
Suicide and its Prevention
among Older Adults
Dr. Marnin J. Heisel, Ph.D., C.Psych.
The University of Western Ontario;
Lawson Health Research Institute
Project ECHO Presentation
Monday, April 17, 2023

Address: Dr. Marnin J. Heisel,
Parkwood Institute Mental Health Care Building,
550 Wellington Rd., Office #F4-365
P.O. Box 5777 STN B.,
London, Ontario, N6A-4V2
Phone: 1-519-685-8500 extension 75981
E-Mail: [email protected]
Web: Meaningfulgroups.com
Contact Information

-American Foundation for Suicide Prevention
-Canadian Institutes of Health Research
-Centre for Aging and Brain Health Innovation, Baycrest
-Employment and Social Development Canada
-Lawson Health Research Institute
-Movember Canada
-Ontario Mental Health Foundation
-Ontario Ministry of Research & Innovation
-Public Health Agency of Canada
-Social Sciences and Humanities Research Council of Canada
-UWO Department of Psychiatry
Funding Acknowledgements

• Thank you to all of my research assistants,
students, clinical trainees, and colleagues who
have collaborated on this work over the years.
• My sincerest thanks to all of my clients and
research participants and to all of the
community members who have made this
work possible and meaningful.
Acknowledgements

Learning objectives:
By the end of this presentation, you will be able to:
1. Demonstrate an increased understanding of the
epidemiology and risk and resiliency factors
associated with suicide among older adults;
2. Show familiarity with a humanistic approach to
suicide risk assessment and response with older adults;
3. Discuss evidence and opportunities for suicide
prevention among older adults across clinical,
community, and population health levels.

Let’s start with a few quick
multiple-choice questions…

1. Which of the following statements is most true of
suicide in Canada?
a) Men in their 70s and older have suicide rates that more
than double the national average.
b) Older adults have higher suicide rates than adolescents
c) More adolescents die by suicide than older adults.
d) Middle-aged men have the nation’s highest suicide rate.
2. The strongest risk factor for suicide among older
adults is ____________.
a) Depression c) Misuse of alcohol/substances
b) Previous suicidal behaviour d) Social isolation

3. Which of the following factors have been shown to
increase risk for suicide AND for MAID?
a) Pain and suffering
b) Depression
c) Loneliness
d) Feelings of meaninglessness
e) Feeling like a burden on others
f) All of the above
g) None of the above

4. Although few clinical trials exist that specifically
focus on older adults, evidence from controlled
clinical research trials supports which of the following
modes of psychotherapy for reducing suicide ideation
or the likelihood of repeating suicidal behaviour?
a) Psychodynamic psychotherapies
b) Interpersonal psychotherapies
c) Cognitive behavioral psychotherapies
d) Supportive psychotherapies
e) All of the above
f) None of the above

5. Research on depression screening in Japan and
telephone support in Italy suggests that __________.
a) Community outreach interventions may help prevent suicide
among older adults.
b) Community-level interventions may be ineffective at
preventing suicide among older adults.
c) Effective communication is required in order to prevent suicide
among older adults.
d) Medication is required in order to prevent suicide among older
adults.

6. Which of the following statements is false regarding
late-life suicide risk?
a) Suicidal thoughts can come and go and increase and decrease
over time.
b) Risk for suicide may be high when someone starts emerging
from a depressive episode.
c) Asking about suicide will plant the idea in an older person’s
mind.
d) Take any threat of suicide or wish to die seriously.

7. Which of the following is a key message in the field
of suicide prevention?
a) When assessing suicide risk, it’s better to be safe than sorry.
b) Suicide prevention is everybody’s business.
c) Don’t ask, don’t tell.
d) Only you can prevent deaths by suicide!


• For at least the past 3 decades, there has been increasing
focus on suicide as a public health issue, and suicide
prevention efforts employing a public health lens.

• In so doing, many have focused on British
Epidemiologist Geoffrey Rose’s Theorem:
“a large number of people at small risk may
give rise to more cases than a small number of
people at high risk”
Rose (1985)

• That having been said, does it make sense to
exclusively focus on preventing suicide among
people at low risk for suicide?
• Should we not also focus on people at
moderate risk?
• And should clinicians not be exceptionally
concerned about people at high risk?

