1
March 31, 2023
NOTE TO: Medicare Advantage Organizations, Prescription Drug Plan Sponsors, and
Other Interested Parties
Announcement of Calendar Year (CY) 2024 Medicare Advantage (MA) Capitation Rates
and Part C and Part D Payment Policies
In accordance with section 1853(b)(1) of the Social Security Act, we are notifying you of the
annual capitation rate for each Medicare Advantage (MA) payment area for CY 2024 and the
risk and other factors to be used in adjusting such rates.
In response to our request for comments on the Advance Notice of Methodological Changes for
CY 2024 MA Capitation Rates and Part C and Part D Payment Policies (CY 2024 Advance
Notice), published on February 1, 2023, CMS received submissions from professional
organizations, MA and Part D sponsors, advocacy groups, physicians, state Medicaid agencies,
pharmaceutical manufacturers, pharmacy benefit managers, pharmacies, and other interested
persons. The Rate Announcement describes and responds to all of the substantive comments
received.
After considering all comments received, we are finalizing policies in the Announcement of CY
2024 MA Capitation Rates and Part C and Part D Payment Policies (CY 2024 Rate
Announcement) that reflect CMS’ commitment to ensuring that people with Medicare receive
equitable, affordable, high quality, and whole-person care now and in the future, especially the
most vulnerable. The policies in the CY 2024 Rate Announcement are an important step in our
efforts to make sure the MA program meets the health care needs of all beneficiaries while
improving the quality and long-term stability of the Medicare program. The CY 2024 Rate
Announcement finalizes an important transition to an updated risk adjustment model that
implements a set of commonsense, clinically-based technical updates needed to keep MA
payments up-to-date and to improve payment accuracy to MA plans.
Specifically, the updated risk adjustment model is developed using ICD-10 codes to align with
the rest of the health care system, which has been using ICD-10 since 2015. It also incorporates
newer data – the current MA risk adjustment model is calibrated with 2014 diagnosis data and
2015 FFS expenditure data and the new model uses 2018 diagnosis data and 2019 expenditure
data. Finally, the revised model includes clinically-based adjustments to ensure that conditions
included in the model are stable predictors of costs. These adjustments help ensure payments
accurately reflect what it costs to care for beneficiaries and make the model less susceptible to
discretionary coding, which can lead to excess payments to MA plans. This is consistent with
updates we have done in the past where we removed or reclassified codes disproportionately
coded in MA compared to Medicare FFS to avoid wasteful spending.

2
Together, these updates improve the model’s ability to predict the cost of care and ensure MA
risk-adjusted payments are as accurate as possible, which ultimately makes sure MA plans are
paid enough to deliver the benefits that their enrollees are entitled to.
The capitation rate tables for 2024 and supporting data are posted on the CMS website at
https://www.cms.gov/Medicare/Health- Plans/MedicareAdvtgSpecRateStats/Ratebooks-and-
Supporting-Data.html. The statutory component of the regional benchmarks, qualifying counties,
and each county’s applicable percentage are also posted on this section of the CMS website.
Attachment I of the Rate Announcement shows the final estimates of the National Per Capita
MA Growth Percentage for 2024 and the National Medicare Fee-for-Service (FFS) Growth
Percentage for 2024, used to calculate the 2024 capitation rates. As discussed in Attachment I,
the final estimate of the National Per Capita MA Growth Percentage for combined aged and
disabled beneficiaries is 1.60 percent, and the final estimate of the FFS Growth Percentage is
2.45 percent. Attachment II provides a set of tables that summarizes many of the key Medicare
assumptions used in the calculation of the growth percentages.
Section 1853(b)(4) of the Social Security Act requires CMS to release county-specific per capita
FFS expenditure information on an annual basis, beginning with March 1, 2001. In accordance
with this requirement, FFS data for CY 2021 were posted on the above website with the Advance
Notice.
Attachment II details the key assumptions and financial information behind the growth
percentages presented in Attachment I.
Attachment III presents responses to Part C payment-related comments on the CY 2024 Advance
Notice.
Attachment IV presents responses to Part D payment-related comments on the Advance Notice.
Attachment V provides the final Part D benefit parameters and details how they are updated.
Attachment VI presents responses to comments on updates for MA and Part D Star Ratings.
Attachment VII contains economic information for significant provisions in the CY 2024 Rate
Announcement.
Attachment VIII contains the CMS-HCC Risk Adjustment Factor and Predictive Ratio tables.
Key Updates from the Advance Notice
Growth Percentages: Attachment I provides the final estimates of the National Per Capita MA
Growth Percentage and the FFS Growth Percentage, also called growth rates, upon which the
capitation rates are based, and information on deductibles for Medical Savings Accounts. Each
year for the Rate Announcement, CMS updates the growth rates to be based on the most current

3
estimate of per capita costs, based on the available historical program experience and projected
trend assumptions at that time. The growth rates change between proposed and final as CMS
incorporates updated data and assumptions. This year, the change in growth rates from the
Advance Notice to the Rate Announcement is due to several key factors, including: additional
CY 2022 experience data that was lower than previously projected, updated modeling to account
for the effects of COVID-19 and other programmatic and demographic changes, lower morbidity
from excess COVID-related deaths, lower total spending by explicitly modeling the shift of hip
and knee replacements from inpatient to outpatient setting, and updated modeling of the effect of
a greater share of dual beneficiaries enrolling in MA. For more information on the overall change
in growth rates, please see the Fact Sheet released in the Newsroom section of the CMS.gov
website that accompanies this Rate Announcement.
Technical Update to Medical Education Payments in the Non-ESRD USPCC Baseline:
CMS is finalizing the technical update to remove MA-related indirect medical
education and direct graduate medical education costs (described in the CY 2024
Advance Notice) from the historical and projected expenditures supporting the final
estimates (being released in this Rate Announcement) of the non-ESRD FFS USPCCs.
The Secretary has directed the CMS Office of the Actuary (OACT) to phase in this
technical update to the USPCCs over a 3-year period beginning with the CY 2024
ratebook, with 33% of the medical education adjustment applied to the USPCCs in
2024. We expect 67% of the 2025 medical education adjustment to be applied in 2025
and 100% of the 2026 value to be applied in 2026.
Calculation of FFS Costs: The Secretary has directed the CMS Office of the Actuary to adjust
the FFS experience for beneficiaries enrolled in Puerto Rico to reflect the propensity of “zero–
dollar” beneficiaries nationwide.
CMS-Hierarchical Condition Categories (CMS-HCC) Risk Adjustment Model (Non-PACE):
CMS is finalizing the updated risk adjustment model proposed in the CY 2024 Advance
Notice, but will phase it in over 3 years. For CY 2024, risk scores will be calculated as a blend
of 67% of the risk scores calculated with the current model (the 2020 model) and 33% of the
risk scores calculated with the updated model (the 2024 model). For CY 2025, we expect risk
scores to be calculated as a blend of 33% of the risk scores calculated with the 2020 model and
67% of the risk scores calculated with the 2024 model, and for CY 2026, we expect 100% of
the risk scores to be calculated with the 2024 model.
Frailty Adjustment for Fully Integrated Dual Eligible Special Needs Plans (FIDE SNPs): CMS is
finalizing frailty factors that do not include the Consumer Assessment of Healthcare Providers
and Systems (CAHPS) survey weight, which is an adjustment that can be used to account for
potential non-response bias. This weight was proposed to be included in the frailty factor
calculation in the CY 2024 Advance Notice. CMS will implement FIDE SNP frailty factors
consistent with the updated CMS-HCC risk adjustment model being finalized for CY 2024. Also,

4
consistent with CMS’ proposal to blend risk scores for CY 2024 (67% current model and 33%
updated model), a blended frailty score for FIDE SNPs will be compared with PACE frailty
calculated in the same manner to determine whether that FIDE SNP has a similar average level
of frailty as PACE. The final frailty factors for CY 2024 can be found in Section L.
Policies Adopted as Described
As in past years, policies in the Advance Notice that are not modified or retracted in the Rate
Announcement become effective for the upcoming payment year. Clarifications in the Rate
Announcement supersede information in the Advance Notice and prior Rate Announcements
as they apply for payment year 2024.
MA Benchmark, Quality Bonus Payments, and Rebate: We will continue to implement the
methodology, as described in the CY 2024 Advance Notice, used to derive the benchmark
county rates, how the qualifying bonus counties are identified, and the applicability of the Star
Ratings.
Location of Network Areas for Private Fee-for-Service (PFFS) Plans in Plan Year 2025: The list
of network areas for plan year 2025 is available on the CMS website at https://www.cms.gov/
Medicare/Health-Plans/PrivateFeeforServicePlans/NetworkRequirements.html.
Direct Graduate Medical Education (DGME) Carve-out Applied to Average Geographic
Adjustments (AGAs): As in past years, we will continue carving out FFS DGME amounts
from the MA capitation rates. (This is different than the technical update related to medical
education payments on behalf of MA enrollees in the Non-ESRD USPCC baseline discussed
above.)
Organ Acquisition Costs for Kidney Transplants: We will continue carving out Kidney
Acquisition Costs (KAC) from the MA capitation rates.
Indirect Medical Education (IME) Phase Out Applied to AGAs: We will continue phasing out
FFS IME amounts from the MA capitation rates.
MA End Stage Renal Disease (ESRD) Rates: We will continue to set MA ESRD rates on a
state basis.
MA Employer Group Waiver Plans (EGWPs): We will continue to use the payment
methodology as described in the Advance Notice, but with the finalized bid-to-benchmark
ratios for 2024 MA EGWP Payment rates as indicated in the table below. These bid-to-
benchmark ratios are weighted by February 2023 enrollment, including retroactive enrollment

5
adjustments made in March 2023 to the February 2023 enrollment file, due to a system
processing error.
1
Applicable Percentage
Bid to Benchmark Ratio
0.95
78.5%
1
77.2%
1.075
76.6%
1.15
76.8%
CMS-HCC Risk Adjustment Model (PACE): For CY 2024, CMS will continue to use the 2017
CMS-HCC risk adjustment model and associated frailty factors to calculate risk scores for
participants in PACE organizations.
CMS-HCC ESRD Risk Adjustment Models:
• For Non-PACE Organizations: For CY 2024, CMS will continue to use the 2023 CMS-
HCC ESRD risk adjustment models to calculate risk scores for beneficiaries in dialysis,
transplant, and post-graft status.
• For PACE Organizations: For CY 2024, CMS will continue to use the 2019 CMS-HCC
ESRD risk adjustment models to calculate risk scores for participants in PACE
organizations with ESRD.
Frailty Adjustment for PACE Organizations: For CY 2024, CMS will continue to use the frailty
factors associated with the 2017 CMS-HCC model (as displayed in Table II-6 of the CY 2024
Advance Notice) to calculate frailty scores for PACE organizations.
Medicare Advantage Coding Pattern Difference Adjustment: For CY 2024, CMS will continue
to apply the statutory minimum MA coding pattern difference adjustment factor of 5.90 percent.
Final 2024 Normalization Factors:
CMS will finalize the 2024 Normalization Factor methodologies as proposed in the Advance
Notice.
For the three CMS-HCC risk adjustment models with a 2019 or 2020 denominator listed below,
CMS will calculate the normalization factors using a five-year linear slope methodology and
updated average FFS risk scores for 2018 through 2022, but continuing to exclude the 2021 risk
score.
• 2024 CMS-HCC model (for non-PACE organizations), for blended risk score
calculations: 1.015
1
For more information, see the HPMS memorandum dated January 31, 2023 regarding the February 2023 MARx plan payment.

6
• 2023 CMS-HCC ESRD dialysis model (for non-PACE organizations): 1.022
• 2023 CMS-HCC ESRD functioning graft model (for non-PACE organizations): 1.028
For the four CMS-HCC risk adjustment models with a 2015 denominator listed below and the
RxHCC models, CMS will calculate the normalization factors using a five-year linear slope
methodology and historical FFS risk scores (2016 through 2020), without including the 2021 and
2022 risk scores.
• 2020 CMS-HCC model (for non-PACE organizations), for blended risk score
calculations: 1.146
• 2017 CMS-HCC model (for PACE organizations): 1.159
• 2019 CMS-HCC ESRD dialysis model (for PACE organizations): 1.100
• 2019 CMS-HCC ESRD functioning graft model (for PACE organizations): 1.159
• 2023 RxHCC model (for non-PACE organizations): 1.063
• 2020 RxHCC model (for PACE organizations): 1.084
Sources of Diagnoses for Risk Scores calculated with CMS-HCC and CMS-HCC ESRD Risk
Adjustment Models:
• For Non-PACE organizations: CMS will continue the policy adopted in the CY 2023
Rate Announcement to calculate risk scores for payment to MA organizations and certain
demonstrations using only risk adjustment-eligible diagnoses from encounter data and
FFS claims.
• For PACE organizations: CMS will continue using the same method of calculating risk
scores that we have been using since CY 2015, which is to pool risk adjustment-eligible
diagnoses from the following sources to calculate a single risk score (with no weighting):
(1) encounter data, (2) Risk Adjustment Processing System (RAPS) data, and (3) FFS
claims.
RxHCC Risk Adjustment Models:
• For Non-PACE Organizations: For CY 2024, we will continue to use the 2023 RxHCC
risk adjustment model to adjust direct subsidy payments for Part D benefits offered by
stand-alone Prescription Drug Plans (PDPs) and Medicare Advantage-Prescription
Drug Plans (MA-PDs).
• For PACE Organizations: For CY 2024, CMS will continue to use the 2020 RxHCC
risk adjustment model to calculate Part D risk scores.
Source of Diagnoses for Risk Scores calculated with the RxHCC Risk Adjustment Models:

7
• For Non-PACE organizations: CMS will continue the policy adopted in the CY 2023
Rate Announcement to calculate Part D risk scores using only risk adjustment-eligible
diagnoses from encounter data and FFS claims.
• For PACE organizations: CMS will continue using the same method of calculating risk
scores that we have been using since CY 2015, which is to pool risk adjustment-eligible
diagnoses from the following sources to calculate a single risk score (with no weighting):
(1) encounter data, (2) RAPS data, and (3) FFS claims.
Inflation Reduction Act Updates: CMS will implement the changes to the Part D drug benefit
made by the Inflation Reduction Act of 2022 as described in the CY 2024 Advance Notice:
• Cost sharing for covered Part D drugs will be eliminated for beneficiaries in the
catastrophic phase of coverage beginning in CY 2024.
• Beginning in CY 2024, the low-income subsidy program (LIS) under Part D will
increase the income limits for the full LIS benefit from 135 percent of the federal poverty
limit (FPL) to 150 percent of the FPL. Medicare beneficiaries earning between 135
percent and 150 percent of the FPL in CY 2024, who meet the resources requirements
under either sections 1860D-14(a)(3)(D) or (E) of the Act, and who would have been
eligible for the partial low-income premium and cost-sharing subsidies and a reduced
deductible under section 1860D-14(a)(2) of the Act had the IRA not been enacted, will be
eligible for full low-income premium and cost-sharing subsidies and a $0 deductible.
• For CY 2024, the deductible will continue not to apply to any Part D covered insulin
product. Also, in the initial coverage phase and the coverage gap phase, cost sharing must
not exceed the applicable copayment amount, which for CY 2024 is $35 for a month’s
supply of each covered insulin product.
2
• For CY 2024, the deductible will continue not to apply to any adult vaccine
recommended by the Advisory Committee on Immunization Practices (ACIP). Also, the
statute requires these vaccines to be exempt from any co-insurance or other cost sharing,
including cost sharing for vaccine administration and dispensing fees for such products,
when administered in accordance with ACIP’s recommendation, for beneficiaries in the
initial coverage and coverage gap phases.
3
• Beginning in CY 2024, the base beneficiary premium (BBP) growth will be held to no
more than 6 percent by statute. The BBP for Part D in 2024 will be the lesser of the BBP
2
The elimination of the deductible for each Part D covered insulin product and implementation of cost-sharing capped at $35 for
a month’s supply of each Part D covered insulin product has been effective as of January 1, 2023. See HPMS Memorandum,
Contract Year 2023 Program Guidance Related to Inflation Reduction Act Changes to Part D Coverage of Vaccines and Insulin,
September 26, 2022.
3
The elimination of the deductible and cost sharing for any adult vaccine recommended by ACIP has been effective as of
January 1, 2023. See HPMS Memorandum, Contract Year 2023 Program Guidance Related to Inflation Reduction Act Changes
to Part D Coverage of Vaccines and Insulin, September 26, 2022.

8
for 2023 increased by 6 percent or the amount that would otherwise apply under the
original methodology if the IRA were not enacted.
Annual Adjustments to Medicare Part D Benefit Parameters in 2024: We will update the defined
standard benefit deductible amount, initial coverage limit, and out-of-pocket (OOP) threshold, by
multiplying the CY 2023 amounts by the CY 2024 Annual Percentage Increase (API) and
rounding as specified by the statute.
Part D Calendar Year Employer Group Waiver Plans Prospective Reinsurance Amount: We are
maintaining the Part D Calendar Year EGWP prospective reinsurance policy as discussed in the
CY 2024 Advance Notice. The average per member per month (PMPM) actual reinsurance
amount paid to Part D Calendar Year EGWPs for the most recently reconciled payment year,
which for purposes of CY 2024 is CY 2021, was $71.09.
Part D Risk Sharing: We will apply no changes to the current threshold risk percentages for CY
2024.
Retiree Drug Subsidy Amounts: We will use the same methodology as in prior years to update
the cost threshold and cost limit for qualified retiree prescription drug plans.
/ s /
Meena Seshamani, M.D., Ph.D.
Director, Center for Medicare
I, Jennifer Wuggazer Lazio, am a Member of the American Academy of Actuaries. I meet the
Qualification Standards of the American Academy of Actuaries to render the actuarial opinion
contained in this Rate Announcement. My opinion is limited to the following sections of this
Rate Announcement: The growth percentages and United States per capita cost estimates
provided and discussed in Attachments I, II and III; the qualifying county determination,
calculations of Fee-for-Service cost, direct graduate medical education carve-out, kidney
acquisition cost carve-out, IME phase out, MA benchmarks, EGWP rates, and ESRD rates
discussed in Attachment III; the Medicare Part D Benefit Parameters: Annual Adjustments for
Defined Standard Benefit in 2024 described in Attachments IV and V; and the economic
information contained in Attachment VII. As noted in Attachment III, the Secretary has directed
the CMS Office of the Actuary to phase in the MA medical education technical correction to the
USPCCs that are used in determining the growth percentages.
/ s /
Jennifer Wuggazer Lazio, F.S.A., M.A.A.A.
Director
Parts C & D Actuarial Group
Office of the Actuary
9
Attachments
10
2024 RATE ANNOUNCEMENT TABLE OF CONTENTS
Announcement of Calendar Year (CY) 2024 Medicare Advantage (MA) Capitation Rates
and Part C and Part D Payment Policies..............................................................................1
Key Updates from the Advance Notice .....................................................................................2
Policies Adopted as Described...................................................................................................4
Attachment I. Final Estimates of the National Per Capita Growth Percentage and the
National Medicare Fee-for-Service Growth Percentage for Calendar Year 2024.............13
Attachment II. Key Assumptions and Financial Information........................................................15
Attachment III. Responses to Public Comments on Part C Payment Policy.................................28
Section A. General Comments.................................................................................................28
Section B. Estimates of the MA and FFS Growth Percentages for 2024 ................................30
Section C. MA Benchmark, Quality Bonus Payments, and Rebate ........................................44
Section D. Calculation of Fee-for-Service Costs.....................................................................45
Section E. Direct Graduate Medical Education .......................................................................55
Section F. Organ Acquisition Costs for Kidney Transplants...................................................55
Section G. IME Phase Out.......................................................................................................55
Section H. MA ESRD Rates ....................................................................................................55
Section I. MA Employer Group Waiver Plans ........................................................................63
Section J. CMS-HCC Risk Adjustment Model for CY 2024 ..................................................65
Section K. End Stage Renal Disease (ESRD) Risk Adjustment Models for CY 2024 .........115
Section L. Frailty Adjustment for Fully Integrated Dual Eligible Special Needs Plans
(FIDE SNPs) and PACE Organizations .......................................................................116
Section M. Medicare Advantage Coding Pattern Adjustment...............................................120
Section N. Normalization Factors..........................................................................................123
Section O. Sources of Diagnoses for Risk Score Calculation for CY 2024 ..........................127
Attachment IV. Responses to Public Comments on Part D Payment Policy...............................128
Section D. Medicare Part D Benefit Parameters: Annual Adjustments for Defined
Section E. Part D Calendar Year Employer Group Waiver Plans Prospective
Section A. RxHCC Risk Adjustment Model .........................................................................128
Section B. Sources of Diagnoses for Part D Risk Score Calculation for CY 2024 ...............130
Section C. Inflation Reduction Act of 2022 Part D Benefit Design Changes .......................130
Standard Benefit in 2024..............................................................................................131
Reinsurance Amount ....................................................................................................132
Section F. Part D Risk Sharing ..............................................................................................133
Attachment V. Final Updated Part D Benefit Parameters for Defined Standard Benefit, Low-
Income Subsidy, and Retiree Drug Subsidy ....................................................................134
Section A. Annual Percentage Increase in Consumer Price index ........................................137
Section B. Calculation Methodology.....................................................................................137
11
Section C. Annual Percentage Increase in Average Expenditures for Part D Drugs per
Eligible Beneficiary (API) ...........................................................................................139
Section D. Estimated Total Covered Part D Spending at Out-of-Pocket Threshold for
Applicable Beneficiaries ..............................................................................................140
Section E. Retiree Drug Subsidy Amounts............................................................................143
Attachment VI. Updates for Part C and D Star Ratings ..............................................................144
Part C and D Star Ratings and Future Measurement Concepts .............................................144
Reminders for 2024 Star Ratings...........................................................................................144
Measure Updates for 2024 Star Ratings ................................................................................145
Extreme and Uncontrollable Circumstances Policy for the 2024 Star Ratings .....................150
Changes to Existing Star Ratings Measures for the 2023 Measurement Year and Beyond..152
Display Measures...................................................................................................................162
Potential New Measure Concepts and Methodological Enhancements for Future Years .....169
Attachment VII. Economic Information for the CY 2024 Rate Announcement .........................179
Section A. Changes in the Payment Methodology for Medicare Advantage and PACE
for CY 2024..................................................................................................................179
A1. Medicare Advantage and PACE non-ESRD Ratebook ............................................179
A2. Indirect Medical Education (IME) Phase Out...........................................................179
A3. Medicare Advantage and PACE ESRD Ratebooks ..................................................180
A4. CMS-HCC Risk Adjustment Model .........................................................................180
A5. ESRD Risk Adjustment ............................................................................................181
A6. Frailty Adjustment for FIDE SNPs...........................................................................181
A7. MA Coding Pattern Adjustment ...............................................................................181
A8. Normalization............................................................................................................181
Section B. Changes in the Payment Methodology for Medicare Part D for CY 2024 ..........181
B1. Part D Risk Adjustment Model .................................................................................181
B2. Annual Percentage Increase for Part D Parameters ..................................................182
Attachment VIII. CMS-HCC Risk Adjustment Factors & Predictive Ratio Tables....................183
Table VIII-2. 2024 CMS-HCC Model Relative Factors for Aged and Disabled New
Table VIII-3. 2024 CMS-HCC Model Relative Factors for New Enrollees in Chronic
Table VIII-5. Predictive Ratios by Deciles of Predicted Risk (sorted low to high): Non-
Table VIII-6. Predictive Ratios by Deciles of Predicted Risk (sorted low to high): Non-
Table VIII-1. 2024 CMS-HCC Model Relative Factors for Continuing Enrollees...............183
Enrollees.......................................................................................................................193
Condition Special Needs Plans (C-SNPs)....................................................................194
Table VIII-4. 2024 CMS-HCC Model with Disease Hierarchies..........................................195
Dual, Aged (Age >=65) Continuing Enrollee ..............................................................197
Dual, Disabled (Age <65) Continuing Enrollee...........................................................197
12
Table VIII-7. Predictive Ratios by Deciles of Predicted Risk (sorted low to high): Full
Benefit Dual, Aged (Age >=65) Continuing Enrollee .................................................198
Table VIII-8. Predictive Ratios by Deciles of Predicted Risk (sorted low to high): Full
Benefit Dual, Disabled (Age <65) Continuing Enrollee ..............................................198
Table VIII-9. Predictive Ratios by Deciles of Predicted Risk (sorted low to high): Partial
Benefit Dual, Aged (Age >=65) Continuing Enrollee .................................................199
Table VIII-10. Predictive Ratios by Deciles of Predicted Risk (sorted low to high):
Partial Benefit Dual, Disabled (Age <65) Continuing Enrollee...................................199
Table VIII-11. Predictive Ratios by Deciles of Predicted Risk (sorted low to high):
Institutional Continuing Enrollee .................................................................................200

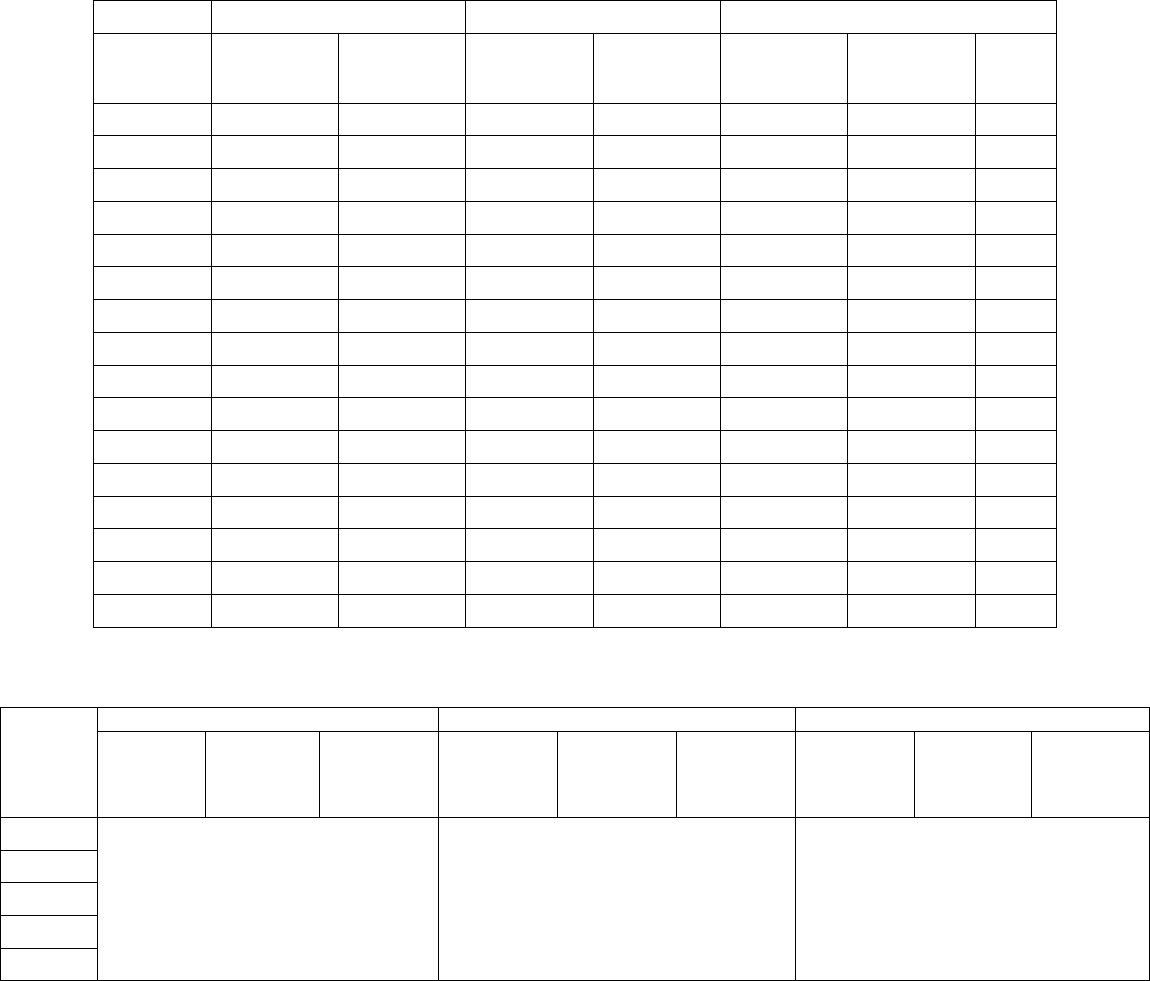
Aged + Disabled
Dialysis–only ESRD
Current projected 2024 FFS USPCC
$1,105.10
$9,544.97
Prior projected 2023 FFS USPCC
1,078.63
9,332.69
Percent change
2.45 %
2.27 %
13
Attachment I. Final Estimates of the National Per Capita Growth Percentage and the
National Medicare Fee-for-Service Growth Percentage for Calendar Year 2024
Table I-1 below shows the National Per Capita MA Growth Percentage (NPCMAGP) for 2024.
An adjustment of -1.77 percent for the combined aged and disabled cohort is included in the
NPCMAGP to account for corrections to prior years’ estimates as required by section
1853(c)(6)(C). The combined aged and disabled change is used in the development of the
ratebook.
Table I-1. Increase in the National Per Capita MA Growth Percentages (NPCMAGP) for
2024
Prior increases
Current increases
NPCMAGP for 2024
with §1853(c)(6)(C)
adjustment
1
2003 to 2023
2003 to 2023
2023 to 2024
2003 to 2024
Aged + Disabled
109.238 %
105.537 %
3.432 %
112.590%
1.60 %
1
Current increases for 2003-2024 divided by the prior increases for 2003-2023.
Table I-2 below provides the change in the FFS United States Per Capita Cost (USPCC), which
was used in the development of the county benchmarks. The percentage change in the FFS
USPCC is shown as the current projected FFS USPCC for 2024 divided by projected FFS
USPCC for 2023 as estimated in the 2023 Rate Announcement released on April 04, 2022.
Table I-2. FFS USPCC Growth Percentage for CY 2024
Table I-3 below shows the monthly actuarial value of the Medicare deductible and coinsurance
for 2023 and 2024. In addition, for 2024, the actuarial value of deductibles and coinsurance is
being shown for non-ESRD only, since MA plan bids for 2024 exclude costs for ESRD
enrollees. These data were furnished by the Office of the Actuary.

14
Table I-3. Monthly Actuarial Value of Medicare Deductible and Coinsurance for 2023 and
2024
2023
2024
Change
2024 non-ESRD
Part A Benefits
$38.18
$36.62
-4.1%
$35.36
Part B Benefits
1
154.95
161.71
4.4
154.36
Total Medicare
193.13
198.33
2.7
189.72
1
Includes the amounts for outpatient psychiatric charges.
Medical Savings Account (MSA) Plans. The maximum deductible for MSA plans for 2024 is
$16,000.

15
Attachment II. Key Assumptions and Financial Information
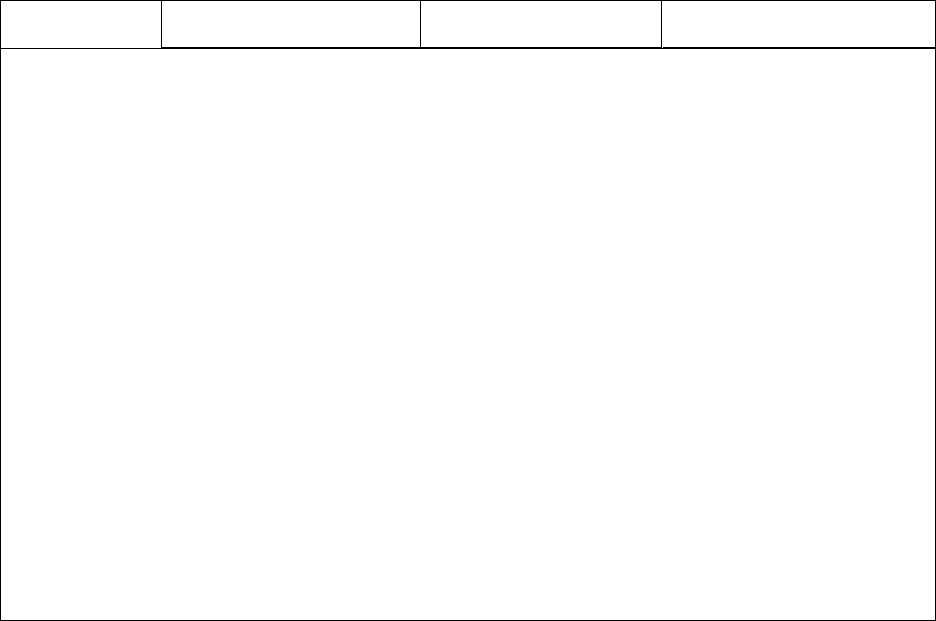
The USPCCs are the basis for the National Per Capita MA Growth Percentage. Below is a table
that compares last year’s estimates of USPCCs with current estimates for 2003 to 2025. In
addition, this table shows the current projections of the USPCCs through 2026. We are also
providing a set of tables that summarize many of the key Medicare assumptions used in the
calculation of the USPCCs. Most of the tables include information for the years 2003 through
2026.
Most of the tables in this attachment present combined aged and disabled non-ESRD data. The
ESRD information presented is for the combined aged-ESRD, disabled-ESRD, and ESRD only.
All of the information provided in this attachment applies to the Medicare Part A and Part B
programs. Caution should be employed in the use of this information. It is based upon
nationwide averages, and local conditions can differ substantially from conditions nationwide.
None of the data presented here pertain to the Medicare Part D prescription drug benefit.
Table II-1. Comparison of Current & Previous Estimates of the Total USPCC – Non-ESRD
Part A
Part B
Part A + Part B
Calendar
year
Current
estimate
Last year’s
estimate
Current
estimate
Last year’s
estimate
Current
estimate
Last year’s
estimate
Ratio
2003
$296.18
$296.18
$247.66
$247.66
$543.84
$543.84
1.000
2004
314.08
314.08
271.06
271.06
585.14
585.14
1.000
2005
334.83
334.83
292.86
292.86
627.69
627.69
1.000
2006
345.30
345.30
313.70
313.70
659.00
659.00
1.000
2007
355.44
355.44
330.68
330.68
686.12
686.12
1.000
2008
371.90
371.90
351.04
351.04
722.94
722.94
1.000
2009
383.91
383.91
367.49
367.35
751.40
751.26
1.000
2010
383.93
383.93
376.34
376.12
760.27
760.05
1.000
2011
387.73
387.73
385.30
385.12
773.03
772.85
1.000
2012
377.37
377.37
391.93
391.76
769.30
769.13
1.000
2013
380.03
380.03
398.72
398.54
778.75
778.57
1.000
2014
370.23
370.23
418.36
418.18
788.59
788.41
1.000
2015
373.86
373.99
435.00
434.95
808.86
808.94
1.000
2016
377.62
377.61
444.28
444.14
821.90
821.75
1.000
2017
383.09
382.91
459.19
459.08
842.28
841.99
1.000
2018
388.12
388.06
489.65
489.43
877.77
877.49
1.000
2019
400.79
400.21
521.89
521.77
922.68
921.98
1.001
2020
403.90
402.19
522.48
522.62
926.38
924.81
1.002

16
Part A
Part B
Part A + Part B
Calendar
year
Current
estimate
Last year’s
estimate
Current
estimate
Last year’s
estimate
Current
estimate
Last year’s
estimate
Ratio
2021
409.38
412.79
569.14
573.53
978.52
986.32
0.992
2022
431.47
447.39
603.83
624.52
1,035.30
1,071.91
0.966
2023
459.23
469.56
658.56
668.36
1,117.79
1,137.92
0.982
2024
464.05
488.33
692.10
707.07
1,156.15
1,195.40
0.967
2025
480.98
509.50
729.01
744.57
1,209.99
1,254.07
0.965
2026
496.85
772.41
1,269.26
Table II-2. Comparison of Current &
Previous
Estimates of the FFS USPCC – Non-ESRD
Part A
Part B
Part A + Part B
Calendar
year
Current
estimate
Last year’s
estimate
Current
estimate
Last year’s
estimate
Current
estimate
Last year’s
estimate
Ratio
2010
$369.60
$371.20
$374.30
$373.99
$743.90
$745.19
0.998
2011
369.45
371.15
383.17
382.92
752.62
754.07
0.998
2012
355.15
356.97
390.70
390.45
745.85
747.42
0.998
2013
361.78
363.75
394.49
394.24
756.27
757.99
0.998
2014
362.07
364.24
409.16
408.89
771.23
773.13
0.998
2015
366.98
369.37
428.06
427.73
795.04
797.10
0.997
2016
369.00
371.57
433.62
433.36
802.62
804.93
0.997
2017
370.97
373.64
448.28
448.06
819.25
821.70
0.997
2018
374.54
377.84
474.15
473.79
848.69
851.63
0.997
2019
380.01
383.05
500.82
500.77
880.83
883.82
0.997
2020
370.93
372.68
473.65
473.99
844.58
846.67
0.998
2021
384.05
388.34
550.73
546.76
934.78
935.10
1.000
2022
398.10
424.46
573.64
598.85
971.74
1,023.31
0.950
2023
428.63
448.03
629.07
630.60
1,057.70
1,078.63
0.981
2024
440.70
465.39
664.40
666.68
1,105.10
1,132.07
0.976
2025
451.09
484.86
698.89
701.28
1,149.98
1,186.14
0.970
2026
459.88
739.42
1,199.30
Table II-3. Comparison of Current & Previous Estimates of the ESRD Dialysis-only FFS
USPCC
Part A
Part B
Part A + Part B
Calendar
year
Current
estimate
Last year’s
estimate
Current
estimate
Last year’s
estimate
Current
estimate
Last year’s
estimate
Ratio
2010
$2,952.75
$2,952.75
$3,881.39
$3,881.39
$6,834.14
$6,834.14
1.000
17
Part A
Part B
Part A + Part B
Calendar
year
Current
estimate
Last year’s
estimate
Current
estimate
Last year’s
estimate
Current
estimate
Last year’s
estimate
Ratio
2011
2,862.38
2,862.38
3,908.01
3,908.01
6,770.39
6,770.39
1.000
2012
2,774.49
2,774.49
3,944.59
3,944.59
6,719.08
6,719.08
1.000
2013
2,794.19
2,794.19
4,088.66
4,088.66
6,882.85
6,882.85
1.000
2014
2,784.52
2,784.52
4,115.70
4,115.70
6,900.22
6,900.22
1.000
2015
2,775.84
2,775.84
4,060.87
4,060.87
6,836.71
6,836.71
1.000
2016
2,895.91
2,895.91
4,081.27
4,081.27
6,977.18
6,977.18
1.000
2017
2,883.27
2,883.27
4,102.66
4,102.66
6,985.93
6,985.93
1.000
2018
2,952.21
2,952.21
4,526.09
4,526.09
7,478.30
7,478.30
1.000
2019
3,040.74
3,040.74
4,614.18
4,614.18
7,654.92
7,654.92
1.000
2020
3,082.55
3,082.55
4,542.51
4,542.51
7,625.06
7,625.06
1.000
2021
3,295.54
3,264.12
4,786.27
5,025.52
8,081.81
8,289.64
0.975
2022
3,395.47
3,646.65
4,863.56
5,279.76
8,259.03
8,926.41
0.925
2023
3,632.99
3,890.68
5,296.62
5,442.01
8,929.61
9,332.69
0.957
2024
3,835.56
4,057.82
5,709.41
5,648.71
9,544.97
9,706.53
0.983
2025
4,084.94
4,242.66
6,778.51
6,426.56
10,863.45
10,669.22
1.018
2026
4,347.69
7,309.00
11,656.69
Table II-4. Basis for ESRD Dialysis-only FFS USPCC Trend
Part A
Part B
Part A & Part B
Calendar
year
All ESRD
cumulative
FFS trend
Adjustment
factor for
dialysis-
only
Adjusted
dialysis-only
cumulative
trend
All ESRD
cumulative
FFS trend
Adjustment
factor for
dialysis-only
Adjusted
dialysis-only
cumulative
trend
All ESRD
cumulative
FFS trend
Adjustment
factor for
dialysis-only
Adjusted
dialysis-only
cumulative
trend
2022 1.02556 1.00465 1.03032 1.01381 1.00230 1.01615 1.01860 1.00327 1.02193
2023 1.09223 1.00931 1.10240 1.10155 1.00461 1.10663 1.09775 1.00652 1.10490
2024 1.14780 1.01400 1.16386 1.18467 1.00693 1.19287 1.16963 1.00976 1.18104
2025 1.21677 1.01871 1.23954 1.40326 1.00925 1.41624 1.32722 1.01278 1.34419
2026 1.28905 1.02344 1.31926 1.50961 1.01157 1.52708 1.41967 1.01597 1.44234
18
Table II-5. Summary of Key Projections
Part A
1
Year
Calendar year
CPI percent change
FY inpatient
PPS update factor
FY Part A total reimbursement
(incurred)
2003 1.4% 3.0%
3.5%
2004 2.1 3.4
8.4
2005 2.7 3.3
8.8
2006 4.1 3.7
5.9
2007 3.3 3.4
5.7
2008 2.3 2.7
7.6
2009 5.8 2.7
6.7
2010 0.0 1.9
3.0
2011 0.0 −0.6
4.5
2012 3.6 −0.1
0.4
2013 1.7 2.8
4.7
2014 1.5 0.9
0.6
2015 1.7 1.4
3.2
2016 0.0 0.9
4.3
2017 0.3 0.2
4.0
2018 2.0 1.8
4.0
2019 2.8 1.9
5.5
2020 1.6 3.1
3.2
2021 1.3
2.9
4.8
2022 5.9
2.5
4.7
2023 8.7
4.3
8.1
2024 3.3
2.8
5.3
2025 1.4
3.1
6.8
2026 2.1 2.9
7.3

19
Part B
2
Physician fee schedule
Calendar year Fees
3
Residual
4
Outpatient hospital
ESRD dialysis update
factor
5
Total
2003
1.4%
4.5%
4.4%
6.8%
2004
3.8
5.9
11.1
9.8
2005
2.1
3.2
10.8
7.0
2006
0.2
4.6
5.1
6.1
2007
-1.4
3.5
8.2
4.3
2008
-0.3
4.0
6.3
4.8
2009
1.4
2.3
5.4
3.9
2010
2.3
2.1
6.6
2.4
2011
0.8
2.3
7.1
2.5%
2.3
2012
-1.2
0.8
7.2
2.1
1.7
2013
-0.1
0.2
7.2
2.3
0.8
2014
0.4
0.6
12.6
2.8
3.4
2015
-0.3
-0.3
7.4
0.0
2.7
2016
-0.4
-0.3
5.2
0.15
1.9
2017
0.1
1.1
7.4
0.55
2.8
2018
0.5
1.1
8.4
0.3
5.7
2019
1.2
2.8
4.9
1.3
5.8
2020
0.2
-11.5
-6.0
1.7
-1.3
2021
4.8
13.1
20.0
1.6
8.7
2022
-1.1
4.0
6.5
1.9
4.9
2023
-0.5
3.4
15.1
3.0
7.4
2024
-1.7
3.5
9.1
1.6
4.8
2025
-1.9
3.0
8.3
2.3
5.6
2026
0.4
2.6
8.3
2.1
5.8
1
Percent change over prior year.
2
Percent change in charges per aged Part B enrollee.
3
Reflects the physician update and legislation affecting physician services—for example, the addition of new preventive services enacted in
1997, 2000, and 2010.
4
Residual factors are factors other than price, including volume of services, intensity of services, and age/sex changes.
5
The ESRD Prospective Payment System was implemented in 2011.

20
Part A
Part B
Calendar year
Aged
Disabled
Aged
Disabled
2003
34.437
5.961
33.038
5.215
2004
34.849
6.283
33.294
5.486
2005
35.257
6.610
33.621
5.776
2006
35.795
6.889
33.975
6.017
2007
36.447
7.167
34.465
6.245
2008
37.378
7.362
35.140
6.438
2009
38.257
7.574
35.832
6.664
2010
39.091
7.832
36.516
6.938
2011
39.950
8.171
37.247
7.254
2012
41.687
8.411
38.546
7.502
2013
43.087
8.629
39.779
7.732
2014
44.533
8.776
41.063
7.894
2015
45.911
8.853
42.311
7.977
2016
47.370
8.862
43.623
7.990
2017
48.893
8.940
44.944
8.007
2018
50.457
8.696
46.310
7.862
2019
52.110
8.531
47.765
7.735
2020
53.684
8.319
49.225
7.573
2021
55.041
8.054
50.513
7.359
2022
56.468
7.703
51.923
7.072
2023
58.030
7.384
53.481
6.785
2024
59.651
7.160
55.023
6.586
2025
61.276
7.093
56.595
6.532
2026
62.914
7.098
58.163
6.537
Non-ESRD Total
Table II-6. Medicare Enrollment Projections (In millions)
Non-ESRD Fee-for-Service
Part A
Part B
Calendar year Aged Disabled Aged Disabled
2003
29.593
5.628
28.097
4.875
2004
29.946 5.931 28.300 5.128
2005
30.014 6.178 28.287 5.339
2006
29.362 6.149 27.459 5.270
2007
28.838 6.225 26.782 5.297
2008
28.613 6.241 26.301 5.311
2009
28.563 6.288 26.071 5.374
2010
28.903 6.455 26.261 5.556
2011
29.210 6.659 26.440 5.736
2012
29.960 6.693 26.744 5.779
2013
30.330 6.691 26.948 5.790
2014
30.603 6.618 27.060 5.732
2015
30.947 6.488 27.274 5.609
2016
31.629 6.378 27.814 5.503
2017
31.916 6.299 27.882 5.361
2018
32.168 5.867 27.926 5.028
2019
32.456 5.467 28.017 4.666
2020
32.221 4.953 27.666 4.202
2021
31.438 4.409 26.816 3.711

21
Part A
Part B
Calendar year
Aged
Disabled
Aged
Disabled
2022
30.802 3.856 26.163 3.224
2023
30.410 3.205 25.703 2.581
2024
30.504 2.652 25.739 2.066
2025
30.941 2.434 26.129 1.864
2026
31.365 2.252 26.482 1.681
ESRD
ESRD - Total
ESRD - Fee-for-Service
Calendar year
Total Part A
Total Part B
Total Part A
Total Part B
2003
0.340
0.331
0.319
0.309
2004
0.353
0.342
0.332
0.321
2005
0.366
0.355
0.344
0.332
2006
0.382
0.370
0.353
0.340
2007
0.396
0.383
0.361
0.347
2008
0.411
0.397
0.367
0.353
2009
0.426
0.412
0.374
0.360
2010
0.442
0.428
0.388
0.373
2011
0.429
0.416
0.371
0.358
2012
0.441
0.429
0.379
0.366
2013
0.454
0.441
0.385
0.372
2014
0.469
0.456
0.390
0.377
2015
0.482
0.468
0.393
0.379
2016
0.496
0.481
0.400
0.384
2017
0.511
0.495
0.404
0.386
2018
0.524
0.507
0.405
0.387
2019
0.537
0.519
0.406
0.387
2020
0.540
0.522
0.396
0.377
2021
0.527
0.511
0.325
0.308
2022
0.509
0.495
0.272
0.258
2023
0.510
0.499
0.245
0.232
2024
0.520
0.508
0.236
0.223
2025
0.531
0.519
0.236
0.223
2026
0.543
0.531
0.237
0.223

22
Table II-7. Part A Projections for non-ESRD (Aged+Disabled)*
Calendar
year
Inpatient
hospital
Home health
agency SNF Managed care
Hospice: Total
re
imbursement
(in millions)
2003
2,594.78
370.63
124.28
457.87
5,733
2004
2,714.57
413.44
133.89
500.73
6,832
2005
2,818.21
450.54
140.87
602.29
8,016
2006
2,755.32
475.07
141.30
766.75
9,368
2007
2,696.33
504.24
143.72
916.90
10,518
2008
2,682.50
536.68
151.00
1,088.37
11,404
2009
2,637.34
551.67
153.86
1,260.14
12,274
2010
2,612.51
571.74
155.18
1,264.21
13,126
2011
2,570.82
623.31
138.31
1,314.41
13,897
2012
2,473.46
541.69
130.82
1,376.07
15,068
2013
2,468.49
540.47
128.47
1,416.56
15,263
2014
2,406.24
534.37
123.89
1,372.06
15,346
2015
2,388.54
530.99
126.08
1,435.16
16,159
2016
2,405.32
504.84
121.44
1,495.94
17,128
2017
2,381.77
484.69
117.35
1,609.39
18,228
2018
2,352.67
465.63
113.87
1,721.35
19,570
2019
2,314.56
444.32
108.47
1,938.76
21,174
2020
2,137.02
450.75
95.42
2,160.64
22,319
2021
2,117.54
421.03
93.28
2,277.75
23,034
2022
2,066.30
440.14
88.44
2,579.80
24,195
2023
2,146.67
417.69
94.63
2,848.53
26,017
2024
2,141.39
403.73
95.65
2,924.58
27,867
2025
2,122.61
434.96
102.09
3,108.74
30,079
2026
2,110.05
449.31
108.55
3,290.82
32,605
*Average reimbursement per enrollee on an incurred basis.

Table II-8. Part B Projections for non-ESRD (Aged+Disabled)*
Calendar year
Physician fee schedule Outpatient hospital Durable medical equipment
2003
$1,226.51
$364.77 $196.96
2004
1,344.01
418.85
195.61
2005
1,397.43
477.65
196.83
2006
1,396.40
497.47
197.78
2007
1,368.35
526.92
195.68
2008
1,367.83
555.09
200.92
2009
1,386.03
587.61
183.61
2010
1,429.74
623.13
183.76
2011
1,459.64
662.97
175.84
2012
1,412.72
697.86
173.70
2013
1,369.64
735.35
152.53
2014
1,351.32
823.34
128.57
2015
1,336.26
876.01
132.77
2016
1,313.75
911.03
120.73
2017
1,293.54
952.81
112.30
2018
1,285.36
1,000.20
127.05
2019
1,300.14
1,018.61
129.06
2020
1,111.11
914.01
123.59
23
2021
1,251.85
1,031.58
121.33
2022
1,208.99
1,014.01
125.84
2023
1,171.90
1,134.23
131.99
2024
1,149.61
1,190.45
133.58
2025
1,139.05
1,266.88
138.33
2026
1,147.58
1,346.13
143.96

Calendar
year
Carrier lab
24
Physician
administered drugs
Other carrier
Intermediary lab
2003
$73.73
$182.58
$147.21
$75.18
2004
78.48
195.20
158.78
2005
80.47
82.71
178.77
184.02
84.16
2006
85.59
185.41
175.66
84.51
2007
90.65
186.97
176.55
84.38
2008
94.50
184.43
182.19
85.78
2009
101.60
196.19
178.46
79.19
2010
103.81
196.41
178.67
80.23
2011
103.85
209.50
179.44
83.31
2012
111.73
209.34
185.17
84.64
2013
111.79
216.91
177.08
81.74
2014
117.60
224.56
173.55
55.45
2015
113.99
252.11
174.94
55.26
2016
100.91
271.45
172.90
56.21
2017
100.65
280.51
177.43
54.99
2018
107.28
304.36
176.15
52.94
2019
108.73
329.41
174.14
50.31
2020
109.18
325.03
166.87
51.77
2021
122.82
340.52
165.36
56.25
2022
112.53
359.41
178.83
52.95
2023
116.31
368.95
184.37
52.89
2024
118.37
389.08
184.22
52.28
2025
128.70
410.19
187.50
54.52
2026
132.58
432.42
191.43
55.03
*Average reimbursement per enrollee on an incurred basis.

25
Calendar year
Other intermediary
Home health agency
Managed care
2003
$113.99
$136.75
$421.40
2004
119.58
156.45
471.37
2005
139.78
179.44
560.31
2006
142.09
202.88
769.94
2007
151.16
232.33
931.18
2008
158.20
252.43
1,104.26
2009
187.44
282.09
1,203.79
2010
193.08
283.25
1,221.29
2011
198.15
254.42
1,276.29
2012
205.08
239.36
1,368.13
2013
194.43
234.07
1,497.49
2014
200.51
227.73
1,703.30
2015
210.37
224.84
1,829.20
2016
214.14
219.09
1,938.69
2017
220.58
208.93
2,096.95
2018
228.23
206.47
2,376.35
2019
236.12
201.48
2,704.42
2020
208.83
187.27
3,062.48
2021
219.92
182.59
3,327.89
2022
214.19
169.26
3,800.44
2023
212.86
177.44
4,341.49
2024
214.10
175.38
4,687.26
2025
221.29
182.19
5,007.97
2026
228.98
194.55
5,384.17
* Average reimbursement per enrollee on an incurred basis.
Table II-9. 2024 Projections by Service Category for non-ESRD (Aged+Disabled)*
Service type
Current
estimate
Last year’s
estimate Ratio
Part A
Inpatient hospital
$2,141.39
$2,303.60
0.930
SNF
403.73
447.80
0.902
Home health agency
95.65
126.49
0.756
Managed care
2,924.58
2,978.53
0.982
Part B
Physician fee schedule
1,149.61
1,170.57
0.982
Outpatient hospital
1,190.45
1,232.65
0.966
Durable medical equipment
133.58
126.40
1.057
Carrier lab
118.37
107.45
1.102
Physician Administered Drugs
389.08
420.58
0.925
Other carrier
184.22
163.46
1.127
Intermediary lab
52.28
44.36
1.179
Other intermediary
214.10
245.56
0.872
Home health agency
175.38
245.69
0.714
Managed care
4,687.26
4,716.27
0.994
* Average reimbursement per enrollee on an incurred basis.

26
Table II-10. Claims Processing Costs as a Fraction of Benefits
Calendar
year
FFS Part A
FFS Part B
Total Part A
Total Part B
2003
0.001849
0.011194
0.001849
0.011194
2004
0.001676
0.010542
0.001676
0.010542
2005
0.001515
0.009540
0.001515
0.009540
2006
0.001245
0.007126
0.001245
0.007126
2007
0.000968
0.006067
0.000968
0.006067
2008
0.000944
0.006414
0.000944
0.006414
2009
0.000844
0.005455
0.000844
0.005455
2010
0.000773
0.005055
0.000773
0.005055
2011
0.000749
0.004396
0.000749
0.004396
2012
0.001008
0.003288
0.001008
0.003288
2013
0.000994
0.002846
0.000994
0.002846
2014
0.001003
0.002884
0.001003
0.002884
2015
0.000952
0.002730
0.000952
0.002730
2016
0.000852
0.002348
0.000852
0.002348
2017
0.000833
0.002111
0.000833
0.002111
2018
0.000836
0.001953
0.000836
0.001953
2019
0.000699
0.001644
0.000699
0.001644
2020
0.000625
0.001536
0.000625
0.001536
2021
0.001038
0.002708
0.000600
0.001399
2022
0.001094
0.002801
0.000582
0.001310
2023
0.001094
0.002801
0.000582
0.001310
2024
0.001094
0.002801
0.000582
0.001310
2025
0.001094
0.002801
0.000582
0.001310
2026
0.001094
0.002801
0.000582
0.001310

27
Approximate Calculation of the USPCC, the National MA Growth Percentage for
Combined (Aged+Disabled) Beneficiaries, and the FFS USPCC (Aged+Disabled)
The following procedure will approximate the actual calculation of the USPCCs from the
underlying assumptions for the contract year for both Part A and Part B.
Part A: The Part A USPCC can be approximated by using the assumptions in the tables titled
“Part A Projections for non-ESRD (Aged+Disabled)” and “Claims Processing Costs as a
Fraction of Benefits.” Information in the “Part A Projections” table is presented on a calendar
year per capita basis. First, add the per capita amounts over all types of providers (excluding
hospice). Next, multiply this amount by 1 plus the loading factor for administrative expenses
from the “Claims Processing Costs” table. Then, divide by 12 to put this amount on a monthly
basis.
Part B: The Part B USPCC can be approximated by using the assumptions in the tables titled
“Part B Projections for non-ESRD (Aged+Disabled)” and “Claims Processing Costs as a
Fraction of Benefits.” Information in the “Part B Projections” table is presented on a calendar
year per capita basis. First, add the per capita amounts over all types of providers. Next, multiply
by 1 plus the loading factor for administrative expenses from the “Claims Processing Costs”
table and then divide by 12 to put this amount on a monthly basis.
The National Per Capita MA Growth Percentage: The National Per Capita MA Growth
Percentage for 2024 (before adjusting for prior years’ over/under estimates) is calculated by
adding the USPCCs for Part A and Part B for 2024 and then dividing by the sum of the current
estimates of the USPCCs for Part A and Part B for 2023.
The FFS USPCC: The tables used to calculate the total USPCC can also be used to approximate
the calculation of the FFS USPCC. The per capita data presented by type of provider in the
projections tables for both Part A and Part B are based on total enrollment. To approximate the
FFS USPCCs, first add the corresponding provider types under Part A and Part B separately. For
the FFS calculations, do not include the managed care provider type. Next, rebase the sum of the
per capita amounts for FFS enrollees, i.e., multiply the sum by total enrollees and divide by FFS
enrollees. (The enrollment tables in this attachment now also include FFS enrollment.) Then,
multiply by 1 plus the loading factor for administrative expenses and divide by 12. The result
will only be approximate because there is an additional adjustment to the FFS data which
accounts for cost plan data which comes through the FFS data system. This cost plan data is in
the total per capita amounts by type of provider, but it is removed for the FFS calculations.

28
Attachment III. Responses to Public Comments on Part C Payment Policy
Section A. General Comments
Comment: CMS received a large number of comments in response to the CY 2024 Advance
Notice, with many supporting the direction of the proposals in the Advance Notice and others
expressing concerns about the impacts of the proposed updates. Commenters who supported the
proposals in the Advance Notice believed that the methods taken to update factors, including the
capitation rates, were sound and that the adjustments, such as those to capitation rates, were
much needed to ensure payment accuracy and preserve the financial integrity of the Medicare
Trust Fund. Commenters also cited overpayments to MA organizations and concerns that
wasteful spending is weakening the Medicare program, placing extra pressure on the Medicare
Trust Fund, and being subsidized by all Medicare beneficiaries via higher Part B premiums. A
number of commenters cited MedPAC’s findings that excess payments to MA organizations will
exceed $27 billion in 2023 and they estimate aggregate excess payments to MA organizations
have totaled nearly $124 billion from 2007 to 2023. One commenter stated that this year’s
projected revenue increase of 1% was an improvement in CMS’ management of the MA
program compared to recent years, such as the projected increase of 8.5% for payment in 2023.
Commenters also emphasized that discretionary coding and perceived ‘gaming’ of codes is a key
part of driving excess payments, and applauded efforts to make the model more accurate and less
susceptible to discretionary coding. Another commenter noted that, while changes to the risk
adjustment model in the proposal and previous policies impacting quality bonuses would tend to
reduce payments to MA organizations, these decreases would be more than offset by an increase
in MA benchmarks driven by increases in diagnostic coding by plans. It was also stated that
though many MA organizations and associations state that if the MA risk score trend is excluded
from the year over year revenue calculation projected payment would decrease, there is no
reason to exclude the risk score growth from the estimate of the year-over-year percentage
change in payment to have an accurate estimate.
The commenters who did not support the proposed changes saw the net effect of the proposals as
cuts to the MA program and urged CMS to maintain stability in the program and not implement
the proposed updates. Many commenters submitted a wide array of suggestions regarding
proposals in the Advance Notice, including the medical education adjustment to the growth
percentages and the updated risk adjustment model. Several commenters stated that the
combined effect of the updates to the growth percentages and the risk adjustment model, as well
as the impact of Star Ratings, would materially affect benchmarks and result in significant
payment reductions. Some commenters stated that the MA risk score trend is not actually part of
the MA payment methodology, and that if the risk score trend were not taken into account the
year-to-year change in payment would be a negative 2.27%, and not a positive 1.03%. These
commenters asserted that a variety of impacts would occur if CMS finalized the proposed
changes including that these proposals would disrupt care, place the health of sicker, lower-

29
income enrollees at risk, and result in increased costs and reduced benefits for MA enrollees.
These commenters highlighted the potential for reduced funding for supplemental benefits and
claimed that these policies would result in reductions in the coverage of dental, hearing, vision,
transportation, and cost sharing for drugs, as well as in hindering the development of complex,
innovative solutions to providing care to Medicare beneficiaries. Further, some commenters
stated that provision of care would suffer and value-based models would also suffer and result in
deteriorating health outcomes.
Response: CMS thanks commenters for their thoughts and input regarding payments made under
the MA program. CMS has a duty to be a steward of the Medicare program. Protecting and
strengthening Medicare for the 65 million Americans who have it now, and all the beneficiaries
in the future, is a key priority for CMS.
Core to this mission is to maintain stability for Medicare beneficiaries in both Medicare FFS and
MA. The policies finalized for CY 2024 are projected to increase average payments to MA
organizations by 3.32% in CY 2024, which will provide continued stability to the MA market
and MA beneficiaries. The policies we are finalizing are commonsense, clinically-based
technical updates that are crucial to ensuring that payments to MA organizations are up to date
and reflect current diagnostic and expenditure trends. These updates ensure accurate payment to
MA organizations and prevent wasteful Medicare spending. These policies were proposed and
finalized using careful analyses, iterative clinical input, and with CMS’ strategic pillars,
especially our commitment to health equity, top of mind.
We respectfully disagree with some commenters’ claims that this reasonable update to payments
in MA is actually a payment cut that will result in increased costs or fewer benefits for
beneficiaries. These comments disregard the payment impact of increases in plan risk scores,
which is an essential element to understanding the full revenue picture for MA organizations.
Well-established historical trend data show that MA organizations continue to increase the
diagnostic codes they submit to CMS for payment, even when models are updated. We have
included assumptions for a reduced MA risk score trend due to the updated model. Moreover, we
note that there have been prior years when the overall expected revenue change was lower than
the 3.32% change projected in this Rate Announcement, and enrollment in MA plans and the
extra payments that MA plans receive from CMS, called rebates, to provide supplemental
benefits that are above and beyond those available in Medicare FFS, consistently increased over
the years, including the years of lower growth in payments. In fact, over the past decade MA has
become a very robust market, where plans compete for enrollment in large part by offering zero
premium plans and generous supplemental benefits. In fact, rebates have more than doubled in
the past five years and rose 20% from 2022 to 2023. The competitiveness of the MA market has
also resulted in beneficiaries having access to on average approximately 61 plans and roughly
60% of enrollees enrolled in zero premium plans.

