
Community Health Needs Assessment
Suicide Attempt Survivor
Support Resources
in Southeastern Pennsylvania
Tony Salvatore
Montgomery County Emergency Service
Norristown, PA
June 2021

Information presented in this report may be triggering to some people. If this occurs or if
you are having thoughts of suicide, please call the National Suicide Prevention Lifeline at 1-
800-273-TALK (8255) or text HOME to 74174 to reach the national Crisis Text Line. Both of
these resources are available 24/7.
You may also call any of the following crisis services in SE PA 24/7:
Bucks County
Lenape Valley Foundation - 800-499-7455
Chester County
Valley Creek Crisis Center - 877-918-2100
Delaware County
Crozer Chester Medical Center Crisis - 610-447-7600
Crisis Connections - 855-889-7827
Montgomery County
MCES - 610-279-6102
ACCESS Mobile Crisis - 1-855-634-HOPE (4673)
Philadelphia County
Northeast Philadelphia - 215-831-2600
Northwest Philadelphia - 215-951-8300
North Philadelphia - 215-707-2577
Center City/South Philadelphia - 215-829-5249
West/Southwest Philadelphia - 215-748-8525
If you or someone that you know is in imminent danger of
attempting suicide call 911 immediately.
CONTENTS
Executive Summary 1
Study Background and Purpose 2
Suicide Incidence in Southeastern Pennsylvania 3
Individuals and Organizations Consulted in Study Planning 4
Role of Suicide Attempt Postvention in Suicide Prevention 5
Suicide Attempts as a Community Health Problem 7
Suicide Attempts are a High Priority Community Health Problem 9
Pertinent Findings from Suicide Attempter Research 11
Study Design and Methodology 12
Suicide Attempt Support Needs Survey 13
Support Resources in Southeastern Pennsylvania 14
The National Suicide Prevention Lifeline as a Resource 15
Recommendations 16
Appendix: Selected Resources for Attempt Survivors 17
Appendix: Suicide Attempt Research Bibliography 19
Community Health Needs Assessment
Suicide Attempt Survivor Support Resources in Southeastern Pennsylvania
EXECUTIVE SUMMARY
Individuals who have made a suicide attempt have the highest risk of dying by a subsequent
suicide attempt. A suicide attempt may occur when an at-risk person develops a strong desire
to die, has a plan and lethal means to bring about his death, and has overcome any protective
factors and the inborn resistance to engage in potentially fatal self-harm. A suicide attempt is a
traumatic event even when it results in little or no self-injury. Those who survive a suicide
attempt need both professional treatment and support in recovering from the attempt and
coping with the stigma, guilt, shame, and other negative sentiments that may follow an
attempt. A significant number of MCES admissions involve individuals who have made or tried
to make a suicide attempt.
MCES undertook an assessment of the availability of support resources in southeastern
Pennsylvania. Only two support groups for persons troubled by suicidal thoughts exist in the
region, one in Bucks County and another in Montgomery County. An online group for suicide
attempt survivors will accept participants from other counties. MCES explored the need for
suicide attempter support with stakeholders in the region and all acknowledged the need as
critical and contributing to ongoing suicide risk. MCES also conducted surveys with inpatients,
Carol’s Place clients, and online. The majority of respondents confirmed the need for suicide
prevention groups in psychiatric hospitals, a 24/7 peer-led warm line for persons dealing with
suicidal thoughts, and the formation of suicide attempter support groups in each county in the
region.
[ 1 ]

