Faculty and Staff
Benefits
Handbook
Faculty and Staff Benefits Handbook
May 2013
May 2013

B
oston University began in April
1839, when delegates of the
Methodist Episcopal church met
in Boston to found the Newbury
Biblical Institute. The insti tute
opened in Newbury, Vermont;
moved to Concord, New Hampshire;
and then moved to Boston. In
May 1869, the Common wealth of
Massa chusetts granted a charter
to Boston Univer sity, and the
School of Theol ogy became its
first department.
Thus founded, Boston University
grew, both reflecting and leading
the growth of U.S. higher educa-
tion. From the date of its charter,
it admitted women students to
all programs—the first university
in the country to do so. In 1872, it
opened the nation’s first College of
Music as well as the School of Law,
which would become the first to
require three years for a degree.
In the following year, it opened
the College of Liberal Arts and the
School of Medicine; one-quarter
of the first medical students were
women. The Graduate School,
established the following year, had
by 1875 arranged for tuition-free
study abroad at universities in
Athens and Rome.
Schools and Colleges have con-
tinued to be established and to
evolve. Today they number 16,
offering a vast range of programs
in education, medicine, dentistry,
communication, liberal arts, law,
engineering, social work, arts,
allied health professions, theology,
and management. The College of
General Studies offers a two-year
program in an interdisciplinary core
curriculum, and then students con-
tinue working toward a bachelor’s
degree at one of BU’s four-year
undergraduate schools and colleges.
Metropolitan College provides a
wide range of courses and degree
programs primarily for those who
wish to pursue coursework at night
and on weekends.
Boston University is the fourth-
largest independent institution of
higher education in the country,
and one of the world’s leading
research universities, with over
thirty thousand students in Boston
on the Charles River Campus and
the Medical Campus as well as
in a growing number of programs
around the world. The University
has more than four thousand fac-
ulty members who teach, conduct
research, and use their professional
expertise to serve their worldwide
community. The University’s addi-
tional staff of more than six thou-
sand employees support the efforts
of the University.
Boston University is in itself a com-
munity of vast scholarly, academic,
and recreational resources. Its
members enjoy access to a variety
of University health services, rec-
reational facilities, and activities,
as well as a state-of-the-art library
system. Tuition remission enables
many employees and their spouses
and dependents to take University
courses with full or partial subsidy.
Several exhibits are open on cam-
pus every day, and a night seldom
passes during the academic year
without at least one public concert,
theatrical or operatic performance,
lecture, seminar, or athletic event.
Faculty, students, and staff work
closely with public schools, social
services, and other groups in
Boston and beyond.
Enduring commitments to teach-
ing, research, global education, and
community engagement are the
touchstones of Boston University’s
proud past and promising future.
About Boston University

Overview
Your Benefits Handbook 1
Health Plan 3
Blue Cross Blue Shield PPO 8
Network Blue New England 11
BU Health Savings Plan 13
Medco/Express Scripts Health Prescription Drug Coverage 19
Health Plan Comparison 28
Dental Health Plan 31
The BU Dental Health Center Plan 34
The Dental Blue Freedom Plan 37
Long-Term Disability Plan 49
Survivor Insurance 55
Basic Life Insurance Plan 57
Group Supplemental Life Insurance Plan 58
Personal and Family Accident Insurance Plan 61
Travel Accident Insurance Plan 64
Supplemental Death Benefit Plan 66
Retirement Plan 67
Supplemental Retirement and Savings Plan 81
Tuition Remission Program 93
Tuition Exchange Program 101
Flexible Benefits Program & Flexible Spending Accounts 107
Other Benefits 117
Administrative Information 123
Contents

Overview

1
T
he benefits plans contained in your Faculty and Staff Benefits
Handbook are organized into several main sections.
Your benefits plans are designed to provide:
• Protection against the high cost of health and dental care
• Protection of your income in case you become totally and permanently
disabled and cannot work
• Financial assistance for your survivors if you die
• An income for your retirement and other future financial needs
• Assistance with educational expenses for you and your
family members
• Other benefits and opportunities to help you fulfill personal and
professional needs
This handbook explains each benefit plan in detail and will answer ques-
tions you may have now or in the future when you need a particular ben-
efit. You and your family members should review the handbook carefully.
As you read the handbook, please keep in mind that we have summa-
rized your benefits; we have not included every detail. If you have ques-
tions about any of the information in this handbook, contact the Benefits
Sec tion of Human Resources at 617-353-4473 or 4487 or by email at
For information regarding time off from work and other employment poli-
cies, refer to your Employee Handbook, Faculty Handbook, or collective
bargaining agreement.
Your Benefits Handbook

B
oston University began in April
1839, when delegates of the
Methodist Episcopal church met
in Boston to found the Newbury
Biblical Institute. The insti tute
opened in Newbury, Vermont;
moved to Concord, New Hampshire;
and then moved to Boston. In
May 1869, the Common wealth of
Massa chusetts granted a charter
to Boston Univer sity, and the
School of Theol ogy became its
first department.
Thus founded, Boston University
grew, both reflecting and leading
the growth of U.S. higher educa-
tion. From the date of its charter,
it admitted women students to
all programs—the first university
in the country to do so. In 1872, it
opened the nation’s first College of
Music as well as the School of Law,
which would become the first to
require three years for a degree.
In the following year, it opened
the College of Liberal Arts and the
School of Medicine; one-quarter
of the first medical students were
women. The Graduate School,
established the following year, had
by 1875 arranged for tuition-free
study abroad at universities in
Athens and Rome.
Schools and Colleges have con-
tinued to be established and to
evolve. Today they number 16,
offering a vast range of programs
in education, medicine, dentistry,
communication, liberal arts, law,
engineering, social work, arts,
allied health professions, theology,
and management. The College of
General Studies offers a two-year
program in an interdisciplinary core
curriculum, and then students con-
tinue working toward a bachelor’s
degree at one of BU’s four-year
undergraduate schools and colleges.
Metropolitan College provides a
wide range of courses and degree
programs primarily for those who
wish to pursue coursework at night
and on weekends.
Boston University is the fourth-
largest independent institution of
higher education in the country,
and one of the world’s leading
research universities, with over
thirty thousand students in Boston
on the Charles River Campus and
the Medical Campus as well as
in a growing number of programs
around the world. The University
has more than four thousand fac-
ulty members who teach, conduct
research, and use their professional
expertise to serve their worldwide
community. The University’s addi-
tional staff of more than six thou-
sand employees support the efforts
of the University.
Boston University is in itself a com-
munity of vast scholarly, academic,
and recreational resources. Its
members enjoy access to a variety
of University health services, rec-
reational facilities, and activities,
as well as a state-of-the-art library
system. Tuition remission enables
many employees and their spouses
and dependents to take University
courses with full or partial subsidy.
Several exhibits are open on cam-
pus every day, and a night seldom
passes during the academic year
without at least one public concert,
theatrical or operatic performance,
lecture, seminar, or athletic event.
Faculty, students, and staff work
closely with public schools, social
services, and other groups in
Boston and beyond.
Enduring commitments to teach-
ing, research, global education, and
community engagement are the
touchstones of Boston University’s
proud past and promising future.
About Boston University
Overview
Your Benefits Handbook 1
Health Plan 3
Blue Cross Blue Shield PPO 8
Network Blue New England 11
BU Health Savings Plan 13
Medco/Express Scripts Health Prescription Drug Coverage 19
Health Plan Comparison 28
Dental Health Plan 31
The BU Dental Health Center Plan 34
The Dental Blue Freedom Plan 37
Long-Term Disability Plan 49
Survivor Insurance 55
Basic Life Insurance Plan 57
Group Supplemental Life Insurance Plan 58
Personal and Family Accident Insurance Plan 61
Travel Accident Insurance Plan 64
Supplemental Death Benefit Plan 66
Retirement Plan 67
Supplemental Retirement and Savings Plan 81
Tuition Remission Program 93
Tuition Exchange Program 101
Flexible Benefits Program & Flexible Spending Accounts 107
Other Benefits 117
Administrative Information 123
Contents

Overview

1
T
he benefits plans contained in your Faculty and Staff Benefits
Handbook are organized into several main sections.
Your benefits plans are designed to provide:
• Protection against the high cost of health and dental care
• Protection of your income in case you become totally and permanently
disabled and cannot work
• Financial assistance for your survivors if you die
• An income for your retirement and other future financial needs
• Assistance with educational expenses for you and your
family members
• Other benefits and opportunities to help you fulfill personal and
professional needs
This handbook explains each benefit plan in detail and will answer ques-
tions you may have now or in the future when you need a particular ben-
efit. You and your family members should review the handbook carefully.
As you read the handbook, please keep in mind that we have summa-
rized your benefits; we have not included every detail. If you have ques-
tions about any of the information in this handbook, contact the Benefits
Sec tion of Human Resources at 617-353-4473 or 4487 or by email at
For information regarding time off from work and other employment poli-
cies, refer to your Employee Handbook, Faculty Handbook, or collective
bargaining agreement.
Your Benefits Handbook

Health Plan
4
T
he Boston University Health Plan offers various options for medical
coverage for you and your eligible family members. Each option offers
certain benefits to protect you against the medical expenses that would
accompany an illness or injury. There are differences in coverage levels and
how services are obtained in each option. You should give serious consider-
ation to which option will best meet your needs for health care benefits. The
cost of coverage under the Health Plan is shared by you and the University.
The information provided in this section will help you decide which type of
coverage under the Boston University Health Plan is best for you and your
family.
Please note: The descriptions of coverages and benefits in this handbook are
based on the provisions of the Health Plan in effect on the date of this hand-
book. The terms of the Health Plan or the University’s contracts with ven-
dors may change. Actual rights and benefits under the Health Plan are based
on the terms of the official Health Plan documents in effect at any particular
time, and those terms will govern over any inconsistent descriptions in this
handbook.
Furthermore, it is common for annual changes to be made in the Health
Plan. Such annual changes are usually described in the annual enrollment
materials.

5
Eligibility
If you are classified by Boston
University (the “University”) as a
regular employee, work 75% or more
of a full-time schedule, and have
an appointment of nine months’ or
more duration, you and your eligible
family members may participate in
the Boston University Health Plan. If
you are eligible and elect coverage,
it will start on the first day of the
month coincident with or next fol-
lowing your date of hire (depending
on your date of hire).
Your eligible family members include:
• Your legally married spouse
• Under certain circumstances,
your former spouse (see
“Special Provisions for Former
Spouses”)
• To the extent required by law,
your children up to age 26
who are:
o Your biological children
o Your legally adopted children
and children lawfully placed
with you for legal adoption
o Your step-children
• Your unmarried, dependent
children age 26 and over who
are mentally or physically handi-
capped and unable to support
themselves as determined by the
health insurance carrier. (To con-
tinue coverage, your child must
have been handicapped before
age 26 and you must contact
the Benefits Section of Human
Resources before your child’s
26th birthday.)
General Rule—If you become ineligible,
you lose coverage (subject to COBRA).
As an exception, if you drop below 75%,
you may be eligible to continue to par-
ticipate in a health plan option at Boston
University. Please confirm your status with
the Benefits Section of Human Resources.
Coverage Levels
There are four levels of coverage
available under the Health Plan:
• Individual coverage
(yourself only)
• Individual plus spouse
(you and your spouse)
• Individual plus child(ren)
(you and one or more of
your children)
• Family coverage (you and your
eligible family members)
Special Provisions for Former
Spouses
If you have family coverage includ-
ing your spouse and you divorce,
your spouse may continue to be
covered under your family coverage
if the divorce order specifically calls
for this and if neither you nor your
former spouse remarries. If you or
your former spouse remarry, your
former spouse’s eligibility for cover-
age ends. Once coverage ends, your
former spouse may continue cover-
age on an individual basis under
COBRA for the remaining period (if
any) until 36 months have gone by
since your divorce.
If your divorce order specifically
requires coverage for your former
spouse to continue beyond the
COBRA continuation period, your
former spouse may be eligible to
continue coverage under an indi-
vidual plan (if available, under
the Health Plan and the various
vendors providing benefits). This
coverage will continue as long as
you continue to be employed at
the University and have made the
appropriate payment for coverage
or until no longer required by the
divorce order or no longer available.
Special Tax Considerations
Under current tax laws, the value of
your former spouse’s health cover-
age is subject to federal income,
Massachusetts state income, and
Social Security taxes. These tax-
able amounts are based on the full
amount of an individual plan (that
is, employee contribution plus
employer contribution) and are
called imputed income. Imputed
income for your former spouse’s
health coverage will be reported as
income on each paycheck, and will
be included in the taxable earnings
shown on your W-2 Form. Coverage
for your former spouse is subject to
imputed income for tax purposes.
Enrollment
To elect this coverage, new employ-
ees must go to Employee Self Service
at www.bu.edu/buworkscentral.
Alternatively, you may complete a
Benefits Enrollment Form available at
www.bu.edu/hr/files/documents/
enrollment_form.pdf. This form will
authorize a pre-tax reduction in
your pay for your share of the cost
under Section 125 of the Internal
Revenue Code.
If you choose coverage that
includes your spouse or dependent
children, coverage is available only
for the family members who are
listed on your enrollment. If you
wish to enroll newly eligible family
members (for example, a newborn,
an adopted child, or a new spouse),
you may do so by obtaining the
Health Plan

necessary forms from the Human
Resources website at www.bu.edu/
hr/home/forms/benefit-forms.
Alternatively, you may request
a paper form from the Benefits
Section of Human Resources by
email at [email protected].
When Coverage Starts
You have 30 days following your
benefit orientation date to enroll.
If you enroll, coverage will become
eective on the first day of the
month coincident with or follow-
ing the date you become eligible. If
you do not enroll during this period,
your next opportunity to enroll will
be during the next open enrollment
period unless you have a qualifying
change in family status, as deter-
mined by the University.
Cost
You and the University share the
cost of your coverage under the
Health Plan.
Currently, the University pays a
portion of the coverage cost as
determined by the University. Your
share of the cost is the dierence
between the total cost of cover-
age and the amount that Boston
University pays. Costs are subject
to change at the beginning of each
plan year. Also, the University may
change the percentage of the cost
that it will pay.
How Health Plan Contributions
Are Paid
You pay for your portion of the
contributions for your Health Plan
coverage with tax-free dollars. This
is because Boston University auto-
matically reduces your pay by the
amount of your payments—before
federal income taxes, state income
taxes, and Social Security taxes are
taken out.
Automatic before-tax premium pay-
ments are allowed under the provi-
sions of Section 125 of the Internal
Revenue Code. These are explained
in more detail in the “Flexible
Benefits” section of this handbook.
Claim and Appeal Time Frames
for Group Health Claims
Group health claims will be reviewed
and appeals processed by the
applicable Plan Vendor within the
time periods required by law. You
may contact the applicable Plan
Vendor for more information about
claim procedures relating to health
benefits administered by that
Vendor under the Plan. Additional
information about claim and appeal
procedures under a Plan Vendor’s
coverage may also be available in the
Plan Vendor’s benefit description.
Under ERISA claims and appeals
must be decided within a reasonable
time, subject to certain maximum
limits summarized as follows:
Initial Claims After receipt of the
claim, the claim must be decided no
later than:
• As soon as possible but no later
than 72 hours for urgent care
claims
• 15 days for pre-service claims
• 30 days for post-service claims
Claimants have 180 days to appeal
a denied claim.
Appeals of Denied Claims After receipt
of the request for review, the appeal
must be decided no later than:
• As soon as possible but no later
than 72 hours for urgent care
claims
• 30 days for pre-service claims
• 60 days for post-service claims
Special rules apply for the continu-
ation or extension of approved ben-
efits or services to be provided over
time (“concurrent care decisions”).
Individuals receiving approved care
over a period of time must have
an opportunity for review before
benefits are reduced or terminated.
Also, urgent care requests for an
extension of approved benefits must
be decided within 24 hours.
Right to an External Review of
Claims
For certain types of denied claims
(e.g., a claim denied for a lack of
medical necessity), the law provides
that a claimant may be entitled to
request an independent, external
review after the Plan’s final internal
adverse benefit determination. A
claimant may contact the applicable
Plan Vendor with any questions on
his or her rights to external review
by an independent organization.
After a final internal adverse benefit
determination, the applicable Plan
Vendor will advise the claimant of
any right the claimant may have
to an independent external review
and the procedure to request such
a review. If the claimant believes his
or her situation is urgent (generally
one in which the claimant’s health
may be in serious jeopardy or in the
opinion of the claimant’s physician,
the claimant may experience pain
that cannot be adequately con-
trolled while the claimant waits for
a decision on the external review of
his or her claim), the claimant may
request an expedited appeal by con-
tacting the applicable Plan Vendor
for more information.
The claimant or someone the claim-
ant names to act for him or her (the
claimant’s authorized representative)
may file a request for external review.
A claimant may contact the appli-
cable Plan Vendor for information
on how to designate an authorized
representative.
6

Your Health Plan Options
Under Blue Cross Blue Shield, you
may choose one of three options:
1. BCBS PPO is a health care pro-
gram that provides two levels
of coverage: in-network and
out-of-network. You receive the
highest level of benefits under
your health care plan when you
choose preferred providers.
These are called your in-network
benefits. You can also choose
non-preferred providers, but your
out-of-pocket costs are higher.
These are called your out-of-
network benefits.
In-Network Coverage Generally
you have full coverage for most
preferred hospital, physician, and
other provider covered services.
And, for some outpatient ser-
vices, you pay a $20 copayment
for each visit. No claim forms are
required.
Out-of-Network Coverage When
you choose non-preferred
providers you must pay a cal-
endar-year deductible for most
out-of-network services. The cal-
endar-year deductible begins on
January 1 and ends on December
31 each year. The deductible
is $500 for each member (or
$1,000 for all family members
enrolled under the same cover-
age). After you have met your
deductible, you pay 20% coinsur-
ance for most out-of-network
covered services. When the
money you paid for the 20%
coinsurance equals $2,000 (this
is the out-of-pocket limit) for a
member in a calendar year (or
$4,000 for all family members
covered under the same mem-
bership), covered benefits for
that member (or that family) will
be provided in full, based on the
allowed charge, for the rest of
that calendar year (but charges
in excess of reasonable and
customary will not be covered).
Bills for covered outpatient ser-
vices are paid by you and then
submitted on claim forms for
reimbursement.
2. Network Blue New England is
similar to a health maintenance
organization (HMO). An HMO is
a group of aliated physicians,
hospitals, and other health care
providers who have agreed to
provide services at reduced fees.
When you join Network Blue
New England, you select a pri-
mary care physician (PCP) from
the Network Blue New England
network. Your PCP will coordi-
nate your care and refer you for
specialty treatment as needed.
Network Blue New England
provides members with a range
of network benefits, including
routine and preventive services
and hospital care. There are no
deductibles and no claim forms.
Generally, network services
coordinated by your PCP are
covered in full; copayments apply
for doctors’ visits, emergency
room visits, and other services, as
specified by Network Blue New
England. If your PCP is aliated
with Boston Medical Center, your
copayments will generally be less
than if your PCP is a non–Boston
Medical Center physician. Care
that is not approved by your PCP
is generally not covered, except
for emergency treatment.
3. BU Health Savings Plan The BU
Health Savings Plan is a High
Deductible Health Plan that com-
bines the coverage features of a
PPO with the flexibility and tax-
eectiveness of a Health Savings
Account (HSA). Premiums are
lower, but deductibles and out-
of-pocket maximums are higher.
Just like the PPO plan, you are
not required to get referrals from
a primary care provider. You
decide which doctor you want to
see. You pay less when you see
“Preferred Providers” that are
part of our nationwide network,
but the choice is always yours.
In-Network Coverage When you
choose preferred providers you
must pay a calendar-year deduct-
ible for most in-network services.
The calendar-year deductible
begins on January 1 and ends
on December 31 each year. The
deductible is $1,500 for indi-
vidual coverage or $3,000 for
any family coverage. After you
have met your deductible, you
pay 10% coinsurance for most in-
network covered services. When
the money you paid for the 10%
coinsurance equals $3,000 for
individual coverage or $6,000
for any family coverage, benefits
will be provided in full, based on
the allowed charge, for the rest of
that calendar year. Bills for cov-
ered outpatient services are paid
by you and then submitted on
claim forms for reimbursement.
Out-of-Network Coverage When
you choose non-preferred
providers you must pay a cal-
endar-year deductible for most
out-of-network services. The cal-
endar year deductible begins on
January 1 and ends on December
31 each year. The deductible
is $3,000 for individual cover-
age or $6,000 for any family
coverage. After you have met
your deductible, you pay 30%
coinsurance for most out-of-
network covered services. When
the money you paid for the 30%
coinsurance equals $6,000 for
individual coverage or $12,000
for any family coverage, benefits
will be provided in full, based on
7

the allowed charge, for the rest
of that calendar year. Bills for cov-
ered outpatient services are paid
by you and then submitted on
claim forms for reimbursement.
Health Savings Account A Health
Savings Account (HSA) is a tax-
advantaged account used in con-
junction with an HSA-eligible high
deductible health plan (HDHP)
that eligible individuals may
establish to pay for current and
future qualified medical expenses
for themselves, their spouse,
and their qualifying dependents.
The BU Health Savings Plan is an
HSA-eligible HDHP. In connec-
tion with the BU Health Savings
Plan, access is provided to an
HSA administered by Fidelity
Investments if you would like
to make your own pre-tax pay-
roll deductions, and/or wish to
receive the BU HSA contribution.
BCBS PPO
How the BCBS PPO Works
The BCBS PPO is a preferred pro-
vider organization (PPO) that com-
bines the advantages of a national
network with the option to use
physicians and facilities outside the
network, but at a higher cost.
When you join the BCBS PPO, you
are not required to choose a pri-
mary care physician. There are two
levels of coverage. The amount of
coverage depends on where you
receive treatment.
When you receive care from a BCBS
PPO participating provider, you are
covered in full, in and out of the
hospital. You pay only $20 for oce
visits and routine physical exams
and $100 for emergency room care
(this fee is waived if you are imme-
diately hospitalized).
The BCBS PPO also gives you the
option to use non-participating
physicians, specialists, and health
care facilities; your benefits cov-
erage, however, will be lower. If
you receive care outside the plan
network, you will receive 80% cov-
erage for most services (based on
reasonable and customary charges)
after you meet an annual deduct-
ible of $500 (individual coverage)
or $1,00 (family coverage). You pay
the remaining 20% (your coinsur-
ance) and any charges above rea-
sonable and customary limits. Once
your 20% coinsurance reaches
the annual out-of-pocket limit of
$2,000 (individual coverage) or
$4,000 (family coverage), the plan
will pay 100% of covered expenses
for the rest of the calendar year.
In some cases for out-of-network
benefits, you may also have to pay
any balance that is in excess of Blue
Cross Blue Shield’s allowed charge.
Certain expenses do not apply
toward your out-of-pocket limit.
They include the following:
• Charges in excess of reasonable
and customary
• Expenses for services not cov-
ered by the plan
• Charges you incur for not follow-
ing precertification procedures
Emergency Care
Blue Cross Blue Shield provides
benefits for emergency medical ser-
vices whether you are in or outside
of Massachusetts. These emer-
gency medical services may include
inpatient or outpatient services by
providers qualified to furnish emer-
gency medical care and that are
needed to evaluate or stabilize your
emergency medical condition.
In an emergency, such as a sus-
pected heart attack, stroke, or poi-
soning, you should go directly to the
nearest medical facility or call 911
(or the local emergency phone num-
ber). You pay a $100 copayment for
in-network or out-of-network emer-
gency room services. This copay-
ment is waived if you are admitted
to the hospital or for an observation
stay. The out-of-network deductible
does not apply.
Within the Enrollment Area
You will receive full coverage after a
$100 copayment per person per visit
for hospital emergency room treat-
ment you receive at a hospital in the
plan network. This copayment will be
waived, however, if you are immedi-
ately admitted to the hospital.
Outside the Enrollment Area
When you are temporarily outside
the enrollment area, the BCBS PPO
will cover emergency room treat-
ment in full (up to reasonable and
customary charges) after a $100
copayment if the illness or injury
is sudden and life-threatening.
Emergency treatment received at a
physician’s oce outside the enroll-
ment area will be covered in full
after a $20 copayment per person
per visit.
Preventive Care
Preventive care is covered 100% in-
network; and 80% after the deduct-
ible for out-of-network services.
Preventive care includes:
• Well-child care exams, including
routine tests, according to age-
based schedule as follows:
o Ten visits during the first year
of life
o Three visits during the second
year of life
o One visit per calendar year
from age 2 through age 18
• Routine adult physical exams,
including related tests, for mem-
8

bers age 19 or older (one per
calendar year)
• Routine GYN exams, including
related lab tests (one per calen-
dar year)
• Routine hearing exams, including
routine tests
• Routine vision exams (one every
12 months)
• Family planning services (oce
visits)
Home Health Care Benefits
The BCBS PPO pays benefits for
medically necessary home care
services and supplies, such as inter-
mittent skilled nursing care and
physical therapy, at 100% when you
use a participating provider, and at
80% (after the deductible) when
you use an out-of-network provider.
Coverage is also provided for the
following services when deter-
mined to be a medically necessary
component of the intermittent
skilled nursing care or physical
therapy:
• Occupational therapy
• Speech therapy
• Medical social work
• Nutritional consultation
• Home health aide
• Durable medical equipment
Out-of-Network Benefits
You may have to file your claim
when you receive a covered service
from a non-preferred provider in
Massachusetts or a non-preferred
provider outside of Massachusetts
who does not have a payment
agreement with the local Blue
Cross Blue Shield Plan. Claims for
out-of-network services should be
filed, along with Blue Cross Blue
9
Shield claim form (available online
from the Benefits Section of Human
Resources), within two years of the
date charges for the service were
incurred, to:
BCBSMA
P.O. Box 986030
Boston, MA 02298
Note: When you receive cov-
ered services outside the United
States, you must file your claim to
the Blue Card Worldwide Service
Center. (The Blue Card Worldwide
International Claim Form you
receive from Blue Cross Blue Shield
will include the address to mail
your claim.) The service center will
prepare your claim, including the
conversion to US currency, and for-
ward it to Blue Cross Blue Shield for
repayment to you.
Utilization Review Requirements
Utilization Review is an impor-
tant feature of the out-of-network
portion of the BCBS PPO. It helps to
ensure that you receive the appro-
priate medical care in the most
cost-ecient setting—whether it be
the hospital, a specialty facility, or
your own home.
Utilization Review includes:
• Preadmission Review—For all
non-emergency and non-
maternity hospital admissions in
the United States, you must call
1-800-327-6716 in advance to
get your stay approved. Within
two working days of receiving
all necessary information, Blue
Cross Blue Shield will determine
if the health care setting is suit-
able to treat your condition.
Failure to follow the preadmis-
sion review procedure may
result in your having to pay for
expenses that otherwise would
be covered.
• Concurrent Review/Discharge
Planning—This program auto-
matically monitors your stay in
the hospital to help ensure that
you are discharged on time and
receive necessary services once
you are discharged.
Be sure to follow Utilization Review pro-
visions. If you do not follow these provi-
sions, plan benefits will be reduced. The
BCBS PPO benefits are automatically
subject to Utilization Review without
any steps on your part.
Services Not Covered
Under the BCBS PPO, no benefits
are provided for the following:
• Ambulance services unless
necessitated by an emergency
or medical necessity or autho-
rized by Blue Cross Blue Shield
for transfer from one facility to
another
• Any claim submitted more than
two years from the date the ser-
vice was rendered
• Blood and blood products
• Care for military service-
connected disabilities for which
the member is legally entitled
to treatment or services
• Charges in excess of the plan
maximum amount or other limit
• Commercial diet plans or weight-
loss programs
• Cosmetic procedures, except
when medically necessary and
considered medical care under
the Internal Revenue Code
• Cost for any services for which
the member is entitled to treat-
ment at government expense or
under Workers’ Compensation or
occupational disability
• Court-ordered examinations and
services

• Custodial or domiciling care to
assist a member in the activities
of daily living or provide room
and board, training in personal
hygiene, and other forms of self-
care; personal care in the home
except when medically necessary
as part of a treatment plan for a
medical condition
• Dental services, including
periodontal, restorative, and orth-
odontic services
• Educational services (including
problems of school performance)
or testing for developmental,
educational, or behavioral prob-
lems except as medically neces-
sary under an early intervention
program
• Equipment for environmental
control or general household use,
such as air filters, air condition-
ers, air purifiers, liquidizers, bath
seats, bedpans, dehumidifiers,
dentures, elevators, heating pads,
hot water bottles, and humidifiers
• Eyeglasses, contact lenses, and
fittings. This exclusion does not
apply to contact lenses that are
required due to cataract surgery,
covered corneal transplants, and
keratoconus
• Health care services that are not
medically necessary
• Health care services that are
considered experimental
• Health care services that are
considered obsolete and no lon-
ger medically justified
• Health care services furnished to
someone other than the member
• Hearing aids
• Infertility services for members
who are not medically infertile
• Missed appointments
• Nicotine gum
• Non-covered services
• Non-durable medical equipment,
unless used as part of the treat-
ment at a medical facility or as
part of approved home health
care services
• Orthotics
• Osteopathic manipulation,
electrolysis, routine foot care,
biofeedback, pain management
programs, massage therapy, and
acupuncture
• Personal comfort items
• Physical examinations for insur-
ance, licensing, or employment
• Private duty nursing
• Private room unless medically
necessary
• Refractive eye surgery
• Rest or custodial care; personal
comfort or convenience items
• Reversal or attempted reversal
of voluntary sterilization (includ-
ing procedures necessary for
conception following voluntary
sterilization)
• Sensory integrative praxis test;
testing for central auditory
processing
• Services for any person who is
not covered under the plan when
the services are rendered
• Services for which no charges
would have been made in the
absence of coverage under this
plan
• Services incurred after termina-
tion of coverage under the plan
• Services incurred prior to the
eective date of coverage
• Services not specifically
described in this plan document
10
• Services not within the scope
of the physician’s, provider’s, or
hospital’s licensure
• Services or supplies given to
you by anyone related to you by
blood, marriage, or adoption or
who ordinarily lives with you
• Surrogate pregnancy (any form
of surrogacy)
• Temporomandibular joint dys-
function treatment limited to
medical services only
• The portion of the charge for a
service or supply in excess of the
usual, customary, and reasonable
(UCR) charge
• Transsexual surgery, including
related procedures and treat-
ments and reversal of such
procedures
• Weight-loss programs or charges
for weight reduction except when
extreme obesity adversely aects
another medical condition and
treatment is medically necessary
as determined by the plan
For a comprehensive list of services
and conditions not covered by the
BCBS PPO, please refer to the
description for the BCBS PPO avail-
able from the Benefits Section of
Human Resources.
Appealing a Denied Claim
If a claim for benefits is partially or
fully denied, you will receive written
notification, which will include the
reasons for the denial, a description
of any information necessary to com-
plete the processing of your claim,
and information on how to submit
the claim for review.
If you have a question regarding
the payment of a claim, you may
write or call:

Member Grievance Program
Blue Cross Blue Shield
of Massachusetts
One Enterprise Drive
Quincy, MA 02171-2126
Phone: 1-800-472-2689
Fax: 617-246-3616
Email: [email protected]
If you write, be sure to include your
identification number and your
telephone number. Letters will be
answered within 30 days or earlier if
required by law.
You have a right to request a full and
fair review of any claim. If you believe
you or a covered family member
were wrongly denied all or part of
your benefits, you may appeal the
decision. You may submit questions
and comments in writing and review
all pertinent plan documents.
Blue Cross Blue Shield of Mass-
achusetts must review your appeal
and make a final decision within a
reasonable period of time. The final
written decision must state specific
reasons and plan provisions on which
the review decision was based.
Network Blue New England
How Network Blue
New England Works
Network Blue New England is a
health plan with a group of aliated
physicians similar to a health main-
tenance organization. When you
join Network Blue, you and each of
your enrolled family members must
choose a primary care physician
(PCP) from the directory of network
doctors. Your PCP will coordinate
all of your medical care. You may
choose a dierent PCP for each
family member (for example, an
internist for you and a pediatrician
for your children).
Your Primary Care Physician (PCP)
Your copayment for oce visits
will depend on where your PCP
practices.
• If your PCP is aliated with
Boston Medical Center (BMC),
your copayments for oce visits
will be $15 per visit. Oce visits
with a specialist to whom you
are referred by your BMC PCP
will also be $15 per visit.
• If your PCP is not aliated with
Boston Medical Center, your
copayments for oce visits will
be $30 per visit. Oce visits with
a specialist to whom you are
referred by your non-BMC ali-
ated PCP will be $30 per visit.
When you receive care in the
Network Blue New England net-
work, you are covered in full, in and
out of the hospital. You pay $15
BMC PCP/$30 non-BMC PCP for
oce visits or $100 for emergency
room care (this fee is waived if you
are immediately hospitalized). You
receive full coverage for routine
physicals after a copayment. Your
PCP will be part of a team of spe-
cialists aliated with the health
center or hospital where your PCP
practices. If your PCP determines
that you need to see a specialist,
your PCP will refer you to a special-
ist within the plan network. If you
require hospitalization, your PCP
(and specialist, if necessary) will
coordinate your admission, and you
will be covered at 100%.
Urgent vs. Emergency Care
Blue Cross Blue Shield provides ben-
efits for emergency medical services
whether you are in or outside of
Massachusetts. These emergency
medical services may include inpa-
tient or outpatient services by
providers qualified to furnish emer-
gency medical care and that are
needed to evaluate or stabilize your
emergency medical condition. In an
emergency, such as a suspected
heart attack, stroke, or poisoning,
you should go directly to the near-
est medical facility or call 911 (or the
local emergency phone number).
You pay a $100 copayment for
in-network or out-of-network
emergency room services. This
copayment is waived if you are
admitted to the hospital or for an
observation stay.
Routine Physicals
Routine physical exams are covered
in full.
Home Health Care Benefits
People often recover more quickly
when recuperating at home, pro-
vided appropriate care is available.
Needed treatment or therapy—such
as services from nurses or physical
therapists—can be provided in the
comfort of your own home as long
as services are ordered by your PCP
or treating physician and are pro-
vided by a participating Coordinated
Home Health Care agency and as
long as your condition warrants
these services. Network Blue New
England pays benefits for covered
charges made by a participating
Coordinated Home Health Care
agency or a participating Visiting
Nurse Association at 100% when
you use a Network Blue network
provider.
Medically necessary home health
care services and supplies include:
• Part-time home health aide
services, consisting primarily
of care for the patient
• Part-time nursing care
• Physical therapy
11

Services Not Covered
Under Network Blue New England,
no benefits are provided for the
following:
• Ambulance services unless
neces sitated by an emergency or
medical necessity or authorized
in advance by the plan for trans-
fer from one facility to another
• Any claim submitted more than
two years from the date the ser-
vice was rendered
• Blood and blood products
• Care for military service-
connected disabilities for which
the member is legally entitled
to treatment or services
• Charges in excess of the plan
maximum amount or other limit
• Commercial diet plans or weight-
loss programs
• Cosmetic procedures, except
when medically necessary and
considered medical care under
the Internal Revenue Code
• Cost for any services for which
the member is entitled to treat-
ment at government expense or
under Workers’ Compensation
or occupational disability laws
• Court-ordered examinations and
services (unless deemed medi-
cally necessary by the plan)
• Custodial or domiciling care to
assist a member in the activities
of daily living or provide room
and board, training in personal
hygiene, and other forms of self-
care; personal care in the home
except when medically necessary
as part of a treatment plan for a
medical condition
• Dental services, including
periodontal, restorative, and
orthodontic services, and
dentures
• Physical examinations for insur-
ance, licensing, or employment
• Private duty nursing
• Private room unless medically
necessary
• Refractive eye surgery
• Reversal or attempted reversal of
voluntary sterilization (including
procedures necessary for con-
ception following voluntary
sterilization)
• Sensory integrative praxis test;
testing for central auditory
processing
• Services incurred prior to the
eective date of coverage
• Services incurred after termina-
tion of coverage under the plan
• Services for any person who is
not covered under the plan when
the services are rendered
• Services for which no charges
would have been made in the
absence of coverage under this
plan
• Services or supplies from anyone
related to you by blood, mar-
riage, or adoption or who ordi-
narily lives with you
• Services not within the scope
of the physician’s, provider’s, or
hospital’s licensure
• Services that require precertifica-
tion, where the precertification
was not obtained or the precertifi-
cation guidance was not followed
• Services that are not medically
necessary
• Services that are considered
experimental
• Services that are considered
obsolete and no longer medically
justified
• Educational services (including
problems of school performance)
or testing for developmental,
educational, or behavioral prob-
lems except as medically neces-
sary under an early intervention
program
• Equipment for environmental
control or general household use,
such as air filters, air condition-
ers, air purifiers, liquidizers, bath
seats, bedpans, dehumidifiers,
elevators, heating pads, hot water
bottles, and humidifiers
• Eyeglasses, contact lenses, and
fittings. This exclusion does not
apply to eyeglasses and contact
lenses that are required due to
cataract surgery, covered corneal
transplants, and keratoconus
• Hearing aids
• Infertility services for members
who are not medically infertile
• Missed appointments
• Non-covered services even if
precertification was mistakenly
given
• Non-dental medical care ser-
vices only to diagnose and
treat temporomandibular joint
dysfunction
• Non-durable medical equipment,
unless used as part of the treat-
ment at a medical facility or as
part of approved home health
care services
• Non-prescription smoking-
cessation aids
• Orthotics
• Osteopathic manipulation,
electrolysis, routine foot care,
biofeedback, pain management
programs, massage therapy, and
acupuncture
• Personal comfort or convenience
items for rest or custodial care
12

• Services at a residential treat-
ment center
• Surrogate pregnancy (any form
of surrogacy)
• The portion of the charge for a
service or supply in excess of the
usual, customary, and reasonable
(UCR) charge
• Transsexual surgery, including
related procedures and treat-
ments and reversal of such
procedures
• Weight-loss programs or charges
for weight reduction except when
extreme obesity adversely aects
another medical condition and
treatment is medically necessary
as determined by the plan
For a comprehensive list of services
and conditions not covered by
Network Blue New England, please
refer to the description for Network
Blue New England available from
the Benefits Section of Human
Resources.
Appealing a Denied Claim
If a claim for benefits is partially or
fully denied, you will receive written
notification, which will include the
reasons for the denial, a descrip-
tion of any information necessary
to complete the processing of your
claim, and information on how to
submit the claim for review.
If you have a question regarding the
payment of a claim, you may write
or call:
Member Grievance Program
Blue Cross Blue Shield
of Massachusetts
One Enterprise Drive
Quincy, MA 02171-2126
Phone: 1-800-472-2689
Fax: 617-246-3616
Email: [email protected]
If you write, be sure to include
your identification number and
your telephone number. Letters
will be answered within 30 days.
You have a right to request a full
and fair review of any claim. If you
believe you or a covered family
member were wrongly denied all or
part of your benefits, you may appeal
the decision. You may submit ques-
tions and comments in writing and
review all pertinent plan documents.
Blue Cross Blue Shield of Massa-
chusetts must review your ap peal
and make a final decision within
a reasonable period of time. The
final written decision must state
specific reasons and plan provisions
on which the review decision was
based.
Additional information about appeal-
ing a denial of benefits is included
in the “Administrative Information”
section of this handbook.
BU Health Savings Plan
How BU Health Savings
Plan Works
The BU Health Savings Plan is a
high deductible health plan (HDHP)
administered by Blue Cross Blue
Shield of Massachusetts and
Medco/Express Scripts. Participants
in this HDHP have access to a
Health Savings Account (HSA)
administered through Fidelity
Investments.
The BU Health Savings Plan oers
the same network of doctors and
hospitals available under the BCBS
PPO, including BMC and its aliated
providers. The BU Health Savings Plan
prescription drug benefit is adminis-
tered through Medco/Express Scripts
and covers the same prescription
drugs as the other University oerings.
The BU Health Savings Plan provides
both in- and out-of-network cover-
age, just like the preferred provider
organization (PPO) plan. However,
the BU Health Savings Plan works
dierently in these key ways:
• Except for certain in-network pre-
ventive care services, all covered
health expenses are subject to
a plan deductible, including pre-
scription drugs.
• Under employee plus child(ren),
employee plus spouse, and fam-
ily coverage, the entire family
deductible must be met before
benefits are payable for any cov-
ered person.
• There are no copays, just coinsur-
ance (once the deductible is met),
even for oce and emergency
room visits, mental health care,
and prescription drugs.
The Deductible
You must meet the plan-year
deductible before you can receive
coverage for most services under
this plan. Your plan year begins
January 1 and ends on December 31
each year.
This table shows the deductibles
for in-network and out-of-network
services.
*If you have a plan that covers
employee plus spouse, or employee
plus child(ren), or family, you must
meet the higher family deductible
before you receive coverage.
Services Received from an
In-Network Provider
Once the deductible is met, most
services are covered 90%. You pay
10% coinsurance. When the amount
13
In-Network
Providers
Out-of-Network
Providers
$1,500 for indi-
vidual coverage,
or $3,000 for any
family coverage*
$3,000 for indi-
vidual coverage,
or $6,000 for any
family coverage*
Annual Deductible
you have paid in deductible and
coinsurance reaches $3,000 for an
individual plan, or $6,000 for any
family plan, covered benefits will be
paid in full (i.e., without any addi-
tional deductibles or coinsurance,
but subject to all plan provisions,
limitations, and exclusions) for the
remainder of that plan year.
Services Received from an
Out-of-Network Provider
Once the deductible is met, most out-
of-network services are covered 70%.
You pay 30% coinsurance. When the
amount you have paid in deductible
and coinsurance reaches $6,000 for
an individual plan, or $12,000 for any
family plan, covered benefits will be
paid in full (i.e., without any additional
deductibles or coinsurance, but sub-
ject to all plan provisions, limitations,
and exclusions) for the remainder
of that plan year.
Certain expenses do not apply
toward your out-of-pocket limit and
are excluded under the plan. They
include the following:
• Charges in excess of reasonable
and customary
• Expenses for services not cov-
ered by the plan
• Charges you incur for not follow-
ing precertification procedures
Emergency Care
Blue Cross Blue Shield provides
benefits for emergency medical
services whether you are in or
outside of Massachusetts. These
emergency medical services may
include inpatient or outpatient
services by providers qualified to
furnish emergency medical care
and that are needed to evaluate or
stabilize your emergency medical
condition. In an emergency, such
as a suspected heart attack, stroke,
or poisoning, you should go directly
Coverage is also provided for the
following services when determined
to be a medically necessary compo-
nent of the intermittent skilled nurs-
ing care or physical therapy:
• Occupational therapy
• Speech therapy
• Medical social work
• Nutritional consultation
• Home health aide
• Durable medical equipment
Utilization Review Requirements
Utilization Review is an important
feature of the out-of-network por-
tion of the BU Health Savings Plan.
It helps to ensure that you receive
the appropriate medical care in the
most cost ecient setting—whether
it be the hospital, a specialty facility,
or your own home.
Utilization Review includes:
• Preadmission Review—For
all non-emergency and non-
maternity hospital admissions
in the United States, you must
call the number on your ID card
in advance to get your stay
approved. Within two working
days of receiving all necessary
information, Blue Cross Blue
Shield will determine if the
health care setting is suitable to
treat your condition. Failure to
follow the preadmission review
procedure may result in your
having to pay for expenses that
otherwise would be covered.
• Concurrent Review/Discharge
Planning—This program auto-
matically monitors your stay in
the hospital to help ensure that
you are discharged on time and
receive necessary services once
you are discharged.
14
to the nearest medical facility or
call 911 (or the local emergency
phone number). You pay a 10%
coinsurance after the deductible
for in-network or out-of-network
emergency room services.
Preventive Care
Preventive care is covered 100%
with no deductible for in-network
care.
Out-of-network preventive care is
covered at 70% with no deductible.
• Well-child care exams, including
routine tests, according to age-
based schedule as follows:
o Ten visits during the first year
of life
o Three visits during the second
year of life
o One visit per calendar year
from age 2 through age 18
• Routine adult physical exams,
including related tests, for mem-
bers age 19 or older (one per
calendar year)
• Routine GYN exams, including
related lab tests (one per calen-
dar year)
• Routine hearing exams, including
routine tests
• Routine vision exams (one every
12 months)
• Family planning services (oce
visits)
Home Health Care Benefits
The BU Health Savings Plan pays
benefits for medically necessary
home care services and supplies,
such as intermittent skilled nursing
care and physical therapy, at 90%
(after the deductible) when you use
a participating provider, and at 70%
(after the deductible) when you use
an out-of-network provider.