30
The updates proposed by CMS in the CY 2024 Advance Notice are technical, data-driven, and
clinically-based updates that improve the accuracy of payments to MA organizations, as required
under the statute governing the MA program. We expect MA organizations that are committed to
their MA business to have strong business plans, long term financial strength, and a business
trajectory beyond a single year.
Though plans will have different impacts for the policies finalized, the robust strength and
competitiveness of the market and high level of choice ensure that the 3.32% nationally averaged
update will result in maintained stability.
Section B. Estimates of the MA and FFS Growth Percentages for 2024
Technical Update to USPCC baseline regarding MA-related Medical Education Expenses
Comment: In the CY 2024 Advance Notice, we proposed a technical change to remove medical
education costs (IME and DGME) paid to hospitals by CMS associated with services furnished
to MA enrollees from the historical and projected expenditures supporting the non-ESRD FFS
USPCCs beginning with the CY 2024 ratebook. Several commenters expressed support for the
technical update to remove medical education payments paid by CMS to hospitals associated
with services furnished to MA enrollees from the non-ESRD FFS USPCC estimates, in order to
make payments to MA organizations more appropriate and accurate.
A few commenters expressed appreciation for CMS’ ongoing efforts regarding data evaluations
and improvements regarding the development of per capita FFS costs, and for the transparency
provided by CMS concerning these efforts. One of these commenters encouraged CMS to
continue to take steps to improve the level of transparency related to the methodologies and
analysis supporting the development of the USPCCs and county benchmarks, such as providing
more details in the Advance Notice on how adjustment factors are calculated including data
source/scope and providing further explanation of changes to methodologies.
Response: We appreciate the support and feedback provided by the commenters.
Comment: A large number of commenters expressed concern regarding the full implementation
of the technical update to the USPCC baseline at one time, and recommended that the change
instead be phased in gradually over multiple years to minimize disruption to premiums and
benefits. Several of these commenters noted that CMS has previously phased in benchmark
changes, citing as examples the statutory phase-in of the Affordable Care Act benchmark
changes and the incremental IME phase-out per section 1853(k)(4)(B)(ii) of the Act.
A couple of commenters requested that the technical update be delayed and not finalized for CY
2024. An additional couple of commenters recommended that CMS not proceed with the
proposed technical update to the USPCCs for CY 2024, requesting instead that CMS provide
more information about the methodology for identifying medical education payments and the

31
adjustments to the county benchmarks and USPCCs. One of these commenters believed there
was insufficient time for stakeholders to analyze the potential impacts of the technical proposal.
Response: We appreciate the commenters’ suggestions to phase in or delay the technical update
to the data used for the USPCC baseline. The Secretary has directed the CMS Office of the
Actuary to phase in the technical update to the data used to develop the USPCCs over a 3-year
period beginning with 33% of this adjustment to the medical education costs applied to the
USPCCs in 2024. We expect 67% of the 2025 medical education adjustment to be applied in
2025 and 100% of the 2026 medical education adjustment to be applied in 2026.
Comment: Several commenters noted that there has already been an adjustment to remove
medical education costs from the county-level benchmarks in prior years. Many commenters
requested clarification regarding how the medical education costs being removed from the non-
ESRD FFS growth rate for the technical change is different than the medical education costs
removed from county-level benchmarks as an adjustment to the Average Geographic Adjustment
(AGA). A few of these commenters inquired whether there is any overlap between the amounts
being removed from the USPCC and those being removed at the county level.
Response: The adjustments to the USPCC and AGA pertain to two different groups of Medicare
beneficiaries: the technical update to the non-ESRD FFS USPCC pertains to excluding IME and
DGME costs associated with MA enrollees (paid directly by CMS to hospitals), whereas the
county level adjustment to the AGA pertains to IME and DGME costs associated with FFS
beneficiaries (paid directly by CMS to hospitals) to determine MA capitation rates as required by
section 1853 of the Act. Historically, IME and DGME payments included in the non-ESRD FFS
USPCCs were sourced from historical inpatient cost reports and included amounts paid on behalf
of both FFS and MA enrollees. The cost reports are used as a source for the baseline projections
of the USPCCs since the data contains more detail of the various components of hospital
payments that are projected separately, including capital, bad debt, and ancillary pass through
payments. In contrast, the IME and DGME payments used to calculate the ratebook IME and
DGME carve-out factors applied to the AGAs were sourced from the FFS claims records and, as
such, the adjustment in the county FFS rate calculation has always been limited to the payments
for FFS admissions. The claim records, and not cost reports, are used in the ratebook medical
education exclusion because the claim records include the beneficiary’s county of residence.
Therefore, no corresponding adjustment is required to the IME phase-out and DGME carve-out
adjustments to the AGAs in the county ratebook calculation to remove costs associated with MA
enrollees. As stated on page 11 of the CY 2024 Advance Notice, the technical update has no
impact on the exclusion of medical education costs from the AGAs used to develop the ratebook.
Comment: A few commenters believed that the explanation of the technical change in the
Advance Notice was limited and did not fully explain how the change will affect cost
projections, why the technical change is being implemented at this time, how the impact was
determined, and the statutory basis for the technical change.

32
Many commenters requested more transparency and details regarding the technical update and
the derivation of the impacts. Specific requests from commenters included the following:
• Further explanation/justification of the need for such a large adjustment, such as detailed
support of the magnitude of the impact of the technical update (including the underlying
data and calculations), information regarding how the technical update compares to the
magnitude of historical IME costs that are removed after the application of the AGA to
the rebased FFS per capita costs, and how the technical update is consistent with the
underlying county claim costs.
• Disclosure of whether CMS has performed a reconciliation of the two sources of
IME/DGME information (IME/DGME payments sourced from historical cost reports
used in the non-ESRD FFS USPCC, and IME/DGME payments sourced from the FFS
claims records used to calculate the county ratebook carve-out factors), and if so,
disclosure of the reconciliation results which could demonstrate whether the two sources
are consistent (to ensure that the FFS IME/GME payments included in the non-ESRD
FFS USPCC align with the IME/GME payments being excluded in the MA ratebook).
• Information regarding the methodology for developing the MA-related IME and DGME
adjustment to the USPCC (to better understand how CMS calculated the projected
estimates for medical education costs for 2022 and 2023), and the impact on the CY 2022
and CY 2023 non-ESRD FFS USPCCs.
• Additional information on the methodology for identifying IME and GME payments for
exclusion.
Response: CMS Office of the Actuary believes that the technical update is consistent with
projecting actuarial estimates of FFS per capita costs for the upcoming contract year, as directed
by statute. Section 1853(c)(1)(D) requires an estimate of the per capita costs for services covered
under Parts A and B for individuals who are not enrolled in an MA plan.
In the CY 2024 Advance Notice, we indicated that, for the CY 2024 ratebook development, the
baseline development and modeling supporting the USPCCs had now been updated to separately
identify the historical and projected costs of IME and DGME paid to hospitals by CMS
associated with services furnished to MA enrollees. This update in the modeling stems from
separate projections of IME and DGME by FFS versus MA coverages.
In this Rate Announcement, we are providing the updated impact of the technical update for
IME/DGME on the final estimate of the CY 2024 non-ESRD FFS USPCC (that is being released
in this Rate Announcement); the following is a demonstration of the impact.
As reflected in Table II-2 of this Rate Announcement, the CY 2024 Part B non-ESRD FFS
USPCC is $664.40. This value is unaffected by the technical update for IME/DGME.

33
The following table illustrates the development of the CY 2024 Part A non-ESRD FFS USPCC
both pre- and post-adjustment.
Projection for Contract Year 2024
With full (100%)
implementation of
technical update
(informational)
With 33%
implementation of
technical update
for CY 2024 rates
a. FFS Enrollment (in millions)
33.16
33.16
Reimbursements (in millions)
b. Legacy approach (i.e., including MA medical
education)
$178,800.9
$178,800.9
c. MA medical education
($11,063.6)
($3,651.0)
d. Admin loading
1.0011
1.0011
e. 2024 Part A non-ESRD FFS USPCC (legacy)
e = [(b * d) / a / 12]
$449.89
$449.89
f. 2024 Part A non-ESRD FFS USPCC (with
exclusion of MA medical education)
f = [(b + c) * d) / a / 12]
$422.05
$440.70
g. 2024 Part B non-ESRD FFS USPCC
$664.40
$664.40
h. 2024 non-ESRD FFS USPCC (legacy)
h = e + g
$1,114.29
$1,114.29
i. 2024 non-ESRD FFS USPCC (with exclusion of
MA medical education)
i = f + g
$1,086.45
$1,105.10
j. 2023 non-ESRD FFS USPCC from CY 2023
Rate Announcement
$1,078.63
$1,078.63
k. CY 2024 FFS growth rate (legacy)
k = h/j – 1 (rounded to hundredth of a percent)
3.31%
3.31%
l. CY 2024 FFS growth rate (with exclusion of
MA medical education)
l = i/j – 1 (rounded to hundredth of a percent)
0.73%
2.45%
m. Impact of technical update on CY 2024 FFS
growth rate
m = l - k
-2.58%
-0.86%

34
The resulting impact of the technical update on the MA growth rate (based on the change in the
non-ESRD Total USPCC, which includes both FFS and Part C projections) is -1.27 percent for
full (100%) implementation of the medical education change (provided for informational
purposes) and -0.42% for 33% implementation in CY 2024.
In response to a commenter’s request for a comparison of the two sources of IME/DGME
information (IME/DGME payments sourced from historical cost reports used in the non-ESRD
FFS USPCC, and IME/DGME payments sourced from the FFS claims records used to calculate
the county ratebook carve-out factors), the following table illustrates the CY 2021 incurred IME
and DGME represented in the FFS USPCC calculations and the ratebook carveouts. Note that
the data in the illustrative table below include experience for both non-ESRD and ESRD FFS
beneficiaries.
Item
CY 2021 Incurred Amount (Billions)
IME
DGME
FFS USPCCs in 2024 Rate Announcement
$6.8
$2.4
2024 Ratebook AGA Carveouts
$6.6
$2.2
USPCCs Minus Ratebook
$0.2
$0.2
Note: $0.2 billion impact represents 0.06 percent of 2021 non-ESRD FFS expenditures.
The results show that the aggregate IME and DGME ratebook carveouts are similar to the
corresponding values in the FFS USPCCs. The difference is largely attributed to the different
data sources for the IME and DGME amounts. That is, the USPCC values for IME/DGME
originate from the inpatient cost reports, whereas the ratebook IME/DGME carveouts are
tabulated from the National Claim History claim records.
Comment: A few commenters expressed concern that the technical update would inappropriately
reduce the non-ESRD FFS growth rate to below the expected growth in per enrollee Medicare
costs.
Another commenter expressed concern that the reduction in the growth rate for the technical
update will exacerbate financial challenges facing not-for-profit health plans and negatively
impact value-based care providers, many of whom are paid based on the payments Medicare
Advantage plans receive from CMS.
Response: We appreciate the concerns raised by the commenters. We note that the non-ESRD
FFS USPCCs in prior ratebook years had included both IME and DGME costs paid to hospitals
on behalf of MA enrollees. Consequently, MA benchmarks had included these admission-related
costs even though CMS, and not MA organizations, had been paying these costs associated with
MA enrollees directly to hospitals. That is, the non-ESRD FFS USPCCs in prior ratebook years
had included amounts paid for IME and GME associated with services for MA enrollees, and
those are not costs for Part A and Part B services “for individuals who are not enrolled in an MA
plan” per section 1853(c)(1)(D). Under authority in sections 1853(c)(1)(D) and 1876(a)(4), the

35
Secretary has directed the CMS Office of the Actuary to phase in the technical update to the
USPCCs over a 3-year period beginning with the CY 2024 ratebook, with 33% of this medical
education adjustment applied to the USPCCs in 2024. We expect 67% of the 2025 medical
education adjustment to be applied in 2025 and 100% of the 2026 value to be applied in 2026.
Comment: A commenter expressed opposition to the technical update, and seemed to suggest
that the technical update could be made to the growth rates without affecting the level of MA
rates, and called into question whether the technical update was an improvement to accuracy of
the USPCC calculation.
Another commenter seemed to suggest that CMS could adjust previous years’ USPCCs in a
manner in which plans would not be “penalized” by the technical change.
Response: The technical update results in a more accurate projection of the USPCCs because the
update properly excludes medical education costs associated with inpatient services furnished to
MA enrollees from the costs for furnishing services to FFS beneficiaries; the non-ESRD FFS
USPCC reflect FFS per capita costs and should not be based on the costs associated with services
furnished to MA enrollees. The statute prescribes the general approach per section 1853(c) to
updating the USPCCs and growth rates, and section 1853 of the Act requires that FFS per capita
costs be used in developing MA rates. As discussed in the CY 2024 Advance Notice, the growth
rates are used in the calculation of MA rates, whereby the MA growth rate is used in the
calculation of the applicable amount per section 1853(k) and the non-ESRD FFS USPCC (and
implicitly the corresponding non-ESRD FFS growth rate) is used in the calculation of the
specified amount per section 1853(n). The CY 2024 FFS growth rate is calculated as the current
projection of the 2024 non-ESRD FFS USPCC (that is being released in this Rate
Announcement) divided by the prior projection of the 2023 non-ESRD FFS USPCC (that was
released in the CY 2023 Rate Announcement). The 2024 non-ESRD FFS USPCC is used in the
calculation formula for the CY 2024 MA county rates.
Comment: A couple of commenters noted that the technical update will affect MA benchmarks
in all counties, even though specific counties may have lower levels of medical education
payments.
Another commenter believed that the technical change would have a higher impact on their
urban service market that has a high concentration of academic medical centers than the national
impact that CMS provided in the CY 2024 Advance Notice.
Response: The technical update is a revision to the national monthly per capita cost (USPCC)
that is applied to all counties as follows. The non-ESRD FFS USPCC and the corresponding
non-ESRD FFS growth percentage are used uniformly in the calculation of the specified amount
(in developing the county level FFS per capita cost estimates under Section 1853(n)(2)(A) of the
Act) for all counties. The non-ESRD Total USPCC and the corresponding MA growth
percentage are applied uniformly in the calculation of the applicable amounts (per Section

36
1853(k)(1)) which serve as a cap on the specified amount which affects the subset of counties
where the rates are at the benchmark cap level. We provided the preliminary impacts of the
technical update in the CY 2024 Advance Notice, and we now provide the final impacts of the
technical update in this Rate Announcement, for the FFS growth rate and the MA growth rate so
that stakeholders can understand how the technical update will impact the county rates in their
plan service area.
Consolidated Appropriations Act, 2023 (CAA, 2023)
Comment: A couple of commenters requested confirmation regarding whether the impacts of the
Consolidated Appropriations Act, 2023 (P.L. 117-328) are included or excluded from the growth
rates.
Response: As indicated on page 14 of the CY 2024 Advance Notice, the USPCCs and growth
rates provided in the CY 2024 Advance Notice did not reflect the impact of CAA, 2023, given
the timing constraints of the recently enacted CAA, 2023, and the statutory timeframe for
releasing the Advance Notice. The USPCCs and growth rates provided in the CY 2024 Rate
Announcement do reflect the provisions of CAA, 2023.
Inflation Reduction Act (IRA) Medicare Part B provisions
Comment: A commenter noted that, under the IRA, inflation rebates paid by manufacturers are
remitted to the Medicare Trust Fund for Part B drugs furnished under MA and FFS. The
commenter indicated that this may create complexities in MA reimbursement assumptions. The
commenter encouraged CMS to ensure that the assumptions related to the cost of Part B
Rebatable Drugs in the MA rate setting model accounts for the total cost incurred by MA
organizations (that is, that the MA rates should reflect the Average Sales Price of a prescription
drug prior to the application of the inflationary rebate).
Also, the commenter indicated that MA plans will be required to provide beneficiaries with
reductions in cost-sharing to ensure that their cost-sharing does not exceed 20% of the net price
of the Part B Rebatable Drug after the application of the inflation rebate. The commenter
encouraged CMS to ensure that projected MA costs for Part B Rebatable Drugs should account
for these reductions in cost-sharing for beneficiaries.
Response: For 2024 MA rate development, CMS assumed that prices for Part B drugs will not
materially exceed the inflation-adjusted payment amounts under section 1847A(i) of the Act.
Therefore, no adjustments to projected Part B FFS expenditures to account for inflation rebates
for 2024 were necessary.
Further, section 1853 of the Act sets forth how the MA capitation rates and benchmarks are set
based on FFS per capita costs.

37
Comment: A commenter noted that the USPCCs for 2023 and thereafter reflect cost projections
related to provisions of the IRA, including exclusion from the Part B deductible for insulin when
it is furnished through durable medical equipment and a $35 cap on beneficiary cost sharing for
insulin. The commenter noted that CMS had indicated in the CY 2024 Advance Notice that these
provisions are expected to increase Part B FFS expenditures beginning with 2023, and requested
more detail on the expected increase.
Response: We estimate that the reduced cost sharing for Part B insulin associated with DME
would reduce FFS beneficiary cost sharing by roughly $20-30 million during CY 2024, which
increases Part B FFS expenditures.
COVID-19
Comment: Many commenters urged additional transparency regarding actuarial assumptions
used to calculate the growth rates pertaining to the COVID-19 pandemic. Specific requests from
commenters included the following:
• More specificity about the extent to which coverage requirements related to the COVID-
19 public health emergency are reflected in estimates of costs, utilization, and growth
rates.
• Additional information on the actuarial assumptions that underlie the accounting of
pandemic-related costs in the calculation of the FFS growth percentage.
• Additional information about how revised USPCC projections (for ex., the 2022 USPCC
restatement) are affected by the emerging experience with COVID-19.
• Detailed information as to the complete costs related to the COVID-19 pandemic and
whether these costs are included in the growth percentages, such as: the annual utilization
trend during 2020-2022, long-term costs, costs for beneficiaries dually eligible for
Medicare and Medicaid that were disproportionately impacted by the pandemic, and the
additional hospital, testing, and vaccination costs associated with COVID-19.
• Assumptions related to future COVID-19 vaccine cost and utilization.
• Any difference in how assumptions related to the COVID-19 impact were applied to the
ESRD population relative to the broader Medicare population.
Response: Several policies and legislative provisions were enacted during the public health
emergency that increased spending; notably, the 3-day inpatient stay requirement to receive
Skilled Nursing Facility (SNF) services was waived, payments for inpatient admission related to
COVID-19 were increased by 20 percent, and the use of telehealth was greatly expanded. The
public health emergency is assumed in the actuarial modeling to end in June 2023, when these
effects are assumed to be eliminated. The results would not be materially affected if the actuarial
modeling had instead assumed the public health emergency to end on the announced date of May
11, 2023, as is currently expected.
38
Actual Medicare FFS per capita spending has been consistently below the pre-pandemic
projections throughout the public health emergency. The following table compares combined
non-ESRD and ESRD FFS per capita spending by major provider category with what was
assumed on a pre-pandemic basis for 2020 through the third quarter of 2022 for each category.
The pre-pandemic baseline reflects utilization trend assumptions developed prior to the onset of
the COVID-19 pandemic but has been updated to reflect certain economic factors, such as actual
price updates, and certain demographic factors, such as the share of individuals enrolling in MA
plans by ESRD status.

2021 2022 2023 2024 2025
2026
-2.50% -4.00% -4.40% -4.40% -3.90%
-2.30%
39
Service Type
Per capita: actual / baseline
2020 2021
2022
Inpatient -6.6% -7.1% -8.7%
Outpatient -16.3% -6.5% -8.6%
Skilled Nursing Facility 2.6% -2.3% 3.1%
Home Health -15.3% -17.9% -24.5%
Physician -12.9% -3.1% -2.7%
Note: The data for 2022 include only the first three quarters.
A number of factors have contributed to this lower spending. First, the deaths from COVID-19
have contributed to a lower average morbidity for the surviving population. Using a matched-
cohort approach we studied the impact of COVID-19 deaths on historical and projected
Medicare FFS morbidity. The resulting estimate of excess morbidity on aggregate per capita
Medicare FFS spending is in the following table:
Over the last several years, a greater proportion of those dually eligible for Medicaid and
Medicare have been enrolling in MA which has decreased the average FFS per capita cost for
inpatient hospital, SNF, and home health spending. In addition, the proportion of hip and knee
replacement surgeries performed in the inpatient setting has dropped dramatically during the
public health emergency, causing a greater shift in spending from the inpatient to outpatient
setting than implicitly assumed in prior projection assumptions. These factors account for a
significant portion of the difference between actual costs and the pre-pandemic baseline.
Assumptions for COVID-19 vaccine in CY 2024 are (i) 47 percent of beneficiaries will receive a
COVID shot with 43 percent represented in Medicare FFS claims; (ii) average doses per utilizer:
1.3; and (iii) average cost per dose: $105.
We studied the impact of the COVID-19 pandemic on historical experience separately for non-
ESRD and ESRD FFS beneficiaries. Accordingly, separate COVID-19 related projection factors
were applied to the non-ESRD and ESRD baseline projections.
ESRD growth rate
Comment: A commenter expressed appreciation for improved transparency regarding the
development of ESRD Dialysis-only FFS USPCCs, further stating that the information provided
in the CY 2024 Advance Notice Attachment I was extremely helpful.
Response: We appreciate the support.

40
Comment: A commenter requested that CMS provide additional detail and explanation into the
significant historical restatements of the ESRD Dialysis-only FFS USPCC, in light of significant
and directionally opposite revisions of some of the USPCCs. Several other commenters noted
that the restated CY 2022 ESRD Dialysis-only FFS USPCC had a significant decrease, which
was a larger decrease than the non-ESRD FFS USPCC, and requested additional information on
the driving factors.
Response: The CY 2022 ESRD Dialysis-only FFS USPCC is lower in the CY 2024 Advance
Notice and 2024 Rate Announcement than in the 2023 Rate Announcement due to reflection of
actual incurred experience through 4
th
quarter 2022 in the CY 2024 Advance Notice and CY
2024 Rate Announcement, whereas the CY 2022 ESRD Dialysis-only FFS USPCC in the CY
2023 Rate Announcement was projected based on actual incurred experience through 4
th
quarter
2020.
Comment: A couple of commenters expressed concerns regarding the volatility of the ESRD
growth percentage, particularly in comparison to non-ESRD growth rates, and urged CMS to
provide clarifying details on the change from last year. One of these commenters expressed
concern with the lack of transparency and requested more detailed information about the
methodologies and assumptions used to calculate the ESRD growth percentage.
A couple of commenters requested that CMS publish expenditure trends for beneficiaries with
ESRD by service category, similar to the file currently published for the non-ESRD FFS
USPCCs, for CY 2022 and onward.
A commenter requested that CMS analyze and disclose the volatility in ESRD per capita costs
that may be stemming from the COVID-19 public health emergency, recent inflationary trends,
and the impact of the 21st Century Cures Act that opened the Medicare Advantage benefit to
beneficiaries with ESRD. Another commenter requested that CMS ensure that the ESRD growth
percentage adequately accounts for the increased costs of the COVID-19 pandemic on the ESRD
population.
A couple of commenters believed that the use of CY 2021 as the base year for 2024 USPCC
estimates results in distorted estimates of per capita cost and has a negative effect on Innovation
Center models that use USPCC estimates as a benchmark for payments, and further believed that
CY 2020 data would also be problematic to use due to the pandemic. One of these commenters
urged CMS to review its USPCC estimates in this context and take steps to mitigate the effect of
health care utilization during the pandemic on the ESRD USPCC estimates, particularly any
differential impact on beneficiaries with chronic kidney disease and ESRD.
A few commenters indicated that, with ESRD enrollment increasing, and with the use of a
modified version of the USPCCs serving as the basis for benchmarks under certain Innovation
Center demonstration programs, it is important for stakeholders to receive information on factors
that contribute to the USPCC development to prevent uncertainty and volatility. A couple of

41
commenters suggested that CMS develop policies that would address and limit the volatility in
the ESRD USPCC and the impact of prior year adjustments, such as limiting prior year
adjustments to no more than 3 percent or spreading downward adjustments greater than 3 percent
over multiple years similar to policies adopted for the Medicare FFS program (e.g., SNF, ESRD
PPS).
Response: The ESRD dialysis USPCCs are derived from the total ESRD USPCC baseline, but
are adjusted for recent trend differences between the total ESRD and dialysis ESRD populations.
Thus, the ESRD dialysis USPCCs are projected using a base year USPCC, CY 2021 for the 2024
dialysis ESRD ratebook, trended from 2021 to 2024 using total ESRD growth with an
“adjustment factor for dialysis only.” The utilization and intensity assumptions supporting the
ESRD trends are based on multiple years of historical experience. The applicable trends are
found in the Attachment II table, “Basis for ESRD Dialysis-only FFS USPCC Trend.”
As discussed in past Rate Announcements, we believe it is important to update the FFS per
capita cost estimates using the most current FFS data available at the time those values are
announced and apply repricing adjustments to reflect changes in FFS payment rules. Similar to
prior Rate Announcements, the method for calculating the county-level non-ESRD rates and the
state-level ESRD rates includes AGAs based on a five-year rolling average of historical claims
experience, which provides some measure of stability in the rates.
The published 2022-2024 “Medicare Unit Cost Increases” by service category (available at
https://www.cms.gov/files/document/ffs-trends-2022-2024.pdf) apply to provider payments for
both ESRD and non-ESRD beneficiaries. Starting with the 2024 Rate Announcement posting, we
will add trends for the ESRD Prospective Payment System (ESRD PPS) base rate.
Comment: A commenter acknowledged that the ESRD PPS policies are outside the scope of the
Advance Notice, but a couple of commenters requested that CMS consider the interactions and
downstream effects on MA ESRD rates of payment systems when developing ESRD PPS
policies and processes, including the Transitional Drug Add-on Payment Adjustment (TDAPA)
and Transitional Add-On Payment Adjustment for New and Innovative Equipment and Supplies
(TPNIES) under the ESRD PPS.
Response: We appreciate the feedback. CMS believes the current methodology for calculating
MA ESRD rates account for products that receive the TDAPA or TPNIES under the ESRD PPS.
The CY 2024 ESRD dialysis-only FFS USPCC reflects our best estimate of the national per-
capita cost, including changes to the ESRD PPS bundled payments for variables such as payment
adjustments to the ESRD PPS base rate, including the TDAPA for certain renal dialysis drugs
and biological products and the TPNIES for certain renal dialysis equipment and supplies.

42
Other Comments on USPCCs and Growth Rates
Comment: A commenter noted that the non-ESRD FFS USPCC estimates for prior years in
Table I-4 of the CY 2024 Advance Notice decreased in comparison to the estimates in the CY
2023 Rate Announcement. The commenter requested additional information about the factors
contributing to the revised projections (beyond the technical update that was proposed in the
Advance Notice for medical education payments), particularly for the 2022 USPCC restatement.
Response: The CY 2022 non-ESRD FFS USPCC is lower in the CY 2024 Advance Notice and
CY 2024 Rate Announcement due to reflection of actual incurred experience through 3rd quarter
2022 in the CY 2024 Advance Notice and through 4th quarter 2022 in the CY 2024 Rate
Announcement, whereas the CY 2022 non-ESRD FFS USPCC in the CY 2023 Rate
Announcement was projected based on experience through 3rd quarter 2021. The actual
experience for 2022 is lower than projected in the CY 2023 Rate Announcement.
Comment: Several commenters expressed concern regarding the level of transparency of the
analysis and assumptions used to calculate the growth percentages, and urged additional
transparency. Specific requests from commenters included the following:
• Detailed information about the factors and assumptions used to calculate the growth
percentages, including additional details on utilization changes and unit costs by type of
service.
• More clarity about the extent to which CMS accounted for finalized payment rates for
Medicare FFS inpatient (IPPS) and outpatient (OPPS) systems, including details on
utilization changes and unit costs by type of service; and if not, reasoning as to why these
payment rates were not taken into account.
• More clarity as to the reasons why the 2024 growth rate estimates are markedly lower
than in prior years, beyond the technical change to medical education costs.
• Any analysis, explanation, and methodologies that the agency utilized and relied upon.
Response: We discussed in the CY 2024 Advance Notice the methodology, sources of data,
assumptions, and trends underlying the MA capitation rates at a level of detail consistent with
past practice. In addition to the information provided in the CY 2024 Advance Notice, CMS also
shared information about actuarial assumptions related to growth rates in its Actuarial User
Group call on February 23, 2023. Participants of the call were invited to ask questions about
assumptions supporting the CY 2024 Advance Notice growth rates. This call was widely
attended by stakeholders, and the call’s agenda and materials are available at
https://www.cms.gov/files/document/february-2023-actuarial-user-group-call-agenda.pdf.
In support of the MA ratebook growth rates, CMS has, as required under section 1853(b)(3),
included an explanation of the assumptions and changes in methodology used in the CY 2024
Rate Announcement; see the key economic assumptions underlying the USPCCs included in

43
Attachment II of this Rate Announcement. Consistent with prior years, with this Rate
Announcement we have published additional information regarding trends for the prior five
years and unit cost increases to the contract year at https://www.cms.gov/Medicare/Health-
Plans/MedicareAdvtgSpecRateStats/FFS-Trends.html.
Additionally, the USPCC projections reflect payment levels based on the most recent Medicare
final regulations for fiscal year 2023 or calendar year 2023.
Further, the 2024 growth rates are lower than in recent years primarily due to actual experience
for 2022 is lower than projected in the 2023 Rate Announcement. The 2024 growth rates also
reflect updated modeling to account for the effects of COVID-19 and other programmatic and
demographic changes, lower morbidity from excess COVID-related deaths, lower total spending
by explicitly modeling the shift of hip and knee replacements from inpatient to outpatient setting,
and updated modeling of the effect of a greater share of dual beneficiaries enrolling in MA.
We believe that this information in the CY 2024 Advance Notice and now this Rate
Announcement provides the necessary support for understanding USPCC levels and trends.
Comment: Several commenters expressed concern that the CY 2024 growth rate estimates were
lower than estimates in the 2022 Medicare Trustees Report, while one of these commenters
acknowledged that the calculations are not inherently performed in the same manner.
Many commenters noted that the proposed CY 2024 growth rates were lower than those finalized
in the CY 2023 Rate Announcement. Commenters believed that the proposed 2024 growth rates
did not fully account for the projected growth in costs. Several commenters encouraged CMS to
finalize a strong FFS growth percentage that fully takes into account the rising cost of care due to
inflation and provider reimbursements, and to appropriately reflect the expected increase in
Medicare costs for 2024. Commenters cited published analyses (e.g., Congressional Budget
Office, Bureau of Labor Statistics, Federal Reserve Bank of Dallas) regarding estimates of the
rate of inflation in the health care sector.
A couple of commenters expressed concern that the development of the MA rates may not fully
account for the range of costs that should be included (e.g. large operational costs, inflation,
labor attrition) that health systems are incurring, especially given that the IME/DGME technical
update reduces the non-ESRD FFS growth rate.
A commenter expressed concern that the growth rate applied to PACE rates failed to keep PACE
payment on track with the rate of inflation for medical care and other associated costs, such as
those related to workforce.
Response: The USPCC modeling approach reflects projected increases in Medicare payment rate
update factors. The projected expenditures for some of the Medicare payment systems include
the expectation of inflation including projected market basket increases for inpatient, SNF, home

44
health agency, and outpatient hospital projections and consumer price index (CPI) updates for
durable medical equipment projections.
The growth percentages are based on CMS’ best estimate of historical program experience and
projected trend at the time those values are announced. We continue to consider it best practice
to base the growth rates on the most recent data and assumptions available at the time those
values are announced. Therefore, for each release of the growth rates, CMS updates historical
enrollment and claims, as well as projection factors, based on the most recent data. For example,
the projections supporting the 2024 growth rates are based on actual experience through
December 31, 2022 and reflect provisions of final 2023 FFS payment regulations.
The baseline supporting the USPCCs and growth rates has been revised since the CY 2024
Advance Notice. A key change since the CY 2024 Advance Notice has been the addition of
experience for 4
th
quarter 2022 for the non-ESRD projections. Further, the projection factors
have been revised for the CY 2024 Rate Announcement to reflect lower morbidity stemming
from excess-COVID deaths, explicit modeling of a shift of hip and knee replacements from
inpatient to outpatient setting, and reflection of a greater share of dual eligible beneficiaries
enrolling in MA.
Section C. MA Benchmark, Quality Bonus Payments, and Rebate
Comment: A few commenters expressed concern that the cap on benchmarks imposed by the
Affordable Care Act limits health plans’ ability to improve coverage for enrollees such as adding
supplemental benefits and reducing cost sharing. A couple of these commenters encouraged
CMS to consider the impact of the benchmark cap on the Administration goal to support health
equity. A commenter stated that the benchmark cap undermines the Quality Bonus Payment
(QBP), whereby high-quality MA plans rated 4-Stars or higher will not receive the full QBP due
to the benchmark cap.
Several commenters suggested that we review our options for exercising discretionary authority
to eliminate the cap or to remove quality bonuses from the cap calculation. A couple of these
commenters referred to legal analyses provided to CMS in previous years regarding this issue
that showed that they believed such changes were legally permissible. A couple of these
commenters expressed concern that the cap is inconsistent with Congressional intent, is contrary
to ensuring that seniors receive the highest possible quality of care, and harms beneficiaries by
undermining value-based care and reducing benefits to enrollees in high quality plans.
Response: As we have stated in response to similar comments in prior Rate Announcements,
while we appreciate the commenters’ concerns, we have not identified discretion under Section
1853(n)(4) of the Act to eliminate application of the pre-Patient Protection and Affordable Care
Act (ACA) (Pub. L. 111-148) rate cap or exclude the bonus payment from the cap calculation.

45
Comment: A commenter expressed support for the QBP policies. Another commenter expressed
concerns regarding quality bonuses and rebates, and suggested that MA rebates be phased out.
And another commenter suggested that CMS explore changes to the rebate percentage, such as
reducing the rebate percentage in relation to increasing levels of a plan’s coding of diagnoses for
risk adjustment.
A commenter expressed concern regarding the high proportion of plans receiving quality bonus
payments based on the current star rating system. Another commenter expressed concern about
the proportion of Special Needs Plans (SNPs) that had reduced quality bonus payments resulting
from a drop in star rating under the current star rating system.
Response: We appreciate the feedback submitted by the commenters regarding quality bonus
payments and MA rebates. The statutory requirements regarding quality bonus payments and the
rebates percentages are prescribed in Sections 1853(o) and 1854(b)(1)(C) of the Act,
respectively.
Comment: A commenter supported CMS’ interpretation of Sections 1853(o)(3)(B) and
1853(c)(1)(B) of the Act with regard to Puerto Rico counties that would have had an urban floor
county rate, whereby more counties in Puerto Rico will continue to qualify for a double bonus.
Response: We appreciate the support.
Comment: A commenter suggested that, for dually eligible beneficiaries enrolled in D-SNPs in
Puerto Rico, the Part B premium buy-downs should be considered part of the A/B bid and not
considered a supplemental benefit, since dually eligible beneficiaries in the mainland would have
the Part B premium covered by Medicaid.
Response: Section 1854 of the Act specifies the costs that may be included in the bid submitted
by each MA organization. Per section 1854(a)(6)(A)(ii), the bid must separately address the costs
attributable to provision of benefits under the Medicare FFS program (as defined in section
1852(a)(1)(B), which is benefits under Parts A and B, excluding hospice and the costs of
acquisition of a kidney for transplant), including, for plan year 2020 and subsequent plan years,
the provision of additional telehealth benefits as described in section 1852(m) (that is, the “A/B
bid”) from costs attributable for supplemental benefits and Part D benefits. Payment of the Part B
premium is not a benefit under Medicare Part A or B. CMS does not have discretion under
section 1854(a)(6)(A) to treat the payment of the Part B premium as a benefit under the Medicare
FFS.
Section D. Calculation of Fee-for-Service Costs
Comment: A commenter expressed support for moving to alternative payment models that
include comprehensive prospective payment to sufficiently and sustainably support primary
care’s role in addressing patient’s health related social needs.

46
Response: We appreciate the feedback from the commenter about the scope of CMMI models.
Comment: A commenter expressed support for the repricing refinements applied to the
development of FFS costs, such as reflecting changes in FFS payment rules.
Another commenter expressed support for the AGA methodology, and further suggested that the
CMS-HCC risk adjustment model proposed for CY 2024 should be used for the purpose of
standardizing the AGA factors regardless of the risk model finalized for CY 2024 payment.
Another commenter suggested that CMS adjust county-level benchmarks for states and regions
that are disproportionately affected by risk model revisions.
Response: We appreciate the support and suggestions from the commenters. As in prior years,
the benchmarks will be standardized with the risk scores calculated using the CMS-HCC risk
adjustment model(s) being used for the payment year (in this case CY 2024), including any
blending/phasing-in of the risk adjustment models.
Comment: A couple of commenters urged additional transparency regarding the rebasing
methodology, given the regional variations in pandemic impacts and to ensure accuracy and
stability. A couple of other commenters suggested that CMS release a preliminary estimate of the
impact of rebasing the county rates at the time of the Advance Notice.
Response: We appreciate the request for transparency and believe that we have been responsive
to stakeholders’ interest in understanding and analyzing the rebasing methodology. As noted on
page 25 of the CY 2024 Advance Notice, CMS released the 2021 FFS cost data by county used
for rebasing county rates in the development of the 2024 ratebook. This data is available on the
CMS website at https://www.cms.gov/Medicare/Health-
Plans/MedicareAdvtgSpecRateStats/FFS-Data.html. Due to timing constraints, this data did not
reflect adjustments for Innovation Center models and demonstrations and the Medicare Shared
Savings Program and Advanced Alternative Payment Models, and do not reflect adjustments for
claim repricing for the most current available Medicare FFS payment rules and parameters.
Starting with the CY 2020 Advance Notice, CMS has published with each Advance Notice the
latest FFS cost data by county used in the development of the non-ESRD ratebooks. For the CY
2019 Advance Notice and prior, this FFS cost data was released at the same time as the Rate
Announcement on the CMS webpage at: https://www.cms.gov/Medicare/Health-
Plans/MedicareAdvtgSpecRateStats/FFS-Data. The accelerated release of the FFS experience
allows stakeholders to conduct basic analyses of the impact of recent program experience on the
geographic adjustments supporting the rates.
Comment: A couple of commenters expressed support for the use of five years of FFS
experience to mitigate any annual fluctuations and anomalies in the data.
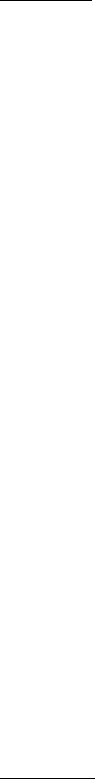
47
Several commenters expressed concerns regarding rebasing the rates for CY 2024 pertaining to
the potential for instability and disparities across counties, such as in Puerto Rico and Florida.
Commenters requested that CMS consider a variety of alternatives, including: an exemption
from rebasing for Puerto Rico given the significant impact of natural disasters and the ongoing
pressures related to COVID-19, not rebasing the MA rates for CY 2024 to improve stability in
the MA program, removal of the 2020 FFS experience from the five-year period used in the
AGA calculation due to the impact of the COVID-19 pandemic, and a suggestion to make an
upward adjustment to the AGA methodology to account for the downward pressure of COVID-
19 impacts on FFS medical costs in 2020 due to suppressed utilization and the impact of natural
disasters which are occurring with greater frequency and severity in recent years.
A couple of commenters encouraged CMS to consider rebasing less frequently (e.g., AGA
update every three years).
Response: We appreciate the feedback submitted by the commenters and appreciate their
concerns about stability in MA county rates.
We note that the impact of rebasing and repricing the historical FFS data had a positive impact
on CY 2024 MA rates in Puerto Rico.
The CY 2020 Advance Notice (page 21) and Rate Announcement (pages 27 and 28) included
discussion and analysis of trends in the FFS data, and concluded that our methodology of using
five years of FFS experience mitigates annual fluctuations and anomalies in the data that may
occur for a variety of reasons. The CY 2023 Advance Notice (pages 24 and 25) also discussed
CMS’ analysis of the trends in the 2020 FFS data that were impacted by the COVID-19
pandemic and affirmed our conclusion that using five years of historical data provides for
stability in the rates despite local or regional events, such as natural or weather-related disasters,
and varying impacts from nationwide events, such as pandemics.
As discussed on page 18 of the CY 2024 Advance Notice, section 1853(c)(1)(D)(ii) of the Act
requires CMS to rebase the county FFS per capita costs periodically, which entails updating the
estimate of each county’s FFS costs using more current FFS claims information. As discussed in
past Rate Announcements, given that MA county rates are based on FFS costs, we believe it is
important to update the FFS per capita cost estimates using the most current FFS data available
and apply repricing adjustments to reflect changes in FFS payment rules. We have stated in
previous Rate Announcements that we anticipate rebasing the rates each year. We have also
previously discussed how the method for calculating the MA county rates includes a five-year
rolling average of historical FFS claims experience, which provides a measure of stability in the
rates. We are finalizing the proposal to rebase the CY 2024 rates.
Comment: A commenter indicated that they expect the impact of rebasing county FFS rates for
CY 2024 to result in a much larger, negative impact in Florida than in most other states, and

48
requested additional detail regarding the drivers of such a negative trend in Florida and the
magnitude of the drivers.
Response: As noted on page 25 of the CY 2024 Advance Notice, CMS released the 2021 FFS
cost data by county used for rebasing county rates in the development of the 2024 ratebook along
with the Advance Notice. This data is available on the CMS website at
https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/FFS-Data.html.
With the Rate Announcement, CMS annually provides a tool and corresponding glossary,
Medicare FFS county 20YY web.xlsm, which provides stakeholders with means to replicate the
FFS rate development. This file is available on the CMS webpage at:
https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Ratebooks-and-
Supporting-Data. Additionally, CMS has included in the CY 2021 and CY 2022 Rate
Announcements a detailed discussion of the rebasing impacts in Florida. Using these two
documents, in conjunction with the spreadsheet Medicare FFS county 20YY web.xlsm,
stakeholders are able to analyze the drivers of changes in FFS per capita costs for specific
counties from one ratebook to another.
Additionally, weighted by September 2022 MA enrollment by county, the overall AGAs
supporting the 2024 non-ESRD, non-PACE rates in Florida changed by less than -0.25 percent
relative to the same measure for the 2023 rates. Therefore, the impact of rebasing for 2024 has a
minimal impact on Florida rates.
Comment: One commenter expressed concern with our proposal to limit our adjustment of the
AGAs for Innovation Center payment and service delivery models to those listed in Table II-B3-
1 of the CY 2024 Advance Notice, and with the proposed exclusion of certain payments under
those models (e.g., care management fees) that are funded through the Innovation Center rather
than the Medicare Part A or B Trust Funds. The commenter inquired about the statutory basis for
excluding these costs from the calculation of MA benchmarks, and was concerned that as APMs
expand in scope that a growing share of FFS spending may be excluded from MA benchmarks.
The commenter expressed concern that the benchmarks may not reflect the cost of providing the
FFS benefit, and that the current approach fails to adequately determine the cost of providing a
benefit to MA enrollees that is comparable to the cost of providing the benefit under FFS.
The commenter is particularly concerned about the exclusion of advance payment of shared
savings and additional reconciliation payments paid to providers under Innovation Center
models. The commenter requested that CMS reconsider policies that exclude Innovation Center
costs and that CMS provide stakeholders with the amounts currently being excluded from the
development of FFS costs.
Response: As explained on pages 29-30 of the CY 2024 Advance Notice, we considered
adjusting the FFS claims experience for care management fees, per-beneficiary-per-month fees,
and/or advance payment of shared savings paid using the Innovation Center appropriation

49
instead of the Medicare Part A or B Trust Funds for other Innovation Center models conducted
in the 2017–2021 period. However, in continuing prior policy, we will not take fees of this type
into account in our adjustments to historical FFS experience when they were not funded under
Medicare Part A or B Trust Funds.
As we discussed on page 20 of the CY 2018 Advance Notice, the fees paid from administrative
accounts authorized by section 1115A of the Act are not from the Parts A and B Trust Funds,
from which Medicare claims are disbursed, so we do not consider those payments to be part of
FFS costs. Per section 1853(c)(1)(D)(i) and (n)(2)(F) of the Act, CMS uses the “adjusted average
per capita cost for the year involved, determined under section 1876(a)(4) [of the Act]” as the
base payment amount for setting MA rates. Section 1876(a)(4) indicates that FFS costs used for
MA rates are based on the estimated amount that would be payable for services covered under
Parts A and B, and types of expenses otherwise reimbursable under Parts A and B (including
administrative costs incurred by organizations described in sections 1816 and 1842). As these
costs described in section 1876(a)(4) of the Act are paid from the Trust Funds, excluding costs
paid from another appropriation is appropriate to determine FFS costs. See also sections 1817
and 1841 of the Act. In addition, section 1853(f) of the Act indicates that payments to MA
organizations shall be made from the Trust Funds “in such proportion as the Secretary
determines reflects the relative weight that benefits under Part A and under Part B represents of
the actuarial value of the total benefits under this title.” Therefore, we will not make an
adjustment to historical FFS claims to account for payments made from the funds appropriated
under section 1115A(f).
Comment: Many commenters requested that we calculate FFS spending using only claims and
utilization data for beneficiaries enrolled in both Part A and Part B (rather than based on such
data for beneficiaries in Part A and/or Part B, as is the practice today), because they believed that
would be a more accurate, reasonable, appropriate, and/or equitable methodology. Several of
these commenters cited MedPAC’s support of benchmarks calculated based on FFS data for
beneficiaries with both Part A and Part B.
Several commenters pointed out that, in order to enroll in an MA plan, beneficiaries are required
to be enrolled in both Part A and Part B, and believe that the benchmark calculations should
align with the population of beneficiaries eligible to enroll in MA plans. One of these
commenters believes the current methodology is inappropriate from an actuarial perspective, as
the current methodology includes beneficiaries who are not eligible to enroll in MA, and stated
that actuarial principles require that an estimate of the benchmark must represent what the MA
enrollee would cost in FFS. Further, the commenter believes the Social Security Act requires that
Part A-only enrollees be excluded from the calculation of county benchmarks to ensure that the
estimate best represents what that enrollee would cost in FFS.
A commenter suggested that the current approach fails to adequately determine the cost of
providing a benefit to MA enrollees that is comparable to the cost of providing the benefit under
50
FFS. Several commenters expressed concern that, as the number of Medicare beneficiaries with
Part A-only grows, MA benchmarks may be distorted as artificially low and fail to reflect the
FFS costs of the population eligible to enroll in Medicare Advantage, which the commenters
believe results in an actuarially inaccurate and inequivalent benchmarks. One commenter noted
that Part A-only enrollment varies by county, whereby certain counties are disproportionately
impacted.
A commenter indicated that the risk adjustment models are calibrated with FFS beneficiaries
enrolled in Part A and Part B, and recommended that risk adjustment and payment rates be based
on the same population.
A few commenters noted that, in a recently released public use file containing information on
geographic variation in Medicare spending, CMS Office of Enterprise Data and Analytics
(OEDA) excluded beneficiaries who were Part A only or Part B only and the document stated the
following regarding per-capita spending for beneficiaries enrolled in Part A only or Part B only:
“Since those beneficiaries are enrolled in only one part of Medicare, per-capita spending for
those beneficiaries cannot be compared directly to spending for beneficiaries that are enrolled in
both Part A and Part B.” A couple of these commenters interpreted this statement and the public
use file methodology to be a “tacit acknowledgement” by CMS that the MA benchmark formula
was incorrect.
A commenter noted that in 2021, CMS had indicated that the agency intended to issue a Request
For Information (RFI) on the topic of revising MA rates to be based on data from beneficiaries
with both Part A and Part B, but no such RFI has been released and the commenter encouraged
CMS to issue an RFI to gather stakeholder input.
A couple of commenters stated that, similar to their belief that the adjustment made to per capita
costs for Medicare beneficiaries who are dually eligible for benefits through the Department of
Veterans Affairs and the Department of Defense (i.e., the VA/DoD adjustment) is needed
because these beneficiaries are not enrolled in MA, a similar adjustment should be made for Part
A-only and Part B-only beneficiaries who are not enrolled in MA (because they are not eligible
to enroll).
Several commenters expressed support for continuing our policy of basing benchmarks in Puerto
Rico on Medicare costs for beneficiaries with both Part A and Part B coverage. A few
commenters requested that we apply a uniform approach in all counties to calculate benchmarks,
pointing to the methodology used by CMS for Puerto Rico rates, to improve payment accuracy
by addressing high MA penetration rates and low FFS Part B enrollment in other areas such as
Hawaii. A couple of commenters suggested that CMS could implement a phased-in approach for
counties with MA penetration over a certain percentage and gradually lower the threshold each
year.

51
A commenter requested that CMS revise the benchmark methodology for counties in Maryland,
to be based on the FFS experience for beneficiaries enrolled in both Part A and Part B similar to
the rate adjustment for Puerto Rico, due to the unique impact of the Total Cost of Care (TCOC)
Model in establishing benchmarks for Maryland. The commenter indicated that Medicare FFS
spending under the TCOC Model is higher than it would otherwise be under typical Medicare
FFS payment rates (e.g., IPPS/OPPS) which results in most Maryland rates being adjusted
downward by a 95% applicable percentage. The commenter indicated that revising the
benchmark methodology as they suggest would incentivize the expansion of MA offerings and
supplemental benefits in Maryland, where MA penetration is currently lower than other areas,
whereby MA plans could then be able to bid further below the benchmarks and offer more
generous supplemental benefits. The commenter noted that CMS has explicitly determined it has
authority to exercise “discretion for the data used to develop the estimate for one geographic
area, based on circumstances unique to that area” for the rates in Puerto Rico and urged CMS to
use this authority to address the unique circumstances present in Maryland to improve equity and
access to care for Maryland beneficiaries.
Response: We refer commenters to the detailed response that we provided in the CY 2020 Rate
Announcement regarding use of FFS data for costs of all Medicare beneficiaries, whereby CMS
concluded that it finds the current ratebook methodology (our longstanding policy of considering
costs of beneficiaries with Part A and/or Part B) to be consistent with the statute at Section
1853(c)(1)(D) of the Act. We continue to believe that it is not necessary to change the
methodology at this time, nor is it required as the statutory language clearly permits CMS to
include Medicare beneficiaries who have Part A only or Part B only. While we recognize that
calculating rates based on data that excludes beneficiaries entitled only to Part A would yield
different results than calculating rates based on our current methodology, that fact alone does not
determine which methodology should be employed.
With respect to Puerto Rico, we have discussed in past Advance Notices and Rate
Announcements that while most Medicare beneficiaries are automatically enrolled in Part B and
must opt out to decline it, beneficiaries in Puerto Rico must take affirmative action to opt in to
Part B coverage. As a result, we believe it is appropriate to adjust the FFS rate calculation for
Puerto Rico used to determine MA rates so that it is based only on the Medicare costs for
beneficiaries with both Part A and Part B.
Further, section 1853(c)(1)(D)(iii) of the Act explicitly requires an adjustment to the estimate of
the FFS per capita cost for individuals dually eligible for benefits through the Department of
Veterans Affairs and the Department of Defense. There is no statutory requirement for excluding
cost data for beneficiaries with coverage for Part A only or Part B only from the information
used to develop the FFS per capita cost estimate.
We appreciate the commenter’s suggestion to revise MA rates in Maryland due to the impact of
the TCOC Model on the FFS experience; however, the statute requires that MA capitation rates

52
be based on FFS per capita costs, not what FFS per capita costs would be under different
(hypothetical) circumstances.
The purpose of the public use file published by OEDA was to “support further analysis” of the
issue of geographic variation in the amount and quality of health care services that Medicare
beneficiaries receive. The statement cited from OEDA’s document (regarding comparing the per-
capita spending of beneficiaries who were Part A only or Part B only with per-capita spending of
beneficiaries enrolled in both Part A and Part B) was noting that beneficiaries enrolled in only
one part of Medicare have different levels of per-capita spending than beneficiaries that are
enrolled in both Part A and Part B. As noted above, while we recognize that calculating rates
based on data that excludes beneficiaries entitled only to Part A would yield different results than
calculating rates based on our current methodology, that fact alone does not determine which
methodology should be employed.
We appreciate the suggestions submitted by commenters, and we will continue to analyze this
issue and consider whether any adjustments to the methodology on this point may be warranted
in future years. For CY 2024 we will continue to calculate FFS spending for the purpose of
establishing MA benchmarks using FFS claims and utilization data for beneficiaries in Part A
and/or Part B.
Comment: The CY 2024 Advance Notice sought public comment on the possibility of adjusting
FFS experience in Puerto Rico to reflect the propensity of zero-dollar beneficiaries nationwide.
Several commenters supported the use of an adjustment to the Puerto Rico MA rates to reflect
the prevalence of zero-dollar beneficiaries nationwide. Commenters believed that such an
adjustment is appropriate because the number of zero claimants in the Puerto Rico FFS
population is a significantly greater proportion of the population relative to the rest of the United
States. One of these commenters stated that the zero-claims adjustment is needed to ensure that
plans in Puerto Rico can maintain benefits for the low-income populations they serve.
Response: The Secretary has directed OACT to adjust the FFS experience for beneficiaries in
Puerto Rico to reflect the propensity of zero-dollar beneficiaries nationwide. For purposes of
making this adjustment, consistent with the Secretary’s instructions, OACT evaluated experience
exclusively for beneficiaries that are enrolled in both Part A and Part B and are not also eligible
for VA coverage.
The updated study analyzed experience for calendar years 2017 through 2021, using the cohort
of FFS beneficiaries enrolled mid-year (i.e., enrolled in both Part A and Part B as of the mid-year
dates used for the study) to approximate the average enrollment for the year. On average, 14.5
percent of Puerto Rico FFS beneficiaries with both Part A and Part B were found to have no
Medicare claim reimbursements per year. This compares to a nationwide, non-territory
proportion of 6.1 percent of FFS beneficiaries without Medicare spending. These results were
applied to the Puerto Rico FFS experience by adjusting the weighting of the enrollment and risk

53
scores for the zero-claim cohort to reflect the nationwide proportion of zero-claim beneficiaries.
The resulting impact was an average increase in the standardized FFS costs in Puerto Rico of 4.4
percent for 2017 through 2021. Accordingly, a 4.4 percent adjustment was applied to the pre-
standardized Puerto Rico FFS rates supporting the CY 2024 ratebook development.
Comment: Many commenters expressed concern regarding the disparity between payment rates
in Puerto Rico and payment rates in the mainland, and urged CMS to explore all potential
options to increase MA benchmark rates in Puerto Rico. One of these commenters encouraged
CMS to work with Congressional leaders and the White House to provide a minimum level of
funding for the MA program in Puerto Rico to improve healthcare infrastructure and quality of
care, and further the goals of health equity. Another commenter urged CMS to take
administrative action to eliminate historic socioeconomic and legal disparities and long-standing
health inequities in federal programs.
A few commenters indicated that the MA rates in Puerto Rico do not adequately cover the
relatively high costs of providing care, and noted that MA plays an important role in addressing
Social Determinants of Health (SDOH) and filling in gaps in the healthcare system in Puerto
Rico. Commenters indicated that the MA program has effectively become a social safety net in
Puerto Rico, in part due to the lack of benefits that would be covered elsewhere (e.g., Part D Low
Income Subsidy).
A commenter recommended that we adjust the MA benchmarks in Puerto Rico to account for the
proportion of dually eligible beneficiaries in the Puerto Rico FFS population.
A few commenters noted that the MA program is critically important in Puerto Rico as the
foundation of Puerto Rico’s healthcare system with high MA penetration, and detailed the
socioeconomic conditions in Puerto Rico, noting the higher proportion of dually eligible
beneficiaries in Puerto Rico whereby plans devote significant resources to addressing health-
related social needs to meet non-clinical needs and to improve health outcomes. A couple of
these commenters indicated that relatively low MA rates in Puerto Rico have contributed to
provider and professional migration from the island, leading to access and quality issues.
Several commenters requested that we consider establishing a minimum AGA of 0.70 for Puerto
Rico. A few commenters noted the level of the standardized benchmarks in Puerto Rico
compared to the national level and other locales over time. A couple of commenters suggested
that a minimum AGA be implemented in a manner that is not budget neutral. One of the
commenters suggested determining a minimum AGA level similar to the geographic adjustment
under the Medicare FFS program or establishing a hold harmless minimum benchmark.
A commenter indicated their belief that a minimum AGA could be implemented by
administrative action and that CMS has the legal authority to establish a minimum AGA. The
commenter indicated that Section 1876(a)(4) does not prescribe one method to be used in
determining the adjusted average per capita cost (AAPCC) for the purposes of setting the MA
54
benchmark for a service area, rather the statute only directs that the Secretary estimates the
AAPCC, giving broad discretion in potential actuarial methods to be used, with a few conditions.
The commenter continued that estimating the AAPCC can be with “actual experience” of FFS
expenditures in a service area, but such expenditure data is only specified to provide “the basis”
of the Secretary’s estimate. The commenter further continued that the Secretary may forgo
“actual experience” of FFS expenditures for an alternate general method, namely an “actuarial
equivalent based on an adequate sample and other information and data.” The commenter
indicated that this broad alternate method confirms the discretion available to the Secretary and
that the AAPCC need not be merely a restatement of actual FFS expenditure experience in a
particular service area. Lastly, the commenter indicated that, whether using “actual experience”
or an “actuarial equivalent” as the basis of estimating AAPCC, the Secretary is not limited to
using expenditure data from the service area for the particular MA benchmark. The commenter
indicated that the statute expressly permits the Secretary to use data from “a geographic area
served by an eligible organization or . . . a similar area.” The commenter indicated that CMS can
select data from a similar geographic area or jurisdiction whose FFS population is expected to be
useful in projecting what the amounts payable to the plan would be for services provided to its
enrollee population in the service area. The commenter continued that it would be reasonable for
the Secretary to look to a “similar area” that is likely to predict with some accuracy what the FFS
expenditures in Puerto Rico would be if its broader population of MA enrollees received care
through FFS. The commenter indicated that a similar jurisdiction would need to be a territory
that is similarly excluded from several federal programs, such as the LIS and SSI, and depends
upon annual appropriations from Congress for Medicaid funding. The commenter continued that
a similar jurisdiction could be an island with the same relatively high costs for utilities and
imported goods and services including national prices for prescription drugs and lab services,
and that a similar jurisdiction would have a high poverty rate, high urbanization, hurricane-
damaged infrastructure. The commenter concluded that the US Virgin Islands (USVI) would
meet these criteria as a similar jurisdiction, such that the AAPCC for Puerto Rico could be
calculated by multiplying the USPCC by the USVI AGA to determine a more accurate estimated
FFS per capita spending in Puerto Rico. The commenter offered that to simplify, the Secretary
could establish a national AGA floor of 0.70 to achieve a similar result. The commenter noted
precedent under the Medicare FFS program for CMS to establish a minimum AGA (e.g., under
the Physician Fee Schedule, ESRD PPS, IPPS).
Further, the commenter noted that, given the very high MA penetration rate in Puerto Rico, the
MA rates in Puerto Rico are based on a relatively small number of FFS beneficiaries. The
commenter provided their recent analysis of FFS data in Puerto Rico which indicated that the
FFS data that is used as the basis for MA rates is not robust and is not representative of MA
enrollees in Puerto Rico, due to the proportion of beneficiaries with zero FFS claims, the
relatively small number of FFS beneficiaries, and the low proportion of dually eligible FFS
beneficiaries in Puerto Rico.