STUDY BACKGROUND AND PURPOSE
In 2001, the National Strategy for Suicide Prevention: Goals and Objectives for Action included an
objective calling for developing guidelines for aftercare treatment of individuals exhibiting suicidal
behavior. In 2005, the First National Conference for Survivors of Suicide Attempts (SOSAs), Health Care
Professionals, and Clergy and Laity offered these recommendations on enhancing service availability for
persons who had survived suicide attempts:
Key providers of community-based services must include primary and specialized mental
health treatment providers as well as clerics and lay members of faith-based
organizations.
The support and treatment resources we provide to survivors of suicide attempts must
be developed and sustained in ways that provide a stigma-free system of aftercare.
These resources also must focus on integrating SOSAs within a strengthened network of
social and community-based supports. Other resources, such as attempt survivor
support groups, are needed as effective means of mitigating the risk of suicidal
behaviors among those who engage in serial suicide attempts.
These objectives and recommendations have been echoed in many subsequent suicide
prevention plans and calls for action. This includes Pennsylvania Statewide Suicide Prevention
Plan (2020): “Promote care coordination between hospitals, crisis, behavioral health providers,
families, and community settings to support suicide attempt survivors and their families.”
The present study looks at the availability and unavailability of resources in Bucks, Chester,
Delaware, Montgomery, and Philadelphia Counties for persons who have made or tried to
make a suicide attempt. It was undertaken by Montgomery County Emergency Service (MCES)
as a nonprofit psychiatric hospital to satisfy the requirement of the Affordable Care Act to
conduct community health needs assessment identify and prioritize the significant health needs
of the community it serves every three years.
“The most glaring gap in the present system of treating suicide attempters seems to be a lack
of follow-up and continuity of treatment.”
Welu (1977)
“Because attempted suicide is the greatest known risk factor for completed suicide, reducing
suicide attempts is an important public health and clinical goal.”
Olfson, Blanco, Wall, Liu, Saha et al (2017)
[ 2 ]
SUICIDE INCIDENCE IN SOUTHEASTERN PENNSYLVANIA
Insofar as every suicide fatality involves a suicide attempt, it may be helpful to look at the
incidence of fatal suicide attempts in the region.
As reported by the Pennsylvania Department of Health, there were 9769 deaths in the state in
the five year period 2015 to 2019 in which the cause of death was intentional self-harm or
suicide. For that period, there were an average of 1954 suicides statewide yearly.
Reported suicides in the five-county region of southeastern Pennsylvania for 2015-2019 were as
follows:
County
Total
%
Age Adjusted Rate
Bucks
443
17.7
12.8/100,000
Chester
336
13.4
12/1/100,000
Delaware
379
15.2
12.3/100,000
Montgomery
547
21.9
12.4/100,000
Philadelphia
794
31.8
10.0/100,000
Total
2499
100.0
There are an average of 500 reported suicides per year in the five-county region, which
accounts for about one-fourth of all suicides in the state. More than one-half of the suicide
deaths in the region over the five-year period occurred in Philadelphia and Montgomery
Counties. The former accounted for just under one-third of all suicides in the region; the latter
experience over one-fifth of all regional suicides for the period.
[ 3 ]

INDIVIDUAL AND ORGANIZATIONS CONSULTED IN STUDY PLANNING
MCES sought input on this study from both internal and outside sources. Sources were
contacted in person; by e-mail and telephone on issues such as study scope, data sources, and
questionnaire design. The following individuals provided suggestions or advice.
Individual
Affiliation
Donna Ambrogi, MSN (Ret.)
Eagleville Hospital
Brian Barber, PhD
Montgomery County Emergency Service
Genevieve Bartuski, PsyD
Southwestern Virginia Mental Health Institute
Marina Cooney, MD
Montgomery County Emergency Service
Ruth Deming, MGPGP
New Directions Support Group
Emily Ferris
Magellan Behavioral Health of Pennsylvania
Paul De Marco
Montgomery County Commitment Office
Terri Erbacher, PhD
Philadelphia College of Osteopathic Medicine
Jess Fenchel
Access Services
Abby Grasso
NAMI-Montgomery County
Erin Hewitt
Montgomery Co. Dept. of Health and Human Services
Garra Lloyd-Lester
NY State Suicide Prevention Center
Govan Martin
Suicide Prevention Alliance, Inc.
Dave McKeighan
Chester County Medical Society
Gabriel Nathan
Suicide Prevention Activist/OCD87
Craig Oliver
Penn Foundation
Susan Shannon
Hopeworx, Inc.
Anna Trout, MSW, CPRP
Montgomery Co. Dept. of Health and Human Services
Dese'Rae L. Stage
Suicide Prevention Activist/livethroughthis.org
Moira Tumelty
Access Services
Matthew Wintersteen, PhD
Thomas Jefferson University/Prevent Suicide PA
In addition, the study was discussed at meetings of the following groups:
Managing Agencies for Excellence (MAX) Behavioral Health Committee
Montgomery County Suicide Prevention Task Force
Montgomery County Community Support Program (CSP)
MCES appreciates the cooperation that these individuals provided in planning or carrying out
the study. MCES is solely responsible for the content of this report.
[ 4 ]