• According to the U.S. Centers for Disease Control
and Prevention (CDC), there are 4 steps to a public
health approach to violence prevention:
• Step 1: Define and Monitor the Problem;
• Step 2: Identify Risk and Protective Factors;
• Step 3: Develop and Test Prevention Strategies;
• Step 4: Assure Widespread Adoption
https://www.cdc.gov/violenceprevention/about/publichealthapproach.html

• Every day, roughly 11 people die by suicide in Canada
• Of those people:
• 9-10 would meet criteria for a mental disorder
• 8 are Male
• 4 are in Ontario
• 2 are over the age of 65
• 1-2 use a firearm (and are male, and older)
Suicide in Canada: A Picture of a Typical Day

• In addition, a further 28 people every day die by
MAID (most of whom are over the age of 60, and
roughly half of whom are Female).
• I no longer think we can address the issue of suicide
among older adults in Canada without simultaneously
considering the issue of MAID.
• Although these are defined as distinct entities, and
relevant data are housed in different locations, there is
considerable overlap between the two.

• According to the World Health Organization
(WHO, 2021), suicide accounts for 1% of all
deaths worldwide, or 703,000 lives lost every year.
• Although a low percentage, this number is
extremely high, exceeds the global number of lives
lost to war & homicide combined, and yet reflects
a recent reduction in deaths by suicide.
• In 2014, the WHO reported over 800,000 annual
deaths to suicide worldwide; in earlier years, this
figure exceeded 1,000,000 lives lost to suicide.
• This reduction appears to support the effectiveness
of suicide prevention strategies and programs.
Epidemiologic Background

• Although suicide is a global problem that
affects people of all social classes, religions,
cultures, ethnicities, and nations of origin,
it does so unequally and inequitably:
• Suicide rates vary by country
• Suicide rates vary by geographic region
• Suicide rates vary by social stratum
• Suicide risk varies by profession
• Suicide risk varies by age
• Suicide risk varies by sex (and sexual identity)
• Suicide risk varies by culture and ethnicity
• Suicide risk varies by health condition

• The costs of suicide are staggering.
• A Canadian report on injury estimated that Suicide
and Self-Harm together accounted for 11% of total
costs of injury in Canada in 2010, and exceeded
$2.9 Billion/year (Parachute, 2015).
• However, there is no price that can capture the
deeper emotional impact of this loss of human life.

• The global older adult population is expanding.
• People are living longer; reduced mortality to childhood
illness and infectious disease* and decreased birth rates
contribute to increased longevity (NIA/WHO, 2011).
• The over-65 population could increase from 524MM
in 2010 to nearly 1.5 Billion people by 2050, or 16%
of the world’s population (U.S. NIA/WHO, 2011).
• 20-25% of the North American population (75MM+)
will be over 65 by 2030 (Statistics Canada, U.S. NIA).
• Nearly 1 in 8 older Canadians is 85+ (Statistics Canada).
* It is yet unclear what medium-to-longer-term impacts
COVID will have on population demographics.
Demographics of the Aging Population

Year
25
20
15
10
5
0
1921 1931 1941 1951 1961 1971 1981 1991 2001 2011 2021 2031 2041
Percentage
65-74 75-84 85+
Older Adults (by age sub-groups) as
% of the Total Population
Canada, 1921-2041
Source: The Canadian Coalition for Seniors’ Mental Health

• Baby-boomers (DOB: 1946-1964) have high rates of
suicide as compared with earlier cohorts.
• More than 9,500 North Americans over 65 die
by suicide annually or more than 18,000 over 55;
this number is growing (CDC, StatsCan).

• Canetto’s “gender paradox of suicide”: women are
far more likely to engage in suicide behaviour, and
yet men are far more likely to die by suicide.
• Older men have the highest rates of suicide globally;
middle-aged men account for the highest number of
deaths by suicide in North America.
• Among North American women, suicide rates are
highest in mid-life.
• Sex and age differences are apparent when reviewing
national and global trends in suicide.
• In North America, men account for 75% of deaths by
suicide, and typically employ highly lethal means.
Sex Differences

• 2020 North American mortality data indicate:
• 45,979 people died by suicide in the U.S.A.,
including 36,551 men or boys (M: 79.5%) and
9,428 women or girls (F: 20.5%), for a national
suicide rate of 13.95/100,000 overall, 22.5/100K
for M, & 5.6/100K for F (U.S. CDC; WISQARS).
• 3,839 people died by “suicide” in Canada,
including 2,874 men or boys (M: 75%) and
965 women or girls (F: 25%) for a national suicide
rate of 10.1/100,000 overall, or 15.2/100K for
M and 5.0/100K for F (Statistics Canada).