55
Response: We appreciate the concerns and recommendations commenters have raised regarding
Puerto Rico. We will continue to analyze these issues and consider whether any refinements to
the methodology may be warranted in future years. As discussed in the CY 2017 Advance
Notice, the law requires that MA benchmarks be based on a county’s average Medicare FFS per
capita costs, and there is no evidence that FFS costs in Puerto Rico are higher than the costs
observed in the FFS claims data and thus no basis for overhauling Puerto Rico’s MA
benchmarks. Section 1853(c)(1)(D) requires an estimate of the per capita costs for services
covered under Parts A and B for individuals who are not enrolled in an MA plan.
As we stated in the CYs 2017 and 2018 Rate Announcements, we believe that the FFS data in
Puerto Rico is sufficient for establishing accurate MA benchmarks.
In response to a commenter’s suggestion that there is precedent under the Medicare FFS program
(e.g., under the Physician Fee Schedule, ESRD PPS, IPPS) for CMS to establish a minimum
AGA, we note that these examples are based on statutory provisions that are neither applicable to
the MA program nor provide a direct analog to the provisions in section 1853 that determine the
formula for setting MA capitation rates.
Section E. Direct Graduate Medical Education
See Attachment III Section titled “Estimates of the MA and FFS Growth Percentages for 2024.”
Section F. Organ Acquisition Costs for Kidney Transplants
Comment: A commenter expressed support for the continued use of the KAC carve-out
calculation methodology.
Response: We appreciate the support.
Comment: A commenter urged CMS to closely monitor the impact of the KAC carve-out, and
suggested that CMS take steps to limit any large decreases in county benchmarks that may result.
Response: We will continue to monitor the amount of kidney acquisition costs to determine
whether refinements and improvements to the methodology for the carve-out adjustment are
warranted.
Section G. IME Phase Out
See Attachment III Section titled “Estimates of the MA and FFS Growth Percentages for 2024”.
Section H. MA ESRD Rates
Comment: The majority of commenters on this topic expressed concerns that ESRD state rates
are not sufficient to cover the cost of care for beneficiaries with ESRD. The commenters
requested that CMS re-examine the methodology to improve the adequacy, stability, and

56
accuracy of MA ESRD benchmarks and payment given the statutory change that allows
beneficiaries with ESRD to directly enroll in MA plans.
Commenters highlighted the potential consequences of inadequate rates, including higher out-of-
pocket costs, reduced benefits, or limited service areas as a result of the increasing enrollment of
beneficiaries with ESRD in MA plans. A commenter stated the increased costs for beneficiaries
with ESRD could increase cost sharing for all MA beneficiaries. Another commenter expressed
concerns that MA plans may limit access to care or dissuade beneficiaries with ESRD from
choosing an MA plan.
Another commenter suggested that the underlying ESRD PPS reduces reimbursements and leads
to the development of inadequate MA ESRD rates.
Response: CMS appreciates the comments regarding MA ESRD payment adequacy given the
increased enrollment into MA plans by beneficiaries with ESRD. CMS continues to analyze
these issues and consider whether, consistent with the statutory requirements for setting ESRD
rates in section 1853(a)(1)(H) of the Act, any refinements to the methodology may be warranted
in future years to ensure appropriate ESRD payment rates.
In regard to the comment that MA plans might adopt a less attractive service area or benefit
designs due to the enrollment of beneficiaries with ESRD in MA, we note that in accordance
with the beneficiary protections at section 1852(b) of the Act and § 422.110, MA organizations
are prohibited from denying, limiting, or conditioning the coverage or furnishing of benefits to
individuals eligible to enroll in an MA plan based on health status factors. Under its own
responsibilities at section 1852(b), CMS may not approve an MA plan if we determine that the
plan design and its benefits are likely to substantially discourage enrollment by certain MA
eligible individuals with the organization.
CMS will continue to monitor and investigate complaints related to plan coverage to determine if
an MA organization has designed its plan benefits in an impermissible way. If warranted, CMS
may take compliance or enforcement actions against an MA organization for failing to meet any
contract requirements, such as providing adequate access to medically necessary services.
Comment: Commenters appreciated CMS’ analysis to explore recommendations to develop MA
ESRD rates at a smaller geographic level than the state level to address geographic differences in
costs. Commenters, citing the analysis in the CY 2024 Advance Notice, questioned the potential
use of the Core-Based Statistical Areas (CBSAs) in MA ESRD rate setting given the Area
Deprivation Index (ADI) analysis. Specifically, they expressed concerns that reduced payments
for rural and medically underserved areas, relative to urban areas, may have negative impacts on
promoting health equity and supported CMS’ proposal to use statewide ESRD rates for CY
2024. The commenters also requested more information on the CYs 2023 and 2024 analyses,
what the change and impact was on ESRD payment rates in CBSAs with a low ADI compared to

57
a high ADI, and the number of MA beneficiaries with ESRD located in the CBSAs with a low
ADI.
However, given payment adequacy concerns, a majority of commenters maintained that CMS
should continue analyzing policy options to change how CMS calculates ESRD payment rates,
and made suggestions such as: calculating ESRD rates at a smaller geographic level, with some
commenters asking CMS to also consider adjustments to rural and medically underserved areas
to ensure beneficiary access to high-quality MA plan options. Many of these commenters stated
calculating the ESRD payment rates at a sub-state level or on a county-level basis with
adjustments may lessen financial pressures associated with delivering care to beneficiaries with
ESRD and reduce disparities among beneficiaries living in more rural and medically-
underserved areas.
A commenter recommended improving the accuracy of state dialysis rates by reflecting the
geographic distribution of MA dialysis patients. The commenter stated CMS could develop state
rates by aggregating county-level per capita costs for FFS dialysis patients weighted by county-
level MA dialysis patient enrollment, and not re-standardize the MA-weighted state rates to
constrain them to be equal to existing state rates. According to the commenter such a method
would align MA payment rates with per capita FFS costs and pay MA plans more fairly based on
the geographic distribution of MA dialysis patients.
A commenter also stated that Puerto Rico would benefit from the implementation of rate changes
based on the ADI analysis, given that ADIs in Puerto Rico are lower than the mainland. The
commenter recommended CMS implement the ADI adjustment to MA ESRD rates.
Response: We thank the commenters for their support of our analyses of sub-state ESRD rates.
Our analysis of potential changes in ESRD rates by CBSA showed that CBSAs representing the
40 percent of enrollment with the highest ADI measures (high levels of socioeconomic
deprivation), were expected to receive CY 2022 ESRD rates that were an average of 2.13 percent
lower under the CBSA-level approach. We believe our long-standing rate-setting approach is fair
and reasonable and while we will continue our use of statewide MA ESRD rates for CY 2024,
we will consider ways to conduct additional analysis into this issue.
CMS appreciates the recommendation to develop MA ESRD rates at a sub-state level. We agree
with commenters that significant changes to the current methodology should be fully examined
prior to implementation. Proposed changes to the MA ESRD rate methodology must be included
in the Advance Notice and subject to public notice and an opportunity to comment before such
changes are adopted, consistent with section 1853(b) of the Act. Consistent with our authority
under section 1853(a)(1)(H) of the Act, CMS will continue taking into consideration
commenters’ concerns and recommendations.
Comment: Commenters provided additional suggestions for revisions to the ESRD rate setting
methodology. Several commenters stated concerns that the Maximum Out-Of-Pocket (MOOP)

58
limit is a factor contributing to underpayment for beneficiaries with ESRD. Some commenters
believe these higher plan costs resulting from the MOOP as applied to MA beneficiaries with
ESRD will be shifted onto beneficiaries without ESRD through higher premiums for all enrollees
and reduced supplemental benefits. Commenters suggested that CMS update the MA benchmark
to incorporate the difference between FFS Medicare out-of-pocket costs and the MA MOOP to
directly increase payments for beneficiaries with ESRD.
Another commenter requested that CMS examine the possibility of applying the QBP percentage
to ESRD benchmarks. The commenter stated that currently, MA plans do not receive quality
bonus payments for coordinating care for ESRD beneficiaries. The commenter stated that the
statute provides that the quality incentive payment should be applied at the contract or plan level,
indicating that MA ESRD membership should be included when increasing benchmarks for
quality.
Response: While we appreciate the suggestions of commenters, we do not find the suggestions to
revise the ESRD rate-setting methodology to be consistent with our interpretation of section
1853 of the Act. As explained in the CY 2012 Advance Notice and CY 2012 Rate
Announcement, CMS interprets the legislative changes made by the ACA to MA payment to
indicate that all MA payment rates, including the separate rates of payment for ESRD enrollees,
should closely align with FFS Medicare costs.
As provided in section 1853(a)(1)(H) of the Act, CMS establishes separate rates of payment to
MA organizations for ESRD beneficiaries enrolled in MA plans. See also §§ 422.254 and
422.304 through 422.308. The rates used for enrollees in dialysis or transplant status are based
on statewide average FFS Medicare costs for ESRD beneficiaries in dialysis status. For enrollees
with functioning graft status, the MA county benchmark rates are the payment rates. The rates
for those in dialysis, transplant, and functioning graft status are also adjusted using a risk
adjustment methodology that is specific to the health care costs for beneficiaries with ESRD in
dialysis, transplant or functioning graft status.
We understand the concern about potential subsidization of ESRD costs by enrollees without
diagnoses of ESRD, however the data CMS uses to calculate the CY 2024 MOOP limits includes
out-of-pocket expenses from beneficiaries with and without diagnoses of ESRD because the
MOOP limits will apply to enrollees with and without diagnoses of ESRD in CY 2024. This
practice avoids discriminating against beneficiaries with diagnoses of ESRD — or any group of
beneficiaries with a particular high-cost condition or health status — that would result if there
were higher premiums, cost sharing, or MOOP amounts applicable only to those individuals with
a certain chronic condition. Additional detail on how CMS finalized MOOP limits calculations,
including the data used and the percentiles of FFS Medicare data projections that should be used
in those calculations is available in the final rule titled “Medicare Program; Maximum Out-of-

59
Pocket (MOOP) Limits and Service Category Cost Sharing Standards” (CMS-4190-FC4) (87 FR
22290) published April 14, 2022.
4
In regard to the commenter’s recommendation for CMS to add a QBP percentage to MA ESRD
benchmarks, section 1853(o) of the Act is clear that the QBP is applied to the applicable
percentage used to calculate the applicable amount under section 1853(n) of the Act, while
ESRD rates are set pursuant to section 1853(a)(1)(H) of the Act (that is, ESRD rates are not set
under subsection (n)).
Comment: Commenters expressed concerns about the market concentration of dialysis providers.
The small number of organizations in the dialysis market impacts MA organization’s ability to
negotiate reimbursement rates close to FFS Medicare rates for dialysis services. Several
commenters cited a MedPAC analysis indicating that, on average, MA contracts are paying more
than the FFS Medicare rate for dialysis treatments.
A commenter stated financial pressure from an inability to negotiate reasonable reimbursement
rates may cause some MA plans to offset higher dialysis spending by reducing costs for other
services or risk losses on beneficiaries with ESRD. The commenter stated sub-state MA ESRD
rate setting could lessen this financial pressure.
Response: CMS appreciates the feedback provided by commenters regarding this issue. Please
refer to the CY 2021 final rule titled, “Medicare Program; Contract Year 2021 Policy and
Technical Changes to the Medicare Advantage Program, Medicare Prescription Drug Benefit
Program, and Medicare Cost Plan Program” (CMS-4190-F) (85 FR 33796), which appeared in
the Federal Register on June 2, 2020, which addresses concerns regarding dialysis provider
concentration, network adequacy requirements, and the challenges MA organizations face in
negotiating reasonable reimbursement for dialysis services.
5
We also note that CMS is prohibited from requiring MA organizations to use particular price
structures for payment to their contracted providers. (See section 1854(a)(6)(B)(iii) of the Act
and § 422.256(a)(2).) In accordance with the beneficiary protections under section 1852(b) and
at § 422.112(a), CMS expects that MA plans will continue to ensure that their plan designs allow
for adequate access to covered services.
CMS appreciates the recommendation to develop MA ESRD rates at a sub-state level. We do not
believe that adopting sub-state MA ESRD rates will fully address the commenters concerns. We
believe our long-standing rate-setting approach is fair and reasonable and while we will continue
4
Refer to CMS’ Medicare Program; Maximum Out-of-Pocket (MOOP) Limits and Service Category Cost Sharing Standards
Final Rule.
5
Refer to CMS’ Medicare Program; Contract Year 2021 Policy and Technical Changes to the Medicare Advantage Program,
Medicare Prescription Drug Benefit Program, and Medicare Cost Plan Program Final Rule.

60
our use of statewide MA ESRD rates for CY 2024, we will consider ways to conduct additional
analysis into this issue.
Comment: Several commenters encouraged CMS to leverage Innovation Center authority and
value-based models to achieve greater stability in MA ESRD payments. A commenter
encouraged the Innovation Center to limit the impact of the negative trend factor on the ESRD
Seamless Care Organizations (ESCOs) in the Comprehensive ESRD Care model. Another
commenter suggested that CMS provide MA plans with the option to participate in the
Innovation Center’s kidney demonstration models.
Commenters also encouraged CMS to explore ways to modernize the Medicare conditions for
coverage and revise the definition of “dialysis facility” to provide beneficiaries with ESRD the
choice to receive care in their preferred home or in-center dialysis setting, when clinically
appropriate.
Several commenters encouraged CMS to expand the ESRD Chronic Condition-Special Needs
Plans (C-SNP) to include beneficiaries with chronic kidney disease (CKD) to slow CKD
progression.
Response: CMS notes that potential demonstrations and modernizing ESRD regulations are
outside the scope of this document.
In the CY 2024 proposed rule titled, “Medicare Program; Contract Year 2024 Policy and
Technical Changes to the Medicare Advantage Program, Medicare Prescription Drug Benefit
Program, Medicare Cost Plan Program, Medicare Parts A, B, C, and D Overpayment Provisions
of the Affordable Care Act and Programs of All-Inclusive Care for the Elderly; Health
Information Technology Standards and Implementation Specifications” (CMS-4201-P) (87 FR
79452), CMS has proposed to revise the C-SNP category named “End Stage Renal Disease
(ESRD) requiring dialysis” to be “Chronic kidney disease (CKD)” with the following conditions:
CKD requiring dialysis/ESRD, and CKD not requiring dialysis.
6
CMS proposed that this
particular change would not be implemented for CY 2024 in order to give CMS time to collect
data and information related to the structuring of the proposed CKD C-SNP plan bid. CMS will
provide additional bid pricing information to MA organizations if this proposal is finalized.
Comment: Commenters expressed concerns that the MA ESRD benchmarks underrepresent the
actual costs of care for ESRD beneficiaries in Puerto Rico. A commenter stated that an
insufficient number of ESRD beneficiaries remain in FFS Medicare in Puerto Rico to predict the
costs of the MA ESRD population. The commenter asked CMS to verify what percentage of the
Medicare ESRD population in Puerto Rico remain in FFS Medicare. The commenter also asked
6
Refer to CMS’ Medicare Program; Contract Year 2024 Policy and Technical Changes to the Medicare Advantage Program,
Medicare Prescription Drug Benefit Program, Medicare Cost Plan Program, Medicare Parts A, B, C, and D Overpayment
Provisions of the Affordable Care Act and Programs of All-Inclusive Care for the Elderly; Health Information Technology
Standards and Implementation Specifications Proposed Rule.

61
if CMS has established a cut-off percentage, below which FFS experience could no longer
accurately predict MA ESRD costs.
Response: CMS appreciates the concerns and suggestions that commenters have raised regarding
ESRD rates in Puerto Rico. As CMS stated in the CY 2018 Rate Announcement, CMS believes
that the FFS data in Puerto Rico is sufficient for establishing accurate MA rates and is consistent
with the statutory requirements that MA capitation rates be based on FFS costs. CMS will
continue to analyze these issues and consider whether, consistent with the statutory requirements
for setting ESRD rates in section 1853(a)(1)(H) of the Act, any refinements to the methodology
may be warranted in future years.
There is a total of 113,000 member months of Puerto Rico dialysis experience for 2017-2021
supporting the development of the 2024 dialysis ESRD rates. We believe that this level of
experience is adequate for setting ESRD dialysis payment rates in Puerto Rico.
Comment: A commenter recommended CMS make changes to the BPT so that the ESRD
subsidy falls under Medicare-covered benefits instead of under Mandatory Supplemental
benefits. The commenter encouraged CMS to make the ESRD and non-ESRD service categories
consistent, merge the ESRD and MA BPT format in the near term, and eliminate the ESRD BPT
filing in the long-term.
Response: We appreciate the suggestions submitted by the commenter related to the BPT.
Section 1853(a)(1)(H) of the Act authorizes CMS to establish “separate rates of payment” with
respect to beneficiaries with ESRD enrolled in MA plans and does not require that a competitive
bidding methodology be used for CMS capitation payments for ESRD enrollees. In setting such
separate rates, CMS has established an approach for paying MA organizations for enrollees with
ESRD that directly use the rates, rather than bids. As such, the ESRD rates are intended to be the
base rate for enrollees with ESRD, and these costs cannot be paid under the rates used in the bids
to determine payment for non-ESRD beneficiaries. Therefore, the ESRD subsidy that is
permitted in plan bids for non-ESRD beneficiaries will remain as a mandatory supplemental
benefit. MA plans (with the exception of ESRD C-SNPs) do not bid on ESRD beneficiaries. At
this time, CMS does not find it necessary to require that MA plans submit a separate A/B bid for
beneficiaries with ESRD. Regarding the commenters request that CMS eliminate the ESRD BPT
filing requirement, CMS notes that MA plans are not required to submit ESRD BPTs (with the
exception of ESRD C-SNPs).
Comment: A commenter suggested that the underlying ESRD PPS reduces reimbursements and
leads to the development of inadequate MA ESRD rates. As noted in similar comments from
prior years, the commenter reiterated the concern that MA ESRD rates are suppressed largely by
policies that inappropriately reduce reimbursement under the ESRD PPS. The commenter cited
examples such as the outlier payment pool and case-mix adjusters that they believe have resulted

62
in inadequate payments from ESRD PPS reimbursement that flow into the MA rate setting
process. The commenter encouraged CMS to explore policy redesigns under the ESRD PPS.
Response: CMS appreciates the feedback provided by commenters regarding the ESRD PPS and
its relationship to the development of the MA ESRD rates. Section 1853(a)(1)(H) of the Act
authorizes CMS to establish “separate rates of payment” with respect to beneficiaries with ESRD
enrolled in MA organizations. Under CMS’ authority under section 1853(a)(1)(H), and in
keeping with CMS’ interpretation of the ACA to more closely align MA payment rates with FFS
costs, the MA ESRD state rates are based on FFS costs. CMS encourages commenters to review
and respond to ESRD PPS rulemaking for the Medicare FFS program.
Comment: Some commenters urged CMS to ensure that reimbursement for new and innovative
treatments are incorporated in the MA ESRD rates in a timelier fashion. The commenters stated
that because MA ESRD rates are calculated using historical cost data, the timing may not align
with when new products will receive the Transitional Drug Add-on Payment Adjustment
(TDAPA) and the Transitional Add-on Payment Adjustment for New and Innovative Equipment
and Supplies (TPNIES) through the FFS ESRD PPS. A commenter stated MA beneficiaries have
reported difficulties obtaining access to new and innovative products. The commenters
recommended CMS develop an alternative payment mechanism for new innovative technologies
to improve access to these treatments for MA beneficiaries with ESRD.
A commenter recommended CMS pay ESRD facilities directly for the TDAPA and TPNIES
payment adjustments during the two-year payment period for MA beneficiaries, and then adjust
MA rates to account for additional FFS payment amounts once products are fully bundled.
Response: CMS appreciates the commenters’ feedback regarding adequately funding new and
innovative products for beneficiaries with ESRD. CMS believes the current methodology for
calculating MA ESRD rates accounts for payment adjustments to the ESRD PPS base rate,
including the TDAPA for certain renal dialysis drugs and biological products and the TPNIES
for certain renal dialysis equipment and supplies under the ESRD PPS. We also note that the
TPNIES and the TDAPA for certain drugs are two-year add-on payment adjustments with no
subsequent modification to the base rate. Only the TDAPA for drugs in new ESRD PPS
functional categories may result in a base rate modification. The CY 2024 dialysis-only ESRD
USPCC reflects our best estimate of the national per-capita cost, including changes to the ESRD
PPS bundled payments for variables such as payment adjustments to the ESRD PPS base rate,
including the TDAPA and TPNIES.
CMS will continue to monitor and investigate complaints related to beneficiary challenges
obtaining access to new and innovative products to determine if an MA organization has
designed its plan benefits in an impermissible way.

63
Section I. MA Employer Group Waiver Plans
Comment: Some commenters expressed their support for EGWPs. Commenters stated EGWPs
are an important healthcare option for many Medicare beneficiaries and the employers who have
chosen to support them in retirement. These commenters believe that EGWPs represent a
successful public-private partnership that enables businesses to give recent retirees the option to
choose a plan that provides quality care, lower premiums, and supplemental benefits. A
commenter stated EGWPs act as critical partners in providing retirees with comprehensive
Medicare benefits with enhanced value-based benefits at a lower premium than FFS Medicare.
Response: We appreciate the support.
Comment: Some commenters expressed appreciation for the inclusion of the preliminary bid-to-
benchmark ratios for EGWPs in the Advance Notice to facilitate more accurate benefit and
premium information for employers and beneficiaries.
Response: We appreciate the support.
Comment: Many commenters recommended CMS exclude negative margin plans from the
calculation of estimated bid-to-benchmark ratios for EGWPs to avoid undermining the
availability of supplemental benefits to improve health equity.
Response: As we noted in the CY 2023 Rate Announcement, we do not believe that there is a
reasonable rationale to exclude these plans because the ratios are intended to be representative of
the market. Negative margin plans are included in the non-EGWP market as well, so the bids of
such plans are included when the bid-to-benchmark ratios are developed. CMS does adjust for
factors which would otherwise result in significant differences between the EGWP and non-
EGWP market. More specifically, while the majority of plans in the EGWP market are PPO
plans, the non-EGWP market is predominantly HMO plans. EGWP individual market bid-to-
benchmark ratios are calculated separately for HMO and PPO plan types by quartile. Unlike the
HMO/PPO difference between EGWP and non-EGWP plans, there is no data to suggest that a
similar difference exists between EGWP and non-EGWP plans regarding negative margin plans
upon which CMS can judge the reasonableness of adjusting the bid-to-benchmark ratios to
account for negative margin plans.
Comment: A commenter suggested that to reduce the number of PBPs submitted, CMS should
establish a process using segment ID to facilitate additional flexibility with Part B buy-downs.
Response: As described in recent past Advance Notices and Rate Announcements, when an MA
organization submits an individual market MA plan bid to CMS, the MA organization is
permitted to use MA rebates to buy down a portion of the Part B premiums for its enrollees in
each PBP by identifying the buydown amount in the BPT as its use of the beneficiary rebate. We
then retain that rebate amount specified by the MA organization in each PBP and coordinate

64
directly with the Social Security Administration (SSA) to ensure that each beneficiary’s Part B
premium is appropriately calculated and takes into account the buy-down amount. Implementing
the bidding waiver as described in the Advance Notice facilitates the communication of this
information throughout CMS systems by maintaining an operational structure that is similar to
the one that exists for individual market MA plans. For this reason, we decline to make the
recommended changes, but we appreciate the commenter’s thoughts on this issue and will
continue to analyze and explore suggestions for refinements to this policy in the future.
Comment: Commenters expressed concerns that the published preliminary bid-to-benchmark
ratios are lagging inflation and lower than expected and expressed concerns that the preliminary
bid-to-benchmark ratios and risk model changes may increase costs for employers who utilize
EGWPs and result in increased premiums or reduced benefits for beneficiaries. Many requested
additional details about how the ratios were calculated.
Response: Please see CYs 2020, 2021, 2022, and 2023 Advance Notices for additional details on
the calculation of bid-to-benchmark ratios; responses to comments on those detailed explanations
are provided in the applicable Rate Announcement. CMS is publishing updated bid-to-
benchmark ratios in this CY 2024 Rate Announcement, using the methodology detailed in the
CY 2024 Advance Notice. CMS published preliminary bid-to-benchmark ratios for the first time
in the CY 2023 Advance Notice as a result of feedback from the industry on the CY 2022 bid
cycle. MA organizations indicated that having this information early provides valuable
information in their negotiations with employer/union groups to create more accurate benefit and
premium quotes for their employer/union groups. Commenters that requested additional details
on how the bid-to-benchmark ratios were calculated did not provide further information on
which details CMS could expand upon.
Comment: A commenter requested that CMS provide updated EGWP ratios based on February
enrollment data before the release of the Rate Announcement.
Response: We appreciate this recommendation. For this CY 2024 Rate Announcement, MA
EGWP ratios are based on February enrollment.
Comment: A commenter suggested adjusting current rate setting to capture differences in the use
of HMO and PPO plans between the EGWP and non-EGWP markets. The commenter believes it
would be more accurate for CMS to segment the benchmark calculation by HMO and PPO
products and adjust the bid-to-benchmark ratio for the differing products accordingly.
Response: We appreciate this suggestion; however, we are continuing to apply our current
methodology for paying EGWPs in CY 2024. Consistent with how we have developed EGWP
payments since 2019, the CY 2024 EGWP payment methodology takes into account the
prevalence of HMO and PPO enrollment in the EGWP market by calculating CY 2024
individual market bid-to-benchmark ratios separately for HMO and PPO plan types by quartile.
CMS then takes into account the prevalence of HMO and PPO enrollment in the EGWP market

65
to combine the ratios by quartile. This methodology is more consistent with the county rates for
individual market plans, which are also not calculated separately for HMO and PPO plan types.
Section J. CMS-HCC Risk Adjustment Model for CY 2024
Comment: Commenters stated their support for the proposed CY 2024 CMS-HCC model, stating
it improves payment accuracy, program integrity and helps address excess payments to MA
organizations that have negatively affected taxpayers and beneficiaries. Specific examples of
support included the following comments:
• Updating the model with more recent underlying data will improve the accuracy of risk
adjustment and payments to MA organizations;
• Updating the model to account for the transition from ICD-9 to ICD-10 provides more
quality diagnostic information;
• Making changes to address variation in coding will decrease the impact of variability in MA
coding compared to FFS.
Response: We thank the commenters for their support. We agree that moving to the 2024 CMS-
HCC model will improve payment accuracy to MA plans and that updating the risk adjustment
model is an essential part of CMS’ duty to effectively run the MA program and be a steward of
the Medicare program.
Comment: Many commenters requested CMS phase in the updated 2024 model over multiple
years.
Response: CMS is finalizing the updated risk adjustment model proposed in the CY 2024
Advance Notice and will phase it in over 3 years. The 3-year phase in is consistent with how
CMS has approached other years in which model updates have been phased in over time (e.g.,
the 2014 model was phased in over 3 years and the CMS-HCC model adopted in the CY 2019
Rate Announcement to address the 21
st
Century Cures requirements was phased in over 4 years,
with additional revisions adopted in the CY 2020 Rate Announcement). For CY 2024, risk scores
will be calculated as the sum of 33% of the risk score calculated using the updated 2024 CMS-
HCC risk adjustment model with 67% of the risk score calculated using the current 2020 CMS-
HCC risk adjustment model. For 2025, we expect risk scores will be calculated as the sum of
67% of the risk score calculated using updated 2024 CMS-HCC risk adjustment model with 33%
of the risk score calculated using the 2020 CMS-HCC risk adjustment model. For 2026, we
expect that 100% of the risk scores will be calculated using the updated model.
Comment: Commenters recommended CMS delay implementation of the CY 2024 CMS-HCC
risk adjustment model, or withdraw it, so there could be more time to assess and understand it,
and make modifications. Some commenters requested that CMS seek additional industry input
before implementing any substantive changes to the risk adjustment model. A few commenters
cited precedent such as an October 2015 memo related to the CY 2017 Advance Notice as an

66
example when CMS solicited early feedback from the public on substantial changes to the risk
adjustment model. Commenters requested that CMS provide at least 60-day notice for changes to
the risk adjustment model. Some commenters cited risk adjustment model changes related to the
21st Century Cures Act that required a 60-day comment period in statute. A few commenters
recommended CMS better align the timing of the Advance Notice with the bid cycle to give MA
organizations more time to analyze impacts. One of these commenters recommended CMS
provide a 60- to 90-day comment period as well as release the Advance Notice between October
and December to give industry more time to analyze changes. Another commenter recommended
that any major risk adjustment model changes should be finalized at least one full year before
plans submit bids for the relevant benefit year.
Response: CMS appreciates the concerns raised by the commenters on the timing of the
implementation of the updated risk adjustment model and the process for comments.
As described in more detail later in this section and illustrated in Table III-1, it is important to
maintain or improve the accuracy of the risk adjustment model by updating it to reflect more
recent relative costs, treatment and utilization patterns, and coding practices. As the current
model ages and is used to predict expenditures for more recent enrollees in MA plans, we
identify in our analysis that predictive accuracy begins to decline. Delaying implementation of a
risk adjustment model that is based on more recent underlying data will prolong the use of a risk
adjustment model that, though still accurate according to CMS’ measures (i.e., having a
predictive ratio between 0.90 and 1.10), is waning in its ability to predict current costs. In
addition, the longer CMS waits to update the risk adjustment model, the more impactful it will be
on the year-over-year bottom line impacts for MA organizations.
It is vital that the CMS-HCC risk adjustment model is as up-to-date as possible and that CMS is
able to implement routine updates that improve accuracy and address variation in coding that
could lead to excess payments to plans. When a risk adjustment model is updated with more
recent underlying data, the relative factors associated with each demographic factor and HCC
reflect more recent costs, coding, and diagnostic patterns. All the updates in the 2024 CMS-HCC
model are steps that CMS has taken before to update the risk adjustment model and are not novel
changes to MA payment. In fact, CMS alerted plans about its commitment to move to ICD-10 in
2018 and to update the underlying data years. CMS is committed to implementing the new 2024
risk adjustment model, given that it reflects more recent data, is built using ICD-10 codes and a
clinically-based review of the best diagnoses to accurately predict Medicare costs.
We acknowledge the commenters’ request for an extended comment period. Per section
1853(b)(2) of the Act, the Advance Notice of proposed changes to the methodology and
assumptions used to determine annual MA capitation rates and the risk and other factors used in
adjusting MA capitation rates under section 1853(a)(1)(C) is required to have a minimum 30-day
comment period. The Advance Notice was released on February 1, 2023 and comments were
accepted through 6 PM Eastern Time on Monday March 6, 2023 (33 days). The statutory

67
requirement for a 60-day comment period applied only to proposals to implement certain
changes to the CMS-HCC model stipulated in the 21st Century Cures Act. As added by the 21st
Century Cures Act, section 1853(a)(1)(I)(iii) required that CMS provide at least 60 days for
public review and comment of proposed changes to the Part C CMS-HCC risk adjustment model
that were specifically based on section 1853(a)(1)(I).
Like in previous years when similar changes were proposed, CMS believes that the period
provided for comments on the CY 2024 Advance Notice is sufficient. In setting these timelines,
we seek to achieve multiple goals, including providing the statutory-required amount of time for
public comment while also releasing the Advance Notice using more current data to calibrate the
model and ensuring that the Rate Announcement is published by the statutory deadline. We
provided the public with sufficient information to review the proposals since we informed the
industry that the evaluation to reclassify the model was underway as far back as 2018 and we
provided a number of resources to evaluate the updated model. Further, the updates proposed are
in line with typical model updates for which CMS has provided a similar or shorter comment
period per the existing statutory requirement at the time. Specifically–
• In the 2018 Report to Congress,
7
CMS stated that it was conducting analyses for the
reclassification of the CMS-HCC risk adjustment model on ICD-10. In addition, CMS
outlined key specific areas in which the reclassification was being examined (e.g., episode of
care codes). The report also provided information for how CMS solicits clinical input, and
how CMS would evaluate the conditions and underlying diagnoses for inclusion in the
payment model.
• In the 2024 Advance Notice and associated releases, CMS provided a variety of information
to support the review and evaluation of the updated risk adjustment model as well as
explained the process used to develop, and the scope of changes made as part of the updated
model. The Advance Notice included or provided a link to sufficient material to evaluate the
updated risk adjustment model: the relative factors for each variable in the updated model, a
table that detailed the differences for every HCC in the current model relative to the updated
model, and the mapping of every ICD-10 diagnosis code that maps to the current 2020 model
and the updated model. In addition, CMS publicly released risk adjustment model software
which can be used to simulate risk scores under the updated model. We also released to each
MA organization and certain demonstrations plan-segment level risk scores for their
enrollees, by every model segment, for the current model, the proposed model, and for an
alternative model that had a subset of the updates. The information provided enabled
evaluation of the impact of various model updates, including the underlying HCC
restructuring (diagnosis to HCC mappings & HCC comparison table), the relative impact of
the updates (relative factor tables), the impact of the updates (plan-segment risk scores &
7
Refer to Section 4. Ongoing Research in the 2018 Report to Congress.

68
model software), and the impact of the changes focused on Principle 10 (plan-segment risk
scores under the proposed and alternative model).
8
• CMS has updated the underlying data in the model many times since the initial
implementation of the CMS-HCC risk adjustment model (see the Advance Notices and Rate
Announcements for 2007, 2009, 2013, 2014, 2017, and 2019). In addition, in the 2014
Advance Notice, CMS proposed a model (the “2014 model”) with similar updates to those in
the 2024 (e.g., data year update, a clinical revision that resulted in newly built HCCs, and
updates based on a review a diagnoses codes that showed indication of variable coding and
removal of certain codes and associated HCCs).
9
For the recent years in which the comment
timeline was extended compared to normal practice CMS made atypical structural updates to
the CMS-HCC model. For example, the 2017 model revised the underlying segmentation
structure of the model moving from a single to six community segments to improve the
sensitivity of the model and add protective features to make unique adjustments for every
health condition based on dual-eligibility status. This change was not phased in and the new
model was implemented 100% in year 1. For the 2019 and 2020 Advance Notices, we
proposed and finalized the changes to risk adjustment that were required in the 21st Century
Cures Act, such as the requirement to add an additional increase to payment when an
individual as multiple conditions – called count variables. The 21st Century Cures Act also
mandated that we provide 60 days comment for those specific changes to MA risk
adjustment, so we released a ‘Part I’ with the risk adjustment changes to comply but released
the remainder of the Advance Notice in ‘Part II’ to ensure we had the most up to date data
and analyses possible. The 2024 CMS-HCC model is not analogous to these situations
because it maintains the same structure adopted in 2017 and 2020.
CMS engages with stakeholders on a regular basis through various lines of communication. We
have regular meetings with various stakeholders – MA organizations, provider groups,
beneficiary advocates, trade groups, expert clinicians, disease specific advocacy groups,
academic researchers, and others – conduct user group calls with the industry, and release
Requests for Information (RFIs). In July of 2022, we released a comprehensive RFI that solicited
feedback for ways to improve the MA program. In response to this RFI, we received roughly
4,000 comments. We will continue to consider additional ways in which we can engage with
stakeholders as we consider changes to the CMS-HCC risk adjustment model for future years,
and appreciate commenter input.
Regarding the comment to align the Rate Announcement with the bid cycle, section
1853(b)(1)(B) of the Act requires the Rate Announcement to be published by the first Monday in
8
Principle 10 -Discretionary diagnostic categories should be excluded from payment models. Diagnoses that are particularly
subject to intentional or unintentional discretionary coding variation or inappropriate coding by health plans/providers, or that are
not clinically or empirically credible as cost predictors, should not increase cost predictions. Excluding these diagnoses reduces
the sensitivity of the model to coding variation and coding proliferation.
9
Refer to Section G. of the 2014 Advance Notice

69
April before the contract year; this is roughly 2 months before the statutorily-set bid submission
date of the first Monday in June.
Comment: Some commenters asked for more information from CMS regarding the updated
model. The information requested included: underlying data used to calibrate the model, analysis
supporting the predictive accuracy of the model, assessment of the model’s impact on certain
subgroups and plan types (e.g., individuals dually eligible for Medicare and Medicaid, all types
of Special Needs Plans (SNPs), and racial and ethnic minorities), and details on the technical and
clinical expert panel review. Examples of the suggestions for analysis and/or additional
information CMS should release to the public included:
• The reclassification methodology including the underlying data used to calibrate the model
so that stakeholders may simulate the proposed model revision and provide meaningful
feedback;
• An analysis on the effect of the case-mix between MA and FFS because of concerns that
sicker beneficiaries are leaving MA for FFS and healthier beneficiaries are moving from
FFS to MA resulting in HCC coefficients that are too high;
• An analysis supporting the predictive accuracy of the model including providing predictive
ratios and r-squared (R
2
) values, similar to what has been provided in previous iterations;
• An analysis to support departing from a recent statement in the Report to Congress that the
2020 model was performing well;
• An analysis to determine if plan-level variations in coding of certain conditions is associated
more with differences in beneficiary composition than upcoding;
• An analysis using the most recent PY 2022 data to reevaluate model estimates;
• Software, coefficients, and diagnosis mappings for an updated model with the updated data
years and ICD-10 changes, but without the Principle 10-focused clinical updates related to
variable coding (the V27 model); and
• Supporting data for removing diagnoses and HCCs, an analysis on diabetes, and other data
justifying Principle 10 (i.e., addressing variable coding).
Response: We appreciate commenters requests. As noted in the Reports to Congress, the CMS-
HCC risk adjustment models have consistently performed well, and the latest Report to Congress
included analyses of the performance of the 2020 risk adjustment model.
10
CMS has updated the
underlying data in the model many times since the initial implementation of the CMS-HCC risk
adjustment model (see the Advance Notices and Rate Announcements for 2007, 2009, 2013,
2014, 2017, and 2019). Further, CMS has always made updates to model calibrations to account
for updates and changes in International Classification of Diseases, Clinical Modification
diagnosis codes. Periodically, CMS conducts a clinical revision of the CMS-HCC model and
rebuilds all the HCCs from the ground up and, in the process, takes into account changes in
10
2018 and 2021 Reports to Congress: https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Risk-
Adjustors-Items/ReportToCongress

70
disease patterns, treatment methods and their costs, and coding practices, as well as
compositional changes within the Medicare population. For example, in 2014 we implemented
an updated CMS-HCC model that included a clinical revision using newly built HCCs using
ICD-9 codes, for which coding patterns had changed in the 10 years since the initial CMS-HCC
model. For CY 2023, CMS proposed and implemented an RxHCC model with changes similar to
those made to the 2024 CMS-HCC model. The CY 2023 RxHCC model was updated based on
more recent underlying data years and the model RxHCCs were reclassified based on the ICD-10
classification system.
As noted in the CY 2024 Advance Notice, the 2024 CMS-HCC model results in more
appropriate relative weights for the HCCs included in the model. CMS weighs a number of
considerations when updating and revising the CMS-HCC model. Since MA plans bear full
financial risk for the population and services they cover, a main objective of risk adjustment is to
minimize incentives for MA plans to compete for the healthiest beneficiaries. The risk
adjustment model accomplishes this by accurately predicting relative risk across subgroups of
beneficiaries and reimbursing plans more for populations that are expected to be sicker and have
more complex health needs. This is achieved through the segmentation of the model that assigns
unique risk scores for each condition based on demographic factors. A key focus of the MA risk
adjustment model is to accurately predict costs that are attributable to characteristics that are
present over time (e.g., chronic conditions that persist or affect longer term costs, demographics,
etc.). In this sense, the model is an insurance-like model that seeks to balance the over and under
prediction errors so that the average actual expenditures for a sufficiently large group of
beneficiaries equals the average predicted expenditures.
Further, because we are using the CMS-HCC model for payment (as compared to an analytic
exercise to predict costs), we follow our longstanding principles when updating the model in
order to ensure both statistical and clinical meaningfulness.
Because of the risk adjustment model’s focus on predicting foreseeable costs, a key factor in
measuring the predictive accuracy of the model is measuring how well it predicts costs over
subgroups of beneficiaries. Predictive accuracy in the CMS-HCC models is measured by the
predictive ratio – the ratio of predicted cost to actual cost – for a group of beneficiaries. While
perfect prediction is a predictive ratio of 1.0, every subgroup does not need to have a predictive
ratio of 1.0 to indicate a high performing model. Rather, when comparing models for groups of
beneficiaries, a predictive ratio closer to 1.0 indicates a better prediction, but a predictive ratio
between 0.90 and 1.10 is generally considered accurate.
11
The predictive ratios for each group of
FFS beneficiaries, when divided into 10 subgroups based on level of risk (i.e., costs predicted by
the model), show that the model predicts well across the spectrum of risk, meaning that, on
11
https://www.cms.gov/files/document/report-congress-risk-adjustment-medicare-advantage-december-2021.pdf, p. 42
71
average, MA plans with varying risk profiles are compensated commensurate with their expected
experience.
By this measure, as explained in more detail below, the 2024 CMS-HCC model that we are
finalizing improves on the predictive accuracy of the 2020 CMS-HCC model.
In addition, in prior years, we either have elected or have been directed by Congress to improve
prediction for selected subgroups of beneficiaries. For example, the 2017 CMS-HCC model
established separate model segments for populations dually enrolled in Medicare and Medicaid.
The 2014 CMS-HCC model, which had a single-segment for all enrollees residing in the
community, under predicted spending for full benefit dual eligible groups in the model sample
by close to 9 percent. Based on these findings, CMS elected to develop a model that improved
prediction for these beneficiaries. Predicting cost for dually eligible beneficiaries in separate
segments improved their predictive ratio to 1.0 and subsequently improved the accuracy of
payments to MA plans, which were increasingly specializing in dual eligible beneficiaries.
Congress, through the 21st Century Cures Act, also directed CMS to make changes to the model
to address concerns about the predictive accuracy of the model for beneficiaries with multiple
chronic conditions and for specific behavioral health conditions. The addition of count variables
and clinical revisions to HCCs improved the predictive ratios. The previous changes we made to
improve the predictive accuracy of the model are maintained in the 2024 CMS-HCC model.
There are a number of reasons to update and revise the CMS-HCC model, all of which improve
or maintain predictive accuracy. We improve accuracy of the model by updating the CMS-HCC
model with more recent underlying data years to better reflect the more recent relative costs and
more recent treatment and utilization patterns for conditions in the model, thereby avoiding any
reductions in predictive accuracy that can result from using relative factors based on older data.
For example, the actual expenditure per person for beneficiaries diagnosed with Multiple
Sclerosis (HCC 77 in the 2020 CMS-HCC model) increased 24.2 percent from $17,966 in the
2014/2015 sample to $22,308 in the 2018/2019 sample. The prevalence of Multiple Sclerosis
also increased by 11.6 percent between the 2014 and 2018. Updating the model with more recent
data results in higher a relative factor for Multiple Sclerosis to better predict cost for MA
beneficiaries. While maintaining or improving the model’s predictive accuracy by decile of
predicted risk is necessary, keeping the model up-to-date with more recent experience is also
necessary. For example, as Table III-1 shows, the current model 2020 CMS-HCC model that is
calibrated using 2014 diagnoses and 2015 costs for 2019 beneficiaries, to their actual cost in
2019, by decile of predicted risk. While the current model maintains predictive accuracy, it is
less accurate than models with more recent data because of inflation, changing beneficiary
characteristics, and differences in diagnostic coding patterns in FFS. Models based on more
recent data and coding patterns are the most accurate possible representation of what experience
is expected to be in future payment years. The 2024 CMS-HCC model is more accurate than the
2020 CMS-HCC model because it reflects more recent relative cost (2019 compared to 2015)
72
and includes clinically meaningful conditions that predict cost developed from experience with
ICD-10.
Measures of model performance that are based on individual observations such as the R
2
, which
measures how well the model explains variation in spending across individuals (rather than
groups), are produced with the risk adjustment model but are not a primary factor when
determining the model’s specification. Given the model’s goal of predicting costs over
subgroups, it is not intended to predict accurately for individuals or small subgroups of
beneficiaries. As such, measures of model performance for individuals are less relevant.
Nevertheless, the 2024 model has an improved R
2
compared to the current 2020 model.
Table III-1 provides predictive ratios by decile of risk, meaning the higher the risk the higher the
risk score, for the current 2020 model using both a 2014 – 2015 sample population (which is
what it was calibrated on) as well as the current 2020 model using the updated 2018 – 2019
sample population (used for the updated 2024 model), and the updated 2024 model using the
2018 – 2019 sample population. The predictive ratios provided in Table III-1 are the ratio of
2019 expenditures predicted by the model for 2019 to the actual 2019 expenditures using 2018
diagnoses. We have also provided predictive ratios by demographic segments in Attachment VIII
Tables VIII-5 – 11 for multiple subpopulations. As indicated in the below table, the current
model for both 2014 – 2015 and 2018 – 2019 sample population continue to predict expenditures
accurately, having predictive ratios between 0.90 and 1.10, but we observed that over time the
accuracy begins to decline. When comparing the same 2018 – 2019 sample population, we see
that for all but one decile the updated model predicts expenditures more accurately than the
current 2020 model.

73
Table III-1 Predictive Ratios by Decile of Predicted Risk
2014/2015
Sample
2018/2019 Sample
Decile 2020 Model 2020 Model 2024 Model
Improvement in
Predictive Risk
Entire sample
1.000
0.974
1.000
-
First (lowest) decile
0.971
0.910
0.970
Second decile
0.985
0.946
0.986
Third decile
0.987
0.943
1.013
Fourth decile
0.986
0.964
1.000
Fifth decile
1.001
0.981
0.994
Sixth decile
1.003
0.977
0.996
Seventh decile
1.005
0.987
0.999
Eighth decile
1.006
0.988
0.998
Ninth decile
1.006
0.993
1.008
Tenth (highest)
1.002
0.966
1.003
Top 5%
0.998
0.948
0.999
Top 1%
0.985
0.922
0.984
Top 0.1%
0.952
0.885
0.966
_
NOTES:
1. “Improvement in Predictive Risk” compares the distance the predictive ratios are from 1.0 for the 2024 model and 2020
model with a 2018 – 2019 sample.
2. A green arrow indicates that the predictive ratio for any specific decile for the 2024 model is closer to 1.0 than the
predictive ratio for the 2020 model with a 2018 – 2019 sample, and vice-versa.
Table III-2 provides the R
2
for the CMS-HCC model segments for the current 2020 CMS-HCC
model and the 2024 CMS-HCC model. As previously stated, CMS uses the predictive ratio as
the primary measure of accuracy for the model and R
2
is less useful in assessing the predictive
accuracy of the MA CMS-HCC risk model. However, we provide the R
2
for the model segments
because it does provide information about the extent to which the model can explain variation in
expenditures between individuals. Table III-2 shows there is slight improvement in all
demographic segments, including Full-Benefit Duals. (Increases in R
2
values indicate
improvement.)
Table III-2 R-Squared by CMS-HCC Model and Demographic Segments
Demographic Segment
2020 Model
(14/15 Sample)
2024 Model
(18/19 Sample)
Non-Dual, Age≥65
0.1257
0.1355
Non-Dual, Age<65
0.1148
0.1472
Full-Benefit Dual, Age≥65
0.1214
0.1246
Full-Benefit Dual, Age<65
0.1317
0.1889

74
Demographic Segment
2020 Model
(14/15 Sample)
2024 Model
(18/19 Sample)
Partial-Benefit Dual, Age≥65
0.1122
0.1159
Partial-Benefit Dual, Age<65
0.0987
0.1589
Institutional
0.1087
0.1200
CMS released a variety of information to support the review and evaluation of the updated risk
adjustment model as well as explaining the process used to develop, and the scope of changes, in
the updated risk model. As previously noted, the Advance Notice included or provided a link to
sufficient material to evaluate the new risk model: the relative factors for each variable in the
updated model, a table that detailed the differences for every HCC in the current model relative
to the new model, and the mapping of every payment ICD-10 diagnosis code under the current
model and the updated model. Though the information released in the Advance Notice was
sufficient to analyze the model, CMS also publicly released risk adjustment model software
which could be used to more quickly simulate risk scores. We also released to each MA
organization and certain demonstrations plan-segment level risk scores for their enrollees, by
every model segment, for both the proposed model and for an alternative model that had a subset
of the updates. The information provided enabled evaluation of the impact of various model
updates, including the underlying HCC restructuring (diagnosis to HCC mappings & HCC
comparison table), the relative impact of the updates (relative factor tables), the impact of the
updates (plan-segment risk scores & model software), and the impact of the changes focused on
Principle 10 (plan-segment risk scores under the proposed and alternative model that had a
subset of the updates in the new risk model we are adopting).
As with every model update, CMS noted in the CY 2024 Advance Notice that there will be
variation in the impact on risk scores depending on the clinical profile of each plan’s enrollees.
All of the model updates (i.e., underlying data updates, denominator update, and ICD-10
reclassification) contribute to changes in the relative costs of conditions, and therefore changes to
the resulting risk scores. Beneficiary risk scores or plan average risk scores may change
depending on an individual beneficiary’s combination of diagnoses or the clinical profile of a
plan’s enrollee population. Further, the risk scores of different subgroups can change differently,
to reflect changes that may be particular to that subgroup or clinical profiles that are more
prominent in a subgroup. These subgroups include dual status, Long Term Institutional (LTI)
status, geographic location, plan type, to the extent that plans focus on enrolling beneficiaries
with different characteristics.
Risk score differences between the current model and the updated model will occur for several
reasons. Specifically, revisions to the models result in changes in the marginal cost attributable to
each HCC, relative to the change in the average cost (i.e., denominator used to set the relative
factors), and can alter the relative factor associated with each HCC, and with the relative values
among HCCs. In addition, changes in the relative factors will result from changing from HCCs
that were created using the ICD-9 classification system to HCCs that were created using the

75
ICD-10 classification system, as well as from the addition or deletion of HCCs to or from the
model.
Comment: Many commenters stated that the updated model will have a significant negative
effect on the availability of supplemental benefits, and specifically identified a variety of benefits
that they thought would be affected. Commenters mentioned increased beneficiary cost sharing,
and reduced supplemental benefits such as transportation, nutritious meals, dental coverage,
hearing coverage, vision coverage, telehealth coverage, fitness and wellness benefits, decreased
cost-sharing, annual vision exams and coverage for glasses or contact lenses, as the
consequences of adopting the new model.
Response: We estimate that the overall impact of the CY 2024 Rate Announcement will be a net
increase of payment of 3.32%. The updated risk adjustment model is one of many factors that
contribute to the net payment increase, and when MA organizations prepare their bids and
benefit packages, they take into account all these factors when they determine the amount of
supplemental benefits they will offer. In addition, MA organizations have a variety of business
decisions that they make when determining how much profit margin they include in their bids,
how to allocate revenue to supplemental benefits, and the amounts that they allocate to each
category of supplemental benefits. Given the competitive nature of the MA program, we
anticipate that MA organizations will strive to minimize the impact of any payment-related
changes on beneficiaries and the scope of benefits available to them. While impacts may vary by
MA plan for a variety of reasons, given the increased revenue projected for MA organizations,
we expect that the availability of supplemental benefits will be stable or grow in CY 2024, as
seen previously in years with comparable updates. Following those payment updates, the MA
market remained stable and enrollment in MA continued to grow.
Comment: Many commenters stated that the updated model will impact care delivery and the
quality of care. Many of these commenters expressed concerns regarding the number of ICD-10
codes that no longer map to HCCs in the model, as well as some of the specific clinical areas that
are not included in the new CMS-HCC risk adjustment model, and expressed concern that the
changes made in the updated model will directly affect patient care. Specifically, commenters
cited that there are over 2,000 net fewer ICD-10 codes mapped to the updated model compared
with the current model. The commenters focused on the changes to the volume of diagnoses
mappings instead of the specific clinical updates, and stated that removing these diagnosis codes
may have significant health implications, and may prevent slowing disease progression from
early stages. In addition, some commenters stated that the conditions removed from the proposed
model are precursors to adverse medical events, and that their removal would disincentivize
catching these conditions early. Some commenters stated that the recalibration of the updated
model lowers HCC coefficients which will result in negative clinical outcomes particularly for
vulnerable populations. A few commenters recommended CMS consult with all medical
specialties prior to making any clinical changes to the HCC reclassification. Commenters
expressed concern of possible unintended consequences to patient care that may occur since they

76
envisioned that clinician coding and documentation practices would become less precise for
early or mild stage disease in response to the model update. Commenters highlighted specific
conditions as areas of concern (which we address in specific responses below).
Response: Risk adjustment is intended to reduce or eliminate “the incentives to enroll only the
healthiest, and thus least expensive, beneficiaries while steering clear of the sickest and
costliest—thereby rewarding Medicare Advantage insurers to the extent that they achieve
genuine efficiencies over traditional Medicare in addressing the same health conditions.”
UnitedHealthcare Ins. Co. v. Becerra, 16 F.4th 867, 873-74 (D.C. Cir. August 13, 2021, reissued
November 1, 2021), cert. denied, 142 S. Ct. 2851 (U.S. June 21, 2022) (No. 21-1140). The risk
adjustment model used for MA payment is not designed to drive clinical behavior to look for
specific conditions or to be the sole purpose for MA organizations or health care providers to
identify and treat conditions that are potential precursors to adverse medical events or
complicating factors in the identification and treatment of other conditions. MA organizations
are required, by their contracts with CMS and section 1852(a) of the Act, to furnish medically
necessary Part A and Part B benefits to their enrollees. Because MA organizations are at
financial risk for the care of their enrollees, changes in the risk adjustment model do not change
the fundamental incentive in a capitated payment system to reduce morbidity and mortality by
identifying and treating early stages of disease. Therefore, we respectfully disagree with
commenters that the changes to the mappings of certain diagnoses or conditions to the HCCs in
the model will disincentive MA organizations from identifying and treating conditions early in
the disease process.
MA organizations submit bids to CMS that request the revenue needed to cover the expected per
beneficiary costs of their enrollee population. Risk adjustment is used to adjust plan bids and
payment based on health status and demographic characteristics such that plans are paid more for
beneficiaries predicted to have higher costs. To accurately predict the likely relative cost of each
beneficiary, it is important to include in the risk adjustment model those diagnoses and
conditions that are reliable predictors of future costs and exclude those that are unreliable
predictors of future costs. For the CY 2024 model, CMS undertook a comprehensive and
thoughtful process, informed by clinical input, to determine the diagnoses and conditions for
inclusion. As a result, the new model will better direct resources to plans with beneficiaries with
higher health care needs.
CMS uses ten longstanding principles, originally introduced in the 1999 Report to Congress and
later expanded and formally established by the 2000 Report to Congress, to group diagnosis
codes into HCCs and select which HCCs are included in the model.
12,13
Regarding the specific
diagnoses and conditions that were included in the updated model, CMS followed these
longstanding principles to group diagnosis codes and build all new HCCs using ICD-10-CM
12
1999 Report to Congress: Proposed Method of Incorporating Health Status Risk Adjusters into Medicare+Choice Payments
13
2000 Report to Congress: Diagnostic Cost Group Hierarchical Condition Category Models for Medicare Risk Adjustment