Be sure to follow Utilization Review pro-
visions. If you do not follow these provi-
sions, plan benefits will be reduced.
Services Not Covered
Under the BU Health Savings Plan,
no benefits are provided for the
following:
• Ambulance services unless
necessitated by an emergency
or medical necessity or autho-
rized by Blue Cross Blue Shield
for transfer from one facility to
another
• Any claim submitted more than
two years from the date the ser-
vice was rendered
• Blood: whole blood; packed red
blood cells; blood donor fees; and
blood storage fees
• Care for military service con-
nected disabilities for which the
member is legally entitled to
treatment or services
• Charges in excess of the plan
maximum amount or other limit
• Commercial diet plans or weight-
loss programs
• Cosmetic procedures, except
when medically necessary and
considered medical care under
the Internal Revenue Code
• Cost for any services for which
the member is entitled to treat-
ment at government expense or
under Workers’ Compensation
or occupational disability
• Court-ordered examinations and
services
• Custodial or domiciling care to
assist a member in the activities
of daily living or provide room
and board, training in personal
hygiene, and other forms of self-
care; personal care in the home
except when medically neces-
sary as part of a treatment plan
for a medical condition
• Dental services, including peri-
odontal, restorative, and orth-
odontic services
• Educational services (includ-
ing problems of school per-
formance) or testing for
developmental, educational, or
behavioral problems except as
medically necessary under an
early intervention program
• Equipment for environmental
control or general household use,
such as air filters, air condition-
ers, air purifiers, liquidizers, bath
seats, bedpans, dehumidifiers,
dentures, elevators, heating
pads, hot water bottles, and
humidifiers
• Eyeglasses, contact lenses, and
fittings. This exclusion does not
apply to contact lenses that are
required due to cataract surgery,
covered corneal transplants, and
keratoconus
• Health care services that are not
medically necessary
• Health care services that are
considered experimental
• Health care services that are
considered obsolete and no lon-
ger medically justified
• Health care services furnished to
someone other than the member
• Hearing aids
• Missed appointments
• Nicotine gum
• Non-covered providers
• Non-covered services
• Non-durable medical equipment,
unless used as part of the treat-
ment at a medical facility or as
part of approved home health
care services
• Orthotics
• Osteopathic manipulation,
electrolysis, routine foot care,
biofeedback, pain management
programs, massage therapy, and
acupuncture
• Personal comfort items
• Physical examinations for insur-
ance, licensing, or employment
• Private duty nursing
• Private room charges
• Refractive eye surgery
• Rest or custodial care; personal
comfort or convenience items
• Reversal or attempted reversal
of voluntary sterilization (includ-
ing procedures necessary for
conception following voluntary
sterilization)
• Sensory integrative praxis test;
testing for central auditory
processing
• Services for any person who is
not covered under the plan when
the services are rendered
• Services for which no charges
would have been made in the
absence of coverage under this
plan
• Services incurred after termina-
tion of coverage under the plan
• Services incurred prior to the
eective date of coverage
• Services not specifically
described in this plan document
• Services not within the scope
of the physician’s, provider’s, or
hospital’s licensure
• Services or supplies given to
you by anyone related to you by
blood, marriage, or adoption or
who ordinarily lives with you
15
Accounts and Other Tax-Favored
Health Plans.” If you have an HSA,
you should carefully review that
publication. If you have legal, tax, or
financial questions about HSAs, you
should consult your own profes-
sional advisor at your own expense.
ERISA does not apply to HSAs and
the University is not a fiduciary of
any HSA.
HSA Eligibility
You are eligible to open a Fidelity
HSA if:
You become covered under the BU
Health Savings Plan, a qualifying
high deductible health plan, and
You are not enrolled in Medicare
and have not received medi-
cal benefits within the last three
months through the Veteran’s
Administration (VA), and
You cannot be claimed as a depen-
dent on another person’s tax return.
You are NOT eligible to open a
Fidelity HSA if:
You are not covered under the BU
Health Savings Plan.
You are enrolled in Medicare or have
received medical benefits within the
last three months through the VA.
You can be claimed as a dependent
on another person’s tax return.
IMPORTANT: You may also not
open an HSA while you are covered
under another health plan that is
not a qualifying HDHP. For exam-
ple, you cannot also be covered
under a health care flexible spend-
ing arrangement (FSA) of your own
or under an FSA of your spouse
through his or her employer. Also,
you cannot be covered as a depen-
dent of your spouse under the
group health plan of your spouse’s
employer if that group health plan
is not a qualifying HDHP.
16
• Surrogate pregnancy (any form
of surrogacy)
• Temporomandibular joint dys-
function treatment limited to
medical services only
• The portion of the charge for a
service or supply in excess of the
usual, customary, and reasonable
(UCR) charge
• Transsexual surgery, including
related procedures and treat-
ments and reversal of such
procedures
• Weight-loss programs or
charges for weight reduction
except when extreme obesity
adversely aects another medi-
cal condition and treatment is
medically necessary as deter-
mined by the plan
Appealing a Denied Claim
If a claim for benefits is partially
or fully denied, you will receive
written notification, which will
include the reasons for the denial, a
description of any information nec-
essary to complete the processing
of your claim, and information on
how to submit the claim for review.
If you have a question regarding the
payment of a claim, you may write
or call:
Member Grievance Program
Blue Cross Blue Shield
of Massachusetts
One Enterprise Drive
Quincy, MA 02171-2126
Phone: 1-800-472-2689
Fax: 617-246-3616
Email: [email protected]
If you write, be sure to include
your identification number and
your telephone number. Letters
will be answered within 30 days.
You have a right to request a full
and fair review of any claim. If
you believe you or a covered fam-
ily member were wrongly denied
all or part of your benefits, you
may appeal the decision. You may
submit questions and comments
in writing and review all pertinent
plan documents.
Blue Cross Blue Shield of Massa-
chusetts must review your ap peal
and make a final decision within
a reasonable period of time. The
final written decision must state
specific reasons and plan provi-
sions on which the review decision
was based.
Additional information about appeal-
ing a denial of benefits is included
in the “Administrative Information”
section of this handbook.
Health Savings Account
(HSA)
A Health Savings Account (HSA)
is a tax-advantaged account used
in conjunction with an HSA-eligible
high deductible health plan (HDHP)
that eligible individuals may estab-
lish to pay for current and future
qualified medical expenses for
themselves, their spouse, and their
qualifying dependents. The BU
Health Savings Plan is an HSA-
eligible HDHP. In connection with
the BU Health Savings Plan, access is
provided to an HSA administered by
Fidelity Investments if you would like
to make your own pre-tax payroll
deductions, and/or wish to receive
the BU HSA contribution. You are,
however, free to choose any HSA
vendor for your own after-tax con-
tributions or move money from your
Fidelity-administered HSA to an
HSA administered by another entity
in accordance with IRS rules.
The legal and tax rules relating to
HSAs can be complicated. A sum-
mary of those rules is contained in
IRS Publication 969 “Health Savings

• When you elect the BU Health
Savings Plan, you may also elect
to open an HSA. If you do, the
University will automatically
deposit $500 as a contribution
to your Fidelity-administered
HSA account.*
• You don’t need to use Fidelity
for the HSA. However, if you
want to automatically have the
HSA contributions come from
your paycheck, you will have to
establish a Fidelity account on
their website NetBenefits® at
netbenefits.com.
• You may elect to contribute to
your HSA, pre-tax, up to the
annual limits. For 2013 the limits
are $3,250 for employee only
and $6,450 if you have fam-
ily coverage. These limits are
reduced by any contributions
by the University to your HSA,
e.g., if the University contributed
$500 to your HSA and you have
employee-only coverage under
the BU Health Savings Plan,
your remaining maximum HSA
contribution for the remainder
of the year would be $2,750
($3,250–$500). If you are age
55 or older in 2013, you may
make additional pre-tax “catch-
up” contributions, up to $1,000
per year.
• You are not required to contrib-
ute to the HSA to participate in
the BU Health Savings Plan.
• You must, however, open a
Fidelity HSA in order to receive
the University contribution to
that HSA.
17
2013 Individual Family
Annual HSA Contribution $3,250 $6,450
Limits
Catch-up Contribution Limit $1,000 $1,000
(for those age 55 and older)
documents/BN_enrollment_
form.pdf.
2. Once you have submitted your
enrollment, your payroll contri-
butions will be set up.
3. Fidelity Investments will be
informed by Human Resources
that you have enrolled and are
eligible to open your Fidelity HSA.
4. Fidelity will contact you via email
or telephone with instructions
to set up your account through
NetBenefits (www.netbenefits.
com).
5. Once you have completed the
account set up, payroll deductions
will begin and your pre-tax contri-
butions will be sent to Fidelity.
6. After your first contribution, BU
will contribute the $500 seed
money. Any money in your HSA
is immediately available for
you to use for qualified medical
expenses.
Your Fidelity HSA Investments
The Fidelity HSA is a Fidelity
brokerage account that has a
“core position” through which all
contributions are deposited and all
disbursements are withdrawn. This
“core position” is an FDIC-Insured
Deposit Sweep. Once your account
balance exceeds $2,500, you can
choose to invest in a broad range
of options, including a full range
of Fidelity mutual funds, more
than 4,000 non-Fidelity funds,
and individual stocks and bonds.
Any earnings on your Fidelity HSA
investments are automatically
reinvested and grow tax free.
Funding Your HSA
• Pre-Tax Contributions—Your pay-
roll deductions are taken on a pre-
tax basis to fund your account.
You may change your payroll
deduction amount on a monthly
• You may also contribute after-
tax funds by check and claim
them as deductions on your
income tax return.
• You may prospectively change
your pre-tax salary reduction
HSA contribution amounts on a
monthly basis.
• You are always 100% vested
in both the amount Boston
University contributes to your
account and in your HSA
contributions.
• You decide whether to save for
qualified expenses you incur now
or in the future; any funds you
withdraw to pay for qualified
medical expenses are tax-free.
• You may request a debit card
and special checkbook to provide
you access to your HSA funds,
and you may use these even if
you terminate employment with
Boston University or drop your
membership in the BU Health
Savings Plan. The debit card
can be requested online at
netbenefits.com or requested
by phone at 800-343-0860.
* The amount (if any) of University
HSA contributions is subject to re-
view and change by the University at
any time. The University reserves the
right, in its sole discretion, to discon-
tinue HSA contributions at any time.
Opening Your Fidelity HSA
You may enroll in the HSA at any
time if you are enrolled in the BU
Health Savings Plan. This is the
process to follow to establish your
account:
1. You may enroll either via
Employee Self Service at www.
bu.edu/buworkscentral or by
completing a paper Benefits
Enrollment Form available
at: www.bu.edu/hr/files/
basis. Total contributions to your
account do not exceed your maxi-
mum annual contribution amount.
• After-Tax Contributions—You may
make after-tax contributions by
check. After-tax contributions
are tax deductible to the extent
that total contributions to your
account do not exceed your
maximum annual contribution
amount.
Accessing Your HSA Funds
Fidelity has three methods by which
you can access your HSA funds to
pay for qualified medical expenses:
• Fidelity BillPay for Health
Savings Accounts—You can
make online payments to
health care providers, compa-
nies, and individuals. You can
set up an automatic schedule
for your payments and keep
track of all bill payments for
qualified medical expenses.
• Fidelity HSA Debit Card—Use at
the point of service.
• Fidelity HSA Checkbook—Use
when you need it.
Distribution Records
You must keep all receipts and
records of medical expenses paid
with your Fidelity HSA funds
to document sufficiently that
distributions have been made
exclusively for qualified medi-
cal expenses. You should keep
these items for your own records;
do not submit them to Fidelity.
Distributions from your HSA will
also be reported by Fidelity to you
and the IRS each tax year on IRS
Form 1099-SA. If your tax return
is audited by the IRS, you might
be asked to provide receipts for
qualified medical expenses paid
for before receiving distributions
from your Fidelity HSA.
Using Your HSA for Nonqualified
Medical Expenses
Distributions from your Fidelity
HSA that are used to pay for or
reimburse nonqualified medical
expenses must be included in your
gross income for tax purposes and
are subject to an additional 20%
penalty. The 20% penalty does not
apply to distributions made if you
become disabled, once you reach
age 65, or after your death.
Using Your HSA for a Dependent
Child
You may use your HSA to pay
for qualified medical expenses
incurred by your dependent child
as long as your child is consid-
ered a dependent for federal tax
purposes. Otherwise, you will pay
a penalty plus taxes. According to
IRS guidelines, a dependent child
for tax purposes includes one of
the following:
• A dependent you can claim on
your tax return
• A dependent that you could
have claimed on your tax return
except that they had gross
income of $3,650 or more
Fidelity HSA Fees
The following fees apply to a Fidelity
HSA:
• Generally, Fidelity HSAs are
subject to an annual account
maintenance fee. This fee is
paid by Boston University as
long as you are actively con-
tributing to the HSA. If you
are not contributing, the fee
is deducted from your account
on a quarterly basis.
• A fee may apply for ordering
checkbooks for your HSA.
Note: Other fees may apply; please
refer to the Brokerage Commission
and Schedule of Fees in the Fidelity
Brokerage HSA Customer Agree-
ment or on NetBenefits for addi-
tional information.
Unused Funds
HSAs are not subject to the use-
it-or-lose-it rule; therefore, funds
remain in your account from year
to year. Any unused funds may
be used to pay for future qualified
medical expenses.
Transfer of Assets
You may transfer funds from
another HSA custodian through
a transfer of assets transaction
as long as the account type is the
same.
Fidelity will coordinate the transfer
from the other institution after you
complete and return the completed
Transfer of Assets form, which can
be found at Fidelity.com > Customer
Service > Find a Form.
The transfer will not be considered
a taxable event and will not be
reported to the IRS. Additionally,
Fidelity does not charge fees on
this transaction. You should always
consult the fee schedule of your
other HSA to understand any fees or
changes that may apply.
Please note that eligible transfers
are not included when calculating
your maximum annual contribution
amount.
How Medicare Aects Your
Fidelity HSA
• Once you are enrolled in
Medicare, you will no longer be
eligible to make contributions,
including catch-up contributions,
to your Fidelity HSA.
• You can use funds in your
Fidelity HSA to pay Medicare
premiums, deductibles, co-pays,
18

and coinsurance under any part
of Medicare. If you are retired
and have retiree health benefits
through a former employer, you
can also use your account to pay
for retiree medical insurance
premiums. You cannot use your
account to purchase Medicare
supplemental insurance, or
“Medigap,” policies.
• Distributions you take after age
65 to pay for expenses other
than qualified medical expenses
will still be considered taxable
income; however, they will no
longer be subject to the 20%
penalty.
Medco/Express Scripts
Health Prescription Drug
Coverage
The guidelines here apply to the
BCBS PPO and Network Blue New
England. The BU Health Savings
Plan oers 80% coverage once the
annual deductible is met. There are
no copayments for members of the
BUHSP.
As a member of the Boston
University Health Plan, you will
automatically be enrolled in the
Medco/Express Scripts Health
Prescription Drug Coverage.
Prescription copayments vary
depending on whether your pre-
scribed medication is a generic,
preferred brand-name, or non-
preferred brand-name drug.
Preferred brand-name medications
are selected based on their clinical
eectiveness and opportunities for
savings. An independent Pharmacy
and Therapeutics Committee at
Medco/Express Scripts updates
this list regularly based on continu-
ous evaluation of medications.
Members can determine if their
brand-name medications are pre-
ferred or non-preferred by logging
on to www.express-scripts.com and
choosing the Drug Information option.
Many preferred and non-preferred
brand-name drugs have a generic
alternative. If you use the generic
drug, your copayment will be $8
for up to a 30-day supply at a retail
pharmacy. Certain medications have
quantity and/or dollar limits. Please
view the Medco Member Brochure
on the Human Resources website at
www.bu.edu/hr/files/documents/
Medco_member_brochure.pdf.
Prior Authorization
The plan covers medically neces-
sary prescription medication.
Some drugs require prior autho-
rization in order to be covered by
the plan. Visit the Medco/Express
Scripts website at www.express-
scripts.com and click on Drug
Information to find out about a
specific medication.
To obtain prior approval, your
doctor should call Medco/Express
Scripts toll-free at 1-800-753-2851.
This call will initiate a review that
typically takes one to two busi-
ness days. Once the review is
complete, Medco/Express Scripts
will notify you and your doctor of
the decision.
Retail Pharmacy
If you need short-term medication
(perhaps for the flu or an ear infec-
tion), under the Retail Network
Pharmacy Service you can take your
prescription to almost any major
chain and many independent phar-
macies, show your ID card, pay your
copayment, and go home with your
prescription.
For preferred brand-name medi-
cations, you will pay 20% coin-
surance, and for non-preferred
brand-name prescriptions, you will
pay 30% coinsurance for up to a
30-day supply of each prescription
with a minimum and maximum
out-of-pocket cost as shown in the
chart below.
Home Delivery
Pharmacy Service
If you take medication for a chronic
condition, such as diabetes or
asthma, you can get a prescrip-
tion from your doctor for up to a
90-day supply plus refills for the
rest of the year, and then order
your medication through the
Home Delivery Pharmacy Service.
You can place your order by mail,
online, over the phone, or by having
your physician fax the prescription
to Medco/Express Scripts. There
are no shipping costs unless you
request express shipping. Regular
mail takes 7–11 days from the date
you place your order; it’s faster if
you order by phone, Internet, or
fax. A refill slip, including the date
you can order the next refill, will
come with every order. It’s safe,
easy, and the lowest-cost way to
purchase your medication. Please
see the chart on the next page.
19
Type of
Medication
Up to a 30-Day Supply
Up to a 30-Day Supply
Preferred 20% coinsurance
Brand-Name minimum cost $30
maximum cost $50
—per each prescription
Non-Preferred 30% coinsurance
Brand-Name minimum cost $50
maximum cost $70
—per each prescription
Generic $8 Copayment
20% coinsurance after deductible
BCBS PPO & Network
Blue New England
BU Health Savings Plan
Retail Pharmacy

Contact Information
Medco/Express Scripts website:
www.express-scripts.com or
Customer Service: 1-800-230-0508.
To refill a Home Delivery Pharmacy
Service prescription: 1-800-4REFILL
(1-800-473-3455).
Appealing a Denied Claim
In the event you receive an adverse
benefit determination following a
request for coverage of a prescrip-
tion benefit claim, you have the right
to appeal the adverse benefit deter-
mination in writing within 180 days
of receipt of notice of the initial cov-
erage decision. To initiate an appeal
for coverage, you or your authorized
representative (such as your physi-
cian) must provide, in writing, your
name, member ID, phone number,
the prescription drug for which
benefit coverage has been denied,
and any additional information that
may be relevant to your appeal. This
information should be mailed to:
Express Scripts
P.O. Box 631850
Irving, TX 75063-0030
Attention: Appeals
A decision regarding your appeal
will be sent to you within 15 days
of receipt of your written request.
The notice will include the specific
reasons for the decision and the
plan provisions on which the deci-
sion is based. You have the right
to receive, upon request and at no
charge, the information used to
review your appeal.
If you are not satisfied with the cover-
age decision made on appeal, you
may request in writing, within 180
days of the receipt of notice of the
decision, a second-level appeal. To
initiate a second-level appeal, you or
your authorized representative (such
as your physician) must provide
in writing your name, member ID,
phone number, the prescription drug
for which benefit coverage has been
denied, and any additional informa-
tion that may be relevant to your
appeal. This information should be
mailed to:
Express Scripts
P.O. Box 631850
Irving, TX 75063-0030
Attention: Appeals
A decision regarding your request
will be sent to you in writing within
15 days of receipt of your written
request for appeal. You have the
right to receive, upon request and
at no charge, the information used
to review your second-level appeal.
The decision made on your second-
level appeal is final and binding.
If you are not satisfied with the
decision of the second-level
appeal, you also have the right
to bring a civil action under sec-
tion 502(a) of the Employee
Retirement Income Security Act of
1974 (ERISA) if your second-level
appeal is denied.
In the case of a claim for coverage
involving urgent care, you will be noti-
fied of the benefit determination within
72 hours of receipt of the claim. An
urgent care claim is any claim for treat-
ment with respect to which the appli-
cation of the time periods for making
non-urgent care determinations could
seriously jeopardize the life or health of
the claimant or the ability of the claim-
ant to regain maximum function, or, in
the opinion of a physician with knowl-
edge of the claimant’s medical condi-
tion, would subject the claimant to
severe pain that cannot be adequately
managed. If the claim does not contain
sucient information to determine
whether, or to what extent, benefits
are covered, you will be notified within
24 hours after receipt of your claim of
the information necessary to complete
the claim. You will then have 48 hours
to provide the information and will
be notified of the decision within 48
hours of receipt of the information.
You have the right to request an
urgent appeal of an adverse benefit
determination if you request cover-
age of a claim that is urgent. Urgent
appeal requests may be oral or writ-
ten. You or your physician may call
1-800-652-4840 or send a written
request to:
Express Scripts
P.O. Box 631850
Irving, TX 75063-0030
Attention: Appeals
In the case of an urgent appeal for
coverage involving urgent care,
you will be notified of the benefit
determination within 72 hours of
receipt of the claim. This coverage
decision is final and binding. You
have the right to receive, upon
request and at no charge, the
information used to review your
appeal. You also have the right
to bring a civil action under sec-
tion 502(a) of ERISA if your final
appeal is denied.
20
Type of
Medication
Up to a 90-Day Supply
Up to a 90-Day Supply
Preferred 20% coinsurance
Brand-Name minimum cost $60
maximum cost $100
—per each prescription
Non-Preferred 30% coinsurance
Brand-Name minimum cost $100
maximum cost $140
—per each prescription
Generic $16 Copayment
20% coinsurance after deductible
BCBS PPO & Network
Blue New England
BU Health Savings Plan
Home Delivery

Other Information
Coordination of Benefits
The Boston University Health Plan
has provisions for coordination of
benefits with other health care plans
covering you or any of your covered
dependents. This prevents overpay-
ments to health care service providers.
If a member is covered by more than
one insurance or self-insurance plan
(including Workers’ Compensation
and auto insurance), the plans will
coordinate the payment of costs so
that total payments will not exceed the
member’s actual expenses.
If you are covered by more than one
medical plan, contact the Benefits
Section of Human Resources for
more information on coordination
of benefits and how to file a claim.
Subrogation and Reimbursement
The Boston University Health Plan
also has a subrogation and reim-
bursement rule. If another party
is, or is claimed to be, responsible
(the “responsible party”) for an ill-
ness or injury inflicted on you or a
covered dependent, the Health Plan
is entitled to reimbursement out of
any recovery from the responsible
party (or any insurer, including
any liability insurer, uninsured or
underinsured motorist insurer, or
homeowner insurer) for amounts
expended by the plan for health
care to the covered individual. The
covered individual must cooperate
with the Health Plan to recover such
amounts. If the covered individual
receives payment from the respon-
sible party (or any insurer, includ-
ing any liability insurer, uninsured
or underinsured motorist insurer,
or homeowner insurer) before
the Health Plan receives amounts
expended for such individual’s
care, the covered individual must
hold any amount recovered from
the responsible party in trust for
the benefit of the Health Plan to
the extent of amounts paid by the
Health Plan for care, and must repay
the Health Plan from the amounts
recovered even if the amounts
recovered do not fully compensate
the covered individual for all of his
or her losses, damages, or expenses.
If You Incur a Total Disability
If you incur a total disability and
begin receiving benefits from the
Boston University Long-Term
Disability Benefits Plan, coverage for
you and your eligible dependents in
the Boston University Health Plan
may continue at no cost to you for
the duration of your total disability
while you continue to receive ben-
efits under the Boston University
Long-Term Disability Plan. The
Benefits Section of Human Resources
will explain this feature to you upon
notification of your disability.
For the first 24 months of your
dis ability, your health plan member-
ship will be continued through Boston
University at no cost to you. During
this time, your Boston University
Health Plan will be your primary
health plan provider (except as oth-
erwise provided under coordination
of benefits). After you have been dis-
abled for 24 months, you must enroll
in Medicare Parts A and B if you are
eligible. At this time, Medicare will
become your primary health plan
provider, with your Boston University
Health Plan as your secondary health
plan provider. In other words, your
claims will be paid by Medicare first;
Boston University Health Plan will
pay for covered services (subject to
required deductibles and coinsur-
ance payments) to the extent that
Medicare did not pay them. Thus,
your overall health benefits will be
the same as those of other Health
Plan members in the same coverage
option as you, except that part of your
benefits will come from Medicare.
There is, however, a monthly pre-
mium for Medicare Part B, which will
become your responsibility upon your
enrollment in Medicare.
Please note: You are responsible for
applying for Medicare coverage after
you have been disabled for two years. If
you are disabled, your medical claims
will be paid by the Boston University
Health Plan as though you have
Medicare coverage, unless you pro-
vide evidence that your application
for Medicare coverage was denied.
If You Die While You Are a
Member of the Plan
If you die while you are a member
of the Health Plan, your enrolled
dependents will be entitled to con-
tinue coverage under COBRA for up
to 36 months.
If You Are Actively Employed
When You Reach Age 65
If you are actively employed by
Boston University at age 65,
your membership in the Boston
University Health Plan will con-
tinue as your primary insur-
ance. You may delay enrolling in
21
Your Health Insurance Coverage Options at Age 65
Boston University Medicare Parts
Health Plan A & B only
Active employee (and spouse) Available (with Available
age 65 and over Medicare as
secondary coverage)
Retired employee (and spouse) Not an option Available
age 65 and over (except for COBRA)
*

Medicare Part B without a penalty
as long as you remain covered as
an employee under the Boston
University Health Plan as a result
of your current employment status.
When you reach age 65, you should
contact the Social Security Admin-
istration by calling 1-800-772-1213
to enroll in Medicare Part A.
If you retire on or after age 65, your
Health Plan coverage will end. You
may decide to continue your Health
Plan coverage through COBRA.
About Medicare
When you reach age 65, you
become entitled to coverage under
Medicare, the health plan admin-
istered through the Social Security
Administration. Medicare coverage
is not automatic; you must enroll
through Social Security.
Medicare coverage has three parts.
• Part A: Provides hospital insur-
ance and requires no premium
payment from you.
• Part B: Provides supplementary
medical insurance and requires a
premium payment from you.
• Part D: Provides prescription
drug coverage.
The chart on page 21 summarizes
health insurance coverage options
available to you at age 65.
Three months before your 65th
birthday, you should contact your
local Social Security oce regarding
Medicare benefits.
In addition to Medicare Parts A
and B, you may also wish to enroll
in a non-group health plan that will
augment your Part B coverage. This
kind of plan, called a “Medicare
Supple ment,” will fill in some of the
gaps in Medicare, giving you more
complete coverage.
The University has entered into an
agreement with Ovations of United
Health Group to oer to retirees the
nationwide Medicare supplement
plans that are available under AARP
Health Care Options. Retirees may
also obtain their prescription drug
coverage through this program.
The cost of the plan must be paid
by the retiree in full. The premium
for these plans will be the same
as the premium paid by all other
AARP members; however, the
annual AARP membership fee for
the first year will be paid on behalf
of the retiree to facilitate enrollment
through the University. Also, the
University will pay the first month’s
premium cost for current employees
who enroll in this plan upon ocial
retirement from Boston University.
In addition, retirees who enroll in one
of the AARP Health Care Options
through the University will also have
the option to enroll in a discount
program oered by United Health
Group which provides discounts for
cosmetic dentistry, assisted living,
hearing care, and wellness care.
For details about AARP Health
Care Options, please call 1-800-
545-1797.
For reimbursement once you have
retired and paid the first month’s
premium, send a copy of your bill or
receipt and your Boston University
ID number to: Benefits Section,
Boston University Human Resources,
25 Buick Street, Boston, MA 02215.
Alternatively, various “Medicare
Advantage Plans” are available
for your consideration. Go to
www.medicare.gov for a list of
plans available as well as what
they cover and the costs. Contact
the Benefits Section of Human
Resources for more information.
Leaves of Absence and No-Pay
Status
If you are on a leave of absence or
no-pay status, you must contact
the Benefits Section of Human
Resources to ask what impact your
absence may have on your partici-
pation in the Health Plan.
• Leave of Absence with Pay If you
are granted a leave of absence
with pay (including sabbatical),
your Health Plan coverage will
continue, provided your usual
payroll deductions continue. If
you wish to discontinue your
membership, you may do so by
notifying, in writing, the Benefits
Section of Human Resources, 25
Buick Street, Boston, MA 02215.
• Leave of Absence Without Pay
and No-Pay Status If you are
granted a leave of absence with-
out pay or no-pay status, you
may continue your Health Plan
coverage during your leave, pro-
vided you pay the employee cost
of continuing this coverage.
If you choose to continue cover-
age, you must contact the Benefits
Section of Human Resources before
you begin your leave to make the
necessary billing arrangements.
This coverage will be automatically
canceled if you fail to make required
payments.
If you do not wish to continue your
coverage during your unpaid leave
of absence, you may discontinue
your membership by notifying,
in writing, the Benefits Section of
Human Resources. Re-enroll ment
in the Boston University Health
Plan will be possible when you
return from a leave of absence or
no-pay status, as long as you con-
tact the Benefits Section of Human
Resources and enroll within 30 days
of the date you return.
22

When Your Coverage Ends
If your employment with the
University terminates for any rea-
son, including retirement at or after
age 65, your Health Plan member-
ship will end when your paid-up
coverage expires.
The date your paid-up coverage
expires depends on your date of
hire. If you were hired on or after
January 1, 1983, the payroll deduc-
tions for your Health Plan coverage
are made on a current basis. This
means, the deduction taken from
your January paycheck or paychecks
will pay for January’s coverage. If
you were hired before January 1,
1983, deductions are taken one
month in advance.
• If you were hired on or after
January 1, 1983, your Health
Plan membership will end
on the last day of the month
in which your employment
terminates.
• If you were hired before January
1, 1983, and you terminate your
employment, your Health Plan
membership will end on the last
day of the month following the
month in which your employ-
ment terminates.
Once the payroll system reflects
the termination of your employ-
ment, the Benefits Section of
Human Resources will automatically
notify you in writing of your last day
of coverage, and of what to do to
continue coverage.
A “certificate of creditable cover-
age” will be provided to you if you
lose coverage under the plan as
required by the Health Insurance
Portability and Accountability Act
of 1996.
In addition to any continuation
provisions provided by Boston
University, you and your covered
dependents may have the right to
extend your coverage for up to 18 or
36 months under the federal con-
tinuation provisions (COBRA).
You may also convert your cover-
age to a non-group individual policy.
Contact the Benefits Section of
Human Resources for details.
Coverage Continuation
Provisions
A federal law known as COBRA
requires that most employers
sponsoring group health plans oer
employees and their families (“quali-
fied beneficiaries”) the opportunity
to elect and pay for a temporary
extension of health coverage called
“continuation coverage” at group
rates in certain instances (“qualifying
events”) where coverage under the
employer’s health plan would other-
wise end. This notice is intended to
inform you, in a summary fashion, of
your rights and obligations under the
continuation coverage provisions of
that law. (Both you and your spouse
should take time to read this notice
carefully.) Under the Plan, qualified
beneficiaries who elect COBRA con-
tinuation coverage must pay for the
coverage.
If you are an employee of the Plan
Sponsor (Boston University) cov-
ered by one of the medical options
maintained by the Plan Sponsor
(the “Plan”), you will become a
qualified beneficiary if you lose your
group health coverage because
either one of the following qualify-
ing events happens:
• Your hours of employment are
reduced, or
• Your employment ends for any
reason other than your gross
misconduct.
If you are the spouse of an
employee covered by the Plan, you
will become a qualified beneficiary
23
if you lose your coverage under the
Plan because any one of the follow-
ing qualifying events happens:
• Your spouse dies;
• Your spouse’s employment ends
for any reason other than his or
her gross misconduct;
• Your spouse’s hours of employ-
ment are reduced;
• You become divorced or legally
separated from your spouse; or
• Your spouse becomes entitled to
Medicare (under Part A,
Part B, or both).
Your dependent children will
become qualified beneficiaries if
they lose coverage under the Plan
because any one of the following
qualifying events happens:
• The parent-employee dies;
• The parent-employee’s hours
of employment are reduced;
• The parent-employee’s employ-
ment ends for any reason other
than his or her gross misconduct;
• The parents become divorced
or legally separated;
• The parent-employee becomes
entitled to Medicare benefits
(Part A, Part B, or both); or
• The child ceases to be eligible
for coverage under the Plan as
a “dependent child.”
Sometimes, filing a proceeding in
bankruptcy under title 11 of the
United States Code can be a qualify-
ing event. If a proceeding in bank-
ruptcy is filed with respect to the
Plan Sponsor and that bankruptcy
results in the loss of coverage of
any retired employee covered under
the Plan, the retired employee will
become a qualified beneficiary with
respect to the bankruptcy. The
retired employee’s spouse or surviv-

ing spouse and dependent children
will also become qualified beneficia-
ries if bankruptcy results in the loss
of their coverage under the Plan.
When Is COBRA Coverage
Available?
The Plan will oer COBRA continua-
tion coverage to qualified beneficiaries
only after the Plan Administrator has
been notified that a qualifying event
has occurred. When the qualifying
event is the end of employment or
reduction of hours of employment,
death of the employee, or the employ-
ee’s becoming entitled to Medicare
benefits (under Part A, Part B, or both),
the Plan Sponsor must notify the Plan
Administrator of the qualifying event.
You Must Give Notice of Some
Qualifying Events
For the other qualifying events
(divorce or legal separation of the
employee and spouse, or a depen-
dent child’s losing eligibility for cov-
erage as a dependent child, etc.), you
must notify the Plan Administrator
within 60 days after the qualifying
event occurs. You must provide this
notice to the Plan Contact listed at
the end of this summary, along with
documentation substantiating the
divorce, legal separation, or loss of
dependent status and the eective
date of such event.
A child who is born to or placed for
adoption with the covered employee
during a period of COBRA continu-
ation coverage will be eligible to
become a qualified beneficiary and
be added to the covered employee’s
COBRA continuation coverage. You
must notify the Plan Administrator
within 60 days after the birth or
placement for adoption occurs. You
must provide this notice to the Plan
Contact listed at the end of this
summary, along with copies of legal
documents substantiating the birth
or placement for adoption and the
eective date of such event.
How Is COBRA Coverage
Provided?
Once the Plan Administrator
receives notice that a qualifying
event has occurred, COBRA con-
tinuation coverage will be oered
to each of the qualified benefi-
ciaries. Each qualified beneficiary
will have an independent right to
elect COBRA continuation cover-
age. Covered employees may elect
COBRA continuation coverage on
behalf of their spouses, and parents
may elect COBRA continuation cov-
erage on behalf of their children.
Under the law, you have at least 60
days from the date you would lose
coverage because of one of the events
described above to inform the Plan
Administrator that you want to elect
continuation coverage. If you do not
elect continuation coverage, your
group health coverage will end. If you
elect continuation coverage, the Plan
Sponsor is required to permit you to
elect and purchase coverage which, as
of the time coverage is being provided,
is identical to the coverage provided
under the Plan to similarly situated
employees or family members.
When the qualifying event is the end
of employment or reduction of the
employee’s hours of employment,
and the employee became entitled
to Medicare benefits less than 18
months before the qualifying event,
COBRA continuation coverage for
qualified beneficiaries other than the
employee lasts until 36 months after
the date of Medicare entitlement.
For example, if a covered employee
becomes entitled to Medicare 8
months before the date on which
his employment terminates, COBRA
continuation coverage for his spouse
and children can last up to 36 months
after the date of Medicare entitle-
ment, which is equal to 28 months
after the date of the qualifying event
(36 months minus 8 months).
When the qualifying event is the
death of the employee, the employ-
ee’s becoming entitled to Medicare
benefits (under Part A, Part B, or
both), your divorce, legal separation,
or a dependent child’s losing eligibil-
ity as a dependent child, COBRA
continuation coverage lasts for up
to a total of 36 months. Otherwise,
when the qualifying event is the end
of employment or reduction of the
employee’s hours of employment,
COBRA continuation coverage
generally lasts for only up to a total
of 18 months. There are two ways
in which this 18-month period of
COBRA continuation coverage can
be extended.
Disability Extension of 18-Month
Period of Continuation Coverage
If you or anyone in your family cov-
ered under the Plan is determined by
the Social Security Administration
to be disabled (for purposes of
Title II [OASDI] or Title XVI [SSI]
of the Social Security Act) and you
notify the Plan Administrator in a
timely fashion, you and your entire
family may be entitled to receive
up to an additional 11 months of
COBRA continuation coverage, for
a total maximum of 29 months. The
qualified beneficiary must notify
the Plan Administrator (see Plan
Contact Information below) in writ-
ing of such a determination of Social
Security disability within 60 days
of that determination and before
the end of the 18-month period of
COBRA continuation coverage. The
disability would have to have started
at some time before the 60th day
of COBRA continuation coverage
and must last at least until the end
of the 18-month period of continu-
ation coverage. The qualified ben-
eficiary must also notify the Plan
24