ROLE OF ATTEMPT POSTVENTION IN SUICIDE PREVENTION
The public health view of prevention consists of three levels. Primary prevention works to deter
the problem. Secondary prevention works to identify the emerging problem and try to stop its
progression. Tertiary prevention involves treating the problem and deterring its recurrence.
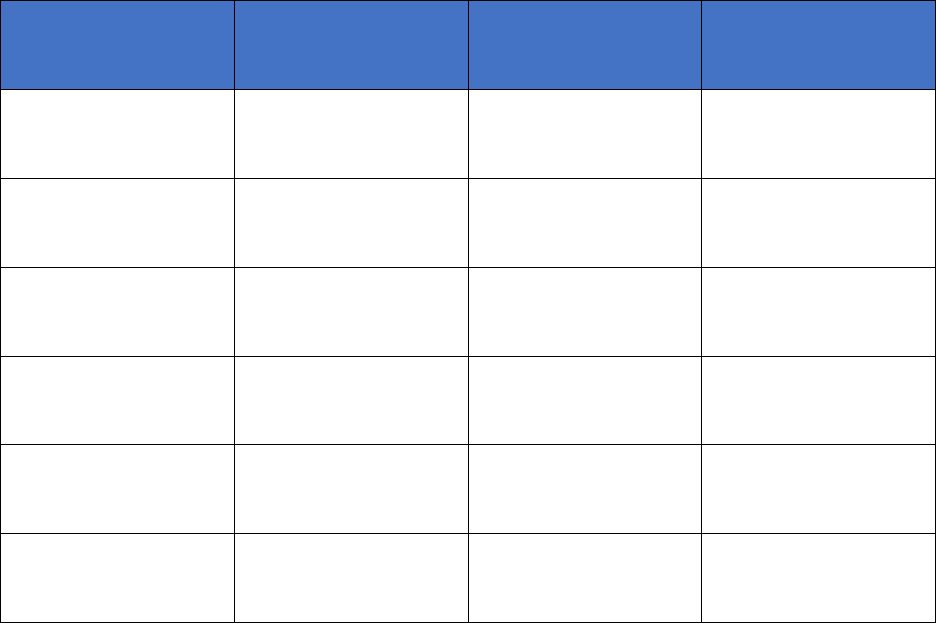
This figure applies the public health model to suicide attempt prevention:
Prevention
Intervention
Postvention
Averting occurrence of a
suicide attempt by:
• Managing specific risk
attempt factors
• Enhancing protective
factors for attempts
Averting suicide attempt
by:
• Identifying and
assessing suicide risk
• Crisis counseling and
referral
Averting suicidality
recurrence by:
• Providing post-attempt
support
• Providing post-attempt
therapy
There is little programming to enhance safety from behavior that may result in a suicide
attempt. Most suicide attempt prevention actually involves direct efforts to dissuade or deter a
person felt to be in imminent danger of making a suicide attempt from doing so. This is most
often accomplished by hot lines, crisis centers, and mobile crisis teams, and police officers. The
last level of suicide prevention is facilitating the recovery of a person experiencing a suicide loss
or surviving a suicide attempt. The latter is known as postvention and is the focus of this study.
Making or trying to make a suicide attempt is a traumatic event. Protective factors have failed,
risk factors are strong, intent to die is severe, a doable plan and lethal means are on hand, and
resistance to potentially fatal self-injury has been overcome. If a suicide attempt does not
proceed, or if it is survived, many of the prerequisites remain. Only intent may subside. Ongoing
suicide risk is very high. Protective factors remain weak. Suicide plans may stay in mind and the
means may continue to be available or accessible. Coming to the brink of ending one’s life r
weakens resistance to do so again if the circumstances fomenting the suicide risk again occur.
An attempt survivor must contend with other issues. The negative life events or problems that
precipitated the progression of the attempt survivor’s suicidality may persist or return.
Stressors such as loss, abuse, chronic illness or pain, disability, substance abuse, mental illness,
financial or housing insecurity, interpersonal conflict, social isolation, and criminal justice
involvement do not subside after a suicide attempt. Feelings of hopelessness, , guilt and shame
that may accrue after a suicide attempt can make the situation worse.
[ 5 ]
Perhaps the most deleterious and compelling impediment to recovery from a suicide attempt is
the stigma the individual may feel from others. While a suicide attempt is often the result of an
individual being overwhelmed by events in her or his life that she or he cannot control and
which have overcome their coping ability, others may see it as selfishness, attention seeking, an
effort at manipulation, or a sign of weakness. In some cases, the self-stigma that may be self-
inflicted. Feelings of stigma may be greater when there have been multiple attempts.
Many suicide attempts result in voluntary or involuntary treatment in a psychiatric inpatient
unit or a psychiatric hospital. An involuntary hospitalization is traumatizing and may cause the
individual to feel angry and betrayed, suspicious of those who might be sources of support, and
less likely to follow the aftercare plan provided at discharge. The days and weeks immediately
after a psychiatric hospitalization, even when not related to suicidality, is a period of high risk
for suicide. This is because the stabilization and safety provided by the hospital are removed
and psychosocial and environmental stressors reassert themselves.
It is the role of postvention to address the challenges that someone contending with the
aftermath of an effort to try to die by suicide or surviving a deliberate suicide attempt.
Postvention can come from various sources and may include:
Information and education about suicide risk and suicide attempts
Self-help and self-care measures to deter the onset of suicidal thoughts
A personal safety plan to use if a suicide crisis occurs
[ 6 ]