77
diagnosis codes. ICD-10-CM diagnosis codes have been used by U.S. providers since October
2015. Moving from ICD-9-CM to ICD-10-CM was a major classification change in the U.S.,
both in terms of the volume of diagnosis codes and in the structure and clinical specificity of
codes, as well as changes in clinical concepts for some conditions. Therefore, we conducted
multi-years analyses (2016/2017, 2017/2018, and 2018/2019) to assess the stability of using
ICD-10 diagnosis codes for the model calibration.
14
Because providers are no longer using ICD-
9, in order to update the underlying data for the model calibration, a reclassification had to occur
to develop HCCs aligned with the ICD-10 classification system. As part of this process, we
determined which diagnoses were the best predictors of prospective costs based on our
longstanding principles for developing risk models.
15
As a result of this reclassification, the
number of HCCs in the payment model increased from 86 to 115. The updates made to the CMS-
HCC model improves its accuracy by reflecting more recent cost and utilization patterns, and by
including conditions that reliably predict Medicare costs, and thus help ensure that higher
payments are available to plans that serve beneficiaries who are expected to have more costly
health care needs.
Relative factor differences between the current model and the proposed model will occur for
several reasons. Since the model update included updated data years and included an HCC
reclassification, changes in the marginal cost attributable to each HCC is driven by both of these
updates. In addition, the relative factors associated with each condition is relative to the change
in average cost (i.e., the updated denominator). As noted above, the risk model was reclassified
increasing the number of HCCs from 86 in the current model to 115 in the updated model. For
this reason, generally comparing HCC coefficients across both models would not be an
appropriate measurement. For those conditions in which the HCC persisted across both models,
some coefficients have increased more than average and some have increased less than average.
For those conditions whose dollar coefficients have increased more than average, the relative
coefficients have increased (see Multiple Sclerosis example discussed earlier in this section). As
noted in the CY 2024 Advance Notice, changes to the condition categories – including additions,
deletions, and revisions – are based on each condition category’s ability to predict costs for
Medicare Parts A and B benefits. Condition categories that do not predict costs well – for
example, because the coefficient is small, the t-value is low, a small number of beneficiaries
have the certain condition, or the condition does not have well-specified diagnostic coding – are
not included in the model. As previously stated, condition categories and the underlying ICD-10
to HCC mappings are evaluated using the longstanding risk adjustment principles. Empirical
data are taken into account along with clinician information and clinician input when evaluating
HCC for inclusion in the model. Empirical data analysis includes reviewing diagnosis
14
In Section 4 Ongoing Research of the 2018 & 2021 Reports to Congress CMS discusses the need to evaluate ICD-10 diagnosis
patterns: https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Risk-Adjustors-Items/ReportToCongress
15
Advance Notice of Methodological Changes for Calendar Year (CY) 2004 Medicare+Choice (M+C) Payment Rates; 2021
Report to Congress on Risk Adjustment in Medicare Advantage (section 2.3 provides further details on the Principles of Risk
Adjustment). See also 2018 and 2021 Reports to Congress
78
frequencies, predictive power, expenditures associated with the condition, chronicity (duration of
a condition), and prospective cost prediction (analyses of concurrent versus prospective costs
implications).
To obtain clinical input throughout the model development process, CMS consulted with a panel
of internal medicine and general practitioners to provide clinical expertise, as the model covers
all body systems and a broad spectrum of diagnoses. The clinicians are practicing physicians, as
well as professors, and health services researchers. A series of discussions with the clinicians
were held over the course of a year to review and discuss the reclassification. The reclassification
process, including the clinical consultation panel review, is an iterative process. The process
involves empirical data investigation and analysis by healthcare economists, clinical research,
and clinician input and review. Multiple iterations of the model are calibrated to evaluate
diagnosis mappings, HCC reconfigurations, clinical hierarchies, and which HCCs are included in
the model for payment. Clinician input was provided, where applicable, for each model iteration.
Decisions regarding the model classification (e.g., how diagnoses are grouped) were made based
on the level of granularity provided in the ICD-10 classification system, the risk adjustment
model principles, examination of the model performance (i.e., predictive accuracy), and for the
initial analysis to further assess which conditions are more discretionary, a review of HCC
frequencies in MA and FFS.
The clinical panel provided insight and recommendations related to the criteria used to evaluate
and treat conditions (e.g., lab findings, test results, physical exams, medications, medical
interventions, etc.); specificity of diagnoses; potential for variable coding for certain diseases or
disease groups; treatment practices; manifestations of conditions in different populations (e.g.,
aged vs. disabled; non-dual vs. full-benefit; dual vs. partial-benefit dual); disease severity and
implications for medical burden; the need for additional medical specialist intervention (i.e.,
whether or not a condition would require evaluation by a specialty clinician); clinical face
validity (i.e., whether the condition is consistent with the relative costs associated with it) and
interpretation of empirical results; clinical similarities and differences between specific diseases
(e.g., Crohn’s disease and ulcerative colitis); relationship of acute and chronic versions of
diseases (e.g., acute hepatitis C and chronic hepatitis C); and implications for predicted costs.
The HCC classification system is exhaustive (i.e., all diagnosis codes map to an HCC). While all
diagnosis codes map to an HCC, only a smaller subset of HCCs are included in the payment
model. When CMS refers to “payment HCC” we are referring to an HCC that is included in the
model for payment, and vice versa for references to “non-payment HCCs.”
Below we address the specific conditions that were re-mapped or grouped differently in the
updated 2024 risk adjustment model and about which concerns were raised by commenters.
There were HCC reconfigurations and underlying diagnosis changes as described in the 2024
Advance Notice. Below we review these changes:
79
• Vascular Disease (Diagnoses related to atherosclerosis, aortic, deep vein thrombosis,
embolism, and other circulatory diseases)
o As identified in the 2024 Advance Notice, the Vascular disease group was reconfigured
from the 2020 CMS-HCC model to the 2024 CMS-HCC model. There are 365 ICD-10
payment diagnosis codes in the vascular disease group. The increased granularity under
the ICD-10 classification system permitted better configuration of the vascular HCCs,
and HCCs 107-108 were reconfigured into three new HCCs, 263, 264, and 267. Under
the current 2020 CMS-HCC model, vascular HCC 108 contains a range of ICD-10 codes,
including those describing atherosclerosis of the aorta, renal artery, and extremities,
except with ulceration or gangrene; specified aneurysms; and peripheral vascular disease.
ICD-10 codes atherosclerosis of arteries of extremities unspecified, with exercise or rest
pain, ulceration, or gangrene are mapped to HCCs in the Vascular disease hierarchy
according to their clinical severity. Based on empirical data (e.g., expenditure patterns,
frequency, predictive accuracy) and clinician input, payment HCCs for atherosclerosis of
arteries of extremities in the updated 2024 CMS-HCC model contain primarily codes for
atherosclerosis with rest pain and with ulceration or gangrene, as they typically indicate
more serious cases.
o In consultation with clinicians, codes that indicate more serious cases of vascular disease
were retained in the payment HCCs, and diagnoses for “other” and “unspecified” disease
were mapped to a non-payment HCC. Diagnosis codes for atherosclerosis of arteries of
the extremities with rest pain were moved to the higher-level payment HCC 264.
Diagnoses “with rest pain” indicates compromised vasculature in the leg and that
vascular disease is likely more widespread, so usually requires intervention. Codes for
atherosclerosis of arteries of the extremities, with intermittent claudication were broken
out as new nonpayment HCC 265 (refer to additional information provided in a later
response). A new HCC 267 was created for Deep Vein Thrombosis and Pulmonary
Embolism due to clinical considerations (similar indications for treatment and cost
implications in a prospective model). Of the remaining codes from 2020 CMS-HCC
model HCC 107, only the more severe manifestations that would consistently and
reliably predict costs prospectively (e.g., aortic aneurysm, ruptured and arterial embolism
and thrombosis) are mapped to payment HCC 264. Diagnosis codes (e.g., Atherosclerosis
of the Aorta) for manifestations or stages of diseases that are not consistently reliably
predictive of future years costs (e.g., involve lifestyle changes, or medical monitoring)
were mapped to the lower level Vascular HCC. The new treatment of the vascular
disorders is consistent with the treatment of coronary atherosclerosis in the CMS-HCC
model, in which the diagnosis of coronary atherosclerosis is non-payment, but the more
severe manifestations of unstable angina and acute myocardial infarction are payment
HCCs.
• Metabolic Diseases (Endocrine related diagnoses)
80
o There are three payment HCCs in the 2020 CMS-HCC model Metabolic disease
group. The 2024 CMS-HCC model Metabolic disease group was expanded to four
HCCs, in the payment model. HCC 23 (Other Significant Endocrine and Metabolic
Disorders) was reconfigured to pull out select conditions with prospective cost
implications. There are 59 ICD-10 payment diagnosis codes in the metabolic disease
group. First, high-cost lysosomal storage disorders with expensive Part B drug
treatments were split out into a new HCC 49 Specified Lysosomal Storage Disorders.
Then metabolic disorders and endocrine disorders were separated based on cost and
clinical considerations into HCC 50 Amyloidosis, Porphyria, and Other Specified
Metabolic Disorders, and HCC 51 Addison’s and Cushing’s Diseases, Acromegaly,
and Other Specified Endocrine Disorders, respectively. Other conditions (e.g.,
aldosteronism) from the 2020 CMS-HCC model HCC 23 that may be more indicative
of lab test results and can be manifestations of other, underlying disorders (e.g., heart
failure), or are primarily treated with lower-cost medications were mapped to a non-
payment HCC based on empirical overprediction (i.e., overprediction of the costs for
beneficiaries with these conditions) and clinical considerations. This is consistent
with the treatment of hypothyroidism and hyperthyroidism, which are not in the 2020
or proposed 2024 CMS-HCC payment models.
• Heart Diseases (Cardiovascular and heart failure diagnoses)
o There are five payment HCCs in the current 2020 CMS-HCC model Heart disease group.
In the reclassified 2024 CMS-HCC model, the Heart disease group was expanded to ten
payment HCCs, due to the split-out of 2020 CMS-HCC model HCC 85 Congestive Heart
Failure into five payment heart failure HCCs (222-226) to account for clinical severity
and cost differences. There is a hierarchy among heart failure HCCs, with new HCC 221
Heart Transplant Status/Complications added to the top of the hierarchy and new split-
out HCC 227 Cardiomyopathy/Myocarditis at the bottom. Multiple different
configurations of heart failure codes were evaluated, and the implemented hierarchy was
finalized based on empirical analyses and consulting clinicians’ input. The HCC structure
captures differences in prospective costs among conditions and has clinical salience.
Principle 10 focused changes are discussed in a later response.
• Blood Disease (Coagulation diagnoses and disorders of immunity)
o There are three payment HCCs in the 2020 CMS-HCC model Blood disease group. In the
2024 CMS-HCC model, the Blood disease group was expanded to seven payment HCCs.
There are 132 ICD-10 payment diagnosis codes in the blood disease group. Specifically,
diagnoses that describe coagulation defects, hemorrhagic conditions, and purpura were
mapped to payment HCC 112 Immune Thrombocytopenia and Specified Coagulation
Defects and Hemorrhagic Conditions or non-payment HCC Thrombocytopenia, Purpura,
Thrombophilia, and Other and Unspecified Hemorrhagic Conditions based on clinical

81
severity, specificity, and the reliability for predicting prospective costs. There are two
payment HCCs (114-115) in the 2024 CMS-HCC model Blood disease group that
describe immune conditions. HCCs 114 Common Variable and Combined
Immunodeficiencies and 115 Specified Immunodeficiencies and White Blood Cell
Disorders contain immune conditions from the 2020 CMS-HCC model HCC 47. This
split-out allows for isolation of the costlier and clinically severe common variable and
combined immunodeficiencies (in 2024 CMS-HCC model HCC 114) from other
specified immunodeficiencies and white blood cell disorders (in 2024 CMS-HCC model
HCC 115), while unspecified, non-specific, and lower-severity immune disorders were
mapped to a non-payment HCC.
• Amputation
o There is one payment HCC in the 2020 CMS-HCC model Amputation disease group,
which was reconfigured to cover initial complications or ongoing costs of lower limb
amputation in the 2024 CMS-HCC model. There are 44 ICD-10 payment diagnosis codes
in the amputation disease group. Diagnosis codes for the acquired absence codes of toe
and finger were mapped to the non-payment HCC Post-Surgical States/Aftercare/Elective
to more accurately classify them based on similar implications for disease burden (e.g.,
similar clinical implications for care) and cost prediction. This is parallel to the RxHCC
model, where these codes similarly map to nonpayment HCCs.
16
• Neurological Diseases (Polyneuropathy diagnoses)
o There are eight payment HCCs in the current 2020 CMS-HCC model Neurological
(Neuro) disease group. In the 2024 CMS-HCC model, the Neuro disease group was
expanded to twelve payment HCCs. There are 200 ICD-10 payment diagnosis codes in
the neurological disease group. Codes in the current 2020 CMS-HCC payment HCC 75
Myasthenia Gravis/Myoneural Disorders and Guillain-Barre Syndrome/Inflammatory
and Toxic Neuropathy were reconfigured into 2024 CMS-HCC model HCCs 193-196.
First, the most underpredicted and chronic codes were pulled out into new payment HCC
193 Chronic Inflammatory Demyelinating Polyneuritis and Multifocal Motor
Neuropathy. The acute Guillain-Barre Syndrome became non-payment HCC 194 in the
2024 model; costs associated with this HCC are predicted reasonably well without being
in the payment model, and this diagnosis will transition to HCC 193 if it becomes long-
lasting/chronic. Myasthenia gravis codes were reconfigured into two payment 2024
CMS-HCC model HCCs based on clinical severity and cost differences: HCC 195
Myasthenia Gravis with (Acute) Exacerbation; and HCC 196 Myasthenia Gravis without
(Acute) Exacerbation and Other Myoneural Disorders. In the 2024 CMS-HCC model,
16
The Rx Hierarchical Condition Categories (RxHCC) model is used in Medicare Part D risk adjustment.
https://www.cms.gov/files/document/2023-announcement.pdf.
82
nonpayment HCC 203 Polyneuropathy, Mononeuropathy, and Other Neurological
Conditions/Injuries remains parallel to the 2020 CMS-HCC model nonpayment HCC 81,
with the addition of several clinically related codes determined not appropriate for the
payment model on empirical, clinical, or coding specificity grounds (narcolepsy and
cataplexy, drug-induced and other polyneuropathies, neuromyopathy and central nervous
system atrophy).
• Diabetes
o There are three payment HCCs in the 2020 CMS-HCC model Diabetes disease group.
The 2024 CMS-HCC model HCC classification has four payment diabetes HCCs, as
HCC 35 Pancreas Transplant Status was added to the top of the hierarchy. There
continue to be three 2024 CMS-HCC model payment HCCs for diabetes with/without
complication, with minor differences in code content compared to the payment HCCs in
2020 CMS-HCC model. There are 344 ICD-10 payment diagnosis codes in the diabetes
disease group. In consultation with clinicians, the diagnosis codes for diabetes with
unspecified complications and with complications related to glycemic (i.e., blood sugar)
control were moved to the lowest payment HCC, 2024 CMS-HCC model HCC 38. This
was due to empirical data regarding coding frequency, as well as clinical considerations
(high blood sugar is the defining characteristic of diabetes, and thus is inherent to the
disorder rather than a complication). Glycemic complications can be acute, side effects of
drug therapy, and of less serious magnitude than complications related to other disease
groups that remain in the 2024 CMS-HCC model HCC 37 Diabetes with Chronic
Complications, and could also be associated with poorer quality of care (poor glycemic
control). Severe acute complications related to glycemic control (e.g., E11641 Type 2
diabetes mellitus with hypoglycemia with coma) remain in the highest HCC, 2024 CMS-
HCC 36. Some drug induced diabetes codes were re-mapped to a non-payment HCC
because the conditions can be temporary/reversible, variable cost profile, and the removal
allows costs to be attributed to conditions that represent the underlying health status.
• Kidney Disease
o There are five payment HCCs in the current 2020 CMS-HCC model Kidney disease
group. In the 2024 CMS-HCC model, there are four payment Kidney HCCs. There is a
straight hierarchy between the payment HCCs. There are 9 ICD-10 payment diagnosis
codes in the kidney disease group. The kidney hierarchy relies on the chronic kidney
disease (CKD) stages to define the payment HCCs. In the 2024 CMS-HCC model, the
2020 CMS-HCC model HCC 138 was replaced with two new, more granular HCCs –
328 Chronic Kidney Disease, Moderate (Stage 3B) and 329 Chronic Kidney Disease,
Moderate (Stage 3, Except 3B) – due to new FY2021 ICD-10 codes that split the broad
range of Glomerular Filtration Rate (GFRs) in stage 3 into 3a, 3b, or 3 unspecified. There
is a specified (a priori) constraint setting HCCs 328 and 329 coefficients equal, so stage 3
83
will continue to have a single payment coefficient until there is sufficient data in later
years to distinguish, estimate, and evaluate separate coefficients for HCCs 328 and 329 in
future model updates. The HCC-level split-out is parallel to the Part D V08 RxHCC
reclassification that was implemented for CY 2023, and provides future flexibility to
reconsider the constraint at the point when underlying data that includes the separate
codes for CKD stages 3a and 3b is used for a recalibration. Due to clinical considerations,
the 2020 CMS-HCC model HCCs 134 and 135, renumbered as HCC 324 Dialysis Status
and HCC 325 Acute Kidney Failure in the 2024 CMS-HCC model, were removed from
the payment model and hierarchy. HCC 324 Dialysis Status captures transitory dialysis,
and the removal from payment allows the costs to flow through to actual conditions that
created the need for dialysis, such as congestive heart failure or sepsis. If dialysis is
chronic, the beneficiary will attain ESRD status and be moved to risk scores calculated
using the ESRD model. HCC 325 Acute Kidney Injury (AKI) is also by definition
transitory. Beneficiaries without transitory disease should receive a CKD diagnosis. If
CKD stage 3 or above (moderate or severe) develops, it will be captured in the payment
model through the CKD HCCs.
• Psychiatric Diseases (Diagnoses related to Schizophrenia, Psychosis, Personality Disorders,
Bipolar Disorders and Major Depression)
o There are four payment HCCs in the 2020 CMS-HCC model Psychiatric disease group.
The 2024 CMS-HCC model Psychiatric disease group was expanded to five payment
HCCs, which remain in a straight hierarchy. There are 438 ICD-10 payment diagnosis
codes in the psychiatric disease group. The top HCC – renumbered from 2020 CMS-HCC
model HCC 57 to 2024 CMS-HCC model HCC 151 Schizophrenia – remains unchanged.
The 2020 CMS-HCC model HCC 58 (Reactive and Unspecified Psychosis) was
reconfigured as 2024 CMS-HCC model HCC 152 Psychosis, Except Schizophrenia.
Several conditions – delusional disorders, manic and depressive (bipolar) disorders,
severe, with psychotic behavior, and major depressive disorder, severe, with psychotic
features – were moved out of the HCC 59 in the 2020 CMS-HCC (current) model into
HCC 152 in the 2024 CMS-HCC model because costs for beneficiaries with these
conditions were underpredicted in the 2020 CMS-HCC model depression HCC 59 and
are clinically consistent with non-schizophrenic psychosis. The 2024 CMS-HCC model
HCC 153 Personality Disorders; Anorexia/Bulimia Nervosa, was reconfigured from
2020 CMS-HCC model HCC 60. Personality disorders were moved up above non-
psychotic depression/bipolar disorders in the reclassified Psychiatric hierarchy because of
their higher associated prospective costs. Consulting clinicians supported this
reorganization as it is reflective of care practices associated with the conditions.
Diagnosis codes for anorexia/bulimia nervosa were moved into 2024 CMS-HCC model
HCC 153 (a payment HCC) based on empirical underprediction in a non-payment 2020
CMS-HCC and consulting clinicians’ input that these conditions have prospective cost
84
implications since they require specialized treatment and frequent institutionalization.
The subsequent two payment 2024 CMS-HCC model HCCs (154-155) relate to
depression and bipolar disorders. The 2020 CMS-HCC model HCC 59 Major
Depressive, Bipolar, and Paranoid Disorders was reconfigured. In addition to the codes
specifying psychosis that were moved up to 2024 CMS-HCC model HCC 152, only
select other codes from the 2020 CMS-HCC model HCC 59 were retained as codes used
in risk adjustment payment, in the 2024 CMS-HCC model HCC 154 Bipolar Disorders
without Psychosis and HCC 155 Major Depression, Moderate or Severe, without
Psychosis. Bipolar disorder was split out as HCC 154 to reflect the greater clinical
severity compared to depression, which it hierarchically excludes. As discussed in the
“Clinical Update using ICD-10 Diagnosis Code” section of the 2024 Advance Notice, the
reclassification was guided by the longstanding 10 risk adjustment principles, including
that diagnoses in the payment model be clinically meaningful (well specified) and should
reliably predict costs in a future year. As such, diagnoses for mild, unspecified,
remission, subsequent encounter, and sequela codes were re-mapped to appropriate non-
payment HCCs. For depression, the 2024 CMS-HCC payment model is limited to ICD-
10 codes specifying moderate or severe major depression. Remaining diagnosis codes
(includes depression codes for mild, unspecified, or in remission, as well as codes for
bipolar disorders in remission) from the 2020 CMS-HCC model HCC 59 were remapped
to the nonpayment depression HCC. These codes represent less-severe conditions with
lower cost implications, and clinicians expected depression would be coded as moderate
or severe if the condition was sufficiently serious. Similarly, codes specifying in
remission were removed as beneficiaries experiencing relapse would likely be coded with
a diagnosis reflecting an active disorder. Diagnosis codes from the 2020 CMS-HCC
model HCC 59 that specify subsequent encounter for or sequela of attempted
suicide/intentional self-harm, were removed from payment, consistent with the removal
of most subsequent encounter and sequelae codes throughout the reclassified 2024
CMS-HCC model. This accounted for the majority of codes from 2020 CMS-HCC model
HCC 59 that were removed from payment in the 2024 CMS-HCC model (>95%).These
codes were remapped to the nonpayment External Causes of Morbidity and Injury disease
groups, as subsequent encounter codes require less intensive follow-up, and sequela
codes are for unspecified late effects of a condition, which are variable in clinical burden
and can be acute, and do not reliably or consistently predict meaningful prospective costs.
(The specific condition that is a sequela should be coded separately, and could enter the
payment model on that basis.) As identified in the underlying ICD-10 diagnosis to HCC
mappings CMS released with the 2024 Advance Notice, the initial encounter diagnosis
codes for attempted suicide/intentional self-harm conditions that are being actively
treated and predict ongoing and prospective costs still map to payment HCCs.
• Musculoskeletal Diseases (Diagnoses related to rheumatoid arthritis and connective tissues).
85
o There are two payment HCCs in the current 2020 CMS-HCC model Musculoskeletal
(MSK) disease group. There are three payment HCCs in the 2024 CMS-HCC model
MSK disease group. There are 1,187 ICD-10 payment diagnosis codes in the
musculoskeletal disease group. The 2020 CMS-HCC model HCC 40 was split into 2024
CMS-HCC model HCC 93 Rheumatoid Arthritis and Other Specified Inflammatory
Rheumatic Disorders and HCC 94 Systemic Lupus Erythematosus and Other Specified
Systemic Connective Tissue Disorders according to the underlying expenditures
associated with these conditions. In consultation with clinicians the conditions were split
rather than combined as they vary in chronicity, severity, and progression. HCC 93
hierarchically excludes HCC 94 so a beneficiary may receive at most one of these two
HCCs. Underpredicted codes (i.e., diagnoses where the model underpredicts costs for
beneficiaries with the condition) were moved from the 2020 CMS-HCC model
nonpayment Neuro (inclusion body myositis) and MSK HCCs (sarcoid arthropathy and
sarcoid myositis) to the payment HCC 93 in the 2024 CMS-HCC model to improve
prediction and enhance clinical coherence (i.e., grouping diagnoses that are clinically
similar). Clinically relevant, cost-similar codes were moved from a payment 2020 CMS-
HCC model Vascular HCC into 2024 CMS-HCC model HCC 94 (other and unspecified
necrotizing vasculopathies). Conditions (e.g., polymyalgia rheumatic, sacroiliitis, and
Sicca (Sjogren’s) syndrome) that were overpredicted (i.e., the mode overpredicted costs
for beneficiaries with these conditions) were moved to a non-payment HCC based on
input from consulting clinicians. For example, Sicca syndrome and sacroiliitis are
localized, whereas other conditions from the 2020 CMS-HCC model HCC 40 are
systemic, and treatment for these conditions is symptom-driven (e.g., eye drops or
sucking candy for Sicca) and unlikely to be associated with prospective costs.
Polymyalgia rheumatica can be clinically variable, is often treated by medications, and is
likely to be picked up by other diagnosis codes in severe cases.
In summary, the CMS-HCC reclassification involved revising condition categories – including
adding, deleting, and reconfiguring categories and clinical hierarchies, and freshly considering
which categories are included in the payment model. The goal was to improve predictive ability,
to better account for current disease patterns, treatment methods and costs, and diagnosis and
coding practices. The resulting model classifies the ~74,000 ICD-10-CM codes into 266 CMS-
HCCs, 115 of which are included in the 2024 CMS-HCC payment model. This increase in
condition categories from the current 2020 CMS-HCC model (204 CMS-HCCs; 86 in payment)
is due to the greater level of detail in ICD-10-CM diagnosis codes, allowing for the development
of HCCs with increased clinical specificity and validity that better capture clinical and cost
differences between conditions. In aggregate, the 2024 CMS-HCC model contains approximately
20 percent fewer ICD-10-CM codes than the 2020 CMS-HCC model. This resulted from the
removal of diagnoses in accordance with CMS’ risk adjustment principles, evaluated based on
(1) empirical data including frequency, sample size, associated expenditures (e.g., overpredicted
under the current model HCC); (2) clinical specificity and salience; (3) reliability to predict

86
prospective costs (including conditions that represent side effects of medical or drug treatment
rather than underlying health status risk); and (4) variable diagnosis or reporting (based on
empirical evidence or clinical input). Table III-3 below provides additional information on the
underlying diagnosis code counts for the current 2020 CMS-HCC model and the 2024 CMS-
HCC model.
Table III-3 Summary Statistics for the 2020 CMS-HCC and 2024 CMS-HCC Classifications
2020 CMS-HCC
Model
2024 CMS-HCC
Model
FY22/23 ICD-10 codes - total
73,926*
73,926*
FY22/23 ICD-10 codes mapped to payment HCCs
9,797 (13.3%)
7,770 (10.5%)
FY22/23 ICD-10 codes mapped to non-payment HCCs
64,129 (86.7%)
66,156 (89.5%)
Added
209
No longer mapped in the 2024 CMS-HCC Model
2,236
No longer mapped – ICD-10 clinical updates
2,161 (96.6%)
No longer mapped – Principle-10 focused updates
75 (3.4%)
HCCs - total
204
266
HCCs – payment
86 (42.2%)
115 (43.2%)
HCCs – non-payment
118 (57.8%)
151 (56.8%)
* The total number of ICD-10 diagnosis codes varies by fiscal year.
Comment: A few commenters stated concerns that the Fact Sheet released with the Advance
Notice did not discuss the methodology, assumptions, and data used for developing the MA risk
score trend. A commenter believed that not providing this additional context may lead to
confusion, misinterpretation, and possibly false conclusion about the impact of the risk score
trend on MA payments. Commenters requested that CMS include the methodological details
behind the MA risk score trend.
Response: Each year, CMS releases an associated Fact Sheet that shows the year-to-year
percentage change in payment associated with the proposed (in the Advance Notice) or finalized
(in the Rate Announcement) policies. The Fact Sheet shows the overall average impact on MA
revenue, as well as the average impact of each individual update or policy proposal. As part of
the impacts released in the Fact Sheet, CMS also estimates the average growth of MA risk scores
in the payment year, known as the MA risk score trend. The MA risk score trend is the average
increase in risk scores, not accounting for normalization and the MA coding pattern adjustment
(which are included separately). The MA risk score trend is included in the Fact Sheet because it
has direct bearing on MA payments and the MA revenue picture would be incomplete without it.
CMS calculates the MA risk score trend by calculating MA risk scores over three prior years,
then calculating the average annual change in risk scores across those three years. All three years
of risk scores are calculated using the risk adjustment model(s) to be used in the upcoming

87
payment year. This average annual change is the MA risk score trend provided in the Advance
Notice and Rate Announcement Fact Sheet. The trend is an industry average and individual
plans’ experience will vary.
Note that the MA risk score trend has a separate impact from the impact of the risk adjustment
model, which is represented in a separate row of the Fact Sheet, and is based on risk score
changes where the underlying data is held steady. Specifically, to measure the risk adjustment
model impact CMS uses the same diagnostic and demographic information run through the
current model and the model(s) for the upcoming payment years (e.g., 2020 diagnoses were used
to calculate 2021 risk scores under each model to calculate the risk adjustment model impact in
the Fact Sheet). The difference between the current model and payment year model(s) risk
scores, accounting for differences in normalization, is represented in the risk adjustment model
impact and normalization row.
By including both the risk adjustment model/normalization impact and the MA risk score trend
in the Fact Sheet, the resulting impact is effectively estimating a year-over-year payment impact
if diagnostic and demographic data are held steady, then further accounting for growth in risk
scores in the payment year based on historical experience. Therefore, it is imperative to consider
the MA risk score trend in concert with the impact of risk adjustment policy proposals to
accurately predict payment impacts in the following year.
It is important to note that every model has its own risk score trend. The current model used for
payment in CY 2023 (the 2020 risk adjustment model) has a risk score trend of 5%. Because we
are blending risk scores from the updated 2024 model with risk scores from the current 2020
model, the effective MA risk score trend of 4.44% is in the Fact Sheet for the CY 2024 Rate
Announcement. This means that though we anticipate an increase in risk scores based on the
diagnoses submitted by plans, the impact on payment is anticipated to be less in the updated
model.
Comment: Many commenters expressed concern that the updated model may have a negative
impact on certain beneficiary populations, locations, and plan types. Multiple commenters
believed that the diabetes changes and model changes where diagnoses are no longer included
for payment will have a negative impact on dually eligible beneficiaries and vulnerable
populations (e.g., minority beneficiaries and those under the federal poverty level), or
beneficiaries in urban or rural areas.
Multiple commenters expressed concerns about the model’s impacts on plans with high
enrollment of dually eligible beneficiaries, and high-risk, chronically complex vulnerable
populations (e.g., Special Needs Plans that serve dually eligible beneficiaries (D-SNPs) or
beneficiaries with certain chronic diseases (C-SNPs). Multiple commenters stated that minorities
and people with low incomes make up a larger share of MA enrollees than they do in FFS, and
that the proposed model will more negatively affect them. Commenters expressed concern about

88
the implication for benefits that SNP beneficiaries have, such as greater access to supplemental
benefits, and stated that, according to their research, the proposed model will have a more
negative impact on D-SNPs and C-SNPs, therefore negatively impacting the beneficiaries’
access to these benefits. Commenters also expressed concern that the negative impact of the
proposed model may disincentivize MA plans from offering C-SNPs. A few commenters
believed the updated model will also negatively impact employer-group waiver plans (EGWPs)
with a commenter noting the inability for EGWPs to adjust bids in response to potentially lower
risk scores.
Response: The updates improve the accuracy of the risk adjustment model and help ensure that
higher payments are available to plans that serve beneficiaries with more costly health care needs
(refer to the predictive accuracy information provided above). Additionally, the updates do not
change features in the CMS-HCC risk adjustment model, first implemented in 2017, that ensure
dually eligible beneficiaries have unique adjustments for every health condition based on their
dual-eligibility status that result in higher payments for those conditions than non-duals. The
updates also do not alter changes first implemented in 2020 that ensure that plans receive an
additional increase in payment based on the number of conditions the beneficiary has.
As previously discussed in this Rate Announcement, conditions in the model are used as
predictors of relative costs, not as direct reimbursement for the treatment of each condition. Plan
bids project the average revenue needed to cover all Part A and B benefits, and the risk score is
used to assess the relative cost of a plan’s enrollee population. Further, it is the total risk score
that predicts the relative cost of a beneficiary, and each factor predicts part of the costs;
therefore, each relative factor cannot be assessed in isolation. If a specific HCC (or diagnosis
code mapped to a specific HCC) is no longer included in the payment model, coefficients of
other HCCs and demographic factors will be increased such that the model continues to predict
the overall total expenditures (please see above for a discussion of the model’s predictive
accuracy over subgroups of beneficiaries by level of risk). Because the updated model improves
upon the current model by incorporating recent costs and utilization patterns and is developed
using ICD-10 codes, and because the model ensures that plans that enroll higher need
beneficiaries receive higher payments, we do not agree that the updated model will negatively
affect beneficiary costs or supplemental benefits, and care delivery (see also response to
comments above).
There will be variation in the impact on risk scores depending on each beneficiary’s clinical mix.
All of the model updates (i.e., underlying data updates, denominator update, and ICD-10
reclassification) contribute to changes in the relative costs of conditions compared to the 2020
CMS- HCC model currently used, and therefore changes to the resulting risk scores. Beneficiary
risk scores or plan average risk scores may change depending on an individual beneficiary’s
combination of diagnoses or the clinical profile of a plan’s enrollee population. CMS has
observed that, on average, predicted risk for dually-eligible populations and those in special
needs plans are higher than non-dually-eligible enrolled beneficiaries. On average, under the new

89
CY 2024 risk adjustment model, risk scores for special needs plans (SNPs) are 50% higher than
non-SNPs. More specifically, risk scores for C-SNPs and D-SNPs are, respectively, 54% and
47% higher than non-SNP beneficiaries. Risk scores, under the 2024 updated model, for dually-
eligible beneficiaries in the community are on average 49% higher compared to non-dually
eligible beneficiaries in the community. While risk scores change in reflection of the underlying
changes in the relative factors associated with each condition, on average, the model continues to
predict higher risk for dually-eligible and SNP enrolled beneficiaries.
In addition, as we did at an industry level, CMS calculated the MA risk score trend for dually-
eligible beneficiaries (i.e., full-dual and partial-dual beneficiaries residing in the community) and
found that the MA risk score trend for these dually eligible beneficiaries is 4.67 percentage
points higher than it is for non-dually eligible beneficiaries. As explained in detail in a later
response, the risk score trend represents the average growth in MA risk scores for the payment
year. As discussed in more detail in a later response in this section, it is imperative to consider
the MA risk score trend in concert with the impact of the updated risk adjustment model (as well
as other changes to payment factors) to accurately predict payment impacts in the following year.
On average, this growth in MA risk scores will more than offset the impact of the new risk
adjustment model and normalization for dually-eligible beneficiaries.
Comment: Commenters stated concern with the CMS review of conditions that focused on
Principle 10 – Discretionary diagnostic categories should be excluded from payment models.
Some commenters noted that removal or constraining of conditions described under Principle 10
may exacerbate health inequities, constrain investments in prevention of severe conditions, and
limit the prevention of subsequent medical events.
Some commenters stated they are supportive of CMS’ decision to update the risk adjustment
model based on more current underlying data, updating the denominator, and some clinical
revisions based on ICD-10, but were specifically opposed to the clinical revisions made under
Principle 10.
Commenters believed that CMS has not released adequate data underlying its determination to
constrain the coefficients for the diabetes and congestive heart failure HCCs. Multiple
commenters stated that CMS does not explain why imposing constraints on these conditions
helps the predictive value of the model. Some commenters believed that the constraining of the
coefficients for the diabetes HCCs in the updated model would delay diagnosis for diabetics and
lead to serious complications by lowering early detection.
Multiple commenters suggested that the removal of the conditions angina pectoris, protein-
calorie malnutrition, and atherosclerosis with intermittent claudication will also affect the ability
to conduct further clinical investigation and intervention. Some of the commenters believed that
the Principle 10-based changes are not clinically appropriate and do not accurately reflect
beneficiary acuity or cost of care. A commenter stated beneficiaries with angina pectoris incur

90
more than twice the expenditures of a typical Medicare beneficiary and four times the hospital
costs. A few commenters, citing their clinical experience, oppose removing angina pectoris and
atherosclerosis of lower extremities with intermittent claudication from the updated model
because these conditions can help with early identification and prevention of more serious
conditions such as fatal cardiovascular disease. A few commenters expressed concern that
removing protein-calorie malnutrition from the model, which can indicate frailty, will also
adversely affect institutional level of care of enrollees and beneficiaries with HIV/AIDS.
Multiple commenters cited internal analysis stating vulnerable populations and minority
communities have higher prevalence rates of conditions identified in Principle 10.
Response: CMS appreciates the feedback and concerns of the commenters.
As described in the 2024 Advance Notice, for conditions in the model where coding in MA was
highest relative to FFS, CMS reviewed these conditions with our clinical experts for evaluation
against the model principles because we believe that this coding differential indicates conditions
where there may be discretionary coding variation. The review is consistent with our evaluation
of condition categories, and the underlying ICD-10 diagnosis code to HCC mappings, against
risk adjustment model development Principle 10. In consultation with clinician input regarding
appropriate classification of identified conditions, this reclassification involved moving some
discretionary diagnosis codes from condition categories included in the CMS-HCC model to
condition categories not included in the model, removing from the model several condition
categories that do not accurately predict the projected cost of a beneficiary, and constraining
HCCs to be equal to each other so that they carry the same weight in the risk score. These
updates serve to maintain the integrity of the condition categories in the model.
CMS approached the inherent tradeoffs involved in designing a classification system using
empirical evidence on frequencies and predictive power, clinical input on relatedness, specificity,
and severity of diagnoses, and professional judgment on incentives and diagnostic patterns
relative to the classification system. Plans with an atypical distribution in their patient population
may experience varying risk scores impacts; however, the actual change in risk score of any
beneficiary with one or more of the conditions described below will depend on the totality of
their risk profile, including their demographic factors and other diagnoses.
• HCC constraints (i.e., hold the coefficients of the HCCs equal to each other such that each
HCC carries the same weight):
o Constrained all Diabetes HCCs (HCC 36, 37, and 38). In the current 2020 CMS-HCC
model the top two diabetes HCCs, 17 and 18, are constrained. When developing the 2024
CMS-HCC model, empirical data showed that the 2020 CMS-HCC model HCC 18 had a
substantially higher prevalence in MA than FFS and HCC 19 had a lower prevalence; the
shift of beneficiaries to a higher HCC in the hierarchy led to further evaluation of the
HCCs. Under the clinical criteria used to code HCC 18, beneficiaries with a range of
91
clinical burden and medical expenditures may be captured in the diabetes with chronic
complications HCC resulting in a diminished capacity for the model to differentiate
between disease severity. For example, there may be instances where a beneficiary is
coded with the more severe manifestation of diabetes based on a laboratory finding (e.g.,
automated urinalysis test that finds protein in the urine) even if the finding is not clinically
significant and has no implications for medical treatment. Thus, the constraint was
expanded to all three diabetes payment HCCs in the 2024 CMS-HCC model. Constraining
the Diabetes HCCs allows expenditures to be attributed to well defined and significant
complications of diabetes captured in other payment HCCs (e.g., chronic kidney disease
and diabetic eye disease).
o Constrained Congestive Heart Failure HCCs (HCCs 224, 225, and 226). In the 2020
CMS-HCC model, all Congestive Heart Failure diagnoses are effectively constrained
because they are included in a single Congestive Heart Failure HCC. In the 2024 CMS-
HCC model in consultation with clinicians the single Congestive Heart Failure HCC was
split into five HCCs to better capture the range of heart failure severity. The most severe
manifestation is left unconstrained, while the less severe split outs of the HCC are
constrained, effectively holding them together as they were under the 2020 CMS-HCC
model while CMS continues to observe clinical variation, coding, and cost patterns for
these HCCs. The newly split out HCC 227 Cardiomyopathy/Myocarditis is not
constrained, but is hierarchically excluded by the heart transplant/failure HCCs 221-226.
• HCC removals:
o HCC 47 Protein-Calorie Malnutrition. The current 2020 CMS-HCC model includes a
single marker (HCC 21) for Protein-Calorie Malnutrition. Empirical data shows that MA
reports severe malnutrition at a lower rate than FFS, moderate malnutrition at a slightly
higher rate, and mild and unspecified malnutrition and cachexia at a much higher rate.
Clinically, the more severe manifestations of protein calorie malnutrition can be useful as
a risk marker for frailty, severe illness, and late- or end-stage disease, and it is likely
correlated with poverty/disadvantaged populations. CMS explored creating two HCCs to
distinguish between severe malnutrition and diagnosis codes for mild, unspecified
malnutrition, and cachexia. However, empirical data show that coding for malnutrition is
variable. Removal of the HCC allows expenditures to flow to the well-specified
underlying conditions (e.g., cancer and HIV).
o HCC 230 Angina Pectoris. In the 2020 CMS-HCC model, HCC 88 Angina Pectoris is
one of five payment HCCs in the Heart disease group. It is at the bottom of a payment
hierarchy with HCC 87 Unstable Angina and Other Acute Ischemic Heart Disease and
HCC 86 Acute Myocardial Infarction. In the 2024 CMS-HCC model the Unstable
Angina and Other Acute Ischemic Heart Disease HCC is in the payment model.
Clinicians and empirical data support that unstable angina (HCC 87) has specific

92
diagnostic criteria, whereas angina pectoris has diagnostic criteria that can result in
coding in situations with little or no significance (e.g., patients exhibiting only chest pain
may receive this diagnosis) and diagnosis and coding may be variable. Therefore,
unstable angina is maintained in the 2024 payment model, while the more variable
manifestation is now mapped to a non-payment HCC.
• HCC 265 Atherosclerosis of Arteries of the Extremities, with Intermittent Claudication.
The Vascular HCC group was restructured (as described above). In consultation with
clinicians, payment codes are focused on peripheral arterial atherosclerosis with
ulceration, gangrene, or rest pain, as these codes indicate more severe manifestations. The
clinical characteristics of intermittent claudication are variable, with some patients
unaware they have the condition in the absence of screening. Therefore, the variation in
coding and clinical implications of this HCC suggest it is not a reliable predictor of
prospective medical expenditures.
Comment: A few commenters stated that CMS is inappropriately reliant on Principle 10 in
adopting changes to make the model more resistant to variable coding. The commenters
requested that CMS provide more transparency on the clinically specific areas impacted by the
Principle 10 updates. A few commenters stated that CMS did not indicate the extent to which the
agency weighted the tenth principle against the other nine. Multiple commenters stated that CMS
did not provide transparency explaining the tradeoffs and inter-relatedness between Principle 10
and other principles. Specifically:
• A few commenters stated that removing diagnosis codes from the model reduces predictive
power and violates Principle 2 (Diagnostic categories should predict medical expenditures).
• One of the commenters believed CMS constraining diabetes and other conditions goes
against the intent of Principle 4 (In creating an individual’s clinical profile, hierarchies
should be used to characterize the person’s illness level within each disease process, while
the effects of unrelated disease processes accumulate).
• A commenter stated CMS’ updated model violates Principle 5 (The diagnostic classification
should encourage specific coding) by paying unspecified diagnoses at the same rate as
conditions with severe acute complications, which does not encourage specific coding.
• A commenter stated the Advance Notice does not fully articulate the various approaches
considered by CMS in shifting ICD codes to different clinical categories in violation of
Principle 9 (The diagnostic classification should assign all ICD-9-CM and ICD-10-CM
codes (exhaustive classification)).
Response: CMS appreciates the feedback and concerns of the commenters.
In rebuilding the diagnostic classification for the 2024 CMS-HCC risk adjustment model,
Principles 7 (monotonicity), 8 (transitivity), and 9 (exhaustive classification) were followed. For
example, if the expenditure weights for the model did not originally satisfy monotonicity,

93
constraints were imposed to create a model that did. Empirical data and clinical assessment were
used to make tradeoffs among other principles. For example, clinical meaningfulness (Principle
1) is often best served by creating a very large number of detailed clinical groupings. But a large
number of groupings must be balanced with adequate sample sizes for each category (Principle
3). Another tradeoff is encouraging specific coding (Principle 5) versus predictive power
(Principle 2). In ICD-10 there are a number of nonspecific codes. If all of the HCCs these codes
are mapped to are included for payment, the relative cost associated with them would be
marginal and less meaningful. The inclusion of HCCs and associated diagnoses must be balanced
with maintaining or improving the predictive power of the model. CMS approached the inherent
tradeoffs involved in designing a classification system using empirical evidence on the frequency
of medical conditions in MA compared to FFS, predictive power, clinical assessment on
relatedness, specificity, and severity of diagnoses, and professional judgment on incentives and
likely provider responses to the classification system. In developing the 2024 CMS-HCC model,
CMS balanced these competing goals to achieve a risk adjustment model that would result in
payments to MA plans that fairly compensate for the higher costs of sicker enrollees while
paying less for healthier enrollees at an aggregate level.
Comment: A commenter believed CMS may have inadvertently introduced bias in the updated
model by only focusing on the coding frequency of diagnoses in MA compared to FFS for the
determination to exclude or include particular diagnoses based on Principle 10. The commenter
recommended CMS either also consider comorbidity in the MA population compared to FFS, not
consider the relative frequency of coding in MA compared to FFS, or find ways to include
incentives for providers not currently in risk arrangements to screen and treat at the same rates as
seen in MA.
Response: We respectfully disagree with the commenter that Principle 10-focused clinical
updates made to the updated risk adjustment model only focused on reviewing the coding
frequency of diagnoses in MA compared to FFS. As explained in the 2024 Advance Notice (at
47), “[f]or conditions in the model where coding in MA was highest relative to FFS, CMS
reviewed these conditions with our clinical experts for evaluation against the model principles
because we believe that this coding differential indicates conditions where there may be
discretionary coding variation.” Also, as stated above, CMS approached the inherent tradeoffs
involved in designing a classification system using empirical evidence on frequencies, predictive
power, clinical input on relatedness, specificity, and severity of diagnoses, and professional
judgment on incentives and diagnostic patterns relative to the classification system.
Comment: Some commenters stated their belief that CMS is incorrect in our analysis of the
impact of the model and that their analysis indicates the model to have a more negative impact
ranging between -3.4 to -3.7% over the whole industry.
Response: We respectfully disagree with commenters. The industry average calculated by CMS
takes into account the change in risk scores compared to the current risk adjustment model and

94
the updated risk adjustment model, and necessarily takes into account normalization. As with
every update of the risk adjustment model, the impact on each plan can vary, depending on the
clinical profiles of their enrollees.
Comment: A few commenters stated their concern about the impact of the proposed model on
Puerto Rico. All of these commenters stated that the proposed model will have the largest
negative effect on Puerto Rico due to the territory’s very high MA penetration, poverty levels,
and higher than national average prevalence rates for diabetes, mental health disorders, and
congestive heart failure. A commenter inquired if CMS evaluated how the impact correlates to
certain metrics like geography and/or evaluate the impact based on the ADI.
Response: The CMS-HCC model is a national model, including large subgroup segments that
capture national variation in costs between the segmented populations. The goal of risk adjusted
payments is to pay accurately using the appropriate relative risk for a beneficiary. There will be
variation in the impact on risk scores depending on each beneficiary’s clinical mix. All of the
model updates (i.e., underlying data updates, denominator update, and ICD-10 reclassification)
contribute to changes in the relative costs of conditions, and therefore changes to the resulting
risk scores. Beneficiary risk scores or plan average risk scores may change depending individual
beneficiary’s combination of diagnoses or the clinical profile of a plan’s enrollee population.
As discussed above, the updated model improves predictive accuracy and helps ensure that
higher payments are available to plans that serve beneficiaries with greater health care needs
(refer to the predictive accuracy information provided above). Conditions in the model are used
as predictors of relative costs, not as direct reimbursement for each condition. As intended, the
model ensures that plans that enroll higher need beneficiaries receive higher payments, and,
therefore, we do not agree that the updated model will disproportionately negatively affect
beneficiaries depending on their region.
We understand that geographically Puerto Rico has a high percentage of beneficiaries with risk
scores calculated using the full benefit dual segment. A previously stated, CMS has observed
that, on average, predicted risk for dually-eligible populations are higher than non-dually-eligible
enrolled beneficiaries. As discussed above, the risk score trend for dually-eligible beneficiaries is
higher than the trend for non-dually eligible beneficiaries. As noted in another response, the MA
risk score trend (i.e., average growth in risk scores for the payment year) for dually eligible
beneficiaries is 4.67 percentage points higher than it is for non-dually eligible beneficiaries and
the risk score trend difference for Puerto Rico is even greater. As discussed in more detail in a
later response in this section, it is imperative to consider the MA risk score trend in concert with
the impact of risk adjustment policy proposals to accurately predict payment impacts in the
following year. When the risk adjustment model/normalization and the MA risk score trend are
taken into account, dually-eligible risk scores are less impacted by the risk adjustment changes.
When considering payment, the full scope of contributing factors must be considered. MA plans
submit bids to CMS that request the total revenue needed to cover the expected per beneficiary

95
costs of their enrollee population. The purpose of the model is to calculate risk scores (that are
used in calculating payments made to plans) to take into account differences in expected costs
for their enrollees and to increase or lower payment based on the relative expected costs. Risk
adjustment is used to adjust plan bids and calculate payments based on health status and
demographic characteristics such that plans are paid more for beneficiaries predicted to have
higher costs due to increased risk. Further, individual coefficients do not represent complete
costs for expected expenditures related to a condition, but only the average increase in the overall
predicted costs for a beneficiary with that condition relative to other conditions used for payment
in the model. Rather, the total relative cost of a beneficiary, or a group of beneficiaries, is
represented by the total risk score.
Comment: Commenters stated their concern that the proposed model will negatively impact
providers engaged in value-based payment models. A commenter noted that many contracts
between plans and their provider partners are based on existing risk models. The commenter
noted the burden that exists by needing to revise these contracts. Some commenters believed the
proposed model may result in physician organizations leaving MA for FFS. A few commenters
noted that the proposed model’s impact on the MA industry will negatively impact what they
believe is a national provider shortage.
Response: CMS thanks the commenters for expressing their concerns. Per section
1854(a)(6)(B)(iii) of the Act, CMS is prohibited from interfering in payment arrangements
between MA organizations and providers with which they contract by requiring specific price
structures for payment. The purpose of the risk adjustment model is to predict the overall relative
expected expenditures for beneficiaries for purposes of paying MA organizations accurately and
fairly for the relative expected costs for the enrollees in their plans. MA organizations in turn
develop provider networks and negotiate payment arrangements with participating providers for
the delivery of covered services to enrollees.
MA organizations are contractually required to cover all Medicare Part A and Part B services
(subject to limited exclusions), maintain adequate networks, and provide quality care. They are
responsible for determining their own revenue needs to cover these services. An updated risk
adjustment model is intended to more appropriately pay plans that are enrolling a sicker
population. In paying plans a capitated payment, CMS contracts with MA organizations for them
to provide coverage of – by furnishing, arranging for, or making payment for – these benefits.
The nature of the MA program, by using capitated payments, allowing MA plans to use a portion
of savings when they bid below the benchmark to furnish additional benefits, and transferring
full financial risk to MA plans, incentivizes MA organizations to develop cost efficiencies in
care provision. Reducing morbidity and mortality by catching early stages of disease in an
inherent expectation of a capitated managed care system.
Section 1852 of the Act requires MA plans to cover Medicare Part A and B benefits (subject to
limited exclusions) for their enrollees and that when the MA plan uses a network of providers

96
and limits coverage to those providers, the MA plan must ensure that covered benefits are
available and accessible to enrollees. These changes in the CMS-HCC risk model used for risk
adjusting payments to MA plans do not limit or change these requirements related to coverage.
We expect that MA organizations will renegotiate or revise the payment arrangements they have
with their contracted providers as necessary to ensure that the MA plan continues to make
benefits available and accessible for enrollees.
The risk adjustment model is not intended to incentivize (or disincentivize) any particular care
modality. This is illustrated by, for example, not weighting diagnoses by site of care. Another
example is allowing costs to flow to demographic variables, which allows some portion of plan
payments to be paid regardless of disease state and thereby provide funds for a wide range of
prevention and intervention approaches, as well as to cover treatment of acute and lower-severity
chronic conditions not included in the risk-adjustment model. Finally, and to reiterate, by using
more recent data in calibrating the model, coefficients are recalculated, and conditions that might
be relatively more costly than they were before will result in higher risk scores for beneficiaries
with such conditions.
Comment: A few commenters stated their view that it is incorrect to determine that coding
differences between MA and FFS are driven by inappropriate coding.
Response: Discretionary coding involves conditions that are diagnosed and coded inconsistently
across providers and plans. Including conditions in the model where there is variation in their
coding can lead to distortion of the marginal costs estimated by the model, reducing the ability of
the HCCs in the model to predict stable costs and accurately predict those costs in alignment
with the severity of the condition. Diagnosis codes that are subject to discretion are not
necessarily or by definition an indication of inappropriate coding.
Comment: Some commenters recommended different methods for updating the CMS-HCC risk
adjustment model, including making updates on a more regular basis, adding drug utilization to
the model, using more sources of data (e.g., home health and skilled nursing facilities), using a
concurrent model, and calibrating a model using MA encounter data. A number of commenters
recommended social drivers be incorporated into the risk adjustment model. Some commenters
offered recommendations on ways to improve the risk adjustment model by incorporating
additional factors that could improve prediction of the relative costs of MA enrollees by
accounting for social risks. Some commenters recommended CMS integrate all Z-codes, Z55
through Z65, into the HCC risk adjustment model. Other examples of recommendations for
future risk adjustment models include:
• Aligning coding expectations between MA and FFS. This includes the FFS program
rejecting claims until an appropriate diagnosis code is included;
• Adding a frailty measure to the risk adjustment model; and
• Applying a single coefficient to conditions with wide ranges of complexity.

97
Response: CMS thanks commenters for their suggestions and feedback on updating the CMS-
HCC risk adjustment model. CMS is committed to ensuring the risk adjustment model continues
to perform well in predicting relative risk.
Comment: Some commenters questioned if the updated risk adjustment model will affect lines of
business outside of Medicare Advantage such as the ACO Reach and Medicare Shared Savings
Program.
Response: The Medicare Shared Savings Program and certain CMMI models have incorporated
the CMS-HCC risk adjustment model into their financial methodologies. CMS is considering the
implications of these changes to the CMS-HCC risk adjustment model for these initiatives.
Comment: A few commenters recommended CMS consider the impact the updated model will
have on one or multiple of the following areas: Health Provider Shortage Areas (HPSA),
Medically Underserved Areas (MUA), high Area Deprivation Index (ADI) locations, high Social
Vulnerability Index (SVI) locations, and/or Opportunity and Enterprise Zones.
Response: CMS thanks the commenters for their recommendations and feedback.
The CMS-HCC model is a national model, including large subgroup segments that capture
national variation in costs between the segmented populations. The goal of risk adjusted
payments is to pay accurately using the appropriate relative risk for a beneficiary. There will be
variation in the impact on risk scores depending on each beneficiary’s clinical mix. As
previously discussed, the model is not intended for provider reimbursement at the service level.
Therefore, the risk adjustment model should not have implications on provider availability.
Regarding vulnerable populations, as previously stated the model is segmented by dual-eligible
status and includes demographic variable to estimate relative risk. Risk scores for dual-eligible
beneficiaries continue to be higher than non-duals on average.
Comment: A commenter wanted to know if the proposed model will use CY 2023 diagnosis
codes.
Response: CMS will use the updated model to calculate risk scores for 2024 payment, using
diagnoses codes from 2023 dates of service.
Comment: One commenter asked CMS to provide logic on the inclusion of some “P” and “Q”
ICD-10 newborn codes within the proposed model.
Response: Certain P and Q codes were moved from nonpayment in the Newborn disease group
to payment in condition-specific disease groups in the updated model. ICD-10 coding guidance
specifies that they may be used regardless of age. P codes are for conditions that originate in the
perinatal period, which may continue throughout a patient’s life. Q codes are for congenital
malformations, deformations, and chromosomal abnormalities, which although present at birth
may not be identified until later in life. In the updated model, these codes are remapped for

98
clinical cohesion to the respective disease-related HCC in the body system, parallel to codes for
the condition from other ICD-10 chapters (i.e., non-congenital forms, not originating in the
perinatal period). Thus, these P and Q codes are added to the model if the condition warrants
inclusion as payment.
Comment: A few commenters stated that CMS made a technical error in Attachment VI, Table
VI-1 related to the Note on Neurology HCCs and disease interactions.
Response: These commenters are correct. The CY 2024 Advance Notice has a technical error in
the table. Under footnote 2 of Attachment VI, Table VI-1, Neurological is defined as HCCs 108-
192; HCCs 195-199, but it should state HCCs 180-192, 195, 196, 198, 199. This has been
corrected in this document. We appreciate the commenters identifying this.
Comment: Several commenters stated either that the proposed risk adjustment model does not
meet the actuarial equivalence requirement in Section 1853(a)(1)(c)(i) of the Social Security Act
or were concerned that the proposed model did not meet the actuarial equivalence requirement
based on the documentation provided in the Advance Notice. A commenter noted their belief
that in order to fulfill its statutory mandate to ensure actuarial equivalence, CMS must only
assess FFS treatment costs and associated diagnoses when updating the model used for MA
payment, and that the use of other criteria, are not valid unless those changes improve the
model’s ability to predict FFS treatment cost. Commenters identified specific diagnoses that they
stated were excluded from the proposed model, which they believe offers evidence that the
proposed model violates this statutory requirement.
Response: Section 1853(a)(1)(c)(i) of the Social Security Act instructs CMS to adjust the
payments made to MA organizations “for such risk factors as age, disability status, gender,
institutional status, and such other factors as the Secretary determines to be appropriate,
including adjustment for health status . . . so as to ensure actuarial equivalence.” It also
authorizes CMS to “add to, modify, or substitute for such adjustment factors [i.e., age, disability
status, gender, etc.] if such changes will improve the determination of actuarial equivalence.”
The 2024 CMS-HCC model satisfies the statutory requirement of actuarial equivalence because,
within the limitations of such a model, it accurately predicts variations in cost, as discussed at
length above. But the statute does not require CMS to show that every single change made from
the previous CMS-HCC model improves its predictive accuracy. CMS retains the discretion and
authority to design the 2024 CMS-HCC payment model so as to achieve actuarial equivalence,
just as earlier payment models were designed to do. Those earlier payment models do not limit
the scope of the Secretary’s authority today.
The Balanced Budget Act of 1997, the initial statutory requirement to implement risk adjustment
based on health status in the MA program, directed the Secretary to implement a risk adjustment
methodology that accounts for variations in per capita costs based on health status and other
demographic factors no later than January 1, 2000. As required by 1853(a)(3)(A), the risk

99
adjustment methodology was to be submitted to Congress in a report that included an evaluation
of the method by an outside, independent actuary of the actuarial soundness of the proposal. The
report that was submitted to Congress in 1999 provided a foundation for the ten principles that
were expanded on in a 2000 report to Congress that CMS still uses today to guide risk
adjustment model development.
17
Each iteration of the risk adjustment model, including the
2024 CMS-HCC model, has maintained or improved upon the previous payment model’s ability
to predict variation in per capita spending across key subgroups of beneficiaries.
18
CMS is obligated to release a report to Congress every three years with information on how
revisions to the risk adjustment model impact the predictive ratios for groups of enrollees in MA
plans by predicted cost and groups defined by the number of chronic conditions of enrollees.
Because CMS has not uniformly collected cost information for beneficiaries enrolled in the MA
program, the report is developed with data on Medicare FFS enrollees, which are the same data
used to calibrate the model. The next report will be released with findings from the 2024 CMS-
HCC model in 2024. In response to comments from stakeholders, predictive ratios are provided
for the 2024 CMS-HCC model overall on page 72 and by model segment in Attachment VIII
Tables VIII-5 to VIII-11.
One commenter wrongly asserts that “under the policies proposed in the Advance Notice, CMS
would fail to satisfy its obligation to ensure actuarial equivalence, as the proposed model does
not appear to be based on an assessment of FFS costs in order to generate appropriate
coefficients to support appropriate MA payments.” The 2024 CMS-HCC model does account for
FFS cost to generate appropriate coefficients. Per-capita payments to MA plans reflect the
relative cost experience in Medicare FFS for a beneficiary population modeled by reference to
demographics, diagnoses, and other factors CMS selects. As discussed above, the 2024 CMS-
HCC model accurately predicts variation in FFS costs.
One commenter implies that CMS must make decisions to update the risk adjustment model
based only on “analysis of whether removing these codes will mean the model more accurately
predicts costs associated with treating certain conditions in FFS” and erroneously claims that “In
order to fulfill its statutory mandate to ensure actuarial equivalence, CMS must assess FFS
treatment costs associated with diagnoses, not use of codes.” The Secretary is provided
discretion in how to adjust for health status. In addition, as discussed before, the risk adjustment
model accurately predicts variation in per capita cost based on health status as intended.
Diagnosis codes from claims or encounter data are used as a measure of health status to predict
variation in cost because those data are the most practicable for developing and implementing a
payment system at the scale required by the Medicare program. An individual diagnosis code or
17
See 1999 Report to Congress: https://www.cms.gov/medicare/health-
plans/medicareadvtgspecratestats/downloads/rtc_riskadjusters1999.pdf, and 2000 Report to Congress: Diagnostic Cost Group
Hierarchical Condition Category Models for Medicare Risk Adjustment
18
For example, see the December 2021 Report to Congress

100
HCC is not a sufficient, nor the only, indicator of a beneficiary’s health status. CMS does not
believe that the reference to health status in Section 1853(a)(1)(C)(i) requires CMS to adjust
payments to MA organizations for the costs they incur for specific diagnoses on submitted
claims or encounter data, in relation to FFS or otherwise. The predictive accuracy for a specific
condition in the model is not a valid criterion on which to assess the model’s actuarial
equivalence because expected relative costs based on health status is ultimately measured by all
conditions and factors in the model used to calculate risk scores.
The statute provides the Secretary discretion in how to account for health status when calculating
payments that reflect the risk of the enrollee, and this extends to the individual HCCs included in
the model. CMS follows the ten principles laid out in the 2000 Report to Congress to group
diagnosis codes into HCCs and select which HCCs are included in the model.
19
These principles
balance clinical considerations, such as creating clinically meaningful groupings of diagnoses
and ensuring only well-specified diagnoses are included in the model, and the predictive
accuracy of the model as measured by the ability of the model to predict accurately across groups
of beneficiaries. As discussed throughout the Rate Announcement, the 2024 CMS-HCC model
accurately predicts variation in expenditures (per capita cost) across groups of beneficiaries.
There is no meaningful difference in the accuracy of each model for groups of beneficiaries by
decile of predicted risk using the beneficiary sample specifically applicable to each model, CMS’
standard measure of accuracy. However, when compared using the same beneficiary sample (i.e.,
2019 beneficiaries, 2018 diagnoses) for both models, the 2024 CMS-HCC is more accurate by
decile of predicted risk than the 2020 CMS-HCC model. The 2024 CMS-HCC model more
accurately reflects MA plan’s expected experience because it was developed with more recent
data. In general, the model predicts higher expenditures for people who have higher actual
predicted risk and less for people who have lower actual predicted risk. The model accurately
predicts total expenditures regardless of whether or not a condition is included in the model.
Spending associated with conditions not included in the model is allocated to other variables in
the model, such as the demographic factors, count variables and conditions in the model
associated with the removed conditions. To the extent that there are changes in the predicted risk
for certain subgroups of beneficiaries, or beneficiaries with certain conditions, those changes can
occur for multiple reasons. The model includes updates to the underlying data years, the
denominator year, and reclassification for ICD-10. As such, relative changes are driven by more
recent enrollment, treatment/utilization, and cost patterns, in addition to the reclassification.
If CMS were not paying MA organizations appropriately for the health status of the beneficiaries
they enroll, many MA plans would not be competitive with the FFS program and enrollment
would likely stagnate. The exact opposite has occurred. Analysis of CMS program statistics
shows that between 2014 (the first year of the last major clinical revision to the risk adjustment
model) and 2021, enrollment in MA grew by 70 percent whereas enrollment in FFS has declined
19
2000 Report to Congress: Diagnostic Cost Group Hierarchical Condition Category Models for Medicare Risk Adjustment.