Canadian Suicide Rates by Sex and Age for 2020
0
10
20
30
40
M
F
All
Source: Statistics Canada
Note: Overall National suicide rate = 10.1/100K

American Suicide Rates by Sex and Age for 2020
0
10
20
30
40
50
60
Chart Title
M
F
All
Source: WISQARS (CDC)
Note: Overall National suicide rate = 13.95/100K

• Suicide rates are often undependable and
underestimate “true” suicide rates, especially if
means of suicide are equivocal (e.g., medication
overdose, Ohberg & Lönnqvist, 1998).
• Ontario has Canada’s most stringent regulations
regarding classification of suicide, making Canada-
wide comparisons difficult.
• Medical Assistance in Dying (MAID), which was
initially legalized in 2016, has complicated things
further.
• Statistics Canada does not report on MAID deaths.

• Although there was a noticeable (10-15%) reduction
in deaths by suicide early into the pandemic, surveys
have noted increased psychological distress, and
health care systems saw increased need.
• Moreover, the number of older adults who died by
suicide in Canada did not decline, consistent with the
fact that the number of older adults who die by
suicide is increasing as the population grows.
• 3,606 individuals died by suicide in Canada in 2000;
by 2020, this figure increased 6.5% to 3,839.
• 402 older adults died by suicide in Canada in 2000;
by 2020, this figure increased by 64% to 658.


Numbers of Deaths by Suicide among Adults 65+ in the U.S. (1999-2020)
Source: WISQARS, U.S. CDC

• Again, these figures do not include deaths by
Medical Assistance in Dying (or MAID).
• The average age of Canadians who accessed MAID
in 2021 was 76.3 years.
• 10,064 Canadians died by MAID in 2021, reflecting
a 32.4% increase over 2020 (in addition to a 34%
annual increase over 2019).
• And so we might not have seen increases in suicide,
per se, during the pandemic; but we have certainly
seen a massive increase in self-determined deaths.
• This will only increase in coming years, as the limits
on MAID are further expanded to include those with
a primary mental disorder.

Source: Health Canada, 2022
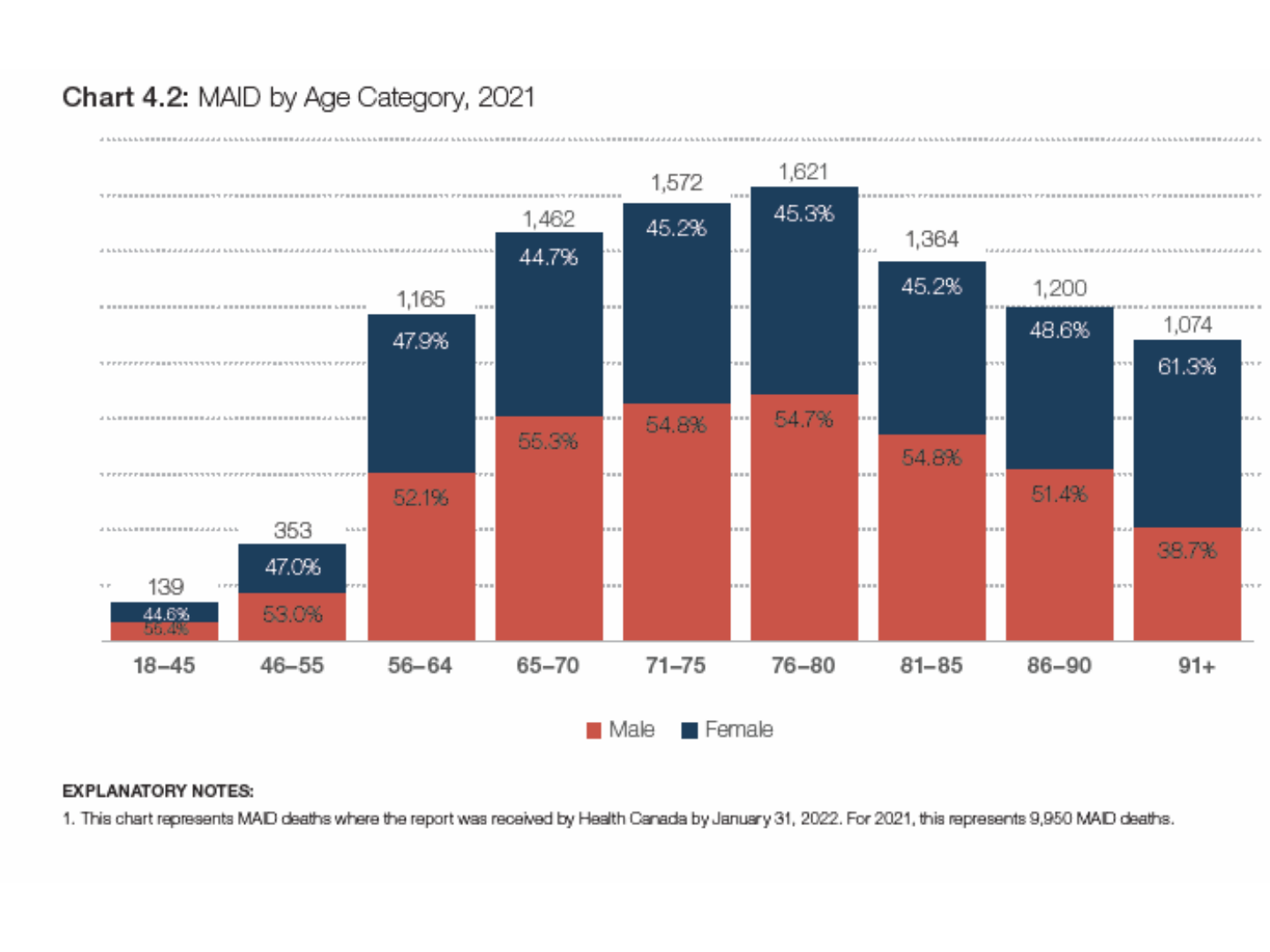
Source: Health Canada, 2022