SUICIDE ATTEMPTS AS A COMMUNITY HEALTH PROBLEM
The Centers for Disease Control and Prevention defines a suicide attempt as “A non-fatal, self-
directed, potentially injurious behavior with intent to die as a result of the behavior. A suicide attempt
might not result in injury. In 2019, the National Survey on Drug Use and Health (NSDUH) found
that 0.6% of adults age 18 and older, 1.4 million persons, in the United States reported they
attempted suicide in in the past year. Among adults across all age groups, the prevalence of
suicide attempt in the past year was highest among young adults 18-25 years old (1.8%).
Among adults age 18 and older, the prevalence of suicide attempts in the past year was highest
among those who report having multiple (two or more) races (1.5%).
A CDC study of 1.2 million “suicidal acts” treated in emergency departments and hospitals
found an increase in incidence of such acts in females and in adults ages 65-74 and an increase
in the lethality of the act in adults ages 20-64 between 2006 and 2015.
The national Youth Risk Behavior Survey (YRBS) found that in 2019, 8.9% of youths interviewed
in 9
th
to 12
th
grade made one or more suicide attempts in the twelve months before the survey.
Medical treatment was necessary in 2.5% of the suicide attempts reported by youths in the
survey. The Pennsylvania Youth Survey reported that one in ten youths in the state attempted
suicide in 2017. The American Association for Suicidology (AAS) estimates that there is a suicide
attempt every 26.6 seconds in the United States.
Data for suicide attempts in general is not available at the state or national levels. The Injuries
in Pennsylvania Report issued by the Pennsylvania Department of Health presents the following
data for 2014 (most recent data) for acute hospital discharges for intentional self-injuries, many
of which were suicide attempts requiring inpatient medical treatment:
Statewide 8524
Bucks County 324
Chester County 243
Delaware County 347
Montgomery County 437
Philadelphia County 1014
This indicates that the five-county region accounts for almost 28% of medically serious
intentional self-injuries in Pennsylvania requiring hospital treatment.
According to the American Foundation for Suicide Prevention (AFSP), it is generally accepted
that there are at least 25 suicide attempts for every death by suicide. This can be used to derive
a rough approximation of the total suicide attempts in the state (47,175) and in the region
(13,050) in 2019.
[ 7 ]

SUICIDE ATTEMPTS ARE A HIGH PRIORITY COMMUNITY HEALTH PROBLEM
A suicide attempt may be thought of as the behavior that may immediately precede and
bring about a suicide fatality. It involves all of the elements of a suicide except death. These
include the intent to die, a plan for how, where, and when, and the means to be used to take
one’s life. A suicide attempt survivor is an individual who had intent to die, a plan for
bringing about her or his death at a specific time and place, and the means to do so, but for
some reason, did not die as intended, planned, and acted.
Of the components of a suicide attempt that did not end in death, intent to die is both the
most serious and transient. It may subside on its own or as the result of intervention or
treatment. A suicide plan once conceived and means once selected are more durable. Plans
remain available and may be revisited if intent returns. A suicide plan and means may also
become more lethal.
A suicide attempt that did not become a suicide is the strongest risk factor for a subsequent
attempt and suicide. The AFSP advises that between 25% and 50% people who kill
themselves had previously attempted suicide. Those who have made suicide attempts are
at higher risk for actually taking their own lives. While most who survive a suicide attempt
do not re-attempt, they remain at high risk, some very high. Of suicide attempt survivors who
required treatment in a hospital, about 5% to 11% go on to die by suicide.
The Interpersonal Psychological Theory (IPPT) of suicide is the prevalent theoretical model of
suicide and has been supported by research across various populations. It posits that a
potentially lethal suicide attempt may occur when an individual has both an intense desire to
die and the ability to take her or his life. Intent may arise from a sense that one is socially
disconnected from significant others or is a burden to them and that they will be better off if
one were dead. The capability for a suicide attempt is achieved when one does not fear dying
and has overcome the inborn resistance to self-directed death. This may come about in various
ways but perhaps the most effective is by making a suicide attempt. Resistance to dying by
one’s on hand weakens with each attempt.
A key tenet of the IPPT and related theories is that a suicide attempt is not primarily the
product of and impulsive decision. Impulsivity makes an attempt more likely but most often it is
the outcome of a process of psychosocial debilitation. The factors driving this process do not
necessarily abate with the attempt, even when the intent to die is lessened. One of the most
dangerous myths of suicide is the belief that surviving a suicide attempt indicates a lack of
intent to die. This misconception ignores the reality that intent may be rekindled by subsequent
life circumstances and/or misperceptions of one’s value to others, may rejoin the strengthened
acquired ability to die by suicide, and restart the downward process towards an attempt.
[ 8 ]

