use.
WHO acknowledges the Hôpitaux Universitaires de Genève (HUG), in particular the members of the Infection Control Programme, for their active participation in developing this material.
All reasonable precautions have been taken by the World Health Organization to verify the information contained in this document. However, the published material is being distributed without warranty of any kind, either expressed
or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use.
WHO acknowledges the Hôpitaux Universitaires de Genève (HUG), in particular the members of the Infection Control Programme, for their active participation in developing this material.
The Hand Hygiene Self-Assessment Framework is a systematic
tool with which to obtain a situation analysis of hand hygiene
promotion and practices within an individual health-care facility.
What is its purpose?
While providing an opportunity to reflect on existing resources and
achievements, the Hand Hygiene Self-Assessment Framework also
helps to focus on future plans and challenges. In particular, it acts
as a diagnostic tool, identifying key issues requiring attention and
improvement. The results can be used to facilitate development
of an action plan for the facility’s hand hygiene promotion
programme. Repeated use of the Hand Hygiene Self-Assessment
Framework will also allow documentation of progress with time.
Overall, this tool should be a catalyst for implementing and sustaining a
comprehensive hand hygiene programme within a health-care facility.
Who should use the Hand Hygiene
Self-Assessment Framework?
This tool should be used by professionals in charge of
implementing a strategy to improve hand hygiene within a health-
care facility. If no strategy is being implemented yet, then it can
also be used by professionals in charge of infection control
or senior managers at the facility directorate. The framework
can be used globally, by health-care facilities at any level of
progress as far as hand hygiene promotion is concerned.
How is it structured?
The Hand Hygiene Self-Assessment Framework is divided into five
components and 27 indicators. The five components reflect the
five elements of the WHO Multimodal Hand Hygiene Improvement
Strategy (http://www.who.int/gpsc/5may/tools/en/index.html ) and
the indicators have been selected to represent the key elements
of each component. These indicators are based on evidence and
expert consensus and have been framed as questions with defined
answers (either “Yes/No” or multiple options) to facilitate self-
assessment. Based on the score achieved for the five components,
the facility is assigned to one of four levels of hand hygiene promotion
and practice: Inadequate, Basic, Intermediate and Advanced.
Inadequate: hand hygiene practices and hand hygiene
promotion are deficient. Significant improvement is required.
Basic: some measures are in place, but not to a
satisfactory standard. Further improvement is required.
Intermediate: an appropriate hand hygiene promotion
strategy is in place and hand hygiene practices have
improved. It is now crucial to develop long-term plans to
ensure that improvement is sustained and progresses.
Advanced: hand hygiene promotion and optimal hand hygiene
practices have been sustained and/or improved, helping
to embed a culture of safety in the health-care setting.
Leadership criteria have also been identified to recognise facilities that
are considered a reference centre and contribute to the promotion
of hand hygiene through research, innovation and information
sharing. The assessment according to leadership criteria should only
be undertaken by facilities having reached the Advanced level.
How does it work?
While completing each component of the Hand Hygiene Self-
Assessment Framework, you should circle or highlight the answer
appropriate to your facility for each question. Each answer is
associated with a score. After completing a component, add up
the scores for the answers you have selected to give a subtotal for
that component. During the interpretation process these subtotals
are then added up to calculate the overall score to identify the
hand hygiene level to which your health-care facility is assigned.
The assessment should not take more than 30 minutes,
provided that the information is easily available.
Within the Framework you will find a column called “WHO
implementation tools” listing the tools made available from
the WHO First Global Patient Safety Challenge to facilitate the
implementation of the WHO Multimodal Hand Hygiene Improvement
Strategy (http://www.who.int/gpsc/5may/tools/en/index.html).
These tools are listed in relation to the relevant indicators included
in the Framework and may be useful when developing an action
plan to address areas identified as needing improvement.
Is the Hand Hygiene Self-Assessment Framework
suitable for inter-facility comparison?
Health-care facilities or national bodies may consider adopting this
tool for external comparison or benchmarking. However, this was
not a primary aim during the development of this tool. In particular,
we would draw attention to the risks inherent in using a self-reported
evaluation tool for external benchmarking and also advise the use
of caution if comparing facilities of different sizes and complexity, in
different socioeconomic settings. It would be essential to consider
these limitations if inter-facility comparison is to be undertaken.
