
PHARMACY PRACTICE EXPERIENCE
PRECEPTOR MANUAL

PAGE 1 | 58
TABLE OF CONTENTS
Introduction 2
Experiential Contact List 5
Snapshot of Experiential (IPPE & APPE) Program 7
Faculty Appointment for Preceptors 10
Quality Assurance 13
Preceptor and Site Requirements 14
Preceptor Roles 16
Lesson Plan 18
Student Log of Patient Care Activities 25
Providing Feedback 27
Grading and Evaluation Form 30
Ad Hoc Evaluations 39
APPE Student Policies 40
Oregon Board of Pharmacy Intern Regulations 44
E*Value 49
Online Preceptor Training 51
Conducting Research with Human Subjects 54
Incident Report Form 56
Change in Rotation Authorization Form 58

PAGE 2 | 58
INTRODUCTION
Dear Valued Preceptor,
On behalf of the College of Pharmacy, I would like to sincerely thank you for providing our students
the opportunity to demonstrate and develop their knowledge, skills, attitude and behavior in your
practice setting. This manual will help you understand your role as a preceptor and how to
develop the critical thinking and clinical skills that will enable our student to develop, recommend
and evaluate pharmaceutical care by integrating patient-specific data with disease-specific and
drug-specific information while considering ethical and quality-of-life factors for patient.
Each
student is also given a corresponding student syllabus and manual that details their curricular
responsibilities. Please ask your student to review with you their course syllabus and manual.
Again, we want to thank you for volunteering your time and energy in helping us fulfill our mission,
“…to advance societal health through leadership in pharmacy education,
research, community engagement, and improved patient care.”
https://youtu.be/9l6umW1tIC8
Brief History
The College can trace its roots back to 1898, when pharmacy was offered alongside chemistry at
what was then the Oregon Agricultural College. In 1917, following the First World War and in
response to a growing demand for medication experts, the department of pharmacy was formed
into a separate school of pharmacy. Starting in 1923 and finishing in 1924, the Corvallis campus
pharmacy building was constructed. In 1952, a PhD program was added, which elevated the
school’s national stature and helped to attract the very best faculty from across the country.
The existing building was renovated and expanded in 1966, doubling the size of the building and
greatly adding to the program’s capacity. It was in 1983 when we formed our first formal affiliation
with OHSU. That affiliation provided for joint faculty appointments and clinical practice sites in
Portland. At the same time, the School of Pharmacy became the College of Pharmacy. Five years
later, in 1988, OHSU established dedicated space for the pharmacy program in Portland, and
created a position for a Dean of Pharmacy Practice.

PAGE 3 | 58
In 2000, the College of Pharmacy began offering the Doctor of Pharmacy degree, the PharmD,
as the sole professional degree. This was to comply with a mandate by the Accreditation Council
on Pharmaceutical Education that all future pharmacy graduates must possess the PharmD
degree to become licensed. The transition to the PharmD degree necessitated additional clinical
curriculum and led to even closer ties with OHSU, and not much later, in 2001 we signed a formal
memorandum of understanding with OHSU establishing a jointly awarded PharmD degree
program.
At the time, students on Marquam Hill campus shared space with other academic programs. In
2006, we were fortunate to be among those that made the move to the South Waterfront, at what
was then the new Center for Health & Healing. For the first time, the College of Pharmacy had
dedicated spaces for classes, labs, and student lounges. Our tenancy was short lived, though,
because in 2014 Oregon State University, OHSU, and Portland State University came together
to jointly construct the Collaborative Life Sciences Building at the waterfront. At the new CLSB,
the College of Pharmacy has a 150-person theater-style lecture hall, three 25-person classrooms,
clinical practice labs, space for Portland based faculty members, and a six-fold increase in
research laboratory space in Portland.
Students spend the first two years of the Pharm.D. program in Corvallis on the main Oregon State
University campus. This offers all the resources of a major research university and a classic
collegiate experience. They spend the third year of the Pharm.D. program in Portland on the
Oregon Health & Science University campus, offering all the benefits of a partnership with a
renowned academic medical center in one of America's most livable cities. While students engage
in hands-on learning during all four years of the program, the fourth year is entirely devoted to
experiential education throughout the state of Oregon and beyond. Pharmacy students engage
with these larger communities through pharmacy professional associations, volunteer and
outreach activities, civic and alumni groups, cultural centers, Beaver athletics, and more.

PAGE 4 | 58
Curriculum
The College has 2 academic departments (Pharmacy Practice and Pharmaceutical Sciences)
with separate degree programs, the PharmD and the PhD, respectively. Additionally, we also offer
a dual PharmD / PhD and PharmD / MBA program. While all of practice sits within the Pharmacy
Practice department, research is performed across both departments, much of it in conjunction
with OHSU. Additionally, faculty from the Pharmaceutical Sciences department also teach as
guest lecturers in Pharmacy Practice courses.
The PharmD curriculum is delivered in a 4-year and quarter-based system that has two major
components to the degree; didactic a.k.a. classroom-based learning and experiential education.
Right from the start, students are licensed by the Oregon Board of Pharmacy and we begin their
experiential learning in community pharmacies. In those settings, students develop skills in patient
counseling, medication therapy management, transitions of care, immunizations, and so much
more.
To view our faculty and the Pharm.D. Curriculum please enter the College of Pharmacy
Website: http://pharmacy.oregonstate.edu/
Experiential Education is 30% of the Pharm.D. curriculum and is divided into two components,
Introductory Pharmacy Practice Experience (IPPE) and Advanced Pharmacy Practice Experience
(APPE). IPPE is delivered during the 1
st
,2
nd
, and 3
rd
profession years and the curriculum is
focused on introducing students to 3 main categories of pharmacy practice, community,
ambulatory care, and acute care. APPE is delivered during the 4
th
and final profession year of
our Pharm.D. Curriculum is a compilation of eight 6 week pharmacy experiences plus an off block
designed to allow each student to further develop, integrate, and apply to actual practice the
knowledge, skills, and behavior that they have learned during the didactic portion of the
curriculum.
The Experiential Education Office (https://pharmacy.oregonstate.edu/Experiential
) is responsible
for recruiting and maintaining rotation sites, assigning rotations to students, delivering
orientations/training for students and preceptors, developing rotation sites to be suitable
experiential “classrooms”, and providing guidance and support for students and preceptors during
rotations. These non-paid pharmacy internship experiences are in true practice sites and are
supervised by licensed pharmacists and, in some cases, in conjunction with other healthcare
professionals such as physicians and nurses who are all passionate about teaching and
mentoring students. In aggregate, the IPPE and APPE rotation sequences are designed and
coordinated to develop and transform students into confident and competent pharmacists who
will be able to deliver pharmaceutical care in a variety of settings to a diverse array of people.

PAGE 5 | 58
CONTACTS
EXPERIENTIAL EDUCATION TEAM
Juancho Ramirez, Pharm.D.
Assistant Dean of Experiential Education
ramireju@ohsu.edu
541-974-2421
Shannon Starwalt, Pharm.D.
Director of Introductory Pharmacy Practice Experiences
Shannon.starwalt@oregonstate.edu
541-737-8035
Nancy Baker
Experiential Education Program Specialist (P4)
nancy.baker@oregonstate.edu
541-737-6745
Miriam Steele
Experiential Education Program Specialist (P1-P3)
Miriam.steele@oregonstate.edu
541-737-2336
Nic Bookman, MPH
Academic and Experiential Assessment Analyst
bookmann@ohsu.edu
503-346-4522

PAGE 6 | 58
COMMOM “HELP” NUMBERS
OSU College of Pharmacy, Main Office, Portland, Phone 503-494-5778
OSU College of Pharmacy, Main Office, Portland, Fax 503-494-8797
OSU College of Pharmacy, Corvallis, Phone 541-737-3424
OSU College of Pharmacy, Corvallis, Fax 541-737-3999
STUDENT HEALTH SERVICES
Oregon State University (OSU) 541-737-9355
Oregon Health & Science University (OHSU) 503-494-8665
OSU STUDENT SERVICES
OSU Financial Aid 541-737-2241
OSU Registrar 541-737-4331
OREGON BOARD OF PHARMACY
Oregon Board of Pharmacy, Phone 971-673-0001
Oregon Board of Pharmacy, Fax 971-673-0002

PAGE 7 | 58
PROGRESSION OF EXPERIENTIAL EXPERIENCES
P1-P3 IPPE Courses
P4 APPE Courses

PAGE 8 | 58
Prior to advancing to the APPE year, each student must complete and pass all of the requirements
of the Pre-APPE Curriculum which includes but not limited to the IPPE sequence and the Pre-
APPE Readiness (PAR) block which occurs at the conclusion of the P3 year. The purpose of the
PAR Block is to assure students’ confidence, competence, and readiness to integrate into
collaborative health care settings and serve diverse patient populations during the advanced
pharmacy practice experiences (APPE) curriculum year. This assurance is based on
demonstrated ability to apply the necessary knowledge, skills, attitudes, and values of the
profession and are assessed via educationally sound assessment strategies. Through the PAR
block, students will be poised to optimize their APPE rotations and set them on a path to career
readiness through faculty, self, and peer evaluation.
The APPE curriculum requires each student to complete a minimum of 1920 hours which is
subdivided into 8 blocks that are 6 weeks (minimum 240hrs) long. Students are also given a 6
week “off block” which can occur at any time after the first block. The “off block” hours does not
count towards the required minimum hours for successful completion of the APPE year. Each
student must complete and pass the following required categories of pharmacy practice
experiences:
• Phar 780 Community
• Phar 785 Ambulatory Care
• Phar 790 General Hospital Adult Medicine
• Phar 792 General Hospital
The required pharmacy practice experiences are provided by organizations that embrace and
practice team-based care which we define as the provision of comprehensive health services to
individuals by at least two health professionals who work collaboratively on shared goals to
achieve care that is safe, effective, efficient, and patient centered.
P4 - APPE Course
Phar 780 - Community
6 weeks
Minimum 240 hrs
Phar 785 - Ambulatory Care
6 weeks
Minimum 240 hrs
Phar 790 - General Medicine
6 weeks
Minimum 240 hrs
Phar 792- General Hospital
6 weeks
Minimum 240 hrs
Phar 795 - Patient Care Elective
6 weeks
Minimum 240 hrs
Phar 795 - Patient Care Elective
6 weeks
Minimum 240 hrs
Phar 795 or 797 - Patient Care
Elective or Non Patient Care 6 weeks Minimum 240 hrs
Phar 795 or 797 - Patient Care
Elective or Non Patient Care
6 weeks
Minimum 240 hrs
*Phar 798 MBA Elective
6 weeks
*For PharmD/MBA Students
TOTAL
Minimum 1920 hrs
In aggregate, the required and elective pharmacy experiences must provide the student the
opportunity to interact with a diverse array of patients in terms of age, gender, ethnicity,
socioeconomic background. In addition, student must be exposed to a variety of practice
environments that allow them to experience direct patient care, medication dispensing,
distribution, administration, and system management.