“The most commonly cited intolerable physical or
psychological suffering reported by individuals
receiving MAID in 2021 was the loss of ability to
engage in meaningful activities (86.3%), followed
closely by the loss of ability to perform activities of
daily living (83.4%).”
-Health Canada (2022)*
*Third Annual Report on Medical Assistance in Dying in Canada 2021

• Psychological problems are not inevitable with aging
•Most middle-aged and older adults are emotionally
well-adjusted.
• However, roughly 15% of adults over 60 suffer from
a mental disorder (WHO, 2017) which can contribute
to poor life satisfaction, functional decline, and
increased mortality, including by suicide.
• Challenges abound in accessing quality mental
healthcare for older adults.
• Innovative approaches are needed.
Mental Health and Aging

Risk and Protective Factors

Suicide Assessment & Prevention for Older Adults
Clinician Pocket-Card
RISK FACTORS:
1. Suicidal Ideation and/or Behaviour
⚫ Prior suicidal behaviour (including suicide attempt), prior
self-harm behaviour, previous expression of suicide ideation
⚫ Feels tired of living and/or wishes to die
⚫ Thinks about suicide, has suicidal wishes and/or desires
⚫ Has a suicide plan/note
⚫ Access to a firearm or other means of suicide
2. Family History
⚫ Family history of suicide, suicide ideation, mental illness

RISK FACTORS (Cont.):
3. Mental Illness (can include)
⚫ Any mental disorder, co-morbidity
⚫ Major depressive disorder
⚫ Any mood disorder
⚫ Psychotic disorder
⚫ Substance misuse disorder/addictions
4. Personality Factors
⚫ Personality disorders
⚫ Emotional instability
⚫ Rigid personality
⚫ Poor coping skills, introversion

RISK FACTORS (Cont.):
5. Medical Illness
⚫ Pain, chronic illness
⚫ Sensory impairment
⚫ Perceived or anticipated/feared illness or decline
6. Negative Life Events and Transitions
⚫ Family discord, separation, death or other losses
⚫ Financial or legal difficulties
⚫ Employment/retirement difficulties
⚫ Relocation stresses
7. Functional Impairment
⚫ Loss of independence
⚫ Problems with activities of daily living

Suicide Assessment & Prevention for Older Adults
Clinician Pocket-Card
RESILIENCY FACTORS:
1. Religious (or spiritual) practice.
2. Sense of meaning and purpose in life.
3. Sense of hope or optimism.
4. Active social networks and support from family and friends.
5. Good health care practices.
6. Positive help-seeking behaviours.
7. Engagement in activities of personal interest.