Hand Hygiene
Self-Assessment Framework 2010
Introduction and user instructions

All reasonable precautions have been taken by the World Health Organization to verify the information contained in this document. However, the published material is being distributed without warranty of any kind, either expressed
or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use.
WHO acknowledges the Hôpitaux Universitaires de Genève (HUG), in particular the members of the Infection Control Programme, for their active participation in developing this material.
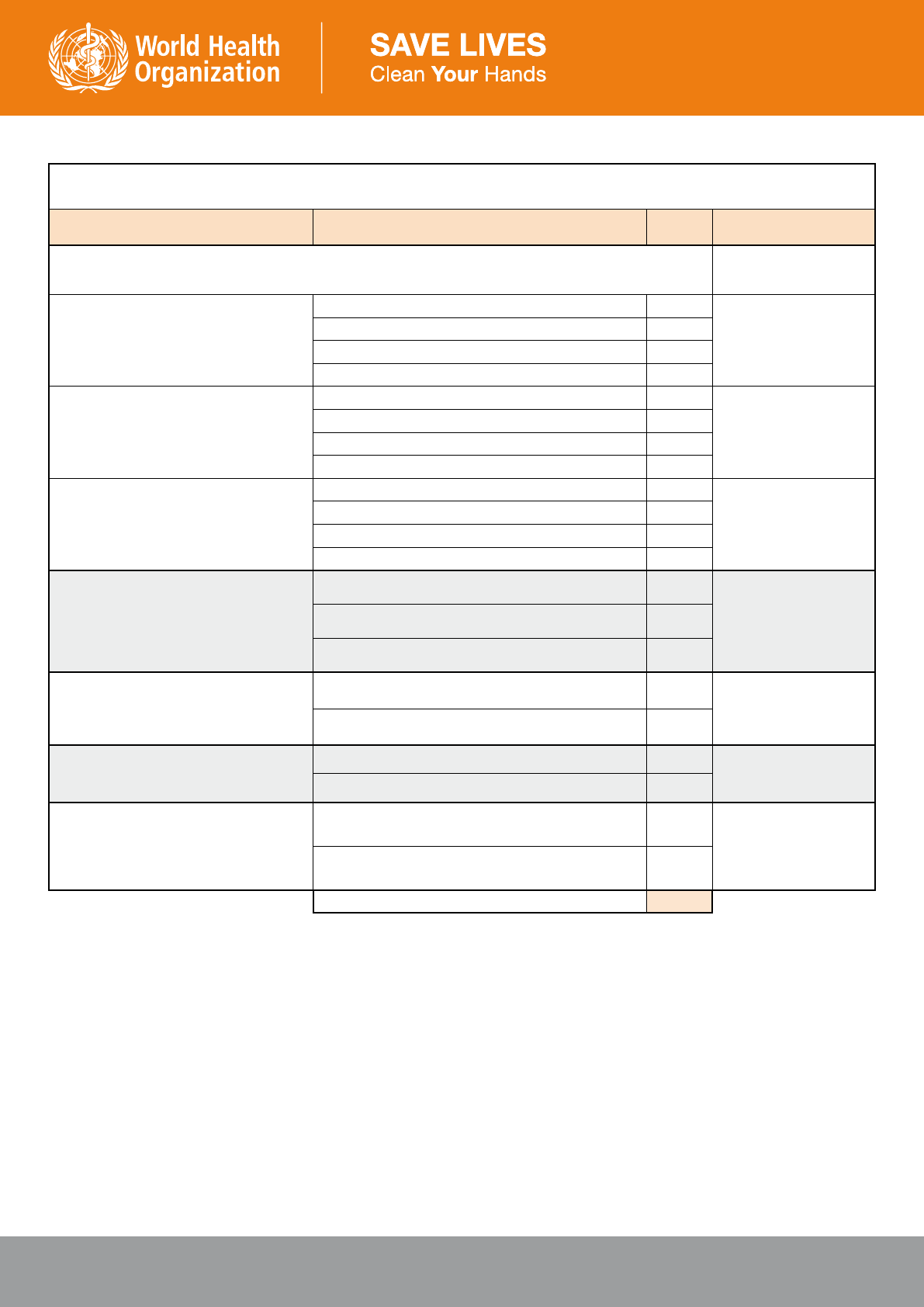
1. System Change
Question Answer Score WHO improvement tools
1.1
How easily available is alcohol-based handrub
in your health-care facility?
