
Offsetting Policy Feedback Effects:
Evidence from the Affordable Care Act
∗
William Hobbs
†
Daniel J. Hopkins
‡
This Draft: October 11, 2019
∗
The authors gratefully acknowledge research assistance from Tiger Brown, Isaiah Gaines, Matt Garber, Saleel
Huprikar, Louis Lin, Sydney Loh, Sam Mitchell, Owen O’Hare, Kalind Parish, Bhavana Penmetsa, Georgia Ray,
Gabby Rothschild, Samantha Washington, and Elena Zhao as well as helpful comments from Robert Erikson, Josh
Kalla, Luke Keele, Dorothy Kronick, Julie Lynch, Marc Meredith, Andrew Reeves, and seminar participants at the
University of Wisconsin’s American Politics Workshop and the 2019 Summer Meeting of the Society for Political
Methodology (MIT). They also express sincere thanks to the Kaiser Family Foundation (especially Mollyann Brodie,
Bianca DeJulio, Liz Hamel, Ashley Kirzinger, Cailey Munana, Elise Sugarman, and Bryan Wu) and the Leonard
Davis Institute of Health Economics at the University of Pennsylvania (especially Daniel Polsky, Yuehan Zhang, and
Jane Zhu) for sharing data and expertise. The panel data reported herein were collected thanks to financial support
from the Annenberg Public Policy Center, the Institute for the Study of Citizens and Politics, the University of
Pennsylvania School of Arts and Sciences and University Research Foundation, and the Russell Sage Foundation
(Awards 94-17-01 and 94-18-07 to Hopkins and Hobbs and 87-11-01 to Seth Goldman and Diana Mutz).
†
Assistant Professor, Department of Human Development and Department of Government, Martha Van Rens-
‡
Professor, Department of Political Science, University of Pennsylvania, 133 S. 36th Street, Philadelphia PA,
Electronic copy available at: https://ssrn.com/abstract=3366994
Abstract
Can politicized, market-based policies generate policy feedbacks? The Affordable Care
Act (ACA) is complex, relying partly on new exchanges, subsidies, and penalties to increase
health insurance enrollment. Yet prior research focuses on changes to Medicaid, a pre-existing
program. We employ several data sets—including a rolling cross-sectional survey (n=117,000)
and a novel, population-based panel—to assess the impacts of the exchanges and individual
mandate on public opinion. Descriptive analyses demonstrate that exchange users are more
supportive of the ACA. However, subsequent analyses using various inferential strategies
indicate that the exchanges’ overall causal effects were limited. These limited feedback effects
are due to heterogeneity, not invisibility: exchange users connected positive experiences with
ACA opinions, but these were offset by price spikes and concentrated, negative attitude
changes among the uninsured.
0
Electronic copy available at: https://ssrn.com/abstract=3366994
Political scientists have long documented the varied ways public policies can reconfigure the
political landscape at the elite and mass levels (Patashnik, 2008; Campbell, 2012). While policies
that are directly implemented by governments commonly generate feedback effects on public opin-
ion (Soss, 1999; Campbell, 2003; Mettler, 2005; Lerman and Weaver, 2014; Nall, 2018), policies
that rely on indirect mechanisms such as private markets or the tax code often do not (Howard,
1999; Mettler, 2011; Morgan and Campbell, 2011; Galvin and Thurston, 2017; Mettler, 2018). In
part, that is because policies which are provided through private actors or the tax code are often
lower in visibility and less easily politicizied (Howard, 1999; Mettler, 2011). These claims are
bolstered by a separate body of research concluding that self-interest typically has limited effects
on public opinion (Citrin and Green, 1990).
Would market-based policies produce feedback effects on mass opinion if they were more
salient? Or would indirect provision remain too difficult to attribute to government-provided
benefits, especially within a highly politicized and polarized context?
We consider these questions within the context of the 2010 Affordable Care Act (ACA). The
ACA was widely considered the most important American social policy reform in decades. Its pri-
mary goal was to expand access to health insurance, as nearly 50 million people lacked insurance
upon enactment (Kaiser Health News, 2012). Unlike certain existing programs such as traditional
Medicare, key elements of the ACA were designed to act principally through market-based mech-
anisms. Its centerpiece was the creation of exchanges on which Americans could purchase private
health insurance. Initially, 75% of the total gains in health insurance enrollment were expected
to come from the exchanges (Congressional Budget Office, 2010). The exchanges were potentially
pivotal not only in expanding access to insurance but also in broadening the ACA’s political sup-
port. The exchanges were designed to serve a large and middle-class constituency, which when
combined with the Medicaid expansion offered the possibility of fostering a cross-class coalition in
support of the law.
The ACA is similar to previously studied market-based policies in that it relies on incremental
policy levers, many of which are individually low-salience measures affecting small and distinct
sub-populations (Patashnik and Oberlander, 2018). Yet, unlike other market-based policies, the
ACA was an extraordinarily salient and politicized initiative that has been at the forefront of
political debates since it was drafted (Hopkins, 2018). The ACA also had profound impacts
1
Electronic copy available at: https://ssrn.com/abstract=3366994

on many Americans that were unlikely to go unnoticed: comprehensive health insurance is a
substantial benefit that significantly improves individuals’ financial security, health care access,
and recipients’ mental health (Finkelstein et al., 2012; Sommers, Gawande and Baicker, 2017).
The law employed sticks as well as carrots, as it entailed substantial new taxes and regulation
(Jacobs and Mettler, 2018) that might be viewed favorably or unfavorably depending on personal
circumstances. It thus has the potential to generate negative policy feedbacks as well, especially
if the offerings on the exchanges were unsatisfactory or disappointing. Whether positively or
negatively, this combination of political visibility and real-world impact may make the ACA’s
exchanges more influential than other market-based policies. Yet to date, research on the ACA’s
impacts has focused primarily on its Medicaid expansion (Clinton and Sances, 2017; Haselswerdt,
2017; Hopkins and Parish, 2019) or its overall impacts (McCabe, 2015; Jacobs and Mettler, 2016,
2018) while research isolating the exchanges’ impacts has been quite limited (but see Hosek, 2016).
1
The paper’s next two sections develop these hypotheses, first briefly sketching how the ex-
changes operate and then using prior research to explain our hypotheses. It subsequently turns to
three sections which evaluate these conflicting predictions empirically. Our tests exploit various
population-based data sets to estimate the impact of the exchanges’ implementation on the ACA
attitudes of those most likely to use them. Specifically, we focus on those who purchase their own
insurance (whether via the exchanges or not) or who lack insurance.
Our initial results are descriptive and set the stage for subsequent causal inferences. Those who
purchase their own insurance became more favorable at precisely the moment when the exchanges
opened. At approximately the same time, those without insurance became less favorable toward
the ACA. To account for the heterogeneity of experiences on the exchanges, we also provide
descriptive results from separate KFF surveys of the non-group insured and Kentucky residents
in the SI.
2
Those using the exchanges who received subsidies felt more positively toward the law.
Do the cross-sectional differences reflect causal effects, or are they instead the products of se-
1
Existing research has also considered exchange enrollment as a dependent variable, demon-
strating that Republicans are less likely to use the exchanges (Lerman, Sadin and Trachtman,
2017; Sances and Clinton, 2019).
2
Kentucky saw the largest initial gains in insurance post-ACA (Hopkins and Parish, 2019),
making it a valuable state to analyze.
2
Electronic copy available at: https://ssrn.com/abstract=3366994
lection into different types of insurance? Building on the call in Campbell (2012) to conduct more
policy feedbacks research focusing on causal inference, one central contribution of this manuscript
is to provide estimates of the exchanges that are credibly causal effects and not subject to alterna-
tive explanations based on selection bias. Rather than relying on a single, decisive test, we assess
the impact of the exchanges through several analyses.
In one, we make use of over-time variation. Evidence from a novel, population-based panel
uncovers no evidence that exchange users overall became disproportionately more positive toward
the ACA after implementation. However, the panel evidence illustrates that those who become
uninsured also become dramatically less supportive of the ACA.
Next, to account for selection into purchasing on the exchanges, we consider whether those
demographically most likely to use the exchanges became more favorable toward the ACA after
implementation. They do not. And we further find that those most likely to be uninsured were
significantly less favorable toward the ACA—and even less likely to identify as Democrats—after
its implementation.
Among its regulations, the ACA limited the premiums that insurers could charge older respon-
dents, making those in their early 60s a most-likely case for positive feedback effects. A regression
discontinuity analysis demonstrates positive changes in attitudes among those with newly capped
premiums. The ACA helped close the previously observed gap between 64-year-olds (who typi-
cally rely on private insurance) and 65-year-olds (who often use Medicare) (Lerman and McCabe,
2017). Finally, using administrative data on exchange pricing and geo-coded HTS respondents,
we find that citizens who purchase insurance via the exchanges become more negative when prices
on their local exchanges spike.
Overall, these results suggest that Americans shifted their attitudes and even partisanship
in response to perceived benefits or costs from the ACA. Feedback effects, however, partially
cancelled out in aggregate, due to concentrated perceived costs and backlash among those likely
to go without insurance. It’s not that the ACA’s market-oriented features were politically invisible.
Instead, their effects were heterogeneous, varying across places and people.
3
Electronic copy available at: https://ssrn.com/abstract=3366994
Background on the ACA’s Exchanges
Some social policies can be summarized succinctly—the ACA cannot be. It is thus valuable to
provide background on the ACA’s design and goals. Doing so enables us to develop targeted
hypotheses about its potential feedback effects, contextualize and justify potential estimation
strategies, and underscore the law’s complexity.
The pre-ACA system of health insurance provision was already a patchwork of public and
private insurance, with private insurance typically tax-subsidized and provided primarily through
employers (Hacker, 2002). While there was a separate insurance market for individuals, insurers
could reject applicants with pre-existing conditions, and the individual market was at once small
and highly variable in the products available (Jones, 2017). On the public side, Medicare was
a federal program that insured a majority of those over 64, while Medicaid was a means-tested
federal-state partnership targeting households with children and varying markedly across states
(Michener, 2018).
Rather than develop or expand a single program, the ACA sought to fill in gaps in the existing
system. The law’s centerpiece was arguably the establishment of exchanges on which individuals
could purchase private insurance. Insurers were only allowed to charge older customers three times
as much as younger customers, and they could no longer deny coverage due to health histories.
Initial projections indicated that by 2019, 24 million Americans would be insured through the
exchanges and 16 million through the Medicaid expansion (Congressional Budget Office, 2010).
As enacted, the law also expanded Medicaid to 138% of the federal poverty line and allowed adults
to participate irrespective of family status. Separate elements ended lifetime caps on insurance
company payments, defined essential health benefits plans must include, and enabled children to
remain on their parents’ insurance until 26.
The exchanges themselves were comprised of various policy levers. As enacted, the exchanges
were bolstered by a new tax penalty or “individual mandate” for Americans who didn’t have
qualifying health insurance, a mandate intended to limit adverse selection. In 2016, 5 million tax
returns made such payments, with a mean payment of $727 (Internal Revenue Service, 2019). The
federal exchanges also had a notoriously rocky roll-out. The healthcare.gov website was plagued
by long waiting times and other technical difficulties during its fall 2013 opening.
4
Electronic copy available at: https://ssrn.com/abstract=3366994