SELECTED RESEARCH FINDINGS ON SUICIDE ATTEMPT SURVIVORS
Key findings from recent studies of suicide attempt survivors’ postvention needs and
preferences, impediments to access to mental health services and recommended changes:
A first suicide attempt creates high risk for suicide; the great majority of completed
suicides occur within a year of the first attempt, hospitalization following the attempt,
as well as a scheduled follow-up visit with a psychiatrist significantly, reduced that risk.
Persons who made suicide attempts had disproportionately elevated risk because of
high levels of economic insecurity associated with unemployment and low income and
educational attainment.
Persons who have made a suicide attempt are may not disclose it to avoid stigma.
Responding to anticipated suicide stigma was found to be significantly associated with
increased suicidality in attempt survivors.
Persons who have made a suicide attempt want practical information countering
stigma, addressing negative community attitudes towards suicide, and promoting hope.
Personal stories of recovery by attempt survivors were identified as very useful.
Person who have made a suicide attempt and treated in a hospital emergency
department provide family information but collateral contacts may not be made and
when they are family members are not always given written information on resources.
Persons who made suicide attempts and participated in a Survivors of Suicide Attempts
peer-led support group for 8-weeks offering peer discussion and information sharing
had a decrease in suicidality and hopelessness and a significant increase in resilience.
Persons who made suicide attempts and who were treated in an emergency psychiatric
unit received follow-up telephone calls from a psychiatric nurse at 8, 30, and 60 days
within one year after discharge made fewer subsequent attempts.
Low social support was strongly associated with suicide attempts among low-income
African American men and women treated at a large, urban hospital. Greater availability
of social supports can be a protective factor for suicide attempts in this population.
Persons who made suicide attempts and who were associated with a suicide education
advocacy project reported a high degree of engagement with mental health services but
experienced stigma, loss of autonomy, issues with assessment and medication.
[ 9 ]

Persons who made suicide attempts and utilized available mental health services
reported dissatisfaction with outpatient and inpatient treatment. Most recommended
that being able to connect with persons with lived experience would be helpful.
Persons who made suicide attempts who are members of gender and sexual minorities
reported severe stigma and hopelessness after their attempts. They identified a need for
peer support to enhance their recovery and reduce the risk of future attempts.
Two-thirds of persons who made a recent suicide attempts surveyed as part of the
National Epidemiological Survey on Alcohol and Related Conditions had a diagnosis of
borderline personality disorder and experienced negative provider attitudes.
Persons who made suicide attempts in a South African study voiced a desire for mental
health services addressing suicide risk and deterring suicidal behavior, teaching self-help
strategies and promoting social connectiveness and support.
A study of psychiatric inpatients who had made suicide attempts found that those who
had made only one attempt reported less social support than those who had made
multiple attempts suggesting that support may be a buffer against further attempts.
Persons who made planned suicide attempts manifest distinct suicide-related clinical
characteristics that are severe and warrant early, targeted intervention and long-term
follow-up by treatment providers.
[ 10 ]
STUDY DESIGN AND METHODOLOGY
The study was generally qualitative in nature and loosely involved a mixed methods approach
including the following activities:
Consultation with groups and organizations involved with suicide prevention, crisis
intervention, and mental health advocacy to determine interest in the topic. A one-page
outline of the proposed study was distributed by e-mail to prospective stakeholders in
the 5-county region.
Review of research articles reporting the need for support by suicide attempt survivors
or findings relevant to this topic.
Review of the literature describing support resources (e.g., peer support, peer-led
groups) for suicide attempt survivors
Identifying existing suicide attempt support resources in SE PA by surveying health and
behavioral health providers serving individuals who have made suicide attempts.
Consultation with a focus group of individuals with lived experience of a suicide attempt
or an interest in developing supports for suicide attempt survivors
Surveying individuals in SE PA who identified as suicide attempt survivors or who had
felt at risk of making a suicide attempt to determine the type of support resources they
feel best supports the needs of persons recovering from a suicide attempt. A copy of the
questionnaire is in the Appendices.
[ 11 ]
SUICIDE ATTEMPT SUPPORT NEEDS SURVEY
Summary:
Majority of respondents do not feel that mental health services do enough to help
suicidal persons
Majority of respondents feel there is a need for a suicide attempters support group
Majority of respondents would seek help from a peer specialists with lived experience of
a suicide attempt
Majority of respondents felt that should be a warm line for persons having thoughts of
suicide
Majority of respondents would seek help from a family member, other trusted person, a
peer specialist, or a peer-led resource if having thoughts of making a suicide attempt
All respondents feel that psychiatric hospitals should have inpatient suicide prevention
groups
Great majority of respondents acted in some way to make a suicide attempt
Almost three-fourths of respondents made two or more suicide attempts
Most respondents who made a suicide attempt sought medical help
Almost one-half of respondents who made attempt had thoughts of suicide in the past
and over one-third had frequent thoughts of suicide
1. Do mental health services offer enough help for suicidal persons?
Strongly Agree 2 5.35
Agree Somewhat 4 10.5%
Strongly Disagree 20 52.6%
Agree Somewhat 12 31.6%
2. Do you feel there is a need for a support group to help persons who have made suicide
attempts?
Yes 36 94.7%
No 0 -
DK 2 5.3%
3. Would you seek help from a peer specialist who had experienced a suicide attempt if one
were available?
Definitely Would 19 50.0%
Probably Would 10 26.3%
Probably Would Not 7 18.4%
Definitely Would Not 0 -
[ 12 ]