Administrator within 30 days of the
date of any final determination by
the Social Security Administration
that he or she is no longer disabled.
You must provide these notices to
the Plan Contact listed at the end
of this summary, along with copies
of correspondence from the Social
Security Administration substantiat-
ing the disability/loss of disability
and the eective date of the applica-
ble SSA determination. Furthermore,
during the period after the 18th
month through the 29th month of
continuation coverage, the monthly
premium cost will be increased to
150% of the applicable premium
relating to continuation coverage.
Second Qualifying Event Extension
of 18-Month Period of Continuation
Coverage
If your family experiences another
qualifying event while receiving 18
months of COBRA continuation
coverage, the spouse and dependent
children in your family can get up to
18 additional months of COBRA con-
tinuation coverage, for a maximum
of 36 months, if notice of the second
qualifying event is properly given to
the Plan Administrator within 60
days of the second qualifying event.
You must provide this notice to the
Plan Contact listed at the end of this
summary, along with copies of docu-
mentation substantiating the second
qualifying event. This extension may
be available to the spouse and any
dependent children receiving con-
tinuation coverage if the employee or
former employee dies, becomes enti-
tled to Medicare benefits (under Part
A, Part B, or both), or gets divorced,
legally separated, or if the dependent
child stops being eligible under the
Plan as a dependent child, but only
if the event would have caused the
spouse or dependent child to lose
coverage under the Plan had the first
qualifying event not occurred.
How Much Does COBRA
Continuation Coverage Cost?
Each qualified beneficiary must
pay the entire cost of continuation
coverage. The amount a quali-
fied beneficiary must pay may not
exceed 102% (or, in the case of an
extension of continuation coverage
due to disability, 150%) of the cost
to the Plan (including both employer
and employee contributions) for
coverage of a similarly situated plan
participant or beneficiary who is not
receiving continuation coverage.
When and How Must Payment for
COBRA Continuation Coverage
Be Made?
First Payment for Continuation Coverage
If you elect continuation cover-
age, you do not have to send any
payment with the election form.
However, you must make your first
payment for continuation coverage
not later than 45 days after the date
of your election. (This is the date
the election notice is postmarked, if
mailed.) If you do not make your first
payment for continuation coverage
in full not later than 45 days after
the date of your election, you will
lose all continuation coverage rights
under the Plan. You are responsible
for making sure that the amount of
your first payment is correct. You
may contact the party responsible
for COBRA administration under the
Plan at the address, phone number,
or email address provided at the end
of this section to confirm the correct
amount of your first payment.
Periodic Payments for Continuation
Coverage
After you make your first payment
for continuation coverage, you
will be required to make periodic
payments for each subsequent
coverage period. The amount due
for each coverage period for each
25
qualified beneficiary is shown in this
notice. The periodic payments can
be made on a monthly basis. Under
the Plan, each of these periodic pay-
ments for continuation coverage is
due on the first day of the month for
that coverage period. If you make
a periodic payment on or before
the first day of the coverage period
to which it applies, your coverage
under the Plan will continue for that
coverage period without any break.
Grace Period for Periodic Payments
Although periodic payments are due
on the dates shown above, you will
be given a grace period of 30 days
after the first day of the coverage
period to make each periodic pay-
ment. Your continuation coverage
will be provided for each coverage
period as long as payment for that
coverage period is made before the
end of the grace period for that pay-
ment. However, if you pay a periodic
payment later than the first day of the
coverage period to which it applies,
but before the end of the grace period
for the coverage period, your cover-
age under the Plan will be suspended
as of the first day of the coverage
period and then retroactively rein-
stated (going back to the first day of
the coverage period) when the peri-
odic payment is received. This means
that any claim you submit for benefits
while your coverage is suspended
may be denied and may have to be
resubmitted once your coverage is
reinstated.
Early Termination of COBRA
COBRA provides that your continu-
ation coverage may be terminated
before the end of the maximum cov-
erage period for any of the following
reasons:
• The Plan Sponsor no longer pro-
vides group health coverage to
any of its employees;

26
• Any required premium for con-
tinuation coverage is not paid in
full on time;
• A qualified beneficiary becomes
covered—after electing COBRA
continuation coverage—under
another group health plan (as an
employee or otherwise) that
does not impose any pre-existing
condition limitation for a pre-
existing condition of the quali-
fied beneficiary;
• A qualified beneficiary becomes
entitled to Medicare (under Part
A, Part B, or both) after electing
COBRA continuation coverage;
• A qualified beneficiary extends
coverage for up to 29 months due
to disability and there has been a
final determination that the indi-
vidual is no longer disabled.
The Health Insurance Portability and
Accountability Act of 1996 (HIPAA)
restricts the extent to which group
health plans may impose pre-existing
condition limitations. HIPAA coor-
dinates COBRA’s other coverage
cut-o rule (in the third bullet above)
with these new limits as follows:
If you become covered by another
group health plan and that plan con-
tains a pre-existing limitation that
aects you, your COBRA coverage
cannot be terminated. However, if
the other plan’s pre-existing condition
does not apply to you by reason of
HIPAA’s restrictions on pre-existing
condition clauses, the Plan Sponsor
may terminate your COBRA coverage.
You do not have to show that you
are insurable to choose continuation
coverage. However, as discussed
above, you will have to pay all the
required premiums for your continu-
ation coverage.
The law also says that, at the
end of the 18-month, 29-month,
or 36-month continuation cover-
age period, you must be allowed to
enroll in an individual conversion
health plan if such an individual
conversion health plan is otherwise
generally available under the Plan.
COBRA continuation coverage may
be terminated for any reason if the
Plan would terminate coverage of a
participant or beneficiary not receiving
continuation coverage (such as fraud).
If You Have Questions
More complete information regarding
your COBRA continuation cover-
age rights is available from the Plan
Administrator. For more information
about your rights under ERISA, includ-
ing COBRA, the Health Insurance
Portability and Accountability Act
(HIPAA), and other laws aecting
group health plans, contact the near-
est regional or district oce of the
U.S. Department of Labor’s Employee
Benefits Security Administration
(EBSA) in your area or visit the
EBSA website at www.dol.gov/ebsa.
(Addresses and phone numbers of
regional and district EBSA oces are
available through EBSA’s website.)
Keep Your Plan Informed of
Address Changes
In order to protect your family’s
rights, you should keep the Benefits
Section of Human Resources
informed of any changes in the
addresses of family members. You
should also keep a copy, for your
records, of any notices you send to
the Plan Administrator.
Plan Contact Information (Plan
Administrator)
Benefits Section of Human
Resources
Boston University
25 Buick Street
Boston, MA 02215
Phone: 617-353-4489
Email: [email protected]
Special Enrollment Rights under
the Health Insurance Portability
and Accountability Act of 1996
(HIPAA)
If you are declining enrollment for
yourself or your dependents (including
your spouse) because of other health
insurance or group health plan cover-
age, you may be able to enroll yourself
and your dependents in this plan if you
or your dependents lose eligibility for
that other coverage (or if the employer
stops contributing toward your or
your dependents’ other coverage).
However, you must request enroll-
ment within 30 days after your or your
dependents’ other coverage ends (or
after the employer stops contributing
toward the other coverage).
In addition, if you have a new
dependent as a result of marriage,
birth, adoption, or placement for
adoption, you may be able to enroll
yourself and your dependents.
However, you must request enroll-
ment within 30 days after the mar-
riage, birth, adoption, or placement
for adoption.
To request special enrollment or
obtain more information, contact
the Benefits Section of Human
Resources.
Special Enrollment Relating to (i)
Termination of Medicaid or CHIP
Coverage and (ii) Eligibility for
Employment Assistance Under
Medicaid or CHIP
A group health plan, and a health
insurance issuer oering group
health insurance coverage in con-
nection with a group health plan,
must permit an employee who is
eligible, but not enrolled, for cover-
age under the terms of the plan (or
a dependent of such an employee
if the dependent is eligible, but not
enrolled, for coverage under such
terms) to enroll for coverage under
the terms of the plan if either of the
following conditions is met:
26
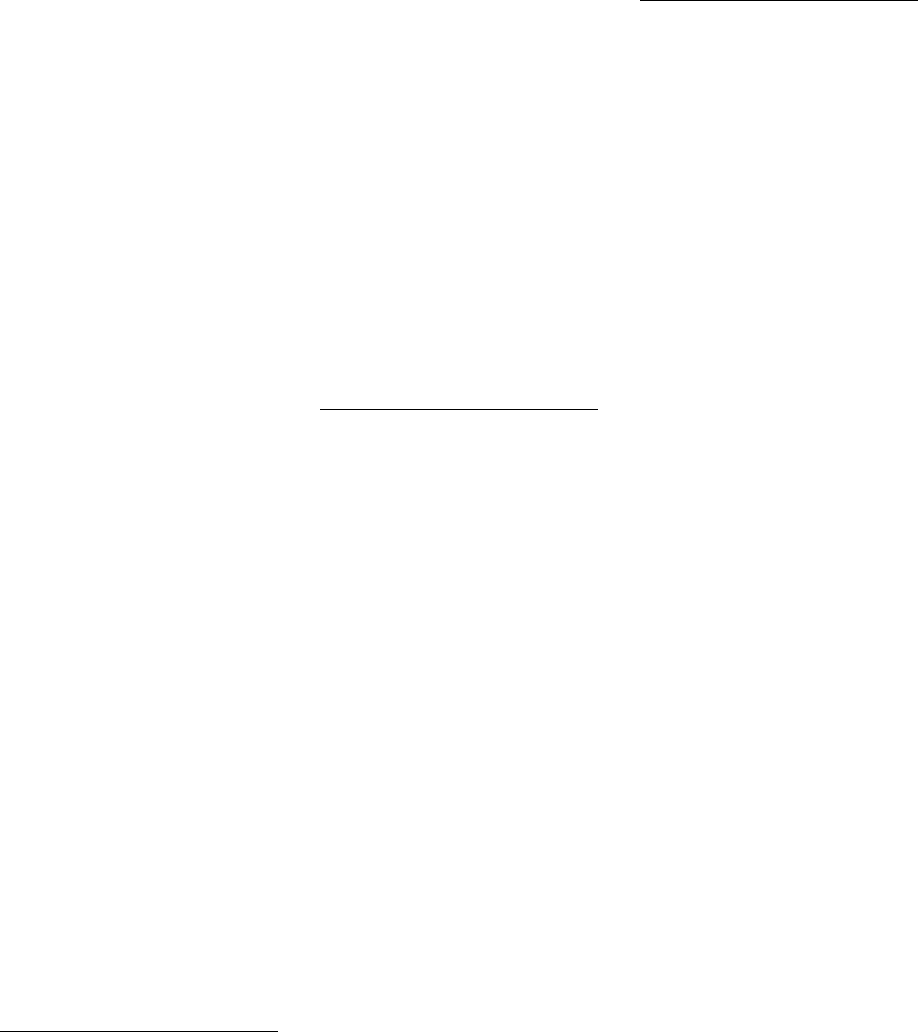
27
(i) The employee or dependent is
covered under a Medicaid plan
under Title XIX of the Social
Security Act or under a State
child health plan (“CHIP”)
under Title XXI of such Act and
coverage of the employee or
dependent under such a plan is
terminated as a result of loss of
eligibility for such coverage and
the employee requests coverage
under the group health plan (or
health insurance coverage) not
later than 60 days after the date
of termination of such coverage.
(ii) The employee or dependent
becomes eligible for assistance,
with respect to coverage under
the group health plan or health
insurance coverage, under such
Medicaid plan or State child
health plan (including under
any waiver or demonstration
project conducted under or in
relation to such a plan), if the
employee requests coverage
under the group health plan or
health insurance coverage not
later than 60 days after the date
the employee or dependent is
determined to be eligible for
such assistance.
To request special enrollment or
obtain more information, contact
the Plan Administrator at the
address and phone number listed in
this handbook on the previous page.
Your Rights Under Newborns’ and
Mothers’ Health Protection Act of
1996 (NMHPA)
Group health plans and health insur-
ance issuers generally may not,
under federal law, restrict benefits
for any hospital length of stay in
connection with childbirth for the
mother or newborn child to less than
48 hours following a vaginal delivery,
or less than 96 hours following a
cesarean section. However, federal
law generally does not prohibit the
mother’s or newborn’s attending
provider, after consulting with the
mother, from discharging the mother
or her newborn earlier than 48
hours (or 96 hours as applicable).
In any case, plans and issuers may
not, under federal law, require that
a provider obtain authorization from
the plan or the insurance issuer for
prescribing a length of stay not in
excess of 48 hours (or 96 hours).
Your Rights Under Women’s
Health and Cancer Rights Act of
1998 (WHCRA)
If you have had or are going to
have a mastectomy, you may be
entitled to certain benefits under the
Women’s Health and Cancer Rights
Act of 1998 (WHCRA). For individu-
als receiving mastectomy-related
benefits, coverage will be provided in
a manner determined in consultation
with the attending physician and the
patient for:
• All stages of reconstruction of
the breast on which the mastec-
tomy was performed
• Surgery and reconstruction of
the other breast to produce a
symmetrical appearance
• Prostheses
• Treatment of physical complica-
tions of the mastectomy, includ-
ing lymphedema
These benefits will be provided
subject to the same deductibles and
coinsurance applicable to other medi-
cal and surgical benefits provided
under your coverage under this Plan.
If you would like more information
on WHCRA benefits, contact the
Benefits Section of Human Resources.
Qualified Medical Child Support
Orders (QMCSOs)
As required by ERISA, the Plan rec-
ognizes qualified medical child sup-
port orders (QMCSOs). A QMCSO
is a court order or an order issued
by a state administrative agency in
accordance with federal and state
laws that requires an alternate
beneficiary (for example, a child or
stepchild) to be covered by a plan
participant’s group health plan.
The Plan honors QMCSOs that meet
the legal requirements for such
orders. It is important to note that
a QMCSO cannot require a plan to
provide a type or form of benefit,
or an option, that is not currently
available from the plan to which the
order is directed, unless receiving
this benefit or option is necessary
to meet the requirements of the
Social Security Act, which relates
to the enforcement of state child
support laws and reimbursement of
Medicaid.
A QMCSO must be provided to the
Plan Administrator to determine if
it meets the legal requirements for
a QMCSO. If it does, the alternate
beneficiary is considered a benefi-
ciary for the purposes of ERISA and
is enrolled as a dependent of the
employee participant. If the Plan
Administrator receives a medical
child support order that relates to
you, you will be notified and then
informed of the decision as to
whether the order is qualified.
A copy of the Plan’s QMCSO pro-
cedures is available, free of charge,
upon written request to the Benefits
Section of Human Resources.

28
Health Plan Comparison
Non-BMC PCP
Out-of-Network
BMC PCP
In-Network
BU Health Savings Plan
BCBS PPO
In-Network
Out-of-Network
Network Blue New England
$20 copayment per visit 80% coverage after deductible $15 copayment per visit $30 copayment per visit 90% coverage after deductible 70% coverage after deductible
$20 copayment per visit 80% coverage after deductible $25 copayment per visit $50 copayment per visit 90% coverage after deductible 70% coverage after deductible
100% coverage 80% coverage after deductible 80% coverage 80% coverage 90% coverage after deductible 70% coverage after deductible
$100 copayment $100 copayment $100 copayment $100 copayment 90% coverage after deductible 70% coverage after deductible
$20 copayment per visit 80% coverage after deductible $15 copayment per visit $30 copayment per visit 90% coverage after deductible 70% coverage after deductible
$20 copayment per visit;
when performed at BU
rehabilitation facility,
100% coverage
80% coverage after deductible $15 copayment per visit;
when performed at BU
rehabilitation facility,
100% coverage
$30 copayment per visit;
when performed at BU
rehabilitation facility,
100% coverage
90% coverage after deductible;
when performed at BU
rehabilitation facility,
coinsurance does not apply
70% coverage after deductible;
when performed at BU
rehabilitation facility,
coinsurance does not apply
100% coverage 80% coverage after deductible 100% coverage when
performed at BMC
$100 per admission when
performed at non-BMC
network facility
90% coverage after deductible 70% coverage after deductible
$20 copayment per visit 80% coverage after deductible $15 copayment per visit $30 copayment per visit 90% coverage after deductible 70% coverage after deductible
100% coverage 80% coverage after deductible 100% coverage 100% coverage 100% coverage 70% coverage;
no deductible
100% coverage 80% coverage
after deductible
100% coverage 100% coverage 100% coverage 70% coverage;
no deductible
None $500 per person;
$1,000 per family
None None $1,500 for individual;
$3,000 any family coverage
$3,000 for individual;
$6,000 any family coverage
None $2,000 per person;
$4,000 family
None None $3,000 for individual;
$6,000 any family coverage
includes deductible
$6,000 for individual;
$12,000 any family coverage
includes deductible
$4,000,000 (combined
in-network
and out-of-network)
$4,000,000 (combined
in-network and out-of-network)
excludes deductible
$4,000,000 $4,000,000 $4,000,000 (combined
in-network
and out-of-network)
$4,000,000 (combined
in-network
and out-of-network)
$20 for most
covered services
Out-of-network services require
a deductible and coinsurance
$15 for most
services
$30 for most
services
In-network services require a
deductible and coinsurance
Out-of-network services require
a deductible and coinsurance
100% for most inpatient and
outpatient services; small
copayment
for some services
80% benefit for most covered
inpatient and outpatient services;
you pay the remaining
20% of expenses
100% for most inpatient and
outpatient services;
small copayment for
some services
100% for most inpatient and
outpatient services;
small copayment for
some services
90% benefit for most covered
inpatient and outpatient services;
you pay the remaining
10% of expenses
70% benefit for most covered
inpatient and outpatient services;
you pay the remaining
30% of expenses
Not required Required Not required Not required Required Required
100% coverage 80% coverage after deductible 100% coverage 100% coverage 100% coverage 70% coverage after deductible
100% coverage 80% coverage after deductible 100% coverage 100% coverage 90% coverage after deductible 70% coverage after deductible
Deductible per Calendar Year
Chiropractic Care
(up to 20 visits per year)
Diagnostic Lab and X-ray
(including MRIs, PET & CT Scans)
Durable Medical Equipment
Emergency Room Visit
(copayment waived if admitted)
Family Planning and
Infertility Services
Inpatient Hospital
Skilled Nursing Facility
(100 days per calendar year)
Physical Therapy
Office Visits
Preventive Care
Eye Exams
(routine)
Claim Forms
Benefit Level
Member Copayments
Lifetime Maximum
Benefit
Out-of-Pocket Maximum
per Calendar Year
Physicians’ Services
Surgical
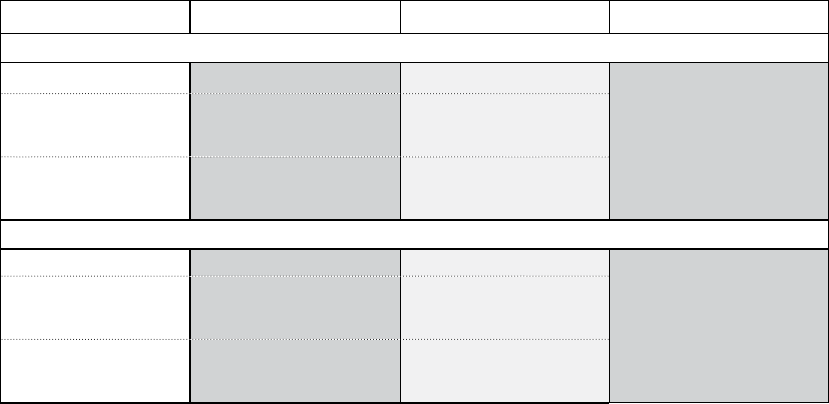
29
Prescription Drug
Coverage
BCBS PPO Network Blue New England BU Health Savings Plan
Retail Pharmacy
Generic
$8 Copayment $8 Copayment
20% coinsurance after deductible
Preferred Brand-Name 20% coinsurance
Minimum cost $30
Maximum cost $50
20% coinsurance
Minimum cost $30
Maximum cost $50
Non-Preferred Brand-Name 30% coinsurance
Minimum cost $50
Maximum cost $70
30% coinsurance
Minimum cost $50
Maximum cost $70
Home Delivery
Generic $16 Copayment $16 Copayment
20% coinsurance after deductible
Preferred Brand-Name 20% coinsurance
Minimum cost $60
Maximum cost $100
20% coinsurance
Minimum cost $60
Maximum cost $100
Non-Preferred Brand-Name 30% coinsurance
Minimum cost $100
Maximum cost $140
30% coinsurance
Minimum cost $100
Maximum cost $140

Overview
Dental Health Plan
32
Y
ou and your eligible family members have the opportunity
to enroll in the Boston University Dental Health Plan.
You and the University share the cost of your coverage under
the Dental Health Plan. The Dental Health Plan is designed to
provide you with high-quality care at an affordable price. There
are two different plans from which to choose:
(1) The BU Dental Health Center Plan or (2) The Dental Blue
Freedom Plan.

33
Eligibility
If you are classified by the University
as a regular employee, work 75% or
more of a full-time schedule, and have
an appointment of nine months’ or
more duration, you and your eligible
family members may participate in
the Boston University Dental Health
Plan starting on the first day of the
month coincident with or following
your first day of work.
Your eligible family members
include:
• Your legally married spouse
• Your children under age 26
• Your unmarried, dependent
children age 26 and older who
are mentally or physically
handicapped
Coverage Levels
There are four levels of coverage
available under the Dental Health
Plan:
• Individual coverage (yourself
only)
• Individual plus spouse (you and
your spouse)
• Individual plus child(ren)
(you and one or more of your
children)
• Family coverage (you and your
eligible family members)
Special Provisions for Former
Spouses
If you have family coverage includ-
ing your spouse and you divorce,
your spouse may continue to be
covered under your family coverage:
• If the divorce order specifically
calls for this, and
• If neither you nor your former
spouse remarries.
If you or your former spouse
remarries, your former spouse’s
eligibility for coverage ends. Once
coverage ends, your former spouse
may continue coverage on an indi-
vidual basis under COBRA for the
remaining period (if any) until 36
months have gone by since your
divorce or separation.
If your divorce order specifically
requires coverage for your former
spouse to continue beyond the
COBRA continuation period, your
former spouse may be eligible to
continue coverage under an indi-
vidual coverage (if available, under
the Health Plan and the various
vendors providing benefits). This
coverage will continue as long as
you continue to be employed at
the University and have made the
appropriate payment for coverage
or until no longer required by the
divorce order or no longer available.
Special Tax Considerations
Under current tax laws, the value
of your former spouse’s dental
coverage is subject to federal
income, Massachusetts state
income, and Social Security taxes.
These taxable amounts are based
on the full amount of an individual
plan (that is, employee contribu-
tion plus employer contribution)
and are called imputed income.
Imputed income for your former
spouse’s dental coverage will be
reported as income on each pay-
check, and will be included in the
taxable earnings shown on your
W-2 Form. Coverage for your for-
mer spouse is subject to imputed
income for tax purposes.
Enrollment
Participation in the Boston University
Dental Health Plan is voluntary. To
elect this coverage, new employees
must go to Employee Self Service
at www.bu.edu/buworkscentral.
Alternatively, you may complete a
Benefits Enrollment Form available
at www.bu.edu/hr/home/forms/
benefit-forms. This form will also
authorize a payroll deduction to pay
for your share of the cost.
If you choose a coverage level that
includes your spouse or dependent
children, coverage is available only
for the family members who are
listed on your enrollment. If you wish
to enroll newly eligible family mem-
bers (for example, an adopted child
or a new spouse), you may do so by
obtaining the necessary forms from
the Human Resources website at
www.bu.edu/hr/home/forms/
benefit-forms. Alternatively, you
may request a paper form from the
Benefits Section of Human Resources
by email at [email protected].
When Coverage Starts
You have 30 days following your
benefit orientation date to enroll.
If you enroll, coverage will become
effective on the first day of the
month coincident with or following
your first day of work. If you do not
enroll during this period, your next
opportunity to enroll will be during
the next open enrollment period.
Cost
You and the University share the
cost of your coverage under the
Dental Health Plan. Currently, the
University pays a portion of the
coverage cost as determined by the
Dental Health Plan
34
University. Your share of the cost
is the difference between the total
cost of coverage and the amount
that Boston University pays. Costs
are subject to change at the begin-
ning of each plan year. Also, the
University may change the percent-
age of the cost that it will pay.
How Dental Health Plan
Contributions Are Paid
You pay for your portion of the
contributions for your Dental
Health Plan coverage with tax-free
dollars. This is because Boston
University automatically reduces
your pay by the amount of your
payments—before federal income
taxes, state income taxes, and
Social Security taxes are taken out.
Automatic before-tax premium pay-
ments are allowed under the provi-
sions of Section 125 of the Internal
Revenue Code. These are explained
in more detail in the “Flexible
Benefits” section of this handbook.
Changing or Stopping Coverage
Because you pay for your coverage
with before-tax dollars, the provi-
sions of Section 125 of the Internal
Revenue Code also govern how
and when you may make changes
in your Dental Health Plan cover-
age. Under the current provisions of
Section 125, you may
• Change the level of your cover-
age (that is, move from individ-
ual to family coverage or vice
versa), or
• Cancel your coverage
once each year, during the annual
open enrollment period.
The only other time you may make
a change in your Dental Health
Plan coverage is if you have an
IRS-approved Qualified Change in
your family or employment status.
Qualified Changes are explained in
the “Flexible Benefits” section of this
handbook.
About the Boston University
Dental Health Centers
There are two Boston University
Dental Health Centers. Both provide
a comprehensive range of dental
services, such as X-rays, cleanings,
fillings, and crowns.
You will be examined by a licensed
staff dentist when you receive your
care at one of the Dental Health
Centers. Preventive services such
as cleanings and X-rays will be pro-
vided by licensed dental hygienists.
If you require any specialty services
such as orthodontics (braces), oral
surgery (extractions), endodontics
(root canals), or periodontics (gum
surgery), both centers can refer you
to the appropriate licensed special-
ist and/or postdoctoral resident
found within either Center.
Your care will be monitored by your
staff dentist at one of the Dental
Health Centers. The standard fees-
for-service provided through the
Dental Health Centers are already
far below those charged by most
private practices. Therefore, the
Dental Health Centers offer you
and your family members a unique
opportunity to obtain quality dental
care at a reasonable price.
The Boston University Dental Health
Centers are conveniently located at:
• 930 Commonwealth Avenue
near the Charles River Campus
Phone: 617-358-1000
• 100 East Newton Street
at the Boston University
Medical Center
Phone: 617-638-4670
The BU Dental Health
Center Plan
How the Plan Works
If you join this plan, you must
receive your dental treatment
from one of the BU Dental
Health Centers located at 930
Commonwealth Avenue and 100
East Newton Street. There is no
coverage for care received out-
side of the Centers (except for
emergency dental treatment at
a participating BCBS Dental Blue
provider).
Covered Services
The Boston University Dental Health
Center Plan covers services listed
on the following chart. Here are two
special features of the plan that you
should remember:
• There are no deductibles for cov-
ered services.
• You do not have to complete
claim forms for services provided
at the Dental Health Centers.
Boston University Dental Health Center Plan
Covered Services
Preventive & Diagnostic
Basic Restorative
Major Restorative
Orthodontia
Annual Maximun Benefit
Orthodontia Lifetime
Maximun Benefit
100%
100%
60%
50%
$1,700 per person,
per year
$2,000 per person,
lifetime
Boston University
Dental Health Center
Dentists*
Type of Service
*The percentage of the cost of a covered service
that is paid by the plan is based on the standard fee
schedule established by the Boston University Dental
Health Centers. You may obtain a copy of the stan-
dard fee schedule by contacting Human Resources at
[email protected] or online at www.bu.edu/hr/home/
forms/benefit-forms.

35
Preventive and Diagnostic
Diagnostic Services
• One complete initial oral exam,
including initial dental history
and charting of the teeth and
supporting structures
• Single-tooth X-rays as needed
• Bitewing X-rays of the crowns of
the teeth (once each six months)
• Full-mouth X-rays (seven or
more films, or panoramic X-ray
with bitewing X-rays; once each
60 months)
• Study models and casts used in
planning treatment (once each
60 months)
• Emergency exams
• Periodic or routine oral exams
(once each six months)
Preventive Services
• Routine cleaning, scaling, and
polishing of the teeth (once each
six months)
• Fluoride treatment for mem-
bers under age 19 (once each
six months)
• Space maintainers required due
to premature loss of teeth for
members under age 19
• Sealants applied to permanent
premolar and molar surfaces
for members under age 14 (one
application each 48 months for
each premolar or molar surface)
Basic Restorative Services
• Amalgam (silver) fillings (lim-
ited to one filling for each tooth
surface in each 12 months). No
benefits are provided for fillings
on tooth surfaces where a seal-
ant was applied within the last
12 months.
• Composite resin (tooth color) fill-
ings on front teeth (limited to one
filling for each tooth surface in
each 12 months). These benefits
include single-surface composite
resin fillings on back teeth.
• Pin retention for fillings
• Stainless steel crowns on pri-
mary (baby) teeth
• Stainless steel crowns on first
permanent (adult) molars for
members under age 16
Prosthetic Maintenance
• Repair of partial or complete
dentures, crowns, and bridges
(once each 12 months)
• Adding teeth to an existing par-
tial or complete denture
• Rebase or reline dentures (once
each 36 months)
• Recementing of crowns, inlays,
onlays, and fixed bridgework
(once each 12 months)
Other Covered Services
• Occlusal adjustments (once each
24 months)
• Services to treat root sensitivity
• General anesthesia when
administered in conjunction
with covered surgical services
• Emergency dental treatment to
relieve acute pain
Major Restorative Services
Oral Surgery
• Tooth extractions
• Root removal
• Biopsies
Periodontics (Gum and Bone)
• Periodontal scaling and root plan-
ing (once in each quadrant each
24 months)
• Periodontal surgery (soft and
hard tissue surgeries; once in
each quadrant each 36 months)
• Periodontal maintenance follow-
ing active periodontal therapy
(once each three months)
Endodontics (Root and Pulp)
• Root canal therapy on permanent
teeth (once in a lifetime for each
tooth)
• Retreatment root canal therapy
on permanent teeth (once in a
lifetime for each tooth)
• Therapeutic pulpotomy on pri-
mary or permanent teeth for
members under age 16
• Other endodontic surgery
intended to treat or remove the
dental root
Prosthodontics (Tooth Replacement)
• Complete or partial dentures,
including services to fabricate,
measure, fit, and adjust them
(once each 60 months for each
arch)
• Fixed bridges, including services
to fabricate, measure, fit, and
adjust them (once each
60 months for each tooth)
• Replacement of dentures and
bridges, but only when they are
installed at least 60 months
after the initial placement, and
only if the existing appliance
cannot be made serviceable
• Temporary partial dentures to
replace any of the six upper or
lower front teeth, but only if
they are installed immediately
following the loss of teeth and
during the period of healing
Crowns, Inlays, and Onlays
• Crowns for members age 16 or
older (once each 60 months for
each tooth). Note: These ben-
efits include single-tooth dental
endosteal implants (the fixture
and abutment portion) when
the implant replaces permanent
teeth through the second molars

(once each 60 months for each
tooth).
• Metallic, porcelain, and compos-
ite resin inlays for members age
16 or older
• Metallic, porcelain, and com-
posite resin onlays for members
age 16 or older (once each 60
months for each tooth)
• Replacement of crowns for
members age 16 or older (once
each 60 months for each tooth)
• Replacement of metallic, porce-
lain, and composite resin onlays
(once each 60 months for each
tooth)
• Replacement of metallic, porce-
lain, and composite resin onlays
for members age 16 or older
(once each 60 months for each
tooth)
• Post and core or crown buildup
for members age 16 or older
(once each 60 months for each
tooth)
Orthodontics
Orthodontic benefits, including
braces and related services dur-
ing treatment, are provided for
adults and children when care is
provided by a dentist located at a
Boston University Dental Health
Center.
Emergency Care
The plan defines “emergency
treatment” as treatment needed
to immediately alleviate pain or
infection or to treat an injury.
Emergency treatment is covered
as a basic restorative service,
regardless of where it is pro-
vided. Emergency treatment
does not include any final resto-
rations (i.e., root canal, crowns,
and dentures).
Non-Covered Dental Services
No benefits are provided by the
Boston University Dental Health
Center Plan for:
• Services, supplies, procedures,
or appliances to treat an illness
or injury for which you have the
right to benefits under govern-
ment programs. These include
the Veterans Administration for
an illness or injury connected to
military service. They also include
programs set up by other local,
state, federal, or foreign laws or
regulations that provide or pay for
health care services and supplies
or that require care or treatment
to be furnished in a public facility.
No benefits are provided if you
could have received governmen-
tal benefits by applying for them
on time. This exclusion does not
include Medicaid or Medicare.
• Charges that are received for or
related to dental care that Blue
Cross Blue Shield considers to be
experimental. The care must be
documented by controlled studies
that determine its merits (such as
its safety) and include sufficient
follow-up studies.
• Charges for appointments that you
do not keep. Dentists may charge
you for failing to keep your sched-
uled appointments. They may do
so if you do not give reasonable
notice to the office. Appointments
that you do not keep are not
counted against any benefit limits
described in this BU Dental Health
Center Plan benefit description.
• A service, supply, procedure, or
appliance that is not described as
a covered dental service in this
BU Dental Health Center Plan
benefit description
• Services, supplies, procedures, or
appliances that do not conform
to Blue Cross Blue Shield dental
policy guidelines
• Any service or supply furnished
along with, in preparation for, or
as a result of a non-covered den-
tal service
• Services, supplies, procedures,
and appliances that are not con-
sidered necessary and appropri-
ate by Blue Cross Blue Shield
• Services, supplies, procedures,
and appliances that are furnished
to someone other than the patient
• Treatment and related services
that are required by third parties
• Free care or care for which you
are not required to pay or for
which you would not be required
to pay if you were not covered
under the BU Dental Health
Center Plan
• Nutrition counseling or instruc-
tions in dental hygiene, including
proper methods of tooth brush-
ing, the use of dental floss, plaque
control programs, and caries
(cavity) susceptibility tests
• Incomplete procedures
• Laboratory or bacteriological tests
• Consultations when the dentist
who renders the consultation pro-
vides treatment
• Restorations for reasons other
than decay or fracture of teeth,
such as erosion, abrasion, or
attrition
• Sealants applied to permanent
premolar or molar surfaces that
have decay or fillings
• Fillings on tooth surfaces where
a sealant was applied within the
last 12 months
• Replacement of a filling within 12
months of the date of the prior
restoration
36

37
• Stainless steel crowns on perma-
nent (adult) teeth, other than on
first permanent (adult) molars for
members under age 16
• Fixed or removable prosthodon-
tics or major restorative proce-
dures for members under age 16
(The BU Dental Health Center
Plan provides the benefit for a
temporary partial denture for
replacement of a lost or missing
tooth. You pay any balance.)
• Temporary complete dentures or
temporary fixed bridges
• Replacement of dentures, bridges,
or space maintainers for reasons
such as theft, abuse, misuse,
misplacement, loss, improper fit,
allergies, breakage, or ingestion
• Duplicate dentures or bridges
• Transplants or any related surgi-
cal or restorative procedures
• Any procedure to save a tooth
when there is a poor statistical
probability (less than a 70%
chance) that the tooth will last
for 60 months (for example,
surgical periodontal regenerative
procedures to stabilize a tooth
loosened due to extensive peri-
odontal disease)
• Cast restorations, copings, or
attachments for installing over-
dentures, including associated
endodontic procedures such as
root canals
• Precision attachments, semipreci-
sion attachments, or copings
• A service to diagnose or treat
temporomandibular joint (TMJ)
disorders or myofascial (mus-
cular) pain, including bruxism
(grinding of the teeth). This
service is covered under the
Blue Cross Blue Shield medical
policies.
• A service, supply, or procedure
when its sole purpose is to
increase the height of teeth
(vertical dimension) or to restore
occlusion
• A separate charge for occlusal
analysis, pulp vitality testing, or
pulp capping since these services
are usually performed as part of
another covered procedure
• Drugs, pharmaceuticals, biologi-
cals, or other prescription agents
or products
• Photographs
• A dentist’s charge to file a
claim. Also, a dentist’s charge
to transcribe or copy your
dental records
• Services and supplies furnished
before your effective date, except
for a multi-stage procedure that
begins before your effective date
and is completed while you are
enrolled under the BU Dental
Health Center Plan
• Services and supplies furnished
after your termination date under
the BU Dental Health Center
Plan. (If your membership under
the BU Dental Health Center
Plan is terminated prior to the
completion date of a procedure
that requires more than one visit,
no benefits are provided for the
entire procedure.)
How to Obtain Benefits
To obtain benefits for services
provided at the Boston University
Dental Health Centers, simply
show your Blue Cross Blue Shield
membership card. You do not
have to complete a claim form for
services provided at the Dental
Health Centers.
The Dental Blue Freedom
Plan
How the Plan Works
This is a unique dental plan,
designed especially for BU employ-
ees who may not be able to conve-
niently receive all their dental care
services at the BU Dental Health
Centers. It provides you three
choices of dental providers; you
decide where to receive treatment
each time you need dental care.
You have access to providers at
the BU Dental Health Centers; Blue
Cross Blue Shield dental network
providers; or you may choose your
own provider. Plan benefits vary
based on where you receive care.
Covered Services
The Dental Blue Freedom Plan cov-
ers services listed on the chart on
the next page.
Preventive and Diagnostic
Diagnostic Services
• One complete initial oral exam,
including initial dental history
and charting of the teeth and
supporting structures
• Single-tooth X-rays as needed
• Bitewing X-rays of the crowns of
the teeth (once each six months)
• Full-mouth X-rays (seven or
more films, or panoramic X-ray
with bitewing X-rays; once each
60 months)
• Study models and casts used in
planning treatment (once each
60 months)
• Emergency exams
• Periodic or routine oral exams
(once each six months)

38
Preventive Services
• Routine cleaning, scaling, and
polishing of the teeth (once each
six months)
• Fluoride treatment for mem-
bers under age 19 (once each
six months)
• Space maintainers required due
to premature loss of teeth for
members under age 19
• Sealants applied to permanent
premolar and molar surfaces
for members under age 14 (one
application each 48 months for
each premolar or molar surface)
Basic Restorative Services
• Amalgam (silver) fillings (lim-
ited to one filling for each tooth
surface in each 12 months). No
benefits are provided for fillings
on tooth surfaces where a seal-
ant was applied within the last 12
months
• Composite resin (tooth color)
fillings on front teeth (limited
to one filling for each tooth
surface in each 12 months).
These benefits include single-
surface composite resin fillings
on back teeth
• Pin retention for fillings
• Stainless steel crowns on
primary (baby) teeth
• Stainless steel crowns on first
permanent (adult) molars for
members under age 16
Prosthetic Maintenance
• Repair of partial or complete
dentures, crowns, and bridges
(once each 12 months)
• Adding teeth to an existing par-
tial or complete denture
• Rebase or reline dentures (once
each 36 months)
• Recementing of crowns, inlays,
onlays, and fixed bridgework
(once each 12 months)
Other Covered Services
• Occlusal adjustments (once each
24 months)
• Services to treat root sensitivity
• General anesthesia when admin-
istered in conjunction with cov-
ered surgical services
• Emergency dental treatment to
relieve acute pain
Major Restorative Services
Oral Surgery
• Tooth extractions
• Root removal
• Biopsies
Periodontics (Gum and Bone)
• Periodontal scaling and root
planing (once in each quadrant
each 24 months)
• Periodontal surgery (soft and
hard tissue surgeries; once
in each quadrant each 36
months)
• Periodontal maintenance follow-
ing active periodontal therapy
(once each three months)
Endodontics (Root and Pulp)
• Root canal therapy on permanent
teeth (once in a lifetime for each
tooth)
• Retreatment root canal therapy
on permanent teeth (once in a
lifetime for each tooth)
• Therapeutic pulpotomy on pri-
mary or permanent teeth for
members under age 16
• Other endodontic surgery
intended to treat or remove
the dental root
*Based on the BU Dental Health Center
Table of Allowance
**Based on lesser of either the dentist’s actual
charge or the allowed charge. If your provider
is in the Dental Blue PPO Network, your share
of the cost of services may be less than if your
provider is in only the Dental Blue Network.
To determine which networks your provider
participates in, review your provider’s profile
on the Blue Cross Blue Shield website at
www.bluecrossma.com/findadoctor.
***Based on the actual charge or the allowed
charge, whichever is less. The allowed charge
is based on a schedule of charges. You may
be responsible for any difference between the
dentist’s actual charge or the allowed charge,
whichever is less.
Deductible
Preventive & Diagnostic
Basic Restorative
Major Restorative
Orthodontics
Annual Maximum
Benefit
Orthodontia Lifetime
Maximum Benefit
None
100%
80%
50%
50%
$50 per person
80%, no deductible
60%, after deductible
40%, after deductible
Not covered
$50 per person
80%, no deductible
60%, after deductible
40%, after deductible
Not covered
Coverage
at Centers*
BCBS Dental
Blue & PPO (in
Massachusetts)
Networks**
BCBS DenteMax
(National)
Network**
Service
$1,700 per person, per year
$2,000 per person, lifetime
Dental Blue Freedom Plan Covered Services
Out-of-Network
Provider***
$50 per person
80%, no deductible
60%, after deductible
40%, after deductible
Not covered