Choose one answer
Not available 0
Ward Infrastructure Survey
Protocol for Evaluation of
Tolerability and Acceptability
of Alcohol-based Handrub
in Use or Planned to be
Introduced:Method 1
Guide to Implementation II.1
Available, but efficacy
1
and tolerability
2
have not
been proven
0
Available only in some wards or in discontinuous
supply (with efficacy
1
and tolerability
2
proven)
5
Available facility-wide with continuous supply
(with efficacy
1
and tolerability
2
proven)
10
Available facility-wide with continuous supply, and at
the point of care
3
in the majority of wards
(with efficacy
1
and tolerability
2
proven)
30
Available facility-wide with continuous supply at each
point of care
3
(with efficacy
1
and tolerability
2
proven)
50
1.2
What is the sink:bed ratio?
Choose one answer
Less than 1:10 0
Ward Infrastructure Survey
Guide to Implementation II.1
At least 1:10 in most wards 5
At least 1:10 facility-wide and 1:1 in isolation rooms
and in intensive care units
10
1.3
Is there a continuous supply of clean, running
water
4
?
No 0
Ward Infrastructure Survey
Guide to Implementation II.1
Yes 10
1.4
Is soap
5
available at each sink?
No 0
Ward Infrastructure Survey
Guide to Implementation II.1
Yes 10
1.5
Are single-use towels available at each sink?
No 0
Ward Infrastructure Survey
Guide to Implementation II.1
Yes 10
1.6
Is there dedicated/available budget for the
continuous procurement of hand hygiene
products (e.g. alcohol-based handrubs)?
No 0
Guide to Implementation II.1
Yes 10
Extra Question: Action plan
Answer this question ONLY if you scored
less than 100 for questions 1.1 to 1.6:
Is there realistic plan in place to improve the
infrastructure
6
in your health-care facility?
No 0
Alcohol-based Handrub
Planning and Costing Tool
Guide to Local Production:
WHO-recommended Handrub
Formulations
Guide to Implementation II.1
Yes 5
System Change subtotal /100
1. Efficacy: The alcohol-based handrub product used
should meet recognised standards of antimicrobial
efficacy for hand antisepsis (ASTM or EN standards).
Alcohol-based handrubs with optimal antimicrobial
efficacy usually contain 75 to 85% ethanol, isopropanol,
or n-propanol, or a combination of these products. The
WHO-recommended formulations contain either 75%
v/v isopropanol, or 80% v/v ethanol.
2. Skin tolerability: The alcohol-based handrub
product is well tolerated by health-care workers skin
(i.e. it does not harm or irritate the skin) when used
in clinical care, as demonstrated by reliable data.
The WHO Protocol for Evaluation of Tolerability and
Acceptability of Alcohol-based Handrub in Use or
Planned to be Introduced can be used as a reference.
3. Point of care: The place where three elements come
together: the patient, the health-care worker, and care
or treatment involving contact with the patient or his/
her surroundings (within the patient zone). Point-of-care
products should be accessible without having to leave
the patient zone (ideally within arms reach of the health-
care worker or within 2 meters).
4. Clean, running water: A water supply that is either
piped in (or where this is not available, from onsite
storage with appropriate disinfection) that meets
appropriate safety standards for microbial and chemical
contamination. Further details can be found in Essential
environmental health standards in health care (Geneva,
World Health Organization, 2008, http://whqlibdoc.who.
int/publications/2008/9789241547239_eng.pdf).
5. Soap: Detergent-based products that contain no
added antimicrobial agents, or may contain these solely
as preservatives. They are available in various forms
including bar soap, tissue, leaf, and liquid preparations.
6. Infrastructure: The “infrastructure” here referred
to includes facilities, equipment, and products that are
required to achieve optimal hand hygiene practices
within the facility. Specifically, it refers to the indicators
included in questions 1.1-1.5 and detailed in the WHO
Guidelines on Hand Hygiene in Health Care 2009, Part I,
Chapter 23.5 (e.g. availability of alcohol based handrub
at all points of care, a continuous supply of clean,
running water and a sink:bed ratio of at least 1:10, with
soap and single-use towels at each sink).
Hand Hygiene Self-Assessment Framework 2010

All reasonable precautions have been taken by the World Health Organization to verify the information contained in this document. However, the published material is being distributed without warranty of any kind, either expressed
or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use.
WHO acknowledges the Hôpitaux Universitaires de Genève (HUG), in particular the members of the Infection Control Programme, for their active participation in developing this material.