PAGE 9 | 58
Direct Patient Care
• Interacting face-to-face with a diverse population of patients
• Optimizing individual patient drug therapy outcomes
• Consulting with and advising patients on self-care products
• Educating patients on the safe and effective use of prescription and nonprescription
medications, dietary supplements, medical equipment and devices, non-drug therapies,
and complementary and alternative therapies
• Providing pharmacist-delivered education and care to patients of diverse cultural,
economic, geographic, or disease state-related backgrounds
• Delivering evidence-based care through the retrieval, evaluation, and application of
findings from the scientific and clinical literature
• Ensuring continuity of quality care as patients transition between healthcare settings
• Engaging in activities designed to further advance evidence-based therapeutic decision-
making, collaborative interprofessional team-based care, clinical services
entrepreneurship, and systems management
Interprofessional interaction and practice
• Engaging in collaborative patient-care decision-making with members of an
interprofessional healthcare team with an emphasis on face-to-face interactions, but also
incorporating other communications options
• Identifying, evaluating, and communicating to healthcare team members the
appropriateness of the patient’s specific pharmacotherapeutic agents, dosing regimens,
dosage forms, routes of administration, delivery systems, etc.
Medication dispensing, distribution, administration, and systems management
• Appropriately dispensing medications to a diverse population of patients
• Participating in the supervision, oversight, and direction of the medication
dispensing/distribution systems
• Administering medications in a safe and legally acceptable manner
• Managing the medication therapy regimen by monitoring patient outcomes
• Identifying and reporting medication errors and adverse drug reactions
• Engaging in pharmacovigilance activities designed to detect, assess, understand, and
prevent drug-related problems
• Participating in the health system’s formulary process
• Interacting with third-party payers to optimize individual patient drug therapy
• Working competently with the technology associated with various practice settings
workload and financial performance in community/ambulatory care and hospital/health
systems environments
• Contributing actively to discussions on health policy, drug approval processes, legal and
regulatory compliance, patient safety, accreditation, and standards setting
• Participating in the management of systems for storage, preparation, and dispensing of
medications
• Allocating and using key resources and supervising pharmacy technical staff

PAGE 10 | 58
• Participating in purchasing activities
• Participating in the management of medication use systems and applying the systems
approach to medication safety
• Participating in the pharmacy’s planning process and quality improvement program
• Conducting a drug utilization review
• Participating in the management of the use of investigational drug products
• Participating in therapeutic protocol development
• Participating in the management of medical emergencies
• Performing prospective and retrospective financial and clinical outcomes analyses to
support formulary recommendations and therapeutic guideline development
FACULTY APPOINTMENT OF PRECEPTORS
Affiliate Faculty Status
The College of Pharmacy may name an individual as an affiliate faculty member if the individual
contributes to and participates in major functions that achieve the mission of the department or
university. Contributions are under the direction of or in collaboration with a regular faculty
member. Examples include:
• providing instruction for students during their experiential education
• co-advising a graduate student with a regular faculty member
• participating in joint programs with OSU faculty
• providing guest lectures in classes or assisting in outreach activities
• advising a student organization with a regular faculty member
Duration: An individual should be named to the affiliate faculty (as compared to courtesy faculty)
when the relationship with the University is expected to be for one year or less. There are
circumstances, however, which merit issuance of the status for a period longer than one year.
The duration of the status will be specified in a letter of notice generated by the department head
and given to the affiliate faculty member. Affiliate faculty status will automatically terminate after
three years unless renewed by the department head. The status may be extended through the
issuance of a new letter of notice. Affiliate faculty status, however, can be revoked at any time
by the Department Head or the Dean.
Determination of Rank: Affiliate faculty members do not hold rank.
Compensation and Concurrent Appointments: An Affiliate /faculty member may not receive
financial compensation from the University. An Affiliate Faculty member may not hold another
OSU position for which he or she is receiving compensation, nor can an individual be an Affiliate
Faculty member in more than one department.

PAGE 11 | 58
Process to Initiate Affiliate Faculty Status: The Assistant Dean of Experiential Education
identifies the Affiliate Faculty Candidate and through the Office of Experiential Education, sends
letters of invitation and corresponding application form. The request to name an Affiliate Faculty
member is submitted to the Dean for approval. The resulting Affiliate Faculty Status form is to
be sent to the dean, along with a proposed Affiliate Faculty member notice letter (either a Non-
Federal Employee or Federal Employee letter as appropriate).
The Assistant Dean of Experiential Education is responsible for ensuring that the status is
warranted and the individual is qualified within the department. The Office of Experiential
Education will maintain all affiliate records and provide to the Office of Human Resources annually
a roster of Affiliate Faculty appointed by the department.
If the Affiliate Faculty member holds a J-1 Exchange Visitors visa, the department must contact
the Office of International Education at the time of initiating Affiliate Faculty status.
Periodic Review: The Director for Experiential Program reviews the appropriateness of
continuation of Affiliate Faculty status no less than annually. The Director for Experiential Program
is expected to be aware of and hold individuals accountable for activities associated with their
OSU affiliation. Documentation of such a review are maintained in the department file.
Promotion: An Affiliate Faculty member is not eligible for promotion.
Privileges: An Affiliate Faculty member is eligible for a University ID card and associated
privileges, such as joining recreational facilities, purchasing parking permits and using library
services. Inter-library loan services are generally available through the Affiliate Faculty member’s
home institution and/or their local library. Questions about inter-library loan services should be
directed to the Head of Access Services in the Valley Library. An Affiliate Faculty member is not
eligible for staff fee privileges. He or she is not eligible for regular employee benefits, such as
sick and vacation leave or medical, dental, or other employee insurance programs.
Supervisor of Record: An Affiliate Faculty member may contribute to the supervision, direction,
and evaluation of a university employee. They may not serve as supervisor of record or take
actions regularly assigned to a university supervisor.
Sponsored Research: An Affiliate Faculty member is not eligible to be a principal investigator.
Faculty Senate Participation: An Affiliate Faculty member does not have voting privileges for
representation in the OSU Faculty Senate.

PAGE 12 | 58
PRECEPTOR & SITE RECRUITMENT
The Experiential Education Office is led by an Assistant Dean of Experiential Education whose
responsibilities include assisting in the development of experiential curricula and opportunities
that fulfill the educational mission of the professional program. In addition, the Assistant Dean of
Experiential Education is responsible for development, implementation, and oversight of
experiential education across the professional pharmacy program by directing related operations
and strategic planning, budgeting and allocation of resources, and management of staff and
preceptors (affiliate faculty) required to meet educational goals and mission of the University and
the College of Pharmacy.
This illustration depicts the process and the
relationships that the Experiential Education
Office develops and maintains in order to ensure
a high quality experience for both student,
preceptor and institution
Together with the Director of IPPE, 2 program
specialists, and an assessment analyst, the
office works collaboratively with region or
practice specific directors, managers, clinical
coordinators, staff pharmacists to coordinate
preceptor training, experiential site development,
and oversight of placement and supervision of
professional students in introductory and
advanced pharmacy practice experience
programs.
This illustration depicts the general process to
identify sites and preceptors for IPPE and APPE
and the maintenance thereof.

PAGE 13 | 58
QUALITY ASSURANCE
The College is committed to helping sites develop and maintain their respective learning
environments in terms of the appropriateness of their pedagogy as it pertains to the learning
objectives of the course syllabus. There are 2 mechanisms that enable the Experiential Education
Office to collect data that can be used to develop plans to improve the site learning environment
and course structure.
1. Site Visits: The Assistant Dean of Experiential Education and the Director of IPPE are
responsible for assessing the needs of each site and determining the plan for addressing
any opportunities to improve the quality of the learning experience. Visiting with
preceptors at their practice site and/or by virtue of technology e.g. telephone and video
conference are essential activities that enables the Experiential Office to obtain valuable
quantitative and qualitative data about the efficacy of their site’s lesson plan and the
preceptor’s ability to teach. As such, a yearly travel budget is developed by the Dean in
order to support these activities.
Recruitment of a new site or preceptor is accompanied by on site evaluation and training
of all personnel, following approval the Affiliation Agreement, to assure all parties
understand and are prepared to meet the curricular expectations of the College.
After the recruiting process, as outlined in the Preceptor & Site Recruitment section, all
active IPPE and APPE sites will be visited by the appropriate experiential faculty
annually in order to conduct the following:
o Address student related issues
o Assess compliance of site and preceptor with requirements
o Forge a collegial relationship
o Conduct needs assessment of site and preceptor
o Support preceptor development
Preceptors, the Assistant Dean, or Director of IPPE may request additional interim site
visit(s) to address unanticipated changes in preceptor or site; or student specific
concerns that require immediate attention.
Site visits are recorded and tracked in order to ensure that each active IPPE and APPE
sties has been visited at least once within the academic year. These data are shared
with the Assessment committee and Dean as part of the annual experiential report.
2. End of Rotation Site/Preceptor Evaluation: At the conclusion of each IPPE and APPE
experience, each student completes a site/preceptor evaluation form that measures the
ability of the site and preceptor to meet the requirements listed in the previous section.
The data provide the Experiential Education Office a continual process to examine each
site. In addition the data in aggregate form are analyzed and distributed to the
preceptors at the end of the year.

PAGE 14 | 58
PRECEPTOR & SITE REQUIREMENTS
A preceptor is an experienced, competent, pharmacist, scientist, or health care provider who is
selected by the College of Pharmacy and prepared to serve as a role model, teacher, supervisor
and evaluator. Preceptors have the responsibility of ensuring that students have a valuable
educational experience while guiding the student toward competence in providing
compassionate, safe and effective pharmaceutical to patients in a health care setting. Preceptors
are chosen on the basis of their commitment to innovative patient-oriented pharmacy practice,
quality pharmacy education and the desire to be a mentor and teacher. Preceptors are
encouraged to allow students independence and offer guidance and direction when needed.
Teaching students should be a rewarding experience for the preceptor as well as the student.
Qualifications
• Must have a valid Board of Pharmacy preceptor license (if a Pharmacist, MD, Nurse,
PA)
• Must possess a terminal professional degree (if not a pharmacist)
• Must complete preceptor (live or web based) orientation training that introduces the
experiential program in terms of academic requirements, policies and procedures.
• Be able to take responsibility for the professional and legal supervision of the student
during the experience.
• Understands that the relationship with the student is one of teacher-student rather than
employer-employee.
• Understands the goals and objectives of the pharmacy experiential program and its
individual experiential courses.
• Demonstrate the principles of professional ethics
Communication Skills
• Possesses and demonstrates broad knowledge
• Explains the basis for actions and decisions
• Answers learner questions clearly and precisely
• Open to conflicting ideas and opinions
• Connects information to broader concepts
• Communicates clear goals and expectation
• Captures learner’s attention
• Makes learning fun
Assessment Skills
• Accurate assessment of learner's knowledge attitudes and skills
• Uses direct observation of the learner
• Provides effective formative and summative feedback
• Performs fair and thoughtful evaluations

PAGE 15 | 58
Teaching Skills
• Provides effective role modeling
• Demonstrates appropriate professional interactions with patients
• Generates interest in the subject matter
• Presents information with organization and clarity
• Organizes and controls the learning experience
• Balances clinical and teaching responsibilities
• Gives appropriate responsibility to the learner
Motivational Skills
• Emphasizes problem solving
• Translates specific cases into general principles
• Promotes active involvement of the learner
• Demonstrates enjoyment and enthusiasm for patient care and teaching
• Develops a supportive relationship with the learner
Site Requirements
• Able to identify preceptor(s) who will coordinate student activities and provide learning
experiences according to the academic goals set forth by the College.
• Must meet all standards of governmental agencies including the Board of Pharmacy, the
Drug Enforcement Administration and the Food and Drug Administration.
• Must not offer any forms of compensation / remuneration to the student in exchange for
their service during rotations.
• Must promote a high level of professionalism in all areas of practice to convey a
standard of excellence in pharmacy practice.
• Be able to offer a safe learning environment for the students.
• (Patient Care Settings) Offer students interdisciplinary contact with other health
professionals and provide patient-oriented care to a diverse population.
• Allow students to have access to current references sufficient in scope to meet the
needs of patient-oriented pharmacy practice.
• Agree to establish an affiliation agreement with the College of Pharmacy.
• Agree to follow the course syllabus and corresponding manual.