By contrast, for Americans making below 400% of the poverty line, the federal government
provided subsidies in the form of the Advanced Premium Tax Credit (APTC). In 2016, 6.1 million
American households received this credit, with a mean subsidy of approximately $4,000 (Internal
Revenue Service, 2019).
3
Prior Research and Hypotheses
Research on policy feedbacks is well established (Campbell, 2012). The developed state of prior
research enables us to begin by stating hypotheses on the ACA’s exchanges specifically.
One study which considers whether market-based policy levers can produce mass-level feedback
effects is Morgan and Campbell’s 2011 analysis of the 2003 Medicare Modernization Act (MMA).
Like the ACA, the MMA was a health policy reform that relied substantially on market-based
mechanisms, though the MMA sought to add a prescription drug benefit to Medicare. Partly using
panel data, Morgan and Campbell show that the MMA’s impacts on public opinion were limited:
its implementation did not lead beneficiaries to support more market-based policies generally, nor
did it improve perceptions of Republicans’ handling of health policy.
Is the imprint of the ACA’s exchanges on public opinion likely to differ from the MMA’s?
Although the ACA’s exchanges rely on private insurers to deliver a government-defined benefit,
the ACA diverges from the MMA in its political profile and benefits provided. The law overall was
the subject of sustained, highly salient political battles that lasted for years after implementation,
a fact which may heighten its salience (see also Gollust et al., 2014; Fowler et al., 2017; Hopkins,
2018). And prior research provides extensive evidence that acquiring health insurance can shape
ACA attitudes, whether through Medicare (Lerman and McCabe, 2017), the ACA overall (Mc-
Cabe, 2015; Jacobs and Mettler, 2016, 2018), or the Medicaid expansion (Hopkins and Parish,
2019).
3
Notably, those with access to qualifying health insurance through employers were ineligible
for subsidies on the exchanges. Separately, people whose incomes prove higher than expected are
required to repay the excess subsidy.
5
Electronic copy available at: https://ssrn.com/abstract=3366994
Potential Limits on the Exchanges’ Feedback Effects
Despite the ACA’s sometimes sizable benefits, there are several reasons the exchanges might
generate muted or even negative feedbacks. We consider three such hypotheses.
First, even if the exchanges benefited the vast majority of users, those benefits might not be
attributed to the ACA. The government’s role in facilitating the provision of insurance is not a
salient feature of the exchanges’ design. The exchanges are simply a marketplace: once customers
are enrolled, their primary interactions are not with government but a private insurer.
Other aspects of the exchanges’ operation are even more opaque, further reducing citizens’ ca-
pacity to trace elements of their insurance back to government action (see also Kogan and Wood
2018; on other policies, see Mettler 2011; Morgan and Campbell 2011; Campbell 2012). For exam-
ple, citizens may not be aware of the ways that government regulations structure the marketplaces,
especially by preventing discrimination based on pre-existing conditions. By contrast, the ACA’s
design might have inadvertently heightened the salience and traceability of one of the law’s least
popular elements, its individual mandate (see also Jacobs and Mettler, 2018). While citizens may
be very aware of the personal costs from the individual mandate, they may not recognize that
the mandate was intended to prevent adverse selection on the exchanges and so keep prices down
while protecting people with pre-existing conditions.
Second, the exchanges provide much more substantial benefits to some than others. The
experiences of those who use the exchanges are likely to differ dramatically depending on their
health care utilization, their eligibility for subsidies, the quality of their state’s exchange, the
options available in their market, and other factors (Chattopadhyay, 2018). A person forced to
buy comprehensive coverage or, conversely, who pays a lot for insurance that leaves her exposed
to significant costs may sour on the ACA; someone with a serious pre-existing condition who
can get heavily subsidized insurance may feel quite differently. Prices on the exchanges also vary
dramatically across the country, meaning that similar people can pay very different premiums
depending on where they live (Kamal et al., 2018). This hypothesis yields an observationally
distinctive prediction from that above, as it leads us to expect that exchange users with different
experiences will differ in their ACA attitudes, too. The exchanges’ impacts will not be null but
heterogeneous.
Third, even if the people on the exchanges both benefited from the exchanges and attributed
6
Electronic copy available at: https://ssrn.com/abstract=3366994
the benefits to the ACA, the population of Americans using the exchanges was relatively small.
As the percentage of an overall population which uses a given policy declines, that policy becomes
“distant” to a large fraction of the electorate, meaning that relatively few people have direct
experience with it (Soss and Schram, 2007). That, in turn, makes citizens more reliant on media
portrayals and partisan cues in generating attitudes (Jacobs and Mettler, 2018).
Moreover, the ACA’s exchanges were one element in a complex package of reforms. Campbell
(2003), Soss and Schram (2007), and Campbell (2012) note that policy feedbacks are more likely
when the policy’s beneficiaries are concentrated in ways which encourage them to identify as a
coherent group and act on their shared interests. But the ACA’s complex, multi-faceted design
means that key beneficiaries have a stake only in specific, often disparate provisions (see also
B´eland, Rocco and Waddan, 2018; Chattopadhyay, 2018). This complexity may fragment the
beneficiary population, reducing its capacity to generate a cohesive identity.
Research Design and Data Sets
Prior research leads us to expect substantial selection bias, as those who anticipate higher health
care bills or are not Republican are more likely to enroll via the exchanges (Lerman, Sadin and
Trachtman, 2017). As a result, any straightforward comparison of people who did or did not use
the exchanges is almost certainly biased.
How, then, to evaluate the exchanges’ impact? Descriptive analyses serve as a useful start-
ing point, since we should expect causal effects to generate associations at a minimum. Cross-
sectionally, it is valuable to know whether those who use the exchanges or receive subsidies think
differently about the ACA than those without insurance or with insurance from elsewhere. Know-
ing which groups of Americans are more likely to use the exchanges also helps identify promising
discontinuities or other strategies for causal inference. In addition, our descriptive analyses allow us
to consider temporal variation: did attitudes toward the ACA among different sub-groups shift at
the time of its implementation? In places, we are able to use panel data to track within-respondent
changes before and after the ACA’s implementation.
Armed with a knowledge of various statistical associations, we then proceed to estimates that
are credibly causally identified. Instead of providing a single, decisive test, we employ multiple
tests with different samples, estimands, outcomes, strengths, and weaknesses. Below, we discuss
7
Electronic copy available at: https://ssrn.com/abstract=3366994

each test in detail; here, we motivate the tests collectively. To help readers keep track of the
various tests, both descriptive and causal, Table 1 lists them.
Question Data: Variables and Subgroups
1. Cross-sectional association
Is there an association between ACA
favorability, purchasing health insurance on
exchanges?
Favorability ratings among:
1) HTS respondents
2) KFF non-group respondents
3) KFF Kentucky respondents
2. Temporal correspondence
Did attitudes change with ACA’s implementa-
tion?
ACA favorability in HTS
Panel-based estimates from [name redacted]
Was change in insurance status in the
post-implementation period related to ACA
favorability?
Association between ACA favorability, insur-
ance source in panel data from [name redacted]
3. Dose-dependence
Is association between ACA
favorability, exchange use related
to level of personal benefit?
Associations between favorability ratings and
subsidies: KFF non-group, KFF Kentucky
4. Within-group change (causal tests)
Was likely benefit from the exchanges related
to ACA favorability?
Association between ACA favorability, insur-
ance source scores over time among HTS respon-
dents under 65
Did ACA’s implementation reduce ACA favora-
bility gap at age 65?
Regression discontinuity using older HTS re-
spondents before, after Jan. 2014
5. Partisan integration
Were those using exchanges favorable toward
the ACA before its implementation?
HTS
Was likely benefit from the exchanges related to
party ID?
Causal tests from above with party ID as out-
come
6. Heterogeneity in exchange effects
Did price changes on local exchanges influence
ACA favorability?
HTS merged with exchange pricing, plan data
Table 1: Research questions, tests, and data sources.
8
Electronic copy available at: https://ssrn.com/abstract=3366994

Data Sources
For these tests, we use a range of available data. One primary source is the KFF’s HTS, a rolling
cross-sectional telephone survey of adults’ attitudes about the ACA and health policy. This
survey has been conducted in most months between 2009 and the present; here, we report results
for 117,234 respondents surveyed between February 2009 and September 2017. On account of its
extraordinary sample size, these surveys provide a unique opportunity to observe the evolution of
Americans’ ACA attitudes, as well as the possibly differing trajectories of key sub-groups.
Our descriptive analyses supplement the HTS with separate KFF surveys of the non-group
insured in 2014, 2015, and 2016 as well as a 2015 survey of Kentucky residents, all of which are
presented in the Supplemental Information (SI). For our causal estimates, we return to the HTS
when using the difference-in-difference estimation strategy based on insurance source scores as
well as that employing a regression discontinuity design for those near the Medicare age threshold.
We also merge a geo-coded version of the HTS with administrative data on exchange pricing to
estimate the effects of local price changes on ACA favorability.
4
Last, we draw on the [name redacted] panel survey administered via Knowledge Networks/GfK.
This panel is unique, as it tracks a nationally representative, probability-based sample which was
recruited through address-based sampling and random-digit dialing over ten years. Specifically,
the panel has 13 separate waves: 5 waves in 2007-2008, 2 waves in 2012 (which included the first
questions about the ACA specifically), 2 waves in 2014, 3 waves in 2016, and 1 wave in 2018.
Table 1 summarizes the data sets employed for each test. See the SI for details.
Descriptive Statistics on ACA Exchanges & Attitudes
To understand the exchanges’ impacts on public opinion, we first need to identify who actually
uses them. In a given year, only a small fraction of American adults enroll through the exchanges,
and those who do have distinctive demographic profiles. Through these descriptive analyses, this
section lays the groundwork for subsequent analyses, as we will be better positioned to identify
confounding variables and promising strategies for causal estimation. In later analyses, we will
4
Specifically, we obtained the administrative data on plan pricing and offerings by geography
for 2014-2017 via the Robert Wood Johnson Foundation’s National Narrow Network Project.
9
Electronic copy available at: https://ssrn.com/abstract=3366994
examine attitudes among people who purchased on the exchanges, as well as the much broader
set of people with demographics similar to those who purchased on the exchanges, compared to
individuals with other insurance sources and their demographically similar cohorts.
Demographic Differences by Insurance Type
SI Figure A1 uses the HTS to illustrate the distribution of types of health insurance before and
after the ACA’s primary provisions came into effect. It shows the decline in the uninsured rate
from 14.4% before January 2014 to 9.7% after. It also shows the uptick in Medicaid receipt that
followed the expansion of Medicaid in some states, from 3.7% to 6.6%.
But overall, these changes are marginal: the basic contours of health care provision in the
U.S. remain much as they were before the ACA. What’s more, the share of U.S. adults who
reported using the exchanges is on average only 2% of the surveyed population after their creation.
Categories of insurance that were less overtly affected by the ACA—employer-provided insurance
and Medicare—remain far and away the largest sources of insurance. These patterns alone place
important limits on the ACA’s direct policy feedback effects: people in the parts of the insurance
market most influenced by the ACA represent a small minority of citizens.
How does the small share of Americans who purchase insurance via the exchanges compare to
other groups? SI Table A1 summarizes the means of several key variables by source of insurance for
post-January 2014 respondents. Consistent with Lerman, Sadin and Trachtman (2017) and Sances
and Clinton (2019), those who bought insurance through the exchanges were more Democratic
than the population overall. Medicaid recipients and those who used the exchanges had similar
partisanship, even though those using the exchanges had higher incomes and were more likely to
be White. This indicates that any causal analyses will have to be wary about selection biases,
especially given the general stability of partisan identification. Jointly, the table and figure also
show that exchange enrollees had lower incomes and were younger than the population overall.
Trends in ACA Attitudes by Insurance Type
Having provided descriptive statistics for our key independent variables, we now do the same for
our dependent variable. Descriptively, is there evidence that ACA favorability differs depending
on Americans’ sources of health insurance?
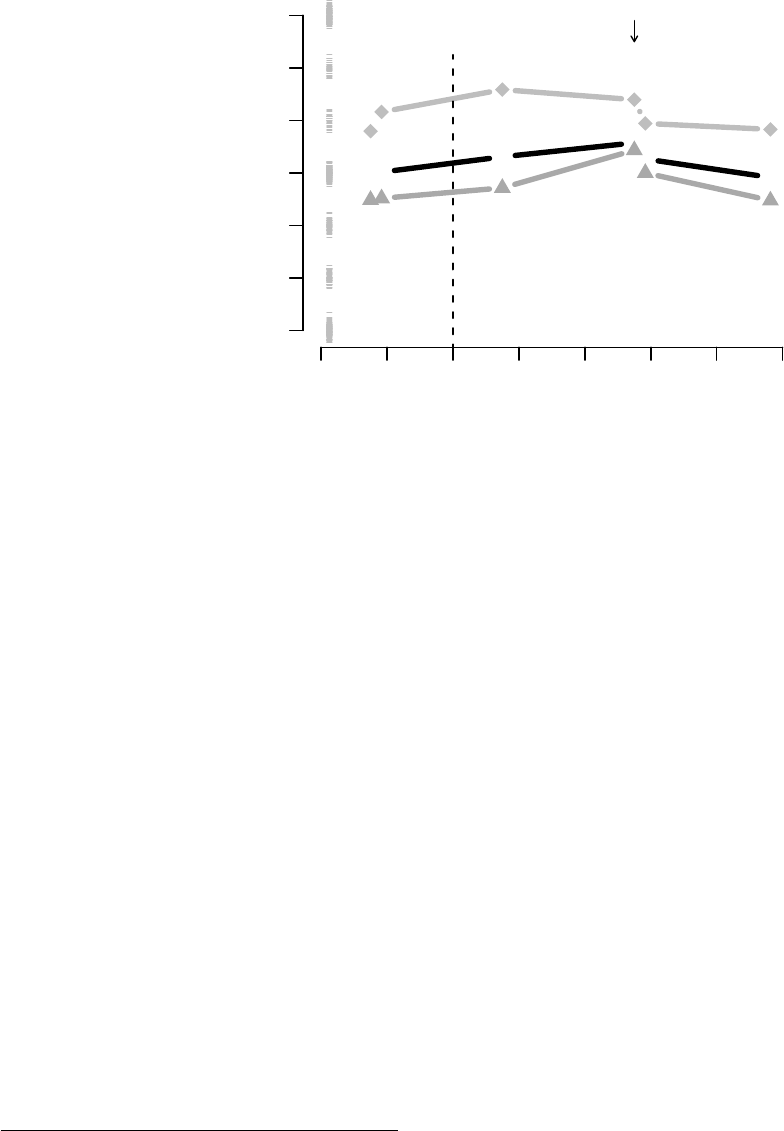
Figure 1 summarizes the trends in a dichotomized measure of ACA favorability by insurance
10
Electronic copy available at: https://ssrn.com/abstract=3366994