2. Training and Education
Question Answer Score WHO improvement tools
2.1
Regarding training of health-care workers in your facility:
2.1a How frequently do health-care
workers receive training regarding hand
hygiene
7
in your facility?
Choose one answer
Never 0
Slides for Education Session
for Trainers, Observers and
Health-care Workers
Hand Hygiene Training Films
Slides Accompanying the
Training Films
Slides for the Hand Hygiene
Co-ordinator
Hand Hygiene Technical
Reference Manual
Hand Hygiene Why, How and
When Brochure
Guide to Implementation II.2
At least once 5
Regular training for medical and nursing staff, or all
professional categories (at least annually)
10
Mandatory training for all professional categories at
commencement of employment, then ongoing regular
training (at least annually)
20
2.1b Is a process in place to confirm
that all health-care workers complete
this training?
No 0
Yes 20
2.2
Are the following WHO documents (available at www.who.int/gpsc/5may/tools), or similar local adaptations, easily
available to all health-care workers?
Guide to Implementation II.2
2.2a The ‘WHO Guidelines on Hand
Hygiene in Health-care: A Summary’
No 0
WHO Guidelines on Hand
Hygiene in Health Care: A
Summary
Yes 5
2.2b The WHO ‘Hand Hygiene
Technical Reference Manual’
No 0
Hand Hygiene Technical
Reference Manual
Yes 5
2.2c The WHO ‘Hand Hygiene: Why,
How and When’ Brochure
No 0
Hand Hygiene Why, How and
When Brochure
Yes 5
2.2d The WHO ‘Glove Use Information’
Leaflet
No 0
Glove Use Information
Leaflet
Yes 5
2.3
Is a professional with adequate skills
8
to serve as trainer for hand hygiene
educational programmes active within the
health-care facility?
No 0
WHO Guidelines on Hand
Hygiene in Health Care
Hand Hygiene Technical
Reference Manual
Hand Hygiene Training Films
Slides Accompanying the
Training Films
Guide to Implementation II.2
Yes 15
2.4
Is a system in place for training and
validation of hand hygiene compliance
observers?
No 0
Yes 15
2.5
Is there is a dedicated budget that allows
for hand hygiene training?
No 0
Template Letter to Advocate
Hand Hygiene to Managers
Template Letter to
communicate Hand Hygiene
Initiatives to Managers
Template Action Plan
Guide to Implementation II.2
and III.1 (page 33)
Yes 10
Training and Education subtotal /100
7. Training in hand hygiene: This training can be done using different methods but
the information conveyed should be based on the WHO multimodal hand hygiene
improvement strategy or similar material. Training should include the following:
• The definition, impact and burden of health care-associated infection (HCAI)
• Major patterns of transmission of health care-associated pathogens
• Prevention of HCAI and the critical role of hand hygiene
• Indications for hand hygiene (based on the WHO ‘My 5 Moments for Hand Hygiene’
approach)
• Correct technique for hand hygiene (refer to ‘How to Handrub’ and ‘How to Hand
Wash’)
8. A professional with adequate skills: Medical staff or nursing staff trained in
Infection Control or Infectious Diseases, whose tasks formally include dedicated time
for staff training. In some settings, this could also be medical or nursing staff involved
in clinical work, with dedicated time to acquire thorough knowledge of the evidence
for and correct practice of hand hygiene (the minimum required knowledge can be
found in the WHO Guidelines on Hand Hygiene in Health Care and the Hand Hygiene
Technical Reference Manual).
Hand Hygiene Self-Assessment Framework 2010

All reasonable precautions have been taken by the World Health Organization to verify the information contained in this document. However, the published material is being distributed without warranty of any kind, either expressed
or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use.
WHO acknowledges the Hôpitaux Universitaires de Genève (HUG), in particular the members of the Infection Control Programme, for their active participation in developing this material.
3. Evaluation and Feedback
Question Answer Score WHO improvement tools
3.1
Are regular (at least annual) ward-based audits undertaken to
assess the availability of handrub, soap, single use towels and other
hand hygiene resources?
No 0
Ward Infrastructure Survey
Guide to Implementation II.3
Yes 10
3.2
Is health care worker knowledge of the following topics assessed at least annually (e.g. after education sessions)?