PAGE 16 | 58
PRECEPTOR ROLES
Each preceptor is a teacher in addition to being a practitioner. Most would
agree that being a preceptor is more than merely allowing a student to
shadow you for a few weeks. Precepting takes preparation before the
student arrives and creative thinking in motivating the student to learn.
The American Society of Health-Systems Pharmacists states that that,
“Preceptors must demonstrate a desire and an aptitude for teaching that
includes mastery of four preceptor roles fulfilled when teaching clinical
problem solving (instructing, modeling, coaching, and facilitating).”
Instructing
Direct instruction is the teaching of content that is foundational in nature. Direct instruction fills
in information that is necessary to acquire before skills can be applied or performed. For
example, before a resident can learn to develop a medication regimen for an asthmatic patient,
he or she needs to master information about asthma, potential treatments for asthma, the latest
research and its implications and other pertinent information about asthma and its
treatment. Direct instruction in the form of assigned books, lectures, articles and discussions
help a resident acquire this information. This preceptor role is appropriate at the beginning of a
residency or learning experience when foundational information is needed before assuming a
responsibility.
Modeling
Modeling is demonstrating a skill or process while "thinking out loud" so the resident can
witness the thoughts or problem-solving process of the preceptor, as well as the observable
actions. For example, the resident observes a preceptor develop a medication therapy regimen
and monitoring plan for an asthma patient while the preceptor simultaneously explains the
thought and problem-solving process that would normally go on silently. The resident sees and
prepares to emulate the modeling example(s).
This preceptor role is most appropriate after it has been determined that the resident has the
appropriate amount of background information and is ready to begin to learn to perform a task
or responsibility.
Coaching
Coaching is allowing a resident to perform a skill while being observed by the preceptor, who
provides ongoing feedback during the process. For example, after the resident has acquired the
necessary background information (direct instruction) and observed the preceptor model the
development of a medication therapy regimen and monitoring plan for an asthma patient
(modeling), the preceptor allows the resident to develop a regimen and monitoring plan for

PAGE 17 | 58
another asthma patient and asks the resident to "think out loud" so the preceptor can observe the
resident's thoughts and actions. The preceptor gives feedback during the process.
This preceptor role is appropriate after the resident has had the opportunity to observe modeling
of the process he/she is about to take on but is not yet ready for independence. The coaching
process allows fine tuning of the resident's skills as well as assuring the preceptor that the resident
is ready to move to greater independence. When the preceptor no longer feels the need to
provide corrective feedback to the resident while they perform the task at hand, it is time to move
to the next preceptor role: facilitating.
Facilitating
Facilitating is allowing the resident to perform independently, while the preceptor remains
available if needed and de-briefing with the resident after the fact. Facilitating occurs when the
preceptor has coached the resident and is confident in his/her ability to function
independently. For example, after assigning readings on asthma, modeling and coaching the
development of medication therapy regimens for asthma patients, the preceptor has observed
the resident do this successfully and no longer needs to provide corrective feedback. The
facilitator gives his/her contact information to the resident, sets up an appointment to meet with
him/her later and leaves him/her with the responsibility for the asthma patients. This preceptor
role is appropriate when both the preceptor and resident feel confident of the resident's ability to
function independently. This role normally occurs toward the end of a learning experience and
the residency as a whole.
Once you have reached the facilitating role, be sure to make residents responsible for
progressively more complex patients. If they
are able to treat typical asthma patients,
ensure they can treat asthma patients with
multiple conditions that must also be
considered. It is important to keep
challenging residents at this stage of their
training.
According to the Joint Commission of
Pharmacy Practitioners (JCPP),
“Pharmacists use a patient-centered
approach in collaboration with other
providers on the health care team to
optimize patient health and medication
outcomes.” Preceptor, in developing their
lesson plan, must consider the patient care
model as depicted here.

PAGE 18 | 58
In order to facilitate learning at any site, preceptor must follow the general step below in
sequential order.
LESSON PLAN
College vs. Site specific syllabus/lesson plan
Each rotation (Community, Ambulatory care, Hospital, General Medicine etc.) have their own
College course designation (Phar + course number) and corresponding syllabus.
• Phar 780 Community
• Phar 785 Ambulatory Care
• Phar 790 General Hospital Adult Medicine
• Phar 792 General Hospital
All hospital or community sites are not the same in terms of the services and patient populations.
As such, all rotations tend to offer unique experiences based on their respective environment,
staff, service and patients. The composition of each experience have unique patient care activities
and projects that differ from each site. Because of this variety, the College syllabus is designed
to be competency driven which provides the flexibility to accommodate the variety of practice
sites. There are 5 main competencies categories:
Learning, Patient Care, Problem Solving, Communication, Professionalism
Each competency category is further described by behavioral anchors that can be mapped to
specific activities and projects. In other words, the syllabus does not have a list of specific activities
and projects. Instead, it describes the behavior that supports the competency.

PAGE 19 | 58
It is recommended that each site develop their specific lesson plan that will be an addendum to
the College syllabus. The sections of the syllabus (college and site) are described below.
• General Description of Experience
Describe your rotation in the context of the service(s) that your practice site offers.
•
General Goal
Frame the aim from the students’ point of view, not from the preceptor’s point of view.
Say, “Students will be competent in X, Y, or Z,” rather than “The course will be teach the
student X, Y, or Z.” For example: “The students will be able to demonstrate an organized
approach to providing pharmaceutical care to a patient who presents with altered mental
status.”
•
Learning Objectives
A learning objective is a goal that describes exactly what the student will be able to
demonstrate after successful completion of the curriculum. A well-designed objective
clearly describes the end result of training. Use verbs that capture the highest
appropriate level of competency based on the student year (P1 vs. P4)
Remember
Understand
Apply
Analyze
Evaluate
Create
Learning objectives must reflect the overall purpose of the experience, and effectively
make the goals tangible. The goals should direct the students’ learning objectives, and
creating the objectives clarifies and frames the true purpose of the experience.
Well-written objectives will ensure that the student knows what s/he should be able to do,
under what conditions, and how well it must be done. If objectives are to be meaningful
and to serve as a map for what the preceptor considers important for students to learn,
then these objectives need to be clear, succinct, and measurable. And students must be
accountable for achieving them.
Objectives must be behavior-specific. Use verbs that describe a student behavior that is
observable. To the degree possible, detail the setting or condition for each objective, at
the level of student behavior.
LOWEST LEVEL
HIGHEST LEVEL
P4

PAGE 20 | 58
Example: The student shall be able to…
I. Remember the procedure to properly prepare a medication
II. Understand disease processes on a systematic level
III. Understand predisposing factors, presenting signs and symptoms, and prognosis
IV. Apply principles of pharmacotherapy to specific disease states
V. Analyze therapeutic options based on primary literature, including classic
therapies and new or controversial options
VI. Create a therapeutic plan based on the presentation of a patient and the
presence of multiple concurrent disorders
• Course Content
This section should be written with the intention of providing the student with a roadmap
of the experience. Please refer to the Sample activity section of this manual.
You should include the following:
Weekly Calendar
Topic of the week
Patient care / non-patient care responsibilities
The default learning activity for a typical experience is to have the students care for
patients within the context of the setting i.e. hospital, community, admin office etc.
Decide the best means for how your student can achieve the learning objectives. What
activities are necessary to provide an opportunity for students to gain the desired
competencies?
• Projects
Special projects can address more learning objectives that do not occur reliably within
the course of usual work with a preceptor. Incorporating Evidence-Based Medicine
(EBM) at the point of clinical care, for instance, might occur in the course of usual care of
patients. To ensure that every student gets the same opportunity to practice these skills
up to a specific level of competence, a separate activity could be required. Each student
could be asked to identify a clinical question amenable to primary literature review, and
submit a written report that describes the clinical situation, the search strategy, and an
analysis of the evidence found, with application back to the original situation.
• Student Requirements
Your site-specific syllabus should also include any procedure, protocol and expectation
that are specific requirements of your site. College policies regarding students are
described in the Student Handbook and the Academic and Professional Standards
Handbook. Experiential student policies are outlines in the Student Policy section of this

PAGE 21 | 58
manual. Examples of site specific policies you should include are listed below.
Attire
Attendance
Professional Behavior
Course Schedule of Activities
HIPAA
Safety Training
• Materials and Resources
List any mandatory and recommended reading that must be completed prior and during
the experience. Therapeutic guideline and land mark studies that are pertinent to your
practice should be included.
Example of additional required/optional text:
Pharmacotherapy: A Pathophysiologic Approach. DiPiro, Talbert, Yee, et al, eds. 7th
edition, 2008.
Pharmacotherapy Casebook: A Patient-Focused Approach. Schwinghammer, ed. 7th
edition, 2008.
SAMPLE Acute Care (General Medicine Template)
Pre-rotation work for students
Review relevant therapeutic guidelines
Review Patho/Phys
Review Medical Terminology
Scheduling
Students should enter this rotation with the requisite of completing a hospital rotation. Ideally,
both hospital and gen med rotations should be paired together, within a same institution, in a 12
week block i.e. hospital then gen med.
Goal of Rotation
To provide students with an opportunity to demonstrate knowledge, skills, attitude and
behavior necessary to provide patient-focused pharmaceutical care in a general
medicine/inpatient practice setting resulting in positive therapeutic outcomes for the
patient.

PAGE 22 | 58
Expectations to be addressed during orientation
Weekly goals / Weekly Topics
Attire
Attendance (minimum hours)
Schedule
Communication
Smartphone use
Commitment/Motivation level
Feedback and Evaluation
Activities
Code Procedures, Dosing, Order Verification Simulation, Rounding, Monitoring, Note writing
(care plans), Pharmacotherapy decision making, Adverse drug event / medical error reporting,
Med Rec (intake, discharge), DI (research/write up), Project, Didactic session, Student
Conferences, Journal Club, Staff meetings
Topic
• COPD
• Heart Failure
• Acute Coronary
Syndrome
• AKI
• Hypertension
• AFib
• DVT
• PE
• Stroke
• Diabetes
• General ID
• Pneumonia
• Sepsis
•
SSTI
• Cellulitis
• UTI
• Alcohol Withdrawal
• Cirrhosis
• DKA
• ICU / Surgical
SAMPLE TOPICS FOR DISCUSSION
TIP for the student: Ask your preceptor to discuss (daily or weekly) topics that pertain to
his / her practice site and pharmacy service. Your job is to review any appropriate
literature, didactic notes, and other pertinent references prior to the discussion.
Acute Care
Acute, Chronic Renal and
End State Renal Disease
Adrenal Insufficiency
Alcohol Withdrawal and drug
dependence
Aminoglycoside and
Vancomycin Dosing
Anticoagulation
Arrhythmias
Diabetes
• Contraindication
• Dose
• Direction
• Indication
• Length of therapy
• Therapeutic class
• Pharmacology
• Precautions
Emergency Medicine
Fluids and Electrolytes
MI
National therapeutic
guidelines
Neurology
Oncology
Obstetric Complications
Pain management
Pharmacokinetics
Respiratory Failures
Sepsis Treatment