39
Prosthodontics (Tooth Replacement)
• Complete or partial dentures,
including services to fabricate,
measure, fit, and adjust them
(once each 60 months for each
arch)
• Fixed bridges, including services
to fabricate, measure, fit, and
adjust them (once each
60 months for each tooth)
• Replacement of dentures and
bridges, but only when they are
installed at least 60 months after
the initial placement, and only if
the existing appliance cannot be
made serviceable
• Temporary partial dentures to
replace any of the six upper or
lower front teeth, but only if they
are installed immediately follow-
ing the loss of teeth and during
the period of healing
Crowns, Inlays, and Onlays
• Crowns for members age 16 or
older (once each 60 months for
each tooth) Note: These ben-
efits include single-tooth dental
endosteal implants (the fixture
and abutment portion) when
the implant replaces permanent
teeth through the second molars
(once each 60 months for each
tooth).
• Metallic, porcelain, and compos-
ite resin inlays for members age
16 or older
• Metallic, porcelain, and com-
posite resin onlays for members
age 16 or older (once each 60
months for each tooth)
• Replacement of crowns for
members age 16 or older (once
each 60 months for each tooth)
• Replacement of metallic, porce-
lain, and composite resin inlays
(once each 60 months for each
tooth)
• Replacement of metallic, porce-
lain, and composite resin onlays
for members age 16 or older
(once each 60 months for each
tooth)
• Post and core or crown buildup
for members age 16 or older
(once each 60 months for each
tooth)
Orthodontics
Orthodontic benefits, including
braces and related services during
treatment, are provided for adults
and children when care is provided
by a dentist located at a Boston
University Dental Health Center.
Emergency Care
The plan defines “emergency treat-
ment” as treatment needed to
immediately alleviate pain or infec-
tion or to treat an injury. Emergency
treatment is covered as a basic
restorative service, regardless of
where it is provided. Emergency
treatment does not include any final
restorations (i.e., root canal, crowns,
and dentures).
Non-Covered Dental Services
No benefits are provided by the
Dental Blue Freedom Plan for:
• Services, supplies, procedures,
or appliances to treat an illness
or injury for which you have the
right to benefits under govern-
ment programs. These include
the Veterans Administration for
an illness or injury connected
to military service. They also
include programs set up by other
local, state, federal, or foreign
laws or regulations that provide
or pay for health care services
and supplies or that require care
or treatment to be furnished
in a public facility. No benefits
are provided if you could have
received governmental benefits
by applying for them on time.
This exclusion does not include
Medicaid or Medicare.
• Charges that are received for or
related to dental care that Blue
Cross Blue Shield considers to be
experimental. The care must be
documented by controlled studies
that determine its merits (such as
its safety) and include sufficient
follow-up studies.
• Charges for appointments that
you do not keep. Dentists may
charge you for failing to keep
your scheduled appointments.
They may do so if you do not give
reasonable notice to the office.
Appointments that you do not
keep are not counted against
any benefit limits described in
this Dental Blue Freedom Plan
benefit description.
• A service, supply, procedure, or
appliance that is not described as
a covered dental service in this
Dental Blue Freedom Plan benefit
description
• Services, supplies, procedures, or
appliances that do not conform
to Blue Cross Blue Shield dental
policy guidelines
• Any service or supply furnished
along with, in preparation for, or
as a result of a non-covered den-
tal service
• Services, supplies, procedures,
and appliances that are not con-
sidered necessary and appropri-
ate by Blue Cross Blue Shield
• Services, supplies, procedures,
and appliances that are furnished
to someone other than the patient
• Treatment and related services
that are required by third parties
• Free care or care for which you
are not required to pay or for

40
which you would not be required
to pay if you were not covered
under the Dental Blue Freedom
Plan
• Nutrition counseling or instruct-
ions in dental hygiene, including
proper methods of tooth brush-
ing, the use of dental floss,
plaque control programs, and
caries (cavity) susceptibility
tests
• Incomplete procedures
• Laboratory or bacteriological
tests
• Consultations when the dentist
who renders the consultation
provides treatment
• Restorations for reasons other
than decay or fracture of teeth,
such as erosion, abrasion, or
attrition
• Sealants applied to permanent
premolar or molar surfaces that
have decay or fillings
• Fillings on tooth surfaces where
a sealant was applied within the
last 12 months
• Replacement of a filling within 12
months of the date of the prior
restoration
• Stainless steel crowns on perma-
nent (adult) teeth, other than on
first permanent (adult) molars
for members under age 16
• Fixed or removable prosthodon-
tics or major restorative proce-
dures for members under age 16.
(The Dental Blue Freedom Plan
provides the benefit for a tempo-
rary partial denture for replace-
ment of a lost or missing tooth.
You pay any balance.)
• Temporary complete dentures or
temporary fixed bridges
• Replacement of dentures,
bridges, or space maintainers
for reasons such as theft, abuse,
misuse, misplacement, loss,
improper fit, allergies, breakage,
or ingestion
• Duplicate dentures or bridges
• Transplants or any related surgi-
cal or restorative procedures
• Any procedure to save a tooth
when there is a poor statistical
probability (less than a 70%
chance) that the tooth will last
for 60 months (for example,
surgical periodontal regenerative
procedures to stabilize a tooth
loosened due to extensive peri-
odontal disease)
• Cast restorations, copings, or
attachments for installing over-
dentures, including associated
endodontic procedures such as
root canals
• Precision attachments, semipre-
cision attachments, or copings
• A service to diagnose or treat
temporomandibular joint (TMJ)
disorders or myofascial (muscu-
lar) pain, including bruxism (grind-
ing of the teeth). This service is
covered under the Blue Cross Blue
Shield medical policies.
• A service, supply, or procedure
when its sole purpose is to
increase the height of teeth
(vertical dimension) or to
restore occlusion
• A separate charge for occlusal
analysis, pulp vitality testing, or
pulp capping since these services
are usually performed as part of
another covered procedure
• Drugs, pharmaceuticals, biologi-
cals, or other prescription agents
or products
• Photographs
• A dentist’s charge to file a
claim. Also, a dentist’s charge to
transcribe or copy your dental
records
• Services and supplies furnished
before your effective date,
except for a multi-stage proce-
dure that begins before your
effective date and is completed
while you are enrolled under the
Dental Blue Freedom Plan.
• Services and supplies furnished
after your termination date under
the Dental Blue Freedom Plan.
(If your membership under the
Dental Blue Freedom Plan is ter-
minated prior to the completion
date of a procedure that requires
more than one visit, no ben-
efits are provided for the entire
procedure.)
Boston University Dental
Health Centers
There are two Boston University
Dental Health Centers. Both provide
a comprehensive range of dental
services, such as X-rays, cleanings,
fillings, and crowns. Fees for dental
services are found in your dental fee
schedule.
Locations: 930 Commonwealth
Avenue, Phone: 617-358-1000
and 100 East Newton Street,
Phone: 617-638-4670.
Key services include: general den-
tistry, dental hygiene, orthodontics,
pediatric dentistry, periodontics,
implantology, prosthodontics, oral
and maxillofacial surgery, and end-
odontics.
In-Network Dentists
BCBS Network
Dental Blue PPO dentists provide
you with the greatest value.
If your provider is in the Dental Blue
PPO Network, your share of the
cost of services may be less than if

41
your provider is in only the Dental
Blue Network. To determine which
networks your provider participates
in, review your provider’s profile
on the Blue Cross Blue Shield
website at www.bluecrossma.com/
findadoctor.
How to Locate a Dentist on
the Web
Go to the Blue Cross Blue Shield
website at www.bluecrossma.com/
findadoctor and look under “Dental
Blue.” If the dentist is in the BCBS
Network, his or her name will be
listed. You may also want to check
to find out if the dentist is in the
PPO Network. If he or she is, your
coinsurance may be lower than for
a dentist not in the PPO Network.
How Fees Are Set
This plan uses dentists in the Dental
Blue Network.
You may use dentists in the Dental
Blue or the Dental Blue PPO net-
works. All of these dentists are
contracted with Blue Cross Blue
Shield. If your dentist is in the PPO
Network, your coinsurance may be
lower than it would be for a dentist
who is not in the PPO Network.
Out-of–Network Dentists
Benefits for covered services by a
non-participating dentist outside of
Massachusetts are provided based
on usual and customary charges.
The allowed charge is based on a
schedule of charges established by
BCBS. You may be responsible for
any difference between the den-
tist’s actual charge or the allowed
charge, whichever is less. You are
also responsible for your deductible
and coinsurance (if applicable), and
charges beyond your calendar-year
maximum.
Out-of-network dentists do not
have contracts with Blue Cross Blue
Shield. Blue Cross Blue Shield will
reimburse you the percentage listed
on the chart of the usual and cus-
tomary charges.
How to File a Claim
BU Dental Health Centers and
BCBS Network Dentists
To obtain benefits for services
provided at the BU Dental Health
Centers or from a Blue Cross Blue
Shield network dentist, show the
dentist your Dental Blue Freedom
identification card. The dentist will
file the claim with Blue Cross Blue
Shield. You do not have to file a
claim form.
Out-of-Network Dentists
The following are procedures for
obtaining benefits if your provider
is not affiliated with a Boston
University Dental Health Center and
is not in the Blue Cross Blue Shield
network:
1. Obtain a claim form from the
Benefits Section of Human
Resources or from the website at
www.bu.edu/hr/home/forms/
benefit-forms.
2. Pay your dentist for services.
3. Submit your claim form with
original itemized bills within two
years of the date you received
the covered dental service to:
Blue Cross Blue Shield of
Massachusetts
P.O. Box 986030
Boston, MA 02298
Blue Cross Blue Shield will review
your claim, then reimburse you for
the claim to the extent of your ben-
efits described in this handbook.
Appealing a Denial for Either
Dental Health Plan
How to Request a Formal
Grievance Review
To request a formal review from
Blue Cross Blue Shield’s Grievance
Program, you (or your authorized
representative) have three options.
The preferred option is for you to
send your grievance in writing to:
Member Grievance Program
Blue Cross Blue Shield of
Massachusetts
One Enterprise Drive
Quincy, MA 02171-2126
Blue Cross Blue Shield will let you
know that your request was received
by sending you a written confirma-
tion within 15 calendar days.
Or, you may email your griev-
ance to Blue Cross Blue Shield’s
Grievance Program email address
at [email protected]. Blue
Cross Blue Shield will let you know
that your request was received by
sending you a confirmation immedi-
ately by email.
Or, you may call Blue Cross Blue
Shield’s Grievance Program at
1-800-462-5601 (extension 63605).
When your request is made by tele-
phone, Blue Cross Blue Shield will
send you a written account of the
grievance within 48 hours of your
phone call.
Once your request is received, Blue
Cross Blue Shield will research the
case in detail, ask for more informa-
tion as needed, and let you know in
writing of the decision or the out-
come of the review. If your grievance
is regarding termination of coverage
for concurrent services that were
previously approved by Blue Cross
Blue Shield, the disputed coverage
will continue until this grievance
review process is completed. This
continuation of coverage does not
42
apply to services that are limited
by dollar or visit maximums and
that exceed those maximums, non-
covered services, or services that
were received prior to the time that
you requested a formal grievance
review, or when a grievance is not
received on a timely basis, based on
the course of treatment.
All grievances must be received by
Blue Cross Blue Shield within one
year of the date of treatment, event,
or circumstance, such as the date
you were told of the service denial
or claim denial.
What to Include in a Grievance
Review Request
Your request for a formal grievance
review should include: the name
and identification number of the
member asking for the review; a
description of the problem; all rel-
evant dates; names of health care
providers or administrative staff
involved; and details of the attempt
that has been made to resolve the
problem. If Blue Cross Blue Shield
needs to review the medical/dental
records and treatment information
that relate to your grievance, Blue
Cross Blue Shield will promptly send
you an authorization form to sign if
needed. You must return this signed
form to Blue Cross Blue Shield. It will
allow for the release of your medi-
cal/dental records. You also have
the right to look at and get copies
(free of charge) of records and cri-
teria that Blue Cross Blue Shield has
and that are relevant to your griev-
ance, including the identity of any
experts who were consulted.
Authorized Representative
You may choose to have another
person act on your behalf during the
grievance review process. You must
designate this person in writing to
Blue Cross Blue Shield. Or, if
you are not able to do this, a person
such as a conservator, a person with
power of attorney, or a family mem-
ber may be your authorized repre-
sentative. Or, he or she may appoint
another party to be the authorized
representative. (When you are an
inpatient, a health care provider may
act as your authorized representa-
tive to ask for an expedited griev-
ance review. You do not have to
designate the health care provider
in writing.)
Who Handles the Grievance
Review
All grievances are reviewed by
individuals who are knowledgeable
about Blue Cross Blue Shield and
the issues involved in the grievance.
The individuals who will review your
grievance will be those who did not
participate in any of Blue Cross Blue
Shield’s prior decisions regarding
the subject of your grievance, nor do
they work for anyone who did. When
a grievance is related to a neces-
sity and appropriateness denial, at
least one grievance reviewer is an
individual who is an actively practic-
ing health care professional in the
same or similar specialty that usually
treats the medical/dental condition,
performs the procedure, or provides
treatment that is the subject of your
grievance.
Response Time
The review and response for Blue
Cross Blue Shield’s formal grievance
review will be completed within 30
calendar days. Every reasonable
effort will be made to speed up the
review of grievances that involve
health care services that are soon to
be obtained by the member. (When
the grievance review is for services
you have already obtained and it
requires a review of your medical/
dental records, the 30-day response
time will not include the days from
when Blue Cross Blue Shield sends
you the authorization form to sign
until it receives your signed authori-
zation form if needed. If Blue Cross
Blue Shield does not receive your
authorization within 30 calendar days
after you are asked for it, Blue Cross
Blue Shield may make a final decision
about your grievance without that
medical/dental information.)
Note: If your grievance review
began after an inquiry, the 30-day
response time will begin on the day
you tell Blue Cross Blue Shield that
you disagree with Blue Cross Blue
Shield’s answer and would like a for-
mal grievance review.
Blue Cross Blue Shield may extend
the time frame to complete a griev-
ance review, with your permission,
in cases when Blue Cross Blue
Shield and the member agree that
additional time is required to fully
investigate and respond to the
grievance. A grievance that is not
acted upon within the specified time
frames will be considered resolved
in favor of the member.
Written Response
Once the grievance review is com-
pleted, Blue Cross Blue Shield will let
you know in writing of the decision
or the outcome of the review. If Blue
Cross Blue Shield continues to deny
coverage for all or part of a health
care service or supply, Blue Cross
Blue Shield’s response will explain the
reasons. It will give you the specific
medical and scientific reasons for the
denial and a description of alternative
treatment, health care services, and
supplies that would be covered.
Grievance Records
Blue Cross Blue Shield will main-
tain a record of all formal griev-
ances, including the response for
each grievance review, for up to
seven years.

Expedited Review for Immediate
or Urgently Needed Services
In place of the formal grievance
review described above, you have
the right to request an “expedited”
review right away when your situ-
ation is for immediate or urgently
needed services. Blue Cross Blue
Shield will review and respond
to grievances for immediate or
urgently needed services as follows:
When your grievance review con-
cerns medical care or treatment for
which waiting for a response under
the grievance review time frames
described above would seriously
jeopardize your life or health or your
ability to regain maximum function
as determined by Blue Cross Blue
Shield or your physician, or if your
physician says that you will have
severe pain that cannot be ade-
quately managed without the care or
treatment that is the subject of the
grievance review, Blue Cross Blue
Shield will review your grievance and
notify you of the decision within 72
hours after your request is received.
When a grievance review is
requested while the member is an
inpatient, Blue Cross Blue Shield
will complete the review and make
a decision regarding the request
before the patient is discharged from
that inpatient stay. Coverage for
those services in dispute will con-
tinue until this review is completed.
A decision to deny payment
for health care services may be
reversed within 48 hours if the
member’s attending physician certi-
fies that a denial for those health
care services would create a sub-
stantial risk of serious harm to the
member if the member were to
wait for the outcome of the normal
grievance process.
A grievance review requested by a
member with a terminal illness will
be completed within five working
days of receiving the request. In this
case, if the expedited review results
in a denial for health care services or
treatment, Blue Cross Blue Shield will
send a letter to the member within
five working days that explains the
specific medical and scientific rea-
sons for the denial and a description
of alternative treatment, health care
services, and supplies that would
be covered and information about
requesting a hearing. When the
member requests a hearing, the hear-
ing will be held within ten days (or
within five working days if the attend-
ing physician determines after con-
sultation with Blue Cross Blue Shield’s
Medical Director and based on stan-
dard medical practice that the effec-
tiveness of the health care service,
supply, or treatment would be materi-
ally reduced if it were not furnished at
the earliest possible date). You and/
or your authorized representative(s)
may attend this hearing.
Appeals Process for Rhode Island
Residents or Services
You may also have the right to
appeal as described in this section
when a claim is denied as being not
necessary and appropriate. If so,
these rights are in addition to the
other rights to appeal that you have
as described in other parts of this
handbook. The following provisions
apply only to:
A member who lives in Rhode Island
and is planning to obtain services
that Blue Cross Blue Shield has
determined are not necessary and
appropriate.
A member who lives outside Rhode
Island and is planning to obtain ser-
vices in Rhode Island that Blue Cross
Blue Shield has determined are not
necessary and appropriate.
Blue Cross Blue Shield decides which
covered services are necessary and
appropriate for your dental condi-
tion based on a review of your dental
records and generally accepted
dental practice. Some of the covered
services described in this handbook
may not be necessary and appropri-
ate for you. If Blue Cross Blue Shield
has determined that services are not
necessary and appropriate for you,
you have the right to the following
appeals process.
Reconsideration
Reconsideration is the first step in
this appeals process. If you receive
a letter denying payment for your
dental services, you may request in
writing that Blue Cross Blue Shield
reconsider its decision by contacting:
Grievance Program
Blue Cross Blue Shield of
Massachusetts
One Enterprise Drive
Quincy, MA 02171-2126
Phone: 1-800-472-2689
Fax: 617-246-3616
Email: [email protected]
You must submit your reconsidera-
tion request within 180 days of the
adverse decision. Along with your let-
ter, you should include any informa-
tion that supports your request. Blue
Cross Blue Shield will review your
request and let you know the out-
come of your reconsideration request
within 15 calendar days after receipt
of all necessary information.
Appeal
An appeal is the second step in this
process. If Blue Cross Blue Shield
continues to deny benefits for all or
part of the original service, you may
request an appeal within 60 days of
receiving the reconsideration denial
letter. Your appeal request should
include any information that sup-
ports your appeal. You may also
inspect and add information to your
Blue Cross Blue Shield case file to
prepare your appeal. In accordance
43

44
with Rhode Island state law, if you
wish to review the information in
your Blue Cross Blue Shield case
file, you must make your request
in writing and include the name of
a dentist who may review your file
on your behalf. Your dentist may
review, interpret, and disclose any
or all of that information to you.
Once received by Blue Cross Blue
Shield, your appeal will be reviewed
by a dentist in the same specialty as
your attending dentist. Blue Cross
Blue Shield will notify you of the
outcome of your appeal within 15
calendar days of receiving all neces-
sary information.
External Appeal
If your appeal is denied, you have
the right to present your case to an
appeals agency that is designated
by Rhode Island and not affiliated
with Blue Cross Blue Shield. If you
request this voluntary external
appeal, Rhode Island requires you
be responsible for half of the cost
of the appeal and Blue Cross Blue
Shield will be responsible for the
remaining half. To file an external
appeal, you must send your request
in writing to:
Grievance Program
Blue Cross Blue Shield of
Massachusetts
One Enterprise Drive
Quincy, MA 02171-2126
Phone: 1-800-472-2689
Fax: 617-246-3616
Email: [email protected]
Along with your request, you must
state your reason(s) for your dis-
agreement with Blue Cross Blue
Shield’s decision and enclose a
check payable to one of the fol-
lowing external appeals agencies:
MassPRO (your fee is $147.50) or
the MAXIMUS Center for Health
Dispute Resolution (your fee is
$144.20).
Within five working days after the
receipt of your written request
and payment for the appeal, Blue
Cross Blue Shield will forward your
request to the external appeals
agency along with Blue Cross Blue
Shield’s portion of the fee and your
entire Blue Cross Blue Shield case
file. The external appeals agency
will notify you in writing of the deci-
sion within ten working days of
receiving all necessary information.
Expedited Appeal
If your situation is an emergency,
you have the right to an expedited
appeal at all three levels of appeal
as stated above. An emergency
requires emergency dental treatment
to relieve acute pain or to control a
dental condition that requires imme-
diate care to prevent permanent
harm to the member. You may
request an expedited reconsideration
or appeal by contacting Blue Cross
Blue Shield at the telephone number
shown in your letter. Blue Cross Blue
Shield will notify you of the result of
your expedited appeal within two
working days or 72 hours, whichever
is sooner, of its receipt. To request
an expedited voluntary external
appeal, you must send your request
in writing to:
Grievance Program
Blue Cross Blue Shield of
Massachusetts
One Enterprise Drive
Quincy, MA 02171-2126
Phone: 1-800-472-2689
Fax: 617-246-3616
Email: [email protected]
Your request should state your
reason(s) for your disagreement
with the decision and include signed
documentation from your dentist
that describes the emergency nature
of your treatment. In addition, you
must also enclose a check payable
to one of the following external
appeals agencies: MassPRO (your
fee is $172.50) or the MAXIMUS
Center for Health Dispute
Resolution (your fee is $144.20).
Within two working days after the
receipt of your written request and
payment for the appeal, Blue Cross
Blue Shield will forward your request
to the external appeals agency along
with Blue Cross Blue Shield’s portion
of the fee and your entire Blue Cross
Blue Shield case file. The external
appeals agency will notify you in
writing of the decision within two
working days or 72 hours, whichever
is sooner, of receiving your request
for a review.
External Appeal Final Decision
If the external appeals agency
upholds the original decision of Blue
Cross Blue Shield, this completes
the appeals process for your case.
But, if the external appeals agency
reverses Blue Cross Blue Shield’s
decision, the claim in dispute will
be reprocessed by Blue Cross Blue
Shield upon receipt of the notice of
the final appeal decision. In addition,
Blue Cross Blue Shield will repay
you for your share of the cost for
the external appeal within 60 days
of the receipt of the notice of the
final appeal decision.
Disability
If You Incur a Total Disability
If you incur a total disability and begin
receiving benefits from the Boston
University Long-Term Disability
Benefits Plan, you may continue your
membership in the Boston University
Dental Health Plan at no cost to you
for the duration of your total disabil-
ity while you receive benefits under
the Boston University Long-Term
Disability Benefits Plan. The Benefits
Section of Human Resources will
explain this feature to you upon notifi-
cation of your disability.

45
If You Die While You Are a Member
of the Plan
Your enrolled dependents will be
entitled to continue coverage for
up to 36 months under COBRA, as
described later in this section.
When You Retire
You and your enrolled dependents
will be entitiled to continue coverage
for up to 18 months under COBRA,
as described later in this section.
Leaves of Absence and
No-Pay Status
If you are on a leave of absence or
no-pay status, you must contact
the Benefits Section of Human
Resources to ask what impact your
absence may have on your participa-
tion in the Dental Plan.
• Leave of Absence with Pay If you
are granted a leave of absence
with pay (including sabbatical),
your Dental Plan coverage will
continue, provided your usual
payroll deductions continue. If
you wish to discontinue your
membership, you may do so by
obtaining the necessary forms
from the Benefits Section of
Human Resources.
• Leave of Absence Without Pay and
No-Pay Status If you are granted a
leave of absence without pay or
no-pay status, you may continue
your Dental Plan coverage during
your leave, provided you pay the
employee cost of continuing this
coverage.
If you choose to continue cover-
age, you must contact the Benefits
Section of Human Resources
before you begin your leave
to make the necessary billing
arrangements. This coverage will
be automatically canceled if you
fail to make required payments.
If you do not wish to continue
your coverage during your unpaid
leave of absence, you may dis-
continue your membership by
obtaining the necessary forms
from the Benefits Section of
Human Resources. Re-enrollment
in the Boston University Dental
Health Plan will be possible
when you return from a leave
of absence or no-pay status, as
long as you contact the Benefits
Section of Human Resources and
enroll within 30 days of the date
you return.
The COBRA continuation of cover-
age provisions would also apply in
this situation should you wish to
elect COBRA coverage.
When Your Coverage Ends
If your employment with the
University terminates for any
reason, including retirement, your
Dental Plan membership will end on
the last day of the month in which
your employment terminates.
Once the payroll system reflects the
termination of your employment,
the Benefits Section of Human
Resources will automatically notify
you in writing of your last day of
coverage, and of what to do to con-
tinue coverage.
In addition to any continuation provi-
sions provided by Boston University,
you and your covered dependents
have the right to extend your cover-
age for up to 18 or 36 months under
the federal continuation provisions
(COBRA) explained in the following
section.
Coverage Continuation
Provisions
A federal law known as COBRA
requires that most employers
sponsoring group dental health
plans offer employees and their
families (“qualified beneficiaries”)
the opportunity to elect and pay
for a temporary extension of dental
health coverage called “continua-
tion coverage” at group rates in cer-
tain instances (“qualifying events”)
where coverage under the employ-
er’s dental health plan would other-
wise end. This notice is intended to
inform you, in a summary fashion,
of your rights and obligations under
the continuation coverage provi-
sions of that law. (Both you and
your spouse should take time to
read this notice carefully.) Under
the Plan, qualified beneficiaries who
elect COBRA continuation coverage
must pay for the coverage.
If you are an employee of the Plan
Sponsor (Boston University) cov-
ered by one of the dental health
plan options maintained by the
Plan Sponsor (the “Plan”), you will
become a qualified beneficiary if you
lose your group dental health cover-
age because either one of the fol-
lowing qualifying events happens:
• Your hours of employment are
reduced, or
• Your employment ends for any
reason other than your gross
misconduct.
If you are the spouse of an employee
covered by the Dental Plan, you will
become a qualified beneficiary if you
lose your coverage under the Dental
Plan because any one of the follow-
ing qualifying events happens:
• Your spouse dies;
• Your spouse’s employment ends
for any reason other than his or
her gross misconduct;
• Your spouse’s hours of employ-
ment are reduced;
• You become divorced or legally
separated from your spouse; or

• Your spouse becomes entitled
to Medicare (under Part A,
Part B, or both).
Your dependent children will
become qualified beneficiaries if
they lose coverage under the Dental
Plan because any one of the follow-
ing qualifying events happens:
• The parent-employee dies;
• The parent-employee’s hours
of employment are reduced;
• The parent-employee’s employ-
ment ends for any reason other
than his or her gross misconduct;
• The parents become divorced
or legally separated;
• The parent-employee becomes
entitled to Medicare benefits
(Part A, Part B, or both); or
• The child ceases to be eligible for
coverage under the Plan as
a “dependent child.”
Sometimes, filing a proceeding
in bankruptcy under title 11 of
the United States Code can be a
qualifying event. If a proceeding in
bankruptcy is filed with respect to
the Dental Plan Sponsor and that
bankruptcy results in the loss of
coverage of any retired employee
covered under the Dental Plan, the
retired employee will become a
qualified beneficiary with respect to
the bankruptcy. The retired employ-
ee’s spouse or surviving spouse and
dependent children will also become
qualified beneficiaries if bankruptcy
results in the loss of their coverage
under the Dental Plan.
When Is COBRA Coverage
Available?
The Dental Plan will offer COBRA
continuation coverage to quali-
fied beneficiaries only after the
Plan Administrator has been noti-
fied that a qualifying event has
occurred. When the qualifying
event is the end of employment
or reduction of hours of employ-
ment, death of the employee, or
the employee’s becoming entitled
to Medicare benefits (under Part A,
Part B, or both), the Plan Sponsor
must notify the Plan Administrator
of the qualifying event.
You Must Give Notice of Some
Qualifying Events
For the other qualifying events
(divorce or legal separation of the
employee and spouse, or a depen-
dent child’s losing eligibility for cov-
erage as a dependent child, etc.), you
must notify the Plan Administrator
within 60 days after the qualifying
event occurs. You must provide this
notice to the Plan Contact listed at
the end of this summary, along with
documentation substantiating the
divorce, legal separation, or loss of
dependent status and the effective
date of such event.
A child who is born to or placed
for adoption with the covered
employee during a period of COBRA
continuation coverage will be eli-
gible to become a qualified benefi-
ciary and be added to the covered
employee’s COBRA continuation
coverage. You must notify the Plan
Administrator within 60 days after
the birth or placement for adoption
occurs. You must provide this notice
to the Plan Contact listed at the end
of this summary, along with copies
of legal documents substantiating
the birth or placement for adoption
and the effective date of such event.
How Is COBRA Coverage
Provided?
Once the Plan Administrator
receives notice that a qualifying
event has occurred, COBRA con-
tinuation coverage will be offered
to each of the qualified benefi-
ciaries. Each qualified beneficiary
will have an independent right to
elect COBRA continuation cover-
age. Covered employees may elect
COBRA continuation coverage on
behalf of their spouses, and parents
may elect COBRA continuation cov-
erage on behalf of their children.
Under the law, you have at least
60 days from the date you would
lose coverage because of one of the
events described above to inform
the Plan Administrator that you
want to elect continuation cover-
age. If you do not elect continuation
coverage, your group dental health
coverage will end. If you elect con-
tinuation coverage, the Plan Sponsor
is required to permit you to elect
and purchase coverage which, as of
the time coverage is being provided,
is identical to the coverage provided
under the Plan to similarly situated
employees or family members.
When the qualifying event is the
end of employment or reduction of
the employee’s hours of employ-
ment, and the employee became
entitled to Medicare benefits less
than 18 months before the qualify-
ing event, COBRA continuation
coverage for qualified benefi-
ciaries other than the employee
lasts until 36 months after the
date of Medicare entitlement. For
example, if a covered employee
becomes entitled to Medicare 8
months before the date on which
his employment terminates,
COBRA continuation coverage for
his spouse and children can last
up to 36 months after the date of
Medicare entitlement, which is
equal to 28 months after the date
of the qualifying event (36 months
minus 8 months).
When the qualifying event is
the death of the employee, the
employee’s becoming entitled to
Medicare benefits (under Part A, Part
46

B, or both), your divorce, legal separa-
tion, or a dependent child’s losing eli-
gibility as a dependent child, COBRA
continuation coverage lasts for up
to a total of 36 months. Otherwise,
when the qualifying event is the end
of employment or reduction of the
employee’s hours of employment,
COBRA continuation coverage gener-
ally lasts for only up to a total of 18
months. There are two ways in which
this 18-month period of COBRA con-
tinuation coverage can be extended.
Disability Extension of 18-Month
Period of Continuation Coverage
If you or anyone in your family
covered under the Dental Plan is
determined by the Social Security
Administration to be disabled (for
purposes of Title II [OASDI] or
Title XVI [SSI] of the Social Security
Act) and you notify the Plan
Administrator in a timely fashion,
you and your entire family may be
entitled to receive up to an addi-
tional 11 months of COBRA continu-
ation coverage, for a total maximum
of 29 months. The disability would
have to have started at some time
before the 60th day of COBRA con-
tinuation coverage and must last at
least until the end of the 18-month
period of continuation coverage.
The qualified beneficiary must also
notify the Plan Administrator within
30 days of the date of any final
determination by the Social Security
Administration that he or she is no
longer disabled. You must provide
these notices to the Plan Contact
listed at the end of this summary,
along with copies of correspon-
dence from the Social Security
Administration substantiating the
disability/loss of disability and the
effective date of the applicable
SSA determination. Furthermore,
during the period after the 18th
month through the 29th month of
continuation coverage, the monthly
premium cost will be increased to
150% of the applicable premium
relating to continuation coverage.
Second Qualifying Event Extension
of 18-Month Period of Continuation
Coverage
If your family experiences another
qualifying event while receiving 18
months of COBRA continuation
coverage, the spouse and depen-
dent children in your family can
get up to 18 additional months of
COBRA continuation coverage,
for a maximum of 36 months, if
notice of the second qualifying
event is properly given to the Plan
Administrator. You must provide
this notice to the Plan Contact
listed at the end of this summary,
along with copies of documenta-
tion substantiating the second
qualifying event. This extension
may be available to the spouse and
any dependent children receiv-
ing continuation coverage if the
employee or former employee dies,
becomes entitled to Medicare ben-
efits (under Part A, Part B, or both),
or gets divorced, legally separated,
or if the dependent child stops
being eligible under the Dental Plan
as a dependent child, but only if
the event would have caused the
spouse or dependent child to lose
coverage under the Plan had the
first qualifying event not occurred.
How Much Does COBRA
Continuation Coverage Cost?
Each qualified beneficiary must
pay the entire cost of continuation
coverage. The amount a quali-
fied beneficiary must pay may not
exceed 102% (or, in the case of an
extension of continuation cover-
age due to disability, 150%) of the
cost to the Dental Plan (includ-
ing both employer and employee
contributions) for coverage of a
similarly situated plan participant
or beneficiary who is not receiving
continuation coverage.
When and How Must Payment
for COBRA Continuation Coverage
Be Made?
First Payment for Continuation Coverage
If you elect continuation cover-
age, you do not have to send any
payment with the election form.
However, you must make your first
payment for continuation coverage
not later than 45 days after the date
of your election. (This is the date
the election notice is postmarked,
if mailed.) If you do not make your
first payment for continuation cov-
erage in full not later than 45 days
after the date of your election, you
will lose all continuation cover-
age rights under the Plan. You are
responsible for making sure that
the amount of your first payment is
correct. You may contact the party
responsible for COBRA administra-
tion under the Plan at the address,
phone number, or email address
provided at the end of this section
to confirm the correct amount of
your first payment.
Periodic Payments for Continuation
Coverage
After you make your first payment
for continuation coverage, you
will be required to make periodic
payments for each subsequent
coverage period. The amount due
for each coverage period for each
qualified beneficiary is shown in this
notice. The periodic payments can
be made on a monthly basis. Under
the Plan, each of these periodic pay-
ments for continuation coverage is
due on the first day of the month for
that coverage period. If you make
a periodic payment on or before
the first day of the coverage period
to which it applies, your coverage
under the Plan will continue for that
coverage period without any break.
47

48
Grace Period for Periodic Payments
Although periodic payments are
due on the dates shown above,
you will be given a grace period
of 30 days after the first day of
the coverage period to make each
periodic payment. Your continu-
ation coverage will be provided
for each coverage period as long
as payment for that coverage
period is made before the end of
the grace period for that payment.
However, if you pay a periodic
payment later than the first day
of the coverage period to which
it applies, but before the end of
the grace period for the coverage
period, your coverage under the
Plan will be suspended as of the
first day of the coverage period
and then retroactively reinstated
(going back to the first day of
the coverage period) when the
periodic payment is received. This
means that any claim you submit
for benefits while your coverage
is suspended may be denied and
may have to be resubmitted once
your coverage is reinstated.
Early Termination of COBRA
COBRA provides that your continu-
ation coverage may be terminated
before the end of the maximum
coverage period for any of the fol-
lowing reasons:
• The Plan Sponsor no longer pro-
vides group dental health cover-
age to any of its employees;
• Any required premium for
continuation coverage is not
paid in full on time;
• A qualified beneficiary becomes
covered—after electing COBRA
continuation coverage—under
another group dental health plan
(as an employee or otherwise)
that does not impose any pre-
existing condition limitation for
a pre-existing condition of the
qualified beneficiary;
• A qualified beneficiary becomes
entitled to Medicare (under Part
A, Part B, or both) after electing
COBRA continuation coverage;
• A qualified beneficiary extends
coverage for up to 29 months due
to disability and there has been a
final determination that the indi-
vidual is no longer disabled.
The Health Insurance Portability
and Accountability Act of 1996
(HIPAA) restricts the extent to
which group dental health plans
may impose pre-existing condition
limitations. HIPAA coordinates
COBRA’s other coverage cut-off
rule (in the third bullet above) with
these new limits as follows:
If you become covered by another
group dental health plan and that
plan contains a pre-existing limita-
tion that affects you, your COBRA
coverage cannot be terminated.
However, if the other plan’s pre-
existing condition does not apply to
you by reason of HIPAA’s restric-
tions on pre-existing condition
clauses, the Plan Sponsor may ter-
minate your COBRA coverage.
You do not have to show that you
are insurable to choose continuation
coverage. However, as discussed
above, you will have to pay all the
required premiums for your continu-
ation coverage.
The law also says that, at the end of
the 18-month, 29-month, or 36-month
continuation coverage period, you
must be allowed to enroll in an indi-
vidual conversion dental health plan if
such an individual conversion dental
health plan is otherwise generally
available under the Plan.
COBRA continuation coverage may
be terminated for any reason if the
Plan would terminate coverage
of a participant or beneficiary not
receiving continuation coverage
(such as fraud).
If You Have Questions
More complete information regard-
ing your COBRA continuation
coverage rights is available from
the Plan Administrator. For more
information about your rights
under ERISA, including COBRA,
the Health Insurance Portability
and Accountability Act (HIPAA),
and other laws affecting group
health plans, contact the nearest
regional or district office of the U.S.
Department of Labor’s Employee
Benefits Security Administration
(EBSA) in your area or visit the
EBSA website at www.dol.gov/
ebsa. (Addresses and phone
numbers of regional and district
EBSA offices are available through
EBSA’s website.)
Plan Contact Information (Plan
Administrator)
Benefits Section of Human Resources
Boston University
25 Buick Street
Boston, MA 02215
Phone: 617-353-4489
Email: [email protected]

Overview
Long-Term Disability Plan

50
O
nce you have completed three years of continuous service with
the University, you will automatically be enrolled in the Long-Term
Disability (LTD) Plan. The LTD Plan is designed to provide a continuing
income to you and your family after a six-month waiting period if you are
unable to work for longer than six months because of a total disability or if
you are partially disabled and are suffering a 20% or greater earnings loss.
Boston University pays the entire cost of your Long-Term Disability Plan.
You may also be eligible for coverage under disability plans not mentioned
in this section. These may include the Short-Term Disability Plan, the
Temporary Disability Plan, or other government-sponsored plans such as
Social Security or Workers’ Compen sation. For additional information, see
your Employee Handbook, the Faculty Handbook, your collective bargaining
agreement, and the “Other Benefits” section of this handbook.