3.2a. The indications for hand hygiene No 0
Hand Hygiene Knowledge
Questionnaire for Health-Care
Workers
Guide to Implementation II.3
Yes 5
3.2b. The correct technique for hand hygiene No 0
Yes 5
3.3 Indirect Monitoring of Hand Hygiene Compliance
3.3a Is consumption of alcohol-based handrub monitored
regularly (at least every 3 months)?
No 0
Soap/Handrub Consumption
Survey
Guide to Implementation II.3
Yes 5
3.3b Is consumption of soap monitored regularly (at least every
3 months)?
No 0
Yes 5
3.3c Is alcohol based handrub consumption at least 20L per
1000 patient-days?
No (or not measured) 0
Yes 5
3.4 Direct Monitoring of Hand Hygiene Compliance
Only complete section 3.4 if hand hygiene compliance observers in your facility have been trained and validated and utilise the WHO
‘My 5 Moments for Hand Hygiene’ (or similar) methodology
3.4a How frequently is direct observation of hand hygiene
compliance performed using the WHO Hand Hygiene
Observation tool (or similar technique)?
Choose one answer
Never 0
WHO Hand Hygiene
Observation form
Hand Hygiene Technical
Reference Manual
Guide to Implementation II.3
Irregularly 5
Annually 10
Every 3 months or more often 15
3.4b What is the overall hand hygiene compliance rate
according to the WHO Hand Hygiene Observation tool (or
similar technique) in your facility?
Choose one answer
≤ 30% 0
Guide to Implementation II.3
Observation form
Data Entry Analysis tools
Instructions for Data Entry
and Analysis
Epi Info
TM
software
9
Data Summary Report
Framework
31 – 40% 5
41 – 50% 10
51 – 60% 15
61 – 70% 20
71 – 80% 25
≥ 81% 30
3.5 Feedback
3.5a Immediate feedback
Is immediate feedback given to health-care workers at the end
of each hand hygiene compliance observation session?
No 0
Guide to Implementation II.3
Observation and Basic
Compliance Calculation forms
Yes 5
3.5b Systematic feedback
Is regular (at least 6 monthly) feedback of data related to hand hygiene indicators with demonstration of trends
over time given to:
Data Summary Report
Framework
Guide to Implementation II.3
3.5b.i Health-care workers? No 0
Yes 7.5
3.5b.ii Facility leadership? No 0
Yes 7.5
Evaluation and Feedback subtotal /100
9. Epi InfoTM: This software can be downloaded free of charge from the CDC website (http://www.cdc.gov/epiinfo/)
Hand Hygiene Self-Assessment Framework 2010
All reasonable precautions have been taken by the World Health Organization to verify the information contained in this document. However, the published material is being distributed without warranty of any kind, either expressed
or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use.
WHO acknowledges the Hôpitaux Universitaires de Genève (HUG), in particular the members of the Infection Control Programme, for their active participation in developing this material.
4. Reminders in the Workplace
Question Answer Score WHO improvement tools
4.1
Are the following posters (or locally produced equivalent with similar content) displayed?
Guide to Implementation II.4
4.1a Poster explaining the indications
for hand hygiene
Choose one answer
Not displayed 0
Your 5 Moments for Hand
Hygiene (Poster)
Displayed in some wards/treatment areas 15
Displayed in most wards/treatment areas 20
Displayed in all wards/treatment areas 25
4.1b Poster explaining the correct use
of handrub
Choose one answer
Not displayed 0
How to Handrub (Poster)
Displayed in some wards/treatment areas 5
Displayed in most wards/treatment areas 10
Displayed in all wards/treatment areas 15
4.1c Poster explaining correct hand-
washing technique
Choose one answer
Not displayed 0
How to Handwash (Poster)
Displayed in some wards/treatment areas 5
Displayed in most wards/treatment areas 7.5
Displayed at every sink in all wards/treatment areas 10
4.2
How frequently does a systematic audit of
all posters for evidence of damage occur,
with replacement as required?
Choose one answer
Never 0
Guide to Implementation II.4
At least annually 10
Every 2-3 months 15
4.3
Is hand hygiene promotion undertaken by
displaying and regularly updating posters
other than those mentioned above?
No 0
Guide to Implementation II.4
Yes 10
4.4
Are hand hygiene information leaflets
available on wards?
No 0
Hand Hygiene: When and
How Leaflet
Guide to Implementation II.4
Yes 10
4.5
Are other workplace reminders located
throughout the facility?