⚫ It is not enough to simply take stock of the
various risk and protective or resiliency factors
present in a given individual; we must
conceptualize how these combine to increase,
maintain, or reduce that individual’s risk for
suicide, over immediate, moderate, and long-
term periods.

Our Conceptual Framework
(e.g., Heisel & Flett, 2014)

Risk Assessment
• Suicide risk assessment must be carried out in a
sensitive fashion, in the context of a trusting
therapeutic relationship
• Rating scales and other measures can be helpful, but
are insufficient on their own to assess risk
• Be aware of validity issues; don’t just take
self-reports at “face value”
• Work within your skill-set and competencies; use of
assessment tools requires appropriate training
• There is no such thing as a “best” screening or
assessment tool; rather certain tools are more
appropriate in particular contexts and populations

• Professional geropsychology guidelines recommend
use of age-specific measures developed and/or
validated with older adults (APA, 2004).
• We saw the need for a tool to specifically assess
older adult suicide risk and resiliency, and developed
the Geriatric Suicide Ideation Scale to meet this need
(GSIS; Heisel & Flett, 2006).
• More recently, we developed an abbreviated, 5-item
GSIS-Screen for use in health screenings, residential
care, and clinical practice (Heisel & Flett, 2022).

CCSMH Suicide Assessment & Prevention for
Older Adults Clinician Pocket-Card
Assessment Process:
1. Establish rapport and assess for suicide risk in a sensitive
and respectful fashion.
2. Respect the dignity of older adults. Acknowledge their
experiences and validate their feelings.
3. Assess for suicide risk factors.
4. Assess for psychological resiliency.
5. Assess for suicide warning signs IS PATH WARM.

Assessment Process (Cont.):
6. Where appropriate, access collateral information
(medical chart, family members, other providers).
7. Be mindful of ambivalent wishes to live and to die.
8. Develop a risk management/action plan.
9. Seek consultation and/or assistance if you do not have
specialized training in mental health or in suicide
prevention.

Suicide Assessment & Prevention for Older
Adults Clinician Pocket-Card
KEY QUESTIONS:
1. Ask about their feelings
⚫ Do you feel tired of living?
⚫ Have you been thinking about suicide?
2. Ask about a suicide plan
⚫ Have you made any specific plans or preparations
(giving away possessions, tying up 'loose ends')?
⚫ Do you have access to lethal means like a gun or other
implements?
3. Ask about their reasons to live
⚫ Who or what makes life so worth living that you would
not harm yourself?

Q: Can suicide be predicted?

• Suicide is a low base-rate phenomenon, and is thus
extremely difficult to predict on an individual basis.
• This yields a problem with specificity.
• Prediction of suicide requires immense sample sizes
and long follow-up periods.
• Most studies do not differentiate imminent from
lifetime elevated risk; but this is what is needed in
healthcare settings.
• The jury is out on the potential effectiveness of
Artificial Intelligence/Machine Learning approaches
in potentially predicting deaths by suicide

Suicide can be prevented!

Prevention
Intervention
Postvention

The Language of Prevention Science
(U.S. Institute of Medicine)
• Universal = At the population level
(primary)
• Selected = For a group with elevated risk
(primary)
• Indicated = For those at imminent risk
(secondary early intervention)
• Prevention strategies are needed at all levels!!

• Public health initiatives (Universal)
• Means restriction (medication packaging, CO, bridge
barriers, firearms, media guidelines)
• Clinician education (screening & intervention)
• Suicide prevention strategies/treatment guidelines
• Community initiatives (Selected)
• Gatekeeper training and response/referral
• Community outreach/support (DeLeo et al., Oyama et al.)
• Clinical initiatives (Indicated)
• Psychotherapy (+ medication, and possibly ECT)
• Emergency Cards and caring letters
• Organizational change
Empirically-Supported Initiatives

• Effective public health approaches can include:
• Education (providers, clients, communities, the media)
• Community outreach (screenings) and response
• Means restriction (e.g., guns, alcohol/drugs, “hot spots”)
• Access to and delivery of effective mental healthcare
• Collaboration between primary care, mental health,
social service providers, older adults and their families
• Enhanced/integrated systems of care
• Grassroots efforts
• Screening high-risk demographics and high-risk settings
• Plus, research, dissemination, and training
(see Mann et al., 2005; Zalsman et al., 2016)