PAGE 23 | 58
Drugs during pregnancy
Drug Information
• Appropriate use of
resource
• Adverse Drug
Interaction
• Brand / Generic
GI Bleeds
Heart Failure
Hepatic Failure
Infectious Disease
Lab Values
Medication Safety
Mental Health
Seizures
Shock Syndromes
Stroke
Surgical Prophylaxis
Toxicology
Thyroid dysfunction
In-Patient Hospital
Calculations (Pharmaceutics
and Kinetics)
Codes
Drug Information
• Appropriate use of
resource
• Adverse Drug
Interaction
• Brand / Generic
• Contraindication
• Dose
• Direction
• Indication
• Length of therapy
• Therapeutic class
• Pharmacology
• Precautions
Emergency Preparedness
Formulary Management
Joint Commission and 797
Standards
Informatics
Infection Control
Investigational Drugs
Lab Values
Maintenance of patient
medication record
Medication Utilization Review
Medication Reconciliation
National therapeutic guidelines
Patient safety initiatives
Pharmacy dosing monitoring
and dosing protocols
Preparation and distribution
of IV and PO medication
Prioritization of orders
(STAT vs routine)
Process and verification
medication orders
• Indication
• Dose
• Route
• Duration
• Safety Measures
• IV (Compatibility,
Stability,
Administration Rate)
Sterile / Non-Sterile
Compounding
Ambulatory Care / Primary Care / Family Practice
Anticoagulation
Asthma/ COPD
Chemical dependence
Collaborative practice agreements
Common anemias
Coronary artery disease
Diabetes Mellitus
Depression
Heart Failure
Hypertension
Lab Values
National therapeutic guidelines
Peptic Ulcer Disease
Pain Management
Physical assessments
Test and procedures
Urinary Tract Infections
Upper respiratory tract infections
gastrointestinal disturbances

PAGE 24 | 58
Geriatric
Alzheimer’s Disease
Anemia
Angina Pectoris
Arthritis
Bowel/Bladder Incontinence
Congestive Heart Failure
Chronic Obstructive Pulmonary Disease
Drug Information
• Appropriate use of resource
• Adverse Drug Interaction
• Brand / Generic
• Contraindication
• Dose
• Direction
• Indication
• Length of therapy
• Therapeutic class
• Pharmacology
• Precautions
Dementia
Depression
Diabetes Mellitus
Hypertension
Insomnia
Osteoporosis
Pain Management
Pneumonia
Parkinson’s Disease
Community
Calculations
(Pharmaceutical)
Compounding (Sterile / Non-
sterile)
Consultations
Drug preparation and
dispensing
Drug Information
• Appropriate use of
resource
• Adverse Drug
Interaction
• Brand / Generic
• Contraindication
• Dose
• Direction
• Indication
• Length of therapy
• Therapeutic class
• Pharmacology
• Precautions
Immunization Service
Medication Therapy
Management
Management duties
• Inventory
management
• Staffing
• Compliance
• HIPAA and OSHA
requirements
Order entry
Over the counter medications
Patient outreach service
• Health awareness
• Health screenings
• Brown bag
• Antibiotic adherence
Pharmacy Law
Therapy for specific disease
state

PAGE 25 | 58
STUDENT LOG OF PATIENT CARE ACTIVITIES
Patient Care Process
According to the Joint Commission of Pharmacy Practitioners (JCPP),
“Pharmacists use a patient-centered approach in collaboration with other
providers on the health care team to optimize patient health and medication
outcomes.”
Using principles of evidence-based practice pharmacists: Collect, Assess,
Plan, Implement, and Follow-up: Monitor and Evaluate
Students are to complete 15 Patient Care Activity Logs per each 6 week
rotation if applicable.
PATIENT CARE ACTIVITY LOG
Student: _______________________________________________________ Date: ______________________
Site: _______________________________________ Site Type: Choose an item. ____________________
Preceptor: ______________________________________________
Patient Gender: Choose an item. Patient Age Choose an item. Population Type: Choose an item.
Disease State(s): ______________________________ Medication(s) Involved: _________________________
Collect
The pharmacist assures the collection of the necessary subjective and objective information about the patient in
order to understand the relevant medical/medication history and clinical status of the patient.
_____ Physical assessment _____ Medication reconciliation
_____ Chart review _____ Other ____________________________
_____ Medical history review
Assess
The pharmacist assesses the information collected and analyzes the clinical effects of the patient’s therapy in the
context of the patient’s overall health goals in order to identify and prioritize problems and achieve optimal care.
Select all that apply.
Order Clarification:
_____ Non-formulary medication
prescribed
_____ Illegible writing
_____ Product unavailable
Drug Product Selection:
_____ Medication needed
but
not prescribed
_____ Prescribed medicat
ion
Drug Regimen:
_____ Wrong dose/route/form
_____ Inappropriate schedule
or duration
_____ Medication not indicated
for condition
_____ More effective/safer
medication available
Contraindication:
Adverse Drug Reaction:
_____ Toxicity
_____ Allergic reaction
_____ Side effect
Inappropriate Compliance:
_____ Underuse
_____ Overuse
_____ Abuse
_____ Patient prefers not to

PAGE 26 | 58
not needed
_____ Medication duplication
_____ Cost of therapy
_____ Safety or efficacy
_____ Ease of use
_____ Age
_____ Disease/condition
_____ Medication interaction
_____ Pregnancy/nursing
take/cannot afford
Referral Needed:
_____ Patient condition warrants
medical attention
_____ Lab value warrants
attention
Plan
The pharmacist develops an individualized patient-centered care plan, in collaboration with other health care
professionals and the patient or caregiver that is evidence-based and cost-effective.
_____ Initiate new therapy/add medication (Rx)
_____ Suggest OTC therapy
_____ Discontinue therapy
_____ Provide medication info/education
_____ Change:
Medication
Dose
Dosage Form
Regimen/schedule/duration
_____ Patient referred to PCP or Specialist
_____ Patient monitoring initiated
_____ Recommend therapeutic drug monitoring
_____ Recommend lab test
_____ Continue unchanged
_____ Payer/processor contacted
_____ Patient counsel/consultation
_____ Other ________________________________
Implement
The pharmacist implements the care plan in collaboration with other health care professionals and the patient or
caregiver.
_____ Recommendation accepted _____ Recommendation accepted w/ modification
_____ Recommendation not accepted _____ Other ______________________________
Follow-up: Monitor and Evaluate / Outcome
The pharmacist monitors and evaluates the effectiveness of the care plan and modifies the plan in collaboration with
other health care professionals and the patient or caregiver is needed.
Please describe the outcome and follow up.

PAGE 27 | 58
PROVIDING FEEDBACK
Feedback
An effective preceptor not only has a positive attitude and self-confidence, but also has good
assessment skills. As such, preceptors need to pay particular attention to the student’s learning
style and examine their teaching style’s effectiveness relative to the curricular goals. Preceptors
should provide adequate feedback, which is required for professional growth and improvement.
Providing general positive accolades is fun and easy to give however, providing constructive,
specific and timely feedback can be difficult especially if the goals of the rotation are not clearly
communicated. It should never be a surprise to any student at the conclusion of the experience
that he/she is not going to pass. Well-timed and appropriate feedback given throughout the
experience gives student the opportunity to improve before it is too late.
TIP for the student: Do not take feedback as a personal attack and let your emotions
distract you from listening to its merits.
It is important for preceptors and students to remember that feedback should be detailed and
specific. A compliment such as “You’re doing a great job” is too general. Students gain the most
benefit from feedback that is descriptive and not subjective. Evaluation forms can serve as an
objective platform to provide students with both positive and negative feedback. While evaluations
still depend on the assessment of the preceptor, the evaluation form tends to separate opinions
from the constructive feedback. Using the form can depersonalize negative feedback so that the
student does not feel threatened.
Types of feedback
TIP for the student: Ask your preceptor to provide you with both types of feedback
during the course of the rotation. Use the evaluation form and the specific goals of the
course to frame the conversations.
Formative (On the go)
• Ongoing, timely, and specific feedback provided to learners throughout the
experiential component.
Summative (Mid-point and Final)
• Formal evaluative process typically at mid- and final evaluations that captures the
overall picture.
• Summarizes the learner’s performance based on a rubric.
Characteristics of effective feedback
• On-going process
• Non-judgmental
• Corrective
• Objective
• Criterion based
• Specific and thoughtful

PAGE 28 | 58
Learning Stages
The development of knowledge, skill, attitude and behavior of students vary depending on their
current rank, pharmacy experience and overall professional maturity. The illustration below
shows the progression of goals (building blocks vs higher function) according to the student’s
rank.
TIP for the student: As a P4 student, you will be asked to recall basic pharmacy
knowledge such as general drug information, therapeutic guidelines, pharmacokinetic
principles, pathophysiology and common disease state presentations. In order to better
prepare for your rotation, you should understand the patient population and the type of
service(s) that your site provides i.e. acute vs. ambulatory and cardiology vs. infectious
disease etc. This will help you focus your studies prior and during the rotation.
Many learning models and theories speculate that in the process of skill development, students
pass through levels of proficiency: novice, advanced beginner, competent, proficient and expert.
Stage 1 – Novice (P1)
Beginners have had no experience of the situations in which they are expected to perform.
Novices are taught rules and answers to common problems to help them perform. The rules and
answers are context-free and independent of specific cases therefore the novice is extremely
limited in terms of how they are able to perform in the practice site. In other words, novices have
no life experience in the application of rules. "Just tell me what I need to do and I'll do it."
TIP: P1 students are truly novices. They lack the experience and knowledge to solve
common problems in the pharmacy often needing to “look up” answers. The goal
should be to provide the student with enough experience and repletion so that they will
be able to comprehend the application of a particular knowledge or skill.

PAGE 29 | 58
Stage 2 – Advanced Beginner (P1-P3)
Advanced beginners are those who can demonstrate marginally acceptable performance. They
have coped with enough real and recurring meaningful situational problems. In order to solve
these problems, the student is required to have prior experience in actual situations for
recognition. These students may have the answers in their memory but sometimes have
difficulty accessing it at the time of the situation. A little prodding will eventually help this type of
student come to the correct answer. However, answers remain to be linear and complex
problem with ambiguous answers are still very difficult to process.
Stage 3 – Competent (P3-P4)
The competent student is typified by one who has been in the same or similar situations for two
or three years. There is conscious, deliberate planning that is characteristic of this skill level
helps achieve efficiency and organization. The competent student still lacks the speed and
flexibility of the proficient student but does have a feeling of mastery and the ability to cope with
and manage the many contingencies of pharmacy practice. The competent person does not yet
have enough experience to recognize a situation in terms of an overall picture or in terms of
which aspects are most salient, most important.
TIP: Being exposed to and solving as many “real life” problems is essential to moving
from the “competent” stage to the “proficient” stage. As such, each student must
proactive in seeking these types of opportunities. Students who do not ask to be
challenged will typically remain in stage 3. Use the sample activities section to help you
and your preceptors identify appropriate activities that will help color your overall
experience.
Stage 4 – Proficient (P4)
Proficient student understands a situation as a whole because they perceive its meaning in
terms of long-term goals and therefore has context. This type of student is able to use past
experiences to expect how he or she will respond to a given situation. In addition, he or she can
now recognize when the expected normal picture does not materialize. He or she is able to
evaluate and analyze potential solution with the use of guideline, rules or maxims. The student's
decision making is less labored because he or she is guided by perspective and past
experiences.
TIP: P4 students by blocks 7-9 should be able to perform at the proficient level in terms
of solving common pharmacotheraphy and/ or pharmacy operational related problems.
Preceptors are aware of the progression of novice to a proficient learner. You should be
aware of your progression against this set of definitions to make sure that you are not
functioning below expectation.
Stage 5 – Expert (Pharmacist)
The expert performer no longer relies on an analytic principle (rule, guideline, maxims) to
connect his or her understanding of the situation to an appropriate action. The expert student,
with an enormous background of experience, now has an intuitive grasp of each situation and is
able to recognize the root cause of the problem without wasteful consideration. The expert
operates from a deep understanding of the total situation. His or her performance becomes fluid
and flexible and highly proficient.