Eligibility
If you are classified by the University
as a regular employee, work a
full-time schedule, and have an
appointment of nine months’ or
more duration, you automatically
become a member of the Long-
Term Disability Plan on the first
day of the month coincident with or
following your completion of three
years of continuous full-time service.
If you are not at work on the day you
would normally become a member,
you will become a member in the
plan on the day you return to work
performing your normal duties.
The three-year service requirement
may be waived, allowing you to
become a member on your first
day of work, if you meet the fol-
lowing requirements:
1. You have a regular full-time
appointment of at least nine
months’ duration with the
University; and
2. You provide the Benefits
Section of Human Resources
with satisfactory evidence that
you had been covered by your
previous employer’s long-term
disability program at the time
you left that employer, and no
more than three months have
passed between the termina-
tion of such coverage and your
first day of employment with
the University; and
3. You submit the evidence of
coverage within 30 days from
the date of your orientation.
You pay nothing for your coverage
under the Long-Term Disability Plan.
The University pays the entire cost
of this plan.
Plan Benefits
As explained below, you may
receive benefits from the plan if you
are a member and become totally
disabled or partially disabled while
you are covered under the plan.
No benefits are provided for any
disabilities commencing before you
were covered under the plan or
after your coverage under the plan
terminates.
“Totally disabled,” for purposes of
the plan, means that, because of
medically determinable illness or
injury:
• You cannot perform each of
the material duties of your own
occupation for which you are
reasonably fitted by training,
education, or experience during
the elimination period and the
next 24 months, and thereafter,
unable to perform the material
duties of any occupation.
“Partial disability,” for purposes of
the plan, means that, because of
your medically determinable illness
or injury:
• While unable to perform all the
material duties of your regular
occupation on a full-time basis
because of injury or illness, you
are:
a. Performing at least one of the
material duties of your regular
occupation or another occupa-
tion on a part-time or full-time
basis; and,
b. Earning currently at least
20% less per month than your
pre-disability earnings.
Note: Either or both of these can satisfy
the elimination period.
“Elimination period,” for purposes
of the plan, refers to the six-month
period during which you must con-
tinuously have a total disability or
partial disability before you can begin
receiving benefits from the plan.
You must be totally disabled or par-
tially disabled and suffering a 20%
earnings loss for at least six consec-
utive months before you can begin
receiving benefits. Benefit payments
will begin on the date you complete
180 days of continuous total and/or
partial disability.
After completing the elimination
period, you will receive monthly
disability benefit payments while
you remain totally or partially
disabled.
If you are totally disabled, each
monthly payment will be 60% of
your monthly base salary, up to a
maximum monthly benefit amount
of $14,500. This means the maxi-
mum covered salary is $24,166.67
per month (or $290,000 per year),
since $24,166.67 times 60% equals
$14,500.
If you are partially disabled, the
amount of your monthly disability
benefit will be adjusted, taking into
consideration the amount of your
earnings while partially disabled. The
monthly benefit for partial disability
is 75% of the difference between
your full-time monthly base salary
and your monthly base salary while
you are partially disabled. For exam-
ple, if your regular full-time monthly
base salary is $1,000 and your salary
while you are partially disabled is
$650, you deduct $650 from $1,000
to get $350. Multiply $350 by 75%
to get $262.50, which is the amount
of your monthly disability benefit.
51
Long-Term Disability Plan
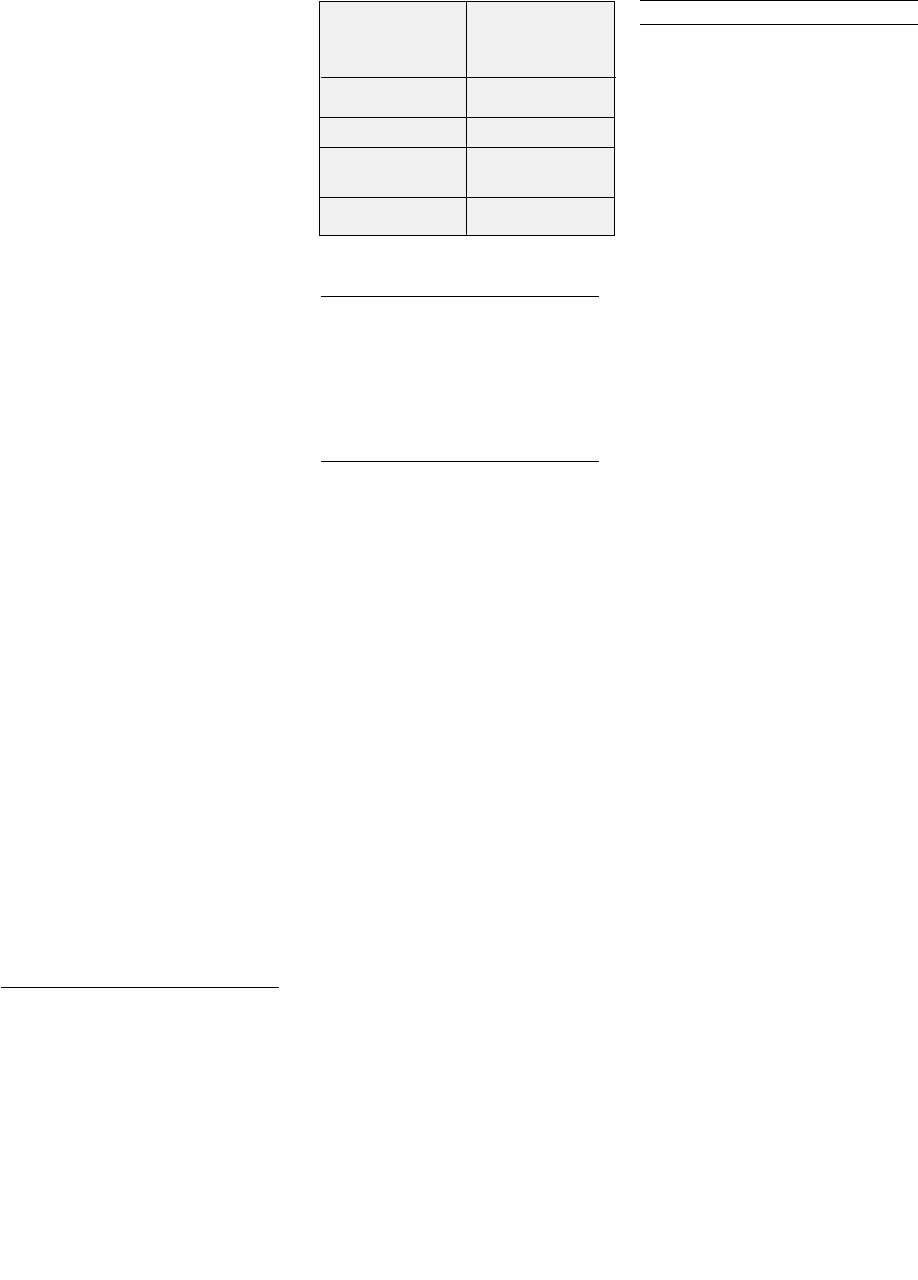
52
Your monthly disability payments
from the plan will be reduced by any
payments you receive from any of
the following sources:
• Social Security (including any
benefits for dependents) or
similar government programs
• Workers’ Compensation or simi-
lar payments, except when they
result from previous injuries or
disabilities
• Any group disability benefits
payable under any group insur-
ance or retirement plan to which
the University contributes
• Sick pay
The plan does, however, guarantee
you a minimum benefit of $100 per
month regardless of your income
from other sources.
You are required to apply for Social
Security benefits should your dis-
ability be expected to extend for
12 months.
On July 1 following the first 12
months during which you have
received disability payments, and
each July 1 thereafter, the amount of
your monthly disability income from
this plan will be increased by 3%.
These increases apply for the first
10 years of disability under this plan
and then stop.
Benefit Duration
The following table illustrates ben-
efit duration periods under the plan.
This is the maximum period that the
plan will pay you benefits as long as
you remain disabled.
Once Long-Term Disability benefits
cease, you may be eligible for ben-
efits from your participation in a
retirement plan or for Social Security
retirement benefits.
How to Obtain Benefits
To claim benefits from the Long-
Term Disability Plan, you should
contact the Benefits Section of
Human Resources as soon as your
partial or total disability begins.
(You should also contact your local
Social Security office to apply for
Disability Insurance benefits.) The
University will assist you in com-
pleting the claim forms and will
forward your claim to the plan’s
Claims Processor.
To process your claim, the insur-
ance company may require you to
be examined by a physician or other
specialist from time to time, at its
own expense. Long-term disability
benefits will be discontinued if you
fail to provide proof of continued
disability or partial disability and
regular attendance of a physician or
refuse to be examined or evaluated
at reasonable intervals or refuse to
receive appropriate available treat-
ment. The employee bears the cost
of regular physician visits while the
insurance company bears the cost
of required examinations.
Proof of claim must be given no later
than 30 days after the end of the elimi-
nation period.
Once the Claims Processor receives
your application for benefits and
supporting documentation, it will
be paid promptly (as long as it is a
valid claim).
If your claim is denied, the Claims
Processor will notify you of the
adverse decision within a reason-
able period of time, but not later
than 45 days after receiving the
claim. This 45-day period may be
extended for up to 30 days, if the
Claims Processor: (1) determines
the extension is necessary because
of matters beyond the plan’s con-
trol, and (2) notifies you, before
Federal Income Tax on
Long-Term Disability Income
Under present federal income tax
laws, your disability benefits are
considered taxable income to you
in the year they are received.
Subrogation and Reimbursement
The Boston University Long-Term
Disability Plan also has a subroga-
tion and reimbursement rule. If
another party is legally responsible
to pay lost earnings resulting from
an illness or injury inflicted on you,
the Long-Term Disability Plan is
entitled to reimbursement out of
any recovery from the responsible
party (or from any insurer) for the
amount of Long-Term Disability
benefits paid by the plan. The cov-
ered individual must cooperate
with the Long-Term Disability Plan
to recover such amounts. If the
covered individual receives pay-
ment from the responsible party (or
any insurer) before the Long-Term
Disability Plan receives amounts
paid as Long-Term Disability ben-
efits, the covered individual must
hold any amount recovered from
the responsible party in trust for the
benefit of the Long-Term Disability
Plan to the extent of the Long-Term
Disability benefits paid by the Long-
Term Disability Plan, and must
repay the Long-Term Disability Plan
from the amounts recovered.
Age When
Benefits Duration of
Commence Benefits
to age 65 but not
60 or younger less than 5 years
61 to 64 5 years
to age 70 but not
65 to 69 less than 1 year
70 and older 1 year

the end of the 45-day period, why
the extension is needed and the
expected decision date. If, before
the end of the first 30-day exten-
sion, the Claims Processor deter-
mines, due to matters beyond the
plan’s control, a decision cannot
be rendered within that extension
period, the determination period
may be extended for up to an addi-
tional 30 days, provided the Claims
Processor notifies you, before the
end of the first 30-day extension
period, why the extension is needed
and the expected decision date.
The notice of extension shall
explain: (1) the standards on which
benefit entitlement is based, (2)
the unresolved issues that prevent
a claim decision, and (3) the addi-
tional information needed. You
have at least 45 days to provide
the information.
The claim determination time
frames begin when a claim is filed,
without regard to whether all the
information necessary to make a
claim determination accompanies
the filing.
If an extension is necessary
because you failed to submit neces-
sary information, the days from
the date the Claims Processor
sends you the extension notice
until you respond to the request
for additional information are not
counted as part of the claim deter-
mination period.
Any denial will include specific
reasons for the denial, and the pro-
visions of the Claims Processor con-
tract on which the denial is based. It
will also explain how to apply for a
review of the denied claim. Where
appropriate, it will also include a
description of any material that is
needed to complete or perfect your
claim, and will explain why such
material is necessary.
Appealing a Denial
The Claims Processor is solely
responsible for determining what
constitutes a covered claim under
this plan. If the Claims Processor
denies your claim for benefits, in
whole or in part, you have a right
to appeal the denial. You have
180 days to appeal a denied claim.
After the receipt of the request for
review, the appeal must be decided
within 45 days unless special cir-
cumstances apply and notice is
given before the first 45-day period
expires. In this case, the decision
on appeal must be rendered within
45 days from the extension.
Additional information (other than
the above time periods) about how to
appeal a denial of benefits is included
in the “Administrative Information”
section of this handbook.
Monthly Retirement Plan
Waiver Benefit
The Monthly Retirement Plan Waiver
Benefit is a special feature of this
plan for those who participate in the
Boston University Retirement Plan.
(See the
“
Retirement Plan” section of
this handbook.) This feature provides
for the Long-Term Disability Plan
to pay your required contributions
and the University’s normal contri-
butions to your Boston University
Retirement Plan account while you
are receiving payments from this
plan. In this way, the plan allows your
Boston University retirement benefits
to accumulate even while you are
receiving disability income. The con-
tribution will continue to be made for
you until you recover, die, or your dis-
ability benefits end. Following is how
this monthly benefit works.
Unless you notify the Benefits
Section of Human Resources
that you want to make a change,
your Retirement Plan benefit
contributions will continue to be
invested with the same invest-
ment sponsor(s) and investment
option(s) that you were using
before becoming disabled. The
Claims Processor will forward
the monthly benefit to the Plan
Administrator to deposit with the
investment of your choice. If you
were dividing your contributions
between Fidelity and TIAA-CREF,
your monthly waiver benefit would
continue to be divided in the same
proportion. You can change your
investment choices for future
waiver benefit contributions at any
time by notifying the investment
sponsor directly.
The monthly waiver benefit equals
the required contribution you were
making to the Retirement Plan at
the time your disability started plus
the University’s contribution. In
addition, on July 1 following the first
12 months during which you have
received disability payments, the
amount of your waiver benefit con-
tributions is increased by 3%. These
increases apply on each subsequent
July 1 for the first 10 years of disabil-
ity and then stop.
The Monthly Retirement Plan
Waiver benefit does not apply to
any payments you were making in
addition to the amounts required
under the Boston University
Retirement Plan. Also, the waiver
benefit credited to your Retirement
Plan account is subject to certain
tax law limits. If your waiver benefit
exceeds the limits, all or a portion
of it will be contributed to your
Retirement Plan accounts on an
after-tax basis or paid to you as
taxable income.
53

54
The following tables outline the spe-
cific percentages of monthly salary
that would continue to be contri-
buted to your Boston University
Retirement Plan during your total
disability under the waiver benefit.
If you contribute to the current
retirement plan (as described in the
“Retirement Plan” section of this
handbook), Table I applies to you.
If you have elected to remain an
active participant in the retire-
ment plan that was in effect on
December 31, 1986 (known as
Boston University Retirement Plan
1965), Table II applies to you.
For more information about how the
Monthly Retirement Plan Waiver
Benefit operates, you should con-
tact the Benefits Section of Human
Resources.
Exclusions and Limitations
As in most plans of this type, there
are some disabilities which are not
Table I
Percentage of Covered Monthly Salary
Attained Age Up to the Integration Level Above the Integration Level
Under 45 8% 13%
45 through 49 10% 15%
50 and above 12% 17%
Table Il
Percentage of Covered Monthly Salary
Attained Age Up to 65 Above 65
Under 45 8% 12%
45 through 49 10% 15%
50 and above 10.3% 18%
covered. Examples of disabilities
excluded from this plan are as
follows:
1. war, declared or undeclared, or
any act of war;
2. intentionally self-inflicted inju-
ries, while sane or insane;
3. participation in a riot;
4. the committing of or attempting
to commit a felony or misde-
meanor;
5. cosmetic surgery unless such
surgery is in connection with
an injury or sickness sustained
while the individual is a covered
person;
6. a gender change, including,
but not limited to, any opera-
tion, drug therapy, or any other
procedure related to a gender
change.
No benefit will be payable during
any period of incarceration.
For more information on exclusions
and limitations, you should con-
tact the Benefits Section of Human
Resources.
Leaves of Absence
If you leave work for any reason for
a prolonged period, you should con-
tact the Benefits Section of Human
Resources to ask how your absence
may affect your participation in this
plan.
When Plan Membership Ends
If you are a member of this plan and
you are not disabled, your participa-
tion will end on the day that either
of the following events occurs:
• You terminate your employment
with Boston University, or
• Your status as a regular
employee ends
If one of these events occurs and
you are disabled under the plan
but not yet receiving benefits, you
should contact the Benefits Section
of Human Resources.

Overview
Survivor Insurance
56
B
oston University offers you insurance plans that provide benefits
to help maintain financial security for your beneficiaries in the
event of your death.
Under the Group Basic Life Insurance Plan, you are automatically provided
with basic coverage equal to one times your annual base salary at no
cost to you as long as you are actively at work on the day your cover-
age becomes effective.
If you wish and are eligible, you can, at your expense, also purchase
Group Supplemental Life Insurance equal to one, two, three, four, or five
times your base annual salary. You may also cover your spouse and
children under this plan.
The Travel Accident Insurance Plan is also provided at no cost to you.
It provides benefits to you or your beneficiaries if you suffer a covered
injury or are injured or killed while traveling on authorized University
business.
The Personal and Family Accident Insurance Plan provides benefits
should you or your family members suffer a covered injury or be killed
as the result of any accident—for University employees this includes
accidents on and off the job—on a worldwide, 24-hour basis. You pay
the cost for the coverage you choose under this plan.
Once you have completed five years of service, the Supplemental
Death Benefit Plan will automatically provide your beneficiaries with
a lump sum payment equal to one month’s base salary in the event of
your death. The benefits under this plan are provided free of charge to
you and apply regardless of the amount of coverage you have under
other University-sponsored plans.
Basic Life Insurance Plan
Eligibility
If you are classified by the
University as a regular employee,
work a full-time schedule, and have
an appoint ment of nine months’
or more duration, you are eligible
to participate in the Basic Life
Insurance Plan on your first day
of active employment.
Coverage
The University will automatically
provide you with basic life insurance
equal to one times your annual base
salary, rounded up to the next high-
est $1,000 if not already an even
multiple of $1,000, to a maximum
of $700,000.
For example, if your annual base
salary is $28,100, your basic life
insurance coverage is $29,000. If
your annual base salary is exactly
$28,000, your basic life insurance
coverage is $28,000.
Your basic life insurance coverage
becomes effective on your first day
of active employment. If you are
absent from active work and not
performing your normal duties on
the day your basic life coverage
would normally begin, you will not
be covered by this insurance until
the day you return to active work.
When the amount of your annual
base salary changes, the amount
of basic life insurance may also
change. For example, if your base
salary increased from $29,100
to $29,300 per year, you would
still have $30,000 in basic life
insurance coverage. If your base
salary increased from $28,800 to
$29,200, your basic life insurance
would increase from $29,000 to
$30,000 of coverage. The change
takes effect on the first of the
month coincident with or next
following the effective date of an
increase in your salary.
If your salary decreases, your basic
life insurance coverage remains the
same. If you are not actively at work
performing your duties on the day a
change in your basic life cov er age
would normally become effective,
the change will not become effec-
tive until the day you return to
active work.
Cost
You pay nothing for your basic life
insurance under this plan. The cost
of this coverage is paid entirely by
the University.
Special Tax Considerations
Under current tax laws, all or a por-
tion of the value of employer-paid
basic life insurance coverage in
excess of $50,000 may be subject
to federal income, Massachusetts
state income, and Social Security
taxes. This taxable amount is called
“imputed income,” and will be
included in the taxable earnings
shown on your W-2 Form.
Payment of Benefits
to Your Beneficiary
This plan will pay the full amount
of your Group Basic Life Insurance
in force at the time of your death
to the beneficiary of your choice.
You choose your beneficiary by
completing a form provided to you
by Human Resources, or from the
website at www.bu.edu/hr/home/
forms/benefit-forms, at the time
your coverage begins. You must
complete, sign, and return the form
to the Benefits Section of Human
Resources for it to become effec-
tive. You may change your benefi-
ciary at any time by completing,
signing, and returning a new form.
If no proper beneficiary designation
is in effect at the time of death,
the benefit goes to the surviving
spouse. In the absence of a surviv-
ing spouse, the benefit is paid to
the first surviving class of the fol-
lowing: children, parents, brothers/
sisters, and estate.
Events Affecting Your Coverage
If You Become Totally Disabled
Once you begin to receive disability
benefits from the University’s Long-
Term Disability Plan, the amount
of life insurance coverage available
is equal to your basic insurance in
effect on the date you stop working
because of your total disability. This
coverage continues at no cost to
you while you are receiving benefit
payments under the Long-Term
Disability Plan.
For full details, contact the Benefits
Section of Human Resources.
If You Continue to Work Beyond
Age 65
If you continue to work beyond age
65, your basic life insurance will be
reduced to a percentage of the cov-
erage in force just prior to your 65th
birthday.
The amount of your insurance
will be rounded to the next higher
$1,000 and reduced to the percent-
age noted on the next page.
57
Survivor Insurance
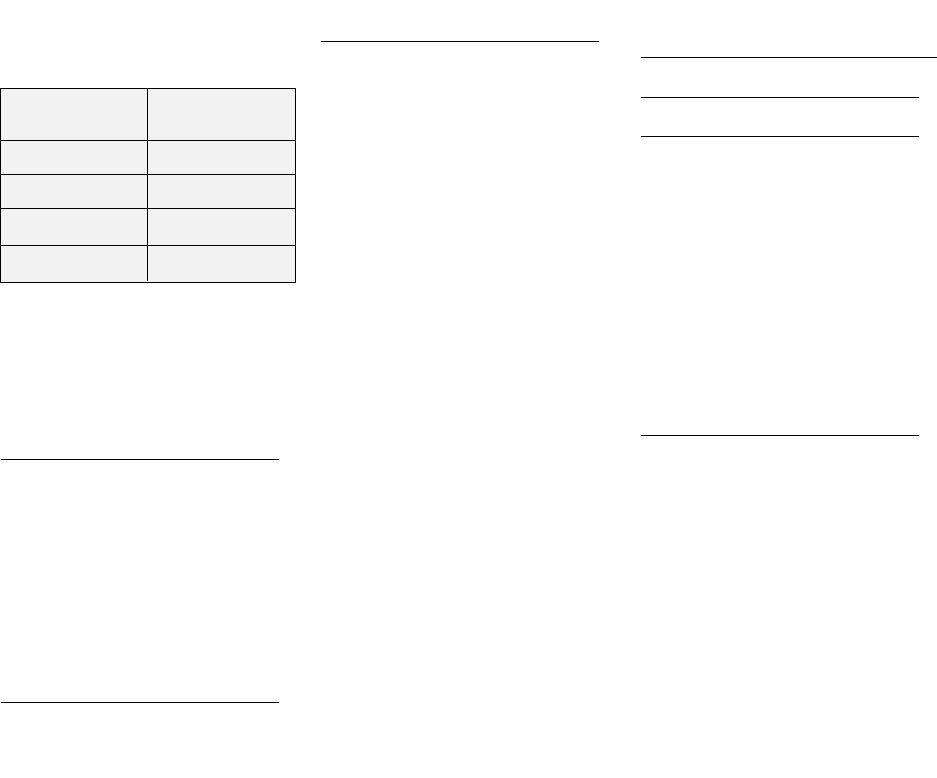
58
This reduction in your coverage
will be made according to the
following schedule:
If you enter the plan after age 65,
your basic life insurance will be
limited to a percentage (determined
according to the schedule above) of
your base salary in effect upon hire.
Termination or Conversion of
Coverage
Your basic life coverage under this
plan will end on the last day of the
month in which you terminate your
employment with the University
or when your status as a regular
employee ends.
When your basic life coverage ends,
you may convert your coverage to
an individual whole life insurance
policy if you apply to the insur-
ance company. If the amount of
your basic life insurance is reduced
be cause of age, you may also con-
vert the lost coverage to an indi-
vidual whole life insurance policy
issued by the insurance company.
You must apply for conversion and
pay your first premium within 31
days after the reduction or termina-
tion of the coverage you wish to
convert. A physical examination
will not be required to convert your
coverage. Your insurance cover-
age will continue during the 31-day
conversion period should you die
during this period.
Group Supplemental Life
Insurance Plan
Eligibility and Coverage
Eligibility for You
If you are classified by the
University as a regular employee,
work a full-time schedule, and
have an appointment of nine
months’ or more duration, you and
your eligible family members are
eligible to participate in the Group
Sup plemental Life Insurance Plan on
your first day of active employment.
Coverage for You
You have the option of purchasing
your own Group Supplemental Life
Insurance coverage for you equal to
one, two, three, four, or five times
the amount of your base annual
salary. If that amount is not
already an even multiple of
$10,000, it is rounded to the next
higher $10,000 up to $2,500,000.
For example:
• If your annual base salary
is $22,000 and you elect Group
Supplemental Life Insurance
equal to one times your annual
base salary, you will have an
additional $30,000 of insurance
for a total amount of $52,000
including the $22,000 basic
insurance that the University
provides.
• If your annual base salary is
$22,000 and you elect Group
Supplemental Life Insurance
equal to two times your annual
base salary, you will have an
additional $50,000 of insurance
for a total amount of $72,000
including the basic insurance
that the University provides.
• If your annual base salary
is $22,000 and you elect Group
Supplemental Life Insurance
How to Obtain Benefits
In the event of your death, your
beneficiary should contact Human
Resources as soon as possible.
The University will then provide
claim forms to your beneficiary and
assist in submitting the forms to the
insurance carrier.
Appealing a Denial
The insurance company is solely
responsible for determining what
constitutes a covered claim under
this plan.
If your beneficiary applies for ben-
efits from this plan and either part or
all of the claim is denied, he or she
has the right to appeal the denial.
Additional information about how to
appeal a denial of benefits is included
in the “Administrative Infor m ation”
section of this handbook.
Percent of
Attained Age Original Benefit
65 65%
70 45%
75 30%
80 and older 20%

equal to three times your annual
base salary, you will have an
additional $70,000 of insurance
for a total amount of $92,000
including the basic insurance
that the University provides.
Coverage for Your Spouse
You may also elect to cover your
spouse individually for an amount in
even multiples of $10,000 but only if
you choose to enroll for supplemental
coverage for yourself. The maximum
coverage amount you may elect
for your spouse is three times your
annual base salary (rounded up to
the next higher multiple of $10,000)
or $100,000, whichever is less.
In the event of divorce, your former
spouse will no longer be covered by
the spousal coverage.
Dependents’ Eligibility
Your child(ren) must be at least
15 days old and less than 19 years
old. Dependent child(ren) must be
unmarried to be considered eligible.
You may enroll your children in
Group Supplemental Life Insurance
coverage if you elect supplemental
coverage for yourself.
Coverage for Your Dependents
Your dependents are eligible for
coverage amounts of $5,000 or
$10,000 of insurance for each child.
Enrolling in Group
Supplemental Life Insurance
Enrolling Yourself in Group
Supplemental Life Insurance
You may enroll in Group
Supplemental Life Insurance cover-
age for yourself for up to $500,000
without evidence of insurability, if
you return a completed and signed
enrollment form to the Benefits
Section of Human Resources within
30 days after your benefits orien-
tation, assuming you commence
active employment as required by
the supplemental life insurance
coverage. In this case, your Group
Supplemental Life Insurance cover-
age becomes effective on the date
you enroll. Any insurance for which
evidence is required will not become
effective until the insurance com-
pany approves the evidence and
all other policy requirements (e.g.,
actively-at-work requirements) are
also satisfied.
If you do not elect Group
Supplemental Life Insurance cover-
age within 30 days after your orien-
tation or you enroll for coverage that
exceeds $500,000, the insurance
company will require you to provide
evidence of insurability. Any insur-
ance for which evidence is required
will not become effective until the
insurance company approves the
evidence.
If you are absent from active
em ploy ment and not performing
your regular duties on the day your
Group Supple mental Life Insurance
coverage would normally begin, you
will not become covered until the
day you return to active work.
If your annual base salary changes,
the amount of Group Supplemental
Life Insurance you have elected will
automatically change to one, two,
three, four, or five times your new
base annual salary. This change
will be effective on the first of the
month on or following the date the
change in your base salary becomes
effective.
If your salary decreases, your Group
Supple mental Life Insurance cover-
age remains the same.
If you are not at work on the day a
change in your Group Supplemental
Life Insurance coverage would nor-
mally become effective, the change
will not become effective until the
day you return to work.
Enrolling Your Spouse in Group
Supplemental Life Insurance
You may enroll your spouse in
Group Supplemental Life Insurance
coverage if you elect supplemental
coverage for yourself. Coverage
is available for your spouse from
$10,000 to $100,000 (not to
exceed three times your base sal-
ary rounded up to the next higher
multiple of $10,000). If you return
a properly completed and signed
enrollment form to the Benefits
Section of Human Resources within
30 days of your benefits orienta-
tion, you may enroll your spouse for
an amount up to $20,000 without
providing evidence of insurability.
In order for dependents (spouse or
child) to be eligible for coverage,
they cannot be hospital or home
confined, and must be able to carry
out their normal activities of daily
living.
The eligibility date for your spouse
is your eligibility date, or the date of
your marriage if later than your eligi-
bility date. If you do not elect Group
Supplemental Life Insurance cover-
age for your spouse within 30 days
after your spouse’s eligibility date
or enroll for coverage that exceeds
$20,000, the insurance company
will require you to provide evidence
of insurability. Any insurance for
which evidence is required will not
become effective until the insurance
company approves the evidence.
Enrolling Your Child for Group
Supplemental Life Insurance
You may enroll your child for Group
Supplemental Life Insurance cover-
age only if you choose to enroll your-
self. Coverage is available for each
child for either $5,000 or $10,000.
You must return your enrollment
form to the Benefits Section of
Human Resources within 30 days of
the child’s eligibility date. In order for
59

dependents (spouse or child) to be
eligible for coverage, they cannot be
hospital or home confined, and must
be able to carry out their normal
activities of daily living.
The eligibility date for your child
is your eligibility date, or any later
date when you first have or adopt
a child. If you do not elect Group
Supplemental Life Insurance for
your child within 30 days of the
child’s eligibility date, the insurance
company will require you to provide
evidence of insur ability for the child.
Any insurance for which evidence
is required will not become effec-
tive until the insurance company
approves the evidence.
To elect Group Supplemental Life
Insurance coverage you must com-
plete an enrollment form, available
from the Benefits Section of Human
Resources or from the website at
www.bu.edu/hr/home/forms/
benefit-forms. This form authorizes
the University to deduct the cost
of the Group Sup plemental Life
Insurance coverage that you desire
from your paychecks. The employee
is automatically the beneficiary of
spouse or dependent life insurance.
Cost
You pay for Group Supplemental
Life Insur ance, if you choose it. The
cost to you depends on your age and
the amount of Group Supplemental
Life Insurance you desire.
The cost of Group Supplemental Life
Insur ance will increase with your age
or with an increase in the amount
of coverage you have. An increase
in cost resulting from a change in
your age will become effective on
the first of the month in which you
have a birthday when your age
bracket changes. An increase in the
amount of coverage resulting from an
increase in your base pay will become
effective on the first of the month
on or following the date the change
becomes effective. You pay for your
portion of the premiums for your
Group Supplemental Life Insurance
with after-tax dollars.
Changing or Stopping Your
Supplemental Life Insurance
Because your premiums for Group
Supplemental Life Insurance are
after-tax contributions, there are
no tax law restrictions as to when
you can change your amount of
coverage, stop your coverage, or
begin your coverage. The insur-
ance company may require you to
provide evidence of insurability if
you increase your coverage or begin
coverage after your initial enroll-
ment period of the 30 days follow-
ing your benefits orientation.
Special Tax Considerations
Under current tax laws, the value of
your spouse’s life insurance cover-
age is subject to federal income,
Massa chusetts state income, and
Social Security taxes. These tax-
able amounts are called “imputed
income.” Imputed income for your
spouse’s life insurance benefit will
be reported as income on each
paycheck, and will be included
in the taxable earnings shown
on your W-2 Form. Coverage for
your spouse is subject to imputed
income for tax purposes.
Events Affecting Your Coverage
If You Become Totally Disabled
Once you begin to receive disability
benefits from the University’s Long-
Term Disability Plan, the amount
of life insurance coverage avail-
able is equal to your supplemental
insurance in effect on the date you
stop working because of your total
disability. This coverage continues
at no cost to you while you are
receiving benefit payments under
the Long-Term Disability Plan. For
full details, contact the Benefits
Section of Human Resources.
If You Continue to Work Beyond
Age 65
If you continue to work beyond
age 65, your Group Supplemental
Life Insurance will be reduced to
a percentage of the coverage in
force just prior to your 65th birth-
day. The amount of your insur-
ance will be rounded to the next
higher $10,000 and reduced by
the percentage noted below. This
reduction in your coverage will be
made according to the following
schedule:
Percent of Original
Attained Age Benefit
65 65%
70 45%
75 30%
80 and older 20%
If you enter the plan after age 65,
your Group Supplemental Life
Insurance will be limited, according
to the schedule, to a percentage of
the coverage you would have been
eligible for before age 65.
If You Retire
When you retire, your Group
Supplemental Life Insurance, and/
or any spouse or child Group
Supplemental Life Insurance you had
elected, will end on the last day of
the month of your retirement.
How to Obtain Benefits
In the event of your death, your
beneficiary should contact Human
Resources as soon as possible.
Your beneficiary for the Group
Supplemental Life Insurance Plan is
the same beneficiary as the one you
designate for the basic life insurance
60
coverage unless you indicate other-
wise. Once notified of your death, the
University will provide claim forms
to your beneficiary and assist in sub-
mitting them to the insurance car-
rier. You are the beneficiary of your
spouse or child coverage. You should
contact Human Resources should
your spouse or child die.
Appealing a Denial
The insurance company is solely
responsible for determining what
constitutes a covered claim under
this plan.
If your beneficiary applies for bene-
fits from this plan and either part or
all of the claim is denied, he or she
has the right to appeal the denial.
Additional information about how to
appeal a denial of benefits is included
in the “Administrative Information”
section of this handbook.
Termination or Portability
of Coverage
All Group Supplemental Life
Insurance coverage under this plan
will end on the last day of the month
in which you terminate your employ-
ment with the University or when
your status as a regular employee
ends. Group Supplemental Life
Insurance for your spouse and/
or child will also end if you die or
receive disability benefits from the
University’s Long-Term Disability
Plan.
The Group Supplemental Life
Insurance in effect for you and your
dependents at the time that your
group coverage ends is portable.
The amount is limited to:
• The lesser of $500,000 for
you or the amount of Group
Supplemental Life Insurance in
effect at the time group coverage
ends
• The lesser of $20,000 for your
spouse or the amount of Group
Supplemental Life Insurance in
effect at the time group coverage
ends
• The lesser of $5,000 for your
dependent child or the amount
of Group Supplemental Life
Insurance in effect at the time
group coverage ends
Administration of your portable
coverage is continued on a direct
bill basis through the life insur-
ance company.
You must apply for portability and
pay your first premium within 31
days after the termination of the
coverage. A physical examination
will not be required. Your insurance
coverage will continue during this
31-day period should you die during
this period.
Personal and Family
Accident Insurance Plan
Eligibility
If you are classified by the University
as a regular employee, work a full-
time schedule, and have an appoint-
ment of nine months’ or more
duration, you and your eligible
family members may participate in
the Personal and Family Accident
Insurance Plan. Also, if you are
insured under this plan and your
employment status changes to less
than full time, you may continue
your coverage under this plan.
For the purposes of the plan, your
eligible dependents are your spouse
and your unmarried dependent chil-
dren from birth through 19 years.
To elect Personal and Family
Accident Insurance coverage, you
must complete an enrollment form
available from the Benefits Section
of Human Resources. Coverage
is effective on the first day of the
month on or following the date you
enroll.
If you do not elect coverage under
this plan within 30 days of your ben-
efits orientation meeting, your next
opportunity to enroll will be during
the open enrollment period. You will
not be required to submit evidence
of good health if you delay your
enrollment.
Coverage
The plan covers you and your
enrolled dependents against any
accidental bodily injuries. For
University employees, this includes
accidents on or off the job world-
wide, 24 hours per day.
Coverage for You
The Personal and Family Accident
Insurance provides financial protec-
tion to you or your beneficiary if
you should die, or lose sight, a limb,
speech or hearing, or become para-
lyzed as the direct result of an acci-
dent. You may choose any amount
of coverage in multiples of $10,000
up to $350,000 (amounts over
$150,000 cannot exceed ten times
your annual base salary).
Coverage for Your Family
If you choose family coverage, the
plan will provide you with addi-
tional financial protection if your
spouse or an eligible dependent
dies or becomes dismembered as
the direct result of an accident. If
you choose family coverage, all
of your dependents are “covered
members” of the plan.
For every $10,000 of insurance
covering you, the coverage amounts
for your family members will be:
• $6,000 coverage for your
spouse, if you have no eligible
children; or
61
62
• $5,000 for your spouse and
$1,500 for each eligible child; or
• $2,000 for each eligible child, if
you have children but no spouse.
For example, suppose you chose
$50,000 of coverage for yourself.
If you are married with no children,
your spouse would be insured for
$30,000 of coverage. If you are mar-
ried with children, coverage would
be $25,000 for your spouse and
$7,500 for each child. If you have
children but no spouse, coverage for
each child would be $10,000.
Cost
The amount you pay depends on
the amount of coverage you want or
whether or not you want coverage
for your family.
How Insurance Premiums
Are Paid
You pay for the cost of the premi-
ums for both you and your family
with tax-free dollars. This is because
Boston University automatically
takes your payments from your pay-
check before federal income, state
income, and Social Security taxes
are taken out.
Automatic before-tax insurance pre-
mium payments are allowed under
the provisions of Section 125 of the
Internal Revenue Code. These provi-
sions are explained in more detail in
the “Flexible Benefits” section of this
handbook.
Changing or Stopping Coverage
Because you pay for your coverage
with before-tax dollars, the provisions
of Section 125 of the Internal Revenue
Code also govern how and when you
may make changes in your Personal
and Family Accident Insurance cov-
erage. Under the current provisions
of Section 125, you may change the
amount of your coverage or can-
cel your coverage once each year,
during the annual open enrollment
period. The only other time you may
make a change in your Personal and
Family Acci dent Insurance coverage
is if you have a Qualified Change in
your family or employment status.
Qualified Changes are explained in
the “Flexible Benefits” section of this
handbook.
Types of Benefits
Benefits, in the event of a covered
loss, are based on the coverage
amounts in effect for you and your
covered family members at the time
of the loss.
Accidental Death Benefits
The plan will pay the full coverage
amount to your beneficiary if you die
as a direct result of an accident. If a
covered member of your family dies
as the direct result of an accident,
you will receive the coverage amount
applicable to that dependent.
If you or any of your covered family
members die as the result of a cov-
ered accident that occurs while you
are either riding as a passenger or
driving a private passenger car while
wearing a seat belt, the plan will
pay a benefit equal to 10% of your
coverage amount or $25,000
(which ever is less). This benefit will
be paid in addition to any other acci-
dental death benefits.
Unless you designate otherwise,
the beneficiary for the Personal
and Family Accident Plan will be
the same as the one you designate
for the Basic Life Insurance Plan.
Beneficiary designations may be
changed at any time by completing
a new form.
If you elect family coverage and you
die as a result of an accident, the
following special provisions apply:
• Extensions of Family Coverage
Coverage for your surviving fam-
ily members will continue, at no
cost to them, for 90 days from
the date of your last premium
payment.
• Education Benefit The plan will
pay, in addition to all other
benefits, 2% of your coverage
amount on behalf of any depen-
dent child who at the time of
your accident was enrolled as a
full-time student in a college or
university. The education benefit
will also be paid to a dependent
child who at the time of your
accident is in the twelfth grade,
if he/she enrolls as a full-time
student in a college or university
within 365 days of the accident.
The education benefit is paid
annually, for a maximum of four
consecutive payments, as long
as the dependent child remains
in college.
If you have no dependent chil-
dren who qualify for the educa-
tion benefit, the plan will pay an
additional benefit of 2% of the
full coverage amount to your
beneficiary.
• Day Care Benefit The plan will
pay, in addition to all other
benefits, the lesser of $3,000
or 3% of your or your spouse’s
coverage amount on behalf of
each insured dependent child
under age seven who at the time
of your accident was attend-
ing a day care center or would
be attending a day care center
within one year. The Day Care
benefit is paid annually, for a
maximum of four consecutive
payments, as long as the depen-
dent child remains enrolled in a
day care center and is under age
seven. If you have no dependent
children who qualify for the Day
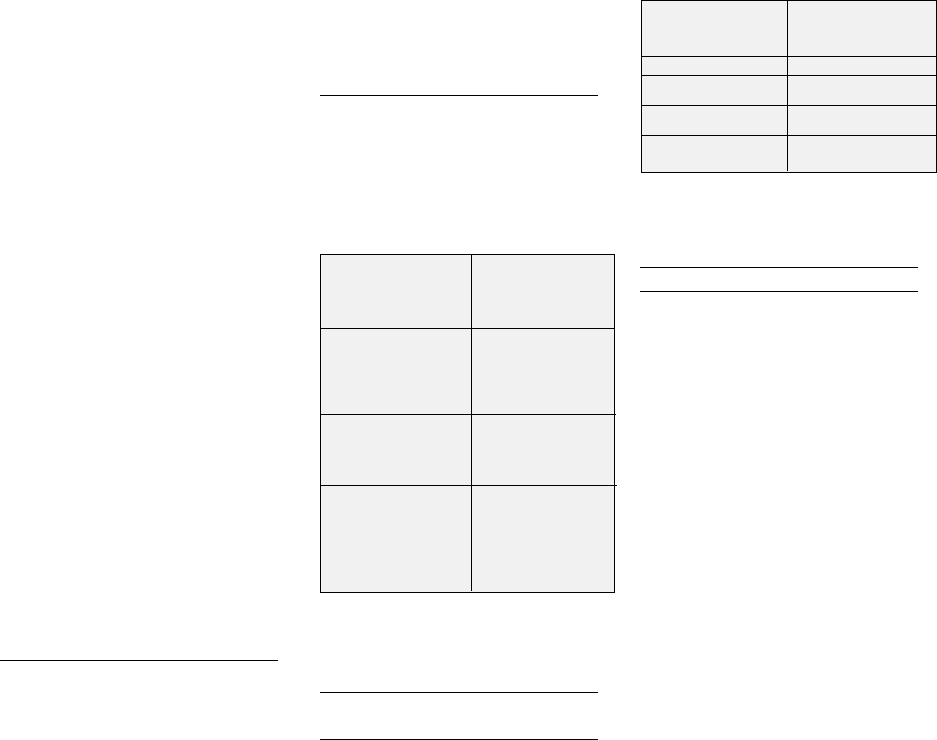
Care benefit, the plan will pay
an additional benefit of 3% of
the full coverage amount up to
$3,000 to your beneficiary.
If you have coverage for yourself
and your family, and both you
and your spouse die within 365
days as a result of the same
accident or separate accidents
within 24 hours of each other,
the amount payable for loss of
the life of your spouse will be
increased to the same amount
payable for your death.
The accidental death benefit is
normally paid in a lump sum of
cash. However, you or your ben-
eficiary may choose to have all
or part of your benefit from the
plan paid in a fixed number of
monthly installments, rather than
in a lump sum.
Accidental Dismemberment
Benefits
If you or a covered member of your
family should become seriously
injured in an accident, the plan will
pay to the injured person:
• 100% of the coverage amount
for the loss of both feet, hands,
the sight of both eyes, speech
and hearing, or any combination
of two of the following: a hand, a
foot, or the sight of one eye.
• 50% of the coverage amount for
the loss of one foot, one hand,
sight of one eye, speech, or
hearing.
• 25% of the coverage amount for
the loss of a thumb and an index
finger on the same hand.
Loss means complete and irrecov-
erable loss. The plan will pay for
the above losses only if they occur
within one year after the date of the
accident and as a direct result of
that accident.
Accidental dismemberment benefits
will be paid in a lump sum of cash.
Loss of Use Benefit
The plan will pay you a loss of use
benefit if you are determined to
be paralyzed within 365 days of
an accident. Benefits will be paid
according to the following schedule:
*For plan purposes, “paralysis” means
complete and irreversible loss of use of a
limb.
If You Continue to Work
Beyond Age 70
If you continue to work beyond age
70, your coverage will be reduced
to a percentage of the coverage in
force just prior to your 70th birth-
day. This reduction in your coverage
will be made according to the fol-
lowing schedule:
If you enter the plan after age
70, your coverage will be limited,
according to the schedule, to a
percentage of the coverage you
would have been eligible for before
age 70. The coverage for a spouse
under age 70, and any dependent
children, will be based on a percent-
age of your coverage prior to age
70 (see the “Coverage for Your
Family” section for examples).
After you reach age 70, the cost of
premiums for coverage for you and
your family will be based on the cost
of your coverage amount prior to
age 70.
Exclusions
In plans of this type, there are
some losses which are not covered.
Excluded losses are those caused by:
• Declared or undeclared war or
an act of either
• Services in the armed forces of
any country
• Suicide or a suicide attempt
while sane or self-destruction or
an attempt to self-destroy while
insane
• The voluntary use of any drug or
controlled substance unless used
as prescribed by a physician
• Sickness, disease, or any bac-
terial infection other than one
related to a cut or wound result-
ing from an accident covered by
this plan
Under this plan, coverage for air
travel is provided while riding as
a passenger, and not as a pilot or
crew member, in any aircraft being
used for the transportation of pas-
sengers except one owned, oper-
ated, or leased by or on behalf of
Boston University. For a complete
explan ation of these exclusions,
contact the Benefits Section of
Human Resources.
Finally, the plan does not provide
coverage for anyone serving full
time in the armed forces of any
country for more than two months.
Pre miums paid for coverage during
such periods of military service will
be refunded.
63
Percent of
Attained Age Original Benefit
70 through 74 82.5%
75 through 79 57.5%
80 through 84 37.5%
85 and older 20.0%
Percent of
Full Coverage
Type Amount
Quadriplegia
(total paralysis* 100%
of both upper
and lower limbs)
Paraplegia (total
paralysis* of both 75%
lower limbs)
Hemiplegia (total
paralysis* of the
upper and lower 50%
limbs on one side
of the body)
64
How to Obtain Benefits
To claim benefits from the Personal
and Family Accident Insurance Plan,
you or your beneficiary should con-
tact the Benefits Section of Human
Resources as soon as possible after
the loss. The Benefits Section of
Human Resources will help you
complete the claims forms and
will forward them to the insurance
company. To process an accidental
dismem berment or paralysis claim,
the insurance company may require
you or your family member(s) to
be examined by a physician at the
company’s expense.
Appealing a Denial
The insurance company is responsi-
ble for determining when benefits will
be paid under this plan. If the insur-
ance company denies your claim for
benefits, consult the Benefits Section
of Human Resources for information
on the procedure for appealing the
denial. Additional information about
how to appeal a denial of benefits
is included in the “Administrative
Information” section of this
handbook.
Leaves of Absence or No-Pay
Status
If you leave active work for any
reason for a prolonged period of
time, you should always contact
the Benefits Section of Human
Resources to ask what effect your
absence may have on your partici-
pation in this plan.
• Leave of Absence with Pay If you
are granted a leave of absence
with pay, your coverage will con-
tinue, provided your usual payroll
deductions continue. If you wish
to discontinue your participation,
you may do so by obtaining the
necessary forms from the Benefits
Section of Human Resources.
• Leave of Absence without Pay
or No-Pay Status If you are
granted a leave of absence with-
out pay or are on no-pay status,
you may continue your cover-
age during your leave provided
you pay the cost of continuing
this coverage. If you choose to
continue coverage, you should
contact the Benefits Section
of Human Resources before
you begin your leave, in order
to make the necessary billing
arrangements. This coverage will
automatically be canceled for
non-payment of bills.
If you choose not to continue
this insurance, coverage will
automatically end on the last day
of the month in which you are
granted such leave. To reinstate
coverage when you return from
your leave, you must re-enroll,
provided you are still eligible.
To do so, contact the Benefits
Section of Human Resources.
Termination and Conversion of
Coverage
Your insurance coverage under
the Personal and Family Accident
Plan will end 31 days after you ter-
minate your employment with the
University or your status as a regu-
lar employee ends.
When your coverage under the
plan ends, you may convert your
coverage for yourself and your cov-
ered dependents to an individual
policy at regular individual policy
rates. You will not have to submit
evidence of good health to convert
your coverage. However, you must
apply, in writing, to the insurance
company within 31 days of the date
your coverage under the Personal
and Family Accident Insurance
Plan ends.
Travel Accident
Insurance Plan
Eligibility
If you are classified by the
University as a regular employee,
work a full-time schedule, and have
an appointment of nine months’
or more duration, you will auto-
matically become a member of
the Travel Accident Insurance Plan.
Your coverage becomes effective on
your first day of active employment.
Coverage
The Travel Accident Insurance Plan
provides financial protection, while
you are traveling on authorized
University business, against death,
paralysis, or loss of sight, speech,
hearing, or limbs resulting directly
from accidental injuries.
How the Plan Works
This plan protects you while travel-
ing on authorized University busi-
ness. In general, your destination
must be away from the campus or
away from your place of employ-
ment, if it is off campus.
You are covered:
• The minute you leave your
home, place of employment, or
other location, whichever occurs
last, for travel on authorized
University business
• When traveling between the
Medical and Charles River
Campuses, if such travel is on
authorized University business
You are not covered:
• For regular commuting to and
from work
• For travel between points on
cam pus (except as described
above) including the athletic
fields
Your coverage ends:
• When you return to your home,
place of employment, or other
location, whichever occurs first
Cost
Boston University pays the entire
cost of your coverage under this
plan.
Types of Benefits
Benefit Amount
Benefits under this plan depend on
your Benefit Amount. Your Benefit
Amount equals five times your
annual base salary up to a maxi-
mum of $1 million of coverage.
Accidental Death Benefit
The plan will pay your Benefit
Amount to your chosen beneficiary
in the event of your accidental
death while traveling on authorized
University business.
When you begin your employ-
ment with the University, you will
be asked to name your beneficiary
on a form provided by the Benefits
Section of Human Resources or
from the website at www.bu.edu/
hr/home/forms/benefit-forms. You
may change your beneficiary at any
time by completing a new form.
Accidental death benefits are nor-
mally paid in a lump sum of cash.
How ever, your beneficiary may
choose to have all or part of your
death benefit de posited to an indi-
vidualized account established by
the insurance carrier on which your
beneficiary may write checks to
withdraw funds as needed.
Accidental Dismemberment
Benefit
If you become seriously injured in
an accident while traveling on
authorized University business, the
plan will pay you:
• 100% of your Benefit Amount for
the loss of both feet, both hands,
the sight of both eyes, both
speech and hearing, or any com-
bination of two of the following:
a hand, a foot, or the sight of
an eye
• 50% of your Benefit Amount for
the loss of one foot, one hand,
the sight of an eye, speech or
hearing
• 25% of your Benefit Amount for
the loss of a thumb and index
finger on the same hand
Loss means complete and irrecover-
able loss.
The plan will pay benefits for
the above losses only if they are
incurred as a direct result of, and
within one year after the date of,
an accident which occurred while
traveling on authorized University
business.
Accidental dismemberment benefits
are normally paid in a lump sum
of cash. However, you may choose to
have all or part of your benefit depos-
ited to an individualized account
established by the insurance carrier
which you may write checks on to
withdraw your funds as needed.
Common Accident Coverage
Limitation
The limit of insurance coverage pay-
able as a result of any one accident
involving any number of University
employees is $3 million. If the total
benefits payable for one accident
exceeds those limits, the amount
payable to each insured person is
reduced proportionately.
Exclusions
As in all plans of this type, there are
some losses that are not covered.
Excluded losses are those caused by:
• Suicide or a suicide attempt
while sane, or self-destruction or
an attempt to self-destroy while
insane
• Declared or undeclared war or
an act of either, within the United
States, Canada, and your country
of permanent residence
• Active service in the armed
forces of any country
• Sickness, disease, or any bacte-
rial infection other than one
related to a cut or wound result-
ing from an accident covered by
this plan
Under this plan, coverage for air
travel is provided while riding as a
passenger, and not as a pilot or
crew member, in any aircraft being
used for the transportation of pas-
sengers except one owned, oper-
ated, or leased by or on behalf of
Boston University. For a complete
explanation of these exclusions,
contact the carrier or the Benefits
Section of Human Resources.
How to Obtain Benefits
To claim benefits under the Travel
Accident Insurance Plan, you or
your beneficiary should contact
the Benefits Section of Human
Resources as soon as possible after
the loss. The Benefits Section will
provide assistance in completing the
claim forms and will forward them
to the insurance carrier. To process
an accidental dismemberment or
disability benefit claim, the insur-
ance company may require you to
be examined by a physician, at no
expense to you.
65