Year
Percent Favorable on ACA
Employer−
Provided
10 12 14 16 18
25
50
75
Medicaid
Medicare
Exchanges Open
Year
25
50
75
10 12 14 16 18
Uninsured
Purchased
Used
Exchanges
Exchanges Open
Figure 1: Dichotomized ACA favorability by health insurance status and source over time. The
survey question for “used exchanges” was introduced in 2014, and it is a subset of “self-purchased”.
It measures whether an individual purchased insurance through the exchanges.
type. The left side illustrates that respondents insured through Medicaid are always more favor-
able toward the ACA than those insured through Medicare or employers, with 61% of Medicaid
recipients reporting favorable attitudes versus 47% for those with employer-provided insurance
and 45% for those on Medicare. The over-time patterns for these groups are roughly similar, with
growing favorability between 2016 and 2018, although the smallest group (Medicaid recipients) is
understandably more variable.
On the right, we see the trends for the insurance categories for whom the ACA’s exchanges
and mandate are especially impactful: those who lack insurance, buy insurance themselves, and
buy insurance via the exchanges. In the period before ACA implementation, those without in-
surance are consistently more favorable toward the ACA than those purchasing insurance on
the individual market. The average ACA favorability for those without insurance is 52% in the
pre-implementation period, as compared to 41% who are self-insured.
But the groups switch places almost immediately after implementation. Favorability among
the uninsured drops sharply in the run-up to implementation and averages just 42% in post-
implementation surveys. By contrast, favorability among those on the individual market rises,
and averages 47% after implementation (see also McCabe, 2015). Such changes could reflect
people’s experiences, as those without insurance faced a newly implemented tax penalty while
those needing to self-insure instead enjoyed a range of new options and protections, alongside
11
Electronic copy available at: https://ssrn.com/abstract=3366994
subsidies in some cases. These sudden attitudinal changes thus provide a valuable motivation for
subsequent analyses. However, such changes might also reflect selection effects.
Finally, we show in the right panel that those who purchased on the exchanges felt partic-
ularly favorably toward the ACA. Like Medicaid recipients, this group is small and so favora-
bility over time is noisy. In the SI, we use a regression model of respondents’ attitudes pre-
implementation to show that exchange users are markedly more favorable—and the uninsured
markedly less favorable—than we would expect based on demographics alone.
Attitudes among the Non-Group Insured
Within the broad categories of insurance status identified above, there are sure to be substantial
variations in people’s experiences. After all, enrollees’ experiences with government-funded pro-
grams like Medicaid can vary substantially (Michener, 2018; Tallevi, 2018), and the variation in
experiences with private insurance is potentially wider still. As a next step, in SI section A.2.1 and
in SI Table A3, we consider the predictors of ACA support among those who were insured through
the non-group insurance market post-implementation. The core descriptive result of those analyses
is that while exchange users generally are no more favorable toward the ACA than others without
group-based insurance like Medicare or employer-provided insurance, those who received subsidies
are a bit more favorable toward the ACA, especially in its first year of full implementation.
Panel-Based Estimates of Trends in ACA Attitudes by Insurance
Figure 1 shows that around the time of the ACA’s implementation, the relationship between peo-
ple’s insurance status and their ACA attitudes shifted: people who purchased their own insurance
became more favorable while the uninsured became less so. But it is quite possible that individuals
who already felt favorably toward the ACA shifted from one insurance source to another.
Panel data provides one way to avoid this challenge, as the same individuals report their
attitudes in multiple waves conducted over time. Here, we draw on the 2012-2018 [name redacted]
panel to evaluate Americans’ attitudes toward the ACA over time.
To be sure, there simply aren’t many respondents who fall into the self-purchased or uninsured
categories. Of the 589 panelists who completed both the November/December 2016 wave and the
October 2018 wave, 38—or 6%—reported in January 2016 that they purchased their insurance
12
Electronic copy available at: https://ssrn.com/abstract=3366994

themselves, and not all used the exchanges. Another 35 panelists—also 6%—reported being
uninsured at that time, an estimate that is lower than the 2016 national benchmark of 11%
(Witters, 2019). But the panel nonetheless provides a critical advantage, as it allows us to observe
how those respondents’ attitudes shifted relative to the population overall. We also get increased
statistical precision from making comparisons within individuals. In these analyses, our outcome
comes from a question the panel has asked since 2012: “Some people think the health care reform
law should be kept as it is. Others want to repeal the entire health care law. Still others are
somewhere in between.” Respondents could reply on a 1-7 scale, with 1 indicating the “health
care reform law should be kept as it is” and 7 indicating that “entire health care law should be
repealed.”
As Figure 2 illustrates, the groups defined by insurance status in 2016 differ at baseline but
largely move in parallel. In particular, there is no evidence that those who purchased insurance
themselves differ markedly in the trajectory of their ACA attitudes compared to other insured
groups, though there is a significant uptick in support for repealing the ACA just after the 2012
election among those without insurance in 2016. Overall, there is little evidence that respondents
who purchased their own insurance in 2016 had a distinctive trajectory. Note, however, that for
those without insurance, there is somewhat less evidence of an improvement in ACA attitudes
between 2016 and 2018.
5
We next estimate OLS models which more fully leverage the panel data set by analyzing
shifts in insurance status as a predictor of shifts in ACA attitudes. This approach tests whether
changes in insurance status are associated with changes in ACA attitudes generally in the post-
implementation era, rather than focusing on changes immediately after implementation.
Specifically, we model 2018 respondents’ views of the ACA as a function of their fall 2018
insurance status, their January 2016 insurance status, attitudes toward the ACA in 2012 and
2016, 2012 partisan identification, and a series of basic demographics such as gender, education
and income. Such models are well suited to isolate the extent to which changes in insurance
status predict subsequent shifts in ACA attitudes. However, they are a conservative test, as we
are isolating people who became uninsured only after 2016, nearly three years after the ACA’s
5
Specifically, those without insurance in January 2016 shifted toward the ACA by 0.30 while
for those with insurance the pro-ACA shift was 0.53.
13
Electronic copy available at: https://ssrn.com/abstract=3366994
●
●
●
●
●
●
Date
ACA Attitudes
Keep ACA 3 4 5 Repeal ACA
2012 2014 2016 2018
Not Covered
All
Self−Purchased
Exchanges
Open
Based on 2016
insurance sources
Figure 2: This figure reports estimates for respondents to the 2012-2018 [name redacted] panel
who completed the November/December 2016 and October 2018 waves conducted through GfK’s
Knowledge Panel. N=589. Insurance status is as of January 2016. The gray horizontal lines at
left report the distribution of the outcome variable for the October 2012 survey.
implementation. As a result, those who were uninsured in the first few years after the ACA’s 2014
implementation will not influence our estimate.
The core results are presented graphically in Figure 3, while SI Table A8 provides the full,
fitted model. Most of the indicators of different insurance statuses are not predictive of 2018
ACA attitudes. Importantly, those who purchased insurance plans themselves in 2018 are not
much more or less supportive of the ACA. However, respondents who were uninsured in 2018
are dramatically less supportive of the ACA, even accounting for 2016 insurance status. The
coefficient is 1.23 (SE=0.43), meaning that those who became uninsured between 2016 and 2018
also downgraded their opinion of the ACA by a whopping 1.23 on a 1-7 scale. That effect is
61% of a standard deviation. It is strongly suggestive of a causal relationship between becoming
uninsured and thinking more negatively toward the ACA.
6
6
As Table A9 illustrates, we reach very similar conclusions with an alternative model specifi-
cation that examines the change in attitudes among those uninsured in January 2016, indicating
14
Electronic copy available at: https://ssrn.com/abstract=3366994

−2 −1 0 1 2
Coefficient on ACA REPEAL Attitudes
●
Uninsured
2016
Uninsured
2018
Figure 3: This figure reports coefficients for being uninsured in 2016 and 2018 (included in the
same model) when predicting 2018 support for ACA repeal using the [name redacted] panel.
Causal Estimates
The following analyses are designed to remove the effects of selection from our estimates to identify
the causal effects of changes in insurance status.
Over-time Changes by Predicted Insurance Source
One common research design for assessing a policy introduced at a specific moment in time is
difference-in-difference estimation. Such estimators isolate whether there were disproportionate
changes in a treated group after the treatment’s administration. Yet when analyzing the HTS,
which was administered as a rolling cross section, we are barred from employing classical difference-
in-difference estimation because there is no fixed control group. There were no federal exchanges
or people using them prior to the ACA’s implementation. What’s more, the exchanges are likely
that this result is robust to alternative specifications.
15
Electronic copy available at: https://ssrn.com/abstract=3366994
to have had system-wide effects, as they may have influenced the insurance status and experiences
of people who were previously uninsured as well as those who previously purchased insurance for
themselves and others. Most importantly, we should avoid using actual insurance status (as we did
in Figure 1) because the people who chose to use the exchanges may have already felt favorably
toward the law.
We attempt to overcome selection concerns by using predicted insurance scores coupled with
temporal variation to estimate the causal impact of using the exchanges (and later of being unin-
sured). In essence, we model who in the data set is more or less likely to use the exchanges
(rather than who chose to), construct synthetic cohorts of likely users, and then evaluate whether
over-time shifts in ACA attitudes were more pronounced among those whom the model flags as
especially likely to be exchange users. In doing so, we are guided by prior work on causal infer-
ence including Athey and Imbens (2006), Heckman and Vytlacil (2007), and Frangakis and Rubin
(2002).
Note that this analysis relies on the timing of implementation, and mimics a difference in
difference design – one where we consider changes in attitudes among those with demographics
similar to those with given insurance sources. In the language of an encouragement design, we
assign intention-to-treat status for all individuals in time periods after 2013 and a probability
of complying – taking up the treatment – based on their demographics, whether or not they
actually purchase a given insurance source. Like in difference-in-difference analyses, we look
for parallel trends (or, more precisely, parallel slopes for likely vs unlikely to purchase) before
the implementation and examine relative changes in attitudes after implementation. Those with
predicted insurance scores close to zero we expect to never take advantage of the exchanges,
and those with lower scores will be more likely to do so. We do not construct matched cohorts
that have very similar attitudes before implementation. We also do not predict insurance source
using variables that could plausibly be changed by the introduction of the exchanges, including
partisanship (we will show changes in partisanship later in the paper).
As an initial step, we isolate respondents who were at all likely to use the exchanges or be
affected by the individual mandate. In practice, this means excluding respondents over 64 (who
are likely on Medicare) or with incomes under $40,000 per year (who are more likely to be on
16
Electronic copy available at: https://ssrn.com/abstract=3366994

Medicaid, for which there is a competing effect).
78
Next, we estimate three separate insurance source scores to identify the types of respondents
who are especially likely to 1) use the exchanges, 2) purchase their own insurance, or 3) be unin-
sured in the post-2014 period. Estimating the probability of self-purchasing allows us to consider
the effects of changing conditions among self-purchasers on ACA attitudes without requiring that
survey respondents link their insurance to government-operated markets. The uninsured score
analysis is important because it considers the possibility of negative feedback effects from the
individual mandate or other sources.
9
These insurance source scores provide one-number summaries of respondents’ probabilities of
falling into specific ACA-related categories given their demographic characteristics.
Health insurance was not available via the exchanges until January 2014, so we use logistic re-
gression to model the predictors of enrolling via the exchanges in that period alone.
1011
Americans’
experiences with the exchanges varied substantially across states (B´eland, Rocco and Waddan,
2016; Jones, 2017), so the insurance source score model includes indicators for respondents’ state of
residence alongside 5 polynomials of respondents’ age in years, indicators for years of educational
attainment, and identification as Asian American, Black, Hispanic, female, or retired. Subsidies
and exchange usage are closely connected to respondents’ incomes, so the insurance source score
7
The minimum income cutoff to remove likely Medicaid recipients varies by state. For sim-
plicity, we set this cutoff at the Medicaid expansion level for all states. Reducing this cutoff to
include lower-income people in non-expansion states does not meaningfully alter our results.
8
Very few people who previously received Medicare or Medicaid transferred into the individual
market post-ACA. In fact, 53% of all respondents who used the exchanges in 2014 had previously
lacked health insurance, and another 19% had previously purchased a plan themselves. See espe-
cially SI Table A2, which reports the shares of people with non-group insurance by their previous
insurance status.
9
Those with higher uninsured scores might also be those who are especially vulnerable to the
erosion of insurance offerings through their employers.
10
To be coded as using the ACA exchanges, respondents answered that they purchased insurance
“From healthcare.gov or [state marketplace name]”.
11
Using linear regression to produce the insurance source scores does not alter our results.
17
Electronic copy available at: https://ssrn.com/abstract=3366994

model also includes measures of respondents’ income, income squared, and income cubed. From
this model, we can then estimate any respondent’s probability of using the exchanges based on
her background characteristics, regardless of whether the exchanges were actually operating when
she was surveyed.
12
SI Table A11 shows the correlations for the three insurance source scores. As expected, given
that those using the exchanges are a subset of those purchasing their own insurance, the scores
for self-purchasing and using the exchanges are correlated at 0.5. Correlations between using
the exchanges and being uninsured (0.14) and self-purchasing and being uninsured (-0.08) are
substantially smaller. Critically, our second-stage estimates depend on the first-stage predictions—
the better we predict in the first stage, the more effectively we isolate those likely to use the
exchanges. SI Table A12 shows the first stage of each model.
Results from Predicted Insurance Score Analyses
To distinguish ACA experiences from long-term shifts, we examine over time associations be-
tween likely insurance use and ACA favorability. Effects driven by the ACA should be apparent
discontinuously in 2013 (when the exchanges first opened) and 2014.
We include the insurance source scores in OLS models predicting dichotomized ACA favora-
bility in each of the six-month increments between early 2010 (when the ACA was passed) and
late 2017. Accordingly, Figure 4 shows 16 separate correlations between ACA favorability and
respondents’ estimated probability of using the exchanges.
13
If the experience of buying insur-
ance via the exchanges shifted ACA attitudes, the insurance source scores should become stronger
predictors of ACA support after the exchanges opened.
Figure 4 illustrates the correlations for a 10 percentage-point change in probability of using the
exchanges, self-purchasing, or going without insurance for each six-month window of time.
14
On
the right side of each graphic, we report the mean change in the effect for estimates after January
12
Because partisan identification is potentially endogenous, and also because it is strongly as-
sociated with health care attitudes (Kriner and Reeves, 2014), we repeat these analyses with
partisanship as the dependent variable below.
13
The minimum sample size for these six-month periods is 1,739 while the maximum is 6,227.
14
One empirical challenge is that even among those under 65, most people making more than
$40,000 per year have access to employer-provided insurance, so the variation in the estimated
18
Electronic copy available at: https://ssrn.com/abstract=3366994