PAGE 30 | 58
GRADING
Grading for all experiential courses is a “pass/no pass” system and is determined by the Assistant
Dean of Experiential Education in collaboration with the supervising preceptor. This decision is
derived from the preceptor evaluation / feedback data from the student evaluation form. The role
of the preceptor is to provide students both formative and summative feedback by using the rubric
(grading scale) outlined on the student evaluation form. The summative feedback is documented
on the midpoint and final evaluation form which is an online process. The College provides
evaluation forms for each type of rotation which can be accessed through the E*Value system
and each Preceptor is required to complete both the midpoint (3
RD
Friday) and final (6
th
Friday).
Students are required to pass all rotations in order to graduate. Information regarding
consequences of a non-passing grade may be found in the Student Handbook under “Academic
and Professional Standards”.
TIP: The formal evaluation process (a.k.a. summative feedback or Final Evaluation) is an
important process because it provides the College your official grade. However,
understanding the “gaps” in knowledge, skill, attitude and behavior as it pertains to what
is expected of a P4 student is equally as important as the grade. Receiving a grade without
knowing your strengths and weaknesses is not an effective use of the evaluation form.
Grading Rubric
Exceptional (4)
· Consistently
performs above
expected level.
Performance can be
described as
impressive or
exceptional.
· After initial
instruction, the
student can
independently
complete all basic
tasks and most
complex tasks.
· Performs at a level
beyond that of an
entry-level
practitioner.
Competent (3)
· Meets expectations
and performs consistently
at expected level.
Performance possesses
strengths with room for
improvement in a few
areas.
· After initial instruction,
the student
independently completes
all basic and routine
tasks and requires limited
prompting or guidance to
complete most complex
tasks.
· Requires little to no
intervention.
Demonstrates near-
readiness for practice in
early APPEs and
performs at the level of
an entry-level practitioner
in later APPEs.
Marginal (2)
· Meets expectations
and performs
consistently at
expected level in only
some areas. Several
performance areas
have room for
improvement.
· After initial
instruction, the student
independently
completes most basic
and routine tasks. The
student requires
guidance to complete
most complex tasks.
· Requires occasional
intervention.
Demonstrates one
performance deficit in
early APPEs and near-
readiness for practice
in later APPEs.
Deficient (1)
· Performs well below
baseline expectations.
Performance
demonstrates worrisome
deficits.
· Student is unable to
satisfactorily and
consistently complete
most basic and routine
tasks despite directed and
repeated guidance. The
preceptor or other
pharmacy personnel must
often complete the tasks.
· Requires repeated
intervention.
Demonstrates multiple
performance deficits in
early APPEs and is clearly
not ready for independent
practice in later APPEs.

PAGE 31 | 58
There are 5 competency categories, Learner, Patient Care, Problem Solving, Professionalism,
and Communication. On the evaluation form, the student’s performance will be rated with the
above scale during midpoint and final. STUDENTS MUST RECEIVE A “2” OR HIGHER IN
EACH COMPETENCY DURING THE FINAL EVALUATION IN ORDER TO RECEIVE A
PASSING GRADE AT THE CONCLUSION OF THE EXPERIENCE.
Students are responsible for making sure that the evaluation is completed by the preceptor. This
is an online process which is facilitated by the E*Value system. All evaluations must be completed
by the last day of the rotation.

PAGE 32 | 58
FINAL APPE ASSESSMENT FORM
Instructions
The final assessment for the APPE program is a pass / no pass system. These assessments
should be completed by the assigned preceptor at midpoint (end of week three) and final
evaluation (end of week six) during each scheduled rotation experience. These evaluations
should be submitted using E*Value. Each student pharmacist will be assessed under the
following outcome categories.
Learning, Patient Care, Problem Solving, Communication, Professionalism
Assessment
All student pharmacists will be assessed using the following four (4) point performance rating
scale for each of the ten (10) global learning objectives that apply to the rotation experience. A
rubric describing each achievement level of performance is provided to assist the preceptor in
determining the rating that best represents the student pharmacist’s performance for each
applicable outcome. The performance rating must fall between the range of 1 and 4. This rating
scale is based on increasing performance levels such that the student pharmacist achieves
competency, relative to a graduating student just entering practice, by the end of the APPE
programmatic year. This means that as the programmatic year progresses, higher
expectations of achievement should be expected by the preceptor and reflected in the
assessment ratings and comments.
Preceptor Comments
Once the performance rating is selected, please use the comment section to provide additional
feedback regarding the student pharmacist’s strengths and achievements as well as areas of
improvement and continued development. Comments will be REQUIRED if the entered score is
2 or lower to provide specific examples of areas needing improvement. Each student
pharmacists will be assigned a final assessment of either PASS or NO PASS which will
originate directly from this evaluation. Once the final assessment is submitted by the preceptor,
the College (through the Assistant Dean for Experiential Education) will be responsible for
validating the assessment. To successfully pass each rotation, the student pharmacist must
receive a final score of 2 or higher on the final assessment in ALL learning objectives that apply
to each specific rotation experience. Receiving a rating of 1 in any outcome equates to a failed
rotation. If a preceptor does select a rating of 1, E-Value will request the preceptor validate the
final score prior to submitting the evaluation. For non-patient care rotations the preceptor may
submit a rating of N/A for the patient care outcomes. All other outcomes are applicable. The

PAGE 33 | 58
N/A performance rating does not contribute to the total available points and will not negatively
impact the final score. In addition, students may be evaluated on rotation specific objectives
beyond the established learning objectives which can be integrated in the evaluation as an
additional learning objective.
I. LEARNING
Demonstrates learning. Develops, integrates, and applies knowledge and skills appropriately
to situations encountered in the practice setting.
Exceptional (4) Competent (3) Marginal (2) Deficient (1)
Examples of performance competence may include:
• Verbally displaying relevant knowledge from the pharmaceutical,
social/behavioral/administrative, and clinical sciences.
• Retaining and applying relevant information from current and prior experiences.
• Self-identifying learning needs and appropriately correcting or enhancing knowledge and
skills.
• Identifying and critically analyzing literature to support decision-making.
• Describing how population-based care principles influence creation of practice guidelines
and care of individual patients.
Strengths and Achievements regarding this area:
Areas for Improvement regarding this area:

PAGE 34 | 58
II. PATIENT CARE
Collects data. Accurately gathers and organizes all relevant subjective and objective
information (e.g., comprehensive medication list, allergies, medical history, pertinent
lab/physical assessment findings, and social determinants of health).
Exceptional (4) Competent (3) Marginal (2) Deficient (1) Not Applicable (N/A)
Examples of patient data collection competence may include:
• Conducting patient/caregiver interviews using an organized structure and
comprehensible wording.
• Efficiently reviewing electronic chart/health records.
• Gathering pertinent information from other health professionals.
•
Performing/reviewing physical assessment findings.
Assesses data. Evaluates drug therapy regimen for appropriateness in achieving optimal
patient outcomes (considering safety, efficacy, adherence). Appropriately prioritizes potential or
current pharmacotherapy problems.
Exceptional (4) Competent (3) Marginal (2) Deficient (1) Not Applicable (N/A)
Examples of patient data assessment and prioritization competence may include:
• Interpreting and verifying prescriptions for accuracy and appropriateness.
• Performing comprehensive medication review.
• Performing medication reconciliation.
•
Performing accurate pharmacy calculations.
Development, implementation, and monitoring of patient care plan (JCPP Plan, Implement,
Monitor) Develops or revises, implements, and evaluates a patient-centered care plan to
optimize drug therapy and clinical outcome.
Exceptional (4) Competent (3) Marginal (2) Deficient (1) Not Applicable (N/A)
Examples of plan development and implementation competence may include:
• Using clinical guidelines, primary literature, and information from other care providers.
• Incorporating patient beliefs, preferences, and living environment constraints to represent
the patient’s best interests.
• Identifying, incorporating, and implementing health and wellness improvement strategies.
• Considering continuity of care across settings.
• Providing patient education and addressing patient questions and concerns about therapy.
• Monitoring patient response to therapy and success in achieving desired therapeutic goals.
•
Appropriately documenting patient interventions and other patient care activities

PAGE 35 | 58
Strengths and Achievements regarding this area:
Areas for Improvement regarding this area:
III. PROBLEM SOLVING
Demonstrating critical thinking and innovation during the problem-solving process.
Critical thinking and innovation are intellectually disciplined processes of skillfully evaluating
information and designing a solution that incorporates new ideas or methods, when appropriate.
Exceptional (4) Competent (3) Marginal (2) Deficient (1)
Examples of problem-solving competency may include:
• Identifying and collecting relevant information.
• Analyzing, evaluating, interpreting, and prioritizing information using logical arguments
and incorporating multiple perspectives.
• Synthesizing and implementing the most viable course of action/solution.
•
Adapting when new or changing situations arise.
Performing management activities that prevent or address problems in a systematic
manner. Effectively participates in the practice/operations management activities using human,
financial, technological, and physical resources to optimize the safety and efficacy of medication
use systems.
Exceptional (4) Competent (3) Marginal (2) Deficient (1)
Examples of management competency may include:
• Applying pharmacy law, ethics, and administrative policies and procedures appropriately.
• Participating in the oversight of the preparation, dispensing, distribution, and
administration of medication by applying professional standards.

PAGE 36 | 58
•
Using technology to optimize efficiency and patient safety.
• Participating in the management of human resources, marketing, billing, quality
assurance processes, or inventory control.
•
Demonstrating leadership when needed.
Strengths and Achievements regarding this area:
Areas for Improvement regarding this area:
IV. COMMUNICATION
Effectively communicates information verbally, non-verbally, and in written form when
interacting with an individual, group, or organization.
Exceptional (4) Competent (3) Marginal (2) Deficient (1)
Examples of verbal and written communication competence may include:
• Listening to others with attention.
• Demonstrating interest, empathy, and respect during conversation
• Communicating articulately, concisely, tactfully, and confidently.
• Providing relevant information appropriately targeted to the audience.
• Writing effective patient care notes and other documents at a level appropriate to the
reader.
• Creating documents that have a clear purpose, appropriate content, logical organization,
correct mechanics, and appropriately cite and reference resources.
Effectively interacts with other members of the health care team or organization.
Exceptional (4) Competent (3) Marginal (2) Deficient (1)

PAGE 37 | 58
Examples of team competence may include:
• Working collaboratively with the interprofessional and pharmacy team.
• Engaging in shared decision making, rather than just making a recommendation to the
team.
• Displaying a willingness to speak up, even against a perceived power gradient
• Identifying and helping to resolve areas of conflict between team members.
• Assessing effectiveness of team performance.
• Adapting one’s role to make the team more effective.
Strengths and Achievements regarding this area:
Areas for Improvement regarding this area:
V. PROFESSIONALISM
Self-Awareness Examines and reflects on personal knowledge, skills, abilities, beliefs, biases,
motivation, and emotions that could enhance or limit personal and professional growth.
Exceptional (4) Competent (3) Marginal (2) Deficient (1)
Examples of self-awareness competence may include:
• Recognizing and accepting responsibility for own work, actions, and consequences.
• Maintaining motivation, attention, and interest during learning and work-related activities.
• Graciously receiving feedback and seeking to improve performance.
• Displaying appropriate humility, confidence, initiative, persistence, and tolerance for
ambiguity.
Professional Behavior Exhibits appropriate behaviors and values that are consistent with the
trust given to the profession by patients, other healthcare providers, and society.