101
by seven percent. Enrollment growth among beneficiaries who are dually enrolled in Medicare
and Medicaid, who on average have higher medical cost and greater health needs, has also been
higher, increasing by more than 125 percent from 2.7 million in 2014 to 6.1 million in 2021,
whereas dual enrollment in FFS has declined by 22 percent from 7.2 million to 5.6 million. Dual
eligible enrollees made up more than one in five (22.1 percent) of MA enrollees in 2021, similar
to the proportion in FFS (19 percent). As enrollment in the program has grown, the number of
organizations offering MA plans has increased, the number of plans offering supplemental
rebates has increased, and plans are profitable. Over the last ten years (2014 – 2023) the average
margin included in plan bids is 4.4 percent while the ratio of the average benchmark to the
average plan bid to provide standard Medicare benefits has increased. In 2014, the adjusted
benchmark was on average 114 percent of the standardized bid, and in 2023 the adjusted
benchmark was on average 152 percent of the standardized bid. The 2024 CMS-HCC model
maintains the same risk adjustment system based on variation in health status that has supported
a robust MA program. The commenters provided no specific evidence in their comments that the
payments they will receive under the 2024 CMS-HCC model are not sufficient to meet their
obligation to provide benefits to the beneficiaries who enroll in their plan.
Comment: One commenter suggested that the documentation standards in Medicare Advantage
differ from the documentation standards in traditional Medicare (i.e., Parts A and B), and that
this difference causes the CMS-HCC risk adjustment model to violate the actuarial equivalence
requirement in Section 1853(a)(1)(c)(i) of the Social Security Act.
Response: The argument, that differing documentation standards between MA and FFS cause the
risk adjustment model to systematically underpay MA organizations in violation of the actuarial
equivalence provision of Section 1853(a)(1)(c)(i) of the Social Security Act, incorrectly
presumes that there are two different standards. As we recently explained, FFS and Medicare
Advantage have the same documentation standard for diagnosis coding. Policy and Technical
Changes to the Medicare Advantage Program for Years 2020 and 2021, Final Rule, 88 Fed. Reg.
6643, 6652-53 n.31, 6657-59 (February 1, 2023). Both programs require all reported diagnoses
to be substantiated by documentation in the beneficiary’s medical records. Moreover, the
commenter is wrong to suggest that MA data is “audited” while FFS data is “unaudited,” or that
coding errors are condoned in FFS. In each program there is i) an identical documentation
standard, ii) an obligation to work in good faith towards compliance with that standard, iii) some
CMS auditing of compliance, and iv) coding errors that nonetheless escape detection. See id. at
6658 n.40, 6659. This has been true since the beginning of the Medicare Advantage program,
and remains true today. There is no reason to presume that the error rate in diagnosis coding in
FFS is meaningfully higher than the error rate in Medicare Advantage.
CMS regularly informs Congress about the use of the CMS-HCC risk adjustment model,
calibrated on FFS data, for calculation of MA payments. Congress has been well informed about
CMS’ implementation of risk adjustment since the advent of the Medicare Advantage program,
often requiring reporting or amending the relevant statutory provisions, without any indication

102
that Congress believed CMS was falling short of the statutory requirement of actuarial
equivalence in payments to MA insurers. To the contrary, Congress has made a holistic
determination that payments to MA organizations based on the CMS-HCC payment model are
higher than they ought to be by at least 5.9%. The statutory adjustment leaves the agency with
asymmetric discretion: CMS is free to find that a larger reduction in payments should be made,
but not a smaller one.
That is not to say that the risk adjustment model achieves perfect accuracy. As noted previously,
the model predicts variation in expenditures for groups of enrollees based on their expected
costs, not expenditures at the individual level.
20
Nevertheless, accuracy is achieved at the
aggregate level, and as we recently explained, the arguments that FFS errors create systematic
underpayment do not adequately account for the offsetting effects of FFS under-coding and the
increased costs associated with FFS over-coding. 88 Fed. Reg. at 6659.
21
In fact, most independent experts have found that if anything, MA organizations are significantly
overpaid even after application of the minimum 5.9% coding pattern adjustment that has been in
place since 2019. MedPAC, for example, estimated that MA risk scores for 2020 were 9.5%
higher than FFS risk scores for similar FFS enrollees (3.6% higher after applying the 5.9%
coding pattern adjustment), resulting in nearly $12 billion in excess payments to MA plans.
MedPAC, Report to the Congress: Medicare Payment Policy 440 (March 2022). Other
independent studies have reached similar findings. See id. at 440-41 (citing studies). Further,
some independent experts estimate that these differentials are increasing. Very recently,
MedPAC estimated that for 2021, MA risk scores were 10.8% higher than FFS risk scores for
similar FFS enrollees (4.9% higher after applying the 5.9% coding pattern adjustment), resulting
in nearly $17 billion in excess payments to MA plans.
22
MedPAC projects that excess payments
to MA plans will reach $23 billion in 2023 if MA coding patterns remains the same as in 2021.
23
CMS is required to operate the MA program and publish payment rates each year. The agency
must therefore act on the basis of the best information available to it at the time, within the
bounds of the discretion afforded to it by Congress; it cannot wait for more complete
information. The history of the CMS-HCC payment model, which has relied on the same
documentation standard and been calibrated on the same data for many years; the amendments to
the Medicare statute indicating a congressional determination that the model was paying MA
20
See UnitedHealthcare, 16 F.4th at 874 (“The model uses data from a large pool of beneficiaries (full sample sizes over 1 million for the CMS-
HCC models) to estimate predicted costs on average for each of the component factors (e.g., age-sex, low income status, individual disease
groups). Using regression analysis on such a vast data sample mutes the effect of individual errors in traditional Medicare data, so long as errors
are not so widespread or systemically skewed as to raise or lower the values of particular relative factors.”) (internal citations and quotation
marks omitted).
21
See also UnitedHealthcare, 16 F.4th at 888 (discussing the effects of underreporting and extraneous expenditures within the
FFS data).
22
MEDPAC, REPORT TO THE CONGRESS: MEDICARE PAYMENT POLICY xxiv, 324-25, 355 (March 2023); LUIS SERNA & ANDY
JOHNSON, MEDPAC PRESENTATION Slides 11, 13 (Jan. 12, 2023), https://www.medpac.gov/wp-
content/uploads/2023/01/MedPAC-MA-status-report-Jan-2023.pdf.
23
Id.

103
organizations more than they ought to be paid; and the weight of expert analysis suggesting that
the model continues to overcompensate those insurers despite the mandatory payment reduction,
all demonstrate that CMS acts within its statutory authority in continuing to operate the risk
adjustment model on FFS cost and diagnosis data while making only the statutory minimum
payment reduction.
Comment: A commenter challenged CMS authority to implement changes to Medicare
Advantage payment policy through the Advance Notice and Rate Announcement. Several
commenters contested CMS authority to make any changes to the Part C risk adjustment model
generally. The commenters argued that what CMS proposes makes fundamental changes to the
MA program that are unprecedented and therefore exceeding the executive branch’s authority to
implement, and that the proposed changes should be implemented through notice and comment
rulemaking.
Response: The commenter mischaracterizes the proposed changes to payment in the 2024
Advance Notice. The proposed changes are not unprecedented. They are ordinary and routine.
The fundamental structure of the Medicare Advantage program remains intact. CMS will
continue to pay MA plans a risk adjusted amount based on the MA plan’s bid to provide
Medicare Parts A and B benefits through adequate provider networks; in addition, for MA plans
that bid under the benchmark, CMS will provide the MA plan a portion of the amount by which
the benchmark exceeds the bid as the MA rebate, to be used to furnish supplemental benefits
(including reductions in cost sharing) or to pay Part B or Part D premiums for their enrollees.
CMS pays MA organizations rebates to cover additional benefits as an incentive for the MA
organization to provide Part A and Part B services for less than the cost to the FFS program, as
measured by the MA benchmark applied in each plan’s bid. By statute, the plan-specific rebate
amount is based on the MA contract’s star rating and the MA organizations ability to cover Parts
A and B benefits for less than the applicable benchmark rate. This Advance Notice and Rate
Announcement does not alter the payment structure; rather it updates the benchmark rates and
other aspects of MA payment calculation.
CMS expects the net impact to aggregate MA payments between 2023 and 2024 as a result of all
changes finalized in this Rate Announcement to increase MA payments by 3.32 percent.
24
CMS
anticipates stable premiums and benefits for beneficiaries in 2024, as seen previously in years
with comparable updates.
The updates made to the CMS-HCC Part C risk adjustment model as finalized in the 2024 Rate
Announcement are not unprecedented. They are similar in scope to risk adjustment model
24
HHS and the GAO have also both identified high amounts of improper payments in the MA program. 88 Fed. Reg. at 6645,
6653. In fiscal year (FY) 2021 for example (based on calendar year 2019 payments), we calculated that CMS made over $15
billion in Part C overpayments, a figure representing nearly 7 percent of total Part C payments. Id. at 6645 n.7 (citing HHS, FY
2021 HHS Agency Financial Report, pg. 211. See https://www.hhs.gov/sites/default/files/fy-2021-hhs-agency-financial-
report.pdf
104
changes proposed and finalized previously through the Advance Notice and Rate Announcement.
The 2024 CMS-HCC model changes are a combination of routine data updates (e.g., updating
the years of data used when calibrating the model) and clinical updates to the Hierarchical
Condition Categories (HCCs) that were required to develop a model using the ICD-10 diagnosis
codes implemented in 2015. For example, CMS recalibrated the MA risk adjustment model with
updated data years and/or made clinical revisions to the risk adjustment model in payment years
2007, 2009, 2013, 2014, 2017, 2019, and 2020. The 2021 Report to Congress provides the
history of the models and changes over the years. A major clinical revision, including the
removal of HCCs for dementia based on Principle 10, was completed for the models that were
implemented for the Program of All-Inclusive Care for the Elderly (PACE) starting in PY 2012
and phased in for MA starting in PY 2014. Updates to the data years–pairwise years of diagnosis
and cost information–to adjust the model coefficients to account for more recent patterns of
health status and cost in the FFS Medicare program are more frequent and last occurred with
model update for PY 2019.
Although requested and suggested by commenters, CMS is not required to use rulemaking in the
Federal Register to adopt a new risk model for MA payment. Section 1853(b)(2) directs that
CMS determine and announce the annual MA capitation rate and the risk and other factors to be
used in adjusting such rates under section 1853(a)(1)(C) for MA payments in each contract year.
Each year, in advance of the final announcement of the rates and risk and other factors, CMS
must “provide for notice to [MA] organizations of proposed changes to be made in the
methodology from the methodology and assumptions used in the previous announcement and
shall provide such organizations an opportunity (in 2017 and each subsequent year, of no less
than 30 days) to comment on such proposed changes.” CMS fully complied with that required
process: the CY 2024 Advance Notice described the changes in methodology and assumptions
for setting the capitation rates and described how CMS developed the risk factors and specific
coefficients for adjusting those capitation rates for age, disability status, gender, institutional
status, eligibility for Medicaid, and health status. This notice and comment process has been in
place since 1985 when CMS first began contracting with private health plans on a capitation
basis, under procedures set forth in section 1876(a)(1)(F) of the Act. All major changes in
payment policy have been implemented through this process. For example, when section
1853(a)(3) was first implemented in 2000 with the initial risk adjustment methodology
developed by CMS, this initial methodology was implemented through an Advance Notice and
Rate Announcement. All subsequent changes to the risk adjustment methodology, including the
establishment of a budget neutrality factor to make risk adjustment payments budget neutral to
the prior demographic-based payments, used in the initial years of CMS-HCC model, and the
subsequent decision by CMS to phase out budget neutrality (which was ratified by Congress in
the DRA) have all been implemented through the section 1853(b) process. Congress has on
several occasions ratified in statute methodologies that CMS established through this section
1853(b) process (e.g., the initial phase in of risk adjustment, the plan to phase out budget
neutrality, providing separate adjustments in the risk adjustment model for dual eligible

105
individuals). Furthermore, section 1853(b)(2) requires only a 30-day comment period, which we
believe is an indication that this period is sufficient for stakeholders to review the changes
proposed in the Advance Notice and provide comment. Prior to the Securing Fairness in
Regulatory Timing Act of 2015 (SFRTA) (Pub. L. 114-106), which amended section 1852(b) to
require that the Advance Notice be issued 60 days before the issuance of the Rate
Announcement, the statute did not require that the comment period be a minimum length.
Although the 21st Century Cures Act required, at section1853(a)(1)(I)(iii), a 60-day comment
period for changes to the risk model under section 1853(a)(1)(I), that comment period does not
apply to future model updates made by the Secretary under the authority granted in Section
1853(a)(1)(C).
Comment: Several commenters stated that they are directionally aligned with CMS’ decision to
update the risk adjustment model based on more current underlying data, updating the
denominator, and some clinical revisions based on ICD-10, but were specifically opposed to the
clinical revisions to select conditions made under Principle 10.
Response: Commenters conflated changes to the model that were exclusively based on Principle
10 and changes that were based on Principle 10 in conjunction with other model principles. The
transition to ICD-10 required CMS to reevaluate all conditions (those ICD-10 diagnoses that
were included in the mapping to payment HCCs in the current 2020 CMS-HCC model as well as
all diagnoses not mapped to payment HCCs in the 2020 CMS-HCC model) against all of the
model principles. Between the 2020 CMS-HCC model and the 2024 CMS-HCC model, 2,236
ICD-10 diagnosis codes no longer map to the model for payment and 209 were added.
Additional information for the 2,236 codes that newly map to non-payment HCCs in the 2024
CMS-HCC model is provided below. These diagnosis codes generally fall into one of six
categories:
1. Subsequent Encounter (codes ending in D) – 6 percent of the diagnosis codes that newly
map to non-payment HCCs under the 2024 CMS-HCC model. Subsequent encounter
codes represent less intensive follow-up treatment. While the cost from subsequent
encounters are included in the model, the diagnosis codes indicating they are from a
subsequent encounter were removed because they do not reliably or consistently predict
meaningful costs. The diagnosis code on the initial encounter is more reliable and
predictive. Costs from these encounters will be attributed to other conditions on the
encounter that are in the model, demographic factors and count variables.
2. Sequela (codes ending in S) – 40 percent of the diagnosis codes that newly map to non-
payment HCCs under the 2024 CMS-HCC model. The initial encounter diagnosis codes
for these conditions that are being actively treated and predict ongoing and prospective
costs still map to payment HCCs. Sequela codes are for late effects of a condition and
indicate variable conditions that can be acute and/or require less follow up medical care.
Because ICD-10 guidelines require the actual late effect (e.g., pain) to be coded
separately, the sequela codes, which are non-specific, are excluded from payment HCCs.
106
Costs from these encounters will be attributed to other conditions on the encounter that
are in the model, demographic factors and count variables.
3. Drug-induced – 8 percent of the diagnosis codes that newly map to non-payment HCCs
under the 2024 CMS-HCC model. ICD-10 codes for drug-induced conditions can be
secondary to poor quality of care related to drug-induced conditions or drug-intensive
styles of care. Re-mapping these conditions to a non-payment HCC focuses the costs on
underlying health status risks rather than the side effects of health care, and because drug-
induced conditions are often temporary/reversible and are unlikely to predict prospective
costs (i.e., the condition is often resolved by stopping the drug). Beneficiaries with a
persisting drug-induced condition are ultimately coded with a diagnosis describing their
condition that is not labeled as “drug-induced.” Thus, expenditures associated with drug-
induced conditions will be reflected in costs modeled for the underlying health condition
prompting drug treatment. For example, costs of chemotherapy and its complications will
load onto associated cancer diagnoses. Only a few codes (16 unique codes and the drug
or chemical induced diabetes E09- code set) were removed from payment primarily
because they are drug-induced. Other drug-induced codes were made nonpayment both
because they are drug-induced and due to another clinical/empirical consideration (for
example, overprediction of the costs for beneficiaries with those conditions in the 2020
CMS-HCC model, clinical considerations based on consulting physicians’
recommendation, or the non-drug-induced version of the condition was also moved to
nonpayment).
4. Complication of Medical Care – 16 percent of the diagnosis codes that newly map to
non-payment HCCs under the 2024 CMS-HCC model. The goal of risk adjustment is to
use health status to predict the relative additional costs of treating the beneficiary, and not
the side effects of medical treatment, which are not reliable predictors of future costs. For
example, in the 2024 CMS-HCC model, relative costs associated with an infection as a
complication of care will load onto the underlying condition prompting the medical care.
Claims data do not allow for determining whether a complication is avoidable. Excluding
complications, such as a surgery performed on the wrong side of the body, avoids using
diagnoses that result from poor quality of care, or more aggressive, procedure-oriented
care. Serious complications would be accounted for by the specified conditions that are
included in the payment model, which would be coded in addition to or instead of
complications codes, especially if they persist in the long-term.
5. Principle 10 only – 3 percent of the diagnosis codes that newly map to non-payment
HCCs under the 2024 CMS-HCC model. These diagnosis codes were removed after
clinical assessment, conducted after the codes were identified for additional clinical
review. The list of HCCs identified for further review is in the subsequent comment
summary and response. As noted before, the clinical panel provided insight and
recommendations related to the criteria used to evaluate and treat conditions (e.g., lab
findings, test results, physical exams, medications, medical interventions, etc.);

107
specificity of diagnoses; potential for variable coding for certain diseases or disease
groups; treatment practices; manifestations of conditions in different populations (e.g.,
aged vs. disabled; non-dual vs. full-benefit; dual vs. partial-benefit dual); disease severity
and implications for medical burden; clinical face validity (i.e., whether the condition is
consistent with the relative costs associated with it) and interpretation of empirical
results; clinical similarities and differences between specific diseases (e.g., Crohn’s
disease and ulcerative colitis); relationship of acute and chronic versions of diseases (e.g.,
acute hepatitis C and chronic hepatitis C); and implications for predicted costs.
6. Other – 28 percent of the diagnosis codes that newly map to non-payment HCCs under
the 2024 CMS-HCC model. This category indicates decisions were made based on a
combination of clinical and empirical reasons that align with model principles such as
clinical meaningfulness (Principle 1), overprediction (Principle 2), diagnostic specificity
(Principle 5), and concerns about coding intensity or clinical discretion (Principle 10.)
As can be determined from the distribution of the reasons for exclusion from the 2024 model, a
significant majority of diagnosis codes (97 percent) were excluded for reasons other than
Principle 10. As noted in the 2024 Advance Notice Fact Sheet, analysis of the most recent data
suggests fully implementing the 2024 CMS-HCC model would reduce MA risk scores by 3.12
percent. A majority of the -3.12 percent impact is due to changes other than those based only on
Principle 10. We calculate the marginal impact of the changes based only on Principle 10 to
be -0.55 percent (e.g., Principle 10 only changes account for -0.55 of the total -3.12 percent
impact).
A list of conditions that commenters were concerned about excluding diagnosis codes from and
the rationale for removing those diagnosis codes is provided in response to other comments in
this section.
Comment: Several commenters stated that the changes to the Part C risk adjustment model
proposed in the 2024 Advance Notice based solely on Principle 10 are intended to reduce
payments to MA organizations because of differences in coding patterns between Medicare
Advantage and FFS and therefore are duplicative of the coding pattern adjustment. Commenters
indicated those changes are not authorized by section 1853(a)(1)(C) of the Social Security Act
and one commenter noted that such changes would require CMS to implement a model based on
MA encounter data.
Response: We disagree. Section 1853(a)(1)(C)(ii) of the Social Security Act requires the
Secretary to reduce payments to MA organizations by at least 5.9% to account for “differences in
coding patterns between Medicare Advantage plans and providers under part[s] A and B.” As
explained above, per-capita payments to MA plans reflect the relative cost experience in
Medicare FFS for a beneficiary population modeled by reference to demographics, diagnoses,
and other factors CMS selects. The per-capita payments initially calculated by the CMS-HCC
model are then reduced in compliance with section 1853(a)(1)(C)(ii). But the enactment of that

108
provision did not diminish the Secretary’s discretion or authority to design the payment model.
And as discussed above, the 2024 CMS-HCC model accurately predicts variation in FFS costs,
just as the 2020 CMS-HCC model did when it was published.
The removal of certain codes from payment HCCs and constraints on the coefficients of certain
HCCs are not the same as the coding pattern adjustment required by section 1853(a)(1)(C) and
do not address the same thing. The adjustment mandated by section 1853(a)(1)(C)(ii) is applied
to each beneficiary’s risk score at every MA plan, which reflects that provision’s focus on coding
pattern differences at a general, program-wide level. Specifically, section (a)(1)(C)(ii) addresses
the incentive for all MA plans to identify more valid, supported codes on all HCCs, and therefore
report more diagnoses (which we do not assume to be inaccurate when evaluating coding pattern
differences between FFS and MA). By reducing each individual risk score by a specified
percentage, the coding pattern adjustment corrects for overall, net differences between MA and
FFS coding. Our process in applying Principle 10 and looking at how often certain codes
appeared within the universe of diagnosed conditions for Medicare beneficiaries in FFS and in
the MA program did not look at general, program-wide differences on all HCCs, but rather at
whether certain differences on particular codes warranted further review to ensure that they are
credible predictors of variation in per capita costs. In circumstances where there is discretion in
coding, beneficiaries with different profiles are attributed with the same HCC and the model’s
ability to differentiate higher-than-average relative costs accurately is diminished.
Principle 10 is well grounded and appropriate to use because it focuses on ensuring that codes
used in the model are clinically and empirically credible predictors of future costs. Because the
coding of additional diagnoses directly increases the payments made to MA organizations,
diagnoses for which the documenting and reporting involves a substantial amount of discretion
present a particular risk to the integrity of the payment model.
25
This risk is distinct from the
more general incentive, which is addressed by Section 1853(a)(1)(C)(ii) of the Social Security
Act, for MA organizations to increase their coding intensity (and therefore their payments) by
reporting as many valid, supported diagnoses as possible.
The model relies on conditions that are well specified, and that consistently and reliably predict
medical costs in a future year. Incentives for discretionary coding, while possibly stronger in
MA, are not unique to MA, and we have seen increases in coding in the FFS program in recent
years. There are several possible drivers. The proportion of payments in FFS tied to value-based
payment models that rely on the CMS-HCC model has grown significantly between the
expenditure year for the 2020 model (2015) and the expenditure year for the 2024 CMS-HCC
model (2019). Further, providers who are both FFS participating providers and in MA networks
may carry over incentives from the MA program into their larger practice. Including diagnosis
25
MedPAC, Report to the Congress: Medicare Payment Policy xxiv, 324-25, 355 (March 2023); Luis Serna & Andy Johnson,
MedPAC Presentation Slides 11, 13 (Jan. 12, 2023),
https://www.medpac.gov/wp-content/uploads/2023/01/MedPAC-MA-status-report-Jan-2023.pdf

109
codes in the model where providers may have an incentive to report a more severe diagnosis
code when clinically not well specified dilutes the cost predicted by the model for more severe
conditions and potentially reduces the sample size of the less severe condition resulting in
unstable predictions between calibrations. As described before, despite including fewer diagnosis
codes, the reclassified payment model maintains or improves predictive accuracy compared to
the model currently in use (the 2020 CMS-HCC model) predictive ratios (ratios of predicted to
actual mean expenditures by predicted expenditure decile) and other measures CMS does not
typically consider, such as the R
2
statistic.
Further, even if there was an overlap between the Principle 10-guided changes in the 2024 CMS-
HCC model compared to the currently used 2020 CMS-HCC model, nothing in section
1853(a)(1)(C) prohibits how CMS has approached this issue in model development. Section
1853(a)(1)(C)(i) authorizes the addition, modification, or removal of a risk factor. The
mandatory, uniform coding pattern adjustment did not (as some commenters suggested) remove
the Secretary’s authority to revise the model to eliminate or constrain particular codes or HCCs
based on our longstanding principles for risk model development for the MA program. Here, the
revisions to address the multiple conditions (as reflected in coded diagnoses) and costs used by
CMS to adjust for overall health status are within the scope of that authority. We note that
commenters alleging duplication with the coding pattern adjustment provided no specific
evidence in their comments that they will be underpaid. There is a range of estimates for the
appropriate coding pattern adjustment, and as noted before, independent experts have found that
if anything, the risk adjustment model has been overpaying MA organizations significantly even
after application of the minimum coding pattern adjustment.
26
The changes finalized in the 2024 CMS-HCC model are incorrectly characterized by the
commenters as a coding intensity or coding pattern adjustment. The changes based on Principle
10 are clinically informed and are intended to ensure a more accurate prediction of variation in
cost based on health status. Removing HCCs for protein-calorie malnutrition, angina pectoris,
and atherosclerosis of arteries of the extremities with intermittent claudication, and separately
constraining the three diabetes HCCs (glycemic, unspecified, or no complications; with chronic
complications; and with severe acute complications) and congestive heart failure (heart failure,
except end-stage and acute; acute heart failure (excludes acute on chronic); and acute on chronic
heart failure) so that each grouping has the same coefficient allocates the FFS spending
associated with those conditions to demographic factors, the count variables, and other
associated conditions in the model that are better specified.
As noted in the Advance Notice, CMS followed a process for identifying ICD-10 codes that may
be subject to discretionary coding. Discretionary coding can occur when providers may make
26
For a discussion of different methods for calculating a coding intensity adjustment see, “Reducing Medicare Advantage
Overpayments” at https://www.crfb.org/papers/reducing-medicare-advantage-overpayments. See also, the 2010 Advance Notice
https://www.cms.gov/medicare/health-plans/medicareadvtgspecratestats/downloads/advance2010.pdf

110
different decisions regarding the diagnosing and documenting of a condition given the same
circumstance, or an MA organization may make a decision that is different from a provider
regarding the reporting of condition for payment. This may occur because clinical indicators are
broad, need significant interpretation, or because the condition is being diagnosed and
documented in situations where it has no clinical significance, or where it does not require or
affect patient care, treatment or management as required by the ICD-10 Coding Guidelines. The
first step in our analysis was to determine whether there are differences in coding patterns
between FFS and MA by condition, because a difference in the rate of diagnosis codes submitted
could be indicative of differences in clinical interpretation. CMS data and independent studies
generally find that the demographic and healthcare utilization patterns between FFS and MA are
similar.
27,28,29
By and large, the prevalence of HCCs is also similar between MA and FFS. In the
Non-Dual Aged segment, the percentage point difference in prevalence between MA and FFS
was within 1 percentage point for 75 of 86 payment HCCs (87 percent). In the Full Benefit Dual
Aged Segment, the percentage point difference in prevalence between MA and FFS was within 1
percent for 72 of the 86 (84 percent) payment HCCs. Therefore, the small number of outlier
HCCs where the difference in prevalence in MA exceeded 1 percent warranted further analysis.
CMS identified the following HCCs in the 2020 CMS-HCC model that had significant variation
in coding between MA and FFS:
1. HCC 18 Diabetes with Chronic Complications
2. HCC 21 Protein-Calorie Malnutrition
3. HCC 22 Morbid Obesity
4. HCC 59 Major Depressive, Bipolar, and Paranoid Disorders
5. HCC 85 Congestive Heart Failure
6. HCC 88 Angina Pectoris
7. HCC 108 Vascular Disease
8. HCC 111 Chronic Obstructive Pulmonary Disease
9. HCC 138 Chronic Kidney Disease, Moderate (Stage 3).
Identifying HCCs with significant coding pattern differences was the first step in CMS’ analysis
before a more intensive clinical review to determine whether the continued reliance on these
diagnosis codes in the payment model was consistent with Principle 10.
Among diagnoses in these nine HCCs that were selected for further clinical review, CMS
determined that the following ICD-10 diagnoses codes are subject to sufficient clinical discretion
27
https://www.commonwealthfund.org/publications/issue-briefs/2021/oct/medicare-advantage-vs-traditional-medicare-
beneficiaries-differ; see also Paul D. Jacobs & Richard Kronick, Getting What We Pay For: How Do Risk-Based Payments to
Medicare Advantage Plans Compare with Alternative Measures of Beneficiary Health Risk, 53 H
EALTH SERVICES RESEARCH
4997, at 5012 (Dec. 2018) (increasing MA risk scores compared to FFS likely outpace relative increases in actual health risk; MA
enrollees are no sicker, and may well be healthier than similar FFS beneficiaries).
28
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9175080/
29
https://www.kff.org/medicare/report/beneficiary-experience-affordability-utilization-and-quality-in-medicare-advantage-and-
traditional-medicare-a-review-of-the-literature/

111
and that removal from payment HCCs in the 2024 CMS-HCC model is appropriate: all ICD-10
diagnosis codes mapped to 2020 CMS-HCC model HCC 21 Protein-Calorie Malnutrition and
HCC 88 Angina Pectoris, and 30 diagnosis codes mapped to HCC 108 Vascular Disease. CMS
further assessed that the coefficients in the 2024 CMS-HCC model for the diabetes HCCs and
some of the Congestive Heart Failure HCCs, which retain most of the ICD-10 codes originally
mapped to the 2020 CMS-HCC model HCCs, should be constrained. Constraining the
coefficients for the diabetes HCCs in the 2024 CMS-HCC model balances the need to predict
cost for clinically meaningful conditions and the need to limit the incentive to report
discretionary codes included in the model for payment. As a group, each set of constrained
HCCs are accurately predicted, although individual HCCs within each group may be under or
over predicted.
The decision to exclude diagnoses was made after careful consideration and consultation with
independent clinicians. Diagnoses mapped to HCC 21 Protein-Calorie Malnutrition had been
included in the 2020 CMS-HCC model because clinically, protein-calorie malnutrition can be
useful as a risk marker for frailty, severe illness, and late- or end-stage disease, and it is likely
correlated with poverty/disadvantaged populations. However, CMS analysis confirmed that the
most commonly reported diagnosis codes mapped to HCC 21 by FFS and MA include less
severe or unspecified protein-calorie malnutrition (E46, E43, E440) and Cachexia (R64). Recent
analysis from the HHS Office of the Inspector General (OIG) found that hospitals correctly
billed FFS Medicare for severe malnutrition diagnosis codes (E41 and E43) for 27 of the 200
claims reviewed. For 164 of the remaining claims OIG found that hospitals used severe
malnutrition diagnosis codes when they should have used codes for other forms of malnutrition
or no malnutrition diagnosis code at all, and for nine of these claims, the medical record
documentation supported a secondary diagnosis code other than a severe malnutrition diagnosis
code.
30
This finding in conjunction with clinician experts’ opinion suggested that including even
the more severe diagnoses mapped to HCC 21 in the 2020 model would create incentives for
wide variation in coding. Because the regression model predicts all FFS costs, any spending
associated with the Protein-Calorie Malnutrition HCCs will be reallocated to correlated
conditions or demographic markers, such as cancer and older ages.
31
As previously stated, the
risk adjustment model is intended to differentiate relative risk such that higher payments are
calculated for sicker beneficiaries with higher disease burden relative to average.
Diagnoses mapped to HCC 88 Angina Pectoris in the 2020 CMS-HCC model were excluded due
to Principle 10 because of a lack of clinical specificity. Decisions regarding whether to diagnose
and document angina pectoris are subject to some discretion, which presents a risk that the
30
https://oig.hhs.gov/oas/reports/region3/31700010.pdf.
31
CMS has explained this type of effect before: “We do note that when specified HCCs are removed from the model, the model
is recalibrated and the same costs are predicted with the new set of HCCs. The relative factors for conditions that are comorbid
with the excluded HCC may increase, as may the various demographic factors.” CY 2014 Rate Announcement at 30-31 (April 1,
2013), https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Downloads/Announcement2014.pdf

112
diagnosis could be used in cases of chest pain that do not require further treatment, and also
when the diagnosis does not affect the care, treatment or management of the beneficiary.
Additionally, HCC 88 included ICD-10 codes for other or unspecified forms of angina pectoris,
including with atherosclerosis. Independent studies have found that incidental detection of
atherosclerosis through CT scans is “relatively prevalent and carr[ies] high risk for asymptomatic
coronary disease.” For example, in a study of 1,494 clinically healthy adults without a history of
CVD, 68% of those who underwent abdominal CT had atherosclerotic lesions with stenosis in
the aorta or its major branches. Thus, there is a likelihood that atherosclerosis is being coded
based on radiology reports for cases that are asymptomatic.
32
This rationale was also applied to
the ICD-10 diagnosis codes previously included for payment in HCC 108 in the 2020 CMS-HCC
model. Arterial Atherosclerosis with intermittent claudication may not be a good predictor of
medical expenditure because evidence suggests that patients with intermittent claudication often
do not require treatment.
33
In response to a comment suggesting that variation in coding between MA and FFS must be
addressed through a model calibrated with MA encounter data, CMS agrees that an MA coding
pattern difference adjustment would no longer need to be applied to the MA risk scores if the
risk adjustment model were calibrated with MA data. While CMS disagrees with commenters
that changes to the 2024 CMS-HCC model based on Principle 10 are duplicative of the coding
intensity adjustment, and disagrees that CMS does not have the authority to make changes to the
risk adjustment model to account for variability in diagnosis codes submitted, CMS agrees that
the statute supports calibrating a model using MA data submitted on encounter data records.
CMS will engage with stakeholders when we move forward with developing such a model.
CMS-HCC Risk Adjustment Model for PACE organizations for CY 2024
Comment: Several commenters opposed CMS’ proposal to use the 2017 CMS-HCC risk
adjustment model for payment to PACE organizations for CY 2024. These commenters urged
that, for CY 2024, CMS transition PACE organizations to the CMS-HCC risk adjustment model
that is currently being used for MA payment (the 2020 CMS-HCC risk adjustment model). These
commenters are concerned that the 2017 CMS-HCC risk adjustment model excludes several
chronic conditions, especially dementia, which is prevalent in the PACE population.
Commenters also pointed to pressure ulcers (HCC 159), moderate chronic kidney disease (HCC
138), and several mental health and substance use disorder HCCs as condition categories that
they believe are critically important for accurate risk adjustment for PACE organizations.
Commenters believe that the frailty adjustment is inadequate to capture the risk of their
32
Suh, B., Song, Y. S., Shin, D. W., Lim, J., Kim, H., Min, S. H., ... & Cho, B. (2018). Incidentally detected atherosclerosis in
the abdominal aorta or its major branches on computed tomography is highly associated with coronary heart disease in
asymptomatic adults. Journal of cardiovascular computed tomography, 12(4), 305-311.
33
Cassar K. (2006). Intermittent claudication. BMJ (Clinical research ed.), 333(7576), 1002–1005.
https://doi.org/10.1136/bmj.39001.562813.DE

113
participants in a model that excludes the aforementioned conditions, which are included for
payment in the 2020 CMS-HCC risk adjustment model. Commenters asserted that PACE
organizations are underpaid using the current risk adjustment methodology because they believe
it fails to recognize the costs of care associated with a complex population, such as PACE
participants. One commenter stated that their ability to provide integrated, quality care to PACE
participants may be compromised because of systematic underpayments they believe are present
for PACE organizations due to the use of the 2017 CMS-HCC risk adjustment model.
Additionally, commenters voiced concern over the misalignment of PACE and MA in regards to
the risk adjustment models used for payment, stating that the misalignment is further exacerbated
by CMS’ proposal to move MA plans to an updated CMS-HCC risk adjustment model that is
calibrated using ICD-10 diagnoses, as well as more recent diagnostic and cost data, thereby
further increasing health disparities. The commenters agreed with CMS that it is important to
update the diagnostic and cost data on which the risk adjustment model is based, and noted that
the model proposed for organizations other than PACE has new categories that reflect more
clinical specificity and validity (i.e., greater level of detail that allows more precision in the
identification of specific conditions). Commenters questioned why these considerations are not
being applied to the risk adjustment model being used for PACE, believing that CMS should use
a payment model for PACE that accurately represents the population they serve.
Generally, commenters believed that it is possible for CMS to use the 2020 CMS-HCC risk
adjustment model to pay PACE organizations, without having to change the diagnostic data
sources currently being submitted by PACE organizations for risk adjustment purposes (which
includes diagnoses submitted to the Risk Adjustment Processing System (RAPS) and the
Encounter Data System (EDS)). Commenters believed that CMS’ past justifications for being
unable to move PACE to the 2020 CMS-HCC risk adjustment model were insufficient or not
credible. Commenters noted that in the 2020 Rate Announcement,
34
CMS stated that they have
done extensive work to improve and facilitate the submission of encounter data and will continue
to do so, however, commenters were only aware of a couple of instances where CMS engaged
with PACE organizations since that time (site visits with some PACE organizations and a PACE-
specific webinar presentation on encounter data). Commenters argued that CMS has used the
data submitted to RAPS and EDS for PACE risk adjustment for several years “without concern
for accuracy or completeness,” and, therefore, CMS’ prior justifications for not moving PACE to
the model used for MA is not a credible barrier to transitioning PACE to a more accurate risk
adjustment model. They recommended that CMS transition PACE to the 2020 CMS-HCC risk
adjustment model using the current method of calculating PACE risk scores (pooling RAPS,
encounter data, and FFS claims), and that during the transition, CMS collaborate with PACE
organizations to address encounter data submission difficulties they may be experiencing.
34
CY 2020 Rate Announcement.

114
Response: CMS will continue the use of the 2017 CMS-HCC risk adjustment model for risk-
adjusted payment to PACE organizations for CY 2024. The 2017 CMS-HCC risk adjustment
model was first adopted for PACE in the 2022 Rate Announcement.
35
CMS acknowledges
concerns from commenters about the inclusion of dementia and other conditions in the model,
and the recommendation to move PACE to the 2020 CMS-HCC risk adjustment model that
includes these conditions. CMS recognizes that using distinct HCCs to calibrate separate models
for PACE and MA may result in differences in predicted risk for individual beneficiaries,
however, we note that the costs associated with conditions that are not in the 2017 CMS-HCC
risk adjustment model for payment, such as dementia, are predicted by comorbid conditions and
demographic factors. To the extent that these costs are not predicted by the model, they are
reflected in the frailty factors.
As noted in the November 1, 2013 HPMS memo titled, “Clarification to Encounter Data
Submissions Memo for PACE Organizations,”
36
PACE organizations are only required to submit
encounter data records for Medicare-covered items and services for which the organization
collects claims. Because PACE organizations are not submitting encounters for all of their
services, we do not have complete encounter data for their members and, therefore, we do not
have a complete diagnostic profile for their members in the encounter data. Without a complete
diagnostic profile, we cannot rely solely on encounter data to calculate PACE risk scores and,
instead, use diagnoses from encounter data as a supplement to RAPS data when calculating risk
scores for payment using the 2017 CMS-HCC risk adjustment model. Because the 2020 CMS-
HCC risk adjustment model was calibrated using FFS diagnoses that were selected using the
filtering method that is used for encounter data, this model is intended to calculate risk scores
using diagnoses submitted on encounter data records and FFS claims (for beneficiaries who
switch from FFS to MA) filtered in the same manner as encounter data records. Since we do not
have complete encounter data from PACE organizations, we are not calculating PACE
beneficiary risk scores using diagnoses solely from encounter data and FFS claims (in contrast to
the long-standing approach to calculating non-PACE beneficiary risk scores), and we cannot
implement the 2020 CMS-HCC risk adjustment model for PACE at this time. Using primarily
RAPS-based diagnostic data (based on specialty filtering) on a model that was developed to
calculate risk scores using encounter data (based on CPT/HCPCS filtering) results in inaccurate
risk scores, and therefore payment.
In the summer of 2022, CMS engaged with some PACE organizations to discuss successes and
challenges they have experienced with submitting encounter data. CMS will conduct analyses to
ascertain the state of encounter data submissions for PACE organizations and continue to work
closely with these organizations to develop further guidance and provide technical assistance
with transitioning PACE organizations fully to encounter data in anticipation of future
implementation of a risk adjustment model for PACE that is calibrated using encounter data
35
CY 2022 Rate Announcement
36
Clarification to Encounter Data Submissions Memo for PACE Organizations, November 1, 2013
115
(such as the one currently used for MA payment in 2023 or a future model). As noted in the 2022
Rate Announcement, CMS continues plans to use a more recently updated model to pay PACE
organizations as soon as it is practicable.
Section K. End Stage Renal Disease (ESRD) Risk Adjustment Models for CY 2024
CMS did not receive comments on the CMS-HCC ESRD risk adjustment models for PACE
organizations for CY 2024. CMS will continue to calculate risk scores for payment of
beneficiaries with ESRD in PACE organizations using the CY 2019 CMS-HCC ESRD risk
adjustment models as proposed in the CY 2024 Advance Notice.
Comment: Two commenters supported the continued use of the CY 2023 CMS-HCC ESRD
Models for 2024.
Response: CMS appreciates the comments. For CY 2024, we will continue to calculate risk
scores for payment of beneficiaries with ESRD in MA plans and certain demonstrations using
the CY 2023 CMS-HCC ESRD risk adjustment models as proposed in the CY 2024 Advance
Notice.
Comment: A couple commenters made recommendations for CMS to engage with stakeholders
when updating the ESRD risk adjustment models in the future; one commenter specifically
requested full transparency, collaboration with plans and providers, and a longer comment period
(i.e., at least 60 days for comment on any proposed changes). A commenter urged that risk
adjustment model changes be finalized at least two years in advance of the implementation date
to allow sufficient time for plans and providers to make necessary operational changes.
Response: Thank you for your comment.
Comment: One commenter requested that CMS move enrollees with a reported dialysis
diagnosis into the ESRD segment automatically.
Response: We believe the commenter is suggesting that CMS use ICD-10 diagnosis codes
related to ESRD as an indicator to calculate risk scores using the ESRD dialysis risk adjustment
model. The ESRD dialysis model is intended to calculate projected risk for beneficiaries
receiving ongoing dialysis treatment. ICD-10 ESRD diagnosis codes are not always indicative of
dialysis treatment. For example, ESRD ICD-10 diagnosis codes can be used in instances where a
beneficiary has an early stage of ESRD that does not require dialysis, or a beneficiary is
receiving acute dialysis for a limited timeframe. To consistently apply ESRD risk scores to
beneficiaries receiving ongoing dialysis, CMS uses notification from a dialysis facility that the
beneficiary is receiving dialysis in a Medicare certified facility. The dialysis facility submits the
notification to CMS on the CMS-2728 form and the payment system uses this information to
apply an ESRD dialysis risk score. This allows CMS to calculate risk scores that are appropriate
for the dialysis population.

116
Section L. Frailty Adjustment for Fully Integrated Dual Eligible Special Needs Plans
(FIDE SNPs) and PACE Organizations
Frailty for FIDE SNPs
Comment: The majority of commenters who made a remark about frailty for FIDE SNPs
expressed concern about the decrease in the frailty factors and the impact on enrollee frailty
scores, especially in combination with the impact of the proposed CMS-HCC risk adjustment
model. Plans cited a number of reasons for their concern, including: general concerns about the
decline in frailty scores and disproportionate impacts on vulnerable and high-need populations
because of payment decreases; concerns that it will be harder for FIDE SNPs to qualify for
frailty because, in order to qualify, the average level of frailty in the FIDE SNP has to be similar
to that in the PACE program; and concerns that the decreases in frailty factors may be anomalous
for full-benefit and/or partial-benefit dually eligible individuals.
Response: We appreciate commenters’ concern regarding the change in the frailty factors. For
CY 2024, CMS proposed to update the frailty factors used to calculate frailty scores for
beneficiaries enrolled in FIDE SNPs in order to align with the 2024 CMS-HCC risk adjustment
model and, in addition, applied a new technical adjustment to account for potential non-response
bias. In reviewing the initial frailty factors produced by the survey results using CMS’ long-
standing methodology, we noticed differences in some of the underlying patterns of frailty
factors relative to prior years. For example, the full-Medicaid 0 Activities of Daily Living (ADL)
group that typically does not predict additional costs due to limitations of ADLs (i.e., predicted a
negative factor) has a positive factor under the recalibrated frailty factors. CMS believes the
differences in patterns of the factors may result from a number of drivers, including declines in
response rates and the underlying FFS population changes. To address these concerns, CMS
newly applied the Consumer Assessment of Healthcare Providers and Systems (CAHPS)
37
survey weight designed to adjust for the potential impact of non-response bias in the CAHPS
survey. While the application of the CAHPS survey weight maintains frailty factor patterns that
are largely consistent with prior years, the application of the weight puts downward pressure on a
number of the frailty factors. We do not believe the frailty factors without the CAHPS survey
weight applied are erroneous as they reflect the results of predicted residual costs from the model
for the survey population.
In consideration of the comments received, for CY 2024, CMS is finalizing updated frailty
factors that align with the 2024 CMS-HCC model, but that were not calculated using the CAHPS
survey weight that was proposed in the CY 2024 Advance Notice.
The final frailty factors for CY 2024 can be found in Table III-4. While we are not applying the
CAHPS survey weight for CY 2024, we will continue to evaluate the underlying patterns driving
37
Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys

117
the changes in the CY 2024 frailty factors and the appropriateness of applying CAHPS survey
weighting to the frailty factors. CMS will take our findings under consideration when making
future updates to the frailty factors.
We note that we must implement frailty factors that align with the CMS-HCC risk adjustment
model to be used in payment, since the frailty factors are calculated by predicting costs that are
not captured by the CMS-HCC risk adjustment model used for payment. For this reason, we are
unable to delay use of the recalibrated frailty factors, as some commenters requested. However,
the frailty factors being finalized for CY 2024 will be phased in on the same schedule as the Part
C model. Frailty scores for FIDE SNPs in CY 2024 will be calculated by blending 67% of the
frailty scores calculated using the frailty factors associated with the 2020 CMS-HCC risk
adjustment model (finalized in the 2022 Rate Announcement
38
) and 33% of the frailty scores
calculated using the frailty factors associated with the 2024 CMS-HCC risk adjustment model.
The blended frailty score will be compared to the PACE level of frailty calculated in the same
manner to determine whether that FIDE SNP has a similar average level of frailty as PACE.
Specifically, we note that the PACE minimum is calculated using the same frailty factors as
those used to calculate the frailty scores for FIDE SNPs, so changes in FIDE SNP frailty scores
will be accompanied by a change in how the PACE minimum is calculated. See the 2012 Rate
Announcement for a discussion of how CMS calculates the PACE minimum.
39
Table III-4 Final Frailty Factors Associated with the 2024 CMS-HCC Model – FIDE SNPs
Number of ADLs
Non-Medicaid
Partial Medicaid
Full Medicaid
0
-0.066
-0.070
0.158
1-2
0.103
0.203
0.230
3-4
0.201
0.203
0.230
5-6
0.201
0.217
0.248
Comment: Some commenters included a recommendation that CMS provide additional
information about how the change in frailty factors was formulated through rulemaking. A few
commenters recommended delaying the implementation of the CY 2024 CMS-HCC risk
adjustment model with the frailty adjustment, or implementing a phased-in approach. A few
commenters asked for more information or wanted CMS to be more transparent about the
process. A commenter recommended that stakeholders have more time before changes are made
to the frailty adjustment and recommended convening a technical expert panel.
Response: Section 1853(a)(1)(B)(iv) of the Act authorizes an additional payment adjustment that
takes into account the frailty of beneficiaries enrolled in Fully Integrated Dual Eligible Special
38
Refer to Section K. Frailty Adjustment for PACE Organizations and FIDE SNPs of the 2022 Advance Notice for the frailty
factors associated with the 2020 CMS-HCC risk adjustment model.
39
Refer to Section L. Frailty Adjustment of the 2012 Rate Announcement for information regarding the establishment of the
PACE minimum.

118
Needs Plans (FIDE SNPs), if the average level of frailty in the FIDE SNP is similar to that in the
PACE program, and CMS has chosen to apply such an adjustment. The frailty adjustment for
FIDE SNPs is part of the risk adjustment methodology. Because section 1853(b) of the Act
provides for the update of risk and other factors used to adjust capitation payments through the
Advance Notice and Rate Announcement, frailty adjustment factors have consistently been
proposed and finalized through the Advance Notice and Rate Announcement since we first
started making these adjustments for frailty for qualifying FIDE SNPs in 2012. As the frailty
factors must be estimated in alignment with the CMS-HCC risk adjustment model being used for
the payment year, it is a component of the methodology used to adjust payments to plans and,
therefore, is appropriately finalized using the process specified in section 1853(b) of the Act. As
previously stated, we must implement frailty factors that align with the CMS-HCC risk
adjustment model to be used in payment, since the frailty factors are calculated by predicting
costs that are not captured by the CMS-HCC model. For this reason, we are unable to delay the
use of the recalibrated frailty factors, as some commenters requested. As discussed previously,
the Advance Notice and Rate Announcement are the appropriate means by which changes are
made to MA payments. This also pertains to frailty factors for FIDE SNPs.
Comment: A few plan commenters recommended allowing additional plan types (e.g., HIDE
SNPs with exclusively aligned enrollment, ESRD C-SNPs, and/or plans that serve any dually
eligible beneficiaries) to be eligible for the frailty adjustment.
Response: By law, CMS must use the same payment methodology for all enrollees in MA plans,
including Special Needs Plans (SNPs), except as explicitly provided for in statute. Section
1853(a)(1)(B)(iv) of the Act authorizes CMS to make frailty-adjusted payments only to certain
dual SNPs – those with fully integrated, capitated contracts with states for Medicaid benefits,
including long term care, and which have similar average levels of frailty as the PACE program.
Thus, CMS cannot make frailty payments to any SNP that does not meet these criteria without
implementing frailty payments program-wide.
CMS has explored ways of incorporating frailty into the risk adjustment model in order to
account for frailty when making risk adjusted payments to all plans and found challenges with a
number of approaches (see the “Evaluation of the CMS-HCC Risk Adjustment Model,”
published March 2011).
40
In addition, as directed by section 17006(f)(2)(b) of the 21st Century
Cures Act, the Government Accountability Office issued a report on issues related to
incorporating functional status into MA risk adjustment in 2018.
41
This study found a number of
challenges with incorporating frailty into the model, including that “stakeholders could face
substantial challenges if the risk adjustment model were revised to account for beneficiary
40
Pope, Gregory C.; Kautter, John; Ingber, Melvin J.; Freeman, Sara; Sekar, Rishi; and Newhart, Cordon. (March 2011).
Evaluation of the CMS-HCC Risk Adjustment Model.
41
GAO Medicare Advantage Benefits and Challenges of Payment Adjustments Based on Beneficiaries’ Ability to Perform Daily
Tasks.

119
functional status, in part because this information is not readily available.” The CMS-HCC risk
adjustment model uses demographic factors and diagnoses to predict relative costs for
subpopulations, with the frailty adjustment used to predict expenditures for community
beneficiaries with functional impairments that are unexplained by the risk adjustment model
alone. Because the frailty factors are calculated using the residual of the CMS-HCC risk
adjustment model (the difference between the predicted expenditure amounts and the actual
expenditure amounts), and frailty scores have an average value of zero, the application of a
frailty adjustment to all MA plans would result in many plans receiving a negative frailty
adjustment.
Frailty for PACE Organizations
Comment: Some commenters expressed concerns with using the HOS-M survey to estimate
frailty because of low response rates, and that reliance on the HOS-M for frailty adjustment does
not consider the challenges faced by people with dementia in completing the survey. Most of
these commenters urged that, if dementia could not be included in the risk adjustment model
used to pay PACE organizations for CY 2024, that CMS modify the CY 2023 HOS-M survey
administration protocol to allow PACE organizations to proactively offer completion assistance
for the survey to their participants living with dementia to increase the likelihood that they are
adequately represented in the survey’s results.
Response: CMS estimates frailty factors to explain additional costs not explained by diagnoses in
the CMS-HCC risk adjustment model. To the extent that these costs are not predicted by the
model, they are likely to be reflected in the frailty factors. CMS calibrates the frailty factors by
regressing the residual, or unexplained costs, from the CMS-HCC risk adjustment model on
counts of activities of daily living (ADLs). Although total costs are included in the calibration of
the 2017 CMS-HCC risk adjustment model, and the associated frailty factors help predict overall
costs where diagnoses are not fully predictive, results for individual organizations may differ due
to differences between the sample used for model calibration and the populations enrolled in
individual plans.
CMS acknowledges the concerns related to improving the response rates for the HOS-M for
PACE participants generally, and among those with dementia. The responses from this survey
are used to determine a beneficiary’s limitations in ADLs for the calculation of a frailty score.
For the HOS-M, CMS will continue to allow a beneficiary to designate a proxy for responding to
the survey, including a PACE staff member. In addition, PACE organizations are able to provide
additional beneficiary contact information to support response rates. We collect survey data in
this manner so that there is consistency across PACE organizations, as this helps to ensure
equitable frailty results for payment.

120
Section M. Medicare Advantage Coding Pattern Adjustment
Comment: Many commenters opposed CMS’ proposed 5.9 percent 2024 coding pattern
adjustment and provided alternate alternative recommendations to the statutory minimum coding
pattern adjustment of 5.9 percent, as summarized below:
• Higher adjustment factor: Several commenters recommended a higher adjustment factor
than the statutory minimum, which they state is inadequate to adjust for differential
patterns of coding between MA and FFS. Commenters expressed concern that the
statutory minimum does not account for the full impact of coding pattern differences, and
multiple commenters highlighted analyses from MedPAC that the coding adjustment
factor should be several percentage points higher. These commenters stated their belief
that excess spending is accelerating the depletion of the Medicare Trust Funds and the
potential savings from fully accounting for the coding pattern differential would increase
solvency of the Trust Funds. A few commenters that recommended a higher coding
pattern adjustment expressed concern that the current application of the minimum
adjustment and the risk adjustment model incentivize plan sponsors to code their
enrollees with as many conditions as possible, driving up payment rates. One commenter
expressed concern that CMS’ current methodology does not address the underlying
causes of coding intensity, thereby undermining the goal of plans competing on the basis
of quality and costs. Another commenter noted their belief that increased payments to
MA plans do not result in better care.
• Lower adjustment factor: One commenter stated that the coding pattern adjustment
results in inappropriately low risk scores that negatively impacts payment for many
nonprofit regional health plans.
• Specific Methodological Recommendations:
o Demographic Estimate of Coding Intensity (DECI). A few commenters
recommended the incorporation of the DECI method to calculate a coding pattern
adjustment factor. Under the assumption that MA does not receive adverse or
favorable selection relative to FFS in terms of health status, the recommended
DECI method controls for demographics, estimating the coding pattern
adjustment by comparing MA risk relative to FFS risk using the CMS-HCC risk
adjustment model, and comparing that relationship against MA risk versus FFS
risk using the Adjusted Average Per Capita Cost (AAPCC) model that is based on
demographics only and was used in payment prior to 2000.
o Targeted approaches:
▪ General targeted comments. Several commenters expressed concern that coding
patterns across the MA landscape are heterogeneous and that failure to recognize

121
these differences across plans by applying an across-the-board coding pattern
adjustment could result in an inequitable outcome. A few commenters
recommended targeted approaches, because of their concern that certain MA
organizations code much more aggressively than others with higher levels of
coding intensity due to various structural payment incentives, including payments
between MA organizations and their contracted providers. Other commenters
stated their concern about the current application of the factor because it does not
adequately adjust for risk score increases above the average, and disadvantages
plans serving primarily low-income and historically underserved communities
that have less administrative resources to focus on diagnosis coding.
▪ Segmented approach. A few commenters suggested a segmented approach to
coding pattern adjustments that recognizes different levels of coding patterns
among plans, such that the lowest coding factor is applied to lower coding plans
while the highest factor is applied to higher coding plans.
▪ Contract-specific approach. A few commenters recommended tailoring the MA
coding pattern adjustment to the relative level of coding intensity seen in
individual MA contracts – rather than the across-the-board coding pattern
adjustment that CMS applies today to all MA contracts. A few commenters
believe that CMS should consider increasing the MA coding pattern adjustment
for all contracts and consider using its statutory authority to vary the coding
pattern adjustment by contract.
A few commenters had recommendations to calibrate the model using different data to address
coding pattern differences between MA and FFS. One commenter recommended a multipronged
approach to addressing coding pattern differences in MA and FFS. Their recommendation
included three parts: 1) develop a risk adjustment model that uses two years of FFS and MA
diagnostic data; 2) exclude diagnoses that are documented only on health risk assessments from
either FFS or MA; and then 3) apply a coding adjustment that fully accounts for the remaining
differences in coding between FFS Medicare and MA plans.
Response: On an annual basis, CMS analyzes coding pattern differences and determines what the
coding pattern adjustment factor should be. Section 1853(a)(1)(C)(ii) of the Act establishes a
minimum MA coding pattern adjustment, which was originally adopted beginning with 2014
payment. The current statutory minimum coding pattern adjustment is 5.9%. We have found that
the minimum adjustment is sufficient to reflect differences in coding patterns between MA plans
and providers under FFS Parts A and B. CMS continues to believe that applying a uniform
adjustment is an appropriate approach. Therefore, we are finalizing our proposed MA coding
pattern adjustment factor for CY 2024.

122
We appreciate the extensive and thoughtful comments and feedback we received on this
proposal. Ensuring that the coding pattern adjustment policy appropriately addresses differences
in coding patterns between the FFS program and MA is essential and we will consider these
recommendations in the development of future coding pattern adjustment proposals.
Comment: A few commenters supported CMS’ proposed 5.9 percent 2024 coding pattern
adjustment.
Response: CMS appreciates the support of the commenters. CMS is finalizing the proposed
adjustment of 5.9 percent for CY 2024.
Comment: One commenter requested sufficient time and information to comment on any
potential changes to the MA coding pattern adjustment in the future.
Response: CMS appreciates the comment. Section 1853(b)(2) requires that CMS provide notice
of proposed changes in the methodology and assumptions for setting MA capitation rates and
risk and other factors used to adjust the capitation payments, with a comment period of at least
30 days to comment on the proposed changes. We will continue to consider additional ways in
which we can engage with stakeholders should we consider changes to the MA coding pattern
adjustment.
Comment: A few commenters recommended that CMS move to a risk adjustment model based
on MA encounter data to improve payment accuracy, which would also eliminate the need for a
coding pattern adjustment.
Response: We appreciate the recommendation to move to an encounter-data based model. CMS
recognizes the benefits of moving to a payment system that is based on MA experience. As
discussed above, public comment would be an essential part of developing an encounter data-
based model.
Comment: A few commenters believed that it is fundamentally incorrect to assume any observed
coding differentials between the FFS and MA populations are driven by inappropriate coding on
the part of MA plans and requested that CMS recognize that higher coding does not necessarily
equate to wrong coding. One commenter stated that CMS should consider that differences in
coding stem from the fact that FFS is unmanaged and under-coded, and that the differences
actually demonstrate the value of MA plans in diagnosing and appropriately managing members’
conditions. One commenter stated that the MA coding pattern adjustment was redundant to the
many structures in place to reduce coding intensity such as the Risk Adjustment Data Validation
audit (RADV).
Response: The MA coding pattern adjustment is not intended to adjust for inaccurate coding, but
it is intended to account for program-wide differences in coding patterns between MA and FFS.
CMS applies the MA coding pattern adjustment to adjust for the impact on MA risk scores of

123
coding patterns that differ from FFS coding, which is the basis of the CMS-HCC model. More
specifically, Section 1853(a)(1)(C)(ii) of the Social Security Act requires the Secretary to reduce
payments to MA organizations by at least 5.9% to account for “differences in coding patterns
between Medicare Advantage plans and providers under part[s] A and B.” This mandatory
adjustment is applied to each beneficiary’s risk score at every MA plan, which reflects how
section 1853(a)(1)(C)(ii) focuses on coding pattern differences at a general, program-wide level.
Specifically, section (a)(1)(C)(ii) addresses the incentive for all MA plans to identify more valid,
supported codes on all HCCs, and therefore report more diagnoses (which we do not assume to
be inaccurate when evaluating coding pattern differences between FFS and MA). By reducing
each individual risk score by a specified percentage, the coding pattern adjustment corrects for
overall, net differences between MA and FFS coding.
Section N. Normalization Factors
CMS did not receive comments on the methodology proposed to calculate the RxHCC risk
adjustment model normalization factors for CY 2024. CMS is finalizing the RxHCC
normalization factor methodology as proposed.
Comment: For the CMS-HCC and CMS-HCC ESRD risk adjustment models, many commenters
were in support of the continued exclusion of the CY 2021 risk score from the calculation of the
normalization factors for CY 2024, consistent with the policy finalized for CY 2023. Some
commenters stated their agreement with CMS’ belief that the decreased 2021 risk score is driven
by reduced utilization in 2020 due to the pandemic and, therefore, should be excluded from the
normalization factor. Several commenters were, in general, supportive of the methodology
proposed to calculate the normalization factors for CY 2024, with a couple expressing their
support only for the proposed methodology for the newer models (the CMS-HCC model
proposed in the 2024 Advance Notice and the CMS-HCC ESRD models finalized in CY 2023).
Response: CMS appreciates the support of the commenters. We are finalizing the normalization
factor methodology for the CMS-HCC and CMS-HCC ESRD risk adjustment models as
proposed.
Comment: Several commenters were generally concerned that the proposed normalization
factors for the CMS-HCC and CMS-HCC ESRD risk adjustment models are overstated, with one
commenter stating their belief that this will translate to fewer benefits for beneficiaries. One
commenter had concerns about applying a common normalization factor across model segments
because they believe that the impact of the COVID-19 pandemic was not the same across
segments, potentially leading to disproportionate impacts of the normalization factor across plans
depending on their beneficiary population. A couple of commenters suggested a more nuanced
approach be used for the inclusion of the 2022 risk score in the normalization factors for the
newer models.