(e.g. hand hygiene campaign screensavers,
badges, stickers, etc)
No 0
SAVE LIVES: Clean Your
Hands Screensaver
Guide to Implementation II.4
Yes 15
Reminders in the Workplace subtotal /100
Hand Hygiene Self-Assessment Framework 2010

All reasonable precautions have been taken by the World Health Organization to verify the information contained in this document. However, the published material is being distributed without warranty of any kind, either expressed
or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use.
WHO acknowledges the Hôpitaux Universitaires de Genève (HUG), in particular the members of the Infection Control Programme, for their active participation in developing this material.
5. Institutional Safety Climate for Hand Hygiene
Question Answer Score WHO improvement tools
5.1
With regard to a hand hygiene team
10
that is dedicated to the promotion and implementation of optimal hand
hygiene practice in your facility:
Guide to Implementation II.5
5.1a Is such a team established? No 0
Yes 5
5.1b Does this team meet on a regular basis (at least monthly)? No 0
Yes 5
5.1c Does this team have dedicated time to conduct active hand hygiene promotion?
(e.g. teaching monitoring hand hygiene performance, organizing new activities)
No 0
Yes 5
5.2
Have the following members of the facility leadership made a clear commitment to support hand hygiene improvement?
(e.g. a written or verbal commitment to hand hygiene promotion received by the majority of health-care workers)
Template Letter to Advocate
Hand Hygiene to Managers
Template Letter to
communicate Hand Hygiene
Initiatives to Managers
Guide to Implementation II.5
5.2a Chief executive officer No 0
Yes 10
5.2b Medical director No 0
Yes 5
5.2c Director of nursing No 0
Yes 5
5.3
Has a clear plan for the promotion of hand hygiene throughout the entire facility for the 5
May (Save Lives Clean Your Hands Annual Initiative) been established ?
No 0
Sustaining Improvement
– Additional Activities for
Consideration by Health-Care
Facilities
Guide to Implementation II.5
Yes 10
5.4
Are systems for identification of Hand Hygiene Leaders from all disciplines in place?
5.4a A system for designation of Hand Hygiene champions
11
No 0
Yes 5
5.4b A system for recognition and utilisation of Hand Hygiene role models
12
No 0
Yes 5
5.5
Regarding patient involvement in hand hygiene promotion:
Guidance on Engaging
Patients and Patient
Organizations in Hand Hygiene
Initiatives
Guide to Implementation II.5
5.5a Are patients informed about the importance of hand hygiene? (e.g. with a leaflet) No 0
Yes 5
5.5b Has a formalised programme of patient engagement been undertaken? No 0
Yes 10
5.6
Are initiatives to support local continuous improvement being applied in your facility, for example:
Sustaining Improvement
– Additional Activities for
Consideration by Health-Care
Facilities
Guide to Implementation II.5
5.6a Hand hygiene E-learning tools No 0
Yes 5
5.6b A hand hygiene institutional target to be achieved is established each year No 0
Yes 5
5.6c A system for intra-institutional sharing of reliable and tested local innovations No 0
Yes 5
5.6d Communications that regularly mention hand hygiene e.g. facility newsletter,
clinical meetings
No 0
Yes 5
5.6e System for personal accountability
13
No 0
Yes 5
5.6f A Buddy system
14
for new employees No 0
Yes 5
Institutional Safety Climate subtotal /100
Hand Hygiene Self-Assessment Framework 2010

All reasonable precautions have been taken by the World Health Organization to verify the information contained in this document. However, the published material is being distributed without warranty of any kind, either expressed
or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use.
WHO acknowledges the Hôpitaux Universitaires de Genève (HUG), in particular the members of the Infection Control Programme, for their active participation in developing this material.
10. Hand hygiene team: The make-up of this team will vary. It is likely to most frequently
consist of an infection control unit, but may range (depending on resources available)
from a single person with the role of managing the hand hygiene programme, to a group
of staff members from various departments within the facility with meetings dedicated to
the hand hygiene programme.
11. Hand hygiene champion: A person who is an advocate for the causes of patient
safety and hand hygiene standards and takes on responsibility for publicizing a project in
his/her ward and/or facility-wide.
12. Hand hygiene role model: A person who serves as an example, whose behaviour is
emulated by others. In particular, a hand hygiene role model should have a hand hygiene
compliance rate of at least 80%, be able to remind others to comply, and be able to teach
practically about the WHO 5 Moments for Hand Hygiene concept.