2014. Neither the scores for using the exchanges nor those for self-purchasing are associated with
meaningful changes in ACA favorability after implementation. On balance, people more likely to
use the exchanges or self-insure don’t show different over-time trends.
However, the scores for being uninsured are associated with markedly more negative ACA
attitudes after implementation. This uninsured score is a catch-all. It identifies both respondents
who actually chose to forego insurance and demographically similar respondents who would have
foregone purchasing on the individual markets had they not had some other source of insurance.
Regardless of the specific mechanisms at work, these results reinforce the claim that the ACA
induced negative experiences for at least some Americans.
●
●
●
●
●
●
●
●
●
●
●
●
●
●
●
●
−0.2 0.0 0.1 0.2
Exchange Score
respondents under 65, income over 40K
ACA Favorability
10 11 12 13 14 15 16 17
Pre−Exchanges Post−Exchanges
−0.03
0.47
●
●
●
●
●
●
●
●
●
●
●
●
●
●
●
●
−0.20 −0.05 0.10
Uninsured vs Self−Purchased Score
respondents under 65, income over 40k
ACA Favorability
10 11 12 13 14 15 16 17
Pre−Exchanges Post−Exchanges
Self−insured
−0.00
●
●
●
●
●
●
●
●
●
●
●
●
●
●
●
●
Uninsured vs Self−Purchased Score
respondents under 65, income over 40k
ACA Favorability
10 11 12 13 14 15 16 17
Pre−Exchanges Post−Exchanges
Uninsured
−0.05***
Figure 4: Over-time associations between insurance source scores, ACA attitudes. These figures
show the effect of increasing the average insurance source score by 10 percentage points.
To formally test the impact of the exchanges’ introduction, we estimate a multi-level model
predicting ACA favorability using the same insurance source scores and timeframe shown in Figure
4, with respondents clustered by the six-month period of their response. We also include an
interaction between the insurance source score and whether the response comes after January 1st,
insurance source scores is relatively small, as illustrated in SI Table A10. Accordingly, we generate
multiple estimates from the second stage over-time models. In some cases, we show the effect of
a 10 percentage point increase in the likelihood of using the exchanges (or of self-purchasing or
going uninsured); in others, we report the effect of a full change from 0 to 1 in the insurance source
score (the typical interpretation of the coefficients), even though this is an extrapolation outside
the range of the observed scores.
19
Electronic copy available at: https://ssrn.com/abstract=3366994

2014, which provides a formal measure of any change in the mapping between the probability of
using the exchanges and ACA favorability. In this test, we use the typical scaling for such models
in which the estimated probability shifts from 0 to 1. The estimates in SI Table A13 otherwise
mirror those presented graphically in Figure 4.
Beyond reporting the same results as in Figure 4, Table A13 provides an additional, if more
peripheral, take-away: the attitudes among those purchasing on the exchanges appeared to be
extremely positive before the ACA’s implementation. This indicates possible ceiling effects that
limit the potential for further increases in favorability.
Expected Insurance Source & Partisanship
We now replicate the insurance source score tests from above using partisan identification as the
outcome. ACA attitudes are strongly associated with partisan identification (e.g. Kriner and
Reeves, 2014), and since partisan identification is strongly resistant to change (Green, Palmquist
and Schickler, 2002), partisanship could limit the extent to which improvements in personal cir-
cumstances can increase favorability toward a politicized policy (Jacobs and Mettler, 2018). At the
same time, any changes in partisan identification induced by the ACA might have far-reaching ef-
fects, since partisan identification can influence a range of political opinions and behaviors (Achen
and Bartels, 2016).
In this, we follow extensive research by considering partisan identification to be causally prior
to ACA attitudes (Green, Palmquist and Schickler, 2002). Democrats are more likely to favor the
ACA and Republicans the reverse. Here, we consider whether changes in exposure to the ACA
and the resulting changes in ACA attitudes correspond with changes in partisanship.
As in some tests above, we use a linear probability model with an indicator for Democratic
identification as the outcome when analyzing the insurance source scores. In select models, we also
show the effect of controlling for ACA favorability on any associations between insurance source
and partisanship. This is an informal mediation analysis. If the standard assumptions hold
15
, the
15
The assumptions underpinning causal mediation analysis are similar to those underpinning
linear regressions, but there are additional assumptions about lack of unmeasured confounding
(or, at minimum, “deconfounding”) along the expanded causal pathway (Pearl, 2013). In our
analysis, for example, a joint effect on ACA favorability and partisanship in the year or so after
20
Electronic copy available at: https://ssrn.com/abstract=3366994

decrease in the size of the partisan identification coefficient after controlling for ACA favorability
roughly corresponds to the size of the mediated effect.
16
In Figure 5, we show that respondents who are more likely to use the exchanges or purchase
insurance do not differ disproportionately in their partisanship after January 2014. However, those
who were more likely to be uninsured shifted disproportionately away from the Democrats and
toward identification as independents. A 10 percentage-point increase in the likelihood of going
without insurance was associated with 3 percentage point decrease (SE=0.7 percentage points) in
the probability of being a Democrat after 2014 compared to before 2014.
17
Not identifying with either major party was also positively associated with the uninsured
scores. Put differently, people whose demographics made them more likely to be uninsured were
also more likely to identify as independents after 2014. At the same time, those predicted to
purchase their own insurance were more likely to identify with a party.
Overall, these results mirror the earlier findings. We find that the people who were relatively
likely to go without insurance shifted away from the Democrats, and those likely to purchase
their own insurance were polarized rather than shifting uniformly toward either party. In other
words, the ACA’s implementation resulted in both positive and negative policy feedback effects,
and these heterogeneous experiences partly cancelled out.
the 2012 election that is not due to the ACA would be such a confounder, and would be especially
concerning if it were concentrated among individuals with high likelihoods of having the insurance
sources considered here. Such a confounder would prove problematic not only for our analyses
but for much of the extant research on the effects of the ACA on political attitudes.
16
If the ACA’s rollout did change partisan identification with the Republicans or Democrats, the
absence of mediation would perhaps be more surprising than the presence of mediation. After all,
such a finding would imply that the ACA had shifted partisanship without influencing attitudes
toward the ACA itself.
17
Note that for the estimates in Figure 5, we are using the full 0 to 1 probability as our inde-
pendent variable. Dividing the y axis by 10 keeps the estimates closer to the observed variability
in our data. For simplicity, the 3 percentage-point decrease above corresponds to a dependent
variable coded 1 for Democrats and 0 otherwise.
21
Electronic copy available at: https://ssrn.com/abstract=3366994

−0.5 0.0 0.5
Insurance Source Scores
Change in Partisanship
2014 on vs. 2013 and earlier
●
●
●
●
●
●
Exchanges Uninsured Self−insured
●
●
DV: Became Democrat
(D=1; I=0.5; R=0)
DV: Became Independent
Control ACA
favorability
Figure 5: Partisanship & Insurance Status Scores. This figure shows estimates for pre- vs. post-
implementation associations between partisanship and the insurance status scores. In each case,
the first estimate is the change in the partisanship-insurance source score association after imple-
mentation while the second reports the same association conditioning on ACA attitudes. Over-
time estimates are shown in the supporting information.
The Discontinuity in Medicare Eligibility
The ACA used various policy levers to modify the availability of health insurance, so we continue
assessing its causal impacts by analyzing its overall impact on older Americans. Specifically, the
ACA provided valuable new opportunities and protections for those in their early 60s: it created
exchanges on which non-elderly adults could purchase insurance—sometimes with subsidies—
while also mandating that insurers not discriminate on the basis of pre-existing conditions. It
also limited premiums for older customers to no more than 3 times those of younger customers.
Some in their early 60s became newly eligible for Medicaid. At the same time, the ACA did not
entail substantial consumer-facing changes to Medicare, the program which insures 68% of adults
65 and older according to the HTS. To the extent that the ACA affected Americans directly, it
was substantially more likely to affect those under 65.
18
18
Policies targeting those 65 and older included free preventative care (for certain services), and
the gradual, partial closing of the “donut hole” in prescription drug coverage between 2010 and
2020.
22
Electronic copy available at: https://ssrn.com/abstract=3366994

We thus assess the ACA’s impacts on those in their early 60s relative to those 65 or slightly
older. There is a precedent for this research design. Studying the period before the ACA’s full im-
plementation, Lerman and McCabe (2017) sought to understand whether Americans’ experiences
with publicly provided insurance through Medicare changed their health policy attitudes.
Our goal is to use regression discontinuity designs to estimate the difference in ACA attitudes
associated with Medicare eligibility both before and after the ACA’s full implementation and
then to compare those estimates. To do so, we turn back to the HTS. We first calculate the
Imbens-Kalyanaraman optimal bandwidth to be 2.42 (Imbens and Kalyanaraman, 2012), so our
initial analyses include respondents ages 62-68. After confirming that key variables do not differ
across the discontinuity
19
we then estimate reduced-form equations in which we regress the four-
category measure of ACA favorability on several variables, including measures picking up time
trends as well as respondents’ age in years; Medicare eligibility via age; levels of education; self-
identification as male, Black, Hispanic, or Asian American; income; and a five-category measure
of partisan identification. In the pre-implementation surveys, we find that being under 65 and
not yet eligible for Medicare produces a coefficient of -0.12 (SE=0.06),
20
meaning that Medicare
eligibility has a nearly significant positive effective on ACA attitudes that averages 10% of the
dependent variable’s standard deviation, consistent with Lerman and McCabe (2017).
A majority of Americans shift their insurance status at 65 with Medicare eligibility, so the key
estimate is not the change at 65 but the extent to which the ACA’s implementation modified that
change. We thus estimate a parallel OLS model for respondents after the ACA’s January 1 2014
implementation, finding that the reduced-form impact of being under 65 became 0.01 (SE=0.06).
Post-implementation, those who are under 65 and so more directly affected by the ACA are no
more supportive than people just slightly older.
For our purposes, the key question is the extent to which the effect declined after the ACA was
implemented, and Figure 6 presents that differenced estimate using dots. Using triangles, Figure
6 shows the comparable estimates via an estimator that does not condition on any variables other
than age. In both cases, the estimated difference is positive, as it varies between 0.13 (SE=0.087)
with controls to 0.183 (SE=0.095) without. Given the four-category dependent variable, the ACA’s
19
See SI Figure A16.
20
See SI Table A15 for the full fitted model.
23
Electronic copy available at: https://ssrn.com/abstract=3366994

●
●
−0.4 −0.2 0.0 0.2
Under 65 favorability
compared to 65 or over
Pre−Implementation Post−Implementation
Effect
Diff.=0.13
SE=0.087
−0.4 −0.2 0.0 0.2
Diff.=0.183
SE=0.095
Figure 6: This figure illustrates the change in ACA attitudes associated with turning 65 and
becoming Medicare eligible for HTS respondents before and after the ACA was implemented. Es-
timates from models conditioning on various potential confounders are shown using dots; estimates
from models without such controls are depicted using triangles.
implementation had a detectable but substantively small overall impact closing the attitudinal gap
between those who were and were not Medicare eligible.
21
Given the ACA’s regulations about age
and insurance pricing, this group is likely to have been more positively affected by the exchanges
than others.
Geographic Variability in Exchange-based Insurance Prices
Do those who use the exchanges largely ignore their personal experience when assessing the ACA,
or they do use personal experience but in different ways depending on their experiences? The
results above show that the ACA’s implementation had heterogeneous effects, suggesting that
limited feedback effects were not due to citizens’ difficulty attributing their experiences to govern-
ment policy. Here, we use price shocks on the ACA exchanges to further differentiate hypotheses
21
This result is of course compatible with a larger effect on the small number of people most
directly affected.
24
Electronic copy available at: https://ssrn.com/abstract=3366994

about the difficulties of political attribution from those emphasizing heterogeneous personal ex-
periences.
Here, we use geographic variation in exchange pricing as leverage to estimate the attitudinal
effects of price changes on local markets. Specifically, customers on the exchanges are divided into
geographic rating areas; in 2017, there were 504 such rating areas across the country. We acquired
data on the insurance options and their prices for rating area and year between 2014 and 2017.
We then developed a crosswalk which enables us to match KFF respondents based on their ZIP
codes and/or counties of residence to their rating area and the corresponding options and prices
available to them.
22
In addition, we also used respondents’ ZIP codes or county of residence to
merge in basic county-level Census demographic information.
Given how few people in the survey use the exchanges—the sample sizes by year for exchange
users are 157, 134, and 151—we fit a multi-level model to borrow strength across the three years
and estimate the effects of price shocks jointly. This multilevel model conditions on the total
number of plans available on each market as well as the mean premium for that year and the
mean change in premiums from the prior year.
23
It also includes random effects for each of
the three years as well as various individual- and county-level covariates. Shown in Table 2,
and in full in the SI, the model suggests that rising average premiums on the ACA exchanges
are associated with sizable declines in ACA favorability for respondents who actually use the
exchanges. The estimated coefficient is −0.19 (SE=0.07), meaning that an increase of one standard
deviation in the mean monthly premium change ($33) is associated with a −0.19 drop on the ACA
favorability scale. That shift is substantively meaningful, as it is a change of -7.6 percentage points
in the dichotomized ACA favorability scale. However, this relationship does not hold for other
respondents or for the uninsured, as the other columns of Table 2 demonstrate. These finding
bolsters the claim that we are detecting the effects of experience with the markets, and not simply
22
Data are missing for 2014 in some rating areas, but overall, we are able to identify the 2014
market conditions for 64% of respondents, 2015 conditions for 91% of respondents, and 2016 and
2017 conditions for 96% of respondents.
23
Note that our interest in the change in premiums from the prior year requires us to exclude
2014.
25
Electronic copy available at: https://ssrn.com/abstract=3366994