Clinical Interventions
• There had been a paucity of RCTs with suicidal
individuals; suicide risk had been a typical exclusion
factor in treatment studies (e.g., Pearson et al., 2001)
• There has been an increase in research on this issue
in recent years; in the U.S., efforts had largely been
spearheaded by military and veterans groups 10-15
years ago, with uptake by other Federal funders
• Efforts are underway in the U.S. and Canada to
develop strategic research priorities for suicide
prevention; these must include focus on older adults
• Health care organizations are increasingly looking at
management approaches

•Lithium
(Angst et al., 1999; Baldessarini et al., 1999; Goodwin, 1999)
•Clozapine (Meltzer et al., 2003)
•Other antipsychotics (Hawton et al, 1998; Palmer et al,1999)
•Antidepressants (Angst et al., 1999)
•ECT (Prudic & Sackeim, 1999)
•These studies were not specific to older adults
MEDICAL INTERVENTIONS

• Cognitive approaches:
• Cognitive Therapy (Brown et al., 2005)
• DBT (Linehan et al., 1991, 2006)
• Problem-Solving Therapy (Salkovskis et al., 1990)
• Interpersonal approaches:
• Brief psychodynamic interpersonal therapy
(Guthrie et al., 2001)
• Interpersonal problem-solving (McLeavey et al., 1994)
• Interpersonal Psychotherapy (Alexopoulos et al., 2009;
Heisel et al., 2009, 2015)
• Meaning-centered approaches (Breitbart et al, 2015;
Heisel et al., 2020; Lapierre et al., 2007)
PSYCHOLOGICAL INTERVENTIONS

• Human beings are more important than things; respect the
inherent value and dignity of all people and honour their
wishes to take an active role in their lives and communities.
• Everyone is unique. No single approach fits equally well
for all people; avoid “cookie-cutter” programs or strategies.
• Take the time to really listen to each client; learn who they
are, their history, hopes, experiences, who matters to them,
and what makes life meaningful for them.
• Ask “how would I like to be treated in their circumstances?”
• Focus on the “here and now” but be open to wishes to
reflect/reminisce and to think about the future.
• Growth and development does not stop at a particular age;
aging is as much a state of mind as of body or of time.
Some Humanistic Principles in Gerontology
Recommendation: Treatment and Management:
• Develop a trusting and genuine therapeutic relationship with
at-risk older adults. Actively and attentively listen to the
client, and take your time. When present, these elements
help contribute to a person feeling heard and respected, and
can help contribute to the older client feeling connected.
• Foster hope in clients who are suicidal. Health care providers
may promote hope by initiating hope-focused conversations.
• Health care providers should explore strategies to assist older
persons find and maintain meaning and purpose in their lives.

• When older adults access mental healthcare services,
they rarely receive recommended care due in part to a
paucity of provider knowledge and skill in suicide risk
detection and intervention (Heisel & Duberstein, 2005).
• Education and training can effectively enhance provider
knowledge and attitudes towards working with suicidal
individuals (Huh et al., 2012; Schmall & Pratt, 1993).
• Educational interventions are needed in order to
enhance provider knowledge and skill in delivering
competent care to those at-risk.
• We initially evaluated focused training sessions
incorporating a set of knowledge translation tools
developed together with the Canadian Coalition for
Seniors’ Mental Health (CCSMH).
Training Needs


⚫ We evaluated dissemination of the CCSMH tools by
delivering half-day workshops to frontline providers
employing these tools.
⚫ We assessed change in knowledge and attitudes toward
working with older adults at-risk for suicide using two
scales we developed for this purpose.
⚫ Findings indicated significant improvement in provider
knowledge and attitudes reflecting greater comfort and
perceived competence in working with older adults
regarding risk for suicide.
CIHR Betty Havens Award for KT in Aging

Enhanced competency in
assessing suicide risk
and providing care for
at-risk older adults
Professional
Skills and
Experience
Attitudes Towards
Working with
At-Risk Older Adults
Knowledge about
Late-Life Suicide
and its Prevention
Our Model

• We will be expanding on this approach in a CIHR-
funded study on screening for suicide risk among
older residents of Ontario Long-Term Care Homes.
• This project involves:
• Educating on-site personnel to sensitively screen for
(and respond appropriately to) suicide risk;
• Evaluate screens for suicide ideation (SI);
• Identify the prevalence of suicide ideation and
behaviour in LTC;
• Test a theoretical model of SI; &
• Explore similar issues with respect to MAID.