13. System for personal accountability: explicit actions are in place to stimulate
health-care workers to be accountable for their behaviour with regard to hand hygiene
practices. Examples are notification by observers or infection control professionals,
reproaches by peers, and reports to higher level facility authorities, with possible
consequences on the individual evaluation.
14. Buddy system: A programme in which each new health-care worker is coupled with
an established, trained health-care worker who takes responsibility for introducing them
to the hand hygiene culture of the health-care setting (including practical training on
indications and technique for performing hand hygiene, and explanation of hand hygiene
promotion initiatives within the facility).
All reasonable precautions have been taken by the World Health Organization to verify the information contained in this document. However, the published material is being distributed without warranty of any kind, either expressed
or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use.
WHO acknowledges the Hôpitaux Universitaires de Genève (HUG), in particular the members of the Infection Control Programme, for their active participation in developing this material.
Hand Hygiene Self-Assessment Framework 2010

All reasonable precautions have been taken by the World Health Organization to verify the information contained in this document. However, the published material is being distributed without warranty of any kind, either expressed
or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use.
WHO acknowledges the Hôpitaux Universitaires de Genève (HUG), in particular the members of the Infection Control Programme, for their active participation in developing this material.
Interpretation: A Four Step Process
1.
Add up your
points.
2.
Determine the
assigned
‘Hand Hygiene Level’
for your facility.
3.
If your facility has reached
the Advanced level, then
complete the Leadership
section overleaf.
(otherwise go to Step 4).
Score
Component Subtotal
1. System Change
2. Education and Training
3. Evaluation and Feedback
4. Reminders in the Workplace
5. Institutional Safety Climate
Total
Total Score (range) Hand Hygiene Level
0 - 125 Inadequate
126 - 250 Basic
251 - 375 Intermediate (or Consolidation)
376 - 500 Advanced (or Embedding)
4.
Review the areas identified by this evaluation
as requiring improvement in your facility
and develop an action plan to address them
(starting with the relevant WHO improvement
tools listed). Keep a copy of this assessment to
compare with repeated uses in the future.
Hand Hygiene Self-Assessment Framework 2010
All reasonable precautions have been taken by the World Health Organization to verify the information contained in this document. However, the published material is being distributed without warranty of any kind, either expressed
or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use.