ACA favorability
Non-Market Market Uninsured
Number of plans
(logged, in sd’s)
0.00 −0.07 −0.00
(0.01) (0.06) (0.03)
Mean Premium
(in sd’s)
0.00 0.04 0.05
(0.01) (0.07) (0.03)
Mean Change in
Premium (in sd’s)
0.00 −0.19
∗∗
−0.02
(0.01) (0.07) (0.04)
Observations 15,987 442 1,772
Month FEs Y Y Y
County-Level Demographics Y Y Y
Clusters (Year) 3 3 3
∗
p<0.05;
∗∗
p<0.01;
∗∗∗
p<0.001
Table 2: This table presents the results of multi-level models fit to KFF respondents from 2015,
2016, and 2017 in which certain insurance market conditions (and various other independent
variables) predict ACA favorability, measured on a 1 to 4 scale.
spurious county-level associations.
24
Conclusion
Which features of policy designs make feedbacks on public opinion more or less likely? Prior
research on other market-based health policies (Morgan and Campbell, 2011)—and on the more
general class of policies administered through back-door mechanisms including private markets and
the tax code (Howard, 1999; Mettler, 2011, 2018)—indicates that they typically do not produce
strong imprints on public opinion. Such policies can be relatively invisible, making them difficult
to trace back to government action.
Key elements of the ACA were administered via market-based mechanisms, making it possible
that the ACA’s exchanges and its individual mandate might leave a similarly faint imprint on
public opinion. Yet the ACA was also highly salient and contentious, so much so that citizens’
partisan predispositions shaped their willingness to enroll via the exchanges. In this paper, we
24
Our respondents are distributed across many counties—in 2015, for example, the 359 respon-
dents using the markets were in 208 counties. As a consequence, we cannot employ county fixed
effects.
26
Electronic copy available at: https://ssrn.com/abstract=3366994
employed a wide range of data sets and analyses to test these competing influences on possible
policy feedback effects.
Overall, we find that while the net effect of the ACA’s core, market-based features was muted,
the ACA’s exchanges and its individual mandate did influence the opinions of those most likely
to be affected. Specifically, differenced regression discontinuity estimates indicate that the ACA
reduced the gap in ACA favorability between those who are 64 and 65. Yet those in their early
60s were among those who benefited most from the ACA, and separate analyses using predicted
insurance sources indicate that the types of people most likely to be uninsured became less favor-
able toward the ACA around the time of its introduction. A conservative test using panel data
demonstrates that those who became uninsured between 2016 and 2018 also became substantially
less favorable toward the ACA. In addition, local price spikes on the ACA exchanges reduced
support for the law, another indication that Americans were able to link their experiences with
their ACA attitudes. Different groups in different places had quite different experiences with the
ACA’s exchanges and its mandate. One key factor limiting the ACA’s mass-level policy feedbacks
was heterogeneity, not invisibility.
The politics of the ACA abound in puzzles and paradoxes. One such puzzle is especially
relevant here: why were Republican repeal efforts in 2017 more successful when it came to ending
the market-based individual mandate than scaling back the Medicaid expansion? Public opinion
is certainly not the sole answer, or even necessarily the most important one (Hertel-Fernandez,
Skocpol and Lynch, 2016; Jones, 2017; Hacker and Pierson, 2018; Patashnik and Oberlander, 2018).
Still, the results uncovered here do suggest a partial explanation: while the Medicaid expansion
induced heightened support for the ACA (Sances and Clinton, 2019; Hopkins and Parish, 2019),
the overall impacts of the ACA’s exchanges and its individual mandate were ambiguous. Those
findings, in turn, may help explain why some of the ACA’s more conservative, market-based
elements were also among the most politically vulnerable.
27
Electronic copy available at: https://ssrn.com/abstract=3366994
References
Achen, Christopher and Larry Bartels. 2016. Democracy for Realists. Princeton University Press.
Athey, Susan and Guido Imbens. 2006. “Identification and inference in nonlinear difference-in-
differences models.” Econometrica 74(2):431–497.
B´eland, Daniel, Philip Rocco and Alex Waddan. 2016. Obamacare wars. University Press of
Kansas.
B´eland, Daniel, Philip Rocco and Alex Waddan. 2018. “Policy Feedback and the Politics of the
Affordable Care Act.” Policy Studies Journal .
Campbell, Andrea. 2003. How policies make citizens. Princeton University Press.
Campbell, Andrea Louise. 2012. “Policy makes mass politics.” Annual Review of Political Science
15:333–351.
Chattopadhyay, Jacqueline. 2018. “Is the Affordable Care Act Cultivating a Cross-Class Con-
stituency?” Journal of Health Politics, Policy and Law 43(4).
Citrin, Jack and Donald Philip Green. 1990. “The Self-Interest Motive in American Public Opin-
ion.” Research in Micropolitics 3(1):1–28.
Clinton, Joshua D and Michael W Sances. 2017. “The Politics of Policy.” American Political
Science Review pp. 1–19.
Congressional Budget Office. 2010. “Letter to Speaker Nancy Pelosi: Estimated Budgetary
Impact of H.R. 3590.”.
URL: https://www.cbo.gov/sites/default/files/111th-congress-2009-
2010/costestimate/amendreconprop.pdf
Finkelstein, Amy, Sarah Taubman, Bill Wright, Mira Bernstein, Jonathan Gruber, Joseph P
Newhouse, Heidi Allen, Katherine Baicker and Oregon Health Study Group. 2012. “The Oregon
health insurance experiment.” The Quarterly journal of economics 127(3):1057–1106.
28
Electronic copy available at: https://ssrn.com/abstract=3366994
Fowler, Erika Franklin, Laura Baum, Coleen Barry, Jeff Niederdeppe and Sarah Gollust. 2017.
“Media Messages and Perceptions of the Affordable Care Act during the Early Phase of Imple-
mentation.” Journal of Health Politics, Policy and Law 42(1):167–195.
Frangakis, Constantine E. and Donald B. Rubin. 2002. “Principal stratification in causal infer-
ence.” Biometrics 58:21–29.
Galvin, Daniel and Chloe Thurston. 2017. “The Democrats’ Misplaced Faith in Policy Feedback.”
The Forum 15(2):333–343.
Gollust, Sarah E., Colleen L. Barry, Jeff Niederdeppe, Laura Baum and Erika Franklin Fowler.
2014. “First Impressions.” Journal of Health Politics, Policy and Law 39(6):1253–1262.
Green, Donald, Bradley Palmquist and Eric Schickler. 2002. Partisan Hearts and Minds. New
Haven, CT: Yale University Press.
Hacker, Jacob S. 2002. The divided welfare state. Cambridge University Press.
Hacker, Jacob S and Paul Pierson. 2018. “The Dog That Almost Barked.” Journal of Health
Politics, Policy and Law 43(4).
Haselswerdt, Jake. 2017. “Expanding Medicaid, Expanding the Electorate.” Journal of health
politics, policy and law 42(4):667–695.
Heckman, James and Edward Vytlacil. 2007. “Econometric evaluation of social programs, part
II.” Handbook of econometrics 6:4875–5143.
Hertel-Fernandez, Alexander, Theda Skocpol and Daniel Lynch. 2016. “Business associations,
conservative networks, and the ongoing republican war over Medicaid expansion.” Journal of
health politics, policy and law 41(2):239–286.
Hopkins, Daniel. 2018. “The Exaggerated Life of Death Panels?” Political Behavior 40(3):681–709.
Hopkins, Daniel J and Kalind Parish. 2019. “The Medicaid Expansion and Attitudes toward the
Affordable Care Act.” Public Opinion Quarterly .
29
Electronic copy available at: https://ssrn.com/abstract=3366994
Hosek, Adrienne. 2016. “Insuring Obamacare on the Health Insurance Marketplace.”. Manuscript,
University of California Davis.
URL: https: // drive. google. com/ file/ d/ 0BwLuq-FTY_ zebWVGYjhZUDZHOEU/ view
Howard, Christopher. 1999. “American Welfare State, or States?” Political Research Quarterly
52(2):421–42.
Imbens, Guido and Karthik Kalyanaraman. 2012. “Optimal bandwidth choice for the regression
discontinuity estimator.” The Review of economic studies 79(3):933–959.
Internal Revenue Service. 2019. “Tax Statistics: Affordable Care Act Items.”.
URL: https: // www. irs. gov/ statistics/ soi-tax-stats-individual-statistical-tables-by-size-of-adjusted-gross-income
Jacobs, Lawrence and Suzanne Mettler. 2016. “Liking Health Reform But Turned Off By Toxic
Politics.” Health Affairs 35(5):915–922.
Jacobs, Lawrence and Suzanne Mettler. 2018. “When and How New Policy Creates New Politics.”
Perspectives on Politics 16(2):345–363.
Jones, David. 2017. Exchange politics. Oxford University Press.
Kaiser Health News. 2012. “KHN Morning Briefing: Thursday, September 13th.”.
URL: https://khn.org/morning-breakout/census-numbers-2/
Kamal, Rabah, Cynthia Cox, Michelle Long, Ashley Semanskee, Marco Ramirez and Larry
Levitt. 2018. “2019 Premium Changes on the ACA Exchanges.”.
URL: https://www.kff.org/health-costs/issue-brief/tracking-2019-premium-changes-on-aca-
exchanges/
Kogan, Vladimir and Thomas Wood. 2018. “Obamacare Implementation and the 2016 Elec-
tion.”. Available at SSRN 3075406. https://papers.ssrn.com/sol3/papers.cfm?abstract_
id=3075406.
Kriner, Douglas and Andrew Reeves. 2014. “Responsive Partisanship.” Journal of Health Politics,
Policy and Law 39(4):717–749.
30
Electronic copy available at: https://ssrn.com/abstract=3366994
Lerman, Amy E and Katherine T McCabe. 2017. “Personal Experience and Public Opinion.” The
Journal of Politics 79(2):624–641.
Lerman, Amy, Meredith Sadin and Samuel Trachtman. 2017. “Policy Uptake as Political Behav-
ior.” American Political Science Review 111(4):755–770.
Lerman, Amy and Vesla Weaver. 2014. Arresting citizenship. University of Chicago Press.
McCabe, Katherine T. 2015. “Attitude Responsiveness and Partisan Bias: Direct Experience with
the Affordable Care Act.” Political Behavior pp. 1–22.
Mettler, Suzanne. 2005. Soldiers to citizens: The GI Bill and the making of the greatest generation.
Oxford University Press on Demand.
Mettler, Suzanne. 2011. The Submerged State. University of Chicago Press.
Mettler, Suzanne. 2018. The Government-Citizen Disconnect. Russell Sage Foundation.
Michener, Jamila. 2018. Fragmented Democracy. New York, NY: Cambridge University Press.
Morgan, Kimberly and Andrea Campbell. 2011. The Delegated Welfare State. Oxford University
Press.
Nall, Clayton. 2018. The road to inequality. New York: Cambridge University Press.
Patashnik, Eric. 2008. Reforms at risk. Princeton, NJ: Princeton University Press.
Patashnik, Eric and Jonathan Oberlander. 2018. “After Defeat.” Journal of Health Politics, Policy
and Law 43(4).
Pearl, Judea. 2013. “Interpretation and Identification of Causal Mediation.” Psychological Methods
19(4):459–481.
Sances, Michael and Joshua Clinton. 2019. “Who Participated in the ACA?” Journal of Health
Politics, Policy, and Law 44(3).
Sommers, Benjamin, Atul Gawande and Katherine Baicker. 2017. “Health insurance coverage and
health—what the recent evidence tells us.”.
31
Electronic copy available at: https://ssrn.com/abstract=3366994
Soss, Joe. 1999. “Lessons of welfare.” American Political Science Review 93(02):363–380.
Soss, Joe and Sanford F Schram. 2007. “A public transformed? Welfare reform as policy feedback.”
American Political Science Review 101(1):111–127.
Tallevi, Ashley. 2018. “Out of Sight, Out of Mind?” Journal of Health Politics, Policy, and Law .
Witters, Dan. 2019. “U.S. Uninsured Rate Rises to Four-Year High.”. January 23.
URL: https://news.gallup.com/poll/246134/uninsured-rate-rises-four-year-high.aspx
32
Electronic copy available at: https://ssrn.com/abstract=3366994
Supplemental Information for “Offsetting Policy Feedback Effects:
Evidence from the Affordable Care Act”
Electronic copy available at: https://ssrn.com/abstract=3366994

Table of Contents
A Supplemental Information 1
A.1 Health Insurance Sources . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1
A.2 KFF Non-Group Surveys . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1
A.3 Benchmarking with a Pre-Implementation Model . . . . . . . . . . . . . . . . . 8
A.4 Panel Details . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11
A.5 Insurance Source Score Tests . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15
A.6 Integration of ACA Attitudes & Partisanship . . . . . . . . . . . . . . . . . . . 18
A.7 Geographic Variability in Exchange-based Insurance Prices . . . . . . . . . . . 22
Electronic copy available at: https://ssrn.com/abstract=3366994