66
Appealing a Denial
The insurance company is respons-
ible for determining whether you
have suf fered a covered loss under
circumstances that entitle you or
your beneficiary to receive benefits
under the plan. If the insurance
company denies your claim for ben-
efits, consult the Benefits Section
of Human Resources for informa-
tion on how to appeal the denial.
Additional information about how to
appeal a denial of benefits is included
in the “Admin istrative Information”
section of this handbook.
Leaves of Absence
If you leave active work for any
reason for a prolonged period of
time, you should always contact
the Benefits Section of Human
Resources to ask how your absence
may affect your participation in
this plan.
Termination of Coverage
Your insurance coverage under this
plan will end on the day you termi-
nate your employment with the
University or your status as a regu-
lar employee ends.
Supplemental Death
Benefit Plan
Eligibility
If you are classified by the
University as a regular employee,
work a full-time schedule, and have
an appointment of nine months’
or more duration, you automati-
cally become a member of the
Supplemental Death Benefit Plan
on the day that you complete five
years of continuous full-time ser-
vice. If you are not actively at work
performing your normal duties on
the day you would normally become
eligible, you will not become a
member of the plan until the day
you return to active work.
Cost
The University provides and pays
the entire cost of the Supplemental
Death Benefit Plan.
You are not required to contribute
anything for this coverage.
Plan Benefits
The Supplemental Death Benefit
Plan will automatically provide your
beneficiary with a lump sum pay-
ment equal to one-twelfth of your
annual base salary in effect on the
date of your death. The benefi-
ciary of the Supplemental Death
Benefit Plan is the beneficiary you
have designated for the Basic Life
Insurance Plan.
How to Obtain Benefits
In the event of your death, your ben-
eficiary should contact the Bene fits
Section of Human Resources as soon
as possible. The Benefits Section will
assist in submitting the claim.
Appealing a Denial
If a claim for benefits under this
plan is denied, your beneficiary
has the right to appeal that deci-
sion to the Plan Administrator or
to the Univer sity’s Committee on
Employee Benefits.
Additional information about how to
appeal a denial of benefits is included
in the “Administrative Information”
section in this handbook.
Tax Considerations
Under current laws, the Supple-
mental Death Benefit payment
is taxable as income in the year
received by the beneficiary.
Leaves of Absence
If you leave active work for
any reason for a period of time
beyond one pay period, you should
contact the Benefits Section of
Human Resources to ask how your
absence may affect your participa-
tion in this plan.
When Plan Membership Ends
Your membership in this plan will
end when you terminate your
employment with the University
or when your status as a regular
employee ends.

Overview
Retirement Plan
68
R
egardless of your age, the time for thinking about retirement is now.
With careful planning, you can help make your retirement years a
more comfortable and secure time of life for you and your family.
Once you have completed the necessary service requirement, the Boston
University Retirement Plan provides you with an opportunity to set aside
money for your retirement. If you make the required participant contribu-
tions to the plan, the University more than matches that contribution.
Both your contributions and the University’s may be invested in any of the
following investment vehicles: guaranteed and variable annuity accounts,
as well as mutual funds available through the Teachers Insurance and
Annuity Association (TIAA), the College Retirement Equities Fund (CREF),
or mutual funds administered by Fidelity Investments.
You have the choice to pay no income tax on the money you contribute to
the plan until withdrawal. The University’s contributions are not taxable
to you when made. In addition, investment earnings accumulate tax-
free until withdrawal.
Alternatively, your contributions to the plan may be made as Roth con-
tributions on an after-tax basis to Fidelity Investments only. If you make
Roth contributions your investment earnings will accumulate tax-free
and will be considered tax-free at the time of withdrawal as long as your
withdrawal is qualified. The University contributions will be considered
taxable income to you at the time of withdrawal regardless of whether
you make before-tax or Roth contributions.
Your Retirement Plan income, together with your Social Security ben-
efits and personal assets, are intended to give you the financial security
you will need during your retirement years. You may also increase
your retirement savings by making contributions to the Supplemental
Retirement and Savings Plan, which is described in the next section of
this handbook.
69
About the Retirement Plan
Once you have satisfied the service
requirement, the Boston University
Retirement Plan provides you with
an opportunity to put aside money
for your retirement. At that time,
you have a choice of contributing
to the plan in one of the following
ways:
Before-Tax Contributions—You
pay no federal or state income
tax on the before-tax money you
put into the plan or the accumu-
lated investment earnings until
you receive it.
Roth Contributions—You pay fed-
eral and state income tax on the
after-tax money you put into the
plan. The investment earnings
accumulate tax-free and are paid
to you tax-free at the time you
receive it as long as the with-
drawal is qualified.
University Contributions—You pay
no federal or state income tax on
the contributions the University
puts into the plan on your behalf
or the accumulated investment
earnings until you receive it.
The tax deferral advantage can,
in effect, increase the amount
you can afford to save now.
To find out more about the Retire-
ment Plan, read this section care-
fully. Then, to begin saving for your
future, contact the Benefits Section
of Human Resources.
Eligibility
If you are an employee of the
University, other than a student,
have a normal work schedule of at
least 50% of a full-time schedule,
and have an appointment of nine
months’ or more duration, you may
participate in the Boston University
Retirement Plan.
As an eligible employee, you can
participate in the plan beginning on
the first day of the month in which
you complete two years of service
with the University. A year of ser-
vice is a 12-month period in which
you complete at least 1,000 hours
of service.
Any prior eligible service with
Boston University will be applied
toward your two-year waiting
period. These provisions apply only
to the eligibility waiting period.
Enrollment
If you would like to enroll in the
Retirement Plan, please log on to
www.bu.edu/buworkscentral and
go to the Employee Self-Service sec-
tion. Under Benefits and Pay click
on “Retirement Plan Enrollment”
and follow the instructions provided
therein.
When you log on, you will be
able to:
• Enroll for the first time
• Open an account with an invest-
ment fund sponsor if you do not
yet have an account with that
sponsor and you want to move
some of your plan money to it
• Change your contribution
amounts
Alternatively, if you wish to enroll
in writing, you may obtain the
forms by logging on to www.
bu.edu/hr/home/forms. Upon
request, forms will be mailed
directly to you by the Benefits
Section of Human Resources.
Completed forms must be returned
to Human Resources at 25 Buick
Street. You need use only one
method of enrollment—online or
paper—not both. Paper enrollments
will be processed as soon as pos-
sible after receipt.
If you previously participated in
another 403(b) or other type of
tax-deferred plan (such as a 401(k)
plan) with a previous employer,
you may be able to roll over your
account balances from that plan to
the Boston Uni versity Supplemental
Retirement and Savings Plan, pro-
vided you meet the plan’s rules and
the rules of the investment fund
sponsors. The Benefits Section of
Human Resources can provide you
with further information on rollovers.
Changing or Stopping Your
Elections
You can make changes in your
elections at any time online or by
filling out a form available from
the Benefits Section of Human
Resources. Your change will be
reflected in the next paycheck
you receive following the date of
your online change or the date the
Benefits Section of Human Resources
receives your election.
You may stop or resume contribu-
tions, or you may change from
making before-tax contributions to
making Roth contributions, or vice
versa. You cannot take back any
contributions or change their tax
status once they are made.
Your ability to change your invest-
ment choices, or to transfer invest-
ments from one fund to another,
depends on your choice of invest-
ments. Some funds (such as TIAA
Retirement Plan

traditional annuities) have limita-
tions on transfers out; other funds
may restrict investments in and
out within a short time to prevent
market timing or other manipulative
practices. You should review the
restrictions in each fund carefully
before making your investment
decision.
How Much You and the
University Contribute
Under the formula effective January
1, 1987, you contribute 3% of your
base salary each payroll period. The
University contributes an amount
each payroll period equal to a per-
centage of your base salary; the
percentage varies according to your
age, as follows:
For Retirement Plan purposes, you
should be familiar with the following
terms:
Base Salary This amount is your
base pay from the University includ-
ing, if applicable, any stipend or
other payments coded for payroll
purposes as benefits-based over-
base payments, excluding over-
time, one-time payments, other
overbase payments, commissions
and bonuses, or the value of any
employee benefits. Base salary
amounts contributed under a salary
reduction agreement to a 403(b)
plan or to the Flexible Benefits
Program or for pre-tax transporta-
tion benefits will be included in base
salary for Retirement Plan purposes.
The tax laws have a maximum limit
on the annual amount of compen-
sation that a retirement plan may
take into account for contribution
purposes. This limit for 2013 is
$255,000. Each year thereafter,
this limit is subject to indexing in
$5,000 increments. That cost of
living increment is adjusted up
with the cost of living increase, but
rounded down to the next lower
$5,000 increment.
Integration Level This amount is
$35,800 for 2013. It is adjusted
each calendar year based on the
Wage Base Increase calculated for
purposes of the Social Security law,
or the increase in the Consumer
Price Index (Wages), whichever is
smaller.
An adjustment in the University’s
contribution percentage based on
a change in your age is made at the
beginning of the month in which
you attain the new age.
The Boston University
Retirement Plan 1965
You may file an election to switch
to the new contribution formula
effective with the beginning of any
calendar year. Once you do so, you
may not go back to the old (1965)
contribution formula again.
Whether you are better off remain-
ing under the 1965 formula or
switching to the new formula will
depend on your personal circum-
stances. You should assess your
situation each year prior to January 1,
when you can switch to the new plan
formula. To help you with your deci-
sion, the Benefits Section of Human
Resources can provide you with the
Integration Level for the coming cal-
endar year and can inform you what
the contribution rates would be for
the year under the 1965 formula or
the new formula based on your cur-
rent base salary.
If you participated in the Boston
University Retirement Plan 1965
and did not choose the new plan
formula, which was effective on
January 1, 1987, you will continue
to contribute each payroll period at
the rate of 3% of the first $7,800 of
your base salary each year and 5%
of your base salary above $7,800.
The University will contribute as
follows:
Before-Tax Contributions
and After-Tax Roth 403(b)
Contributions
The Retirement Plan gives you a
choice as to whether you want
to make your contributions on a
before-tax or after-tax basis or a
combination of tax-deferred and
Roth after-tax.
• Before-Tax Contributions—You
will not have to pay any taxes
(except Social Security) on the
portion of pay you put into the
plan. According to federal law,
When Your The University
Age Is Contributes
Under 45 5% of the first $7,800 of
base salary PLUS
7% of your base salary
above $7,800
45 through 49 7% of the first $7,800
of base salary PLUS
10% of your base salary
above $7,800
50 and above 7.3% of the first $7,800
of base salary PLUS
13% of your base salary
above $7,800
70
When Your The University
Age Is Contributes
Under 45 5% of your base salary
up to the Integration
Level PLUS 10% of your
base salary above
the Integration Level
45 through 49 7% of your base salary
up to the Integration
Level PLUS 12% of your
base salary above
the Integration Level
50 and above 9% of your base salary
up to the Integration
Level PLUS 14% of your
base salary above the
Integration Level

such before-tax contributions are
treated as University contribu-
tions. Therefore, your contribu-
tions are not considered taxable
income, and you are not required
to pay income taxes on that
money, or investment earnings,
until you receive payment of your
accounts. This will normally be
after your retirement, when your
taxable income and your tax rate
may be lower.
Your before-tax contributions, as
well as after-tax Roth contribu-
tions, are subject to applicable
Social Security tax withholdings.
• After-Tax Roth 403(b)
Contributions—
(Available Only with Fidelity
Investments)—Your contributions
will be made on an after-tax basis.
Earnings on your Roth 403(b)
account are tax-free when with-
drawn as long as the withdrawal
is qualified. A qualified with-
drawal is one that is taken (i) no
earlier than the fifth calendar year
after the year of your first Roth
contribution and (ii) after you
have attained age 59
1
⁄2, become
disabled, or die.
• After-Tax Contributions—
(Other than Roth)—Members who
were making after-tax contribu-
tions prior to January 1, 2009, and
members in non-U.S. locations
may continue to make after-tax
(non-Roth) contributions. The
earnings on this type of contribu-
tion are taxable when withdrawn.
Investment Choices
You choose how contributions to
your accounts from you and the
University will be invested from
among the following investment
fund sponsors. Boston University
assumes no responsibility for your
choice of investments. Since you
choose the investment options for
your account, you have the respon-
sibility for the financial results. The
plan is intended to be a participant-
directed plan as described in
Section 404(c) of the Employee
Retirement Income Security Act
of 1974 as amended (ERISA) and
Department of Labor regulations
governing section 404(c) plans.
This means that fiduciaries of the
plan are relieved of liability for
any losses that are the result of
investment instructions given by a
participant or beneficiary under the
participant-directed investment fea-
ture of the plan.
You should consult a professional
financial advisor for investment
advice and financial planning assis-
tance before choosing an investment
option. Further information may be
obtained directly from the invest-
ment fund sponsors. You should
read the prospectus or other infor-
mation describing an investment
fund carefully before investing.
Fidelity Investments
Fidelity Investments is a mutual fund
company that offers many funds
with a wide variety of investments:
short-term, bonds, and stocks. The
investment objectives and policies of
each fund, as well as the expenses
and fees for the fund, are described
in its prospectus, which you should
read. Investments for the Boston
University Retirement Plan are made
through the Fidelity Tax-Exempt
Services Company.
Teachers Insurance and Annuity
Association and College
Retirement Equities Fund
(TIAA-CREF)
TIAA-CREF is a financial services
company. TIAA-CREF offers
guaranteed and variable annuity
accounts, as well as mutual funds
covering a broad range of asset
classes.
In order to obtain a detailed
description of the funds offered by
Fidelity and TIAA-CREF you should
contact the Benefits Section of
Human Resources.
Investment Restrictions
Each investment fund sponsor
places certain restrictions on your
investments. For complete, current
details on restrictions, you should
refer to the printed materials avail-
able from each of the investment
fund sponsors. Following are expla-
nations of some of the important
restrictions.
The following rules apply to how
future contributions to the plan are
invested:
1. You may choose to invest your
own future before-tax contribu-
tions in any of the TIAA-CREF
funds or Fidelity funds, but you
cannot split your contributions
between the two. Similarly,
University contributions cannot
be split. This means that you
could put all of your own con-
tributions in TIAA-CREF and all
the University’s contributions in
Fidelity, or vice versa, but you
cannot otherwise split the contri-
butions between TIAA-CREF and
Fidelity.
2. If you choose to invest your
before-tax contributions and
University contributions in TIAA-
CREF funds, you can split contri-
butions between TIAA and CREF
in any combination you choose.
3. If you choose to invest in Fidelity
funds (Fidelity funds are available
for both pre-tax and Roth after-
tax contributions), you can split
contributions among its funds in
any combination you choose.
71
72
4. Subject to the restrictions on
Roth after-tax contributions, you
can change your choice of where
to invest future contributions as
often as once a month.
The following rules apply for moving
account balances from one invest-
ment sponsor to another:
1. For a TIAA Group Retirement
Annuity Account issued after
June 1, 2005:
While you are employed at the
University transfers can be
made out of the TIAA Traditional
Annuity Account into CREF or
Fidelity by use of a transfer pay-
out annuity but only by spread-
ing the amount transferred
out over a nine-year period. At
termination of service, transfers
may be made from the TIAA
Traditional Annuity Account to
CREF or Fidelity over a five-year
period, or, within the first 120
days following separation from
service, in a lump sum, which is
subject to a 2.5% surrender fee.
For a TIAA Retirement Annuity
Account issued prior to June 1,
2005:
Transfers can be made out of
the TIAA Traditional Annuity
Account into CREF or Fidelity by
use of a transfer payout annu-
ity but only by spreading the
amount transferred out over
a nine-year period.
2. Transfers out of CREF into TIAA
or Fidelity may be made in any
amount at any time.
3. Transfers out of Fidelity into TIAA
or CREF may be made in any
amount at any time, except that
TIAA and CREF cannot accept
Roth after-tax contributions.
4. Transfers among Fidelity funds
may be made at any time, but a
fee may be charged if more than
four transfers are made in a cal-
endar year.
Other restrictions or requirements
may apply. See the disclosure materi-
als for any fund you are considering.
Statements of Your Accounts
You will receive quarterly state-
ments by mail directly from
TIAA-CREF. Fidelity’s quarterly
statements are available online
at Fidelity NetBenefits.
Contribution Limitations
The tax laws limit the amount of
before-tax and after-tax Roth con-
tributions that you can make to this
plan each calendar year.
Under the current rules, these limits
will not affect your ability to make
the required employee 3% of base
salary contributions (or contributions
under the grandfathered 1965 plan if
you are still under that formula).
Internal Revenue Code Section
415 also places a limit on the total
amount which may be contrib-
uted by the University and by you
(before-tax, after-tax Roth, and any
other after-tax contributions) in a
calendar year. If the sum of your
contributions and the University’s
contributions exceed any of the
limits, certain IRS-mandated reduc-
tions apply.
Lastly, matching contributions by
the University are subject to the
requirements of Internal Revenue
Code Section 401(m). If these
requirements are not satisfied,
matching contributions for cer-
tain participants may have to be
reduced. If the 401(m) limitation
should affect you, any amounts that
would be reduced or returned on
your behalf will be returned to you
and will be mailed to you in the form
of a check by your investment fund
sponsor. This amount will be treated
as taxable income, and you will
receive a Form 1099 for the tax year
in which you receive the returned
contributions from your investment
fund sponsor for tax filing purposes.
Refer to “How Much You and the
University Contribute” for further
contribution limitations.
Note: Special rules and limits apply
if, during a calendar year, you also
participate in another plan main-
tained by a business you own or
control. For example, if you have
consulting or other self-employ-
ment income and participate in a
self-employed plan to which you
make contributions, the special
rules may affect you. If this situation
applies to you, consult a qualified
tax professional for advice.
The Benefits Section of Human
Resources will assist you in calcu-
lating the limits that apply to you.
In-Plan Roth Rollover
When taking an eligible distribu-
tion (as defined below), you may
elect to convert all or a portion
of your Plan Account (other than
your Roth Contribution Account)
to a Roth Contribution Account
as an In-Plan Roth Rollover. This
Rollover actually occurs within the
Plan. You do not receive a check
and then contribute it to the Plan.
An eligible distribution is (i) a
distribution to an active Member
on or after attaining age 65; (ii) a
distribution made upon termination
of employment, becoming disabled,
or retirement; (iii) a distribution
upon the Member’s death; or (iv)
any distribution that would other-
wise qualify as an eligible rollover
distribution.
A key benefit of a Roth is the poten-
tial for federally tax-free earnings

73
and withdrawals. Converting to a
Roth 403(b) can be beneficial if you
expect your tax rate to increase in
the future, because you pay taxes
on the money you convert now.
You are advised to consult a tax
advisor to better understand these
requirements. The full amount of
any conversions to a Roth 403(b)
processed in a calendar year will be
considered taxable income in that
calendar year.
Forms of Payment
Your plan benefits will normally
start when you retire or you may
also start your benefits once
you reach age 65 regardless of
whether you are retired or still
employed. However, if you wish,
you may postpone the start of
your benefits while you are still
working for the University.
You have some choices as to the
form of payment of your retirement
benefits. However, if you are mar-
ried, federal law provides that you
must receive your benefits in the
form of a 50% Joint and Survivor
Annuity, with your spouse as ben-
eficiary, unless your spouse agrees
in writing to your choice of another
form of payment. Your spouse’s
signature must be witnessed by a
plan representative or notarized by
a notary public.
Particularly if you have large plan
account balances (or other retire-
ment plan accumulations, includ-
ing other 403(b) arrangements,
employer-qualified plans, or IRAs),
your choice of a form of payment
may affect your tax and estate plan-
ning. Consult a qualified advisor if
you have any questions.
Descriptions of the forms of pay-
ment provided by each of the
investment sponsors follow.
Fidelity
Lump Sum You may elect to receive
a lump sum distribution from Fidelity
for the full value of your accounts at
the time of the payment.
Installment Withdrawal Program
As an alternative, you may elect to
maintain your account balances
with Fidelity and receive periodic
withdrawals from your account until
you have exhausted your account
balances. You may designate the
amount and the frequency of these
withdrawals (subject to certain min-
imums required by the tax law).
Rollover You may also elect to roll
over all or a portion of the account
balances in your Fidelity funds into
an individual retirement account
(IRA) or another plan you par-
ticipate in that accepts rollovers,
provided you meet certain tax law
requirements. If you wish, you may
use the proceeds of your account
to purchase an annuity through
TIAA-CREF or another insurance
company. You may wish to consult
with your financial advisor before
selecting this option.
TIAA Traditional Annuity
A lifetime annuity may be received
from your TIAA Traditional
Annuity Account. Lifetime annu-
ity income is the only payment
method that ensures you will
never outlive your retirement
income. It is also a permanent
arrangement. Once you begin
receiving payments, you may not
stop them. The actual amount of
income you receive at retirement
depends primarily on the amount
in your TIAA account, your age
when payments begin, and the
form of payment you choose (see
“Annuity Forms of Payment”).
For Group Retirement Annuity
(GRA) contracts issued after June 1,
2005, you may also receive a fixed
period annuity of five to thirty years
(subject to IRS restrictions). At the
end of the fixed period chosen, all
payments cease.
TIAA cash withdrawals can be
taken in ten substantially equal pay-
ments over a period of nine years.
Once the amount of your TIAA
annuity payment is determined, it
can be increased or decreased by
changes in dividends, but cannot fall
below the contractually guaranteed
level.
TIAA Real Estate Account and
CREF Forms of Payment
Lump Sum You may receive a
lump sum distribution from TIAA
Real Estate Account and CREF for
all or part of the full value of your
accounts at the time of payment.
Fixed Period Payments TIAA Real
Estate Account and CREF accu-
mulations may be taken over any
period between two and thirty
years, subject to IRS restrictions.
At the end of the selected period,
payments will end.
TIAA Real Estate Account and CREF
Annuity A lifetime annuity may
be received from your TIAA Real
Estate Account and CREF Account.
Lifetime annuity income is the only
payment method that ensures you
will never outlive your retirement
income. It is also a permanent
arrangement. Once you begin
receiving payments, you may not
stop them. The actual amount of
income you receive at retirement
depends primarily on the amount
in your account, your age when
payments begin, and the form of
payment you choose (see “Annuity
Forms of Payment”).
Annuity Forms of Payment (Applies
to TIAA-CREF Payments Only) The
following is a description of the

74
types of lifetime annuities TIAA-
CREF provides for moneys invested
with them. These annuity options
would also be available if you
transferred Fidelity funds to TIAA-
CREF at retirement. Just before you
are scheduled to start receiving
your income, you will be provided
detailed information by TIAA-CREF
to help you choose the option that
best meets your needs.
Subject to certain minimum dis-
tribution requirements, you also
can choose to receive part of your
TIAA or CREF accumulation under
one option and the balance under
another option. Of course, instead
of an annuity option, you may also
choose to take all or part of your
accounts in cash (subject to TIAA’s
rules); however, this will reduce
the amount of annuity income you
receive. You should note when
reviewing the different annuity
options that the size of the monthly
payments depends not only on your
age and account balances, but also
on the age of your spouse or other
beneficiary.
Single Life Annuity Pays you an
income for as long as you live. This
option provides a larger monthly
income for you than the other
options. However, all payments
will stop at your death.
Life Annuity with 10-, 15-, or 20-Year
Guaranteed Period Pays you an
income for as long as you live, with
installments guaranteed to continue
during the first 10, 15, or 20 years,
as you select, whether you live or
die. If you live beyond the guaran-
teed period, payments continue for
your lifetime. If you die during the
guaranteed period, payments will
continue to your beneficiary for the
balance of the guaranteed period.
Survivor Annuity Pays you an
income for life. If your spouse or
another second annuitant you des-
ignated lives longer than you, he or
she continues to receive an income
for life. The amount of the income
continuing to the survivor depends
on which option you choose from
the four options listed below. The
amount of the annuity payable to
you at the onset of each of these
options is different; the more you
choose to have paid to your survi-
vor, the smaller the income to you
during your lifetime.
Each of these survivor options is
available with a 10-, 15-, or 20-year
guaranteed period. This provides
that if both you and your spouse (or
another designated second annui-
tant) die during the first 10, 15, or 20
years (whichever you select), pay-
ments continue to another named
beneficiary for the balance of the
guaranteed period you selected.
1. Full Benefit to Survivor The full
amount of the annuity continues
for as long as you both live. If
your spouse (or other second
annuitant) lives longer than you,
he or she receives, for his or
her remaining lifetime, the full
amount of the income you were
receiving.
2. Two-Thirds Benefit to Survivor The
full amount of the annuity con-
tinues for as long as you both
live. If your spouse (or other sec-
ond annuitant) lives longer than
you, he or she receives, for his
or her remaining lifetime, two-
thirds of the income you were
receiving. If you live longer than
your spouse (or other second
annuitant), you will receive two-
thirds of the income you were
receiving.
3. Three-Fourths Benefit to Annuity
Partner The full amount of the
annuity continues for as long
as you both live. If your spouse
(or other second annuitant)
lives longer than you, he or she
receives, for his or her remain-
ing lifetime, three-fourths of the
income you were receiving. If you
live longer than your spouse (or
other second annuitant), there
is no reduction in your lifetime
income.
4. Half Benefit to Annuity Partner The
full amount of the annuity con-
tinues for as long as you both
live. If your spouse (or other
second annuitant) lives longer
than you, he or she receives, for
his or her remaining lifetime,
one-half of the income you were
receiving. If you live longer, ben-
efits continue to you at the full
amount.
Installment Refund (For TIAA Only)
Pays you an income for as long as
you live. If you die before the full
value of your TIAA account (cal-
culated as of the date your benefit
payments began) has been paid
out, your beneficiary will receive
the same monthly income you were
receiving before your death until
the remaining value of your account
has been paid out. When the plan
has paid out the value of your entire
TIAA accumulation, all payments
stop. This option is not available for
CREF funds, and is only available for
your TIAA funds if your contract was
in effect before February 1, 1985.
The Interest Payment
Retirement Option
This option, which applies to your
TIAA Traditional Annuity accumu-
lation only, provides monthly pay-
ments that consist only of current
interest and dividends credited
to your TIAA Traditional Annuity
Account balance each month.
Because only the interest is paid,
your principal remains untouched.
This option is available to those

75
age 55 or older and does not sat-
isfy the federal minimum distribu-
tion requirements.
Required Minimum Distribution
Option
This option is available to those
age 70
1
⁄2 or older who have termi-
nated their employment with the
University. Under this option, you
receive periodic payments that sat-
isfy the federal minimum distribu-
tion requirements.
TIAA-CREF Mutual Funds
The only form of payment available
under the TIAA-CREF Mutual Funds
is a full or partial cash withdrawal
of your account balance. Partial
cash withdrawals must be at least
$1,000.
Your Spouse’s Rights
Under federal pension legislation
(Retirement Equity Act of 1984),
if you choose any annuity method
of payment other than a Survivor
Annuity with your spouse as the
survivor, your spouse must give
written consent which acknowl-
edges that his or her rights to
survivor benefits are being waived.
Your spouse’s signature must be
witnessed by a plan representative
or notarized by a notary public.
Federal pension law (ERISA) pro-
vides that if you are married at the
time of your death, your spouse
is entitled to receive, as primary
beneficiary, your qualified preretire-
ment survivor death benefits under
a retirement or tax-deferred annuity
plan covered by ERISA. If you name
someone other than your spouse
as primary beneficiary, your spouse
must consent to this primary ben-
eficiary designation by completing a
Spousal Waiver. Then the qualified
preretirement survivor annuity death
benefits will be payable to such
primary beneficiary. If you elected
only a portion to be paid to the des-
ignated beneficiary, then the remain-
der will be payable to your spouse.
If you designate your spouse as
beneficiary and the individual later
ceases to be your spouse, such des-
ignation will be deemed void and
your ex-spouse will have no rights
as a beneficiary unless redesignated
as a beneficiary by you subsequent
to becoming your ex-spouse or as
otherwise provided under a quali-
fied domestic relations order under
IRS Code Section 414(p).
To comply with the federal Defense
of Marriage Act (DOMA), a par-
ticipant with a spouse of the same
gender is not treated as a married
participant for purposes of applying
these requirements (for example,
the consent of a same-gender
spouse is not required for a partici-
pant to designate someone other
than his/her same-gender spouse
as beneficiary). However, a same-
gender spouse shall automatically
be the beneficiary if the participant
does not elect a beneficiary.
If You Die Before You Begin
to Receive Benefits
If you die before your retirement
income begins, the current full
value of your account balances in
all investment funds will be pay-
able to your beneficiary under any
of the payment options elected by
the beneficiary and allowed by the
investment fund sponsor (subject
to IRS minimum payment rules).
You choose a beneficiary at the
time you enroll in the plan, and
you may change your beneficiary
at any time by filing a new form
with the Benefits Section of Human
Resources. However, if you are mar-
ried, federal law requires that your
spouse be your beneficiary unless
your spouse consents in writing to
your naming another beneficiary
and this consent is witnessed by a
plan representative or notarized by a
notary public.
If your marital status changes after
you become a participant (you
marry, divorce, or separate, or your
spouse dies), be sure to contact
the Benefits Section of Human
Resources immediately to make
any appropriate changes in your
designated beneficiary. If you are
divorced and then re-marry, your
prior beneficiary designation(s) will
become invalid and your current
spouse will automatically become
your beneficiary unless you desig-
nate another beneficiary with your
current spouse’s written consent
(witnessed by a plan representative
or notary public).
Under current federal income tax
laws, your beneficiary must receive
the entire value of your accounts
within five years of your death.
As an exception to this rule, pay-
ments may be made in the form of
an annuity or installments to your
designated beneficiary (including
your spouse). If an annuity is paid,
it must be an annuity with a guar-
anteed period or a fixed period no
longer than your designated benefi-
ciary’s life expectancy.
Generally, annuity or installment
payments must begin by the end
of the year after the year of your
death. However, if your spouse is
your designated beneficiary, he or
she may postpone the start of ben-
efits until a later date, but not later
than the date on which you would
have reached age 70
1
⁄2.
Fidelity allows your beneficiary to
receive a lump sum distribution of
the account balances, to roll over
your account balances into an IRA
or other plan with payments under

76
IRS minimum distribution rules,
or to receive the full value of the
account over a five-year period.
TIAA-CREF allows you to choose
one of the following options, which
are explained in detail in your annu-
ity contract(s), for payment of the
death benefit, or you may leave the
choice to your beneficiary.
1. Income for the life of the benefi-
ciary with payments stopping at
the time of his or her death
2. Income for the lifetime of the
beneficiary, with a minimum
number of payments guaranteed
in any event. The period of guar-
anteed payments must be 10, 15,
or 20 years (subject to IRS rules).
3. Income for a fixed period of
years (subject to IRS rules)
4. Subject to IRS rules, the accumu-
lation may be left on deposit with
TIAA-CREF for future payment
under any of the above options
5. A lump sum distribution of the
account balances or rollover into
an IRA or other plan with pay-
ments under IRS minimum distri-
bution rules
Note: Full or partial cash with-
drawals are the only form of pay-
ment available under the TIAA
Real Estate Account and CREF
Mutual Funds. Balances may
be transferred from the mutual
funds to any of the annuity
accounts to receive the payment
methods described above.
Federal pension legislation requires
that if you die leaving a surviving
spouse and have not named a ben-
eficiary, all of your death benefit will
be paid to your spouse.
The selection of a beneficiary and the
form of payment to the beneficiary
should you die can have important
income and estate tax consequences.
See a qualified advisor if you have
questions about these subjects.
Required Minimum Payment
Rules
Payments must start by April 1 fol-
lowing the year you reach age 70½
or terminate employment with
Boston University, if later. If you do
not receive or start your payments
on time or if the payments are less
than the required minimum amount,
you will have to pay a federal tax
penalty of 50% of the amount
that was required to be distributed
but was not distributed (unless
you show reasonable cause to the
Internal Revenue Service). See the
“Forms of Payment” section for
your choices.
If You Become Disabled
(Contribution Waiver)
If you should become totally dis-
abled, you will be eligible for a
waiver of your required contribu-
tions to this plan. Your disability
insurance, in effect, “pays” your
required contributions and the
University’s contributions. This ben-
efit will continue until you recover
or die, or until your disability
benefits end (see the “Long-Term
Disability” section of this handbook
for additional information concern-
ing the waiver benefit).
The University pays the entire cost
of this protection for you.
If You Leave the University
Prior to age 65, you may not
withdraw any of the funds in your
Retirement Plan accounts under any
circumstances as long as you are
employed at the University.
If your employment with Boston
University ends at any time before
you attain age 65, you are fully
“vested” in all your Retirement Plan
funds. You will receive payment of
your accounts as follows:
Fidelity
1. You may elect to receive a lump
sum distribution of your moneys
invested in these accounts.
2. You may leave funds on deposit
for distribution at a later date.
Under current tax laws, payments
must start by the April 1 following
the calendar year when you reach
age 70
1
⁄2. You may not make con-
tributions directly to your Fidelity
accounts.
3. You may roll over your account to
an IRA or other plan that accepts
rollovers, provided that you meet
federal tax law requirements.
TIAA-CREF
1. For Retirement Annuity (RA) con-
tracts issued prior to June 1, 2005:
(a) If your TIAA contract is less
than $2,000 in value, you may
apply for a lump sum distribu-
tion of the full value of your
account. You may then roll over
your lump sum payment into an
IRA or other plan that accepts
rollovers, provided you meet
federal tax law requirements.
(b) If your TIAA contract is at least
$2,000 in value, you may begin
receiving lifetime annuity pay-
ments or elect TIAA’s Transfer
Payout Annuity. Under current
tax laws, payments must start
by the April 1 following the year
in which you reach age 70
1
⁄2 or
upon retirement, whichever is
later.
2. For Group Retirement Annuity
(GRA) contracts issued after
June 1, 2005:
(a) You may apply for a lump
sum distribution of the full
value of your account within

77
a 120-day period following
your termination of employ-
ment. A withdrawal charge
of 2.5% applies to such lump
sum withdrawals. You may
then roll over your lump sum
payment into an IRA or other
plan that accepts rollovers,
provided you meet federal tax
law requirements.
(b) You may receive a fixed-period
annuity of five to thirty years
(subject to IRS restrictions).
3. You may elect to receive a
lump sum distribution of moneys
invested in CREF. This may be
rolled over into an IRA or other
plan that accepts rollovers, pro-
vided you meet federal tax law
requirements.
The rights of your spouse, which
were described earlier (see “Your
Spouse’s Rights”), also apply to
the choice of a form of payment
for benefits due when you termi-
nate your employment with the
University.
Tax Considerations When You
Receive Benefits
Federal income tax must be with-
held from the taxable portion of all
plan benefits you or your benefi-
ciary receive, unless you or your
beneficiary elect otherwise (but see
the last paragraph of this section for
an exception).
Under current federal law, ordinary
income tax applies to payments to
you from your plan accounts (not
including qualified payments from
an after-tax Roth account and not
including payments considered
to be a return of after-tax contri-
butions you have made—these
are recovered without additional
income tax under specific rules for
determining the after-tax portion of
each payment).
In addition, a 10% penalty tax
applies to all payments you receive
before you reach age 59
1
⁄2, except
certain payments in the form of an
annuity. The 10% penalty tax does
not apply if payments are received
because of your death, disability, or
early retirement at age 55 or older;
or in connection with a Qualified
Domestic Relations Order; or in
amounts which do not exceed your
tax-deductible medical expenses
or certain amounts spent for health
insurance in the event of your
extended unemployment.
You may be able to postpone pay-
ment of taxes if you are able to
roll over your plan distribution to
an IRA or other plan that accepts
rollovers.
Any contributions in the plan may
be rolled over to an IRA or another
403(b) arrangement or qualified
plan that accepts such contribu-
tions in order to continue earning
tax-deferred interest or investment
gains.
All cash distributions from the
plan, except those payable as an
annuity or in periodic installments
for at least 10 years, those payable
to non-spouse beneficiaries, and
those mandated by minimum dis-
tribution rules, will be eligible for
direct rollover to an IRA or another
plan that will accept them. If these
distributions are not directly rolled
over to an IRA (or to another
employer 403(b) plan that will
accept them), they will be subject
to mandatory 20% federal income
tax withholding.
Leaves of Absence
If you are granted a leave of absence
at full pay, the University’s and your
normal contributions to the plan
will continue. If you are granted a
leave of absence at partial pay, the
University’s and your contributions
will be based on your reduced base
salary.
Your contributions will stop if you
are granted an unpaid leave of
absence. However, they will start
again, automatically, with the first
paycheck you receive when you
return.
If you are granted a military leave
of absence, upon your return while
you are protected by the veterans’
reemployment laws, the University
will contribute to the plan an
amount representing the contribu-
tions that would normally have been
made during your military leave
provided you make the required
employee contributions.
Remember, if you leave work for
any reason for a prolonged period
of time, you should always contact
the Benefits Section of Human
Resources to ask what effect your
absence may have on this and
other University-sponsored benefits
plans.
Administrative Fees
Please refer to the Fee Disclosure
document at www.bu.edu/hr/files/
documents/BN_Fee_Notice.pdf for
further details.
Fidelity
At distribution, certain Fidelity
funds may charge a redemption
fee. These fees are described in
the fund prospectus. In addition,
expenses related to mutual fund
management are assessed before
mutual fund earnings are credited
to your account.