PAGE 38 | 58
Exceptional (4) Competent (3) Marginal (2) Deficient (1)
Examples of professional behavior competence may include:
• Demonstrating altruism, integrity, trustworthiness, flexibility, and respect in all
interactions.
• Displaying preparation, initiative, and accountability consistent with a commitment to
excellence.
• Providing care in a manner that is legal, ethical, and compassionate.
• Maintaining standards for professional conduct (e.g., attire, language, punctuality,
attendance, commitment, confidentiality)
• Demonstrating the skills and attitudes necessary for self-directed, life-long learning.
•
Gracefully managing stressful situations.
Strengths and Achievements regarding this area:
Areas for Improvement regarding this area:
FINAL GRADE
PASS
NO PASS

PAGE 40 | 58
From the ad hoc evaluation page, you will have different options for the type of feedback you
would like to provide. Once you have filled out each cell you can follow the prompts until
completion.
APPE STUDENT POLICIES
All students must comply with the following requirements of the College of Pharmacy before
entering patient care areas.
Standard of Academic and Professional Conduct
All of these standards, as outlined in the Student Handbook, are expected of each student during
each rotation. Students who fail to adhere to these standards and the following guidelines are
subject to disciplinary action and removal from the site which in turn will jeopardize the student's
progress and completion of the APPE curriculum.
License, Certifications, Training (see OSU Student Handbook for complete policy)
Must adhere to the Oregon Health Authority’s policy on Health Profession Student Clinical
Training Standards: https://www.oregon.gov/oha/HPA/HP/Pages/sct.aspx
• Blood borne Pathogens Training
• CPR certification
• Complete Annual Tb Monitoring
• Health Insurance
• HIPPA Training
• Immunization policy for the College of Pharmacy and the policy for each practice site
• Pass background checks from the College (OSU and OHSU)
• Pass drug testing
• Professional Liability Insurance

PAGE 41 | 58
• Valid/Active OR Intern License and other appropriate State Pharmacy Intern License
Remuneration
Students are not allowed to accept any forms of compensation from the site / preceptor in
exchange for their service during rotations. Rotations hours that are paid will not satisfy any
curricular objectives and requirements. Students who violate this policy will be immediately
removed from the rotation and will be referred to the Academic and Professional Standards
Committee.
Confidentiality, Diversity, and Harassment Training
All pharmacy students receive training on issues relating to confidentiality (including Health
Insurance Portability and Accountability Act training), diversity, and harassment. These training
sessions assure that student, staff, faculty and patient information is handled appropriately and
that students, staff, faculty and patients find an environment that is welcoming and respectful.
Training sessions offered by the College occur early in the first professional year and again before
pharmacy students move to the OHSU campus, and they are mandatory. Individual experiential
sites may have additional training requirements.
Identification
Pharm.D. students are required to wear a nametag while representing the College at any
experiential site or event. The nametag must be approved by the College and identify them as an
OSU/OHSU student. Students may not use nametags from places of employment while
completing clerkship experiences.
Attendance Policy
1. Students are expected to complete a minimum of 40 hours per week at their APPE site as
described in the syllabus of each rotation i.e. students must average a minimum of 40 hours
per week. They are expected to be at the site for all regularly scheduled activities associated
with the course and this may include weekend and evening commitments.
2. Students must adhere to any site policies highlighted by the preceptor or authorized personnel.
3. Students must notify the preceptor of tardiness and/or absence as soon as possible. If the
preceptor is unavailable then other responsible (site) personnel should then be contacted. The
student must also notify the Assistant Dean of Experiential Education of all absences.
4. Any hours missed must be completed at a later date within the scheduled duration of
the rotation, to be determined by the preceptor and, if needed, the Assistant Dean of
Experiential Education. The student must notify the Office of Pharmacy Practice Experience
Program of schedules arranged by the preceptor for the completion of missed hours.

PAGE 42 | 58
5. Any extraordinary circumstances or extended illnesses will be reviewed and assessed by the
preceptor and the Assistant Dean of Experiential Education with the supervising preceptor.
6. Unexcused absences totaling more than 3 days or 24 contact hours over the course of any
rotation will result in an automatic grade of No-Pass for that rotation and student will be
assigned to and required to perform a similar rotation at a later date as determined by the
College.
7. In addition to illness or personal emergencies, students may be granted a total of three (3)
excused days to be used for the purpose of attending professional meetings not associated
with their individual rotations. Student must obtain permission from their preceptors to utilize
one or more of these days and must also notify the Assistant Dean of Experiential Education
of this intention. The preceptor will determine how this time will be made up in order to satisfy
rotation expectations.
8. Students will not be expected to attend their rotations during OSU recognized holidays.
Rotations follow the academic calendar, which is based on a quarter system and the following
schedule reflects holidays and vacation days recognized by OSU/OHSU College of Pharmacy:
Independence Day, Labor Day, Thanksgiving Day, Christmas Day, New Year’s Day,
Martin Luther King Day, Memorial Day
NOTE: STUDENTS MUST STILL BE ABLE TO MEET THE 40HR PER WEEK REQUIREMENT
9. Student will not be excused from their rotations for work e.g. paid internships.
10. Students are solely responsible for accurately maintaining their Internship Hours Log in
E*Value.
Changing a Rotation
Changing rotations sites and preceptors is a normal occurrence during the APPE year due to
mostly unpredictable situations such as change in staff (promotion, dismissal, change in job duties
etc). During these types of scenarios, the Experiential Office will find a replacement rotation that
will allow affected student to progress towards graduation without delay.
Student may petition the Experiential Office to change one elective by first notifying the Assistant
Dean of Experiential Education. If approved to proceed with the change, the student must then
gain the approval from both the previously scheduled and new preceptor. This entire process is
facilitated by the Change in Rotation Request Form
.
General Liability Insurance
Students enrolled in College of Pharmacy experiential courses are provided with general
insurance ($1,000,000 per incident; $3,000,000 total per year), purchased by the College of
Pharmacy. However, it also required that students purchase their own, additional professional
liability insurance.

PAGE 43 | 58
Student Health and Health Insurance
Pharmacy students are exposed to risks in experiential practice sites and on the OHSU medical
campus. Additionally, many experiential practice sites require students to have adequate health
insurance. Therefore, all students are required to purchase the OHSU student health insurance
plan (SHIP) which covers students for an entire year. Information about the 19/20 SHIP can be
found here:
http://www.ohsu.edu/xd/education/student-services/joseph-trainer-health-wellness-
center/insurance-plan/index.cfm.
A student may be able to request that another health insurance plan, such as the plan provided
by OSU Student Health Services, a spouse’s employer etc., substitute for the OHSU plan.
Students must follow all OHSU procedures for requesting such a substitution. Waivers are only
granted to students who have another plan that is comparable in coverage.
Waivers must be renewed annually. Waiver procedures, deadlines, and requirements are
described in detail on the OHSU Student Health Services website:
http://www.ohsu.edu/xd/education/student-services/joseph-trainer-health-wellness-
center/insurance-plan/student-insurance-waiver.cfm.
Guidelines for Exposure Management/Medical Services
Any potential exposure to any infectious agents should be discussed with the Experiential Office
and OSU Student Service as soon as possible whether or not the preceptor feels that the
exposure was real and significant. The student should seek immediate medical evaluation and
care with employee health at the site or, if directed, with the nearest urgent care/ED, health care
facility or personal physician of choice. The preceptor should provide guidance to the student
regarding this.
If body fluid exposure / needle stick occurs:
• Immediately remove gloves, clothing soaked with blood or other high-risk body fluids.
• Wash any potentially exposed site with antiseptic soap and water, unless material entered
the eyes. In this case, the eyes should be flushed constantly for 15 minutes.
• Contact the OSU Experiential Programs and Student Service.
• Most institutions will want the student to fill out an Incident Report or Accident Report form.
These forms should not be filled out or signed until Advanced Practice Experience
Coordinator has consulted with Risk Management.
• If a significant exposure is determined to have occurred, the Experiential Office and Student
Service will work closely with the student and site to determine the best course of action. If
the possibility exists that the student is at any risk for contracting HIV or Hepatitis B or C,
the student will receive appropriate counseling and education as well as confidential
laboratory work.
PAGE 44 | 58
• If the Experiential Office and Student Service cannot be reached students should first be
seen by their preferred medical insurance provider. Students who do not carry personal
medical insurance but have paid for the mandatory Health Fee are entitled to services at:
U of O- Eugene, OSU-Corvallis, PSU- Portland, Eastern Oregon State College- La Grande,
Southern Oregon- Ashland, OIT – K-Falls.
Student and Patient Safety Policies
Disclosure of Criminal Activity
Pharm.D. students must immediately disclose any encounters with law enforcement to a member
of the Office of Student Services or Executive Associate Dean. Encounters with law enforcement
include criminal activity, alleged criminal activity, citations, arrests, or any other interactions that
result from student behavior, or circumstances in which law enforcement intervenes and the
student is present. The disclosure will be referred to the Academic and Professional Standards
committee, but the Executive Associate Dean may determine that immediate removal from
practice sites or Suspension is appropriate until circumstances surrounding the incident can be
clarified. Failure to disclose may result in Dismissal from the College.
Disclosure of Board of Pharmacy Action
Pharm.D. students must also immediately disclose any action taken against them by a Board of
Pharmacy, including but not limited to warning, probation, and revocation of licensure. Failure to
do so could result in Dismissal from the Pharm.D. Program.
OREGON BOARD OF PHARMACY INTERN REGULATIONS
DIVISION 31 INTERNSHIP REGULATIONS
http://arcweb.sos.state.or.us/pages/rules/oars_800/oar_855/855_031.html
Definitions
(1) An "intern" means any person who:
(a) Is enrolled in a course of study and is in good academic standing at a school or college of
pharmacy that is approved by the Oregon Board of Pharmacy (Board); or
(b) Is a graduate of a school or college of pharmacy that is approved by the Board; or
(c) Is a foreign pharmacy graduate and holds a certificate from the Foreign Pharmacy Graduate
Equivalency Committee (FPGEC); and
(d) Is licensed with the Board as an intern.
(2) A "preceptor" means a pharmacist or a person licensed by the Board to supervise the
internship training of an intern.
(3) "Internship" means a professional experiential program or work experience.
(a) "Traditional Pharmacy-practice Internship (TPI)" means experience toward achieving
competency in the practice of pharmacy for which no academic credit is granted to the intern.
(b) "School-based Rotational Internship (SRI)" means experience toward achieving competency
in the practice of pharmacy in programs developed and administered by a school of pharmacy.

PAGE 45 | 58
(c) "Other Internship" means experience toward achieving competency in the practice of
pharmacy, other than in an internship as defined in (a) or (b), in a program approved by a school
of pharmacy or the Board.
(4) “School of pharmacy”: In this division of rules, “school of pharmacy” means a school or college
of pharmacy that is approved by the Board.
855-031-0010
Intern License Application
(1) Applications for licensure as an intern may be obtained from the Board office or from the Board
web site at www.pharmacy.state.or.us.
(a) Failure to completely, accurately and honestly answer all questions on the application form for
licensure or renewal of licensure is grounds for discipline;
(b) Failure to disclose any arrest for a felony or misdemeanor, or any indictment for a felony may
result in denial of the application.
(2) The Board may issue a license to a qualified intern after the receipt of:
(a) A completed application;
(b) Payment of the fee prescribed in OAR 855-110-0005;
(c) A current, passport regulation size photograph (full front, head to shoulders);
(d) Any fingerprint card or other documentation required by the Board to conduct a criminal
background check; and
(e) Confirmation from a school of pharmacy that the applicant is enrolled in a course of study,
except for foreign pharmacy graduates who must:
(A) Provide a copy of a valid visa permitting full-time employment;
(B) Provide the original certificate issued by the Foreign Pharmacy Graduate Equivalency
Examination Committee; and
(C) Provide evidence that they have passed the Test of English as a Foreign Language (TOEFL)
Internet-based Test (IBT) with a minimum score of 26 in Speaking, 21 in Reading, 18 in Listening
and 24 in Writing, however scores will be accepted until June 30, 2010 from candidates who have
already passed or are scheduled to take the TOEFL and the Test of Spoken English (TSE).
(3) The Board may issue an intern license after processing the application, however unless the
applicant is a foreign graduate or an applicant for licensure by reciprocity, it is not valid until the
intern has started a course of study. For licenses issued after May 1, 2010, the initial license is
valid until the last day of November following the second anniversary of issue unless terminated
automatically by any one of the following events. Renewed licenses are valid for two years unless
terminated automatically by any one of the following events:
(a) Licensure to practice pharmacy is granted in any state; or
(b) The licensee, other than a foreign pharmacy graduate or an applicant for licensure by
reciprocity, fails to maintain enrollment or active registration in a pharmacy degree program for a
period greater than one year; or
(c) The licensee, other than a foreign pharmacy graduate or an applicant for licensure by
reciprocity, has been graduated from a school of pharmacy for 12 months;
(d) The intern is dismissed, terminated or expelled by the school of pharmacy, or withdraws from
the program.
(4) An intern must surrender their license to the Board within 30 days of one of the above events.
(5) Notwithstanding the requirements of section (3) above, upon written request the Board may