A Supplemental Information
A.1 Health Insurance Sources
A.2 KFF Non-Group Surveys
A.2.1 Attitudes among the Non-Group Insured
Those with non-group insurance include people who purchase insurance on the exchanges or oth-
erwise purchase their insurance directly, but exclude those insured through Medicare, Medicaid,
or an employer as well as the uninsured. This group’s members were among those most directly
affected by the ACA. Below, we present similar estimates for another group that saw dispropor-
tionate impacts from the ACA: Kentucky residents, whose state saw the most dramatic decline in
its post-ACA uninsured rate.
To be sure, the non-group insured is a select population, as its members differ from those
with other sources of insurance in terms of their age, income, employment, and various other
0.0
0.1
0.2
0.3
0.4
Exchange
Medicaid
Other
Self−Purchased
Uninsured
Medicare
Employer−Insured
Before
1/14
After
1/14
Figure A1: Distribution of HTS respondents by health insurance source before and after the ACA’s
January 2014 implementation.
1
Electronic copy available at: https://ssrn.com/abstract=3366994

Income Education Age Male Black Hispanic Party ID N
Used Exchanges 59.8 14.7 47 0.50 0.12 0.13 2.5 1,074
Medicaid 26.8 12.7 46 0.42 0.23 0.21 2.5 3,469
Other 57.5 13.4 44 0.54 0.00 0.45 2.6 2,499
Uninsured 37.1 12.5 41 0.58 0.17 0.33 2.8 5,069
Medicare 58.5 14.3 70 0.44 0.09 0.05 2.9 12,379
Employer-Insured 106.6 15.3 48 0.53 0.10 0.09 2.9 22,624
Self-Purchased 76.6 14.6 53 0.51 0.09 0.09 3.0 4,708
All 77.9 14.4 52 0.51 0.11 0.12 2.9 52,424
Table A1: Key covariates and their associations with insurance sources, respondents to surveys
after December 2013. “Used exchanges” is a subset of “self-purchased.” Party ID is a 5 point
scale. All summary values are means.
Prior Coverage Non-group, Non-group,
All Exchange only
Covered by a different plan you purchased yourself 0.24 0.19
Covered by an employer 0.21 0.14
Covered by COBRA 0.05 0.04
Had Medicaid or other public coverage 0.06 0.06
Was uninsured 0.38 0.53
Covered by parents 0.01 0.01
Covered by family member (non-specific) 0.00 0.00
Military/VA 0.00 0.00
Same coverage/no change (non-specific) 0.01 0.00
Had coverage from some other source 0.01 0.01
Don’t know 0.01 0.01
Refused 0.01 0.01
Table A2: This table shows the prior insurance sources for respondents in the KFF 2014 non-group
survey.
factors. It is also a moving target. But such an examination can nonetheless identify variation in
ACA attitudes that might plausibly be connected to variation in Americans’ experiences with the
exchanges.
25
25
Among those who have non-group insurance, there are a few key distinctions that may ap-
pear in respondents’ ACA attitudes. For one, while many of these respondents purchased health
insurance through the exchanges, others used a broker or purchased a policy directly from an
insurance company. Some of these respondents have plans which meet the requirements for sale
on the exchanges, while others do not.
2
Electronic copy available at: https://ssrn.com/abstract=3366994

In the years immediately following the ACA’s implementation, KFF surveyed Americans who
got their insurance on the non-group market, whether using the exchanges or not.
26
The non-group
data includes several variables of interest: whether respondents purchased insurance through the
exchanges, whether their plan qualifies for sale on the exchanges, and whether they received a
subsidy to pay for the plan.
Using the four-category measure of ACA favorability as our outcome, we estimate linear mod-
els which predict ACA attitudes as a function of basic demographics including age, education,
five-category partisan identification, and identification as male, Asian American, Black, and His-
panic/Latinx. The models also include indicator variables for being surveyed on a landline as well
as the respondent’s stratum if surveyed in 2014.
27
The models also include a five-category mea-
sure of respondents’ income as a percentage of the Federal Poverty Line. Determinations about
enrollees’ eligibility for subsidies as well as their size are made based on this coarse measure.
SI Table A3 uses OLS models fit separately for each year to examine the correlates of four-
category ACA favorability when looking at those on the non-group insurance market. Simply
buying insurance that meets the regulations for exchange-traded plans has no strong association on
its own, as none of the corresponding coefficients even reach the size of their standard errors. The
coefficient for people who themselves bought insurance on the exchanges is consistently positive
and in the range of 0.16 to 0.21; the precision-weighted average is 0.18. While the signal isn’t
overwhelming, this result is consistent with the claim that exchange users were somewhat more
supportive of the ACA.
One of the ACA’s key policy levers was to subsidize lower-income Americans using the ex-
changes.
28
Receiving a subsidy is associated with more favorable ACA attitudes in all three
surveys, with coefficients of 0.49 (SE=0.11), 0.14 (SE=0.11), and 0.09 (SE=0.11). In 2014, people
26
The 2014, 2015, and 2016 surveys of individuals on the non-group market included 742, 804,
and 786 respondents between ages 18 and 64, respectively.
27
The 2014 survey included over-samples of those who are “very high poverty” and “high
poverty”; our models include indicator variables for being in these strata.
28
To validate the self-reported measure of subsidy receipt, we confirmed that subsidy receipt
is concentrated among lower-income respondents. While just 7% of 2014 non-group respondents
with incomes over 400% of FPL report receiving subsidies, 59% of those with lower incomes do.
3
Electronic copy available at: https://ssrn.com/abstract=3366994

who reported receiving subsidies were markedly more favorable toward the ACA, a relationship
that has attenuated since. Substantively, the association between receiving a subsidy and eval-
uating the ACA favorably declined markedly between 2014 and 2016 (p=0.01, two-sided). It’s
possible that the people opting into the ACA markets have changed over time, and that explains
the declining relationship. But it’s also possible that initial impact of the subsidies waned as their
recipients adjusted to them or as conditions in the marketplaces changed.
A.2.2 Attitudes in Kentucky, 2015
American adults who don’t have group-based insurance are one especially instructive group; the
attitudes of residents of specific states with unique post-ACA trajectories are another. Kentucky
was one of the few Republican-leaning states to create its own health insurance exchange, known
as “Kynect,” as well as expand its Medicaid program (Hertel-Fernandez, Skocpol and Lynch,
2016). It saw among the largest increases in its percentage of insured residents—and in late 2015,
its voters elected Republican Matt Bevin Governor after he had promised to shut down Kynect.
At the time of Bevin’s election, the Kaiser Family Foundation conducted a poll of Kentucky res-
idents (which included 692 respondents under 65) and asked various questions about respondents’
attitudes toward the ACA and health insurance. Here, we estimate models similar to those just
above in which we regress the four-category measure of ACA favorability on a variety of standard
demographic questions as well as respondents’ sources of insurance (if any). Even in Kentucky,
the survey data indicate that only 10% of adults under 65 had insurance they purchased them-
selves, and just 21% of those respondents reported having gotten their insurance through Kynect.
What’s more, only 13% of adults who purchased their own insurance—and just 2% of adults un-
der 65 overall—report receiving a subsidy to help with their insurance premiums.
29
As with some
other analyses, the coefficients are not meant to provide causal estimates, but they do provide
conditional correlations which will guide other inquiries.
Table A4 presents the fitted models. In some, we include a measure for whether the respondent
used Kynect while in the others we do not. People who purchase their own insurance are not
noticeably different from other Kentucky respondents, with coefficients that are substantively
29
Again, we restrict our analyses to those under 65 given that the exchanges target that popu-
lation.
4
Electronic copy available at: https://ssrn.com/abstract=3366994
small and inconsistent in their signs. Nor is there evidence that people who use the “Kynect”
exchange were more favorable—there, the coefficients are: -0.20 (SE=0.15) or -0.24 (SE=0.15).
But conditional on income, partisanship, and other background characteristics, respondents who
receive Medicaid are somewhat more favorable toward the ACA than others, with coefficients
varying from 0.21 (SE=0.15) to 0.35 (SE=0.15) depending on the specification.
We observe too few people receiving a subsidy to estimate its correlation with any precision,
but it is noteworthy that the coefficient corresponding to receiving a subsidy is substantively very
large, at 0.32-0.46. Still, this estimate for Kentucky residents with subsidies matches the estimate
from the analyses of all adults with non-group insurance in 2014 nationwide closely. As best
we can tell, receiving a subsidy is associated with a substantial boost in ACA favorability, even
conditional on income, education, and indicators for respondents’ racial/ethnic backgrounds.
5
Electronic copy available at: https://ssrn.com/abstract=3366994

ACA favorability
2014 2015 2016
Age −0.01 −0.001 −0.004
(0.003) (0.003) (0.003)
Education - 12 years −0.12 −0.25 0.08
(0.17) (0.17) (0.23)
Education - 13 −0.02 −0.14 −0.60
(0.28) (0.29) (0.49)
Education - 14 0.10 −0.38
∗
0.29
(0.17) (0.17) (0.24)
Education - 16 0.24 −0.34 0.17
(0.18) (0.18) (0.24)
Education - 19 0.45
∗
−0.10 0.37
(0.20) (0.20) (0.26)
Income (percentage of 0.01 −0.02 −0.04
Federal Poverty Line) (0.03) (0.02) (0.03)
Male −0.09 0.04 0.02
(0.09) (0.08) (0.09)
Hispanic 0.55
∗∗∗
−0.004 −0.48
(0.14) (0.13) (0.27)
Black 0.47
∗∗∗
0.08 0.55
∗∗∗
(0.14) (0.13) (0.16)
Asian 0.66
∗∗
0.13 −0.29
(0.25) (0.22) (0.24)
Weak Democrat −0.28
∗
0.07 −0.36
∗∗
(0.13) (0.12) (0.13)
Independent −0.63
∗∗∗
−0.83
∗∗∗
−0.63
∗∗∗
(0.12) (0.12) (0.13)
Weak Republican −0.98
∗∗∗
−1.13
∗∗∗
−1.16
∗∗∗
(0.15) (0.14) (0.16)
Strong Republican −1.27
∗∗∗
−1.18
∗∗∗
−1.23
∗∗∗
(0.13) (0.11) (0.13)
Health Plan Meets
Exchange Regulations
0.06 −0.05 0.16
(0.19) (0.14) (0.14)
Used exchange 0.21 0.19 0.16
(0.19) (0.13) (0.13)
Insurance subsidized 0.49
∗∗∗
0.14 0.09
(0.11) (0.11) (0.11)
Intercept 2.69
∗∗∗
3.42
∗∗∗
2.89
∗∗∗
(0.28) (0.26) (0.30)
Observations 577 687 538
∗
p<0.05;
∗∗
p<0.01;
∗∗∗
p<0.001
Table A3: Models of ACA favorability among the non-group insured, surveyed by KFF in 2014-
2016 (full models). Note that measures of the respondents’ strata for the 2014 survey and use of
a cell phone and family size for all three surveys were also included.
6
Electronic copy available at: https://ssrn.com/abstract=3366994

ACA favorability
Model 1 Model 2 Model 3 Model 4
Received Medicaid 0.30
∗
0.21 0.35
∗
0.27
(0.14) (0.15) (0.15) (0.15)
Purchased Own Insurance 0.11 −0.06 0.12 −0.07
(0.18) (0.20) (0.18) (0.20)
Employer-Provided Insurance 0.03 −0.09 0.005 −0.12
(0.13) (0.15) (0.14) (0.15)
Received Subsidy 0.32 0.46
(0.40) (0.41)
Insured 0.41
∗
0.41
∗
(0.20) (0.20)
Used Kynect −0.20 −0.24
(0.15) (0.15)
Employed −0.17 −0.14 −0.15 −0.12
(0.11) (0.11) (0.11) (0.11)
Male −0.10 −0.07 −0.10 −0.08
(0.10) (0.10) (0.10) (0.10)
Income - 25 −0.42
∗∗
−0.38
∗
−0.44
∗∗
−0.40
∗
(0.16) (0.16) (0.16) (0.16)
Income - 35 −0.24 −0.23 −0.26 −0.25
(0.18) (0.18) (0.18) (0.18)
Income - 45 −0.53
∗∗
−0.49
∗∗
−0.53
∗∗
−0.50
∗∗
(0.18) (0.18) (0.18) (0.18)
Income - 62.5 −0.50
∗∗
−0.46
∗
−0.53
∗∗
−0.48
∗∗
(0.18) (0.18) (0.18) (0.18)
Income - 82.5 −0.39 −0.35 −0.40 −0.36
(0.23) (0.23) (0.23) (0.23)
Income - 95 −0.46 −0.40 −0.47 −0.41
(0.29) (0.29) (0.29) (0.29)
Income - 200 −0.64
∗∗
−0.60
∗∗
−0.65
∗∗
−0.62
∗∗
(0.20) (0.20) (0.20) (0.20)
Age −0.01 −0.01 −0.01 −0.01
(0.004) (0.004) (0.004) (0.004)
Black 0.45
∗
0.46
∗
0.45
∗
0.45
∗
(0.19) (0.19) (0.19) (0.19)
Hispanic −0.18 −0.08 −0.19 −0.08
(0.27) (0.27) (0.27) (0.27)
Weak Democrat −0.18 −0.20 −0.18 −0.19
(0.16) (0.16) (0.16) (0.16)
Independent −0.85
∗∗∗
−0.85
∗∗∗
−0.84
∗∗∗
−0.84
∗∗∗
(0.15) (0.15) (0.15) (0.15)
Weak Republican −0.78
∗∗∗
−0.78
∗∗∗
−0.78
∗∗∗
−0.79
∗∗∗
(0.16) (0.16) (0.16) (0.16)
Strong Republican −1.06
∗∗∗
−1.06
∗∗∗
−1.07
∗∗∗
−1.07
∗∗∗
(0.12) (0.12) (0.12) (0.12)
Education - 10 −0.04 −0.14 0.01 −0.09
(0.30) (0.30) (0.30) (0.30)
Education - 12 −0.12 −0.18 −0.09 −0.14
(0.27) (0.27) (0.28) (0.28)
Education - 13 −0.20 −0.26 −0.15 −0.21
(0.28) (0.29) (0.29) (0.29)
Education - 14 0.09 0.02 0.13 0.06
(0.29) (0.29) (0.29) (0.29)
Education - 16 0.06 −0.01 0.10 0.03
(0.30) (0.30) (0.30) (0.30)
Education - 17 −0.08 −0.15 −0.05 −0.12
(0.58) (0.58) (0.58) (0.58)
Education - 19 0.17 0.12 0.21 0.16
(0.31) (0.31) (0.31) (0.31)
Intercept 3.60
∗∗∗
3.32
∗∗∗
3.58
∗∗∗
3.31
∗∗∗
(0.33) (0.36) (0.33) (0.36)
Observations 567 567 567 567
∗
p<0.05;
∗∗
p<0.01;
∗∗∗
p<0.001
Table A4: OLS models of respondents to the 2015 Kentucky KFF survey (full model).
7
Electronic copy available at: https://ssrn.com/abstract=3366994