78
TIAA-CREF
TIAA-CREF charges fees for
administering the transactions
involved in the plan. For all TIAA-
CREF annuities, the operating
charge will be deducted from
investment earnings before earn-
ings are credited to your account.
Lump sum withdrawals from the
TIAA Traditional Annuity Account
under a Group Retirement Annuity
Policy issued after June 1, 2005,
are subject to a 2.5% surrender
fee.
Loss of Benefits
There may be circumstances which
may result in a reduction in the
value of your account(s), such as:
• The fees/redemption charges
(described above) that relate
directly to your investments will
be deducted directly from your
account.
• A payment from your account
was required under the terms of
a Qualified Domestic Relations
Order.
• You failed to repay a participant
loan on a timely basis and an
offset of that amount occurred in
your account.
• The value of the investments
in your plan account could
decrease in response to market
conditions.
How to Obtain Benefits
Fidelity
You should contact Fidelity or
the Benefits Section of Human
Resources for a distribution form.
Fidelity has counselors who will
provide you with information that
may help you in deciding which
distribution option best meets your
financial needs.
TIAA-CREF
You should contact TIAA-CREF
for an application for benefit pay-
ment. Before you choose a payment
form, TIAA-CREF will supply you
with a statement of your accounts
and illustrations of your projected
income under various payment
options to help you decide which
payment option is best for you.
TIAA-CREF has consultants who
will assist you in deciding which
distribution option or combination
of options is best suited for your
individual circumstances.
Appealing a Denial
If you or your beneficiary apply for
benefits and your claim is denied,
in whole or in part, you may con-
sult the Benefits Section of Human
Resources for information about
how to appeal the denial.
Additional information about appeal-
ing a denial of benefits is included
in the “Administrative Information”
section of this handbook.
Other Important
Information
Contributions to this plan are sub-
ject to the provisions and limita-
tions of the Internal Revenue Code
and IRS regulations and rulings,
including the contribution limits in
Sections 402(g), 401(m), and 415.
All University contributions to this
plan must be used for the benefit
of plan members and beneficiaries.
Once made, the contributions can-
not be taken back by the University,
except if made as a result of a mis-
take of fact.
A mistaken over-contribution to
your account by the University will
be returned to the University. A con-
tribution by you that exceeds any of
the limits or is otherwise a mistake
will be returned to you, in accor-
dance with IRS rules.
Payments to Others
Your rights under the Retirement
Plan cannot be assigned or used as
collateral, and your accounts are
not generally subject to attachment
or garnishment. However, under
federal law, the plan must honor
a Qualified Domestic Relations
Order from a court requiring pay-
ment to a divorced or separated
spouse or for child support or a
lien on your accounts for pay-
ment of overdue taxes and certain
other specified types of liens and
attachments. A copy of the Plan’s
Qualified Domestic Relations Order
Procedures is available at no cost
upon request to the Benefits Section
of Human Resources.
To comply with the federal Defense
of Marriage Act (DOMA), a par-
ticipant with a spouse of the same
gender is not treated as a married
participant for purposes of applying
these QDRO rules.

79
Termination of Participation
Your participation in the Retirement
Plan ends when you retire or oth-
erwise terminate your employ-
ment with Boston University. It
will also end if your status as a
regular employee ends, or if you
stop contributing. From the date
that your participation ends until
your accounts are fully distributed
to you, you will be considered a for-
mer member, or, if you voluntarily
stopped contributions, a suspended
member.
This Plan Is Not Insured by the
PBGC
Retirement Plan benefits are not
guaranteed by the Pension Benefit
Guaranty Corporation (PBGC),
which does not cover plans such as
this one with individual accounts for
each participant. Upon termination
of the plan, you would be eligible
to receive the total amount in your
accounts.

Overview
Supplemental Retirement and Savings Plan
82
I
n addition to the Boston University Retirement Plan, you may also accum-
ulate funds for your future through the Boston University Supplemental
Retirement and Savings Plan. Your contributions to the plan are made
through payroll deduction and may be invested in any of the following
investment vehicles: Teachers Insurance and Annuity Association (TIAA),
the College Retirement Equities Fund (CREF), or any of the mutual funds
managed by Fidelity Investments.
The contributions you make to the plan may at your election be used
to increase the retirement income you receive under the University’s
Retirement Plan and will add to the financial security you can build with
Social Security and your personal assets.
You have the choice to pay no income tax on the money you contribute
to the plan until withdrawal. In addition, investment earnings accu-
mulate tax-free until withdrawal. Alternatively, your contributions to
the plan may be made as Roth contributions on an after-tax basis to
Fidelity Investments only. If you make Roth contributions, your invest-
ment earnings will accumulate tax-free and will be considered tax-free
at the time of withdrawal as long as your withdrawal is qualified.
83
About the Supple men tal
Retirement and Savings Plan
The Supplemental Retirement and
Savings Plan offers you the oppor-
tunity to set aside additional money
for your future. You have a choice
of contributing to the plan in the fol-
lowing ways:
Before-Tax Contributions—You pay
no federal or state income tax on
the before-tax money you put into
the plan or the accumulated invest-
ment earnings until you receive
it. These are referred to as “tax-
deferred contributions.”
After-Tax Roth Contributions—You
pay federal and state income tax
on the after-tax money you put into
the plan. The investment earnings
accumulate tax-free and are paid to
you tax-free at the time you receive
it as long as the withdrawal is quali-
fied. Roth contributions may only be
made through Fidelity Investments.
To find out more about the Supple-
mental Retirement and Savings Plan,
read this section carefully. Then, to
begin saving for your future, con-
tact the Benefits Section of Human
Resources.
Eligibility
You are eligible to participate in
this plan if you are an employee of
the University (other than a leased
employee or an employee who is a
bona fide student who is enrolled in
and regularly attending classes).
If eligible, you may begin par-
ticipating in the plan on the next
payroll following the receipt of your
application.
Enrollment
Participation in the Supplemental
Retirement and Savings Plan is vol-
untary. If you would like to enroll in
the Supplemental Retirement and
Savings Plan, please log on to www.
bu.edu/buworkscentral and go the
Employee Self-Service section.
When you log on, you will be able
to:
• Enroll for the first time
• Open an account with an invest-
ment fund sponsor if you do not
yet have an account with that
sponsor and you want to move
some of your plan money to it
• Change your contribution
amounts
Alternatively, if you wish to enroll in
writing, you may obtain the forms
by logging on to www.bu.edu/hr and
going to the Forms & Documents
section. Upon request, forms will
be mailed directly to you by
the Benefits Section of Human
Resources. Completed forms must
be returned to Human Resources at
25 Buick Street. You need only use
one method of enrollment—online
or paper—not both. Paper enroll-
ments will be processed as soon as
possible after receipt.
Changing or Stopping Your
Elections
You may change or stop your
election at any time via Employee
Self-Service at www.bu.edu/
buworkscental or by obtaining
the appropriate form from www.
bu.edu/hr/home/forms/benefit-
forms.
Your change will be reflected in the
next paycheck you receive follow-
ing the date of your online change
or the date the Benefits Section of
Human Resources receives your
election.
You may stop or reduce contribu-
tions on a prospective basis only;
that is, you cannot take back any
contributions once they are made.
Your ability to change your invest-
ment choices, or to transfer invest-
ments from one fund to another,
depends on your initial choice of
investments. You should review
the restrictions in each fund care-
fully before making your invest-
ment decision.
If you previously participated in
another 403(b) or other type of
tax-deferred plan (such as a 401(k)
plan) with a previous employer,
you may be able to roll over your
account balances from that plan to
the Boston University Retirement
Plan or the Supplemental Retirement
and Savings Plan, provided you meet
the plan’s rules and the rules of
the investment fund sponsors. The
Benefits Section of Human Resources
can provide you with further informa-
tion on rollovers.
Tax-Deferred Contributions
and After-Tax Roth 403(b)
Contributions
The Supplemental Retirement and
Savings Plan gives you a choice as
to whether you want to make your
contributions on a tax-deferred or
after-tax basis or a combination of
tax-deferred and Roth after-tax.
Supplemental Retirement and Savings Plan

84
• Tax-Deferred Contributions—You
will not have to pay any taxes
(except Social Security withhold-
ing) on the portion of pay you put
into the plan. According to fed-
eral law, such tax-deferred contri-
butions are treated as University
contributions. Therefore, your
contributions are not considered
taxable income, and you are
not required to pay federal or
Massachusetts income taxes on
that money until you receive pay-
ment of your accounts. This will
normally be after your retirement,
when your taxable income and
your tax rate may be lower. You
may make tax-deferred contribu-
tions by entering into a “salary
reduction” agreement with the
University when you enroll. Your
salary reduction (tax-deferred)
contributions, as well as Roth
403(b) contributions, are subject
to applicable Social Security tax
withholdings.
• Roth 403(b) Contributions (Only
with Fidelity Investments)—Your
contributions will be made on an
after-tax basis. Earnings on your
Roth 403(b) account are tax-free
when withdrawn as long as the
withdrawal is qualified. A quali-
fied withdrawal is one that is
taken (i) no earlier than the fifth
calendar year after the year of
your first Roth contribution and
(ii) after you have attained age
59
1
⁄2, become disabled, or die.
How Much You Can Contribute
You may contribute any portion you
choose of your weekly or monthly
pay, subject to tax law limits. Several
limits and rules apply, but the limit
that will affect most participants for
2013 is $17,500 (not yet age 50) or
$23,000 (age 50 or more at the end
of the year). The limit applies to your
combined contributions on a tax-
deferred and after-tax basis to this
plan and to the Boston University
Retirement Plan.
These amounts are indexed for
inflation each year, but only in $500
increments. The new limits will be
communicated to participants after
the IRS announces them for any par-
ticular year.
Other limits may apply in certain
situations; the Benefits Section of
Human Resources will communicate
with you if any limit applies to your
contributions.
You must contribute the same por-
tion of your pay each payroll period,
and you must make your contribu-
tion by salary reduction. No lump
sum cash contributions are permit-
ted. These rules are due to Internal
Revenue Code regulations.
Note: Special rules and limits apply
if, during a calendar year, you also
participate in another plan main-
tained by a business you own or
control. For example, if you have
consulting or other self-employment
income and participate in a self-
employed plan to which you make
contributions, the special rules may
affect you. If this situation applies to
you, consult a qualified tax profes-
sional for advice on how the limits
apply to you.
Investment Choices
You choose how contributions to
your accounts will be invested from
among the following investment
fund sponsors. Boston University
has no responsibility for your choice
of investments. Since you choose
the investment options for the
account, you have the responsibil-
ity for the financial results. The
plan is intended to be a participant-
directed plan as described in Section
404(c) of the Employee Retirement
Income Security Act of 1974 as
amended (ERISA) and Department
of Labor regulations governing sec-
tion 404(c) plans. This means that
fiduciaries of the plan are relieved
of liability for any losses that are
the result of investment instructions
given by a participant or benefi-
ciary under the participant-directed
investment feature of the plan.
You should consult a professional
financial advisor for investment
advice and financial planning assis-
tance before choosing an investment
option. Further information may be
obtained directly from the invest-
ment fund sponsors. You should
read the prospectus or other infor-
mation carefully before investing.
Fidelity Investments
Fidelity Investments is a mutual fund
company which offers many funds
with a wide variety of investments:
short-term, bonds, and stocks. The
investment objectives and policies of
each fund, as well as the expenses
and fees for the fund, are described
in its prospectus, which you should
read. Investments for the Boston
University Supplemental Retirement
and Savings Plan are made through
the Fidelity Tax-Exempt Services
Company.
Teachers Insurance and Annuity
Association and College
Retirement Equities Fund
(TIAA-CREF)
TIAA-CREF is a financial services
company. TIAA-CREF offers guaran-
teed and variable annuity accounts,
as well as mutual funds covering a
broad range of asset classes.
In order to obtain a detailed
description of the funds offered by
Fidelity and TIAA-CREF, you should
contact the Benefits Section of
Human Resources.
85
Investment Restrictions
Each investment fund sponsor
places certain restrictions on your
investments. For complete, current
details on restrictions, you should
refer to the printed materials avail-
able from each of the investment
fund sponsors. Following are expla-
nations of some of the most impor-
tant restrictions.
The following rules apply to how
future contributions to the plan are
invested:
1. You may choose to invest your
own future tax-deferred con-
tributions in either the TIAA-
CREF family of funds or in the
Fidelity family of funds (Fidelity
funds are available for both tax-
deferred and Roth after-tax con-
tributions), or you may split your
contributions between the two.
2. If you choose to invest your tax-
deferred contributions in the
TIAA-CREF funds, you may split
contributions between TIAA and
CREF in any combination you
choose.
3. If you choose to invest in the
Fidelity funds, you may split your
contributions among the funds in
any combination you choose.
4. Subject to the restrictions on
Roth after-tax contributions, you
can change your choice of where
to invest future contributions as
often as once a month.
The following rules apply for moving
account balances from one invest-
ment sponsor to another:
1. Transfers can be made out of
TIAA into CREF or Fidelity in any
amount at any time.
2. Transfers can be made out of
CREF into TIAA or Fidelity in any
amount at any time.
3. Transfers can be made out of
Fidelity into TIAA or CREF in any
amount at any time, except that
TIAA and CREF cannot accept
Roth after-tax contributions.
4. Transfers among Fidelity funds
can be made at any time, but
a fee may be charged if more
than four transfers are made
in the calendar year.
In-Plan Roth Rollover
When taking an eligible distribution
(as defined below), you may elect
to convert all or a portion of your
Plan Account (other than your Roth
Contribution Account) to a Roth
Contribution Account as an In-Plan
Roth Rollover. This Rollover actually
occurs within the Plan. You do not
receive a check and then contribute
it to the Plan. An eligible distribu-
tion is (i) a distribution to an active
Member on or after attaining age
65; (ii) a distribution made upon
termination of employment, becom-
ing disabled, or retirement; (iii) a
distribution upon the Member’s
death; or (iv) any distribution that
would otherwise qualify as an eli-
gible rollover distribution.
A key benefit of a Roth is the poten-
tial for federally tax-free earnings
and withdrawals. Converting to a
Roth 403(b) can be beneficial if you
expect your tax rate to increase in
the future, because you pay taxes
on the money you convert now.
You are advised to consult a tax
advisor to better understand these
requirements. The full amount of
any conversions to a Roth 403(b)
processed in a calendar year will be
considered taxable income in that
calendar year.
Statements of Your Accounts
You will receive quarterly state-
ments by mail directly from TIAA-
CREF. Fidelity’s quarterly statements
are available online at Fidelity
NetBenefits.
Withdrawals While Employed
by Boston University
The Supplemental Retirement and
Savings Plan is intended to provide
long-term savings opportunities for
your retirement years. However,
while you are employed, there may
be circumstances in which you will
need to make a withdrawal for other
important financial needs.
The Internal Revenue Service places
restrictions on withdrawals. You
may not withdraw post-1988 con-
tributions while still employed by
Boston University unless you:
• Reach age 59½; or
• Are able to prove financial
hardship
Post-1988 earnings are not available
for withdrawal while you are work-
ing at Boston University until you
reach age 59½.
For purposes of making withdraw-
als under the Plan, the IRS defines
financial hardship as the need for
funds to meet certain immediate
and heavy expenses. Funds must
not be reasonably available from
other sources. Federal withdrawal
rules limit hardship withdrawals to
needs such as:
• The purchase price of your pri-
mary residence
• Higher education expenses for
you or your dependents
• Major uninsured medical
expenses for you or your
dependents
86
• Expenses to prevent eviction
from your primary residence or
mortgage foreclosure
• Funeral expenses for your par-
ents, spouse, children, or other
tax dependent
• Expenses for the repair of your
primary residence that would
qualify for casualty deduction
under federal tax rules (but with-
out regard to the 10% limit)
Boston University must abide by
these rules in considering requests
for hardship withdrawals.
You may withdraw contributions
credited to your TIAA-CREF Group
SRA account prior to January 1, 1989,
and related earnings at any time.
You may start making withdraw-
als or start receiving installment or
annuity payments from the plan
once you reach age 59½ even
though you are still employed at
Boston University.
Withdrawals are paid as a lump
sum in cash. To make a with-
drawal, you must complete and
submit the appropriate withdrawal
form. These forms are available
directly from Fidelity Investments
and TIAA-CREF.
Please note: In general, if you are under
age 59½ when you make an in-service
withdrawal, unless an exception applies,
your money will be subject to a 10%
penalty tax, in addition to regular income
tax (see “Tax Consider ations When You
Receive Benefits”).
Loans While Employed by
Boston University
You may borrow money against
your Supplemental Retirement and
Savings Plan accumulations while
employed by the University. IRS
rules limit the maximum loan you
may take from this Plan. Through
this loan feature, you have access to
your Supplemental Retirement and
Savings Plan accumulations, up to
permissible limits, without the need
to experience a triggering event
including meeting the financial hard-
ship provisions listed above. For
detailed information about the loan
provisions, contact TIAA-CREF or
Fidelity directly.
Forms of Payment
You or your beneficiary may begin
receiving payment of your plan ben-
efits, other than in-service withdraw-
als, when you retire, die, become
disabled, or terminate your employ-
ment with Boston University. Some
choices regarding the form of pay-
ment are available. However, if your
total account balances are $5,000
or less, the plan has the right to pay
them out in a lump sum in cash.
Any payments you receive before
age 59½ may be subject to a
10% penalty tax in addition to
regular income tax (see “Tax
Considerations When You Receive
Benefits”) unless one of a limited
number of exceptions applies.
You may elect to receive a lump
sum distribution of the full value of
your accounts from either TIAA-
CREF or Fidelity.
As an alternative to a lump sum
distribution, benefits attributable to
contributions made to the Boston
University Supplemental Retirement
and Savings Plan may be received in
one of the following forms.
Fidelity
Installment Withdrawal Program
As an alternative, you may elect
to maintain your account balances
with Fidelity and receive install-
ment withdrawals until you have
exhausted your account balances.
You may designate the amount and
the frequency of these withdrawals.
Rollover You may also roll over the
account balances in your Fidelity
funds into an individual retirement
account (IRA) or another plan you
participate in that accepts roll-
overs, provided you meet federal
requirements. If you wish, you may
use the proceeds of your account
to purchase an annuity through
TIAA-CREF or another insurance
company. You may wish to consult
with your financial advisor before
selecting this option.
TIAA Fixed Annuity
A lifetime annuity may be received
from your TIAA Traditional Annuity
Account. Lifetime annuity income
is the only payment method that
ensures you will never outlive your
retirement income. It is also a per-
manent arrangement. Once you
begin receiving payments, you may
not stop them. The actual amount
of income you receive at retirement
depends primarily on the amount in
your TIAA account, your age when
payments begin, and the form of
payment you choose (see “Annuity
Forms of Payment”).
Once the amount of your TIAA fixed
annuity is determined, it can be
increased or decreased by changes
in dividends, but cannot fall below
the contractually guaranteed level.
TIAA Real Estate Account and
CREF Forms of Payment
Lump Sum You may receive a lump
sum distribution from TIAA Real
Estate Account and CREF for all
or part of the full value of your
accounts at the time of payment.
Fixed Period Payments TIAA Real
Estate Account and CREF accumula-
tions may be taken over any period
between two and 30 years, subject
to IRS restrictions. At the end of the
selected period, payments will end.

87
TIAA Real Estate Account and CREF
Annuity A lifetime annuity may
be received from your TIAA Real
Estate Account and CREF Account.
Lifetime annuity income is the only
payment method that ensures you
will never outlive your retirement
income. It is also a permanent
arrangement. Once you begin
receiving payments, you may not
stop them. The actual amount of
income you receive at retirement
depends primarily on the amount
in your account, your age when
payments begin, and the form of
payment you choose (see “Annuity
Forms of Payment”).
Annuity Forms of Payment (Applies
to TIAA-CREF Payments Only)
The following is a description of
the types of annuities TIAA-CREF
provides for moneys invested with
them. These annuity options would
also be available if you transferred
Fidelity funds to TIAA-CREF at
retirement. Just before you are
scheduled to start receiving your
income, you will be asked to choose
the option that best meets your
needs. Information is available from
TIAA-CREF to help you decide.
Subject to certain minimum require-
ments, you also may choose to
receive part of a contract’s accu-
mulation under one option, and the
balance under another option. Of
course, when you choose an annu-
ity option, you may also choose
to take a portion of your accounts
in cash; however, this will reduce
the amount of annuity income you
receive. You should note when
reviewing these options that the
size of the monthly payments
depends not only on your age and
account balances, but may also
depend on the age of your spouse
or other beneficiary.
Single Life Annuity Pays you an
income for as long as you live. This
option provides a larger monthly
income for you than the other
options. However, all payments
will stop at your death.
Life Annuity with 10-, 15-, or 20-Year
Guaranteed Period Pays you an
income for as long as you live, with
installments guaranteed to continue
during the first 10, 15, or 20 years, as
you select, whether you live or die.
If you live beyond the guaranteed
period, payments continue for your
lifetime. If you die during the guar-
anteed period, payments continue to
your beneficiary for the balance of
the guaranteed period.
Survivor Annuity Pays you an
income for life. If your spouse or
second annuitant lives longer than
you, he or she continues to receive
an income for life. The amount of
the income continuing to the sur-
vivor depends on which option you
choose from the four options listed
below. The amount of the annuity
payable to you at the onset of each
of these options is different; the
more you choose to make payable
to your survivor, the smaller your
own income during your lifetime.
Each of these survivor options is
available with a 10-, 15-, or 20-year
guaranteed period. This provides
that if both you and your spouse or
second annuitant die during the first
10-, 15-, or 20-years (whichever you
select), the option that you select
continues to another named benefi-
ciary for the balance of the guaran-
teed period.
1. Full Benefit to Survivor The full
amount of the annuity continues
for as long as you both live. If
your spouse (or other second
annuitant) lives longer than you,
he or she receives, for his or
her remaining lifetime, the full
amount of the income you were
receiving.
2. Two-Thirds Benefit to Survivor
The full amount of the annu-
ity continues for as long as you
both live. Upon your death or the
death of your spouse (or other
second annuitant), the payments
are reduced to two-thirds of the
amount that you were receiving
and are continued to the survivor
for life.
3. Three-Fourths Benefit to
Survivor The full amount of the
annuity continues for as long as
you both live. If your spouse (or
other second annuitant) lives lon-
ger than you, he or she receives,
for his or her remaining lifetime,
three-fourths of the income you
were receiving.
If you live longer than your
spouse (or other second annui-
tant), you will receive three-
fourths of the income you were
receiving.
4. Half Benefit to Survivor The full
amount of the annuity continues
for as long as you both live. If
your spouse (or other second
annuitant) lives longer than you,
he or she receives, for his or her
remaining lifetime, one-half of
the income you were receiving.
If you live longer, the benefit
continues at the full amount.
Fixed Period Annuity Pays you
an income for a fixed period you
choose, from two to 10 years. If you
die during the period chosen, pay-
ments in the same amount that you
were receiving will continue to your
beneficiary for the remainder of the
period. At the end of the period, all
payments stop.

88
Required Minimum Distribution
Option
This option is available to those
age 70½ or older who have termi-
nated their employment with the
University. Under this option, you
receive periodic payments that sat-
isfy the federal minimum distribu-
tion requirements.
In-Plan Roth Rollovers
A Member, Former Member, or
Member’s Beneficiary who may
take an eligible distribution (as
defined below) may elect to convert
all or a portion of his Plan Account
(other than his Roth Contribution
Account) to a Roth Contribution
Account as an In-Plan Roth Rollover.
This rollover actually occurs within
the Plan. You do not receive a check
and then contribute it to the Plan.
An eligible distribution is (i) a dis-
tribution to an active Member on
or after attaining age 65; (ii) a dis-
tribution made upon termination of
employment, becoming disabled, or
retirement; (iii) a distribution upon
the Member’s death; or (iv) any
distribution that would otherwise
qualify as an eligible rollover
distribution.
Your Spouse’s Rights
Under federal pension legislation,
if you choose any annuity method
of payment other than a survivor
annuity with your spouse as the sur-
vivor, your spouse must give written
consent which acknowledges that
his or her rights to survivor benefits
are being waived. Your spouse’s
signature must be witnessed by a
plan representative or notarized by a
notary public.
Federal pension law (ERISA) pro-
vides that if you are married at the
time of your death, your spouse
is entitled to receive, as primary
beneficiary, your qualified preretire-
ment survivor death benefits under
a retirement or tax-deferred annuity
plan covered by ERISA. If you name
someone other than your spouse
as primary beneficiary, your spouse
must consent to this primary ben-
eficiary designation by completing a
Spousal Waiver. Then the qualified
preretirement survivor annuity death
benefits will be payable to such
primary beneficiary. If you elected
only a portion to be paid to the des-
ignated beneficiary, then the remain-
der will be payable to your spouse.
If you designate your spouse as
beneficiary and the individual later
ceases to be your spouse, such
designation will be deemed void and
your ex-spouse will have no rights
as a beneficiary unless redesignated
as a beneficiary by you subsequent
to becoming your ex-spouse or
as otherwise provided under a
Qualified Domestic Relations Order
under IRS Code Section 414(p).
To comply with the federal Defense
of Marriage Act (DOMA), a par-
ticipant with a spouse of the same
gender is not treated as a married
participant for purposes of applying
these requirements (for example,
the consent of a same-gender
spouse is not required for a partici-
pant to designate someone other
than his/her same-gender spouse
as beneficiary). However, a same-
gender spouse shall automatically
be the beneficiary if the participant
does not elect a beneficiary.
If You Die Before You Begin to
Receive Benefits
If you die before your retirement
income begins, the full current
value of your account balances in
all investment funds will be pay-
able to your beneficiary under any
of the payment options elected by
the beneficiary and allowed by the
investment fund sponsor (subject to
IRS minimum payment rules).
You choose a beneficiary at the
time you enroll in the plan, and
you may change your beneficiary
at any time by filing a new form
with the Benefits Section of Human
Resources. However, if you are mar-
ried, federal law requires that your
spouse be your beneficiary, unless
your spouse consents in writing to
your naming another beneficiary and
this consent is witnessed by a plan
representative or notarized by a
notary public.
If you designate your spouse as
beneficiary and the individual later
ceases to be your spouse, such des-
ignation will be deemed void and
your ex-spouse will have no rights
as a beneficiary unless redesignated
as a beneficiary by you subsequent
to becoming your ex-spouse or as
otherwise provided under a Qualified
Domestic Relations Order under IRS
Code Section 414 (p).
If your marital status changes after
you enroll in this plan (you marry,
divorce or separate, or your spouse
dies), be sure to contact the Benefits
Section of Human Resources
immediately to make any appro-
priate changes in your designated
beneficiary. If you marry or you are
divorced and then re-marry, your
prior beneficiary designation(s) will
become invalid and your current
spouse will automatically become
your beneficiary unless you desig-
nate another beneficiary with your
current spouse’s written consent
(witnessed by a plan representative
or notary public).
Under current federal income tax
laws, your beneficiary must receive
the entire value of your accounts
within five years of your death,
unless payments are made in the
form of an annuity or installments to
89
your designated beneficiary (includ-
ing your spouse). If an annuity is
paid, it must be an annuity with a
guaranteed period or fixed period no
longer than your designated benefi-
ciary’s life expectancy.
If your spouse is your designated
beneficiary, he or she may postpone
the start of benefits until a later
date, but until no later than the date
on which you would have reached
age 70
1
⁄2.
Fidelity allows your beneficiary to
receive a lump sum distribution
of the account balances, or to roll
over your account balances into an
IRA or another plan that accepts
such rollovers, or to receive the full
value of the account over a five-year
period. A non-spouse beneficiary’s
rollover option is limited only to a
direct rollover to an IRA in accor-
dance with federal tax law.
TIAA-CREF allows you to choose
one of the following options, which
are explained in detail in your annu-
ity contract(s), for payment of the
death benefit, or you may leave the
choice to your beneficiary.
1. Income for the lifetime of the
beneficiary with payments stop-
ping at the time of his or her
death.
2. Income for the lifetime of the
beneficiary, with a minimum
number of payments guaranteed
in any event. The period of guar-
anteed payments may be 10, 15,
or 20 years (subject to IRS rules).
3. Income for a fixed period
(subject to IRS rules).
4. Subject to IRS rules, the accumu-
lation may be left on deposit with
TIAA-CREF for future payment
under any of the above options.
5. A lump sum distribution of the
account balances, or roll-over
to an IRA or other plan that will
accept the rollover.
TIAA-CREF also has a rule that if
you die leaving a surviving spouse
and have not named a beneficiary,
part of your death benefit will be
paid as an annuity to your spouse,
and the balance will be paid in a sin-
gle sum to your estate. The income
payable to your spouse will be one
half the amount that would have
been payable to you had you cho-
sen to begin your annuity payments
under the option described as half
benefit to survivor with a 10-year
guaranteed period, on the first day
of the month in which you died.
Required Minimum Payment Rules
Payments must start by April 1
following the year you reach age
70
1
⁄2 or terminate employment
with Boston University, if later. If
you do not receive or start your
payments on time or if the pay-
ments are less than the required
minimum amount, you will have to
pay a federal tax penalty of 50% of
the amount that was required to be
distributed but was not distributed
(unless you show reasonable cause
to the Internal Revenue Service).
See the “Forms of Payment” sec-
tion for your choices.
If You Leave the University
If your employment with Boston
University ends at any time before
retirement, you are fully “vested”
in all of your Supplemental
Retirement and Savings Plan funds.
You will receive payment of your
accounts as follows:
Fidelity
1. You may elect to receive a lump
sum distribution of the moneys
invested in your accounts.
2. You may leave funds on account
for distribution at a later date (no
later than April 1 following the
calendar year when you reach
age 70
1
⁄2). You may not make
contributions directly to your
Fidelity accounts.
3. You may roll over all or a por-
tion of your account into an IRA
or other plan that will accept the
rollover, provided you meet fed-
eral requirements.
TIAA-CREF
1. You may receive a lump sum dis-
tribution of the full value of your
accounts. If you take a lump sum
payment, you may be able to roll
over all or a portion of it into an
IRA or other plan that will accept
the rollover.
2. You may leave all accumulated
moneys in your TIAA-CREF
accounts and receive an annuity.
You may begin receiving annu-
ity payments at any time, but no
later than April 1 following the
calendar year when you reach
age 70
1
⁄2.
3. You may leave funds in your
account for distribution at a later
date (subject to the age 70
1
⁄2
rule).
The rights for your spouse, which
were described earlier (see “Your
Spouse’s Rights”), also apply to the
choice of a form of payment for ben-
efits due when you terminate your
employment with the University.
Tax Considerations When You
Receive Benefits
Federal and state income tax must
be withheld from the taxable por-
tion of all plan benefits you or
your beneficiary receive, unless
you or your beneficiary elect oth-
erwise (but see the last paragraph
of this section for an exception).
90
Under current federal law, ordi-
nary income tax applies to taxable
payments to you from your plan
accounts. Qualified withdrawals
from a Roth contributions account
are tax-free.
A 10% penalty tax applies to all
payments you receive before you
reach age 59
1
⁄2, except payments in
the form of an annuity. The 10%
penalty tax does not apply if pay-
ments are received because of your
death, disability, or early retirement
at age 55 or older; or in connection
with a Qualified Domestic Relations
Order; or in amounts that do not
exceed your tax-deductible medical
expenses or certain amounts spent
for health insurance in the event of
your extended unemployment or to
qualified withdrawals from a Roth
contributions account.
You may be able to postpone
payment of taxes if you are able
to transfer or roll over your plan
distribution to an IRA or another
plan that accepts rollovers. All cash
distributions from the plan except
those payable as an annuity or in
periodic installments for at least 10
years, those mandated by minimum
distribution rules, and hardship with-
drawals, will be eligible for direct
transfer to an IRA or another plan
that accepts rollovers. If these distri-
butions are not directly rolled over to
an IRA (or to another employer plan
that will accept them), they will be
subject to mandatory 20% federal
income tax withholding.
Leaves of Absence
If you are granted a leave of absence
at full pay, your normal contributions
to the plan will continue (unless you
make a change). If you are granted
a leave of absence at partial pay,
please contact the Benefits Section
of Human Resources.
Your contributions will stop if you
are granted an unpaid leave of
absence. However, they will start
again, automatically, with the first
paycheck you receive when you
return (unless you make a change).
Remember, if you leave work for
any reason for a prolonged period of
time, you should always contact
the Benefits Section of Human
Resources to ask what effect your
absence may have on this and other
University-sponsored benefit plans.
Administrative Fees
There are fees associated with
loans. These may change from time
to time. See Fee Disclosure at www.
bu.edu/hr/files/documents/BN_
Fee_Notice.pdf for further details.
Fidelity
At distribution, certain Fidelity
funds may charge a redemption
fee. These fees are described in
the fund prospectus. In addition,
expenses related to mutual fund
management are assessed before
mutual fund earnings are credited
to your account.
TIAA-CREF
TIAA-CREF charges fees for admin-
istering the transactions involved
in the plan. There is no expense
charge deducted from contributions
to TIAA. This cost is included by
lowering the dividend interest rate.
For purchase of annuity contracts,
as described under “If You Leave
the University,” there is no expense
charge if the annuity contract has
been in force for 34 months or
more, or if the purchase is of an
annuity contract owned by a person
age 60 or older.
For all other purchases, there is an
expense charge determined sepa-
rately for each TIAA or CREF
contract and deducted from the
accumulation being purchased. This
charge is 10% of the accumulation
being purchased less one tenth of
1% of that accumulation for each
month elapsed since the contract’s
date of issue—but in no event more
than $50 per contract.
Loss of Benefits
There may be circumstances which
may result in a reduction in the
value of your account(s), such as:
• The fees/redemption charges
(described above) that relate
directly to your investments
will be deducted directly from
your account.
• A payment from your account
was required under the terms of
a Qualified Domestic Relations
Order.
• You failed to repay a par-
ticipant loan on a timely basis
and an offset of that amount
occurred in your account.
• The value of the investments
in your plan account could
decrease in response to market
conditions.
How to Obtain Benefits
Fidelity
You should contact Fidelity for a
distribution form or you may down-
load one from the Human Resources
website at www.bu.edu/hr/home/
forms. Fidelity has counselors who
will provide you with information
that may help you in deciding which
distribution option best meets your
financial needs.
TIAA-CREF
You should contact TIAA-CREF
for an application for benefit pay-
ment. Before you choose a payment

91
form, TIAA-CREF will supply you
with a statement of your accounts
and illustrations of your projected
income under various payment
options to help you decide which
payment option is best for you.
Appealing a Denial
If you or your beneficiary apply
for benefits from this plan and
your claim is denied, in whole or in
part, you may consult the Benefits
Section of Human Resources for
information about how to appeal the
denial.
Additional information about
appealing a denial of benefits is
included in the “Administrative
Information” section of this hand-
book.
Payment to Others
Your rights under the Supplemental
Retirement and Savings Plan cannot
be assigned or used as collateral, and
your accounts are not generally sub-
ject to garnishment. However, under
federal law, the plan must honor a
Qualified Domestic Relations Order
from a court requiring payment to a
divorced or separated spouse or
for child support or a lien on your
account for the payment of over-
due taxes, or to satisfy certain
other court orders. A copy of the
Plan’s Qualified Domestic Relations
Order Procedures is available at no
cost upon request to the Benefits
Section of Human Resources.
To comply with the federal Defense
of Marriage Act (DOMA), a par-
ticipant with a spouse of the same
gender is not treated as a married
participant for purposes of applying
these QDRO rules.
Correction of Mistakes
If through a payroll processing or
other error, the wrong amount is
taken from your paycheck or con-
tributed to your plan account, or
if an adjustment is necessary to
meet one of the tax law limits on
contributions to your accounts,
the Benefits Section of Human
Resources has the right to correct
the mistake or make the necessary
adjustment. Any over-contribu-
tion amounts debited from your
accounts will be repaid to you (less
withholdings, if applicable).
Termination of Participation
Your participation in the Supple-
mental Retirement and Savings Plan
ends when you retire or otherwise
terminate your employment with
the University. It will also end when
your status as a regular employee
changes, or when you stop contrib-
uting. From the date that your par-
ticipation ends until your accounts
are fully distributed to you, you will
be considered a former member, or,
if you voluntarily stopped contribu-
tions, a suspended member.
This Plan Is Not Insured by
the PBGC
Supplemental Retirement and
Savings Plan benefits are not guaran-
teed by the Pension Benefit Guaranty
Corporation (PBGC), which does not
cover plans such as this one with
individual accounts for each partici-
pant. Upon termination of the plan,
you would be eligible to receive the
total amount in your accounts.