124
A few commenters were specifically concerned about CMS’ proposed methodology to exclude
the 2021 risk score (based on 2020 dates of service) from the calculation of the risk adjustment
model normalization factors for CY 2024. A couple of these commenters believed that excluding
the 2021 risk score data continues to deviate from CMS’ longstanding methodology to use risk
scores based on the most recent data available so as to reflect recent FFS experience. There was
concern by a couple of commenters that excluding more recent years (for the older models), or
weighting post-pandemic risk scores equally with pre-pandemic risk scores (for the newer
models), may not be appropriate as the risk score experience may not be the same in the two time
periods. A couple of commenters also stated that removing the 2021 risk score data from the
normalization methodology increases the negative normalization adjustment, resulting in further
reduction to risk scores and resulting payments. One of these commenters believed CMS’
proposed methodology was contrary to CMS’ data that showed continued lower risk scores in
FFS while another questioned the accuracy of the normalization factors when excluding the 2021
risk score. One commenter requested that CMS explain how it plans to address the anomalous
2020 utilization patterns in future years, and voiced concern that utilization in 2021 and 2022
may also be anomalous. This commenter asked that CMS be consistent with how it uses the 2021
risk score in normalization in that, if it is excluded for CY 2024, that it continues to be excluded
in the future.
A couple of commenters supported CMS’ proposed methodology to calculate the normalization
factors for the newer models (those with a 2019 or 2020 denominator) using risk scores from
2018-2022, excluding 2021, but opposed the proposed methodology for the older models (those
with a 2015 denominator) to exclude both 2021 and 2022 risk scores. These commenters
believed that the CMS should be consistent with its methodology across models and that the
2022 risk score should be included for both newer and older models so as not to overstate the
normalization factor for the older models, which would lead to insufficient MA payments. They
believe that the pre-pandemic experience may not reflect post-pandemic experience and by
excluding more recent years from the older models, CMS is further deviating from its
longstanding methodology to use recent FFS experience in the calculation of the normalization
factor. Alternate methodologies for including 2022 in the normalization factor for the older
models were suggested by a few commenters, such as using more years in the trend, projecting
the trend differently, weighting 2022 risk scores more heavily to reflect more relevant and recent
FFS experience, or blending.
Several commenters also requested that CMS be more transparent in its normalization factor
calculation by releasing more data, providing more methodological information, further
explaining its rationale for the proposed policy, or establishing a Technical Expert Panel to
discuss the calculation of the normalization factor.
Response: CMS appreciates commenters’ concerns regarding the calculation of the
normalization factors for CY 2024. We believe, however, the proposed methodologies – using a
linear approach with the most recent five years of data, with the exclusion of 2021 (2018–2022,
125
excluding 2021) for newer models, and using a linear approach with the exclusion of 2021 and
2022 (2016-2020) for the older models – are better projections of the applicable average FFS risk
score in 2024.
The goal of the normalization factor is to accurately predict the FFS risk score in the payment
year, thereby maintaining an average FFS risk score of 1.0 across the entire FFS population.
CMS believes that the inclusion of the 2021 risk score in the slope calculation will result in a
projected risk score (i.e., normalization factor) that is significantly below what the actual average
FFS risk score is likely to be in 2024 whether the risk score is based on the current or proposed
CMS-HCC model. In other words, including the 2021 risk score in either projection results in an
unrealistic estimate of the 2024 FFS risk score.
Including the 2021 risk score and applying our typical methodology for the current CMS-HCC
model yields a CY 2024 normalization factor that is lower than the actual 2022 FFS risk score.
For the proposed model, if the 2021 risk score were included in the calculation using our typical
methodology, the CY 2024 normalization factor would be 0.8% higher than the 2022 risk score.
CMS believes it is unlikely that 2024 risk scores will be lower than 2022 risk scores, or that risk
scores will grow by only 0.8% over two years. In addition, in all of the years used to identify the
trend in risk scores prior to 2021, risk scores progressively increased; the decreases in utilization
in 2020 were irregular due to the pandemic. The objective of the normalization factor is to
project the payment year risk scores as accurately as possible to maintain the 1.0, given the
information known at the time the projected scores are calculated. Given this objective, CMS
believes that the decreases in utilization in 2020 due to the pandemic are not reflective of future
health care utilization and should not be included in the calculation of the normalization factors.
Including the 2022 risk score and applying our typical methodology for the current CMS-HCC
model yields a CY 2024 normalization factor that is lower than the 2022 FFS risk score. As
noted above, CMS believes it to be unlikely that 2024 risk scores will be lower than 2022 risk
scores. Given the increase in the 2022 actual FFS risk score relative to 2021 and the continuous
increase in the average FFS risk score prior to the pandemic, it is not reasonable to apply a
normalization factor that is lower than the most recent risk score data point in the trend. While
we think it is important to incorporate more recent years of data in the trend to reflect current
risk, updating the data must be balanced with projecting a risk score that is reflective of what the
average 2024 FFS risk score is likely to be in order to establish the appropriate normalization
factor.
CMS appreciates commenters’ concerns about the impact of the COVID-19 pandemic on
utilization and diagnoses submission, and the potential effects on risk adjusted payments. CMS
carefully considered the use of the 2021 FFS risk score in the calculation of the slope used to
project the normalization factors for the CMS-HCC risk adjustment models for CY 2024. The
2021 risk score, which is based on diagnoses from 2020 dates of service, is significantly lower
than the 2020 risk score, which was based on diagnoses from 2019 dates of service. Prior to

126
2021, risk scores progressively increased in the years used to identify the trend in risk scores. We
believe that the decrease in the 2021 risk score is driven primarily by reduced utilization in 2020
due to the pandemic. While CMS understands the uncertainty surrounding the future impact of
the COVID-19 pandemic and the use of the 2020 utilization data, every year CMS re-evaluates
the data and bases policy decisions on the information available. We will continue to monitor
and analyze underlying risk score trends and their drivers. The public will have an opportunity to
comment on future proposed policies.
While there is inherent uncertainty with any prediction of future values, the proposed approaches
to calculating the normalization factors for CY 2024 maintain the stability of using our
longstanding five-year linear slope methodology while balancing the impact of the pandemic on
the normalization factor projection and the progressive increase in risk scores evident in the
historical trend prior to 2021.
Comment: A couple of commenters requested further rationale for CMS’ proposal to include
2020 utilization and data for development of the MA benchmarks and growth rates but not for
the CY 2024 normalization factors. A couple of commenters also questioned CMS’ use of 2020
as the denominator year for the proposed CMS-HCC risk adjustment model because the 2020
denominator uses 2020 expenditures/2020 dates of service. These commenters were concerned
that CMS is being inconsistent in its use of the 2020 experience across the policies proposed in
the 2024 Advance Notice.
Response: We understand that commenters are concerned about the treatment of 2020 data in
some of CMS’ MA payment policies. CMS carefully considered the appropriateness of 2020
data and made a determination based on how the data is being used (e.g., as part of an average
versus part of a trend), and the reasonableness of the impact of the data on what is being
measured. As described in more detail below, the impact of an inconsistent data point differs
when used to calculate an average versus a projected value. Prior to establishing MA
benchmarks for CY 2024, the trends in the 2020 FFS data used to establish the benchmarks were
analyzed. Some specific regions did experience decreased per-capita costs while other regions
experienced increased per-capita costs when compared to the 2019 national average per-capita
costs. However, because the ratebook FFS average geographic adjustments (AGAs) use data to
develop a relative index that averages out to 1.0, the level of the 2020 FFS claims is not
impactful for this measure. Furthermore, for ratebook development, CMS uses an average of five
years of FFS experience for each county, so annual fluctuations and anomalies in the data that
may occur for a variety of reasons are mitigated. Calculating and using a five-year average
provides stability in the rates despite local or regional events, such as natural or weather-related
disasters, and varying impacts from nationwide events, such as pandemics.
Distinct from calculating the benchmarks, normalization factors are calculated using five years
of historical data to create a trend that is projected out to a future payment year. As described in
the CY 2023 Advance Notice, when calculating a trend, one anomalous data point can have a
127
large impact on the projected value, which can pull the slope up or down significantly and lead to
a projection that does not reasonably estimate a future value. This trending issue does not apply
with rebasing where historical data are used to calculate a five-year rolling average in the AGA
calculation for ratebook development, so the impact of any one year of anomalous utilization is
moderated by four other years of data.
Prior to proposing the CY 2024 normalization factors for the CMS-HCC and CMS-HCC ESRD
risk adjustment models, CMS carefully considered the impact of using the 2021 risk score (2020
dates of service) in the calculation of the slope used to project the 2024 FFS risk score (i.e., the
normalization factor). CMS believes that the decrease in utilization due to the pandemic was
irregular and not reflective of future health care utilization, and, if the data were used to project a
future risk score, would result in an underestimate of the normalization factor. The policy of
excluding the 2021 risk score (2020 dates of service) from the normalization factor calculation is
consistent with the approach we used to project FFS USPCCs in the 2023 Rate Announcement in
that 2020 data are excluded. Like the methodology used to calculate normalization factors, the
methodology used to estimate national FFS spending projects a future value based on a trend.
For both estimates, which rely on trending and projecting using historical data, CMS consistently
excluded the 2020 data.
As noted by commenters, CMS used a 2020 denominator to create relative factors for the
proposed CMS-HCC risk adjustment model. In order to use the risk adjustment model to
calculate risk scores for payment, we create relative factors for each demographic factor and
HCC in the model. The relative factors are used to calculate risk scores for individual
beneficiaries. CMS creates relative factors by dividing all the model-based dollar coefficients by
the average per capita predicted expenditures for a specific year (the “denominator year”). To
calculate a model denominator, in this case the average per capita predicted expenditures for
2020 (i.e., the 2020 denominator), we do not use actual expenditures, but rather, we apply the
proposed CMS-HCC model to 2019 diagnoses from a cohort of 2020 beneficiaries, and produce
a predicted average per capita expenditure for 2020. Therefore, actual 2020 experience –
utilization or expenditures – is not reflected in the 2020 denominator.
Section O. Sources of Diagnoses for Risk Score Calculation for CY 2024
CMS did not receive comments within the scope of the policy as to which sources of diagnoses
are used for risk score calculation for CY 2024.
For non-PACE organizations, for CY 2024, CMS will continue the policy adopted in the CY
2023 Rate Announcement to calculate risk scores for payment to MA organizations and certain
demonstrations using only risk adjustment-eligible diagnoses from encounter data and FFS
claims.
For PACE organizations, for CY 2024, CMS will continue using the same method of calculating
risk scores under the CMS-HCC and ESRD models that we have been using since CY 2015,

128
which is to pool risk adjustment-eligible diagnoses from the following sources to calculate a
single risk score (with no weighting): (1) encounter data, (2) Risk Adjustment Processing System
(RAPS) data, and (3) FFS claims.
Attachment IV. Responses to Public Comments on Part D Payment Policy
Section A. RxHCC Risk Adjustment Model
Comment: Of the commenters that commented specifically on the proposal to continue using the
2023 RxHCC model for CY 2024, most expressed concerns about the impact of using the 2023
model in CY 2024 given the plan design changes called for in the IRA. These commenters
believed that changes such as the elimination of cost-sharing in the catastrophic phase of
coverage and cost-sharing caps on insulin and vaccines would result in increased plan liability
that would not be accounted for in the 2023 RxHCC model. Some commenters expressed
additional concerns about the impact that underestimation of plan liability would have on low-
income beneficiaries, beneficiaries with high-cost medications, and beneficiaries in D-SNP
plans. Some commenters supported updating the RxHCC model in CY 2025 to reflect plan
design changes to appropriately reflect relative risks of Part D enrollees. A couple of
commenters recommended CMS take specific steps in CY 2024 to account for the proposal to
use the 2023 RxHCC model in CY 2024 (e.g., providing flexibility to adjust margins during the
rebate reallocation process).
Response: CMS appreciates the commenters’ concerns. As noted in the CY 2024 Advance
Notice, the IRA was enacted well into the timeline needed to conduct a revision to the RxHCC
risk adjustment model to reflect these recent benefit changes for CY 2024. We acknowledge that
these benefit changes can result in changes to plan liability for beneficiaries with conditions that
result in an increased likelihood of reaching the catastrophic phase of the benefit. It requires
extensive time to prepare the data to update the model, run the recalibration and calculate the
relative factors, review the output, and finalize an updated model for publication in the Advance
Notice. For example, for the RxHCC risk adjustment model, this work includes re-mapping all
the Prescription Drug Event data to reflect the new plan liability, and re-estimating the RxHCC
coefficients based on the updated plan liability. For these reasons, the insufficient time CMS had
to recalibrate the RxHCC risk adjustment model to account for plan design changes called for by
the IRA made an update infeasible.
We note that any changes to plan liability as a result of IRA changes to the Part D benefit are not
expected to be large. Further, to the extent that any plans’ resulting revenue need for the plan’s
liability under the CY 2024 benefit sufficiently exceeds what they projected in their bid, then the
Part D sponsor would be compensated for some of their losses through the Part D risk corridors.
As discussed in the Advance Notice, we will be recalibrating the model based on the updated
benefit structure for CY 2025.

129
For CY 2024 CMS will continue to use the RxHCC Risk Adjustment Models as discussed in the
2024 Advance Notice:
• For Non-PACE Organizations: For CY 2024, we will continue to use the 2023 RxHCC
risk adjustment model to adjust direct subsidy payments for Part D benefits offered by
stand-alone Prescription Drug Plans (PDPs) and Medicare Advantage-Prescription
Drug Plans (MA-PDs).
• For PACE Organizations: For CY 2024, CMS will continue to use the 2020 RxHCC
risk adjustment model to calculate Part D risk scores.
Comment: A few commenters expressed concerns about the combined effects of changes to the
CMS-HCC risk adjustment model and the RxHCC model. One commenter believed that the
CMS-HCC changes could threaten the ability of MA plans to use rebate dollars to buy down the
Part D premiums, while another believed that the removal of codes from the CMS-HCC model
would cause discrepancies between plan coding activities for risk adjustment between the Part C
and Part D programs. Another commenter suggested revising RxHCC model coefficients for any
conditions, such as diabetes, which were being removed or disincentivized in the CMS-HCC
model.
Response: CMS appreciates the commenters’ concerns. These two models have always had key
differences, among them that the CMS-HCC risk adjustment model predicts the costs of Part A
and Part B benefits, while the RxHCC model predicts plan liability for prescription drugs
covered under the Part D program. Because the models predict different costs, it has always been
the case that they have HCCs that are formulated differently or that are in one model and not the
other. The CMS-HCC risk adjustment model is being updated to improve the prediction of costs
for the Part A and Part B benefits, using updated data and a reclassification of the HCCs so they
are based on the ICD-10 classification system. For CY 2023, the RxHCC model was updated to
improve the prediction of plan liability for Part D prescription drug costs by calibrating the
model on more recent data years and using newly built HCCs reflected a reclassification using
ICD-10 codes. In this way, for CY 2024, the RxHCC and CMS-HCC models will be more
closely aligned. We do not anticipate that changes to the CMS-HCC model will cause
discrepancies in plan coding activities between the Part C and Part D programs.
Comment: Several commenters recommended that CMS examine other methods where the
underlying data and structure of the RxHCC model could be modified for CY 2025. These
commenters believed that the model underpredicts plan liability for common therapeutic areas,
especially for newer, high-cost treatments and for low-income beneficiaries. Some of these
commenters also believed that the redesign of the Part D benefit in CY 2025 could lead to
incentives for plans to select beneficiaries with more favorable risk, so the model should be
updated to mitigate this potential.

130
Response: CMS appreciates the commenters’ concerns. As discussed in the Advance Notice, we
will be recalibrating the model based on the updated benefit structure for CY 2025 and will take
this feedback into account as part of the development and recalibration process. We consistently
look for ways to improve our models and thank the commenters for their thoughts.
Comment: A few commenters suggested steps such as including drug utilization markers similar
to those in the commercial market, as well as updating the model with more recent claims data to
reflect more recent drug costs and improve the predictive power of the model.
Response: CMS thanks the commenters for their suggestions. We understand that in certain
programs such as the Marketplace where a combined medical and drug model is utilized, the
methodological approach for predicting relative costs that are specific to that population may be
different from the approach used in MA. CMS uses the RxHCC risk adjustment model to adjust
the direct subsidy payments for Part D benefits offered by stand-alone prescription drug plans
and MA-Part D plans. Having the RxHCC model used to predict drug costs separate from the
CMS-HCC model used to predict medical costs enables a single model – the RxHCC model – to
account for differences in predicted plan liability for prescription drugs among distinct subgroups
of Part D eligible beneficiaries.
Comment: A majority of commenters recommended that CMS release information about the
recalibration of the RxHCC model that incorporates the updated benefit structure in advance of
the CY 2025 Advance Notice, with many of these commenters also recommending that CMS
allow for a 60-day comment period for the RxHCC model so that plans have more time to
evaluate the methodological changes.
Response: We thank the commenters for their recommendations.
Section B. Sources of Diagnoses for Part D Risk Score Calculation for CY 2024
Please refer to Attachment III, Section O. for comments and responses regarding sources of
diagnoses.
Section C. Inflation Reduction Act of 2022 Part D Benefit Design Changes
Comment: Many commenters expressed support for CMS’ implementation of the IRA changes
in place for 2024.
Response: CMS thanks the commenters for their support.
Comment: A commenter expressed opposition to CMS’ implementation of the IRA changes in
place for 2024, stating that the changes will lead to reduced benefits, increased cost-sharing, and
increased premiums.
Response: CMS appreciates the commenter’s concerns. We note that the IRA changes in place
for 2024 are mandated by statute and anticipate that these changes will increase the affordability

131
and accessibility of Part D drugs for Medicare beneficiaries. Furthermore, the premium
stabilization requirements will prevent unaffordable increases in premiums owed by Part D
beneficiaries.
Comment: A commenter requested clarification that the low-income cost sharing subsidy will
continue to cover the full cost of a claim with respect to ACIP-recommended vaccines and
covered insulin products for LIS beneficiaries up to the low-income patient payment in the
coverage gap. Another commenter argued that the low-income cost sharing subsidy used to
calculate the coverage gap discount with respect to covered insulin products for LIS beneficiaries
should be calculated based on the full cost of the drug rather than the maximum LIS copayment.
Response: For LIS beneficiaries in the coverage gap in 2024, the low-income cost-sharing
subsidy will continue to cover the full cost of an ACIP-recommended vaccine and a covered
insulin product up to the maximum LIS copayment in accordance with section 1860D-
14(a)(1)(C) of the Act. As such, the low-income cost sharing subsidy will continue to cover the
full cost of ACIP-recommended vaccines and covered insulin products up to the lesser of the
applicable copayment amount or nominal copayment amount. LIS-eligible beneficiaries are not
applicable beneficiaries and do not receive a coverage gap discount. Additionally, we clarify that
when we stated in the CY 2024 Advance Notice that no cost will be incurred by LIS and non-LIS
beneficiaries for ACIP-recommended adult vaccines and, therefore, no costs will count as
TrOOP toward the OOP threshold for beneficiary progression into the catastrophic phase, we
were speaking only of the amount actually paid by the beneficiary and not the low-income cost
sharing subsidy amount.
Section D. Medicare Part D Benefit Parameters: Annual Adjustments for Defined
Standard Benefit in 2024
Comment: A few commenters requested that CMS consider the impact of the 2023 pharmacy
price concession rule when calculating the API and CPI in the Rate Announcement. A
commenter believes that the pharmacy price concession rule will reduce the negotiated price of
drugs and patient drug spending, and therefore the effect of the pharmacy price concession rule
should be considered when calculating the API and CPI. Some commenters also requested that
CMS consider the changes to the coverage of ACIP-recommended vaccines and covered insulin
products in the calculation of the API and CPI for 2024.
Response: CMS appreciates the commenters’ suggestions and concerns. Under section 1860D-
2(b)(6) of the Act, the API is defined as the annual percentage increase in average per capita
aggregate expenditures for covered Part D drugs in the United States for Part D eligible
individuals for the 12-month period ending in July 2023. The calculation does not involve a
projection of the time period where the pharmacy price concession rule is effective. Additionally,
changes to the coverage of ACIP-recommended vaccines and covered insulin products will not
impact the calculation of the API for 2024 because the calculation is based on total drug

132
spending. Our estimate of API includes expected increases in the total drug spending as a result
of additional coverage required for ACIP-recommended vaccines and covered insulin products
during January through July 2023.
Section 1860D-14(a)(4) of the Act requires CMS to use the annual percentage increase in the
CPI for the 12-month period ending in September of the previous year. The calculation also does
not involve a projection of the time period where the pharmacy price concession rule is effective.
Finally, the annual percentage increase in the CPI is determined using the actual September 2022
value as calculated by the Bureau of Labor Statistics and an estimate of the September 2023 CPI
based on projections from the President’s FY2024 Budget.
Comment: A commenter also requested more transparency as to how the value of the 1.09
adjustment that CMS made to the calculation of total gross covered drug costs for 2024 was
determined.
Response: We evaluated the impact of the change in coverage for ACIP-recommended vaccines
and covered insulin products according to Part D historic claims data in 2021 by using
continuance tables for the LIS and Non-LIS populations, and calculating the allowed cost
corresponding to the true out-of-pocket cost (TrOOP) threshold. The adjustments to the
calculation of the allowed cost at the catastrophic threshold are necessary because beneficiaries
take a longer time to reach the TrOOP threshold, and, thus, the catastrophic phase when they pay
less cost sharing prior to the catastrophic phase.
These adjustments have also been updated from those in the CY 2024 Advance Notice to reflect
that the low-income cost sharing subsidy, when applicable, will continue to count toward
TrOOP. As noted above, we clarify that when we stated in the CY 2024 Advance Notice that no
cost will be incurred by LIS and non-LIS beneficiaries for ACIP-recommended adult vaccines
and, therefore, no costs will count as TrOOP toward the OOP threshold for beneficiary
progression into the catastrophic phase, we were speaking only of the amount actually paid by
the beneficiary and not the low-income cost sharing subsidy amount.
Section E. Part D Calendar Year Employer Group Waiver Plans Prospective Reinsurance
Amount
Comment: One commenter supported our policy of paying prospective reinsurance amounts to
Part D EGWPs and recommended that CMS add a trend adjustment to the methodology so that
prospective reinsurance payments take into account the amount by which reinsurance is
projected to increase in the current payment year relative to the most recently reconciled
payment year.
Response: CMS thanks the commenter for their support and recommendation. We do not believe
it would be appropriate to adjust prospective reinsurance payments for CY 2024 by a trend factor

133
when we did not propose to do so in the Advance Notice. Although we decline to add a trend
factor at this time, we will consider this recommendation as we continue to refine our
methodology for future years
Section F. Part D Risk Sharing
Comment: A commenter suggested that CMS consider narrowing risk corridors to help manage
premium increases on beneficiaries.
Response: We appreciate the commenter’s suggestion. Under section 1860D-15(e)(3)(C) of the
Act and § 423.336(a)(2)(ii), CMS may establish a risk corridor with higher threshold risk
percentages for Part D risk sharing. However, the statute does not permit CMS to narrow the
corridors relative to the CY 2011 thresholds.

134
Attachment V. Final Updated Part D Benefit Parameters for Defined Standard Benefit,
Low-Income Subsidy, and Retiree Drug Subsidy
Table V-1. Updated API and CPI for 2024
Annual percentage
trend for 2023
Prior year
revisions
API for 2024
API
6.42%
1.50%
8.01%
September CPI (all items, U.S. city average)
3.81%
3.87%
7.83%
Table V-2. Updated Part D Benefit Parameters for Defined Standard Benefit, Low-Income
Subsidy and Retiree Drug Subsidy
2023
2024
42
Standard Benefit
Deductible
$505
$545
Initial Coverage Limit
$4,660
$5,030
Out-of-Pocket Threshold
$7,400
$8,000
Total Covered Part D Spending a t Out-of-Pocket Threshold for Non-
Applicable Beneficiaries (1)(6)
$10,516.25
$11,477.39
Estimated Total Covered Part D Spending for Applicable Beneficiaries
(2)(6)
$11,206.28
$12,447.11
Minimum Cost Sharing in Catastrophic Coverage Portion of the Benefit
Generic/Preferred Multi-Source Drug
$4.15
Not Applicable
Other
$10.35
Not Applicable
Full Subsidy-Full Benefit Dual Eligible (FBDE) Beneficiaries (3)
Deductible
$0.00
$0.00
Copayments for Institutionalized Beneficiaries [category code 3]
Copayments for Beneficiaries Receiving Home and Community-Based
Services] [category code 3] (4)
$0.00
$0.00
Maximum Copayments for Non-Institutionalized Beneficiaries
Up to or at 100% FPL [category code 2]
Up to Out-of-Pocket Threshold
$0.00
$0.00
Generic/Preferred Multi-Source Drug
$1.45
$1.55
Other
$4.30
$4.60
Above Out-of-Pocket Threshold
Between 100% and 150% of FPL [category code 1]
Up to Out-of-Pocket Threshold
$0.00
Not Applicable
Generic/Preferred Multi-Source Drug
$4.15
$4.50
Other $10.35 $11.20
Above Out-of-Pocket Threshold
$0.00
Not Applicable
42
These parameters reflect additional plan coverage required for covered insulin products under section 1860D-2(b)(9) of the
Act, as added by section 11406 of the IRA, and ACIP-recommended vaccines under section 1860D-2(b)(8) of the Act, as added
by section 11401 of the IRA.

135
2023
2024
42
Full Subsidy-Non-FBDE Beneficiaries (3)
Applied or eligible for QMB/SLMB/QI or SSI, income at or below 135%
FPL in 2023 or at or below 150 % FPL for 2024 and beyond and
resources ≤ $9,090 (individuals, 2023) or ≤ $13,630 (couples, 2023)
[category code 1] (5)
Deductible
$0.00
$0.00
Maximum Copayments up to Out-of-Pocket Threshold
Generic/Preferred Multi-Source Drug
$4.15
$4.50
Other
$10.35
$11.20
Maximum Copayments above Out-of-Pocket Threshold
$0.00
Not
Applicable
Partial Subsidy (3) (Revised to Full Subsidy Effective 1/1/24)
Applied and income below 150% FPL and resources below $15,160
(individual, 2023) or $30,240 (couples, 2023) [category code 4] 5
Deductible
$104
Not Applicable
Coinsurance up to Out-of-Pocket Threshold
15%
Not Applicable
Maximum Copayments above Out-of-Pocket Threshold
Generic/Preferred Multi-Source Drug
$4.15
Not Applicable
Other
$10.35
Not Applicable
Retiree Drug Subsidy Amounts
Cost Threshold $505 $545
Cost Limit
$10,350
$11,200
(1) For a beneficiary who is not considered an “applicable beneficiary,” as defined at section
1860D-14A(g)(1) of the Act, and is not eligible for the Medicare Coverage Gap Discount
Program, this is the amount of total drug spending required to reach the OOP threshold in the
defined standard benefit. There is a 1 percent adjustment for the estimated total covered Part D
spending at catastrophic for non-applicable beneficiaries because beneficiaries take a longer time
to reach the catastrophic phase threshold when they pay less cost sharing for insulins and vaccines
(no more than a $35 copay per month’s supply of each covered insulin product and a $0 copay on
ACIP-recommended adult vaccines) under the 2024 defined standard benefit. This adjustment has
been updated from the 7 percent adjustment in the CY 2024 Advance Notice to reflect that the
low-income cost sharing subsidy, when applicable, will continue to count toward TrOOP.
(2) For a beneficiary who is an “applicable beneficiary,” as defined at section 1860D-
14A(g)(1) of the Act, and is eligible for the Medicare Coverage Gap Discount Program, this is the
estimated average amount of total drug spending required to reach the OOP threshold in the
defined standard benefit. There is a 3 percent adjustment for the estimated total covered Part D
spending at catastrophic for applicable beneficiaries. This adjustment has been updated from the 9
percent adjustment in the CY 2024 Advance Notice to account for the fact that beneficiaries take
a longer time to reach the catastrophic phase threshold when they pay less cost sharing for
insulins and vaccines (no more than a $35 copay per month’s supply of each covered insulin
136
product and a $0 copay on ACIP-recommended adult vaccines) under the 2024 defined standard
benefit.
(3) The LIS eligibility categories and corresponding cost-sharing benefits are sometimes
referred to using category codes as follows:
• Category Code 1 – Non-institutionalized FBDE beneficiaries with incomes between 100%
and 150% of FPL (beginning in CY 2024) and full-subsidy-non-FBDE beneficiaries. Note
that LIS beneficiaries that would previously fall into category code 4 fall into category
code 1 beginning in CY 2024 – see note for category code 4 below.
• Category Code 2 – Non-institutionalized FBDE beneficiaries with incomes up to 100% of
the FPL.
• Category Code 3 – FBDE beneficiaries who are institutionalized or would be
institutionalized if they were not receiving home and community-based services.
• Category Code 4 – Partial subsidy beneficiaries through CY 2023. Beneficiaries with
incomes between 135 percent and 150 percent of the FPL, who meet the resource
standards under either of sections 1860D-14(a)(3)(D) or (E) of the Act, and who would
have been eligible for the partial LIS benefit absent the enactment of the IRA, will be
eligible for the full LIS benefit. These category 4 beneficiaries will now have the same
Part D benefit parameters as beneficiaries in category 1 of the LIS. Category 2 and 3 of
the LIS remain unchanged.
(4) Per section 1860D-14(a)(1)(D)(i) of the Act, full-benefit dually eligible beneficiaries who
are receiving home and community-based services qualify for zero cost sharing if the individuals
(or couple) would have been institutionalized otherwise.
(5) The resource limits for CY 2024 will be provided via the annual HPMS memo entitled
“2024 Resource and Cost-Sharing Limits for Low-Income Subsidy (LIS)” that is expected to be
released during the usual timeframe after the September 2023 CPI has been made available by the
Bureau of Labor Statistics. Additionally, these amounts include $1,500 per person for burial
expenses. Also, beneficiaries that would have been eligible for the partial LIS benefit had the IRA
not been enacted will be eligible for the full LIS benefit if they meet either of the resource
standard described at sections 1860D-14(a)(3)(D) or (E) of the Act.
(6) The allowed amounts for total covered Part D spending at the out-of-pocket threshold
reflect the slower progression through the benefit due to the new requirements for covered insulin
products and ACIP-recommended vaccines at sections 1860D-2(b)(9) and 1860D-2(b)(8) of the
Act. For non-LIS beneficiaries, these amounts reflect that the manufacturer Coverage Gap
Discount will be calculated similarly for covered insulin products, ACIP-recommended vaccines,
and other drugs. For LIS beneficiaries, these amounts reflect that the low-income cost sharing
subsidy, when applicable, will continue to count toward TrOOP.

137
Section A. Annual Percentage Increase in Consumer Price index
Annual Percentage Increase in Consumer Price Index, September (September CPI)
Section 1860D-14(a)(4) of the Act requires CMS to use the annual percentage increase in the
CPI for the 12-month period ending in September 2023 to update the maximum copayments up
to the out-of-pocket threshold for full-benefit dually eligible enrollees with incomes not
exceeding 100 percent of the Federal Poverty Level. These copayments are increased from $1.45
per generic, preferred drug that is a multi-source drug, or biosimilar, and from $4.30 for all other
drugs in 2023 and rounded to the nearest multiple of $0.05 and $0.10 respectively.
43
Section B. Calculation Methodology
Annual Percentage Increase in Average Expenditures for Part D Drugs per Eligible
Beneficiary (API)
For contract years 2006 and 2007, the APIs, as defined in section 1860D-2(b)(6) of the Act, were
based on the National Health Expenditure (NHE) prescription drug per capita estimates because
sufficient Part D program data was not available. Beginning with contract year 2008, the APIs
are based on Part D program data. For the CY 2024 benefit parameters, Part D program data will
be used to calculate the annual percentage trend as follows:
2022– 2023
2021– 2022
= $4,916.80/$4,620.25=1.064
In the formula, the average per capita cost for August 2021 – July 2022 is calculated from actual
Part D PDE data, and the average per capita cost for August 2022 – July 2023 is calculated based
on actual Part D PDE data for prescription drug claims with service dates from August 2022 –
December 2022 and projected through July 2023.
The 2024 benefit parameters reflect the 2023 annual percentage trend, as well as an update for
revision to prior year estimates for API. Based on updated NHE prescription per capita costs and
PDE data, the annual percentage increases are now calculated as summarized by Table V-3.
Table V-3. Revised Prior Years’ Annual Percentage Increases
Year
Prior Estimates of
Annual Percentage
Trend
Revised Annual
Percentage Trend
2006
7.30%
7.30%
2007
5.92%
5.92%
2008
4.69%
4.69%
43
Per section 1860D-14(a)(4)(A) of the Act, the copayments are increased from the unrounded 2023 values of $4.1508 for multi-
source generic or preferred drugs, and $10.3507 for all other drugs.

138
Year
Prior Estimates of
Annual Percentage
Trend
Revised Annual
Percentage Trend
2009
3.14%
3.14%
2010
2.36%
2.36%
2011
2.15%
2.15%
2012
2.53%
2.53%
2013
-3.14%
-3.14%
2014
10.12%
10.12%
2015
9.89%
9.89%
2016
4.02%
4.02%
2017
1.87%
1.87%
2018
4.05%
4.05%
2019
4.92%
4.92%
2020
5.06%
5.06%
2021
4.69%
4.69%
2022
5.80%
7.37%
Accordingly, the CY 2024 benefit parameters reflects a multiplicative update of 1.50 percent for
prior year revisions. In summary, the outlined in Section A are updated by 8.01 percent for, as
summarized by Table V-4.
Table V-4. Annual Percentage Increase
Annual percentage trend for July 2023 6.42%
Prior year revisions 1.50%
Annual percentage increase for 2024 8.01%
Note: Percentages are multiplicative, not additive. Values are carried to additional decimal places
and may not agree to the rounded values presented above.
Annual Percentage Increase for Out-of-Pocket Threshold
In accordance with section 1860D-2(b)(4)(B), we calculated the change in the out-of-pocket
threshold using the 2023 threshold value of $7,400 as our starting point. To calculate the 2024
value, we applied the 2024 API described above and rounded to the nearest $50. The resulting
2024 out-of-pocket threshold value is $8,000.
Annual Percentage Increase in Consumer Price Index, September (September CPI)
To ensure that plan sponsors and CMS have sufficient time to incorporate cost-sharing
requirements into the development of the benefit, any marketing materials, and necessary

139
systems, CMS includes in its methodology to calculate the annual percentage increase in the CPI
for the 12-month period ending in September 2023, an estimate of the September 2023 CPI
based on projections from the President’s FY2024 Budget.
The September 2022 value is from the Bureau of Labor Statistics. The annual percentage trend in
the September CPI for CY 2024 is calculated as follows:
Projected September 2023 CPI
Actual September 2022 CPI
or $308.1/$296.8=1.038
(Source: President’s FY2024 Budget and Bureau of Labor Statistics, Department of
Labor)
The CY 2024 benefit parameters reflects the CY 2023 annual percentage trend in the September
CPI of 3.81 percent, as well as a 3.87 percent multiplicative correction for the revision to last
year’s estimate. The CY 2023 annual percentage trend in the CPI can be found in Table V-5
below.
Table V-5. Cumulative Annual Percentage Increase in September CPI
Annual percentage trend for September 2023
3.81%
Prior year revisions
3.87%
Annual percentage increase for 2024
7.83%
Note: Percentages are multiplicative, not additive. Values are carried to
additional decimal places and may not agree to the rounded values presented
above.
Section C. Annual Percentage Increase in Average Expenditures for Part D Drugs per
Eligible Beneficiary (API)
Section 1860D-2(b)(6) of the Act defines the API as “the annual percentage increase in average
per capita aggregate expenditures for covered Part D drugs in the United States for Part D
eligible individuals, as determined by the Secretary for the 12-month period ending in July of the
previous year using such methods as the Secretary shall specify.” The following defined standard
Part D prescription drug benefit parameters are updated using the “annual percentage increase”:
Deductible: From $505 in 2023 and rounded to the nearest multiple of $5.
Initial Coverage Limit: From $4,660 in 2023 and rounded to the nearest multiple of $10.
Out-of-Pocket Threshold: From $7,400 in 2023 and rounded to the nearest multiple of $50.
Maximum Copayments up to the Out-of-Pocket Threshold for Certain Low-Income Full
Subsidy Eligible Beneficiaries: From $4.15 per generic, preferred drug that is a multi-source

140
drug, or biosimilar and $10.35 for all other drugs in CY 2023, rounded to the nearest multiple of
$0.05.
Table V-6. Part D Benefit Parameters for Defined Standard Benefit for 2023 and 2024 for
Non-LIS Beneficiaries
2023
2024
44
Deductible
Phase
Cost sharing: 100% Cost sharing: 100%
Deductible: $505 Deductible: $545
Initial
Coverage
Phase
Cost sharing: 25% Cost sharing: 25%
Initial Coverage Limit: $4,660 Initial Coverage Limit: $5,030
Coverage Gap
Applicable
Drugs:
Cost sharing:
25% (1)
Non-applicable
Drugs
Cost sharing:
25%
Applicable
Drugs
Cost sharing:
25% (1)
Non-applicable
Drugs
Cost sharing:
25%
Out-of-Pocket Threshold: $7,400 Out-of-Pocket Threshold: $8,000
Catastrophic
Coverage
Cost sharing: Greater of 5% or
$4.15 (Generic/Preferred Multi-
Source Drug) / $10.35 (Other)
Cost Sharing: 0%
(1) The 25% coinsurance for applicable drugs for non-LIS beneficiaries during the coverage
gap reflects the application of the 70% Medicare Coverage Gap Discount Program discount.
Section D. Estimated Total Covered Part D Spending at Out-of-Pocket Threshold for
Applicable Beneficiaries
For CY 2024, the estimated total gross covered prescription drug costs at the out-of-pocket
threshold for applicable beneficiaries will be calculated given the following basic assumptions:
• 100 percent beneficiary cost-sharing in the deductible phase.
• 25 percent beneficiary cost-sharing in the initial coverage phase.
• 25 percent beneficiary cost-sharing for non-applicable drugs purchased in the coverage
gap phase of the benefit.
44
These parameters reflect additional plan coverage required for covered insulin products under section 1860D-2(b)(9) of the
Act, as added by section 11406 of the IRA, and ACIP-recommended vaccines under section 1860D-2(b)(8) of the Act, as added
by section 11401 of the IRA.

141
• 95 percent cost-sharing for the ingredient cost and sales tax for applicable drugs
purchased in the coverage gap phase of the benefit—consisting of 25 percent beneficiary
coinsurance and 70 percent Medicare Coverage Gap Discount Program discount.
• 25 percent cost-sharing for the dispensing of applicable drugs and vaccine administration
fees not associated with ACIP-recommended vaccines drugs purchased in the coverage
gap phase of the benefit.
In this estimate, it is assumed that the dispensing and vaccine administration fees account for
0.042 percent of the gross covered brand drug costs used by non-LIS beneficiaries in the
coverage gap. Therefore, a 75 percent reduction in cost-sharing for dispensing and vaccine
administration fees results in an overall reduction of 0.030 percent to 94.970 percent in cost-
sharing for applicable (brand) drugs in the coverage gap.
The CY 2024 calculation of the estimated total gross covered prescription drug costs at out-of-
pocket (OOP) threshold for applicable beneficiaries is as follows:
(ICL+ )
100% beneficiary cost sharing in the gap
weighted gap coinsurance factor
∗
($5,030 + )
$6,333.75
89.782%
∗ 1.03 = $12,447.11
• ICL is the Initial Coverage Limit equal to $5,030.
• Insulin and Vaccine Adjustment=1.03.
• 100 percent beneficiary cost sharing in the gap is the estimated total drug spending in the
gap assuming 100 percent coinsurance and is equivalent to:
(OOP threshold) – (OOP costs up to the ICL) or $8,000 − $1,666.25 = $6,333.75
Weighted gap coinsurance factor is calculated as follows:
(Brand Gross Drug Cost Below Catastrophic [GDCB] % for non-LIS × gap cost
sharing for applicable drugs) + (Generic GDCB % for non-LIS × 25% gap cost
sharing for non-applicable drugs)
or
(92.59% × 94.970%) + (7.41% × 25.00%) = 89.782%
o Brand GDCB % for non-LIS is the percentage of gross covered drug costs below
the OOP threshold for applicable beneficiaries (i.e., non-LIS) attributable to
applicable drugs, as reported on the 2022 PDEs.

142
o Gap cost sharing for applicable drugs is the coinsurance incurred by applicable
beneficiaries (i.e., non-LIS) for applicable drugs in the coverage gap, where:
Coinsurance for applicable drugs is calculated as follows:
• [(percentage of gross covered brand drug costs attributable to
ingredient cost and sales tax) × (cost-sharing percentage)] + [(percentage
of gross covered brand drug costs attributable to dispensing and vaccine
administration fees not associated with ACIP-recommended vaccines) ×
(cost-sharing coinsurance percentage)]
or
94.970% = [(99.958% × 95%) + (0.042% × 25%)]
o Generic GDCB % for non-LIS is the percentage of gross covered drug costs
below the OOP threshold for applicable beneficiaries (i.e., non-LIS) attributable
to non-applicable drugs as reported on the 2022 PDEs.
Gap cost sharing for non-applicable drugs is the coinsurance incurred by
applicable beneficiaries (i.e., non-LIS) for non-applicable drugs in the coverage
gap.
Table V-7. Updated Total Gross Covered Drug Costs at the Out-of-Pocket Threshold
for Applicable and Non-Applicable Beneficiaries in CY 2024
2023
2024
45
Total Gross Covered Drug Costs at Out-of-Pocket Threshold for Non-
Applicable Beneficiaries (1) $10,516.25 $11,477.39
Estimated Total Gross Covered Drug Costs for Applicable
Beneficiaries (2)
$11,206.28
$12,447.11
(1) For a beneficiary who is not considered an “applicable beneficiary,” as defined at section
1860D-14A(g)(1) of the Act, and is not eligible for the Medicare Coverage Gap Discount
Program, this is the amount of total drug spending required to reach the OOP threshold in the
defined standard benefit.
(2) For a beneficiary who is an “applicable beneficiary,” as defined at section 1860D-
14A(g)(1) of the Act, and is eligible for the Medicare Coverage Gap Discount Program, this is the
estimated average amount of total drug spending required to reach the OOP threshold in the
defined standard benefit.
45
These figures have been updated from those in the CY 2024 Advance Notice to reflect the fact that beneficiaries take a longer
time to reach the catastrophic phase threshold when they pay less cost sharing for insulins and vaccines (no more than $35 copay
per month’s supply of each insulin product and $0 copay on ACIP-recommended adult vaccines) under the 2024 defined standard
benefit.

143
Section E. Retiree Drug Subsidy Amounts
Per 42 CFR 423.886(b)(3), the cost threshold and cost limit for qualified retiree prescription drug
plans are updated using the API, as defined previously in this document. The updated cost
threshold is rounded to the nearest multiple of $5 and the updated cost limit is rounded to the
nearest multiple of $50. The cost threshold and cost limit are defined as $505 and $10,350,
respectively, for plans that end in CY 2023, and as $545 and $11,200 for plans that end in CY
2024.
Table V-8. Updated Retiree Drug Subsidy Amounts in 2024
2023
2024
Retiree Drug Subsidy Amounts
Cost Threshold
$505 $545
Cost Limit
$10,350
$11,200

144
Attachment VI. Updates for Part C and D Star Ratings
Part C and D Star Ratings and Future Measurement Concepts
The Part C and D Star Ratings measure the quality of and reflect the experiences of beneficiaries
in Medicare Advantage (MA) and Prescription Drug Plans (PDPs or Part D plans), assist
beneficiaries in finding the best plan for their needs, and determine eligibility for MA Quality
Bonus Payments. The Star Ratings support CMS’ efforts to make the patient the focus in all of
our programs and to create incentives to eliminate health disparities.
The methodology for the Star Ratings system for the Part C and D programs is codified at §§
422.160 - 422.166 and 423.180 - 423.186. In the Advance Notice, we provided information and
updates as required by §§ 422.164(c)(2), (d), (e)(2) and (f)(1); 422.166(f)(2); 423.184(c)(2), (d),
(e)(2), and (f)(1); and 423.186(f)(2). We appreciate the feedback we received on potential future
measures and concepts for the Star Ratings. We reviewed the comments and will consider them
as we identify future enhancements to the Star Ratings program. Some commenters requested
additional resources to track current and future Star Ratings measures and methodological
enhancements. We will consider making additional resources available to help Part C and D
sponsors keep track of future changes.
Reminders for 2024 Star Ratings
CMS finalized the application of Tukey outlier deletion for non-CAHPS measures beginning
with the 2024 Star Ratings in the CY 2021 final rule (85 FR 33832-36).
46
We also finalized the
addition of the Transitions of Care and Follow-up after Emergency Department Visit for Patients
with Multiple Chronic Conditions measures to be added to the 2024 Star Ratings in the CY 2022
final rule (86 FR 5921-26). Additionally, the Plan All-Cause Readmissions measure will be
returned to the 2024 Star Ratings after being delayed due to the suspended collection of CAHPS
and HEDIS data in 2020.
47
We provide various datasets and reports to plan sponsors throughout the year. Part C and D
sponsors should regularly review their underlying measure data that are the basis for the Star
46
In the CY 2021 final rule, we finalized use of Tukey outlier deletion effective for the Star Ratings issued in October 2023 and
subsequent years. (85 FR 33833-36) In the rulemakings since that time, we have not proposed to eliminate the Tukey outlier
deletion aspect of the Star Ratings methodology. As we stated in May 2022 final rule (87 FR 27766), we will implement Tukey
outlier deletion beginning with the 2024 Star Ratings to help improve stability of cut points and prevent cut points from being
influenced by outliers. However, it appears that the sentence in §§ 422.166(a)(2)(i) and 423.186(a)(2)(i) (“Effective for the Star
Ratings issued in October 2023 and subsequent years, prior to applying mean resampling with hierarchal clustering, Tukey outer
fence outliers are removed.”) was inadvertently removed from the codified regulation text. In the Medicare Program; Contract
Year 2024 Policy and Technical Changes to the Medicare Advantage Program, Medicare Prescription Drug Benefit Program,
Medicare Cost Plan Program, Medicare Parts A, B, C, and D Overpayment Provisions of the Affordable Care Act and Programs
of All-Inclusive Care for the Elderly; Health Information Technology Standards and Implementation Specifications proposed rule
which appeared in the Federal Register on December 27, 2022 (hereinafter referred to as the December 2022 proposed rule) (87
FR 79452), we proposed a technical amendment to fix this codification error from the May 2022 final rule.
47
See the Announcement of Calendar Year (CY) 2022 Medicare Advantage (MA) Capitation Rates and Part C and Part D
Payment Policies, page 97.

145
Ratings and immediately alert CMS if errors or anomalies are identified so any issues can be
resolved prior to the first plan preview period.
As described at §§ 422.164(h) and 423.184(h), CMS annually sets and announces a deadline for
MA and Part D organizations to request that CMS or the Independent Review Entity (IRE)
review its Part C appeals data or CMS review its Complaints Tracking Module (CTM) data.
CMS is announcing a deadline of June 30, 2023 for all contracts to make their requests for
review of the 2022 appeals and CTM measure data for the 2024 Star Ratings. Sponsoring
organizations can view and monitor their Part C appeals timeliness and effectuation compliance
data on the Medical Appeal Search website. Sponsoring organizations should refer to the May
10, 2019 HPMS memorandum, “Complaints Tracking Module (CTM) File Layout Change and
Updated Standard Operating Procedures,” for instructions on how to request a review of CTM
data.
Measure Updates for 2024 Star Ratings
The measures that will be used to calculate the 2024 Star Ratings are listed in Table VI-1 with
information about the measure type, weight, and measurement year.
Table VI-1: 2024 Star Ratings Measures
Part C
or D
Measure
Measure Type
Weight
Measurement
Year
Improvement
Measure
Included in
the 2024 CAI
Values
C
Breast Cancer
Screening
Process Measure
1
1/1/2022 –
12/31/2022
Yes
Yes
C
Colorectal Cancer
Screening
Process Measure
1
1/1/2022 –
12/31/2022
Yes
Yes
C
Annual Flu Vaccine
Process Measure
1
3/2023 – 6/2023
Yes
Yes
C
Controlling Blood
Pressure
Intermediate
Outcome
Measure
3
1/1/2022 –
12/31/2022
Yes
Yes
C
Monitoring Physical
Activity
Process Measure
1
7/2022 –
11/2022
Yes
Yes
C
Special Needs Plan
(SNP) Care
Management
Process Measure
1
1/1/2022 –
12/31/2022
Yes
No
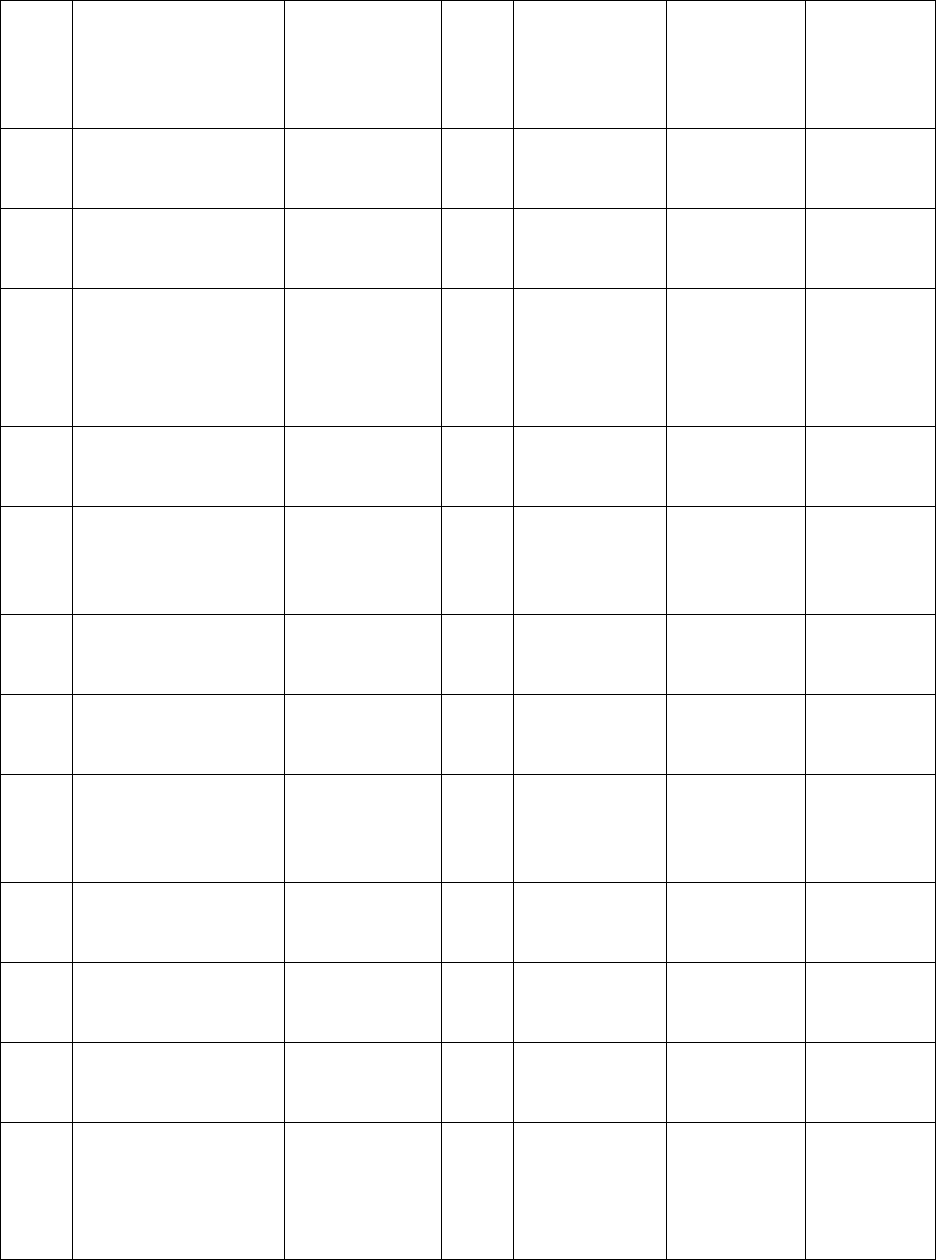
146
Part C
or D
Measure
Measure Type
Weight
Measurement
Year
Improvement
Measure
Included in
the 2024 CAI
Values
C
Care for Older Adults –
Medication Review
Process Measure
1
1/1/2022 –
12/31/2022
Yes
No
C
Care for Older Adults–
Pain Assessment
Process Measure
1
1/1/2022 –
12/31/2022
Yes
No
C
Osteoporosis
Management
in
Women who had a
Fracture
Process Measure
1
1/1/2022 –
12/31/2022
Yes
Yes
C
Diabetes Care – Eye
Exam
Process Measure
1
1/1/2022 –
12/31/2022
Yes
Yes
C
Diabetes Care – Blood
Sugar Controlled
Intermediate
Outcome
Measure
3
1/1/2022 –
12/31/2022
Yes
Yes
C
Reducing the Risk of
Falling
Process Measure
1
7/2022 –
11/2022
Yes
Yes
C
Improving Bladder
Control
Process Measure
1
7/2022 –
11/2022
Yes
Yes
C
Medication
Reconciliation Post
-
Discharge
Process Measure
1
1/1/2022 –
12/31/2022
Yes
Yes
C
Plan All-cause
Readmissions
Outcome
Measure
1
1/1/2022 –
12/31/2022
No
No
C
Transitions of Care
Process Measure
1
1/1/2022 –
12/31/2022
No
No
C
Follow-up after
Emergency Room Visit
Process Measure
1
1/1/2022 –
12/31/2022
No
No
C
Getting Needed Care
Patients’
Experience and
Complaints
Measure
4
3/2023 – 6/2023
Yes
No

147
Part C
or D
Measure
Measure Type
Weight
Measurement
Year
Improvement
Measure
Included in
the 2024 CAI
Values
C
Getting Appointments
and Care Quickly
Patients’
Experience and
Complaints
Measure
4
3/2023 – 6/2023
Yes
No
C
Customer Service
Patients’
Experience and
Complaints
Measure
4
3/2023 – 6/2023
Yes
No
C
Rating of Health Care
Quality
Patients’
Experience and
Complaints
Measure
4
3/2023 – 6/2023
Yes
No
C
Rating of Health Plan
Patients’
Experience and
Complaints
Measure
4
3/2023 – 6/2023
Yes
No
C
Care Coordination
Patients’
Experience and
Complaints
Measure
4
3/2023 – 6/2023
Yes
No
C
Complaints about the
Health Plan
Patients’
Experience and
Complaints
Measure
4
1/1/2022 –
12/31/2022
Yes
No
C
Members Choosing to
Leave the Plan
Patients’
Experience and
Complaints
Measure
4
1/1/2022 –
12/31/2022
Yes
No
C
Health Plan Quality
Improvement
Improvement
Measure
5
NA
No
No
C
Plan Makes Timely
Decisions about
Appeals
Measures
Capturing Access
4
1/1/2022 –
12/31/2022
Yes
No

148
Part C
or D
Measure
Measure Type
Weight
Measurement
Year
Improvement
Measure
Included in
the 2024 CAI
Values
C
Reviewing Appeals
Decisions
Measures
Capturing Access
4
1/1/2022 –
12/31/2022
Yes
No
C
Call Center – Foreign
Language Interpreter
and TTY Availability
Measures
Capturing Access
4
2/2023 – 5/2023
Yes
No
C
Statin Therapy for
Patients with
Cardiovascular Disease
Process Measure
1
1/1/2022 –
12/31/2022
Yes
Yes
D
Call Center – Foreign
Language
Interpreter
and TTY Availability
Measures
Capturing Access
4
2/2023 – 5/2023
Yes
No
D
Complaints about the
Drug Plan
Patients’
Experience and
Complaints
Measure
4
1/1/2022 –
12/31/2022
Yes
No
D
Members Choosing to
Leave the Plan
Patients’
Experience and
Complaints
Measure
4
1/1/2022 –
12/31/2022
Yes
No
D
Drug Plan Quality
Improvement
Improvement
Measure
5
NA
No
No
D
Rating of Drug Plan
Patients’
Experience and
Complaints
Measure
4
3/2023 – 6/2023
Yes
No
D
Getting Needed
Prescription Drugs
Patients’
Experience and
Complaints
Measure
4
3/2023 – 6/2023
Yes
No
D
MPF Price Accuracy
Process Measure
1
1/1/2022 –
9/30/2022
Yes
No

149
Part C
or D
Measure
Measure Type
Weight
Measurement
Year
Improvement
Measure
Included in
the 2024 CAI
Values
D
Medication Adherence
for Diabetes
Medications
Intermediate
Outcome
Measure
3
1/1/2022 –
12/31/2022
Yes
Yes
D
Medication Adherence
for Hypertension (RAS
antagonists)
Intermediate
Outcome
Measure
3
1/1/2022 –
12/31/2022
Yes
Yes
D
Medication Adherence
for Cholesterol
(Statins)
Intermediate
Outcome
Measure
3
1/1/2022 –
12/31/2022
Yes
Yes
D
MTM Program
Completion Rate for
CMR
Process Measure
1
1/1/2022 –
12/31/2022
Yes
Yes
D
Statin Use in Persons
with Diabetes
Process Measure
1
1/1/2022 –
12/31/2022
Yes
Yes
Improvement Measures (Part C & D) for the 2024 Star Ratings. Under §§ 422.164(f) and
423.184(f), improvement measures are calculated using performance measures that meet specific
conditions. Table VI-1 includes information about which measures will be used to calculate the
improvement measures for the 2024 Star Ratings. As stated in §§ 422.164(f)(4)(i) and
423.184(f)(4)(i), CMS will only include measures in the improvement calculations at the contract
level if numeric value scores are available for both the current and prior year.
2024 Star Ratings Program and the Categorical Adjustment Index
The methodology for the Categorical Adjustment Index (CAI) is described at §§ 422.166(f)(2)
and 423.186(f)(2), as well as in the annual Medicare Part C & D Star Ratings Technical Notes
available on CMS’ Part C and D Star Ratings website. As finalized at §§ 422.166(f)(2) and
423.186(f)(2), all measures identified as candidate measures will be included in the
determination of the 2024 CAI values. The measure set for the 2024 CAI (for both Part C and D)
is identified in Table VI-1.
In keeping with our commitment to transparency, a summary of the analysis of the candidate
measure set that includes the minimum, median, and maximum values for the within-contract
variation for the low-income subsidy (LIS)/dual eligible (DE) differences are posted with the
2024 CAI values on CMS’ Part C and D Star Ratings website.
150
Commenters supported continuing the CAI. There were suggestions for adding additional
measures and identifying an alternative to the CAI. We will take these suggestions into
consideration; however, Star Ratings methodological changes must be adopted through
rulemaking. We also note that certain measures, such as the CAHPS measures, are excluded
from the CAI pursuant to §§ 422.166(f)(2)(ii)(A) and 423.186(f)(2)(ii)(A) because they are
already case-mix adjusted.
Extreme and Uncontrollable Circumstances Policy for the 2024 Star Ratings
Extreme and uncontrollable circumstances such as natural disasters can directly affect
Medicare beneficiaries and providers, as well as the Parts C and D organizations that provide
beneficiaries with important medical care and prescription drug coverage. An affected
contract is identified based on these criteria:
(1) Its service area is within an “emergency area” during an “emergency period” as
defined in section 1135(g)(1) of the Act;
(2) Its service area is within a geographic area designated in a major disaster
declaration under the Stafford Act and the Secretary exercised authority under
section 1135 of the Act based on the same triggering event(s); and
(3) A certain minimum percentage (25 percent or 60 percent) of the enrollees under
the contract must reside in a Federal Emergency Management Agency (FEMA)-
designated Individual Assistance area at the time of the extreme and uncontrollable
circumstance. (See §§ 422.166(i) and 423.186(i)).
We use the start date of the incident period to determine which year of Star Ratings could be
affected, regardless of whether the incident period extends to another calendar year (§§
422.166(i) and 423.186(i)).
Under the 25 percent rules at §§ 422.166(i)(2)–(6) and 423.186(i)(2)–(5), contracts with at
least 25 percent of their service area in a FEMA-designated Individual Assistance area in
2022 will receive the higher of their measure-level rating from the current and prior Star
Ratings years for purposes of calculating the 2024 Star Ratings (thus, for 2024 Star Ratings,
affected contracts will receive the higher of their measure-level ratings from 2023 or 2024
for the applicable measures). See also 84 FR 15770–77. The numeric scores for contracts
with 60 percent or more of their enrollees living in FEMA-designated Individual Assistance
areas at the time of the extreme and uncontrollable circumstance are excluded from: (1) the
measure-level cut point calculations for non-CAHPS measures; and (2) the performance
summary and variance thresholds for the reward factor as described at §§ 422.166(i)(9)(i)
and (i)(10)(i), and 423.186(i)(7)(i) and (i)(8)(i). Table VI-2 lists the emergency areas
affected by emergency declarations first issued in 2022, as defined in section 1135 of the
Act, and the exercise of the Secretary’s authority under section 1135 of the Act.