−0.10
−0.05
0.00
0.05
0.10
0.15
Exchange
Medicaid
Other
Self−Purchased
Uninsured
Medicare
Employer−Insured
Actual − Expected
ACA Favorability
Before 1/14
After 1/14
Figure A2: Actual versus expected favorability by insurance source. Expected favorability is es-
timated using a linear regression on all respondents in the pre-2014 period. The actual versus
expected estimates are the observed ACA attitudes minus the predicted ACA attitudes.
A.3 Benchmarking with a Pre-Implementation Model
To contextualize the results in the main manuscript on favorability by insurance source, we here
consider expected ACA favorability by insurance source. Using the same basic demographic vari-
ables as in the insurance source score analysis below, we predict favorability toward the ACA in
the pre-implementation period. We then calculate the difference between actual ACA favorability
and predicted favorability for all insurance types. Figure A2 shows these differences, with ex-
change users significantly more favorable toward the ACA than their demographics would suggest
while those without insurance were significantly more negative.
30
SI Table A5 shows the model
predicting favorability by demographics from which expected favorability is estimated.
Like the earlier results, this analysis is subject to selection concerns. Even so, it provides a
sense of the magnitude of the potential selection effect. Also, SI Figure A3 shows these same
30
Note that the pre-implementation differences are model residuals—the key point here is the
difference pre- and post-implementation.
8
Electronic copy available at: https://ssrn.com/abstract=3366994

effects multiplied by the population size within each insurance category. Even subtle changes in
attitudes among those with employer-provided insurance or Medicare—much larger groups than
exchange users—can have an aggregate impact on ACA attitudes equal to that generated by much
more dramatic shifts among exchange users themselves.
−0.010
−0.005
0.000
0.005
Exchange
Medicaid
Other
Self−Purchased
Uninsured
Medicare
Employer−Insured
Actual − Expected ACA
Favorability x Pop Size
Before 1/14
After 1/14
Figure A3: This figure presents the difference between each group’s actual ACA favorability and
its expected ACA favorability given its demographics multiplied by its overall population size.
When summed, very small declines in attitudes among those with employer-provided insurance
are similar in size to the total increase in ACA favorability among Medicaid recipients.
9
Electronic copy available at: https://ssrn.com/abstract=3366994

ACA Favorability
Education - 10 −0.02
(0.02)
Education - 12 −0.07
∗∗∗
(0.02)
Education - 13 −0.05
∗∗
(0.02)
Education - 14 −0.04
∗
(0.02)
Education - 16 0.004
(0.02)
Education - 17 0.06
∗∗
(0.02)
Education - 19 0.11
∗∗∗
(0.02)
Income −0.06
∗∗∗
(0.01)
Income
2
−0.01
(0.01)
Income
3
0.02
∗∗
(0.01)
Age 0.003
(0.01)
Age
2
0.02
∗
(0.01)
Age
3
−0.04
∗∗∗
(0.01)
Age
4
−0.003
(0.002)
Age
5
0.01
∗∗∗
(0.002)
Black 0.37
∗∗∗
(0.01)
Hispanic 0.22
∗∗∗
(0.01)
Asian 0.20
∗∗∗
(0.02)
Male −0.05
∗∗∗
(0.01)
Retired 0.03
∗∗∗
(0.01)
Constant 0.32
∗∗∗
(0.03)
Observations 34,169
F Statistic 62.42
Table A5: ACA favorability model using demographics only, HTS data pre-implementation. State
fixed effects not shown.
10
Electronic copy available at: https://ssrn.com/abstract=3366994

A.4 Panel Details
Wave Start Date End Date N
Wave 1 October 2nd, 2007 December 31st, 2007 19,190
Wave 2 January 1st, 2008 March 31st, 2008 17,747
Wave 3 April 2nd, 2008 August 28th, 2008 20,052
Wave 4 August 29th, 2008 November 4th, 2008 19,241
Wave 5 November 5th, 2008 January 20th, 2009 19,234
Wave 6 October 19th, 2012 October 29th, 2012 2,606
Wave 7 November 14th, 2012 January 29th, 2013 2,471
Wave 8 October 17th, 2014 October 31st, 2014 1,693
Wave 9 November 19th, 2014 January 14th, 2015 1,493
Wave 10 January 22nd, 2016 February 8th, 2016 1,562
Wave 11 October 14th, 2016 October 24th, 2016 1,227
Wave 12 November 28th, 2016 December 7th, 2016 1,075
Wave 13 October 23rd, 2018 November 5th, 2018 1,024
Table A6: This table summarizes the panel waves and sample sizes.
Here, we detail the demographics of our GfK-based panel. Our respondents are older than the
U.S. population, but that is to be expected: they had to be 18 in late 2007 to participate. On a
variety of other metrics, even the sample which participated in the final waves are a reasonable
approximation of the target population of U.S. adults over 25 (see Appendix Table A7). For
example, our sample’s mean income in 2016 was $58.4K, which is not far from the 2015 U.S.
median household income of $54.9K. Of particular importance is the fact that there is no evidence
of heightened attrition rates among those who are less politically engaged. We merged our data
with validated vote histories provided by the data vendor Catalist and found that voter turnout
was essentially indistinguishable among those who did and did not remain in the panel between
2012 and 2016. Specifically, 2008 turnout was 69.4% among the 2,471 respondents to the post-
election 2012 wave and 69.0% among the 1,075 respondents who participated in post-election 2016
wave.
11
Electronic copy available at: https://ssrn.com/abstract=3366994

Min Max Mean Miss. Mean Miss. Mean Miss. ACS
2008 2008 2008 2008 2012 2012 2016 2016 2015
Income ’08* 2.50 250.00 61.38 0.31 57.72 0.07 58.40 0.00 54.89
Years of Ed. ’08 4.00 19.00 14.33 0.00 13.76 0.00 13.68 0.00
HS Degree ’08 0.00 1.00 0.96 0.00 0.94 0.00 0.94 0.00 0.87
Has BA ’08 0.00 1.00 0.40 0.00 0.31 0.00 0.30 0.00 0.30
Party ID ’08 1.00 7.00 3.87 0.15 3.82 0.17 3.87 0.14
Union Hsh. ’08 0.00 1.00 0.09 0.00 0.12 0.00 0.13 0.00
Catholic ’08 0.00 1.00 0.16 0.00 0.21 0.00 0.20 0.00
Protestant ’08 0.00 1.00 0.27 0.00 0.31 0.00 0.33 0.00
Female ’08 0.00 1.00 0.56 0.00 0.53 0.00 0.50 0.00 0.51
Age ’08 18.00 110.00 50.13 0.00 47.12 0.00 48.84 0.00
Over 65 ’08 0.00 1.00 0.17 0.00 0.14 0.00 0.15 0.00 0.15
Black ’08 0.00 1.00 0.09 0.00 0.13 0.00 0.12 0.00 0.13
Hispanic ’08 0.00 1.00 0.06 0.00 0.10 0.00 0.10 0.00 0.17
White ’08 0.00 1.00 0.80 0.00 0.71 0.00 0.71 0.00 0.77
Voted ’12 0.69 .21 0.69 0.21
Table A7: Demographics for the (1) 19,241 respondents to panel wave 4 in 2008; (2) 2,471 respon-
dents to panel wave 7 in 2012; (3) 1,075 respondents to panel wave 16 in November-December 2016.
“Miss.” refers to the share of that variable which is missing for respondents to the designated
panel wave. The American Community Survey benchmarks come from July 1, 2015 estimates for
the full U.S. population. The asterisk (*) denotes that the U.S. Census reports median household
income, not mean income.
12
Electronic copy available at: https://ssrn.com/abstract=3366994

Repeal ACA (1-7)
Intercept 3.56
∗
(0.35)
Uninsured, Fall ’18 1.23
∗
(0.43)
Uninsured, Jan. ’16 −0.03
(0.40)
Jan. ’16: Medicare −0.13
(0.33)
Jan. ’16: Plan through parent −0.91
(1.10)
Jan. ’16: Plan through employer −0.15
(0.34)
Jan. ’16: Self-purchased plan −0.62
(0.40)
Jan. ’16 Insurance: Refused −1.04
(0.99)
Jan. ’16: Other government insurance −0.30
(0.47)
Jan. ’16: Somewhere else 0.38
(0.45)
Jan. ’18: Medicare 0.07
(0.37)
Jan. ’18: Plan through parent 2.80
(1.66)
Jan. ’18: Plan through employer 0.45
(0.39)
Jan. ’18: Self-purchased plan 0.56
(0.46)
Jan. ’18 Insurance: Refused 1.03
(1.76)
Jan. ’18: Other government insurance 0.75
(0.53)
Jan. ’18: Somewhere else −0.68
(0.51)
Oct. ’12: Repeal ACA 0.60
∗
(0.11)
Nov. ’12-Jan. ’13: Repeal ACA −0.02
(0.10)
Oct. ’16: Repeal ACA 0.76
∗
(0.08)
Oct. ’12: GOP Partisan ID 0.34
∗
(0.07)
Oct. ’12: Years of Education 0.10
(0.06)
Oct. ’12: White 0.19
(0.14)
Oct. ’12: Black −0.27
(0.22)
Fall ’07: Income 0.01
(0.05)
Oct. ’12: Female 0.02
(0.11)
Oct. ’12: Age 0.24
∗
(0.08)
Fall ’07: Union household 0.13
(0.17)
Fall ’07: Catholic −0.05
(0.15)
Fall ’07: Protestant 0.21
(0.13)
R
2
0.65
Num. obs. 567
∗
p < 0.05
Table A8: This table presents an OLS model of fall 2018 anti-ACA attitudes, measured on a 1-7
scale, as a function of various variables.
13
Electronic copy available at: https://ssrn.com/abstract=3366994

Repeal ACA ’18 Repeal ACA ’18
Model 1 Model 2
(Intercept) 3.83
∗
3.78
∗
(0.26) (0.29)
Jan. ’16: Medicare 0.04 −0.14
(0.28) (0.29)
Jan. ’16: Plan through parent −0.78 −0.73
(1.09) (1.10)
Jan. ’16: Plan through employer 0.08 0.04
(0.27) (0.27)
Jan. ’16: Self-purchased plan −0.31 −0.33
(0.33) (0.33)
Jan. ’16 Insurance: Refused −0.98 −1.02
(0.99) (0.99)
Jan. ’16: Other government program 0.19 0.10
(0.41) (0.41)
Jan. ’16: Other insurance 0.34 0.19
(0.42) (0.43)
Jan. ’16: Uninsured 0.53 0.54
(0.35) (0.35)
Oct. ’12: ACA attitudes 0.61
∗
0.59
∗
(0.10) (0.11)
Nov. ’12-Jan. ’13: ACA attitudes 0.03 0.03
(0.10) (0.10)
Oct. ’16: ACA attitudes 0.75
∗
0.76
∗
(0.08) (0.08)
Oct. ’12: GOP partisan ID 0.35
∗
0.32
∗
(0.07) (0.07)
Oct. ’12: Years of Ed. 0.09
(0.06)
Oct. ’12: White 0.17
(0.14)
Oct. ’12: Black −0.20
(0.22)
Fall ’07: Income 0.00
(0.05)
Oct. ’12: Female 0.04
(0.11)
Oct. ’12: Age 0.18
∗
(0.08)
Fall ’07: Union Household 0.12
(0.17)
Fall ’07: Catholic −0.09
(0.15)
Fall ’07: Protestant 0.19
(0.13)
R
2
0.62 0.63
Num. obs. 573 573
∗
p < 0.05
Table A9: This table presents an OLS model of fall 2018 anti-ACA attitudes, measured on a 1-7
scale, as a function of various variables.
14
Electronic copy available at: https://ssrn.com/abstract=3366994