PAGE 46 | 58
waive any of the requirements of this rule if a waiver will further public health and safety. A waiver
granted under this section shall only be effective when it is issued in writing.
855-031-0020
Intern Requirements and Responsibilities
(1) A licensed intern may practice in any one or a combination of the following approved internship
experience areas:
(a) Traditional Pharmacy-practice Internship (TPI): an intern may not work in a TPI until after
satisfactorily completing the first academic year in a school of pharmacy. An intern working in a
TPI must be supervised by a licensed pharmacist or pharmacist preceptor;
(b) School-based Rotational Internship (SRI): an intern must be supervised by a licensed
pharmacist or other person approved by a school of pharmacy to obtain credit for SRI hours;
(c) Other Internship.
(2) An intern may not work more than 48 hours per week in SRIs and must comply with all
supervision and ratio requirements.
(3) An intern must verify that their preceptor is currently licensed with the Board.
(4) An intern may not work in the practice of pharmacy unless supervised by a licensed
pharmacist, except when an intern is working in a federal facility, however, to obtain credit for SRI
experience in a federal facility located in Oregon, the intern must be licensed with the Board.
(5) An intern who is working in a pharmacy or other place of business must conspicuously display
their intern license in the pharmacy or place of business and must be clearly identified as an intern
at all times.
(6) An intern may perform only the duties listed in Division 25 of this Chapter before completion
of the first academic year in a school of pharmacy.
(7) An intern may, after successful completion of their first academic year, perform the duties of
an intern listed in Division 019 of this Chapter, but only after successful completion of coursework
corresponding to those duties at their school of pharmacy and only with the permission of their
supervising pharmacist.
(8) An intern is responsible for his or her own actions and must comply with all Board regulations.
(9) An intern must notify the Board within 15 days of any change in their academic status that
might affect their eligibility to work as an intern.
(10) An intern must notify the Board in writing within 15 days of a change in permanent residence
and TPI site.
(11) An intern must report to the Board within 10 days if they are:
(a) Convicted of a misdemeanor or a felony; or
(b) Arrested for a felony.
(12) An intern who has reasonable cause to believe that another licensee (of the Board or any
other Health Professional Regulatory Board) has engaged in prohibited or unprofessional conduct
as these terms are defined in OAR 855-006-0005, must report that conduct to the board
responsible for the licensee who is believed to have engaged in the conduct. The intern shall
report the conduct without undue delay, but in no event later than 10 working days after the intern
learns of the conduct unless federal laws relating to confidentiality or the protection of health
information prohibit disclosure.
(13) If needed by an intern for compliance with another Board’s requirement, an intern must
maintain written or electronic records that support the number of TPI hours claimed by an intern

PAGE 47 | 58
and have those hours certified by a preceptor.
(14) An intern may make a voluntary report to the Board on any preceptor's aptitude and
professionalism in performing the duties of a preceptor. An intern must make such a report upon
request by the Board.
855-031-0026
Ratio & Supervision
(1) A pharmacist may not supervise more than one intern at a time at a TPI site who performs
the duties of an intern as listed in OAR 855-019-0200(3)(g). A pharmacist may supervise more
than one intern if only one intern performs the duties of an intern as listed in OAR 855-019-
0200(3)(g) and if other interns supervised by the pharmacist perform the duties listed in OAR
855-025-0040.
(2) A preceptor may not supervise more than two interns simultaneously during a shift at an SRI
site where patient specific recommendations for care or medications are provided without prior
written authorization of the Board.
(3) With the written approval of a school of pharmacy, and when in their professional judgment it
is appropriate, a preceptor may supervise up to 10 interns at public-health outreach programs
such as informational health fairs that provide general information but not direct patient care.
(4) For immunization clinics, an immunizing pharmacist may supervise up to two immunizing
interns.
(5) A licensed preceptor may delegate the preceptor responsibilities to another licensed
pharmacist or preceptor.
(6) The majority of an intern’s overall experience must be with a licensed pharmacist preceptor.
855-031-0030
Out-of-State Internship Experience
(1) In order for an Oregon intern to obtain credit for SRI experiences outside the State of Oregon,
an intern must:
(a) Be licensed as required by state laws and rules in the state in which they will practice;
(b) Meet or exceed the minimum SRI requirements of the Board;
(2) In order for an out-of-state intern to practice in the State of Oregon, the intern must meet all
requirements of these rules.
855-031-0045
School and Preceptor Registration and Responsibilities
(1) A preceptor license may be issued by the Board upon receipt of a completed application.
(2) A pharmacist preceptor must have been an actively practicing pharmacist for at least one year
immediately prior to supervising an intern.
(3) A preceptor license must be renewed biennially and will expire on June 30 in odd numbered
years.
(4) The preceptor may report to the Board voluntarily, the progress and aptitude of an intern under
the preceptor's supervision, or must do so upon request of the Board.
(5) The preceptor must be responsible for supervision of the majority of the intern's SRI hours and
must provide the intern with internship experiences, which in the preceptor's judgment will
increase the intern's competency in the practice of pharmacy.
(6) Before supervising an intern in an SRI program, a preceptor must complete any training

PAGE 48 | 58
program required by the school of pharmacy.
(7) A preceptor must advise each school of pharmacy when they are supervising students from
more than one school at the same time. This applies to both in-state and out-of-state schools or
colleges of pharmacy.
(8) A preceptor must verify that their intern is currently licensed with the Board.
(9) A pharmacist acting as a preceptor in a federal facility is not required to be licensed as a
pharmacist in Oregon, but is required to be licensed as a preceptor with the Board.
(10) The school of pharmacy must maintain a record of each intern’s SRIs. This record must be
made available to the Board upon request.
(11) A school of pharmacy located in Oregon must submit a report on their experiential education
program to the Board at the end of each academic year. This report must include the names of
students who successfully completed the program and graduated from the school. The school
must maintain a list of preceptors and SRI sites, in and out-of-state, approved by the school and
must make this list available to the Board upon request.
(12) All records related to a student must be available for three years after the student graduates.
855-031-0050
Eligibility for Exams — Foreign Pharmacy Graduates
In addition to the other requirements of this Division, a foreign pharmacy graduate must complete
1440 internship hours before applying to take the Multistate Pharmacy Jurisprudence
Examination (MPJE) and before applying for licensure as a pharmacist as specified in OAR 855-
019-0150. Evidence of completing this requirement must be provided to the Board by the
applicant and must be authenticated by each preceptor.
855-031-0055
Eligibility for Exams and Pharmacist Licensure
(1) An intern is eligible to take the North American Pharmacist Licensure Examination
(NAPLEX) and the MPJE, upon graduation and notification to the Board by the school of
pharmacy that their degree, with not less than 1440 hours of SRI, has been conferred.
(2) Upon meeting all requirements for pharmacist licensure, and before practicing pharmacy in
the State of Oregon, a person must:
(a) Complete an application for licensure including providing any fingerprint card or other
documentation required by the Board to conduct a criminal background check;
(b) Pay the license fee as prescribed in OAR 855-110; and
(c) Obtain a license, which will expire on June 30 in odd numbered years.
The official copy of an Oregon Administrative Rule is contained in the Administrative Order filed
at the Archives Division, 800 Summer St. NE, Salem, Oregon 97310. Any discrepancies with
the published version are satisfied in favor of the Administrative Order. The Oregon
Administrative Rules and the Oregon Bulletin are copyrighted by the Oregon Secretary of State.

PAGE 49 | 58
E*VALUE
E*Value is an online student / preceptor / site management system that allows the College to
electronically store and track demographic and academic information and communicate with
Preceptors and Students. Students and Preceptors are given unique web account / profile with
a secure login ID and password. Students and preceptors are able to access rotation schedules,
online evaluations forms, syllabi, rotation manuals and the CEI preceptor training portal by using
this URL
https://www.e-value.net/index.cfm
What do you need to do:
• Update your contact information
• Check your student schedule
• View the course syllabus and rotation manual
• View and complete your midpoint and final evaluation
• View and complete your online preceptor training

PAGE 50 | 58
WHERE TO FIND SYLLABI AND MANUALS
You can find the APPE Syllabi, manual, and other forms on your EValue Homepage. You will
need to first log onto your EValue profile and, once logged in, you should be able to see these
on a page like below.
HOW TO LOG IN and VIEW THE EVALUATION FORM
Your EValue log in ID and Password will be provided to you by the experiential office and once
you log in, you can find your student’s evaluation form by following this pathway from the
homepage: “Evaluations” Tab> “Complete Pending Evaluations” > “Edit Evaluation”. The
evaluation form is very easy to use (point and click). Based on the rubric that is posted at the
beginning of the form, please enter your ratings under each competency category and add your
comments/feedback as necessary. It is very important to scroll down to the bottom of the page
so that you can enter your grade (see below) and also “submit” the form.

PAGE 51 | 58
ONLINE PRECEPTOR TRAINING
We value the time and energy that you devote to our students and, as a valued OSU Affiliate
Faculty, we want to support you. Our online preceptor training, which is provided by the
CEImpact (CEI), is accessed through our web based experiential student management system
called EValue. In order to access the CEI preceptor training CE modules for free, you must first
log into your EValue account by following the instructions below.

PAGE 52 | 58
Log into EValue www.e-value.net by using your unique EValue ID and Password.
Select the “learning module” tab on top your homepage then select “Connect to CEI Account”
Then select “here” which is located after the intro paragraph.
After the pathway listed above you will be taken to the actual CEI website.
Select what state you practice in from the drop down box (first login only).
Enter the OSU subscription code (ORSTATE19) in the box at the bottom of left side column.
Required for no cost courses.