151
Table VI-2: List of Section 1135 Waivers Issued in Relation to the FEMA Major Disaster
Declarations
Section
1135
Waiver
Date
Issued
Waiver or Modification
of Requirements Under
Section 1135 of the
Social Security Act
FEMA
Incident
Type
Affected
State
Incident
Start
Date
5/9/2022
New Mexico Wildfires
and Straight-line Winds
Wildfires
New Mexico
4/5/2022
8/2/2022
Kentucky Severe Storms,
Flooding, Landslides, and
Mudslides
Severe
Storms,
Flooding,
Landslides,
and
Mudslides
Kentucky
7/26/2022
9/20/2022
Tropical Storm/Hurricane
Fiona
Hurricane
Puerto Rico
9/17/2022
9/26/2022
Hurricane Ian
Hurricane
Florida
9/23/2022
9/30/2022
Hurricane Ian
Hurricane
South Carolina
9/25/2022
Table VI-3 lists the states and territories with Individual Assistance designations from the
FEMA major disaster declarations.

152
Table VI-3: Individual Assistance Counties and County-Equivalents in FEMA Major
Disaster Declared States/Territories
FEMA
Declaration
State
FEMA Individual Assistance Counties or County-
Equivalents
DR-4652-
NM
New
Mexico
Colfax, Lincoln, Mora, San Miguel, Valencia
DR-4663-
KY
Kentucky
Breathitt, Clay, Floyd, Knott, Lee, Leslie, Letcher,
Magoffin, Martin, Owsley, Perry, Pike, Whitley
DR-4671-
PR
Puerto
Rico
Adjuntas, Aguada, Aguadilla, Aguas Buenas, Aibonito,
Anasco, Arecibo, Arroyo, Barceloneta, Barranquitas,
Bayamon, Cabo Rojo, Caguas, Camuy, Canovanas,
Carolina, Catano, Cayey, Ceiba, Ciales, Cidra, Coamo,
Comerio, Corozal, Culebra, Dorado, Fajardo, Florida,
Guanica, Guayama, Guayanilla, Guaynabo, G
urabo,
Hatillo, Hormigueros, Humacao, Isabela, Jayuya, Juana
Diaz, Juncos, Lajas, Lares, Las Marias, Las Piedras, Loiza,
Luquillo, Manati, Maricao, Maunabo, Mayaguez, Moca,
Morovis, Naguabo, Naranjito, Orocovis, Patillas, Penuelas,
Ponce, Quebradillas, Rin
con, Rio Grande, Sabana Grande,
Salinas, San German, San Juan, San Lorenzo, San
Sebastian, Santa Isabel, Toa Alta, Toa Baja, Trujillo Alto,
Utuado, Vega Alta, Vega Baja, Vieques, Villalba, Yabucoa,
Yauco
DR-4673-
FL
Florida
Brevard, Charlotte, Collier, DeSoto, Flagler, Glades,
Hardee, Hendry, Highlands, Hillsborough, Lake, Lee,
Manatee, Monroe, Okeechobee, Orange, Osceola, Palm
Beach, Pasco, Pinellas, Polk, Putnam, Sarasota, Seminole,
St. Johns, Volusia
DR-4677-
SC
South
Carolina
Charleston, Georgetown, Horry
Changes to Existing Star Ratings Measures for the 2023 Measurement Year and Beyond
CMS solicits feedback on new measure concepts as well as measure updates through the annual
Advance Notice and Rate Announcement process. We also provide advance notice regarding
measures considered for implementation as future Star Ratings measures. As codified at §§
422.164(c)(2)–(4), 423.184(c)(2)–(4), 422.164(d)(2), and 423.184(d)(2), new measures and
measures with substantive specification changes must be added or updated through rulemaking,
and must remain on the display page for at least two years prior to becoming a Star Ratings
measure. In addition, CMS uses the Advance Notice and Rate Announcement process to
announce non-substantive specification changes as described at §§ 422.164(d)(1) and
423.184(d)(1) and to remove measures as described at §§ 422.164(e) and 423.184(e). We
described a number of measure concepts and changes in the Advance Notice and summarize

153
significant comments on those issues here. We encourage interested parties to provide comments
directly to measure developers during their public comment periods. For example, the National
Committee for Quality Assurance (NCQA) and the Pharmacy Quality Alliance (PQA) regularly
solicit public comments on new measures, changes to existing measures, and measure
retirements.
As part of the CMS National Quality Strategy and Medicare Value-Based Care Strategy, CMS is
committed to aligning a subset of measures across all our programs and ensuring we measure
quality across the entire care continuum in a way that promotes the best, safest, and most
equitable care for all individuals. Improving alignment of measures across federal programs and
with private payers will reduce provider burden while also improving the effectiveness and
comparability of measures across quality programs. Across our CMS quality rating and value-
based care programs, where applicable, we are considering including what CMS is calling a
“Universal Foundation”
48
of quality measures which is a subset of measures that are aligned
across programs. This “Universal Foundation” is a building block to which programs will add
additional aligned or program-specific measures. As a start, each program is considering which
measures included in the “Universal Foundation” are not currently in their programs and the
steps to add them over time if appropriate.
Having this “Universal Foundation” will support efforts to ensure high quality care for the more
than 150 million Americans covered by our programs and serve as an alignment standard for the
rest of the health care system. The “Universal Foundation” will 1) focus provider attention, 2)
reduce provider burden, 3) allow for consistent stratification of measures to identify disparities in
care, 4) accelerate the transition to interoperable, digital quality measures, and 5) allow for cross-
comparisons across quality and value-based care programs, to better understand what drives
quality and equity improvement and what does not. The preliminary set of measures included in
the Adult “Universal Foundation” are listed in Table VI-4 with information about whether the
measures are currently in the Star Ratings program. The set of measures will evolve over time to
meet the needs of individuals served across CMS program.
Table VI-4: Preliminary Adult Universal Foundation Measures
Meaningful
Measure 2.0
Domain
Measure
Part C and D Star Ratings
Wellness and
Prevention
Colorectal Cancer Screening (HEDIS)
Currently in Star Ratings
Breast Cancer Screening (HEDIS)
Currently in Star Ratings
48
https://www.nejm.org/doi/full/10.1056/NEJMp2215539?query=featured_homeye

154
Meaningful
Measure 2.0
Domain
Measure
Part C and D Star Ratings
Adult Immunization Status (HEDIS)
Solicited feedback on this measure
in the Advance Notice
Chronic
Conditions
Controlling High Blood Pressure
(HEDIS)
Currently in Star Ratings
Diabetes: Hemoglobin A1c Poor
Control (>9%) (HEDIS)
Currently in Star Ratings (reversed
score so higher scores are better)
Behavioral
Health
Screening for Depression and Follow-
Up Plan (HEDIS)
Solicited feedback on this measure
in the Advance Notice
Initiation and Engagement of Substance
Use Disorder Treatment (HEDIS)
Currently on display page
Seamless care
coordination
Plan all-cause readmissions or Hospital
all-cause readmissions (HEDIS)
Currently in Star Ratings
Person-centered
care
Consumer Assessment of Healthcare
Providers and Systems (CAHPS):
Overall Rating Measures (CAHPS)
Currently in Star Ratings
Equity
Screening for Social Drivers of Health/
Social Need Screening and Intervention
(HEDIS)
Solicited feedback in the 2023
Advance Notice/Rate
Announcement about the NCQA
measure focused on Screening and
Referral to Services for Social
Needs
There was overwhelming support from commenters regarding CMS’ goal of aligning measures
across federal and private payers, and many of the commenters applauded CMS for its leadership
and efforts to streamline quality and performance measures across its many programs. Many
commenters agreed that aligning health plans and providers on a streamlined set of quality
measures could reduce administrative burden and ensure everyone is working toward the same
patient goals and outcomes. A small number of commenters suggested a variety of different
measures to add to the Universal Foundation, including measures related to women’s health
issues, tobacco use screening and intervention, patient safety, Part D medication adherence, rare
diseases, and patient activation. A commenter recommended measures that support primary care
providers, such as measures focused on relationships, access to care, comprehensiveness of care,
trust in physicians, and person-centeredness. Other commenters suggested a focus on outcome
measures rather than process measures. A handful of commenters raised issues related to the
newer measures under the Universal Foundation and whether electronic health records and the
electronic clinical data systems (ECDS) were available and ready to support accurate data
collection for these measures. Other commenters wanted more information about what programs
155
would be included in the Universal Foundation, timelines for implementing new measures in
each program included in the Universal Foundation, and how measures will be added to or
removed from the Universal Foundation over time as the focus evolves.
There was mixed reaction to some of the measures in the Universal Foundation. For Social Need
Screening and Intervention, some commenters strongly supported including this measure, but
others were concerned about data collection issues with this measure and challenges of having
clinicians screen for issues that they are not adequately able to address. We also received
feedback on the Adult Immunization Status, Initiation and Engagement of Substance Use
Disorder (SUD) Treatment, and Depression Screening and Follow-up measures; this feedback is
described below under the Display Measures section. We will take these comments into
consideration as we move forward. Any additional measures added to the Star Ratings would
need to go through rulemaking.
Optional Exclusions for HEDIS Measures (Part C). For selected HEDIS measures, plans may
choose whether or not they applied optional exclusions. NCQA reviewed all applicable HEDIS
measures to determine whether the optional exclusions could be required. NCQA is making
updates to the following Star Ratings and display measures for measurement year 2023 (2025
Star Ratings):
• Controlling Blood Pressure: The optional exclusions for pregnancy, end-stage renal
disease/dialysis/nephrectomy/kidney transplant, and non-acute inpatient admissions are
now required.
• Colorectal Cancer Screening: The optional exclusions for colorectal cancer and total
colectomy are now required.
• Kidney Health Evaluation for Patients with Diabetes: The optional exclusions for
polycystic ovary syndrome, gestational diabetes, and steroid-induced diabetes are now
required.
For all HEDIS measures that are part of the Star Ratings and display page, the optional exclusion
for enrollees who died during the measurement year became a required exclusion for
measurement year 2023. These updates would be non-substantive under § 422.164(d)(1)(i) since
they narrow the population covered under the measures. Most commenters supported making the
optional exclusions required. We have shared feedback received with NCQA.
Care for Older Adults (COA) – Pain Assessment (Part C). NCQA is considering retiring the
COA Pain Assessment indicator from the HEDIS measurement set for the following reasons: 1)
pain assessments should be multidimensional, and the current indicator cannot ensure this; 2) the
current indicator does not differentiate between acute and chronic pain; and 3) the measure also
does not assess follow up, and evidence suggests that pain assessment alone does not improve
quality of care. Additionally, the current measure is only reported for SNPs; however, a wider
population of MA enrollees would benefit from a pain assessment and follow-up measure.
Therefore, NCQA is conceptualizing a new Chronic Pain Assessment and Follow-up measure
156
described below in the section on Potential New Measure Concepts and Methodological
Enhancements for Future Years. NCQA obtained feedback from their Committee for
Performance Measurement (CPM) in September 2022 and solicited public comment on the
proposed retirement of this measure as part of the HEDIS public comment period in February
2023. Pending results of public comment, NCQA would seek approval from the CPM in May
2023 for retirement of this measure in measurement year 2025. As a reminder, in the December
2022 proposed rule, CMS proposed adding a rule at §§ 422.164(e)(1)(iii) and 423.184(e)(1)(iii)
to allow removal of a Star Ratings measure, without separate rulemaking, when a measure
steward other than CMS retires a measure.
Most commenters opposed the retirement of the COA – Pain Assessment measure until a
replacement measure has been introduced and carefully evaluated given that pain is a frequent
symptom of illness and disease in the older beneficiaries. We have shared this feedback with
NCQA for their consideration.
COA – Functional Status Assessment and Medication Review (Part C). NCQA is also
exploring the development of new measures for Functional Status Assessment and Medication
Review that may eventually replace these indicators of the COA measure and be reported for a
wider population than only enrollees of SNPs. Any potential new measures are currently planned
for development for measurement year 2025 and beyond. If new measures are developed and
implemented, NCQA would propose retirement of the existing COA measures. If NCQA retires
the existing measures, CMS would consider replacing the retired measures in the Star Ratings
with the new ones consistent with the process specified in § 422.164(c).
We received mixed reaction to the development of new measures for a wider population than
only enrollees in SNPs. Some commenters did not want the current COA measures retired until
new measures are available. Other commenters wanted more information on the value of
broadening the population for these measures, as well as more information about the specifics of
these potential new measures. We have shared this feedback with NCQA for their consideration.
Diabetes Care – Eye Exam and Diabetes Care – Blood Sugar Controlled (Part C). NCQA is
reviewing these two measures for potential updates to the existing specifications and updates that
leverage standardized electronic clinical data. NCQA is re-evaluating the approach to identify
whether an enrollee has diabetes and would be included in the denominator to reflect the
evolution of claims data coding practices, pharmacy practices, and the use of electronic clinical
data. The current method identifies enrollees if they have at least two outpatient encounters with
a diagnosis of diabetes on different dates of service or at least one inpatient encounter with a
diagnosis of diabetes or a prescription for a diabetes medication. Potential updates include 1)
simplifying the current claims-based denominator approach to identify enrollees if they have at
least two encounters (in any setting except lab) on different dates of service with a diagnosis of
diabetes; and 2) revising the current pharmacy-based denominator approach to require a diabetes
diagnosis for those enrollees identified through a dispensed diabetes medication alone (this
157
would obviate the need for the existing exclusions of polycystic ovary syndrome, gestational
diabetes, or steroid-induced diabetes). These potential clarifications for measurement year 2024
would be non-substantive under § 422.164(d)(iv) by adding clarifications for the documentation
requirements to identify enrollees with diabetes. As such, if NCQA proceeds, CMS will apply
the update to the measures beginning with the 2024 measurement year (2026 Star Ratings).
These changes would also apply to the Kidney Health Evaluation for Patients with Diabetes (Part
C) measure currently on the display page and being proposed for the 2026 Star Ratings in the
Medicare Program; Contract Year 2024 Policy and Technical Changes to the Medicare
Advantage Program, Medicare Prescription Drug Benefit Program, Medicare Cost Plan Program,
Medicare Parts A, B, C, and D Overpayment Provisions of the Affordable Care Act (ACA) and
Programs of All-Inclusive Care for the Elderly; Health Information Technology Standards and
Implementation Specifications proposed rule which appeared in the Federal Register on
December 27, 2022 (87 FR 79452, 2024 Part C and D proposed rule).
In the Advance Notice, we stated that NCQA is also evaluating the potential removal of the
hybrid reporting method for the Diabetes Care - Eye Exam and Diabetes Care - Blood Sugar
Controlled measures for measurement year 2024 and beyond. The measures would then be
specified for the Administrative or ECDS reporting methods. Currently, NCQA is not
considering removal of the hybrid method for Diabetes Care - Blood Sugar Controlled. They are
continuing to consider for the Diabetes Care–Eye Exam measure to remove hybrid reporting and
transition to administrative-only reporting. The administrative reporting method utilizes claims
data and supplemental data. The hybrid reporting method utilizes claims data, supplemental data,
and sampling to include medical record review. The removal of hybrid reporting from the
Diabetes Care–Eye Exam measure will remove the sampling component and transition the
measure to administrative-only reporting in measurement year 2024. Removing hybrid reporting
will not change the data sources that health plans can use; the change is to the reporting method
only. Health plans will no longer be able to assess performance based on a sample of members
when the hybrid method is removed, but they can perform year-round chart review and have it
audited as non-standard supplemental data to report for the measure.
NCQA is also considering excluding enrollees with bilateral eye enucleation from the Diabetes
Care – Eye Exam measure starting with measurement year 2024. This change would be non-
substantive as described at § 422.164(d)(1)(i) since it narrows the population covered by the
measure. Another potential update that NCQA is considering is the incorporation of a Glucose
Management Indicator (GMI) as an additional method to assess numerator compliance in the
existing Diabetes Care – Blood Sugar Controlled measure for measurement year 2024 or beyond.
GMI is a calculation derived from continuous glucose monitoring devices that assesses average
blood sugar values and can provide information directly to patients and physicians at more
frequent intervals. Based on guidelines from the American Diabetes Association, GMI can serve

158
as an alternative method for HbA1c for use in clinical management.
49
NCQA is evaluating the
inclusion of GMI alongside HbA1c as two methods to assess the numerator. In cases where
enrollees have results available for both methods in the measurement year, the most recent result
should be used (regardless of whether it is a GMI or HbA1c result). In cases where enrollees
have results available for both methods on the same day, the HbA1c result should be used. If
NCQA decides to add additional tests that meet the numerator requirements, it would be a non-
substantive update as described at § 422.164(d)(1)(iv)(A). If this update is made, NCQA is
considering renaming the measure Glycemic Status Assessment for Patients With Diabetes.
Commenters generally supported revising the specifications for identifying enrollees with
diabetes. Most of the commenters were opposed to the removal of the hybrid reporting method
for the Diabetes Care – Eye Exam measure. Some commenters noted that GMI was problematic
as it is not as precise as HbA1c. Other commenters noted that GMI is self-administered and not
all patients can afford continuous glucose monitoring devices. GMI would be an alternative to
HbA1c so would not be required. We have shared this feedback with NCQA for their
consideration as they continue to explore updates to these measures.
Breast Cancer Screening (Part C). For measurement year 2024, NCQA is considering revising
the eligible population for this measure to be more inclusive of individuals who should be
screened for breast cancer. The revised eligible population would include members 52-74 years
of age who are recommended for routine breast cancer screening, including transgender and
gender-diverse members. For example, this would include transgender men with sex assigned at
birth as female, and transgender women with sex assigned at birth as male but who have
undergone estrogen hormone therapy. The intent of this change is to ensure that all members in
need of breast cancer screening are included in the eligible population, meaningfully improving
quality of care for a population that currently experiences disparities as it relates to preventive
screenings. However, given the relatively small size of the additional population to include
transgender and non-binary individuals, this change will not meaningfully impact either the
numerator or denominator of the measure. If NCQA decides to expand the population included
in the denominator, it would be a non-substantive update as described at § 422.164(d)(1)(ii)
given less than 0.3% of adults 50 years old and older identify as transgender or nonbinary.
50
Most commenters supported revising the eligible population for this measure. We have shared
the feedback received with NCQA as they continue to explore updates to this measure.
Statin Use in Persons with Diabetes (SUPD) (Part D). CMS will make the following non-
substantive updates to the SUPD measure beginning with the 2024 measurement year and 2026
Star Ratings: 1) to use continuous enrollment (CE) to fully align with the PQA specifications and
to no longer adjust for member-years (MYs), and 2) to align with the PQA age criteria
49
American Diabetes Association Professional Practice Committee. 6. Glycemic targets: Standards of Medical Care in
Diabetes—2022. Diabetes Care 2022; 45 (Suppl. 1); S83–S96.
50
https://www.pewresearch.org/fact-tank/2022/06/07/about-5-of-young-adults-in-the-u-s-say-their-gender-is-different-from-
their-sex-assigned-at-birth/.
159
specifications. CMS previously solicited feedback on using the CE specifications instead of MYs
in the 2023 Advance Notice. These two changes (using CE and eligibility for the SUPD measure
by the PQA’s age criteria at the start of the measurement year) are non-substantive updates under
§ 423.184(d)(1) because they are updates with no change to the intent of the measure or the
target population.
The SUPD measure analyzes the percent of Part D beneficiaries, ages 40 to 75 years, who were
dispensed at least two diabetes medication fills that received a statin medication fill during the
measurement period. As a reminder, a higher rate for the SUPD measure indicates better
performance. CMS adapted the SUPD measure from the PQA specifications, and CMS currently
adjusts Part D enrollment based on MYs to account for beneficiaries who are enrolled for only
part of the contract year. For example, if a beneficiary is enrolled for 6 out of 12 months of the
year, they will count as only 0.5 MYs in the rate calculation. However, the current PQA
specifications use CE instead of MYs. As stated in the 2022 PQA measure manual, the
beneficiary’s index prescription start date (IPSD) begins on the earliest date of service for a
diabetes medication during the measurement year. Beneficiaries are continuously enrolled during
the measurement year with one allowable gap in enrollment which may be up to 31 days during
the measurement year.
Beginning with measurement year 2024, CMS will use CE to fully align with the PQA
specifications and to no longer adjust for MYs; this update would be non-substantive. This
update is consistent with the update to use CE for the Part D medication adherence measures as
described immediately below. In applying CE, CMS will also align with the PQA age criteria
specifications for the SUPD measure; a beneficiary will be eligible for the measure based on
their age at the start of the measurement year regardless of whether the beneficiary ages in or out
during the measurement year. This will be a non-substantive change from CMS’ current
specifications with the MY adjustment in which a beneficiary is eligible for inclusion in the
SUPD measure from the month the beneficiary meets the minimum age restriction and ending
with the month before they exceed the maximum age restriction.
We analyzed year of service (YOS) 2021 data as of January 2022 limited to contracts with a
denominator greater than 30 members and compared rates using MYs and CE. We found that 88
percent of beneficiaries included in the measure using MYs were also in the denominator using
CE. Overall, the mean SUPD rates using CE were slightly higher than rates using MYs by
around 0.3 percentage points. For MA-PDs (non-MMPs), the mean rates increased from 85.08
percent to 85.51 percent with CE. About 45 percent of MA-PD contracts’ rates stayed relatively
the same, 43 percent increased, and 12 percent decreased. For PDPs, the mean rates increased
from 82.00 percent to 82.38 percent. We found 55 percent of PDP contracts’ rates stayed
relatively the same, 43 percent increased, and 2 percent decreased. Finally, we found that there
was a slight increase in SUPD rates across MA-PDs and PDPs for both female and male
beneficiaries, as well as individuals with LIS, dual eligibility, disability, and by race (Black,
Hispanic, American Indian/Alaska Native, and Multiracial).

160
Commenters in response to the CY 2024 Advance Notice were supportive of these non-
substantive measure updates to the SUPD measure, and we will apply starting with the 2024
measurement year for the 2026 Star Ratings.
Medication Adherence for Diabetes Medication/Medication Adherence for Hypertension
(RAS Antagonists)/Medication Adherence for Cholesterol (Statins) (Part D). In the 2023
Rate Announcement, CMS solicited initial feedback on implementing risk adjustment of the
medication adherence measures based on sociodemographic (SDS) characteristics (age, gender,
dual eligibility/ LIS status, and disability status) according to the PQA specifications and
endorsed by the National Quality Forum (NQF).
Implementing SDS risk adjustment is a substantive change according to § 423.184(d)(2). CMS
proposed this change for the 2026 measurement year and 2028 Star Ratings in the 2024 Part C
and D proposed rule published on December 27, 2022 (87 FR 79616-79617). CMS also included
data analysis and additional information in the 2024 Part C and D proposed rule (87 FR 79617-
79618) to provide a more complete picture of the potential updates to the measures. The
proposed substantive change will be addressed through the rulemaking process.
We signaled that there may be a few non-substantive changes made to the adherence measures in
the Announcement of Calendar Year (CY) 2023 Medicare Advantage (MA) Capitation Rates and
Part C and Part D Payment Policies.
51
In addition, CMS will make the following non-substantive
changes to the three adherence measures to fully align with the current PQA measure
specifications which are endorsed by the NQF: 1) no longer adjust for MYs; instead apply the
PQA’s measure specifications to use CE as defined by the treatment period and exclude
beneficiaries with more than 1-day gap in enrollment during the treatment period and 2) no
longer adjust for inpatient (IP) or SNF stays as the PQA specifications do not include these
adjustments. As a reminder, in accordance with § 423.184(d)(1), non-substantive changes may
be adopted during or in advance of the measurement period through the Advance Notice/Rate
Announcement process. We plan to implement CE starting with the 2024 measurement year for
the 2026 Star Ratings. We plan to remove the IP/SNF stay adjustment from the adherence
measures starting with the 2026 measurement year for the 2028 Star Ratings, which is the same
time we proposed to implement the SDS risk adjustment change, but is not dependent on
finalizing the SDS risk adjustment proposal.
Commenters were supportive of the non-substantive update to the medication adherence
measures to apply CE instead of MYs to align with the PQA. CMS will implement the CE to the
medication adherence measures starting with the 2024 measurement year (2026 Star Ratings).
We received a comment requesting clarification on whether a beneficiary who has a gap in
enrollment would be excluded from the entire measurement period when applying CE. CMS will
no longer account for beneficiaries who are enrolled for only part of the measurement year in the
51
Please refer to the Announcement of Calendar Year (CY) 2023 Medicare Advantage (MA) Capitation Rates and Part C and
Part D Payment Policies at the following website: https://www.cms.gov/files/document/2023-announcement.pdf.
161
contract. Based on the PQA measure specifications, the treatment period for the adherence
measures begins on the index prescription start date (IPSD) and extends through whichever
comes first: the last of day of enrollment during the measurement year, death, or the end of the
measurement year. For example, a beneficiary who is CE in one contract for 6 months and then
disenrolls from that contract in July of the same measurement year would be included in the
measure calculation for that contract if they meet all of the other measure criteria, even though
the beneficiary was CE for only 6 months of the measurement year. Beneficiaries are CE during
the measurement year with an allowable one 1-day gap in enrollment during the treatment
period.
Several commenters were not supportive of the removal of the IP/SNF stay adjustment from the
medication adherence measures. Some commenters expressed concern that removal of the
IP/SNF stay adjustment would disproportionately impact plans with a higher proportion of
beneficiary stays or institutional special needs plans (I-SNPs). As a reminder, the IP/SNF stay
adjustment is not included in the PQA measure specifications. We performed contract-level
analysis of the SDS risk adjustment with and without IP/SNF stay adjustment as discussed in the
2024 Part C and D proposed rule. The majority of contracts did not have a change in their
medication adherence rates. These findings were also consistent for contracts with SNPs. We
found that more contracts with SNPs (including I-SNPs) increased in their rates or stayed the
same than decreased. CMS will move forward with this measure specification update in order to
align with the measure steward, and remove the IP/SNF stay adjustment starting with the 2026
measurement year (2028 Star Ratings).
A few commenters suggested additional medication adherence measure specification changes,
such as excluding beneficiaries in I-SNPs or residing in long-term care (LTC) facilities who are
receiving palliative care or excluding certain GLP-1 agonists which may be used for weight loss.
As a reminder, Part D does not cover medications for weight loss based on section 1927(d)(2) of
the Social Security Act. PQA is the measure steward for the adherence measures, and CMS has
shared specification comments received with the PQA.
MTM Program Completion Rate MTM Program Completion Rate for Comprehensive
Medication Review (CMR) (Part D). The data for this measure are reported by contracts to
CMS in the Health Plan Management System (HPMS) per the Part D Reporting Requirements
(OMB control number 0938-0992). Independent validation of these data is performed in
accordance with § 423.514(j) (OMB control number 0938-1115), and the results are due in
HPMS by June 30 of the year following the reporting period. Beneficiaries who are in hospice at
any point during the reporting period are excluded from this measure. The Medicare Enrollment
Database (EDB) is used to exclude beneficiaries in hospice. Starting with the 2023 reporting
period for the 2025 Star Ratings, CMS will use the EDB data to identify beneficiaries in hospice
in June after the reporting period, which aligns with when the Part D Reporting Requirements
data are pulled from HPMS. The data validation results are pulled in July of the year following
the reporting period. Commenters supported this change. This is a non-substantive change as

162
described at § 423.184(d)(1) since this change does not meaningfully impact the numerator or
denominator of the measure. In addition, the prevalence of beneficiaries in hospice is low (less
than 4% of MTM program enrollees).
Display Measures
Display measures on CMS.gov are published separately from the Star Ratings and include
measures that are transitioned from inclusion in the Star Ratings, new or updated measures
before inclusion into the Star Ratings, and informational-only measures. Organizations and
sponsors have the opportunity to preview the data for their display measures prior to release on
CMS.gov. We anticipate all 2023 display measures will continue to be shown on CMS.gov in
2024 unless noted below.
Depression Screening and Follow-Up (Part C). We solicited feedback regarding whether to
add the HEDIS Depression Screening and Follow-up for Adolescents and Adults measure to the
2026 Star Ratings display page (using data from the 2024 measurement year). As CMS’
Behavioral Health Strategy includes using quality measures to “drive health systems, providers,
practices and clinicians, and community-based providers toward delivery of high value care”
(CMS Behavioral Health Strategy | CMS), we are considering behavioral health measures that
could potentially be added to the Star Ratings program in the future through rulemaking. The
HEDIS measure, “Depression Screening and Follow-up,” measures the percentage of members
who were screened for clinical depression using a standardized instrument and, if screened
positive, received follow-up care. This aligns with the U.S. Preventive Services Task Force
recommendations regarding screening and follow-up for depression (Depression in Adults:
Screening - Healthy People 2030 | health.gov) and supports CMS’ efforts to implement the
Universal Foundation set of measures across quality programs.
Most commenters supported adding the Depression Screening and Follow-up measure to the
display page and eventually the Star Ratings. However, some commenters raised concerns about
the availability of data needed for this measure and recommended allowing time for clinical data
systems to capture this type of information. A few commenters also raised concerns about the
impact of state laws and regulations on the ability to share mental health information with
primary care providers without patient consent and the impact this may have on providing
follow-up care. CMS will take this feedback into consideration and we have also shared this
feedback with NCQA for their consideration. We plan to add this measure to the 2026 Star
Ratings display page (using data from the 2024 measurement year). For this measure to be added
to the Star Ratings, it would need to be adopted through rulemaking.
Initiation and Engagement of Substance Use Disorder (SUD) Treatment (Part C). Prior to
measurement year 2022, this measure was called Initiation and Engagement for Alcohol and
Other Drug Abuse or Dependence Treatment. This HEDIS measure is currently on our display
page. For measurement year 2022, NCQA updated the measure to change it from “member-
163
based” to “episode-based”; lengthened the negative substance use disorder (SUD) history period
from 60 days to 194 days to limit the number of members receiving ongoing treatment who
inadvertently fall into the denominator; removed emergency department visits and medically
managed withdrawal services from the negative SUD history period; removed the requirement
that a psychosocial treatment encounter accompany pharmacotherapy; and split the adult age
stratification between 18-64 years and 65+ years to better highlight any gaps in care between
different age groups. Since many individuals with SUD attempt treatment multiple times before
they are able to successfully engage, the revision of the measure to an “episode-based”
framework allows for each recovery attempt to count independently, which should result in a
more valid representation of engagement with SUD treatment for health plan populations.
Additionally, emergency department visits and withdrawal services alone are not suggestive of
ongoing or planned treatment for individuals with SUD and thus do not signal that a member is
already engaged in comprehensive care so these were removed from the measure’s negative
SUD history period. The requirement that psychosocial treatment accompany pharmacotherapy
was also removed to align with the most current clinical practice guidelines (e.g., allowing for
patients who may not accept concomitant psychosocial treatment).
We are considering potentially adding this measure to the Star Ratings in the future pending
rulemaking. This would support CMS’ efforts to implement the Universal Foundation set of
measures across quality programs. Commenters did not support adding this measure to the Star
Ratings and raised concerns about confidentiality, state and federal regulations regarding
disclosure of alcohol and SUD information without written authorization, and individuals
refusing to admit an SUD problem. We have shared this feedback with NCQA for their
consideration. We will take the comments into consideration as we consider adding this measure
to the Star Ratings. For this measure to be added to the Star Ratings, it would need to be adopted
through rulemaking.
Timely Follow-up After Acute Exacerbations of Chronic Conditions (Part C). This clinical
quality measure assesses the percentage of acute events requiring an emergency department visit
or hospitalization for one of six chronic conditions, where outpatient, non-emergent follow-up is
received within a guideline-recommended timeframe after discharge to the community for each
chronic condition:
1. Hypertension: Within 7 days
2. Asthma: Within 14 days
3. Congestive Heart Failure (CHF): Within 14 days
4. Coronary Artery Disease (CAD): Within 14 days
5. Chronic Obstructive Pulmonary Disease (COPD): Within 30 days
6. Diabetes: Within 30 days.
Follow-up care is a critical aspect of care coordination, ensuring patients understand and are
adhering to their medication regimen, providers are monitoring patients for adverse events, and

164
providers are educating patients to recognize warning signs. This measure was originally
developed using MA encounter data submitted by MA contracts reflecting care received 2014-
2016. The measure is constructed at the contract level. Details regarding measure specifications
and validation are available from NQF (NQF 34455) and the measure steward, IMPAQ
International.
52
The measure calculation was subsequently replicated using encounter data from 2016 to 2020.
Contract-level measure performance rates were found to be roughly stable over time with mean
and median performance rates varying from 69-70% and 71-73%, respectively, between 2016
and 2019, before declining in 2020.
CMS solicited comments on adding this measure to the display page starting with the 2024 Star
Ratings and potential future inclusion of this measure in the Part C Star Ratings pending
rulemaking. We received mixed support for this measure. While a few supported the measure
due to the importance of follow-up care, others suggested the measure is duplicative of existing
Star Ratings measures. We appreciate all comments received and will not proceed with adding
the measure to the display page at this time.
Adult Immunization Status (Part C and D). We appreciate the feedback we received from last
year’s Advance Notice on replacing the current CAHPS influenza vaccination measure with the
HEDIS influenza indicator from the Adult Immunization Status measure. Some commenters
suggested that it would be more reliable than self-reported CAHPS data, while other commenters
noted that the electronic data sources would have incomplete vaccination status data since
patients can receive vaccines in community settings with or without an insurance claim. Many
commenters cited discrepancies between HEDIS immunization data with self-reported CAHPS
data. Some commenters suggested supplementing electronic data sources with other data sources
to have more complete information. CMS will continue to take this feedback into consideration.
Any changes to the current influenza measure in Star Ratings would need to be proposed through
rulemaking.
CMS plans to add NCQA’s Adult Immunization Status measure to the 2026 display page starting
with data from the 2024 measurement year. This measure assesses the receipt of influenza,
Td/Tdap, zoster, and pneumococcal vaccines. This measure is specified for the HEDIS ECDS
Reporting Standard and captures receipt of vaccinations using data from a variety of electronic
sources such as administrative claims, immunization registries, and EHRs, among others. For
HEDIS measurement year 2023, NCQA has made a series of updates to the measure, including
updating the pneumococcal indicator to assess adults 66 and older who received any of the
following vaccines between age 19 and the end of the measurement period: pneumococcal
conjugate vaccine (PCV) 20, PCV15, PCV13, or pneumococcal polysaccharide vaccine (PPSV)
23; removing the exclusions for chemotherapy, bone marrow transplant, and
52
See https://www.qualityforum.org/QPS/3455.
165
immunocompromising conditions; and expanding the age range for influenza and Td/Tdap
vaccination status to Medicare enrollees age 19 and older and zoster for age 50 and older. We
also continue to consider this measure as a potential future Star Ratings measure pending
rulemaking. This measure is also part of the Universal Foundation set of measures that CMS is
considering proposing across quality programs. Commenters expressed mixed support for this
measure. Some commenters supported it and highlighted the benefits of it being a comprehensive
measure of vaccinations. Other commenters were opposed to it, expressing concerns about
obtaining complete vaccination data, inaccurate or incomplete information in immunization
registries, and enrollee resistance to vaccines given the increasingly politicized nature of
vaccinations. We have shared this feedback with NCQA. We will take these comments into
consideration as we consider adding this measure to the Star Ratings in the future through
rulemaking.
Concurrent Use of Opioids and Benzodiazepines (COB), Polypharmacy Use of Multiple
Anticholinergic Medications in Older Adults (Poly-ACH), and Polypharmacy Use of
Multiple Central Nervous System Active Medications in Older Adults (Poly-CNS) (Part D).
We announced in the 2020 Rate Announcement that these measures would be on the display
page for 2021 and 2022, and that CMS would consider adding them to the Star Ratings in the
future. In the 2024 Part C and D proposed rule (87 FR 79619-79620), CMS proposed to move
the COB, Poly-ACH, and Poly-CNS measures from the display page to the 2026 Star Ratings
(2024 measurement year). See the proposed rule for further information, and these proposals will
be addressed through the rulemaking process.
Additionally, CMS will make a non-substantive update for the 2024 measurement year to align
with the PQA measure specifications to use CE and no longer adjust for MYs. We did not
receive much feedback regarding the non-substantive update to use CE instead of MYs. One
commenter requested clarification on whether a member who has a gap in enrollment would be
excluded from the entire measurement period when applying CE. According to the PQA measure
specifications for CE for the COB and the two Polypharmacy measures, there is one allowable
gap in enrollment of up to 31 days during the measurement year. Therefore, when the enrollment
is verified monthly, the beneficiary may not have more than a one-month gap in coverage for
CE. We will implement this non-substantive update to align with the PQA measure
specifications for the 2024 measurement year.
We received measure specification comments to exclude LTC residents and add risk adjustment
to these measures. We have shared these specification-related comments with the measure
steward, PQA.
Antipsychotic Use in Persons with Dementia, Overall (APD)/Antipsychotic Use in Persons
with Dementia, in Long-Term Nursing Home Residents (APD-LTNH) (Part D). These
measures currently reported on the display page are adapted from the APD measure developed
by the PQA. The PQA recently made the following measure specification updates in their 2023
166
measure manual to the APD measure: 1) slight modification in the APD measure description; 2)
updated definition to reflect appropriate indication for antipsychotic use; 3) added major
depression diagnosis as an exclusion to the numerator; and 4) removed the “>60 cumulative days
supply” language from the denominator. In the 2023 measure manual, PQA slightly modified the
APD description from “the percentage of individuals at least 65 years of age with dementia who
received an antipsychotic medication without evidence of a psychotic disorder” to “the
percentage of individuals at least 65 years of age with dementia who received an antipsychotic
medication without evidence of an appropriate indication for an antipsychotic use.” Additionally,
the PQA updated the definition to reflect appropriate indication for antipsychotic use to align
with FDA approved uses as individuals having one or more claims with schizophrenia, bipolar
disorder, Huntington’s disease, or Tourette’s syndrome in the primary diagnosis or any other
diagnosis fields during the measurement year. Furthermore, beneficiaries taking an antipsychotic
with an FDA approved indication for treatment of major depression diagnosis (i.e., depression
resistant to treatment) is a new exclusion added to the numerator. However, the PQA developed
the following process to exclude beneficiaries with major depression diagnosis. The update to
remove beneficiaries with major depression diagnosis was approved by the PQA’s Quality
Measure Expert Panel:
1) one or more prescription claim for an antipsychotic indicated for major depression
during the measurement year. The antipsychotic medications would be based on the
PQA’s NDC lists; and
2) one or more prescription claim for an antidepressant during the measurement year. The
antidepressant medications would be based on the PQA’s NDC lists; and
3) major depression at any time during the measurement year based on the diagnosis
codes provided by the PQA.
Currently, we identify beneficiaries for the denominator who have either a dementia diagnosis
and/or two or more prescription claims with unique dates of service (DOS) and a total days’
supply greater than 60 cumulative days for a cholinesterase inhibitor or N-methyl-D-aspartate
(NMDA) receptor antagonist during the measurement year. However, in PQA’s 2023 measure
manual, PQA updates the APD measure specifications by removing the requirement for “greater
than 60 cumulative days’ supply” in the denominator since there is no known rationale for
including this requirement in addition to the 2 or more prescription claims on different dates of
service since beneficiaries can be eligible for the denominator with either prescription claims or
diagnosis. Furthermore, the removal of > 60 days’ cumulative supply would more accurately
align the APD measure with the other PQA measures.
We tested the updated PQA measure specifications for both APD measures using 2021 PDE data
with contracts with greater than 30 member-years. A total of 809 Part D contracts were included
in the APD measure analysis and 418 Part D contracts for the APD-LTNH measure. With the

167
added major depression exclusion, the numerator decreased for both APD measures. We found
that 6.0% of beneficiaries in the APD denominator population were diagnosed with major
depression and 10.1% of beneficiaries from the APD-LTNH denominator. For the APD measure,
the mean rate for all contracts improved from 8.57% to 7.10% with the updated measure
specifications. Similarly, for the APD-LTNH measure, the mean rate overall improved from
7.99% to 5.96%. As a reminder, a lower rate indicates better performance for both APD
measures. The tables below provide more information on the change in rates after applying the
updated specifications.
Table VI-5. APD Rate Distribution for Contracts with > 30 Denominator Member-Years
Contract
Type
Percentile Distributions
Number of
contracts
Mean Min p25 p50 p75 p90 Max
YOS 2021
PDE with
Current
Measure
Specifications
All
Contracts
809
8.57%
0.00%
6.09%
7.85%
10.09%
13.05%
30.75%
MAPDs
749
8.52%
0.00%
5.93%
7.67%
10.10%
13.62%
30.75%
MAPDs
(non-
MMP)
711
8.62%
0.00%
5.97%
7.72%
10.22%
13.76%
30.75%
PDPs
60
9.19%
5.24%
8.46%
9.04%
9.93%
11.53%
12.44%
YOS 2021
PDE with
Updated
Measure
Specifications
All
Contracts
809
7.10%
0.00%
4.75%
6.22%
8.13%
11.66%
34.06%
MAPDs
749
7.08%
0.00%
4.62%
6.05%
8.13%
11.95%
34.06%
MAPDs
(non-
MMP)
711
7.15%
0.00%
4.64%
6.12%
8.17%
12.00%
34.06%
PDPs
60
7.32%
2.33%
6.48%
7.30%
8.11%
9.15%
10.06%

168
Table VI-6: APD-LTNH Rate Distribution for Contracts with >30 Denominator Member-
Years
Contract
Type
Percentile Distributions
Number of
contracts
Mean Min p25 p50 p75 p90 Max
YOS 2021
PDE with
Current
Measure
Specifications
All
Contracts
418
7.99%
0.00%
4.95%
7.50%
10.37%
13.49%
20.67%
MAPDs
373
7.92%
0.00%
4.69%
7.41%
10.37%
13.49%
20.67%
MAPDs
(non-
MMP)
338
8.27%
0.00%
5.18%
7.87%
10.67%
14.15%
20.67%
PDPs
45
8.57%
2.93%
6.66%
7.58%
9.70%
13.05%
17.51%
YOS 2021
PDE with
Updated
Measure
Specifications
All
Contracts
418
5.96%
0.00%
3.67%
5.44%
7.81%
10.46%
27.18%
MAPDs
373
5.86%
0.00%
3.54%
5.30%
7.71%
10.27%
27.18%
MAPDs
(non-
MMP)
338
6.09%
0.00%
3.74%
5.53%
7.95%
10.88%
27.18%
PDPs
45
6.77%
3.03%
5.05%
5.99%
8.78%
10.65%
11.79%
Based on the results of the analysis, CMS plans to implement the updated measure specifications
on the display page for the 2023 measurement year.
One commenter requested that APD and APD-LTNH measures consider permitting the use of
low-dose, short-term use of antipsychotics in certain situations. Another commenter was
concerned with the impact and appropriateness of the APD and APD-LTNH measures in
medically complex individuals with dementia. We have shared these comments with the PQA.
The majority of commenters were supportive of the measure specification updates to the APD
and APD-LTNH measures to align with the PQA. We will implement the measure specification
updates to the APD and APD-LTNH measures for the 2023 measurement year.
Initial Opioid Prescribing - Long Duration (IOP-LD) (Part D). We began reporting the IOP-
LD measure in the 2023 display page (2021 measurement year). Currently, beneficiaries enrolled
in hospice, with a cancer diagnosis, with a sickle cell disease diagnosis, or receiving palliative
care during the measurement year or the 90 days prior to the measurement period are excluded
from the measure. However, CMS will align with current PQA measure specifications, and
therefore, these beneficiaries will be excluded from the measure during the measurement year or
90 days prior to the index prescription start date (IPSD), the earliest date of service for an opioid
medication during the measurement year. CMS plans to update the IOP-LD measure on the
display page for the 2023 measurement year.

169
The majority of commenters supported this measure specification update to the IOP-LD
measure. CMS will continue to exclude beneficiaries with an exclusion diagnosis during the
measurement year. However, with this measure specification update beginning in the 2023
measurement year, only beneficiaries with an exclusion diagnosis 90 days prior to the IPSD will
be excluded rather than excluding all beneficiaries who have an exclusion diagnosis 90 days
prior to the measurement year.
We also received one measure specification comment to exclude LTC residents from the IOP-
LD measure. We have shared this specification-related feedback with the PQA.
Medication Adherence for HIV/AIDs (Antiretrovirals) (ADH-ARV)/Antipsychotic Use in
Persons with Dementia, Overall (APD)/Antipsychotic Use in Persons with Dementia, in
Long-Term Nursing Home Residents (APD-LTNH)/Use of Opioids at High Dosage in
Persons without Cancer (OHD)/Use of Opioids from Multiple Providers in Persons without
Cancer (OMP)/Initial Opioid Prescribing -Long Duration (IOP-LD) (Part D). Similar to the
other Part D Patient Safety measures discussed above, CMS will align with the PQA measure
specifications to use CE and no longer adjust for MYs. Currently, we do not have an exact
timeline to update these display page and Patient Safety measures, but we will announce it in
advance to sponsors.
Commenters were supportive of this specification change to align with the PQA by updating the
measures from MYs to CE. We will provide more information when the timeline for these
measure changes is finalized.
Potential New Measure Concepts and Methodological Enhancements for Future Years
Health Equity (Part C and D). CMS continues to consider additional ways to advance health
equity in the Part C and D programs. CMS released confidential stratified reports to Part C and D
sponsors in HPMS in Spring 2022 to help contracts identify disparities in care by LIS/DE and
disability status for most Part C and D Star Ratings measures. Commenters were supportive of
providing confidential stratified reports to Part C and D sponsors and a few recommended
releasing the stratified reports publicly. CMS will consider releasing the stratified reports
publicly in the future. A variety of stratified reports are currently available through the CMS
Office of Minority Health website at https://www.cms.gov/about-cms/agency-
information/omh/research-and-data/stratified-reporting.
Chronic Pain Assessment and Follow-up (Part C). NCQA is exploring a new measure for
measurement year 2025 that would assess chronic pain and follow-up in Medicare enrollees age
65 and older. They are currently proposing two indicators for this measure. The first indicator
would assess if enrollees with chronic pain received a multidimensional pain assessment, and the
second indicator would assess if some type of follow-up was received among enrollees who
tested positive for pain on the multidimensional assessment. Most commenters supported this
170
measure concept but some requested more information about measure specifications. We shared
feedback received with NCQA for their consideration as they continue to develop this measure.
Cross-Cutting: Sexual Orientation and Gender Identity for HEDIS Measures (Part C).
NCQA is evaluating approaches to update applicable HEDIS measure specifications where
eligible populations are currently defined with gendered language to ensure inclusive and
gender-affirming approaches aligned with measure intent. Any potential changes to HEDIS
measures, such as Breast Cancer Screening, would be considered for measurement year 2024 or
beyond. These potential updates for measurement year 2024 or beyond would be non-substantive
under § 422.164(d)(1)(ii) because the changes are not expected to meaningfully impact the
numerator or denominator of the affected measures. Most commenters supported these updates
although some requested a longer timeframe before implementation. We shared feedback
received with NCQA.
Cross-Cutting: Identifying Chronic Conditions in HEDIS Measures (Part C). NCQA is
reevaluating how to identify those with chronic conditions (e.g., diabetes, bipolar disorder,
advanced illness) with the goal of updating the claims-based approach that is currently used
across HEDIS measures to identify conditions by incorporating clinical data. The potential
revised claims method would identify members with a condition if they have at least two
encounters with the diagnosis (in any setting except lab) on different dates of service. This would
be in place of the current method which has unneeded complexity by looking for at least two
visits (e.g., outpatient, observation, telephone, emergency department, non-acute inpatient
encounters) on different dates of service or at least one inpatient encounter or discharge with a
diagnosis. These potential updates would simplify the way conditions are identified and would
impact the following Star Ratings and display measures: Diabetes Care – Eye Exam, Diabetes
Care - Blood Sugar Controlled, Follow-up After Emergency Department Visit for Patients with
Multiple Chronic Conditions, and Kidney Health Evaluation for Patients with Diabetes. Potential
updates would also apply to how advanced illness diagnoses are identified as part of the cross-
cutting advanced illness and frailty exclusion. This exclusion is implemented in the following
Star Ratings measures: Breast Cancer Screening, Colorectal Cancer Screening, Controlling High
Blood Pressure, Diabetes Care - Eye Exam, Diabetes Care – Blood Sugar Controlled, Kidney
Health Evaluation for Patients with Diabetes, Osteoporosis Management in Women Who Had a
Fracture, Statin Therapy for Patients With Cardiovascular Disease. These potential updates for
measurement year 2024 would be non-substantive under § 422.164(d)(1)(iv) by adding
clarifications for the documentation requirements to identify enrollees with chronic conditions.
Most commenters supported these updates. We shared feedback received with NCQA for their
consideration as they make measure updates.
Blood Pressure Control Measures (Part C). NCQA is exploring the development of new blood
pressure control measures that utilize the capabilities of digital quality measures and leverage
standardized electronic clinical data. The current Controlling Blood Pressure measure included in
Part C Star Ratings assesses the percentage of members 18-85 years of age with hypertension
171
whose blood pressure was adequately controlled (<140/90 mmHg). The numerator currently
assesses if control was reached by using only the most recent blood pressure reading available.
NCQA is planning to test a new approach which takes an average of blood pressure readings
over time and will also explore alternative evidence-based blood pressure control thresholds
(<130/80 mmHg). Their testing efforts will also inform the development of an accompanying
HEDIS blood pressure control measure for patients with diabetes. The new measures are being
explored for measurement year 2025 and beyond, and if implemented, would eventually replace
the current HEDIS measures related to blood pressure. If new measures are introduced, NCQA
would propose retirement of the existing blood pressure measures.
Most commenters supported NCQA’s work to develop a new blood pressure control measure.
Some commenters requested additional clarification about the number of readings that would be
counted in the measure, whether blood pressure outliers would be removed, whether blood
pressure readings from remote patient monitoring would be included in the average, and whether
patients with only one screening in a year would be excluded from the measure. Other
commenters raised questions about alternative blood pressure thresholds under consideration.
We have shared this feedback with NCQA for their consideration as they continue to explore the
development of a new blood pressure control measure.
Kidney Health (Part C). NCQA is exploring potential measure concepts for kidney health
management related to person-centered outcomes, shared decision making, and preparedness for
kidney failure for the future. Commenters expressed strong support for these measure concepts.
We have shared this feedback with NCQA for their consideration as they continue to explore
measures related to kidney health management.
Social Connection Screening and Intervention (Part C). NCQA is continuing to work on
developing a potential new measure that assesses the percentage of members age 65 and older
who were screened using pre-specified instruments at least once during the measurement period
for social isolation, loneliness, or inadequate social support and received a corresponding
intervention if they screened positive. NCQA has begun measure development work in this area
focused on members 65 and older, because much of the evidence for screening and interventions
is focused on this age group; however, NCQA plans to explore including those under 65 in the
future. The proposed measure will have two indicators, one for social connection screening and
one for social connection intervention. This measure would be reported using electronic clinical
data, including data from electronic health records, registries, case management systems, and
administrative claims. NCQA is considering stratifying the potential measure by age (65-74, 75-
84, and 85+) and race/ethnicity. Most commenters supported these updates although some
wanted clarification about the measure and possible interventions as well as more time to
implement any changes. We have shared feedback received with NCQA.
Broadening the Mental Health Conditions Assessed by Health Outcomes Survey (HOS)
(Part C). CMS continues to explore ways to enhance the HOS to provide MA contracts with

172
useful and actionable feedback about their enrollee populations. For example, we are exploring
whether to broaden the mental health items in the survey to ensure we have the data to assess
whether enrollees with social risk factors such as low-income status are experiencing more issues
with poor mental health. This effort supports CMS’ focus on health equity.
The existing HOS mental health measures focus broadly on emotional problems with an
emphasis on depression. While depression is a significant health problem in the Medicare
population that has been linked to poor health outcomes, many older adults live with mental
health conditions beyond depression. For example, 1.2% to 15% of community samples of
persons over 60 years of age show anxiety symptoms.
53
We are exploring ways to measure a
broader array of mental health conditions and provide more actionable feedback and data to
health plans for quality improvement. The 2-item measure of Generalized Anxiety Disorder
(GAD-2) is used clinically as a way to screen anxiety disorders generally and Generalized
Anxiety Disorder more specifically.
54
In combination with the Patient Health Questionnaire-2
(PHQ-2) that is currently on the HOS and is used as a screening tool for depression, the
combined questions (GAD-2 and PHQ-2) make up the PHQ-4, which functions well as a general
mental health screening tool. Adding the GAD-2, therefore, could widen the scope of
measurement of HOS to anxiety disorders and enhance the survey’s ability to screen for mental
health needs.
CMS received mixed feedback about broadening the mental health conditions assessed by HOS.
Although over half of commenters were generally supportive, some commenters made a variety
of different suggestions such as rewording the GAD-2, considering whether there are similar
questions on the HOS, and evaluating whether the HOS is the best vehicle to assess anxiety
disorders. The remaining commenters did not support adding the GAD-2 measure to HOS, citing
reasons such as low prevalence of anxiety in older adults, limitations of HOS such as small
sample sizes, and issues with patient-reported outcome measures.
We will take this feedback into consideration as we continue to explore enhancements to HOS.
There is growing concern that anxiety disorders, similar to depression, are underrecognized and
undertreated in older adults.
55
Recent data from the Medicare Current Beneficiary Survey
(MCBS) and other sources suggest that the prevalence of anxiety disorders and depression
spiked during the COVID-19 pandemic. For example, one analysis of MCBS data found 24% of
adults ages 65 and older with Medicare reported anxiety or depression in August 2020, a rate that
is substantially higher than the 11% of older adults with Medicare who reported depression or
53
Bryant, C., Jackson, H., & Ames, D. (2008). The prevalence of anxiety in older adults: methodological issues and a review of
the literature. Journal of Affective Disorders, 109(3): 233-250.
54
Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Monahan, P.O.; Löwe B. (2007). Anxiety disorders in primary care: prevalence,
impairment, comorbidity, and detection. Ann Intern Med, 146:317-325.
55
Seniors With Anxiety Frequently Don’t Get Help. Here’s Why. | Kaiser Health News (khn.org).