4. Do you think that there should be a 24/7 peer warm line for persons with thoughts of
suicide?
Yes 34 89.5%
No 1 2.6%
DK 3 7.9$
5. What would you do to get help if you had thoughts of making a suicide attempt?
Family Member, Friend, Other Trusted Person 10 26.3%
Peer Specialist or Other Peer-led Resource 9 23.7%
Use W.R.A.P. or Safety Plan 3 7.9%
Hot Line, Crisis Center, Mobile Crisis Team 8 21.0%
Hospital Emergency Department 6 15.8%
6. Should psychiatric hospitals have suicide prevention groups for current patients?
Strongly Agree 25 65.8%
Agree 13 34.2%
Strongly Disagree 0 -
Disagree 0 -
7. Have you ever made a suicide attempt, i.e., wanted to die and did something to try to end
your life?
Yes 33 86.8%
No 5 13.2%
8. If yes, how many suicide attempts have you made?
One 9 27.3%
Two to four 19 57.6%
Five or more 4 12.1%
9. If yes, did you ever require medical treatment for hurting yourself in a suicide attempt?
Received care at a hospital/healthcare provider 24 72.7%
Did not seek medical treatment 5 15.1%
Did not need medical treatment 4 12.1%
10. If yes, have you ever had thoughts of making a suicide attempt or making another attempt?
Have had thoughts in the past 16 48.5%
Have frequent thoughts 12 36.4%
Have not had any thoughts 5 15.1%
[ 13 ]

SUPPORT RESOURCES IN SOUTHEASTERN PENNSYLVANIA
An internet search and inquiries to stakeholders did not identify any community-based support
groups or other resources in the region with the explicit mission or purpose of aiding or
supporting suicide attempt survivors. The following resources offering help to persons troubled
by suicidal thoughts and behaviors are presently available in the five-county area. At the time of
this writing, all groups are meeting online because of COVID-19.
Bucks County
Alternatives to Suicide Peer-to-Peer Support Group: Sponsored by NAMI Bucks County.
Meets 2
nd
and 4
th
Tuesdays and every Saturday. “The opportunity to talk openly about
suicide and feelings of deep emotional distress with others who have or are
experiencing similar struggles.”
Chester County
None located
Delaware County
None located
Montgomery County
Alternatives to Suicide Peer-to-Peer Support Group: Program of Resources for Human
Development initiated in March 2019, hosting weekly meetings in Abington, PA, where
individuals can discuss and explore suicidal thoughts and feelings.
Philadelphia County
None located
Regional
AFSP of Greater Philadelphia includes the page “I’ve survived a suicide attempt” on its
website at https://afsp.org/after-an-attempt offering information for suicide attempt
survivors.
[ 14 ]
THE NATIONAL SUICIDE PREVENTION LIFELINE AS A RESOURCE
MCES has been part of the National Suicide Prevention Lifeline since 2014. We frequently
receive on the Lifeline are from individuals who feel at risk of making a suicide attempt. There
are now three other Lifeline call centers in SE PA. How can this availability and accessibility be
used to optimally serve suicide attempt survivors and others at risk of suicidal behavior? A 2007
publication, Lifeline Service and Outreach Strategies Suggested by Suicide Attempt Survivors,
offers several recommendations that are still timely:
Crisis line workers should recognize that attempt survivors who are struggling with
thoughts of suicide often feel immobilized. Just calling the hotline is a big step.
Therefore, working with a caller to develop a plan—including encouraging him/her to
call back and report on progress—will have helped the person substantially.
Follow-up calls for attempt survivors would be both welcome and beneficial. Primarily,
helping survivors set “achievable goals” and empowering them to facilitate their own
linkages to services would be most helpful. The crisis line worker could then follow-up
with the caller to see how the call went.
The Lifeline should offer resources dealing with the issue of isolation and opportunities
for callers to become involved in groups or organizations in their communities.
Some “suicide prevention lines” only serve persons who are suicidal. Suicide prevention
lines, such as the Lifeline, should serve not only imminently suicidal persons but also
persons in emotional distress, to help them before they are in danger.
The Lifeline should engage peers (i.e., attempt survivors) to be “mentors” for persons
who have recently attempted suicide, providing understanding, support, and hope.
When people call, they need is warmth and compassion, not someone who is going to
take information quickly and then move to an intervention as quickly as possible. If a
survivor believes the person answering the call is taking a clinical position, they will
likely hang up, stop talking, or not tell the truth about what is going on.
Crisis line workers should be direct, talk about suicide, and not hide it under other things
such as depression.
Full or part-time crisis workers primarily trained and experienced in mental health crisis
intervention staff three of the four Lifeline centers in SE PA, including MCES. Some of these
recommendations suggest that suicide attempt postvention should be added to their skill set.
[15]