• In order to improve suicide prevention, we need to:
• raise awareness
• improve risk detection
• enhance understanding of risk/resiliency factors
• develop and test innovative interventions
• develop/deliver individualized approaches to care
• improve education and training for professionals
• engage in knowledge translation and dissemination
• revise/adapt/test policy changes
• MAKE IT A NATIONAL PRIORITY!
Research and Clinical/Systemic Needs

• Canada does not yet have a National Strategy for
Suicide Prevention!
• Healthcare in Canada is managed at the level of the
provinces and territories not at a Federal level.
• Nevertheless, Federal efforts are underway regarding
suicide prevention, including:
• a “Federal Framework” for suicide prevention,
• efforts to develop strategic research priorities,
• a national demonstration project,
• focused scoping reviews,
• a proposed 3-digit suicide prevention crisis line.

Do suicide prevention strategies work?

• The global suicide rate decreased by 36% overall
from 2000-2019, ranging from a 17% decline in the
Eastern Mediterranean Region to more than a 47%
decline in Europe and Western Pacific Regions.
• This suggests that suicide prevention strategies,
guidelines, and other initiatives are effective.
• Yet, in the Americas, it INCREASED by 17%.
• More work clearly remains to be done!


• Treating mental health problems is necessary.
• Existing approaches tend to be reactive, focusing on
treatment of symptoms and disorders, rather than
on promoting mental health and well-being among
older adults; “upstream” approaches are also needed.
• More attention is needed to building social
connections and support and in enhancing
psychological resiliency (i.e., the ability to cope
with stress, bounce back, and learn and grow from
adversity) and well-being.
What Can We Do?

• Although there has been a paucity of research explicitly
focusing on the prevention of suicide among older
adults, community efforts have shown promise in
reducing risk (DeLeo et al., 2002; Oyama et al., 2005);
benefits were mainly found for women
(Duberstein, Heisel, & Conwell, 2011).
• “Upstream” preventive interventions are needed
designed to enhance psychological resiliency for
middle-aged and older men (CCSMH, 2006).
• It was with those considerations in mind that my
colleagues and I developed Meaning-Centered Men’s
Groups (MCMG; Heisel et al., 2016, 2018, 2020).


• Group meetings focus on discussions of:
• Meaning in work and career
• Meaning in productivity and societal contribution
• Meaning in mentorship and volunteerism
• Meaning in leisure and recreation
• Meaning in relationships, love, and friendship
• Attitudes towards life’s challenges and transitions
• Attitudes towards positive experiences
• Generativity, spirituality, and end-of-life issues

• We pivoted our groups online during the pandemic.
• We then further adapted them (as Online Meaning-
Centered Groups or OMG) for delivery to Retirement
Home residents and other Ontarians over 60 struggling
with loneliness, isolation, and pandemic-related
psychological distress (CABHI and New Horizons).
• We have received Movember funding to adapt MCMG
for Veterans and First-Responders facing a career
transition and are actively recruiting for this study.
• www.meaningfulgroups.com
What’s Next?

• We cannot predict who will die by suicide; however, we can
and must assess suicide risk (and resiliency)
• Outreach is critical for detecting at-risk individuals;
don’t forget to follow-through
• Make suicide risk assessment part of usual practice, even
when you don’t think it’s present
• Routinely assess access to firearms and other lethal means
• Assess history of suicidal behaviour; one of the strongest
risk factors for death by suicide
• Be open to discussions of suicide-it takes time and should
• Consider use of rating scales
• Work in teams wherever possible
• Communication among providers is absolutely critical
Treatment Implications

• This is a free webinar series, taking place on roughly a
monthly basis, focusing on suicide and its prevention.
Everyone is welcome.
• Feel free to e-mail me to ask for your e-mail to be added to
our distribution list: [email protected]

• Recent decades have witnessed an increased
public health focus in the field of suicide prevention.
• This has helped the field move away from
exclusively clinical approaches, promoted evaluation
of intervention programs, and communicated the
message that suicide is not solely a clinical, medical,
or biological entity, but one with clear psychological
and social contributors and implications.
• However, we need to ensure that we do not go too
far in the other direction.
• Innovative, multi-level, multi-perspective, and truly
interdisciplinary approaches are needed.
Summary

• Moreover, we must take into consideration the lived
experience of older adults, their family members
and other supports, and healthcare providers if we
wish to truly impact the health and well-being of
older adults and not only prevent suicide but
enhance life.

Thank You