PAGE 53 | 58
Select “Preceptor” from left side list or “Preceptor” button under search box.
Free courses will show as NO COST.
If the majority of the preceptor courses do not show NO COST, resubmit the OSU subscription
code at the bottom of the left column.
You should be able to register for courses with a zero balance due. If not, please notify

PAGE 54 | 58
There are many of interesting topics available and you simply will need to decide what
module(s) you want. Again, the preceptor modules are free and are paid for by the College;
therefore, when you register for a module you will notice that your payment balance is zero.
CONDUCTING RESEARCH WITH HUMAN SUBJECTS
Drafted and approved by the OSU College of Pharmacy Research and Scholarship Committee.
Date: 7 May 2018.
Background: PharmD students participating in experiential programs access patients and patient
healthcare records as part of their professional education and practice. Students may wish to
conduct research using patient data; for example, to evaluate prescription behaviors, medication
adverse effects, or the effect of therapeutic guidelines. Most research involving humans or data
collected from humans require approval from the Institutional Review Board (IRB). This guidance
provides an interpretation of the existing guidelines available at
http://research.oregonstate.edu/irb/policies-and-guidance-investigators/guidance/chart-review
and
http://research.oregonstate.edu/sites/research.oregonstate.edu/files/irb/comparison_research_v_non
_research_v12292017.pdf.
Note that this document provides a general summary of IRB regulations but is specific to OSU. All
COP students are required to follow OSU IRB policies. However, COP students access the patient
records at many different healthcare and pharmacy facilities. Each of these settings will have an
IRB, ethics board, or other regulatory processes in place to oversee use of patient data. All COP
students must also comply with the regulations in place at the site at which patient records are
obtained/accessed.
By and large, PharmD students in the experiential programs interact with patients and patient-related
data in the following ways:
1. Access to patients and patient records to provide healthcare to individual patients. This type of
activity is not considered ‘human subjects research’ and does not require IRB approval.
2. Access to patient records for the purpose of quality improvement or quality assessment.
a. In this scenario, patient data collected as part of routine medical care are used to
evaluate healthcare delivery and interventions. This can include drug use
evaluations. Typically, for these studies the student/investigator does not intend to
publish or present their work externally.
b. This type of work is typically not considered human subjects research, although
some exceptions may apply. Note that the IRB for some healthcare facilities (eg, VA
Portland Healthcare System) maintain a separate process for approving quality
improvement/quality assessment studies. A request for determination can be sent
submitted to the IRB to assess if a particular project requires IRB oversight or is
exempt.
3. Access to existing patient records for descriptive or analytic purposes with an intent to
disseminate results (eg publication or presentation).
a) In the case that personally identifiable data (i.e., data that can be linked in any way to
individuals) or any of the 18 protected health identifiers (PHI) specified under HIPAA are
included in the collected data, the research activity is considered ‘human subjects research’
and requires IRB approval.
a
Please also refer to items 3a and 3b below for further guidance.
Note, the student’s mentor/preceptor may choose to fully de-identify the patient data by
removing all PHI and personally identifiable information (for instance, by removing names,
MRN, all dates, and other identifiers). If the mentor provides coded data to the student, the
mentor must apply for and obtain IRB approval for the project since the mentor has access to

PAGE 55 | 58
the identifiers and the codes
b
.
b) In the case that human data cannot be linked in any way to individuals (for instance, analysis
published or publicly available datasets), the research activity is not considered to include
‘human subjects’ and would not require IRB review. When in doubt, a determination request
can be submitted to the OSU IRB at
IRB@oregonstate.edu or visit
https://research.oregonstate.edu/irb.
3. Collection of data through direct interaction (includes phone calls, etc.) with patients or through
intervention with the intention to disseminate the results is considered ‘human subjects research’
and requires IRB review
c
. A research study meets the criteria of a clinical trial if one or more
human subjects are prospectively assigned to one or more interventions (which may include
placebo or other control) to evaluate the effects of those interventions on health-related
biomedical or behavioral outcomes (see https://grants.nih.gov/policy/clinical-trials/definition.htm
).
OSU Students are not allowed to serve as Principal Investigators on such projects but they may
participate as co-investigators after completion of human ethics training available through the
OSU IRB office.
a) Student presentations, such as posters, simply to document the educational experience or to
fulfill programmatic requirements are not considered ‘dissemination of results’.
b) Student presentations, such as posters, at professional or scientific meetings outside OSU
that make the results of the data collection publicly available are considered ‘dissemination
of results’. Students wishing to make patient-related data publicly available must have IRB
approval.
Footnote comments:
a
Note that HIPAA authorization and consent or a waiver from the site will also be required.
b
If the Principal Investigator is an OSU person, that person would need to submit an IRB
application only if identifiable or coded data were being provided to other OSU persons. If instead,
a non-OSU person is de-identifying the data and then giving it to the student (so no one at OSU
ever has identifiable data) it may not need IRB review. De-identification must be done by
someone other than the student before the student accesses the data.
c
If conducted at the clinical site/covered entity, HIPAA authorization or waiver from the site may
also be required.
Glossary
Coded: Identifying information (such as name or social security number) that would enable the
investigator to readily ascertain the identity of the individual to whom the private information or
specimens pertain has been replaced with a study-specific number, letter, symbol, or combination
thereof (i.e., the coded identifier); and a key linking the coded identifier to personal/medical
identifiers exists, enabling linkage of the identifying information to the private information or
specimens.
De-identified: When collected, data contained identifiers or information that would permit
identification of the individual(s) about whom the data were collected, but the identifiers or indirect
links to identity have been removed and no longer exist anywhere in any form. Exception: When
coded data are shared between researchers and a data use agreement is in place between the
institutions that no identifiers will be shared, these data are considered de-identified. This exception
does not apply when the holder of the key is involved in the research. For example, a PI sharing
coded data with a student researcher is conducting research with identifiable data because it is their
responsibility to oversee all aspects of the study.
Individually identifiable: The identity of the subject is or may readily be ascertained by the
investigator or associated with the information. Individually identifiable information is not limited to
name, date of birth, or contact information.
For questions regarding this policy, please contact the OSU IRB Office at IRB@oregonstate.edu
.

PAGE 56 | 58
INCIDENT REPORT FORM
INSTRUCTIONS
This form is to be used to report bodily fluid exposures, needle sticks, and similar injuries to College of
Pharmacy faculty, staff and students. Complete this form and return it to the Director of Experiential
Programs within 24 hours of the exposure or injury.
Name of Person Injured
Click here to enter text.
Unique Identification Number (UID)
Click here to enter text.
Contact Phone Number
Click here to enter text.
Email Address
Click here to enter text.
Today’s Date
Click here to enter a date.
Date of Exposure
Click here to enter a date.
Time of Exposure
Click here to enter a time.
Brief Description of Exposure
Click here to enter text.
TYPE(S) OF EXPOSURE OR INJURY
LOCATION WHERE EXPOSURE OR
INJURY OCCURRED
☐
Needle
☐
Introductory Pharmacy Practice Education
site or visit
☐
Lancet
☐
Advanced Pharmacy Practice Education site
☐
Glass
☐
College of Pharmacy event
☐
Blood
☐
Student organization event
☐
Bodily fluid other than blood
☐
Student employment, internship, or volunteer
site
☐
Other (specify): Click here to enter text.
☐
Other (specify): Click here to enter text.
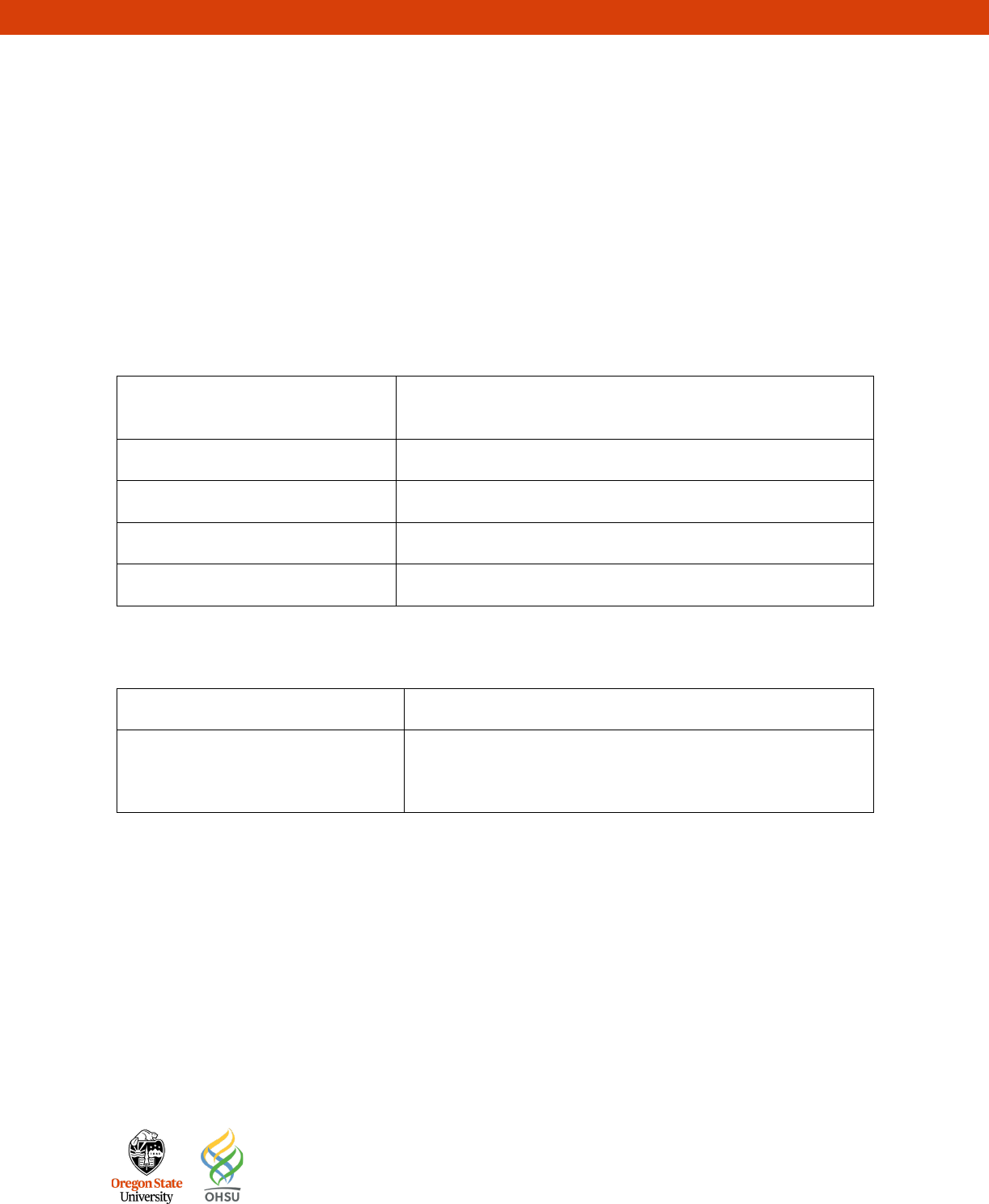
PAGE 57 | 58
THE EXPOSURE OCCURRED
EXPOSED OR INJURED BODY PART(S)
☐
Before use of the sharp
☐
Face/Head/Neck
☐
After use of the sharp
☐
Torso
☐
During use of the sharp
☐
Arm
☐
No sharp used or not applicable
☐
Hand
☐
Leg/Foot
Faculty/Staff/Student’s Medical
Provider
Click here to enter text.
Date Provider Seen
Click here to enter a date.
Patient/Source Name
Click here to enter text.
Patient/Source Contact Information
Click here to enter text.
Patient/Source Medical Provider
Click here to enter text.
TO BE COMPLETED BY COLLEGE OF PHARMACY FACULTY/STAFF
Date of Source Testing
Click here to enter a date.
Additional Information or Follow-Up
Click here to enter text.

PAGE 58 | 58
Change in Rotation Authorization Form
Instructions: Please have this form signed by both preceptors involved in the change after discussion of
the proposed changes in your APPE schedule with the Assistant Dean of Experiential Education. Please
return the completed form back to the Experiential Education office. Any proposed changes must be
discussed at least 6 weeks in advance.
Student’s Name: ______________________________________________________________________
Brief reason for change: ________________________________________________________________
____________________________________________________________________________________
____________________________________________________________________________________
____________________________________________________________________________________
____________________________________________________________________________________
Rotation Currently Assigned to:
Rotation Site_____________________________________________________
Rotation Type____________________________________
Rotation Dates___________________________________
Preceptors Name_________________________________________________
Preceptors Signature______________________________________________
Rotation Changing to:
Rotation Site_____________________________________________________
Rotation Type____________________________________
Rotation Dates___________________________________
Preceptors Name_________________________________________________
Preceptors Signature______________________________________________
Approved by: _______________________________________________ Date: __________________
Assistant Dean of Experiential Education