RECOMMENDATIONS
1. The county suicide prevention task forces in region or other appropriate stakeholder
should facilitate the formation of a suicide attempters support group in their respective
counties.
2. The county suicide prevention task forces in Chester, Delaware, and Philadelphia
Counties or other appropriate stakeholder should facilitate the formation of an
Alternatives to Suicide Peer-to-Peer Support Group in their respective county.
3. Freestanding psychiatric hospitals and psychiatric units at community hospitals in the
region should initiate voluntary inpatient suicide prevention groups for their inpatients.
4. Freestanding psychiatric hospitals should include information for patients and family
members on dealing with thoughts of suicide and resources for suicide attempt
survivors in the discharge packets required by The Joint Commission.
5. Certified Peer Specialists in the region should receive training to enable them to provide
peer counseling to persons seeking their help with thoughts of suicide or other suicidal
behavior.
6. The county suicide prevention task forces in region or other appropriate stakeholder
should facilitate the expansion of peer-led warm lines to offer support 24/7 to persons
having thoughts of suicide.
7. Create a State Suicide Attempt Survivor web site in Pennsylvania.
Here are examples from other states:
Suicide Prevention: attempt survivors | Mass.gov https://www.mass.gov/info-
details/suicide-prevention-attempt-survivors
FL Department of Children and Families https://www.myflfamilies.com/service-
programs/samh/prevention/suicide-prevention/suicide-attempt-survivors.shtml
Attempt Survivors : Lifeline (suicidepreventionlifeline.org)
https://suicidepreventionlifeline.org/help-yourself/attempt-survivors/
Survivors of Suicide Attempt — South Dakota Suicide Prevention
(sdsuicideprevention.org) https://sdsuicideprevention.org/survivors/survivors-of-
suicide-attempt/
[16]

SELECTED RESOURCES FOR ATTEMPT SURVIVORS
This listing is not exhaustive and is for information only. Inclusion does not imply endorsement.
Support Groups Development
Manual for Support Groups for Suicide Attempt Survivors. Didi Hirsch Mental Health Services,
https://didihirsch.org/wp-
content/uploads/Manual_for_Support_Groups_for_Suicide_Attempt_Survivors.pdf
Support Group Facilitation Guide. Mental Health America.
https://www.mhanational.org/sites/default/files/MHA%20Support%20Group%20Facilitation%2
0Guide%202016.pdf
Self-help Guides
“A Guide for Taking Care of Yourself after your Treatment in the Emergency Department.”
SAMHSA. https://store.samhsa.gov/product/A-Guide-for-Taking-Care-of-Yourself-After-Your-
Treatment-in-the-Emergency-Department/SMA18-4355ENG
A Journey Toward Health and Hope: Your Handbook for Recovery After a Suicide Attempt.
SAMHSA. https://suicidology.org/wp-
content/uploads/2019/06/HandbookForRecoveryAfterAttemptSAMHSA.pdf
"Now Matters Now" Ursala Whiteside. Teaches specific emotion regulation skills.
https://www.youtube.com/watch?v=JV81fmuvqoI&list=UU_NQ14VoXhmabaSZ4RWgKWw
Toolkit for People who have been Impacted by a Suicide Attempt. Mental Health Commission of
Canada, Ottawa, ON. https://www.mentalhealthcommission.ca/sites/default/files/2018-
05/suicide_attempt_toolkit_eng.pdf
Web Sites
“After an Attempt” AFSP. https://afsp.org/after-an-attempt
“After a Suicide Attempt” Beyond Blue. https://www.beyondblue.org.au/the-facts/suicide-
prevention/after-a-suicide-attempt
“Live Through This” Resource supporting and advocating for persons who have made a suicide
attempt and educating others about suicide. https://livethroughthis.org
“With Help Comes Hope: Support for Persons Living with Suicidal Thoughts and Suicide
Attempts.” https://lifelineforattemptsurvivors.org/for-friends-family/7-things-attempt-
survivors-wish-their-families-and-friends-knew/
[ 17 ]

Connections. https://livedexp.academy/ Directory those who have survived attempts can use to
connect with others who have “been there” for support.
“Lived Experience Academy” https://livedexp.academy Educational website to help suicide
attempt survivors after they have gotten through a suicidal crisis,
“A Voice at the Table” http://avoiceatthetable.org/index.html “The national ‘home base’ for
the Family & Friends emotionally impacted by the suicidal crisis of a loved one.”
“Suicide is Different” https://www.suicideisdifferent.org/ A site for “suicide caregivers” who are
“struggling with someone with thoughts of suicide.”
[ 18 ]