WHO acknowledges the Hôpitaux Universitaires de Genève (HUG), in particular the members of the Infection Control Programme, for their active participation in developing this material.
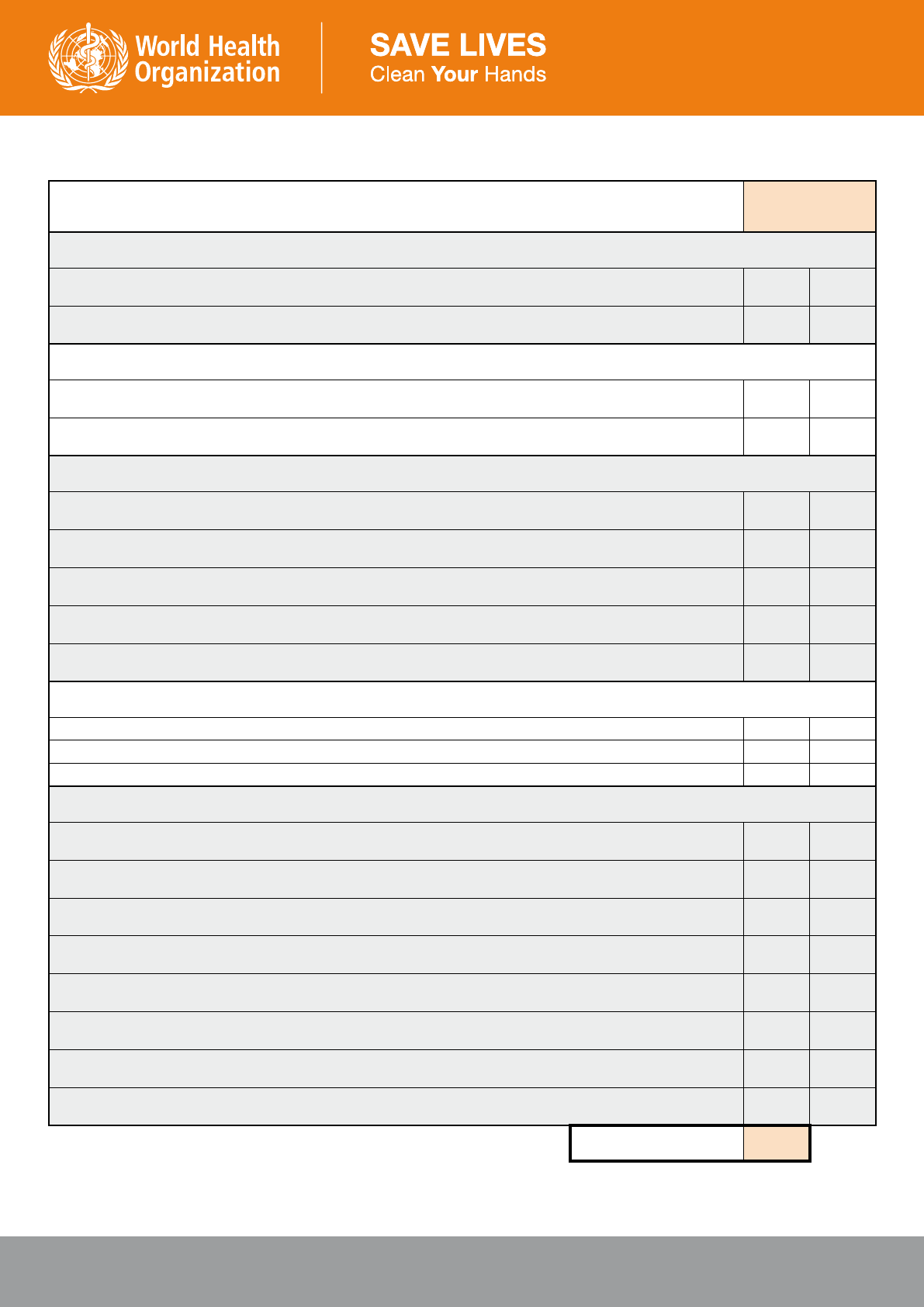
Leadership Criteria
Answer
(circle one)
System Change
Has a cost-benefit analysis of infrastructure changes required for the performance of optimal hand hygiene at the point
of care been performed?
Yes No
Does alcohol-based handrubbing account for at least 80% of hand hygiene actions performed in your facility?
Yes No
Training and Education
Has the hand hygiene team undertaken training of representatives from other facilities in the area of hand hygiene
promotion?
Yes No
Have hand hygiene principles been incorporated into local medical and nursing educational curricula?
Yes No
Evaluation and Feedback
Are specific healthcare associated infections (HCAIs) monitored? (eg. Staphylococcus aureus bacteremia, Gram
negative bacteremia, device-related infections)
Yes No
Is a system in place for monitoring of HCAI in high risk-settings? (e.g. intensive care and neonatal units)
Yes No
Is a facility-wide prevalence survey of HCAI performed (at least) annually?
Yes No
Are HCAI rates presented to facility leadership and to health-care workers in conjunction with hand hygiene compliance
rates?
Yes No
Is structured evaluation undertaken to understand the obstacles to optimal hand hygiene compliance and the causes of
HCAI at the local level, and results reported to the facility leadership?
Yes No
Reminders in the Workplace
Is a system in place for creation of new posters designed by local health-care workers? Yes No
Are posters created in your facility used in other facilities? Yes No
Have innovative types of hand hygiene reminders been developed and tested at the facility? Yes No
Institutional Safety Climate
Has a local hand hygiene research agenda addressing issues identified by the WHO Guidelines as requiring further
investigation been developed?
Yes No
Has your facility participated actively in publications or conference presentations (oral or poster) in the area of hand
hygiene?
Yes No
Are patients invited to remind health-care workers to perform hand hygiene?
Yes No
Are patients and visitors educated to correctly perform hand hygiene?
Yes No
Does your facility contribute to and support the national hand hygiene campaign (if existing)?
Yes No
Is impact evaluation of the hand hygiene campaign incorporated into forward planning of the infection control
programme?
Yes No
Does your facility set an annual target for improvement of hand hygiene compliance facility-wide?
Yes No
If the facility has such a target, was it achieved last year?
Yes No
Total /20
Your facility has reached the Hand Hygiene Leadership level if you
answered “yes” to at least one leadership criteria per category and
its total leadership score is 12 or more. Congratulations and thank you!
Hand Hygiene Self-Assessment Framework 2010