A.5 Insurance Source Score Tests
Market score Uninsured score Self-purchased score
Mean 0.03 0.06 0.10
SD 0.02 0.06 0.04
Min 0.00 0.00 0.01
Max 0.34 0.75 0.54
Table A10: Summary statistics for insurance source scores. Given that we observe a relatively
small amount of variability in these scores, we limit our interpretation of coefficient sizes in several
analyses to a change of 0.1 in the scores. Although the models themselves are no different depend-
ing on this scaling, this limited interpretation is perhaps more clear and faithful to the amount of
variation in the data we have available.
Predicted Insurance Source
Exchanges Uninsured Self-purchased
Exchanges 1.00 0.14 0.53
Uninsured 0.14 1.00 -0.08
Self-purchased 0.53 -0.08 1.00
Table A11: Exchange scores are highly correlated with self-purchased scores because exchanges
are a subset of the self-purchased in the data.
15
Electronic copy available at: https://ssrn.com/abstract=3366994

Exchanges Uninsured Self-Purchased
Education - 10 −0.01 −0.18
∗∗∗
−0.05
∗
(0.02 (0.03 (0.03)
Education - 12 0.001 −0.26
∗∗∗
−0.04
(0.01 (0.02 (0.03)
Education - 13 0.01 −0.29
∗∗∗
−0.04
∗
(0.01 (0.02 (0.03)
Education - 14 −0.001 −0.30
∗∗∗
−0.04
(0.01 (0.02 (0.03)
Education - 16 0.02 −0.31
∗∗∗
−0.01
(0.01 (0.02 (0.03)
Education - 17 0.002 −0.31
∗∗∗
−0.02
(0.02 (0.03 (0.03)
Education - 19 0.01 −0.33
∗∗∗
−0.03
(0.01 (0.02 (0.03)
Income −0.01 −0.01 −0.004
(0.02 (0.03 (0.03)
Income
2
0.02
∗∗∗
0.03
∗∗∗
0.02
∗∗∗
(0.005 (0.01 (0.01)
Income
3
−0.01 −0.02 −0.01
(0.01 (0.02 (0.02)
Age 0.78
∗∗∗
−2.04
∗∗∗
2.55
∗∗∗
(0.18 (0.28 (0.31)
Age
2
0.04 −1.03
∗∗∗
0.51
∗
(0.18 (0.27 (0.30)
Age
3
0.30
∗
1.52
∗∗∗
0.57
∗
(0.17 (0.26 (0.30)
Age
4
−0.04 0.05 0.26
(0.17 (0.26 (0.29)
Age
5
0.24 0.41 0.57
∗∗
(0.17 (0.25 (0.29)
Black −0.002 0.01 −0.03
∗∗∗
(0.004 (0.01 (0.01)
Hispanic 0.003 0.03
∗∗∗
−0.01
(0.004 (0.01 (0.01)
Asian −0.01
∗∗∗
−0.02
∗∗
−0.01
(0.01 (0.01 (0.01)
Male 0.002 0.001 0.02
∗∗∗
(0.002 (0.004 (0.004)
Retired 0.0001 −0.02
∗∗
0.05
∗∗∗
(0.01 (0.01 (0.01)
Constant 0.01 0.31
∗∗∗
0.10
∗∗∗
(0.02 (0.03 (0.03)
Observations 17,018 19,688 19,688
F Statistic 3.38 17.82 5.33
Table A12: Insurance source score models. State fixed effects not shown.
16
Electronic copy available at: https://ssrn.com/abstract=3366994

ACA favorability
Purchased on Exchanges Uninsured Self-Insured
Intercept 0.45
∗∗∗
0.45
∗∗∗
0.58
∗∗∗
(0.01) (0.01) (0.01)
Insurance Source Score 0.71
∗∗∗
◦ 0.18
∗∗∗
−1.18
∗∗∗
◦
(0.19) (0.06) (0.09)
Post-Implementation 0.01 0.03
∗
−0.01
(0.02) (0.02) (0.02)
Post-Implementation ×
Insurance Source Score
−0.39 −0.52
∗∗∗
−0.04
(0.26) (0.08) (0.13)
Observations 35,474 35,474 35,474
Number of period random-effects 10 10 10
∗
p<0.05;
∗∗
p<0.01;
∗∗∗
p<0.001; ◦ leads to prediction outside 0-1
Table A13: This table presents the results of a multi-level model predicting four-category ACA
favorability. Unlike the figure above, these scores estimate moving from 0% to 100% probability.
This extrapolates from the observed data, since the demographic variables do not strongly predict
purchasing on the exchanges and being uninsured. The insurance source score result for purchasing
on the exchanges suggests that these groups were already extremely favorable toward the law, and
perhaps could only maintain that high opinion or lower it.
17
Electronic copy available at: https://ssrn.com/abstract=3366994

A.6 Integration of ACA Attitudes & Partisanship
●
●
●
●
●
●
●
●
●
●
●
●
●
●
●
●
−0.2 0.0 0.2
Exchange Score
respondents under 65, income over 40k
Democrat
10 11 12 13 14 15 16 17
Pre−Exchanges Post−Exchanges
0.03
0.52
●
●
●
●
●
●
●
●
●
●
●
●
●
●
●
●
−0.20 −0.05 0.05
Uninsured vs Self−Purchased Score
respondents under 65, income over 40k
Democrat
10 11 12 13 14 15 16 17
Pre−Exchanges Post−Exchanges
Self−insured
0.00
●
●
●
●
●
●
●
●
●
●
●
●
●
●
●
●
Uninsured vs Self−Purchased Score
respondents under 65, income over 40k
Democrat
10 11 12 13 14 15 16 17
Pre−Exchanges Post−Exchanges
Uninsured
−0.02***
Figure A4: Over-time associations between insurance source scores, partisan identification. This
figure shows the effect of a 10-percentage-point increase over the mean score. The uninsured
score is meant to capture the effect of the individual mandate on ACA attitudes. However, the
uninsured score is a catch-all score—it identifies both those groups who chose to forego insurance
rather than purchase insurance on the individual market and those groups who would have foregone
purchasing on the individual markets had they not had some other source of insurance, such as an
employer-based health plan. Partisanship here is measured via 1=Democrat, 0.5=Independent,
and 0=Republican.
●
●
●
●
●
●
●
●
●
●
●
●
●
●
●
●
−0.3 −0.1 0.1 0.3
Exchange Score
respondents under 65, income over 40k
Independent
10 11 12 13 14 15 16 17
Pre−Exchanges Post−Exchanges
0.05
0.42
●
●
●
●
●
●
●
●
●
●
●
●
●
●
●
●
−0.10 0.00 0.10
Uninsured vs Self−Purchased Score
respondents under 65, income over 40k
Independent
10 11 12 13 14 15 16 17
Pre−Exchanges Post−Exchanges
Self−insured
−0.04**
●
●
●
●
●
●
●
●
●
●
●
●
●
●
●
●
Uninsured vs Self−Purchased Score
respondents under 65, income over 40k
Independent
10 11 12 13 14 15 16 17
Pre−Exchanges Post−Exchanges
Uninsured
0.03**
Figure A5: Over-time associations between insurance source scores, identification as independent.
This figure shows the effect of a 10-percentage-point increase over the mean score.
18
Electronic copy available at: https://ssrn.com/abstract=3366994

Party ID Identify as Independent
(Identify as Democrat)
(control ACA) (control ACA)
Under 65 −0.02 −0.01 −0.01 −0.04
∗
(0.02) (0.02) (0.02) (0.02)
Post-Implementation −0.05
∗∗∗
−0.04
∗∗∗
−0.02 −0.05
∗∗
(0.02) (0.01) (0.02) (0.02)
Post-Implementation x Under 65 0.02
∗
0.01 0.01 0.04
∗∗
(0.01) (0.01) (0.02) (0.02)
ACA favorability 0.16
∗∗∗
−0.04
∗∗∗
(0.003) (0.004)
Observations 11,276 9,499 11,276 9,499
∗
p<0.05;
∗∗
p<0.01;
∗∗∗
p<0.001
Table A14: “Democrat” is measured via 3-category partisan identification, with Democrat coded
1, Republican coded 0, and Independent coded 0.5.
19
Electronic copy available at: https://ssrn.com/abstract=3366994

Pre-ACA Post-ACA
Intercept 3.57
∗
1.91
(1.24) (1.37)
Age > 64 −0.12 0.01
(0.06) (0.06)
Age −0.02 −0.00
(0.02) (0.02)
Survey Month 1.92
∗
1.43
(0.92) (1.65)
Survey Month Sq. −2.18 −0.60
(1.14) (1.00)
Education 0.05
∗
0.03
∗
(0.01) (0.01)
Black 0.49
∗
0.44
∗
(0.06) (0.05)
Hispanic 0.37
∗
0.40
∗
(0.07) (0.06)
Asian Am. 0.29
∗
0.28
∗
(0.13) (0.13)
Male −0.04 −0.01
(0.03) (0.03)
Income 0.20 0.09
(0.29) (0.26)
Weak Dem −0.24
∗
−0.85
∗
(0.05) (0.05)
Pure Independent −0.96
∗
−0.82
∗
(0.06) (0.05)
Weak GOP −1.60
∗
−0.94
∗
(0.05) (0.05)
Strong GOP −1.60
∗
−1.56
∗
(0.04) (0.04)
R
2
0.42 0.32
N 3843 4791
∗
p < 0.05
Table A15: These tables present the RDD models fit to respondents between 62 and 68 before
(left) and after (right) the ACA’s implementation.
20
Electronic copy available at: https://ssrn.com/abstract=3366994

Beta SE t-value
Education -0.108 0.133 -0.813
Black 0.015 0.013 1.158
Hispanic 0.008 0.011 0.698
Asian American 0.012 0.005 2.285
Male -0.000 0.022 -0.020
Republican -0.024 0.080 -0.296
Income -1.250 2.912 -0.429
Table A16: This table presents checks of the key assumption underpinning the RDD analyses,
which is that potentially confounding variables are distributed smoothly at the point of the dis-
continuity. Using the same specification as in the RDD models in Table A15, it presents the
coefficient, standard error, and t-value from models in which the listed variable is the dependent
variable predicted by being 65 or older. As the table makes clear, none of these variables are
significantly different for those just over 65 years old save for being Asian American, which is
slightly more common just over 65.
21
Electronic copy available at: https://ssrn.com/abstract=3366994

A.7 Geographic Variability in Exchange-based Insurance Prices
ACA favorability
Non-Market Market Uninsured
Weak Democrat −0.63
∗∗∗
−0.19 −0.42
∗∗∗
(0.02) (0.15) (0.07)
Independent −0.87
∗∗∗
−0.60
∗∗∗
−0.63
∗∗∗
(0.03) (0.16) (0.07)
Weak Republican −1.01
∗∗∗
−0.94
∗∗∗
−0.50
∗∗∗
(0.03) (0.15) (0.07)
Strong Republican −1.51
∗∗∗
−1.27
∗∗∗
−0.91
∗∗∗
(0.02) (0.14) (0.08)
Education 0.03
∗∗∗
−0.01 −0.03
∗∗
(0.003) (0.02) (0.01)
Income −0.0003
∗
−0.001 −0.002
∗∗
(0.0001) (0.001) (0.001)
Black 0.37
∗∗∗
0.40
∗
0.36
∗∗∗
(0.03) (0.16) (0.07)
Hispanic 0.28
∗∗∗
0.01 0.46
∗∗∗
(0.03) (0.16) (0.07)
Asian 0.20
∗∗∗
0.74
∗
0.19
(0.05) (0.35) (0.19)
Age −0.001 0.001 −0.01
∗∗∗
(0.0005) (0.004) (0.002)
County % Black 2010 −0.20
∗
0.54 0.38
(0.08) (0.53) (0.23)
County % Hispanic 2010 0.03 0.23 0.38
∗
(0.06) (0.36) (0.17)
County Med. Hsh. Inc. 2010 −0.0000 0.0000 −0.0000
(0.0000) (0.0000) (0.0000)
County % Poor 2010 0.003 1.01 −0.16
(0.30) (1.81) (0.92)
County % Unemployed 2010 5.15
∗∗∗
−6.40 2.24
(0.90) (6.14) (2.62)
County ∆ % Unemployed 2010-16 3.56
∗∗
−2.43 4.30
(1.15) (7.88) (3.51)
County % with BA 2010 0.97
∗∗∗
1.24 0.48
(0.13) (0.79) (0.40)
Number of plans (logged, in
sd’s)
0.001 −0.07 −0.004
(0.01) (0.06) (0.03)
Mean Premium (in sd’s)
0.004 0.04 0.05
(0.01) (0.07) (0.03)
Mean Change in Premium (in
sd’s)
0.001 −0.19
∗∗
−0.02
(0.01) (0.07) (0.04)
Constant 2.17
∗∗∗
2.87
∗∗∗
2.65
∗∗∗
(0.14) (0.70) (0.34)
Month FEs Y Y Y
County-Level Demographics Y Y Y
Clusters (Year) 3 3 3
Note:
∗
p<0.05;
∗∗
p<0.01;
∗∗∗
p<0.001
Table A17: This table presents the results of the full multi-level models fit to KFF respondents from
2015, 2016, and 2017 in which certain insurance market conditions (and various other independent
variables) predict ACA favorability, measured on a 1 to 4 scale.
22
Electronic copy available at: https://ssrn.com/abstract=3366994