SOURCES
The following publications were reviewed in the course of this study. Findings pertinent to the
focus of this study are summarized above.
Bantjes J. 'Don't push me aside, Doctor': Suicide attempters talk about their support
needs, service delivery and suicide prevention in South Africa. Health Psychology Open.
2017 Sep 8;4(2):2055102917726202..
Berardelli I, Forte A, Innamorati M, Imbastaro B, Montalbani M. et al. Clinical Differences
Between Single and Multiple Suicide Attempters, Suicide Ideators, and Non-suicidal
Inpatients. Frontiers of Psychiatry. 2020 Dec 15;11:605140. doi:
10.3389/fpsyt.2020.605140. PMID: 33384631; PMCID: PMC7769945.
Bostwick, J, Pabbati, C, Geske, M, McKean, A. Suicide Attempts as a Risk Factor for
Completed Suicide: Even More Lethal than we Knew. American Journal of Psychiatry 2016
173:11; 1094-1100
Chaudhury, S. Singh, T., Burke, A., Stanley, B., Mann, J, Grunebaum, M., Sublette, M.
Oquendo, M. (2016). Clinical Correlates of Planned and Unplanned Suicide Attempts.
Journal of Nervous and Mental Disease, 204(11), 806–811.
Karen Chesley, Nancy E Loring-McNulty, Process of suicide: perspective of the suicide
attempter, Journal of the American Psychiatric Nurses Association, 9: 2, 2003, 41-45,
Compton M, Thompson N, Kaslow N. Social environment factors associated with suicide
attempt among low-income African Americans: the protective role of family
relationships and social support. Social Psychiatry and Psychiatr Epidemiology. 2005
Mar;40(3):175-85.
Exbrayat S, Coudrot C, Gourdon X, Gay A, Sevos J, Pellet J, Trombert-Paviot B, Massoubre
C. Effect of telephone follow-up on repeated suicide attempt in patients discharged from
an emergency psychiatry department: a controlled study. BMC Psychiatry. 2017 Mar
20;17(1):96.
Hom, M. A., Albury, E. A., Gomez, M. M., Christensen, K., Stanley, I.et al.. (2020). Suicide
attempt survivors’ experiences with mental health care services: A mixed methods
study. Professional Psychology: Research and Practice, 51(2), 172–183.
[ 19 ]

Hom, M., Bauer, B, Stanley, I, Boffa, J, Stage, D, et al. (2020). Suicide attempt survivors’
recommendations for improving mental health treatment for attempt
survivors. Psychological Services. Advance online
publication. https://doi.org/10.1037/ser0000415
Hom, M, Davis, L., & Joiner, T. (2018). Survivors of Suicide Attempts (SOSA) support
group: Preliminary findings from an open-label trial. Psychological Services, 15(3), 289-
297.
García de la Garza Á, Blanco C, Olfson M, Wall MM. Identification of Suicide Attempt
Risk Factors in a National US Survey Using Machine Learning. JAMA
Psychiatry. Published online January 06, 2021. doi:10.1001/jamapsychiatry.2020.4165
Oexle, N., Herrmann, K., Staiger, T., Sheehan, L., Rüsch, N., & Krumm, S. (2019). Stigma
and suicidality among suicide attempt survivors: A qualitative study. Death Studies,
43(6), 381–388.
Mayer, L., Rüsch, N., Frey, L., Nadorff, M., Drapeau, C, Sheehan, L. and Oexle, N. (2020),
Anticipated Suicide Stigma, Secrecy, and Suicidality among Suicide Attempt Survivors.
Suicide and Life Threatening Behavior, 50:706-713.
McGill K, Hackney S, Skehan J. Information needs of people after a suicide attempt: A
thematic analysis. Patient Education and Counseling. 2019 Jun;102(6):1119-1124. doi:
10.1016/j.pec.2019.01.003. Epub 2019 Jan 8. PMID: 30679002.
Olfson M, Blanco C, Wall M, Liu SM, Saha TD, Pickering RP, Grant BF. National Trends in
Suicide Attempts among Adults in the United States. JAMA Psychiatry. 2017 Nov
1;74(11):1095-1103. doi: 10.1001/jamapsychiatry.2017.2582. PMID: 28903161; PMCID:
PMC5710225.
Jessica Rassy, Diane Daneau, Caroline Larue, Elham Rahme, Nancy Low et al.
(2020) Measuring Quality of Care Received by Suicide Attempters in the Emergency
Department, Archives of Suicide Research, DOI: 10.1080/13811118.2020.1793043
Stellrecht, N, Gordon, K, Van Orden, K, et al. Clinical applications of the interpersonal-
psychological theory of attempted and completed suicide. Journal of Clinical Psychology
2006;62:211-222.
Taylor M. Binnix, Carol Rambo, Seth Abrutyn, Anna S. Mueller (2017): The
Dialectics of Stigma, Silence, and Misunderstanding in Suicidality Survival Narratives,
Deviant Behavior, DOI: 10.1080/01639625.2017.1399753
[20 ]

Robert J. Valuck, Anne M. Libby, Tami D. Benton, Dwight L. Evans, A Descriptive Analysis
of 10,000 Suicide Attempters in United States Managed Care Plans,1998–2005. Primary
Psychiatry. 2007;14(11):52-60
Stanley I, Boffa J, Joiner, T. PTSD From a Suicide Attempt: Phenomenological and
Diagnostic Considerations. Psychiatry. 2019 Spring; 82(1):57-71. doi:
10.1080/00332747.2018.1485373. Epub 2018 Sep 5. PMID: 30183554; PMCID:
PMC6401333.
Williams, S, Frey, L., Stage, D, Cerel, J. (2018). Exploring lived experience in gender and
sexual minority suicide attempt survivors. American Journal of Orthopsychiatry, 88(6),
691–700.
[ 21 ]