173
anxiety in 2018.
56
Rates are even higher among younger beneficiaries. An analysis of United
States Census Bureau COVID-19 Household Pulse Survey data collected between April 23, 2020
and March 1, 2021 found 43% of Medicare beneficiaries with disabilities (i.e., under age 65) had
symptoms of generalized anxiety disorder and 37% had symptoms of major depressive
disorder.
57
Given the impact of anxiety disorders on health, we will continue to consider how
best to measure.
Measuring Access to Mental Health Care on HOS (Part C). Since 2006, the HOS has used
seven items from the Veterans RAND 12-Item Health Survey (VR-12) to calculate mental health
summary scores. In addition, one HOS question from the VR-12 assesses change in emotional
health compared with one year ago but is not used in the calculation of the summary scores. Two
additional mental health items measure mild, moderate, or severe depression. One item assesses
memory problems.
These mental health-related questions do not address access to care, but access to mental health
care could be useful to measure for quality improvement. There are existing surveys that include
questions to assess need for and access to mental health services.
58, 59
These questions include
whether an appointment was made (or attempted) during the last 6 or 12 months, how difficult it
was to make appointments, whether psychiatric medications were prescribed or other treatment
conducted as soon as needed, or whether there were challenges in filling psychiatric
prescriptions. These types of measures could help plans assess variation in access to mental
health care.
Commenters expressed support for measuring mental health care access. However, most
commenters suggested that HOS may not be the right vehicle for this type of measure. They
believe HOS is already too long, that it has declining response rates and small sample sizes, and
that plans cannot act on the findings or track outcomes. A couple of commenters questioned
whether a self-reported measure is appropriate for tracking access to mental health care. CMS
will take this feedback into consideration as we continue to explore how best to capture
challenges Medicare beneficiaries face in accessing mental health care.
Addressing Unmet Health-Related Social Needs on HOS (Part C). In the 2023 Advance
Notice and Rate Announcement we described a new HEDIS measure focused on screening and
referral to services for social needs that NCQA refers to as the Social Need Screening and
56
Koma, W; True, S.; Biniek, J.F.; Cubanski, J.; Orgera, K.; Garfield, R. One in four older adults report anxiety or depression
amid the COVID-19 Pandemic. KFF, 2020, Oct 9. Accessed March 9, 2023: https://www.kff.org/medicare/issue-brief/one-in-
four-older-adults-report-anxiety-or-depression-amid-the-covid-19-pandemic/
57
Friedman C. (2022). The mental health of Medicare beneficiaries with disabilities during the COVID-19 pandemic. Rehabil
Psychol, 67(1):20-27.
58
Agency for Healthcare Research and Quality (AHRQ). (2021, May). Supplemental items for CAHPS Clinician & Group Adult
Survey 3.0/3.1: Access to Mental Health Services. https://www.ahrq.gov/cahps/surveys-guidance/item-sets/cg/suppl-
mentalhealth-cg30-adult.html.
59
Kyanko KA, Curry LA, Keene DE, et al. Does primary care fill the gap in access to specialty mental health care? A mixed
methods study. J Gen Intern Med. 2022:1-7.
174
Intervention (SNS-E) measure. This measure focuses on whether members were screened at least
once during the measurement year. Commenters to the Advance Notice generally supported its
use, but some requested CMS eventually go beyond this measure to include not just screening
and referrals but also access to appropriate services.
CMS is working on developing an additional measure that would complement the SNS-E
measure as we expand our work related to health equity. This new measure would be a survey-
based assessment of enrollee health-related social needs, specifically housing instability, food
insecurity, and transportation availability. Each question set would begin with an initial
screening item. The subsequent items would assess whether the respondent has received
assistance and whether a need currently exists. While the SNS-E measure aims to capture
screening and assessment by the plan and its providers, we are considering potential HOS
questions that would focus on enrollees’ perceptions of unmet needs and of the plans’ assessment
and intervention. The HOS questions would also provide additional information about ongoing
unmet needs even if the plan intervened. The HOS measure will provide important patient-
reported data that will complement the HEDIS SNS-E measure. Unlike the SNS-E, the HOS
measure will ask respondents whether they received assistance from their plan or provider and
whether they are currently struggling with unmet needs.
While most commenters see the value of addressing unmet health-related social needs and its
role in health equity, CMS received mixed feedback about adding questions regarding screening
and assistance with unmet social needs to HOS. Although more than half of commenters
supported adding related questions to HOS, other commenters raised the following concerns:
plans and providers do not have full control over which services are sought and provided;
geographic differences in the availability of community resources and interventions; adding
these items to HOS could duplicate the data from NCQA’s Social Need Screening and
Intervention (SNS-E) measure; and HOS may not be the appropriate vehicle for collecting this
information. CMS will take this feedback into consideration as we continue to explore how best
we can capture ongoing unmet needs to ensure beneficiaries are getting the support they need.
CAHPS (Part C and D).
Web Mode of Data Collection
As noted in the 2023 Advance Notice and Rate Announcement, in an effort to increase response
rates for the MA and PDP CAHPS surveys, CMS tested the effects on response rates and survey
scores of a web-based mode, as an addition to the current mixed mode protocol. The testing also
allowed for assessment of the impact of the web mode on the current MA and PDP CAHPS
survey instruments with the Agency for Healthcare Research and Quality’s (AHRQ) 5.1 Health
Plan Survey wording clarifications for explicit references to care received via telehealth (phone
or video). Commenters to the 2023 Advance Notice overwhelmingly supported the addition of a
175
web mode for the MA and PDP CAHPS survey as part of the mixed mode data collection
protocol.
In the CAHPS field test we found that for enrollees with email addresses, the web-mail-phone
protocol increased MA response rates by 4 percentage points; we found little change to response
rates for PDPs. We believe that the availability of better email addresses across all contracts will
help improve response rates overall and may help contribute to cost savings for plans in the long
run, as web responses should be less costly.
Nearly all commenters supported the addition of a web-based mode but a few were concerned
the web option would introduce bias. Based on testing and evaluation, CMS believes that there is
little to no risk of bias based on the addition of a web-based mode. The use of a three-phase
sequential multimode approach, web followed by mail followed by telephone, allows MA
enrollees choices about how to respond. It maintains or increases response rates for all groups of
Medicare enrollees and is available to those with or without broadband or telephone access.
While the increases in response rates vary slightly by enrollee characteristics, this does not create
bias, as scores from those randomized for the web-mail-phone protocol were similar to those
randomized for the mail-phone protocol in our field test. Of 39 items compared between the
web-mail-phone and mail-phone protocols, none differed in case-mix adjusted mean score at
p<0.01 and only two differed at p<0.05, a pattern consistent with chance. Thus, there is no
evidence of a mode effect on scores from the web-mail-phone protocol relative to the mail-phone
protocol.
In our testing we saw different rates of email availability by plan and, while this may influence
response rate gains, it would not bias plan scores because response by web results in scores
similar to those obtained under the mail-phone protocol. Similarly, no effect on scores over time
is anticipated. To increase the likelihood of responses, health and drug plans should maintain
accurate contact information, including email addresses when available, for their enrollees. In the
field test a majority of respondents in the web-mail-phone protocol still chose to respond by mail
or phone. Among respondents with an available email address, 79% chose to respond by mail or
phone. Further, the composition of respondents is similar in the web-mail-phone and mail-phone
protocols. We compared respondents to the web-mail-phone and mail-phone protocols by age,
sex, LIS/DE status, race/ethnicity, education, and health status, and respondents were quite
similar; the overall pattern of differences was consistent with chance.
A few commenters felt that the addition of web mode should be considered a substantive change,
suggesting it would change the denominator of the CAHPS measures. CMS disagrees that this is
a substantive change because the denominator remains enrollees with at least 6 months of
continuous enrollment at the time of sampling. With this change, the same people with Medicare
are included. The addition of web to the mail-phone survey protocol does not change the
specification for the numerator or denominator. Further, the focus of the survey questions that

176
make up the CAHPS survey has not changed, so Part C and D sponsors would be implementing
the same efforts to improve patient experiences of care.
A few commenters asked for additional information about how the web mode will be
implemented. CMS tested and will add the web mode to the existing method of administration by
using a pre-notification letter, an email with reminder (beginning in 2024) or letter survey
invitation with personalized URL to complete the survey online, up to two mailings of the
questionnaire for non-respondents, and telephone follow-up of non-respondents. This is a multi-
pronged, comprehensive survey administration protocol that avoids the weaknesses of reliance
upon mail or telephone administration alone. Additional details about the protocols can be found
in the MA and PDP CAHPS survey OMB package at https://www.cms.gov/Regulations-and-
Guidance/Legislation/PaperworkReductionActof1995/PRA-Listing-Items/CMS-R-246. Similar
to mail and phone administration, the web survey will be conducted in accordance with CMS
protocols and technical specifications. The MA and PDP CAHPS survey can only be
administered by CMS-approved vendors who have met CMS requirements for systems security
and procedures to safeguard data in a manner compliant with the Health Insurance Portability
and Accountability Act (HIPAA) as described at 45 CFR Part 160 and Part 164.
CMS also sought comment on the AHRQ’s 5.1 clarifications that explicitly added references to
in-person, phone, or video appointments to a few of the CAHPS survey items asking about
health care experiences. The survey instructions already ask the respondent to think about the
times they got health care in person, by phone, or by video call when completing the survey, so
the modified question wording just reminds the respondent of the instructions. In the field test we
did not find evidence that the 5.1 changes affect scores on the CAHPS Star Ratings measures.
Commenters generally supported the 5.1 wording changes that are inclusive of telehealth.
As discussed in the Advance Notice, we are planning to implement the web-based mode (as an
addition to the current mixed mode protocol) as well as the 5.1 wording clarifications (to
explicitly include telehealth or use terms appropriate to both telehealth and in-person visits) in
the 2024 CAHPS survey implementation used for the 2025 Star Ratings. These changes were
included in an OMB Paperwork Reduction Act package referenced above for the MA and PDP
CAHPS surveys. We note that while the 2024 Part C and D proposed rule did propose to amend
§§ 422.164(d)(1) and 423.184(d)(1) described at 87 FR 79622 to add collection of survey data
through another mode of survey administration to the non-exhaustive list of non-substantive
measure updates that can be made without rulemaking, that proposal is only a clarification. The
current regulations permit non-substantive changes like those described in this section to be done
through the Advance Notice/Rate Announcement process. As we stated in the 2024 Part C and D
proposed rule, the expansion of how data are collected is non-substantive because there is no
change to the information that is being collected; the only change is the way in which it is
collected. The CAHPS 5.1 wording changes are also non-substantive as specified at §§
422.164(d)(1)(iv)(C) and 423.184(d)(1)(iv)(C) because they reiterate the existing instructions
when answering the questions.
177
Updates to Survey Questions
Also, as noted in the 2023 Advance Notice and Rate Announcement, we tested some additional
questions for potential implementation as part of the MA and PDP CAHPS survey. The new
survey items capture more detail or test new approaches to topics covered in the current MA and
PDP CAHPS surveys (e.g., patient-provider communication, getting test results, communication
between providers), and also new topics (e.g., perceived unfair or insensitive treatment).
Commenters to the 2023 Advance Notice supported adding questions on unfair or insensitive
treatment to the survey, as long as consideration is given to survey length.
The question on unfair treatment asked whether in the last 6 months anyone from a clinic,
emergency room, or doctor’s office treated the enrollee in an unfair or insensitive way because of
their disability, age, culture or religion, language or accent, race or ethnicity, sex (female or
male), sexual orientation, gender or gender identity, or income. While few enrollees reported
experiencing unfair treatment overall, unfair treatment by health condition was most common,
followed by unfair treatment by disability and age. Across MA contracts in the field test, 9.4
percent of respondents endorsed one or more reasons for being treated in an unfair or insensitive
way.
Nearly all commenters on the CY 2024 Advance Notice supported the intent of the question on
unfair treatment, although some shared concerns about the question being added to the MA
CAHPS Survey; for example, some commenters recommended that CMS control for factors that
might affect responses. CMS is considering using the same case-mix adjustors for unfair
treatment as for other CAHPS measures. We will consider this item as a display page measure
for 2025 Star Ratings. If it were to be considered as a future Star Ratings measure, once CMS
has more experience with the measure, we would put the potential measure through the Measures
Under Consideration process, with future rulemaking used to adopt the measure for the Star
Ratings program.
We also tested modifications to the Getting Appointments and Care Quickly measure. For
example, we tested a question that would replace the current question “In the last 6 months, how
often did you see the person you came to see within 15 minutes of your appointment time?” in
the existing three-item composite measure. The replacement question that did not focus on the
exact amount of time waiting did not test well. As an alternative, we considered removing the
question related to waiting more than 15 minutes, since telehealth and type of provider may
influence how enrollees respond to this item. This would reduce the Getting Appointments and
Care Quickly measure to the existing two items:
• In the last 6 months, when you needed care right away, how often did you get care as
soon as you needed?
• In the last 6 months, how often did you get an appointment for a check-up or routine care
as soon as you needed?

178
Although this change would reduce the reliability of the measure somewhat, a two-item Getting
Appointments and Care Quickly measure would still have high reliability with a mean reliability
of 0.75.
60
We solicited stakeholder feedback on removing this question from the Getting
Appointments and Care Quickly measure starting with the 2024 survey administered for the
2025 Star Ratings. This change would be considered non-substantive as described at §
422.164(d)(1) since it would not change the population covered by this measure, the two existing
questions that would continue to be included in the measure, and the intent of the measure that
focuses on the individual’s experience of getting care as soon as needed. CMS received
overwhelming support for removing the 15-minute wait time question from the Getting
Appointments and Care Quickly measure. We will remove this question from Getting
Appointments and Care Quickly for the 2025 Star Ratings.
We also tested some potential alternative questions for the current questions included in the Care
Coordination measure focused on how often doctors, nurses, or health care providers explain the
results of tests, how often the explanations were easy to understand, and how often the
information was as much as was needed. We are conducting ongoing analysis of these questions
to see whether they would fit into an updated Care Coordination measure. CMS will take this
feedback into consideration as we continue to explore alternative questions.
60
See https://www.rand.org/pubs/technical_reports/TR653.html for a description of reliability and what is considered sufficient
reliability to discern differences among groups.
179
Attachment VII. Economic Information for the CY 2024 Rate Announcement
Below, we provide the economic information for significant provisions in the Rate
Announcement. Provisions not specifically addressed below are intended to represent a
continuation of the policies established for CY 2023 and, as a result, do not have an impact
associated with them.
Section A. Changes in the Payment Methodology for Medicare Advantage and PACE for
CY 2024
A1. Medicare Advantage and PACE non-ESRD Ratebook
The FFS growth percentage for the 2024 MA non-ESRD rates is estimated to be 2.45 percent,
and the MA growth percentage for the 2024 MA non-ESRD rates is estimated to be 1.60 percent.
The MA non-ESRD ratebook impact summarized here is calculated by comparing 2024 Part C
expenditures reflecting these growth rate assumptions to the expected 2024 Part C expenditures
assuming the MA non-ESRD ratebook remains unchanged from that finalized for 2023. The net
impact on the Medicare Trust Funds for CY 2024 is expected to be $8.1 billion. This figure
accounts for the impact of the benchmark rate cap, MA rebate, and MA EGWP policies, as well
as the portion of the difference between benchmarks and bids that the government retains and the
portion of the program costs covered by Part B premiums.
The MA growth percentage, used to calculate the 2024 PACE non-ESRD rates as well as in
development of the applicable amount used in setting MA non-ESRD rates, is estimated to
be 1.60 percent. The PACE non-ESRD ratebook impact is calculated by comparing the 2024
PACE expenditures reflecting this growth rate assumption to the expected 2024 PACE
expenditures assuming that the PACE non-ESRD ratebook remains unchanged from the CY
2023 PACE non-ESRD ratebook. The net impact on the Medicare Trust Funds for CY 2024
for the PACE ratebook change is expected to be $30 million. This figure accounts for the
portion of the program costs covered by Part B premiums.
The net impact on the Medicare Trust Funds for CY 2024 of implementing the zero-claims
adjustment in Puerto Rico is expected to be $260 million.
A2. Indirect Medical Education (IME) Phase Out
Section 161 of the Medicare Improvements for Patients and Providers Act of 2008 (MIPPA)
(Pub. L. 110-275) amended section 1853(k)(4) of the Act to require CMS to phase out indirect
medical education (IME) amounts from pre-ACA MA capitation rates, which are used to set
the cap on MA benchmarks and are used as the basis for PACE non-ESRD capitation rates.
Note that section 1894(d)(3) of the Act provides that the IME payment phase-out does not
apply to PACE capitation rates. Section 1853(n)(2)(A)(i) and (n)(2)(F) of the Act provides
that the IME phase-out is applied in developing the post-ACA MA benchmarks. Per statute,
180
the maximum incremental IME phase-out is 0.60 percent of the FFS rate per year. We
estimated the impact of the IME phase-out change between 2023 and 2024. Since the
maximum IME reduction is 8.4 percent in 2023 and 9.0 percent in 2024, we calculate the
impact as the difference for those counties with IME percentages of at least 8.4 percent, with
the maximum impact of 0.6 percent (i.e., the difference between 8.4 and 9.0 percent). Also,
since the IME reduction to MA benchmarks is increasing, the impact is considered to be a net
savings to the Medicare Trust Funds.
In payment year 2024, there are no counties that have IME amounts greater than 8.4 percent of
the FFS rate. Since all counties have IME amounts less than 8.4 percent of their respective FFS
rates, there is no impact by the change in the IME phase-out percentage in 2024. For the ESRD
ratebook, all IME amounts used for MA ESRD rates are less than 8.4 percent of the FFS rate, so
there is no impact from the IME phase-out change on the ESRD ratebook for 2024.
Note that the statutorily prescribed methodology for calculating the IME phase-out in 2024 is the
same as that provided by statute for CY 2023; we are providing this impact assessment for
informational purposes.
A3. Medicare Advantage and PACE ESRD Ratebooks
The FFS growth percentage for the 2024 MA ESRD rates is estimated to be 2.27 percent. The
impact on the MA and PACE ESRD ratebooks is calculated by comparing projected 2024 Part C
expenditures with this growth rate assumption to the expected 2024 Part C expenditures with the
assumption that the MA and PACE ESRD ratebooks would have been unchanged from those
finalized for 2023. The net impact on the Medicare Trust Funds for CY 2024 is expected to be
$440 million. This figure accounts for the portion of the program costs covered by Part B
premiums.
A4. CMS-HCC Risk Adjustment Model
For CY 2024, CMS is finalizing an updated CMS-HCC risk adjustment model for organizations
other than PACE, with a 3-year phase in beginning in CY 2024 when the risk scores will be
calculated as the sum of 33% of the risk score calculated with the updated model (the 2024
model) and 67% of the risk score calculated with the current model (the 2020 model). The CY
2024 impact on MA risk scores of the finalized CMS-HCC risk adjustment model with a 3-year
phase in starting at 33% is projected to be -2.16%, which represents a $7.6 billion net savings to
the Medicare Trust Fund in 2024.When estimating the impact of the proposed model, the impact
takes into account the portion of the difference between benchmarks and bids that the
government retains and the portion of the program costs covered by Part B premiums.
Section B. Changes in the Payment Methodology for Medicare Part D for CY 2024
181
A5. ESRD Risk Adjustment
For CY 2024, CMS is continuing the use of the ESRD risk adjustment models implemented in
CY 2023. Therefore, no economic impact is applicable.
A6. Frailty Adjustment for FIDE SNPs
For CY 2024, CMS is calculating frailty scores for FIDE SNPs by blending 67% of the frailty
scores calculated with the frailty factors used for CY 2023 (associated with the 2020 CMS-HCC
model) and 33% of the frailty scores calculated with the updated frailty factors being finalized
for CY 2024 that do not include the CAHPS survey weight (associated with the finalized 2024
CMS-HCC risk adjustment model). To calculate impacts, CMS utilized the survey results from
the 2021 HOS / HOS-M to estimate frailty scores based on the frailty factors used for CY 2023
(the current model) and the frailty factors being finalized for CY 2024 (the updated model), and
blended them as is being finalized. The CY 2024 impact of transitioning to frailty scores
calculated using the updated frailty factors, relative to CY 2023, is a change in frailty scores of -
0.58%, which represents a net savings of less than $10 million dollars to the Medicare Trust
Funds in 2024.
A7. MA Coding Pattern Adjustment
For CY 2024, we will continue to apply the statutory minimum coding pattern difference
adjustment (5.90%). There is no change in policy from CY 2023, and we applied the same factor
for CY 2023, therefore the year-over-year impact is zero.
A8. Normalization
The normalization factors serve to offset the trend in risk scores and maintain a 1.0 average FFS
risk score. For CY 2024, for the CMS-HCC risk adjustment models with a 2019 or 2020
denominator, CMS will calculate the normalization factors using a five-year linear slope
methodology and updated average FFS risk scores for 2018 through 2022, but continuing to
exclude the 2021 risk score as was done for the CY 2023 normalization factor. For the CMSHCC
risk adjustment models with a 2015 denominator and the RxHCC models, CMS will calculate
the normalization factors using a five-year linear slope methodology and historical FFS risk
scores (2016 through 2020). Since normalization is applied to risk scores to maintain the same
average risk scores in each program year-over-year, the impact of normalization is zero.
B1. Part D Risk Adjustment Model
For CY 2024, we are continuing the use of the RxHCC risk adjustment model that was
implemented in CY 2023. Therefore, no economic impact is applicable.
182
B2. Annual Percentage Increase for Part D Parameters
The methodology for updating other Part D parameters for CY 2024 remains unchanged from
that used for CY 2023. As a result, updating the other Part D parameters does not have an impact
on the Medicare Trust Fund alone; the impact of such parameter updates is dependent on the
behavior and bid assumptions of Part D plan sponsors.

183
Attachment VIII. CMS-HCC Risk Adjustment Factors & Predictive Ratio Tables
Table VIII-1. 2024 CMS-HCC Model Relative Factors for Continuing Enrollees
Variable Description Label
Community,
NonDual,
Aged
Community,
NonDual,
Disabled
Community,
FBDual,
Aged
Community,
FBDual,
Disabled
Community,
PBDual,
Aged
Community,
PBDual,
Disabled
Institutional
Female
0-34 Years
-
0.238
-
0.346
-
0.454
0.948
35-44 Years
-
0.288
-
0.332
-
0.420
0.810
45-54 Years
-
0.340
-
0.384
-
0.404
1.031
55-59 Years
-
0.385
-
0.421
-
0.424
0.949
60-64 Years
-
0.436
-
0.502
-
0.414
0.881
65-69 Years
0.330
-
0.435
-
0.365
-
1.188
70-74 Years
0.395
-
0.506
-
0.423
-
1.119
75-79 Years
0.465
-
0.596
-
0.485
-
0.965
80-84 Years
0.524
-
0.665
-
0.544
-
0.862
85-89 Years
0.624
-
0.775
-
0.618
-
0.750
90-94 Years
0.737
-
0.869
-
0.738
-
0.627
95 Years or Over
0.742
-
0.877
-
0.835
-
0.481
Male
0-34 Years
-
0.106
-
0.191
-
0.306
0.826
35-44 Years
-
0.154
-
0.204
-
0.261
0.719
45-54 Years
-
0.215
-
0.293
-
0.300
0.991
55-59 Years
-
0.283
-
0.410
-
0.353
0.989
60-64 Years
-
0.345
-
0.504
-
0.374
0.917
65-69 Years
0.332
-
0.531
-
0.375
-
1.275
70-74 Years
0.396
-
0.626
-
0.417
-
1.224
75-79 Years
0.502
-
0.714
-
0.498
-
1.319
80-84 Years
0.571
-
0.789
-
0.565
-
1.238
85-89 Years
0.664
-
0.907
-
0.615
-
1.135
90-94 Years
0.800
-
0.993
-
0.712
-
0.946
95 Years or Over
0.896
-
1.058
-
0.904
-
0.825
Medicaid and Originally Disabled Interactions
Originally Disabled, Female
0.228
-
0.160
-
0.103
-
-
Originally Disabled, Male
0.135
-
0.158
-
0.075
-
-
Medicaid
-
-
-
-
-
-
0.130

184
Variable Description Label
Community,
NonDual,
Aged
Community,
NonDual,
Disabled
Community,
FBDual,
Aged
Community,
FBDual,
Disabled
Community,
PBDual,
Aged
Community,
PBDual,
Disabled
Institutional
Disease Coefficients
HCC1
HIV/AIDS
0.301
0.213
0.397
0.237
0.196
0.109
1.322
HCC2
Septicemia, Sepsis, Systemic
Inflammatory Response
Syndrome/Shock
0.500 0.598 0.649 0.780 0.447 0.591 0.605
HCC6
Opportunistic Infections
0.381
0.763
0.588
0.833
0.518
0.685
0.728
HCC17
Cancer Metastatic to Lung,
Liver, Brain, and Other Organs;
Acute Myeloid Leukemia
Except Promyelocytic
4.209 3.995 3.896 4.235 3.946 4.103 1.952
HCC18
Cancer Metastatic to Bone,
Other and Unspecified
Metastatic Cancer; Acute
Leukemia Except Myeloid
2.341 2.486 2.277 2.537 2.166 2.403 1.110
HCC19
Myelodysplastic Syndromes,
Multiple Myeloma, and Other
Cancers
1.798 1.989 1.563 1.661 1.520 1.554 0.957
HCC20
Lung and Other Severe Cancers
1.136
0.978
1.166
1.173
1.214
1.067
0.672
HCC21
Lymphoma and Other Cancers
0.671
0.540
0.654
0.739
0.627
0.618
0.493
HCC22
Bladder, Colorectal, and Other
Cancers
0.363 0.366 0.382 0.409 0.410 0.351 0.314
HCC23
Prostate, Breast, and Other
Cancers and Tumors
0.186 0.233 0.196 0.218 0.203 0.237 0.197
HCC35
Pancreas Transplant Status
0.949
1.393
1.117
0.573
1.117
2.740
1.106
HCC36
Diabetes with Severe Acute
Complications
0.166 0.191 0.186 0.235 0.166 0.210 0.280
HCC37
Diabetes with Chronic
Complications
0.166 0.191 0.186 0.235 0.166 0.210 0.280
HCC38
Diabetes with Glycemic,
Unspecified, or No
Complications
0.166 0.191 0.186 0.235 0.166 0.210 0.280
HCC48
Morbid Obesity
0.186
0.144
0.300
0.178
0.164
0.118
0.442
HCC49
Specified Lysosomal Storage
Disorders
9.256 13.778 2.833 6.399 3.269 7.771 1.528

185
Variable Description Label
Community,
NonDual,
Aged
Community,
NonDual,
Disabled
Community,
FBDual,
Aged
Community,
FBDual,
Disabled
Community,
PBDual,
Aged
Community,
PBDual,
Disabled
Institutional
HCC50
Amyloidosis, Porphyria, and
Other Specified Metabolic
Disorders
0.648 0.883 0.555 0.789 0.435 0.529 0.362
HCC51
Addison's and Cushing's
Diseases, Acromegaly, and
Other Specified Endocrine
Disorders
0.510 0.606 0.634 0.654 0.313 0.393 0.620
HCC62
Liver Transplant
Status/Complications
0.376 0.184 0.261 0.409 0.571 0.271 0.593
HCC63
Chronic Liver Failure/End-
Stage Liver Disorders
0.962 1.032 1.102 1.209 0.861 1.101 0.894
HCC64
Cirrhosis of Liver
0.447
0.383
0.475
0.414
0.391
0.270
0.378
HCC65
Chronic Hepatitis
0.185
0.248
0.101
0.220
0.156
0.189
0.378
HCC68
Cholangitis and Obstruction of
Bile Duct Without Gallstones
0.388 0.383 0.085 0.354 0.391 0.270 0.090
HCC77
Intestine Transplant
Status/Complications
1.172 6.301 5.039 6.161 5.039 5.039 5.089
HCC78
Intestinal
Obstruction/Perforation
0.326 0.534 0.382 0.548 0.478 0.688 0.380
HCC79
Chronic Pancreatitis
0.357
0.574
0.525
0.799
0.444
0.709
0.218
HCC80
Crohn's Disease (Regional
Enteritis)
0.550 0.635 0.490 0.651 0.479 0.603 0.374
HCC81
Ulcerative Colitis
0.244
0.285
0.201
0.286
0.205
0.237
0.258
HCC92
Bone/Joint/Muscle/Severe Soft
Tissue Infections/Necrosis
0.479 0.529 0.611 0.632 0.471 0.539 0.556
HCC93
Rheumatoid Arthritis and Other
Specified Inflammatory
Rheumatic Disorders
0.617 0.470 0.439 0.384 0.405 0.288 0.297
HCC94
Systemic Lupus Erythematosus
and Other Specified Systemic
Connective Tissue Disorders
0.268 0.239 0.237 0.250 0.224 0.196 0.297
HCC107
Sickle Cell Anemia (Hb-SS)
and Thalassemia Beta Zero
0.457 1.449 0.610 1.939 0.303 1.569 0.692

186
Variable Description Label
Community,
NonDual,
Aged
Community,
NonDual,
Disabled
Community,
FBDual,
Aged
Community,
FBDual,
Disabled
Community,
PBDual,
Aged
Community,
PBDual,
Disabled
Institutional
HCC108
Sickle Cell Disorders, Except
Sickle Cell Anemia (Hb-SS)
and Thalassemia Beta Zero;
Beta Thalassemia Major
0.146 0.386 0.103 0.408 0.303 0.416 0.098
HCC109
Acquired Hemolytic, Aplastic,
and Sideroblastic Anemias
1.144 1.815 1.048 1.541 1.009 1.514 0.529
HCC111
Hemophilia, Male
4.639
30.706
15.539
31.424
11.201
32.199
6.310
HCC112
Immune Thrombocytopenia
and Specified Coagulation
Defects and Hemorrhagic
Conditions
0.450 0.640 0.460 0.634 0.574 0.708 0.516
HCC114
Common Variable and
Combined Immunodeficiencies
2.262 2.598 2.016 2.670 2.137 2.789 0.691
HCC115
Specified Immunodeficiencies
and White Blood Cell
Disorders
0.565 0.692 0.438 0.498 0.302 0.613 0.691
HCC125
Dementia, Severe
0.341
0.296
0.438
0.367
0.401
0.345
-
HCC126
Dementia, Moderate
0.341
0.296
0.438
0.367
0.401
0.345
-
HCC127
Dementia, Mild or Unspecified
0.341
0.296
0.438
0.367
0.401
0.345
-
HCC135
Drug Use with Psychotic
Complications
0.424 0.637 0.702 1.181 0.522 0.922 0.297
HCC136
Alcohol Use with Psychotic
Complications
0.424 0.637 0.502 1.181 0.522 0.922 0.297
HCC137
Drug Use Disorder,
Moderate/Severe, or Drug Use
with Non-Psychotic
Complications
0.424 0.365 0.502 0.471 0.394 0.348 0.297
HCC138
Drug Use Disorder, Mild,
Uncomplicated, Except
Cannabis
0.423 0.264 0.502 0.384 0.355 0.348 0.297
HCC139
Alcohol Use Disorder,
Moderate/Severe, or Alcohol
Use with Specified Non-
Psychotic Complications
0.242 0.207 0.478 0.250 0.308 0.159 -

187
Variable Description Label
Community,
NonDual,
Aged
Community,
NonDual,
Disabled
Community,
FBDual,
Aged
Community,
FBDual,
Disabled
Community,
PBDual,
Aged
Community,
PBDual,
Disabled
Institutional
HCC151
Schizophrenia
0.511
0.380
0.591
0.414
0.501
0.304
0.449
HCC152
Psychosis, Except
Schizophrenia
0.484 0.290 0.579 0.255 0.501 0.247 0.208
HCC153
Personality Disorders;
Anorexia/Bulimia Nervosa
0.396 0.290 0.420 0.255 0.464 0.232 0.199
HCC154
Bipolar Disorders without
Psychosis
0.351 0.166 0.349 0.126 0.314 0.108 0.199
HCC155
Major Depression, Moderate or
Severe, without Psychosis
0.299 0.166 0.316 0.126 0.269 0.108 0.199
HCC180
Quadriplegia
1.125
0.986
1.068
1.095
1.311
1.399
0.735
HCC181
Paraplegia
0.942
0.648
0.859
0.832
0.883
0.852
0.563
HCC182
Spinal Cord Disorders/Injuries
0.478
0.368
0.402
0.308
0.401
0.316
0.270
HCC190
Amyotrophic Lateral Sclerosis
and Other Motor Neuron
Disease, Spinal Muscular
Atrophy
1.175 1.792 1.427 3.642 0.640 1.243 0.628
HCC191
Quadriplegic Cerebral Palsy
0.855
0.743
0.393
0.466
0.840
0.104
-
HCC192
Cerebral Palsy, Except
Quadriplegic
0.314 0.129 - 0.067 0.220 0.104 -
HCC193
Chronic Inflammatory
Demyelinating Polyneuritis and
Multifocal Motor Neuropathy
1.692 1.427 0.957 0.939 1.149 0.850 0.913
HCC195
Myasthenia Gravis with
(Acute) Exacerbation
2.909 3.633 2.153 3.323 2.690 1.779 1.837
HCC196
Myasthenia Gravis without
(Acute) Exacerbation and Other
Myoneural Disorders
0.516 0.642 0.503 0.507 0.427 0.248 0.486
HCC197
Muscular Dystrophy
0.426
0.632
0.369
0.681
0.162
0.145
0.292
HCC198
Multiple Sclerosis
0.647
0.908
0.791
1.143
0.569
0.770
0.226
HCC199
Parkinson and Other
Degenerative Disease of Basal
Ganglia
0.615 0.517 0.634 0.504 0.474 0.354 0.219

188
Variable Description Label
Community,
NonDual,
Aged
Community,
NonDual,
Disabled
Community,
FBDual,
Aged
Community,
FBDual,
Disabled
Community,
PBDual,
Aged
Community,
PBDual,
Disabled
Institutional
HCC200
Friedreich and Other
Hereditary Ataxias; Huntington
Disease
0.279 0.208 0.165 0.281 0.050 0.428 -
HCC201
Seizure Disorders and
Convulsions
0.245 0.196 0.233 0.170 0.245 0.202 0.131
HCC202
Coma, Brain
Compression/Anoxic Damage
0.543 0.238 0.721 0.279 0.549 0.309 0.097
HCC211
Respirator
Dependence/Tracheostomy
Status/Complications
0.879 0.878 1.981 1.418 1.022 0.590 1.570
HCC212
Respiratory Arrest
0.370
0.510
0.573
0.662
0.409
0.493
0.258
HCC213
Cardio-Respiratory Failure and
Shock
0.370 0.510 0.573 0.662 0.409 0.493 0.258
HCC221
Heart Transplant
Status/Complications
1.053 0.999 1.412 1.781 0.880 1.371 0.840
HCC222
End-Stage Heart Failure
2.505
5.770
2.927
6.612
3.009
6.106
0.826
HCC223
Heart Failure with Heart Assist
Device/Artificial Heart
2.505 5.770 2.927 6.612 3.009 6.106 0.826
HCC224
Acute on Chronic Heart Failure
0.360
0.442
0.406
0.537
0.311
0.411
0.217
HCC225
Acute Heart Failure (Excludes
Acute on Chronic)
0.360 0.442 0.406 0.537 0.311 0.411 0.217
HCC226
Heart Failure, Except End-
Stage and Acute
0.360 0.442 0.406 0.537 0.311 0.411 0.217
HCC227
Cardiomyopathy/Myocarditis
0.189
0.200
0.173
0.198
0.145
0.186
0.189
HCC228
Acute Myocardial Infarction
0.252
0.254
0.493
0.517
0.324
0.407
0.310
HCC229
Unstable Angina and Other
Acute Ischemic Heart Disease
0.240 0.254 0.325 0.458 0.278 0.315 0.310
HCC238
Specified Heart Arrhythmias
0.299
0.296
0.407
0.304
0.293
0.261
0.245
HCC248
Intracranial Hemorrhage
0.239
0.180
0.377
0.332
0.313
0.183
0.081
HCC249
Ischemic or Unspecified Stroke
0.239
0.180
0.377
0.277
0.299
0.172
0.081
HCC253
Hemiplegia/Hemiparesis
0.387
0.320
0.437
0.390
0.437
0.403
-
HCC254
Monoplegia, Other Paralytic
Syndromes
0.321 0.172 0.292 0.365 0.290 0.335 -

189
Variable Description Label
Community,
NonDual,
Aged
Community,
NonDual,
Disabled
Community,
FBDual,
Aged
Community,
FBDual,
Disabled
Community,
PBDual,
Aged
Community,
PBDual,
Disabled
Institutional
HCC263
Atherosclerosis of Arteries of
the Extremities with Ulceration
or Gangrene
1.118 1.066 1.432 1.276 1.007 1.056 0.696
HCC264
Vascular Disease with
Complications
0.455 0.520 0.498 0.461 0.513 0.622 0.338
HCC267
Deep Vein Thrombosis and
Pulmonary Embolism
0.294 0.431 0.445 0.568 0.338 0.498 0.245
HCC276
Lung Transplant
Status/Complications
2.531 1.583 2.210 2.292 2.961 1.277 3.085
HCC277
Cystic Fibrosis
0.998
2.818
1.340
3.760
0.650
3.829
0.873
HCC278
Idiopathic Pulmonary Fibrosis
and Lung Involvement in
Systemic Sclerosis
0.818 1.209 0.791 1.640 0.650 0.937 0.873
HCC279
Severe Persistent Asthma
0.818
0.842
0.594
0.808
0.650
0.804
0.873
HCC280
Chronic Obstructive Pulmonary
Disease, Interstitial Lung
Disorders, and Other Chronic
Lung Disorders
0.319 0.209 0.390 0.281 0.321 0.234 0.312
HCC282
Aspiration and Specified
Bacterial Pneumonias
0.440 0.362 0.538 0.269 0.409 0.173 0.353
HCC283
Empyema, Lung Abscess
0.204
-
0.131
0.074
-
-
-
HCC298
Severe Diabetic Eye Disease,
Retinal Vein Occlusion, and
Vitreous Hemorrhage
0.336 0.364 0.323 0.319 0.327 0.301 0.545
HCC300
Exudative Macular
Degeneration
0.596 0.366 0.370 0.255 0.459 0.380 0.196
HCC326
Chronic Kidney Disease, Stage
5
0.815 0.927 0.985 0.946 0.965 1.050 0.958
HCC327
Chronic Kidney Disease,
Severe (Stage 4)
0.514 0.523 0.565 0.661 0.484 0.447 0.462
HCC328
Chronic Kidney Disease,
Moderate (Stage 3B)
0.127 0.179 0.116 0.181 0.140 0.178 0.145
HCC329
Chronic Kidney Disease,
Moderate (Stage 3, Except 3B)
0.127 0.179 0.116 0.181 0.140 0.178 0.145

190
Variable Description Label
Community,
NonDual,
Aged
Community,
NonDual,
Disabled
Community,
FBDual,
Aged
Community,
FBDual,
Disabled
Community,
PBDual,
Aged
Community,
PBDual,
Disabled
Institutional
HCC379
Pressure Ulcer of Skin with
Necrosis Through to Muscle,
Tendon, or Bone
1.965 2.140 2.580 2.570 2.349 2.349 1.420
HCC380
Chronic Ulcer of Skin, Except
Pressure, Through to Bone or
Muscle
1.078 1.091 1.422 1.285 1.268 1.378 0.839
HCC381
Pressure Ulcer of Skin with
Full Thickness Skin Loss
1.075 1.091 1.379 1.192 1.136 1.089 0.423
HCC382
Pressure Ulcer of Skin with
Partial Thickness Skin Loss
0.838 0.994 1.029 0.935 0.845 0.937 0.343
HCC383
Chronic Ulcer of Skin, Except
Pressure, Not Specified as
Through to Bone or Muscle
0.646 0.707 0.890 0.707 0.660 0.654 0.343
HCC385
Severe Skin Burn
1.291
0.234
2.362
0.857
-
0.204
-
HCC387
Pemphigus, Pemphigoid, and
Other Specified Autoimmune
Skin Disorders
0.406 0.302 0.658 0.622 0.477 0.498 0.125
HCC397
Major Head Injury with Loss of
Consciousness > 1 Hour
0.199 0.150 0.349 0.190 0.128 0.052 0.085
HCC398
Major Head Injury with Loss of
Consciousness < 1 Hour or
Unspecified
0.199 0.150 0.349 0.190 0.128 0.052 0.085
HCC399
Major Head Injury without
Loss of Consciousness
0.199 0.150 0.349 0.190 0.128 0.052 0.085
HCC401
Vertebral Fractures without
Spinal Cord Injury
0.522 0.605 0.622 0.559 0.538 0.412 0.231
HCC402
Hip Fracture/Dislocation
0.467
0.561
0.561
0.570
0.499
0.527
0.089
HCC405
Traumatic Amputations and
Complications
0.598 0.577 0.799 0.844 0.639 0.698 0.284
HCC409
Amputation Status, Lower
Limb/Amputation
Complications
0.598 0.562 0.799 0.844 0.604 0.623 0.284

191
Variable Description Label
Community,
NonDual,
Aged
Community,
NonDual,
Disabled
Community,
FBDual,
Aged
Community,
FBDual,
Disabled
Community,
PBDual,
Aged
Community,
PBDual,
Disabled
Institutional
HCC454
Stem Cell, Including Bone
Marrow, Transplant
Status/Complications
1.068 0.452 1.326 0.608 1.338 0.416 1.596
HCC463
Artificial Openings for Feeding
or Elimination
0.673 0.914 0.891 0.947 0.526 0.853 0.634
Disease Interactions
DIABETES_HF
Diabetes*Heart Failure
0.112
0.023
0.183
0.041
0.164
0.053
0.209
HF_CHR_
LUNG
Heart Failure*Chronic Lung
Disorder
0.078 0.062 0.109 0.097 0.140 0.108 0.145
HF_KIDNEY
Heart Failure*Kidney
0.176
0.314
0.194
0.420
0.140
0.328
-
CHR_LUNG_CARD
_RESP_FAIL
Chronic Lung
Disorder*Cardiorespiratory
Failure
0.254 0.242 0.340 0.275 0.329 0.270 0.331
HF_HCC238
Heart Failure*Specified Heart
Arrhythmias
0.077 0.257 0.140 0.372 0.135 0.314 -
gSubUseDisorder_
gPsych_
Substance Use
Disorder*Psychiatric
- 0.087 - 0.152 - 0.149 -
Disabled/Disease Interactions
DISABLED_
HF
Disabled, Heart Failure - - - - - - 0.488
DISABLED_
ULCER_
Disabled, Skin Ulcer - - - - - - 0.537
DISABLED_
CANCER
Disabled, Cancer - - - - - - 0.367
DISABLED_
NEURO_
Disabled, Neurological - - - - - - 0.154
DISABLED_
CHR_LUNG
Disabled, Chronic Lung
Disorder
- - - - - - 0.278
Payment HCC Counts
D1
1 payment HCCs
-
-
-
-
-
-
-
D2
2 payment HCCs
-
-
-
-
-
-
-
D3
3 payment HCCs
-
-
-
-
-
-
-
D4
4 payment HCCs
-
-
-
-
-
-
-
D5
5 payment HCCs
0.050
0.088
0.049
0.095
0.016
0.105
-

192
Variable Description Label
Community,
NonDual,
Aged
Community,
NonDual,
Disabled
Community,
FBDual,
Aged
Community,
FBDual,
Disabled
Community,
PBDual,
Aged
Community,
PBDual,
Disabled
Institutional
D6
6 payment HCCs
0.102
0.223
0.071
0.245
0.096
0.191
-
D7
7 payment HCCs
0.188
0.380
0.160
0.472
0.207
0.435
-
D8
8 payment HCCs
0.316
0.440
0.267
0.607
0.345
0.581
-
D9
9 payment HCCs
0.444
0.750
0.353
0.841
0.345
0.823
-
D10P
10 or more payment HCCs
0.728
1.431
0.746
1.471
0.901
1.268
0.373
NOTES:
1. The denominator used is $10,402.34.
2. In the “disease interactions” and “disabled interactions,” the variables are defined as follows:
Cancer = HCCs 17-23
Cardiorespiratory Failure = HCCs 211-213
Chronic Lung Disorder = HCCs 276-280
Diabetes = HCCs 35-38
Heart Failure = HCCs 221-226
Kidney = HCCs 326-329
Neurological = HCCs 180-192, 195, 196, 198, 199
Psychiatric = HCCs 151-155
Skin Ulcer = HCCs 379-382
Specified Heart Arrhythmias = HCC 238
Substance Use = HCCs 135-139
SOURCE: 2018-2019 100% Medicare data.

193
Table VIII-2. 2024 CMS-HCC Model Relative Factors for Aged and Disabled New Enrollees
Non-Medicaid &
Non-Originally
Disabled
Medicaid &
Non-Originally
Disabled
Non-Medicaid &
Originally
Disabled
Medicaid &
Originally
Disabled
Female
0-34 Years
0.711
1.025
-
-
35-44 Years
0.950
1.303
-
-
45-54 Years
1.155
1.415
-
-
55-59 Years
1.152
1.289
-
-
60-64 Years
1.212
1.396
-
-
65 Years
0.532
0.986
1.212
1.599
66 Years
0.532
0.990
1.276
1.599
67 Years
0.557
1.004
1.276
1.599
68 Years
0.584
1.004
1.276
2.021
69 Years
0.625
1.004
1.276
2.021
70-74 Years
0.694
1.043
1.276
2.021
75-79 Years
0.901
1.128
1.276
2.021
80-84 Years
0.988
1.342
1.276
2.021
85-89 Years
1.287
1.563
1.287
2.021
90-94 Years
1.287
1.712
1.287
2.021
95 Years or Over
1.287
1.712
1.287
2.021
Male
0-34 Years
0.409
0.738
-
-
35-44 Years
0.669
1.264
-
-
45-54 Years
0.906
1.420
-
-
55-59 Years
0.984
1.477
-
-
60-64 Years
1.057
1.542
-
-
65 Years
0.567
1.182
1.057
1.727
66 Years
0.576
1.234
1.155
1.959
67 Years
0.617
1.319
1.155
1.959
68 Years
0.678
1.367
1.155
1.959
69 Years
0.684
1.455
1.297
1.959
70-74 Years
0.808
1.455
1.297
1.959
75-79 Years
1.049
1.455
1.297
2.813
80-84 Years
1.245
1.503
1.297
2.813
85-89 Years
1.516
1.682
1.516
2.813
90-94 Years
1.516
1.981
1.516
2.813
95 Years or Over
1.516
1.981
1.516
2.813
NOTES:
3. The denominator used is $10,402.34.
4. For payment purposes, a new enrollee is a beneficiary who did not have 12 months of Part B eligibility in the data
collection year. CMS-HCC new enrollee models are not based on diagnoses, but include factors for different age and
sex combinations by Medicaid and the original reason for Medicare entitlement.
SOURCE: 2018-2019 100% Medicare data.

194
Table VIII-3. 2024 CMS-HCC Model Relative Factors for New Enrollees in Chronic Condition
Special Needs Plans (C-SNPs)
Non-Medicaid &
Non-Originally
Disabled
Medicaid &
Non-Originally
Disabled
Non-Medicaid &
Originally
Disabled
Medicaid &
Originally
Disabled
Female
0-34 Years
1.332
1.655
-
-
35-44 Years
1.332
1.655
-
-
45-54 Years
1.536
1.965
-
-
55-59 Years
1.536
1.989
-
-
60-64 Years
1.628
2.030
-
-
65 Years
0.900
1.285
1.708
2.085
66 Years
0.900
1.285
1.708
2.085
67 Years
0.940
1.351
1.719
2.148
68 Years
1.004
1.351
1.745
2.148
69 Years
1.020
1.467
1.755
2.233
70-74 Years
1.195
1.634
1.929
2.295
75-79 Years
1.419
1.885
2.032
2.484
80-84 Years
1.612
2.061
2.239
2.735
85-89 Years
1.833
2.250
2.239
2.735
90-94 Years
2.016
2.400
2.239
2.735
95 Years or Over
2.016
2.400
2.239
2.735
Male
0-34 Years
1.206
1.485
-
-
35-44 Years
1.206
1.485
-
-
45-54 Years
1.472
1.845
-
-
55-59 Years
1.552
1.994
-
-
60-64 Years
1.642
2.035
-
-
65 Years
0.944
1.422
1.642
2.035
66 Years
0.944
1.422
1.659
2.150
67 Years
0.985
1.477
1.659
2.195
68 Years
1.005
1.477
1.659
2.195
69 Years
1.065
1.477
1.677
2.246
70-74 Years
1.216
1.735
1.807
2.316
75-79 Years
1.496
1.952
2.039
2.487
80-84 Years
1.704
2.194
2.155
2.573
85-89 Years
1.924
2.403
2.346
2.573
90-94 Years
2.142
2.403
2.346
2.573
95 Years or Over
2.142
2.403
2.346
2.573
NOTES:
1. The denominator used is $10,402.34.
2. For payment purposes, a new enrollee is a beneficiary who did not have 12 months of Part B eligibility in the data
collection year. CMS-HCC new enrollee models are not based on diagnoses, but include factors for different age and
sex combinations by Medicaid and the original reason for Medicare entitlement.
SOURCE: 2018-2019 100% Medicare data.

195
Table VIII-4. 2024 CMS-HCC Model with Disease Hierarchies
CMS-HCC If the Disease Group is listed in this column…
…Then drop the
CMS-HCC listed in
this column
CMS-HCC Hierarchical Condition Category Label
17
Cancer Metastatic to Lung, Liver, Brain, and Other Organs; Acute Myeloid
Leukemia Except Promyelocytic
18, 19, 20, 21, 22, 23
18
Cancer Metastatic to Bone, Other and Unspecified Metastatic Cancer;
Acute Leukemia Except Myeloid
19, 20, 21, 22, 23
19
Myelodysplastic Syndromes, Multiple Myeloma, and Other Cancers
20, 21, 22, 23
20
Lung and Other Severe Cancers
21, 22, 23
21
Lymphoma and Other Cancers
22, 23
22
Bladder, Colorectal, and Other Cancers
23
35
Pancreas Transplant Status
36, 37, 38
36
Diabetes with Severe Acute Complications
37, 38
37
Diabetes with Chronic Complications
38
62
Liver Transplant Status/Complications
63, 64, 65, 68
63
Chronic Liver Failure/End-Stage Liver Disorders
64, 65, 68, 202
64
Cirrhosis of Liver
65, 68
77
Intestine Transplant Status/Complications
78, 80, 81
80
Crohn's Disease (Regional Enteritis)
81
93
Rheumatoid Arthritis and Other Specified Inflammatory Rheumatic
Disorders
94
107
Sickle Cell Anemia (Hb-SS) and Thalassemia Beta Zero
108
111
Hemophilia, Male
112
114
Common Variable and Combined Immunodeficiencies
115
125
Dementia, Severe
126, 127
126
Dementia, Moderate
127
135
Drug Use with Psychotic Complications
136, 137, 138, 139
136
Alcohol Use with Psychotic Complications
137, 138, 139
137
Drug Use Disorder, Moderate/Severe, or Drug Use with Non-Psychotic
Complications
138, 139
138
Drug Use Disorder, Mild, Uncomplicated, Except Cannabis
139
151
Schizophrenia
152, 153, 154, 155
152
Psychosis, Except Schizophrenia
153, 154, 155
153
Personality Disorders; Anorexia/Bulimia Nervosa
154, 155
154
Bipolar Disorders without Psychosis
155
180
Quadriplegia
181, 182, 253, 254
181
Paraplegia
182, 254
191 Quadriplegic Cerebral Palsy
180, 181, 182, 192,
253, 254
192 Cerebral Palsy, Except Quadriplegic
180, 181, 182, 253,
254
195
Myasthenia Gravis with (Acute) Exacerbation
196
211
Respirator Dependence/Tracheostomy Status/Complications
212, 213
212
Respiratory Arrest
213

196
CMS-HCC If the Disease Group is listed in this column…
…Then drop the
CMS-HCC listed in
this column
CMS-HCC Hierarchical Condition Category Label
221 Heart Transplant Status/Complications
222, 223, 224, 225,
226, 227
222 End-Stage Heart Failure
223, 224, 225, 226,
227
223
Heart Failure with Heart Assist Device/Artificial Heart
224, 225, 226, 227
224
Acute on Chronic Heart Failure
225, 226, 227
225
Acute Heart Failure (Excludes Acute on Chronic)
226, 227
226
Heart Failure, Except End-Stage and Acute
227
228
Acute Myocardial Infarction
229
248
Intracranial Hemorrhage
249
253
Hemiplegia/Hemiparesis
254
263
Atherosclerosis of Arteries of the Extremities with Ulceration or Gangrene
264, 383, 409
276
Lung Transplant Status/Complications
277, 278, 279, 280
277
Cystic Fibrosis
278, 279, 280
278
Idiopathic Pulmonary Fibrosis and Lung Involvement in Systemic Sclerosis
279, 280
279
Severe Persistent Asthma
280
282
Aspiration and Specified Bacterial Pneumonias
283
326
Chronic Kidney Disease, Stage 5
327, 328, 329
327
Chronic Kidney Disease, Severe (Stage 4)
328, 329
328
Chronic Kidney Disease, Moderate (Stage 3B)
329
379
Pressure Ulcer of Skin with Necrosis Through to Muscle, Tendon, or Bone
380, 381, 382, 383
380
Chronic Ulcer of Skin, Except Pressure, Through to Bone or Muscle
381, 382, 383
381
Pressure Ulcer of Skin with Full Thickness Skin Loss
382, 383
382
Pressure Ulcer of Skin with Partial Thickness Skin Loss
383
397
Major Head Injury with Loss of Consciousness > 1 Hour
202, 398, 399
398
Major Head Injury with Loss of Consciousness < 1 Hour or Unspecified
202, 399
405
Traumatic Amputations and Complications
409
How Payments are Made with a Disease Hierarchy
EXAMPLE: If a beneficiary triggers HCCs 195 (Myasthenia Gravis with (Acute) Exacerbation) and 196 (Myasthenia Gravis
without (Acute) Exacerbation and Other Myoneural Disorders), then HCC 196 will be dropped. In other words, payment will
always be associated with the HCC in column 1 if an HCC in column 3 also occurs during the same collection period. Therefore,
the organization’s payment will be based on HCC 195 rather than HCC 196.
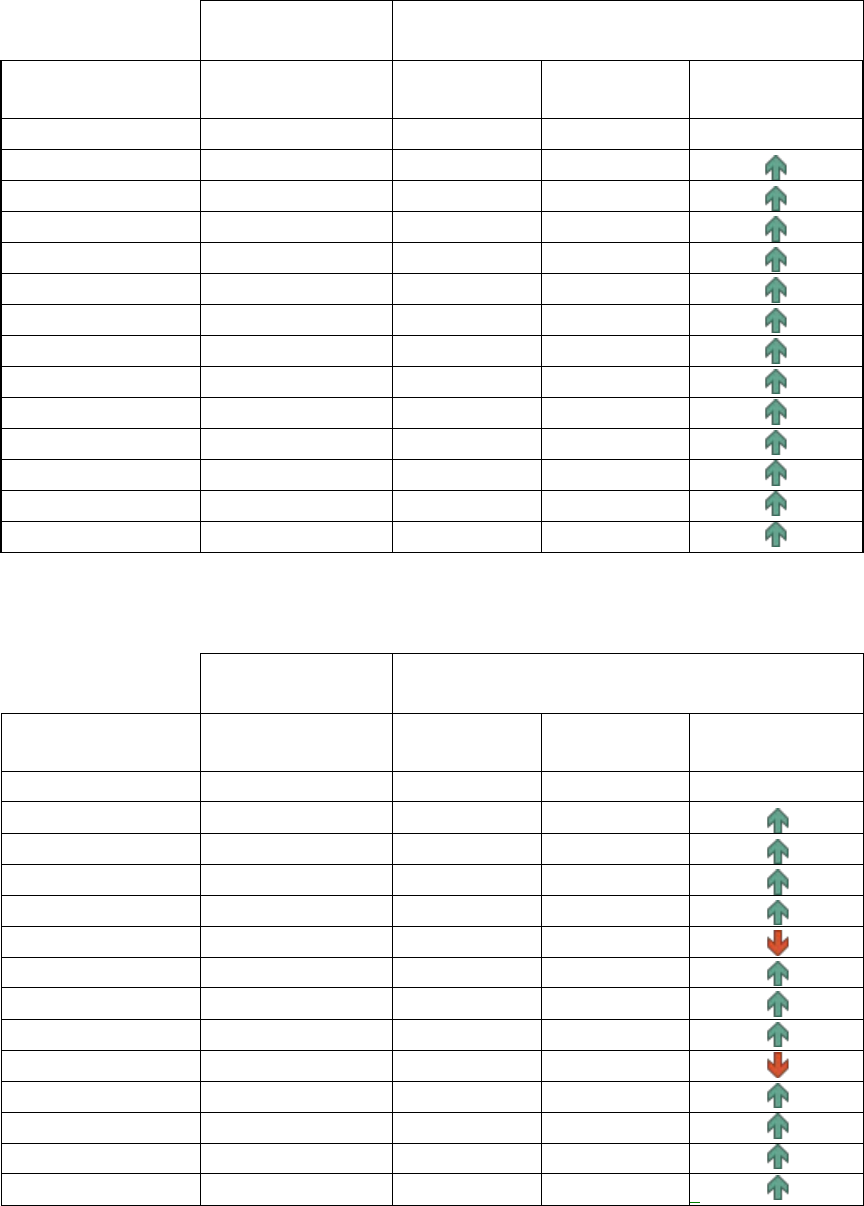
197
Table VIII-5. Predictive Ratios by Deciles of Predicted Risk (sorted low to high):
Non-Dual, Aged (Age >=65) Continuing Enrollee
2014/2015 Sample 2018/2019 Sample
Deciles
2020 Model 2020 Model 2024 Model
Improvement in
Predictive Risk
Entire sample
1.000
0.968
1.000
-
First (lowest) decile
0.968
0.902
0.977
Second decile
0.983
0.938
0.981
Third decile
0.996
0.940
1.026
Fourth decile
0.989
0.958
1.003
Fifth decile
1.003
0.977
0.995
Sixth decile
1.002
0.970
0.993
Seventh decile
1.005
0.983
0.996
Eighth decile
1.003
0.982
0.996
Ninth decile
1.003
0.987
1.006
Tenth (highest)
1.003
0.963
1.003
Top 5%
1.000
0.942
1.000
Top 1%
0.984
0.917
0.987
Top 0.1%
0.959
0.879
0.967
Table VIII-6. Predictive Ratios by Deciles of Predicted Risk (sorted low to high):
Non-Dual, Disabled (Age <65) Continuing Enrollee
2014/2015 Sample 2018/2019 Sample
Deciles
2020 Model 2020 Model 2024 Model
Improvement in
Predictive Risk
Entire sample
1.000
0.979
1.000
-
First (lowest) decile
1.090
1.100
0.932
_
_
Second decile
0.959
0.975
0.990
Third decile
0.982
0.964
0.983
Fourth decile
0.982
0.977
1.011
Fifth decile
0.952
0.968
0.955
Sixth decile
0.997
0.965
0.997
Seventh decile
0.983
0.972
0.997
Eighth decile
1.008
1.004
1.002
Ninth decile
1.028
1.013
1.022
Tenth (highest)
1.001
0.959
1.004
Top 5%
0.991
0.935
0.998
Top 1%
0.999
0.922
0.981
Top 0.1%
0.979
0.874
0.960

198
Table VIII-7. Predictive Ratios by Deciles of Predicted Risk (sorted low to high):
Full Benefit Dual, Aged (Age >=65) Continuing Enrollee
2014/2015 Sample 2018/2019 Sample
Deciles
2020 Model 2020 Model 2024 Model
Improvement in
Predictive Risk
Entire sample
1.000
1.002
1.000
-
First (lowest) decile
0.969
0.949
0.996
Second decile
1.006
0.980
1.029
Third decile
0.988
1.012
1.015
Fourth decile
0.994
0.996
0.983
Fifth decile
1.006
1.017
0.986
Sixth decile
1.000
1.006
0.997
Seventh decile
1.004
1.012
0.992
Eighth decile
1.003
1.014
1.002
Ninth decile
1.002
1.009
1.002
Tenth (highest)
1.001
0.991
1.003
Top 5%
1.004
0.983
1.002
Top 1%
0.978
0.938
0.979
Top 0.1%
0.915
0.844
0.919
_
Table VIII-8. Predictive Ratios by Deciles of Predicted Risk (sorted low to high):
Full Benefit Dual, Disabled (Age <65) Continuing Enrollee
2014/2015 Sample 2018/2019 Sample
Deciles
2020 Model 2020 Model _ 2024 Model
Improvement in
Predictive Risk
Entire sample 1.000 0.988 1.000 -
First (lowest) decile 1.076 1.008 0.967
Second decile 1.016 1.004 1.053
Third decile 0.893 0.869 0.904
Fourth decile 0.940 0.957 0.970
Fifth decile 0.992 0.985 1.005
Sixth decile 0.999 1.010 1.005
Seventh decile 1.020 0.995 1.013
Eighth decile 1.019 0.999 0.996
Ninth decile 1.008 1.014 1.016
Tenth (highest) 1.002 0.983 1.002
Top 5% 0.996 0.974 0.995
Top 1% 0.984 0.954 0.983
Top 0.1% 0.873 0.986 1.007

199
Table VIII-9. Predictive Ratios by Deciles of Predicted Risk (sorted low to high):
Partial Benefit Dual, Aged (Age >=65) Continuing Enrollee
2014/2015 Sample 2018/2019 Sample
Deciles
2020 Model 2020 Model 2024 Model
Improvement in
Predictive Risk
Entire sample
1.000
0.992
1.000
-
First (lowest) decile
0.998
0.942
1.000
Second decile
0.998
0.987
1.023
Third decile
0.977
0.933
0.999
Fourth decile
0.987
0.992
1.001
Fifth decile
0.999
0.989
0.976
Sixth decile
1.004
1.016
0.983
Seventh decile
1.003
1.013
1.006
Eighth decile
1.006
1.017
1.000
Ninth decile
1.006
1.021
1.009
Tenth (highest)
0.999
0.968
1.000
Top 5%
0.994
0.951
1.000
Top 1%
0.999
0.931
0.985
Top 0.1%
0.981
0.870
0.981
_
_
Table VIII-10. Predictive Ratios by Deciles of Predicted Risk (sorted low to high):
Partial Benefit Dual, Disabled (Age <65) Continuing Enrollee
2014/2015 Sample 2018/2019 Sample
Deciles
2020 Model 2020 Model 2024 Model
Improvement in
Predictive Risk
Entire sample
1.000
0.988
1.000
-
First (lowest) decile
0.935
0.878
0.989
Second decile
1.020
1.023
0.896
Third decile
0.988
0.955
1.045
Fourth decile
0.979
0.991
1.002
Fifth decile
0.982
0.979
0.996
Sixth decile
0.999
0.988
1.003
Seventh decile
1.011
1.012
0.999
Eighth decile
1.025
1.032
0.996
Ninth decile
1.010
1.019
1.022
Tenth (highest)
0.996
0.963
1.000
Top 5%
0.989
0.944
0.997
Top 1%
1.002
0.939
0.981
Top 0.1%
1.076
0.932
0.968

200
Table VIII-11. Predictive Ratios by Deciles of Predicted Risk (sorted low to high):
Institutional Continuing Enrollee
2014/2015 Sample 2018/2019 Sample
Deciles
2020 Model 2020 Model 2024 Model
Improvement in
Predictive Risk
Entire sample
1.000
0.951
1.000
-
First (lowest) decile
0.858
0.788
0.824
Second decile
0.959
0.877
0.932
Third decile
0.995
0.928
0.977
Fourth decile
1.000
0.949
1.011
Fifth decile
1.022
0.968
1.029
Sixth decile
1.023
0.976
1.035
Seventh decile
1.026
0.982
1.028
Eighth decile
1.020
0.975
1.028
Ninth decile
1.015
0.970
1.014
Tenth (highest)
0.989
0.952
0.992
Top 5%
0.984
0.939
0.978
Top 1%
0.967
0.900
0.918
Top 0.1%
0.954
0.865
0.859
_
NOTES:
1. “Improvement in Predictive Risk” compares the distance the predictive ratios are from 1.0 for the 2024 model and
2020 model with a 2018 – 2019 sample.
2. For example, a green arrow indicates that the predictive ratio for any specific decile for the 2024 model is closer to 1.0
than the predictive ratio for the 2020 model with a 2018 – 2019 sample, and vice-versa.