Overview
Tuition Remission Program
94
T
he Tuition Remission Program provides regular full-time
employees with an outstanding education benefit. You and
your family can take advantage of a wide range of courses and
degree programs offered by the University.
Eligibility for benefits for you begin on the first day of the semester
on or following your date of hire.
Eligibility for benefits for your spouse and dependent children begin
on the first day of the semester after you have completed the
appropriate service requirements.
95
Eligibility
If you are a regular full-time employee
and have an appointment of nine
months’ or more duration you, your
spouse, and your dependent chil-
dren are eligible to participate in
the Tuition Remission Program.
Your eligible dependent children are
those whom you claim as exemp-
tions on your federal income tax
return during the calendar years in
which they are enrolled in under-
graduate degree programs at Boston
University. They include:
Your unmarried dependent
children or stepchildren
Certain age limits apply to eligible
dependent children (see “Benefits
for Your Dependent Children”).
How the Program Works
What Is Covered The Tuition Remis -
s ion Program covers undergraduate
and graduate courses taken by you
or your spouse and undergraduate
courses taken by your dependent
children.
The Tuition Remission Program
applies only to courses offered by
Boston University. No assistance is
provided for courses taken at other
colleges or universities.
When to Apply Once you have regis-
tered for your class(es), if you would
like to apply for the tuition remission
benefit for yourself, your spouse, or
your unmarried dependent children,
you may apply online at Employee
Self Service at BUworks Central
at www.bu.edu/buworkscentral.
Alternatively, you may complete a
Benefits Enrollment Form available
at www.bu.edu/hr/home/forms/
benefit-forms.
Upon request, paper forms will also
be mailed directly to you by the
Benefits Section of Human Resources.
Completed paper forms must be
returned to Human Resources at 25
Buick Street. You need only use one
method of application—online or
paper—not both.
Covered students under the Tuition
Remission Program (employees,
spouses, or children) register for
classes separately through the
Registrar’s Office and then receive
credit from the Tuition Remission
Program on their student accounts
for approved credit hours.
How Approval Works Employees,
spouses, and children receiving ben-
efits are registered for classes on a
space-available basis.
Participating employees, spouses, or
dependents are responsible for meet-
ing admission requirements or pre-
requisites for any course or program.
Tuition Remission Does Not Cover
Fees and Other Expenses, (e.g., Books,
Lab Fees, Etc.) Registration fees and
other fees, except the Continuing
Student Fee, must be paid by cov-
ered students when they register for
courses as those fees and expenses
are not covered by tuition remission.
Covered students must also pay for
their books, lab fees, late fees, and
any necessary classroom materials
as those fees and expenses are not
covered by tuition remission. Tuition
remission also does not cover room
and board.
Tuition Remission Benefits
Tuition remission benefits are
granted on a semester basis. For the
purposes of the program, the two
summer sessions are treated as one
academic semester.
If a service requirement applies to
the tuition remission benefits for
your spouse or dependent children,
only continuous and full-time service
with Boston University is counted
toward fulfilling that requirement.
Such service is measured from
the date you become an eligible
employee (see prior “Eligibility” sec-
tion) up to and including the first day
instruction begins.
Full-time employees are only eli-
gible to receive tuition remission
benefits as “employees.” It is Boston
University’s policy that if you are a
full-time regular employee you may
not be enrolled at Boston University
as a full-time student. Full-time
student status is 12 or more cred-
its. If you are a full-time regular
employee, you are not eligible for
benefits as a spouse or dependent
of another employee.
An explanation of the benefits avail-
able to you, your spouse, and your
dependent children follows.
Benefits for You
If you were hired on or before
July 1, 1981 As an eligible employee
you are entitled to 100% tuition
remission for up to 8 credit hours
of courses you take each semester.
This includes graduate and under-
graduate courses (see discussion
below regarding the taxability of
graduate courses).
If your employment ends before the
first day instruction begins*, you will
be required to pay the full tuition for
all courses taken that semester.
Tuition Remission Program

96
If your employment ends after the
first day instruction begins*, but
before the final exam end date** for
the semester, your benefits will con-
tinue until the end of the semester.
If you were hired on or before June
30, 1985, but after July 1, 1981 As an
eligible employee you are entitled
to 100% tuition remission for the
first 4 credit hours and 90% tuition
remission for the next 4 credit hours
of courses you take each semester.
This includes graduate and under-
graduate courses.
If your employment ends before the
first day instruction begins*, you will
be required to pay the full tuition for
all courses taken that semester.
If your employment ends after the
first day instruction begins*, but
before the final exam end date** for
the semester, your benefits will con-
tinue until the end of the semester.
If you were hired on or after July 1,
1985 As an eligible employee you
are entitled to 100% tuition remis-
sion for the first 4 credit hours and
90% tuition remission for the next
4 credit hours of courses you take
each semester. This includes gradu-
ate or undergraduate courses.
If your employment ends before the
final exam end date or the end of
session date** for the semester, you
will be required to pay full tuition
for all courses taken that semester.
If you are involuntarily terminated
from your position, no payment will
be due.
The first day “instruction begins” for
the semester is defined as the date pub-
lished in the Boston University Office
of the University Registrar Official
Academic Calendar: Charles River.
The “final exam end” date or the “end of
session” date for the semester is defined as
the date published in the Boston University
Office of the University Registrar Official
Service Requirement
Your spouse will be eligible for
tuition remission benefits once you
have completed 12 months of eligible
service (i.e., continuous and full-time
service) at Boston University.
If you and your spouse are both
employed at Boston University and
are both eligible for tuition remis-
sion benefits, you and your spouse
are individually eligible to receive
tuition remission as employees. You
and your spouse are not eligible to
receive benefits as a spouse.
Benefits for Your Dependent
Children
Once you have satisfied the service
requirement described below, each
of your eligible unmarried depen-
dent children may take up to eight
semesters through the tuition
remission Program, as long as they
apply, are admitted to, and are
enrolled in undergraduate degree
programs at Boston University or
as seniors at Boston University
Academy. The amount of tuition
remission benefits granted for
their courses depends upon your
length of eligible service with the
University. Tuition remission is not
available for any graduate courses
taken by dependent children.
If your employment ends before the
first day of classes, your dependent
will be required to pay full tuition for
the courses taken that semester. If
your employment ends before the
last day of classes, your dependent’s
benefits will continue until the end
of the semester.
Service Requirements
Your unmarried dependent children
may receive 50% tuition remission
for courses taken once you have
completed four months of eligible
Academic Calendar: Charles River. For the
fall and spring semesters, it is the “final
exam end date”; for summer session, it is
the Summer II “end of session” date.
Courses Scheduled During Work Hours
If a course you want to take is sched-
uled during normal working hours,
you must have your department chair
or supervisor sign your tuition remis-
sion form in order for the benefit to
be approved. The University reserves
the right to refuse to allow you to
attend a class under the Tuition
Remission Program if it conflicts with
the needs of your department.
You must report all courses taken,
not only courses covered by the
Tuition Remission Program, to
determine if there is a conflict with
the needs of your department.
You will not receive pay while
attending a class during scheduled
work hours.
If you are taking more than 8 cred-
its, you must have the approval of
the Dean or Vice President for your
unit before applying for the benefit.
Benefits for Your Spouse
Once you have satisfied the service
requirement described below, your
spouse will be granted 50% tuition
remission each semester for all
courses taken at Boston University.
This includes graduate and under-
graduate courses.
If your employment ends before the
first day of class, your spouse will
be required to pay full tuition for the
courses taken that semester. If your
employment ends before the last day
of classes, your spouse’s benefits
will continue until the end of the
semester.
*
**

97
service (i.e., continuous and full-
time service) and:
If you were hired prior to January 1,
1995, they may receive 100% tuition
remission for courses taken after
you have completed 16 months of
eligible service.
If you were hired on or after January 1,
1995, they may receive 90% tuition
remission for courses taken after
you have completed 16 months of
eligible service.
In the event your unmarried depen-
dent children have received eight
semesters of tuition remission ben-
efits and need an additional semes-
ter to complete their undergraduate
studies, it may be possible to repay
the University for one semester of
tuition remission benefits that were
previously received in exchange
for tuition remission benefits for a
prospective semester. Please con-
tact the Benefits Section of Human
Resources for additional information
regarding this provision.
Proof of Relationship Requirement
Full-time employees are only eligible
to receive tuition remission benefits
as an employee. You are not eligible
for additional benefits as a depen-
dent child of another employee eli-
gible for tuition remission benefits.
Proof of relationship to the employee
must be provided for eligible
unmarried dependent children. The
employee must provide the following:
• A copy of the dependent’s
birth certificate, or
• A copy of the adoption
certification, or
• A copy of the most recent tax
return listing your dependent(s)
These documents will be kept in
confidential files in the Benefits
Section of Human Resources.
Age Limit for Dependent Children
Dependent children are no longer
eligible for benefits under this pro-
gram after the end of the semester
in which they reach age 27. The
exceptions to this provision are:
Military Service For unmarried
dependent children who are honor-
ably discharged veterans, the period
of eligibility will be extended beyond
age 27 by the number of months of
their military service, up to a maxi-
mum of 48 months.
Disability Dependent children whose
disabilities prevent them from com-
pleting undergraduate work within
eight semesters by the time they
reach age 27, must submit a written
request for an extension of tuition
remission eligibility to the Benefits
Section of Human Resources. A
physician’s statement indicating
diagnosis, period of disability, and
prognosis must accompany the
request, along with a letter of recom-
mendation from Boston University’s
Disability Services regarding the stu-
dent status of your dependent child.
Special Provisions Protecting Benefits
for Dependent Children
Once Your Dependent Children Begin
Receiving Benefits If you retire
from the University at age 55 or
later and have completed 10 or
more years of continuous full-time
service with the University after
age 45, your eligible unmarried
dependent children may continue
to receive tuition remission ben-
efits in an undergraduate degree
program at the University pursuant
to terms specified herein.
If you should die while employed at
the University, or are receiving dis-
ability benefits from the University’s
Long-Term Disability Plan, your
eligible unmarried dependent
children may continue to receive
tuition remission benefits through
the semester in which your death
occurred, subject to the Program’s
limits, as long as they remain eligible.
In subsequent semesters, your years
of continuous full-time service up to
the time when you became disabled
or died, will be used to determine the
number of additional semesters up
to a maximum of eight semesters for
which each child is eligible in accor-
dance with the following table:
For example, if you died with 10 or
more years of continuous full-time
service with Boston University
and at the time of your death, your
dependent child had received six
semesters of tuition remission, he
or she would be eligible for two
more semesters of tuition remis-
sion, for a maximum of eight
semesters.
Before Your Dependent Children Begin
Receiving Benefits If you retire from
the University at age 55 or later and
have completed 10 or more years
of continuous full-time service with
the University after age 45, the
University will provide your eligible
unmarried dependent children with
eight semesters of tuition remission
benefits in an undergraduate degree
program at the University pursuant
to terms specified herein.
If you should die while employed
at the University, or are receiv-
ing disability benefits from the
University Long-Term Disability
Plan, the University will provide
your eligible unmarried dependent
Employee’s years of Number of
continuous full-time semesters
service per child
3 but less than 6 2
6 but less than 9 4
9 but less than 10 6
10 or more 8

98
children with up to eight semesters
of tuition remission benefits in an
undergraduate degree program at
the University depending upon your
years of continuous full-time service
at the point of your disability or
death, in accordance with the fol-
lowing table:
Benefits During Authorized
Absences from Work
The following applies to tuition
remission benefits for you, your
spouse, and your dependent chil-
dren while you are on an approved
leave of absence or sabbatical.
Paid Leaves of Absence and Sabbaticals
Tuition remission benefits con-
tinue while you are on an approved
leave of absence with pay. Tuition
remission benefits also continue
if you are a faculty member on an
approved sabbatical with pay. The
period of time you are on leave
of absence or sabbatical counts
toward any service requirements
specified in the program.
Unpaid Leaves of Absence
With prior approval from Human
Resources, tuition remission ben-
efits may be continued during an
approved unpaid leave of absence
that is taken for one of the following
reasons:
1. Research purposes
2. Instruction
3. Government or other service
deemed by the University to
be in the public interest
4. Other activities as may be
approved by the University
If you take an approved leave of
absence without pay for any reason
other than those explained above,
tuition remission benefits will termi-
nate for the duration of your leave
on the earlier of the following dates:
1. The beginning of a semester fol-
lowing or coincident with the
first day of your leave; or
2. At the end of any semester in
which you begin your leave.
While you are on approved leave
of absence without pay, you can
accrue service (up to 24 months)
toward meeting the Program’s
service requirement.
Extended Military Leave
If you go on an extended military
leave, you will accrue service
toward meeting the Program’s
service requirements for the entire
period of the leave, provided you
return to regular, full-time employ-
ment with the University following
military service and within the time
when your veteran’s re-employ-
ment rights are protected.
Medical Leave of Absence
During an approved leave of
absence due to temporary dis-
ability, benefits continue for your
dependent children until the end of
a semester in which you complete
six months of such leave with-
out pay. You can accrue up to six
months of service toward meeting
the Program’s service requirements
while on a temporary disability.
Boston University Courses
Excluded from the Tuition
Remission Program
Benefits are not granted for
the following:
• Applied music fees
• Courses offered through the
School of Medicine (except for
courses offered in the Division
of Graduate Medical Sciences
and master’s degree program
courses in the School of Public
Health)
• Courses offered through the
Goldman School of Dental
Medicine
• Courses offered for all execu-
tive graduate programs, such
as the Executive Master of
Business Administration,
the Executive Engineering
Program, the Executive Master
of Science in Investment
Management Program, and the
Executive Master in Business
Administration in Health Care
• Courses offered for the
Accelerated Master of Human
Resource Education
• Non-credit courses or courses
awarding Continuing Ed Units
(CEUs)
• Online courses
• Room, board, and non-tuition
portion of study abroad program
(for example, air fare and books)
• Courses not offered for credit,
such as the courses offered at
the Center for English Language
& Orientation Programs,
Continuing Education, and
some Certificate Programs at
Metropolitan College.
Employee’s years of Number of
continuous full-time semesters
service per child
3 but less than 6 2
6 but less than 9 4
9 but less than 10 6
10 or more 8
99
Income Tax Considerations
The tuition remission benefits you,
your spouse, or your dependent chil-
dren receive may be subject to fed-
eral income taxes, Massachusetts
state income taxes, and FICA taxes.
Under current tax laws, the follow-
ing provisions apply:
Under current tax law effective
January 1, 2002, up to $5,250 in
value for graduate tuition remis-
sion benefits for employees are,
generally, not considered taxable
income. Graduate tuition remission
in excess of $5,250 per calendar
year for employees and all gradu-
ate tuition remission benefits for
spouses are generally subject to
federal, state, and FICA taxation.
Tuition remission benefits for
undergraduate courses are gener-
ally tax-free.
Due to nearly continuous changes
in the tax laws, please contact
the Benefits Section of Human
Resources for the current status
concerning the taxability of tuition
remission benefits. You may also
want to consult with a tax advisor.
Administrative Information
About the Program
Type of Program
The Boston University Tuition
Remission Program is an unfunded
educational assistance program. It
is not subject to the provisions of
the Employment Retirement Income
Security Act (ERISA) of 1974. Any
determinations by Boston University
regarding eligibility for the Tuition
Remission Program or benefits
thereunder are final, binding, and
conclusive.
Program Amendment or
Termination
Boston University intends to con-
tinue the Tuition Remission Program
indefinitely; however, the University
reserves the right in its discretion to
amend, suspend, or terminate the
program at any time.
For Additional Information
For additional information concern-
ing the Tuition Remission Program,
contact the Benefits Section of
Human Resources.

Tuition Exchange Program
102
B
oston University is a member of the Tuition Exchange Program,
Inc. (TE), a national organization that administers tuition scholar-
ships for dependent children of employees from member colleges and
universities.
Each year Boston University’s agreement with the Tuition Exchange
Program, Inc. permits up to 10 students who are planning to enter their
first year of college the following academic year to enroll in undergradu-
ate degree programs at over 580 participating colleges and universities
located in 46 states and the United Kingdom.

103
Eligibility
Your dependent children are eligible
to apply to participate in the Tuition
Exchange Program if you are a
regular full-time employee with an
appointment of nine months’ or
more duration, and if you will have
completed at least 16 months of
service prior to the start of the fall
semester at Boston University. Only
one dependent per family may par-
ticipate in the program at a time.
Your eligible dependent children are
those whom you claim as exemp-
tions on your federal income tax
return during the calendar years in
which they are enrolled in under-
graduate degree programs through
the Tuition Exchange Program. Only
your unmarried dependent children
or stepchildren who are under age
27 qualify for this program.
Your dependent children are not
eligible for additional benefits as a
dependent child of another employee
eligible for Tuition Exchange benefits.
Proof of Relationship Requirement
Proof of relationship to the
employee must be provided for
eligible unmarried dependent chil-
dren. The employee must provide
the following:
• A copy of the dependent’s birth
certificate, or
• A copy of the adoption
certification, or
• A copy of the most recent tax
return listing your dependent
These documents will be kept in
confidential files in the Benefits
Section of Human Resources.
Age Limit for Dependent Children
Dependent children are no longer
eligible for benefits under this pro-
gram after the end of the semester
in which they reach age 27. The
exceptions to this provision are:
Military Service For unmarried
dependent children who are honor-
ably discharged veterans, the period
of eligibility will be extended beyond
age 27 by the number of months of
their military service, up to a maxi-
mum of 48 months.
How the Program Works
Students must be admitted as full-
time undergraduate degree candi-
dates at Tuition Exchange member
institutions in order to be eligible for
this program.
All students must apply to the insti-
tution in which the dependent child
is interested and meet all admis-
sions criteria of the admitting insti-
tution. Scholarships are available for
a maximum of four years (8 semes-
ters/12 trimesters) of full-time
academic study in an undergraduate
degree program. Summer sessions
are excluded from this scholarship.
Enrollment must be re-certified
annually. This means that you
must maintain eligibility for Tuition
Exchange benefits at Boston
University for the full duration of
the scholarship period in order to
receive full benefits under the Tuition
Exchange Program.
Once you have satisfied the Boston
University service requirement
described above, each of your eli-
gible unmarried dependent children
may take up to 8 semesters or 12
trimesters through the Tuition
Exchange Program, as long as they
apply, are admitted to, and are
enrolled in an undergraduate degree
program at a participating Tuition
Exchange institution. However, only
one of your dependent children may
participate in the Tuition Exchange
Program at any given time.
Having a child participate in the
Tuition Exchange Program does
not preclude your other child(ren)
from participating in the Tuition
Remission Plan at Boston University,
at the same time.
Boston University will award up to
10 new Tuition Exchange scholar-
ships for undergraduate education
in each academic year. Each schol-
arship is awarded for a maximum
of 8 semesters or 12 trimesters to
cover four academic years of full-
time undergraduate study at partici-
pating Tuition Exchange institutions.
Because the University must balance
the number of Tuition Exchange stu-
dents it “exports” to other member
institutions with those it “imports”
for enrollment at Boston University,
the number of scholarships avail-
able for eligible dependents of
Boston University employees in any
academic year is limited. Tuition
Exchange scholarship availability
is dependent on the availability of
spaces at the admitting institution.
The maximum semesters available
for Tuition Exchange benefits are
aggregated with Tuition Remission
benefits received at Boston
University. Therefore, your eligible
dependent child may not receive
more than 8 semesters/12 trimes-
ters of combined Tuition Remission
and Tuition Exchange benefits.
Tuition Exchange Program

104
If your employment ends before
the first day of classes, and your
dependent elects to enroll or con-
tinue enrollment at a participating
institution, your dependent will be
responsible for the full tuition for
the courses taken that semester,
as determined by the admitting
institution. If your employment ends
before the last day of classes during
a given semester, your dependent’s
benefits will continue until the end
of that semester.
Scholarship Amount
Each Tuition Exchange member
institution determines the value of
the scholarship it awards to each
incoming student and records this
on the Tuition Exchange Scholarship
Certification Form. Benefits vary
by member institution. There is a
minimum amount set by the Tuition
Exchange, Inc. ($31,500 for the
2013/2014 academic year). Schools
with tuition rates higher than this
amount may opt to award only the
minimum. Students are responsible
for any costs which exceed the
awarded benefit level.
How to Apply for Tuition
Exchange Benefits
1. Review the list of Tuition Exchange
institutions available at the
Tuition Exchange, Inc. website
at www.tuitionexchange.org.
2. Complete and submit the Boston
University Tuition Exchange
Preliminary Application to Human
Resources. This application must
be received by Human Resources
no later than the deadline prior
to the beginning of the academic
year for which you are apply-
ing. Example: Applications for
fall 2014 must be received by
December 16, 2013.
3. Tuition Exchange scholarship
candidates must apply for admis-
sion to each member institution
they wish to attend and complete
any financial assistance docu-
ments required by that institution.
Selection Process
Up to 10 dependent children who are
planning to enter their first year of
college the following academic year
will be selected from the applicant
group each academic year as can-
didates eligible to apply for Tuition
Exchange scholarships. Applicant
decisions will be made following
review of the application submitted
by the deadline. All eligible appli-
cants will be notified of their status
no later than December 21.
First priority will be given to appli-
cants whose sponsoring employee has
the greatest length of employment
service at Boston University. Length
of service is based on years of con-
tinuous full-time service at Boston
University. Among the applicants
whose sponsoring employees have
the same length of continuous ser-
vice, priority will be determined by
whether another dependent of the
employee has used the scholarship.
If all selection criteria are equal,
a lottery system will be used.
Applicants who are not selected will
be placed on a wait list using length
of service and will be notified if an
opening becomes available.
Once a Tuition Exchange scholar-
ship has been awarded, enrollment
must be re-certified annually by the
Boston University Tuition Exchange
Liaison Officer. Certification must
be confirmed for returning students
no later than January 15 prior to
the beginning of the next academic
year. Renewing Tuition Exchange
students must meet all required
academic and behavioral standards
of the admitting institution to qual-
ify for re-certification.
Completion of the application form
for participation in the Tuition
Exchange Program does not guar-
antee selection as a candidate,
nor admission to the selected
participating institutions. Selection
as a candidate eligible to receive a
Tuition Exchange scholarship also
does not guarantee final selection
as a Tuition Exchange scholarship
recipient. Final selection is deter-
mined by the Tuition Exchange
member institution. Your depen-
dent children must meet admis-
sion requirements of participating
Tuition Exchange institutions and
are subject to all academic rules,
regulations, and fees which may
apply. They must also be accepted
by the Tuition Exchange institution
as an “import” student eligible for a
Tuition Exchange scholarship.
In the event that any or all of the top
qualified applicants are unable to
enroll at an institution participating
in the Tuition Exchange Program in
the year of application, eligibility will
be offered to applicants on the wait
list.
Special Provisions Protecting Benefits
for Dependent Children
Once Your
Dependent Children Begin Receiving
Benefits If you retire from the
University at age 55 or later and
have completed 10 or more years of
continuous full-time service with the
University after age 45, your eligible
unmarried dependent children may
continue to receive tuition exchange
benefits in an undergraduate degree
program pursuant to terms speci-
fied herein.
If you should die while employed at
the University, or are receiving dis-
ability benefits from the University’s
Long-Term Disability Plan, your eli-
gible unmarried dependent children
may continue to receive Tuition
Exchange benefits through the
semester subject to the program’s

105
limits, as long as they remain eligi-
ble. In subsequent semesters, your
years of continuous full-time service
up to the time when you became
disabled or die will be used to
determine the number of additional
semesters, up to a maximum of 8
semesters/12 trimesters, for which
each child is eligible in accordance
with the following table:
Paid Leaves of Absence and Sabbaticals
Tuition Exchange benefits continue
while you are on an approved
leave of absence with pay. Tuition
Exchange benefits also continue
if you are a faculty member on an
approved sabbatical with pay. In
addition, the period of time you are
on leave of absence or sabbatical will
count toward any service require-
ments specified in the program.
Administrative Information
About the Program
Type of Program
The Boston University Tuition
Exchange Program is an unfunded
educational assistance program. It
is not subject to the provisions of
the Employment Retirement Income
Security Act (ERISA) of 1974.
Program Amendment or Termination
Boston University intends to con-
tinue the Tuition Exchange Program
indefinitely; however, the University
reserves the right in its discretion to
amend, suspend, or terminate the
program at any time.
For Additional Information
For additional information concern-
ing the Tuition Exchange Program,
contact the Benefits Section of
Human Resources.
Employee’s years of Number of
continuous full-time semesters
service per child
3 but less than 6 2
6 but less than 9 4
9 but less than 10 6
10 or more 8

Flexible Benefits Program &
Flexible Spending Accounts
108
T
he Flexible Benefits Program offers you a substantial tax savings
opportunity. It allows you to pay for eligible expenses using tax-
free dollars—money taken out of your paycheck before income or Social
Security taxes have been deducted.
The Flexible Benefits Program has three components:
• Automatic Before-Tax Health Care and Accident Insurance Contributions
If you enroll in the Boston University Health Plan, the Boston
University Dental Health Plan, or elect coverage under the Personal
and Family Accident Insurance Plan, your share of the cost for these
plans will automatically be deducted from your paycheck on a before-
tax basis.
• Flexible Spending Account—Dependent Care This account allows you to
set aside before-tax dollars to help pay for day care services for your
eligible dependents.
• Flexible Spending Account—Health Care This account allows you to set
aside before-tax dollars to help pay for certain uninsured health care
expenses.
Because of its tax-exempt features, the Flexible Benefits Program is strictly
regulated by the federal government. If you would like to participate in the
program, please read this section carefully, and also discuss how the pro-
gram may benefit you with your own tax advisor or financial planner.
109
Eligibility
You are eligible to participate in the
Flexible Benefits Program if you are
a regular employee of the University
and your annual base salary is
$10,000 or more.
How the Program Works
The Flexible Benefits Program
allows you to use your annual base
salary to your best advantage.
It offers the following components:
• Automatic Before-Tax Health,
Dental, and Accident Insurance
Contributions If you participate
in the Boston University Health
Plan, the Boston University
Dental Health Plan, or elect
coverage under the Personal
and Family Accident Insurance
Plan, you will automatically pay
your insurance premiums with
before-tax dollars. The Flexible
Benefits Program does not
change the eligibility, benefits,
or other features of those plans;
it just offers a way to pay the
required employee premiums on
a before-tax basis. (For informa-
tion concerning these plans, read
the “Health Plan,”“Dental Plan,”
and “Survivor” sections of this
handbook.)
• Flexible Spending Account—
Dependent Care This voluntary
reimbursement account is
designed to help you pay for
the cost of care for your eligible
dependents.
• Flexible Spending Account—Health
Care This voluntary reimburse-
ment account is designed to help
you pay for the cost of health
care expenses not covered by a
group insurance plan.
Under current tax laws, contri-
butions to the Flexible Benefits
Program are free from federal
income taxes, state income taxes,
and Social Security taxes.
Participation
Automatic Before-Tax Health,
Dental, and Accident Insurance
Contributions
If you elect coverage under any of
the previously mentioned health,
dental, and survivor insurance plans,
your participation in this component
of the Flexible Benefits Program is
automatic. This means that your
premium payments will be deducted
from your paycheck using before-
tax dollars.
Dependent and Health Care
Flexible Spending Accounts (FSAs)
Participation in these accounts is
voluntary. You can choose to enroll
in one or both. After you enroll, a
dependent care reimbursement
account and/or a health care
reimbursement account will be
established in your name and your
contributions will be taken from
your salary, using before-tax dollars.
Enrollment
Automatic Before-Tax Health and
Accident Insurance Contributions
You enroll in the Automatic Before-
Tax Health, Dental, and Accident
Insurance Contributions component
of the Flexible Benefits Program at
the same time you enroll in group
coverage under the eligible health,
dental, and accident insurance
plans. Enrollment forms are avail-
able from the Benefits Section of
Human Resources.
Flexible Spending Accounts (FSAs)
The open enrollment period for
these accounts will be held each
year from mid-November to mid-
December or such earlier period as
the Plan Administrator may specify.
If you enroll during an open enroll-
ment period, your participation will
become effective on the following
January 1. If you are hired after the
close of an open enrollment period,
you will have 30 days from your
benefit orientation date to enroll.
In both cases, participation will
continue through the following plan
year:
• FSA—Dependent Care
Plan Year—January 1 to
December 31
• FSA—Health Care Plan Year—
January 1 to March 15
of following year
When you complete a Flexible
Spending Account enrollment, you
must indicate the total amount of
money you wish to put into the
account during the plan year.
Once you have enrolled, your
choices remain in effect until the
next open enrollment period, unless:
• There is a Qualified Change in
your family or employment
status (examples of quali-
fied changes are listed under
“Changing or Stopping Your
Contributions”), or
• You become ineligible to par-
ticipate in the Flexible Benefits
Program for any reason.
Flexible Benefits Program
& Flexible Spending Accounts

110
Contributions
Before-Tax Health, Dental, and
Accident Insurance Contributions
Your contributions are your portion
of the cost for your coverage under
the health, dental, and accident
insurance plans you elect. Maximum
contributions under this component
of the Flexible Benefits Program are
the sum of your monthly premiums
for the plan year.
Flexible Spending Account (FSA)
Contributions
You may contribute up to $5,000 to
the FSA—Dependent Care and up
to $5,000 to the FSA—Health Care.
(Beginning in 2013, the maximum
will be reduced to $2,500 for FSA—
Health Care.) However, tax law rules
may limit your FSA—Dependent
Care maximum (see the heading
“Maximum Contributions” later in
this section).
Changing or Stopping
Your Contributions
Under current IRS regulations, you
may change your participation sta-
tus in the Flexible Benefits Program
only during the annual open enroll-
ment period or as the result of a
Qualified Change in your family or
employment status.
Qualified Changes include:
• Marriage
• Birth or adoption of a child
• Start or loss of your spouse’s
employment
• Change in employment status
(for you or your spouse)
from part-time to full-time or
from full-time to part-time
• Divorce
• Death of your spouse or
other dependent
• Retirement
• Your death
• Leave of absence or sabbatical
for you or your spouse
• Termination of your employment
with Boston University
The change in your participation or
contributions must be because of
and consistent with the Qualified
Change and must meet all IRS
requirements for changing your
election. You may not change from
one health plan option to another
at any time other than the annual
Open Enrollment Period. You will
have 30 days from the date the
Qualified Change occurs to notify
the Benefits Section of Human
Resources and make any changes.
Your change will generally become
effective on the effective date of the
qualifying event except as otherwise
required by law.
Tax Advantages of the Program
The Flexible Benefits Program pro-
vides an opportunity for you to pay
eligible health and dependent care
expenses on a before-tax basis.
• Advantages for Dependent Care
Expenses Under the Internal
Revenue Code, you can obtain
a tax advantage for dependent
care expenses by paying for
them with the tax-free dol-
lars you put into your FSA—
Dependent Care or by claiming
them as a tax credit on your fed-
eral income tax return forms.
You Cannot Use Both Methods
for the Same Expenses The
amount you contribute to a FSA
—Dependent Care will reduce,
dollar-for-dollar, the amount you
may claim as a tax credit. Consult
a tax advisor for details.
If You Pay Federal Income Taxes,
Social Security Taxes, and
Massachusetts State Income
Taxes In many cases, the FSA—
Dependent Care will be more
advantageous than the federal
dependent care tax credit,
depending upon income level and
number of dependents.
We encourage you to talk
to a tax advisor to help you
determine whether the FSA—
Dependent Care or the federal
dependent care tax credit is
more advantageous to you.
• Advantages for Health Care
Expenses The FSA—Health
Care will be appropriate for you
if you expect to have eligible
uninsured medical expenses
below 7.5% of your adjusted
gross income in the coming
calendar year. Expenses below
this level are not deductible for
federal income tax purposes.
As a result, the FSA—Health
Care may offer you an advantage
which you cannot duplicate on
your tax return.
Of course, your own tax situation
will dictate exactly what the
Flexible Spending Accounts can
do for you. For more specific
information about how these
Flexible Spending Accounts may
apply to you, we encourage you
to talk to a tax advisor.
Potential Impact on Your Social
Security Income
Your participation in the Flexible
Benefits Program will have the effect
of reducing your Social Security
taxable wages by the value of your
designated salary reduction amount.
This results in an immediate tax
savings to you. It could also serve to
reduce your future Social Security
benefits.

111
How Flexible Spending
Accounts Work
• You estimate what your unin-
sured medical and/or depen-
dent care expenses will be for
the coming year, and designate
that amount on the appropriate
enrollment form. You should
estimate conservatively because
amounts not used for eligible
expenses during a plan year
must be forfeited (this is an IRS
rule).
• The amount you elect to contrib-
ute will come out of your pay-
check in equal installments for
the number of pay periods you
designate.
• The portion of your salary that
goes into an account will not
count as taxable income, so you
have an immediate tax savings.
• When you have an eligible
expense, you file a claim to get
reimbursed. You are responsible
for paying providers; reimburse-
ment checks will be made out in
your name.
• Under federal law, if you make
contributions to a reimburse-
ment account which are not
used to pay for eligible expenses
incurred during that plan year,
you will forfeit the unused bal-
ance after the end of the plan
year.
• Also, expenses incurred before
your participation commences
or after you cease participation
cannot be reimbursed.
Account Statements
Reports showing your current
account balance will be issued peri-
odically. You should monitor your
account closely toward the end of
each plan year.
How to File a Claim
Claims for reimbursement may be
filed at any time and must repre-
sent expenses incurred during the
current plan year while you were
participating in the Plan. Expenses
incurred before you enroll cannot
be reimbursed. A claim is “incurred”
when the services relating to that
claim were provided.
Claim forms are available from
the Benefits Section of Human
Resources or from the website at
www.bu.edu/hr/home/forms/
benefit-forms. When you complete
a claim form, include any informa-
tion or documentation required for
the verification of health or depen-
dent care expenses. You must sub-
mit an original invoice, or if you have
paid in advance, an original receipt
with your claim form.
Claim forms received by the 10th
of a month will be processed that
month. You will be reimbursed in the
last paycheck of the month in which
your claim form was received.
• For dependent care expenses, you
will be reimbursed up to the bal-
ance in your account at the time
your claim is submitted. If the
expenses you submit are greater
than your account balance,
you will be reimbursed up to
your account balance. Qualified
expenses that were submitted
but not paid will be carried over
to the next month, and an addi-
tional payment will be issued to
you during the next regular pro-
cessing cycle.
• For health care expenses, you can
be reimbursed up to the amount
you choose to contribute (reduced
by any prior reimbursements for
the plan year).
Treatment of Year-End Expenses You
have until March 31 following the
end of a given plan year to sub-
mit claims for reimbursement of
expenses incurred during that plan
year. Account balances remain-
ing after that date will, by law, be
forfeited. You may not use current
plan year account balances to pay
for expenses incurred in a prior plan
year. Prior plan year expenses must
be paid with prior plan year account
balances. Also, unused amounts
cannot be carried over and used to
reimburse expenses incurred in a
later year.
If You Should Leave Boston University:
• FSA—Dependent Care You
may continue to submit claims
for reimbursement of eli-
gible dependent care expenses
incurred through the last day
of your employment at Boston
University. However, such claims
must be submitted no later than
March 31 following the end of
that calendar year. Any account
balances remaining after that
date will, by law, be forfeited.
• FSA—Health Care In certain
circumstances, you may elect
to continue your participation
in your account through federal
health care coverage continu-
ation provisions under COBRA
but only to the extent required
by COBRA. To do so, you must
make your election within 60
days after the end of the month
in which you leave Boston
University. If you elect to con-
tinue your participation, your
contributions will be made with
after-tax dollars.
If you elect to discontinue your
participation, your account bal-
ance will be frozen as of the date
your employment ends. You
may continue to submit claims
for reimbursement of expenses
incurred through the last day
of your employment. However,
112
such claims must be submitted
no later than March 31 following
the end of that calendar year.
Any account balance remaining
after that date will, by law,
be forfeited.
If You Should Become Totally Disabled
or Die
You or your survivors may continue
to submit claims for expenses
incurred before the time of total
disability or death. However, such
claims must be submitted no later
than March 31 following the end of
that calendar year. Any account bal-
ances remaining after that date will,
by law, be forfeited.
Use of Forfeitures
Forfeited account balances will
remain part of the University’s
assets. Under no circumstances
may any forfeitures be used to
directly benefit any individual plan
participant.
Information to Remember
Flexible Spending Accounts have
some limitations. These limitations
are based on federal regulations
required because of the tax-exempt
feature of the accounts. For example:
• You must re-enroll in the
accounts during each annual
open enrollment period. You
do this by completing new
enrollment forms. If you do not
complete a new enrollment, your
participation in the accounts
will cease at the end of the plan
year, and you will not be able to
enroll again until the next open
enrollment period (unless there is
a Qualified Change in your family
status).
• Flexible Spending Accounts can
be used only for the purposes
for which they are set up—that
is, dependent care expenses or
health care expenses, respec-
tively.
• Your decisions regarding how
much money you will contrib-
ute to the accounts for the plan
year are fixed (unless there is a
Qualified Change in your family
status). You cannot choose to
stop, reduce, or increase your
contributions during the plan
year.
• If the full values of the accounts
are not used up during the plan
year, you forfeit the remaining
balances.
Because of the requirement to
forfeit any unused account bal-
ances, Flexible Spending Accounts
should be used only for predictable
expenses. You should, therefore,
estimate conservatively.
Following are specific details con-
cerning the Dependent and Health
Care Flexible Spending Accounts.
Flexible Spending Account—
Dependent Care
The FSA—Dependent Care is
designed to help you pay for the
cost of eligible expenses for the care
of qualified dependents incurred in
the calendar year during which and
while you participate in this plan. An
expense is “incurred” when the ser-
vices relating to that expense were
provided.
Because your individual situation
determines whether or not the
account is appropriate for you, we
urge you to consult a tax advisor
before enrolling in a FSA Dependent
Care.
Eligible Expenses cover Qualifying
Services to Qualifying Individuals.
Qualifying Services are work-
related dependent care services
performed in order for you and your
spouse, if you are married, to remain
employed or look for work.
Qualifying Services can be provided:
• In your home
• Outside of your home, provided
the dependent regularly spends
at least eight hours per day in
your household, or the depen-
dent is under 13 years of age
• By a dependent care center or
facility if it provides care to six or
more individuals (excluding resi-
dents of the center) and receives
a fee, payment, or grant for the
services. These services qualify
only if the center complies with
all the applicable state and
municipal laws and regulations.
You must make payments for child
and dependent care to someone you
(and your spouse) cannot claim as
a dependent. If you make payments
to your child, he or she cannot be
your dependent and must be age 19
or older by the end of the year. You
cannot make payments to:
a. Your spouse
b. The parent of your qualifying indi-
vidual if your qualifying individual
is your child and under age 13
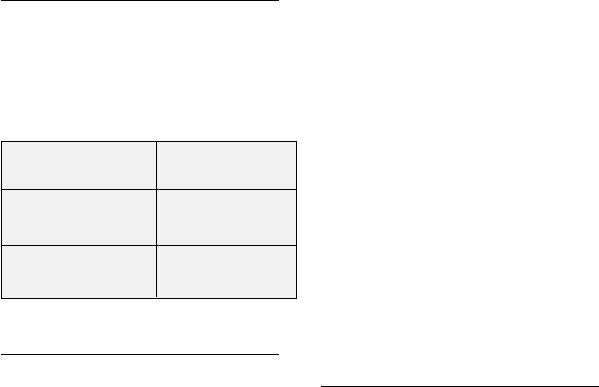
113
Child and dependent care expenses
must be work-related to qualify.
Expenses are considered work-
related only if both of the following
are true:
• They allow you (and your
spouse if you are married)
to work or look for work.
• They are for a qualifying
individual’s care.
Qualifying nursery school expenses
can be reimbursed, but kindergarten
and grade school tuition expenses
and the cost of overnight camp can-
not be.
If qualifying care is provided in
your home, the provider could be
a housekeeper, nanny, live-in, or
other individual, as long as his or her
primary job is to provide qualifying
dependent care services. In such
cases, eligible expenses may include
food and lodging for the caregiver.
Qualifying Individuals are:
1. Your qualifying child who is your
dependent and who was under
age 13 when the care was pro-
vided;
2. Your spouse who was not physi-
cally or mentally able to care for
himself or herself and lived with
you for more than half the year;
or
3. A person who was not physi-
cally or mentally able to care for
himself or herself, lived with you
for more than half the year, and
either:
a. Was your dependent, or
b. Would have been your depen-
dent except that:
i. He or she received gross income
of $3,500 or more,
ii. He or she filed a joint return, or
iii. You, or your spouse if filing
jointly, could be claimed as a
dependent on someone else’s
income tax return.
If You Are Divorced or Separated
If you are divorced or legally sepa-
rated, or if you and your spouse
lived apart for the last six months
of the calendar year, your children
under the age of 13 will generally
be considered your dependents if
you had custody of them for the
greater portion of that calendar
year. Consult your own tax advisor
for more information.
Maximum Contributions
Federal tax laws place limitations on
the amount you can contribute to
a FSA—Dependent Care each plan
year.
Other Contribution Limitations
1. If you are married, your contribu-
tions are limited to the least of
the following:
• Your earned income (after reduc-
tions in pay for contributions to
other benefit plans) for the plan
year; or your spouse’s earned
income for the plan year.
Under federal law, if your spouse
is not employed during a month
that you incur eligible dependent
care expenses, because he/she
is a full-time student or is totally
incapacitated, your spouse’s
earned income for that month
will be treated as being either:
• $250 if you incurred eligible
expenses for one Qualifying
Individual; or
• $500 if you incurred eligible
expenses for two or more
Qualifying Individuals.
2. If you are single, your contribu-
tions may not be in excess of
your earned income (after reduc-
tions in taxable pay for contribu-
tions to other benefit plans) for
the plan year.
3. The federal maximum contribu-
tion limit applies to contribu-
tions made to this and other
dependent care reimbursement
accounts you or your spouse
participate in during a given year.
Therefore, if you start working
at Boston University after the
beginning of the plan year and
would like to participate in the
Dependent Care Reimbursement
Account, you must consider
any contributions made to your
previous employer’s dependent
care plan when determining your
maximum contribution limit
for this account.
Filing Claims
You can be reimbursed from your
account once a month by filing a
claim form with the Benefits Section
of Human Resources.
You do not have to pay for eligible
dependent care expenses before
being reimbursed for them. However,
the Plan Administrator may ask you
to verify your claims and can with-
hold payment if you do not forward
the requested information.
Note: IRS regulations require substantia-
tion of claim.
Your maximum
If you are: contribution is:
Single or married
filing jointly $5,000
Married filing
separately $2,500
114
When you file claims for eligible
dependent care expenses, you must
include a Taxpayer Identification
Number (TIN) for each provider. An
individual’s TIN is typically his or her
Social Security number. Also, when
you file your tax return, you will
have to include a special form that
will include the name(s) and TIN(s)
of your caregiver(s). For additional
information concerning TINs, con-
tact the Benefits Section of Human
Resources.
If you file a claim and it is denied, in
whole or in part, you have a right to
appeal the denial. Information about
a denial of benefits is included in the
“Administrative Information” sec-
tion of this handbook.
Flexible Spending Account—
Health Care
The FSA—Health Care is designed
to help you pay for eligible health
care expenses incurred by you
and your dependents in the plan
year during which and while you
participate in this plan. A claim is
“incurred” when the services relat-
ing to that claim were provided.
Eligible Health Care Expenses
Before opening a FSA—Health Care,
you should be reasonably certain
you will have eligible health care
expenses during the year. As a
guideline for the amount you should
budget, you may wish to consider
your health plan deductibles and the
out-of-pocket expenses you might
have to pay during the year.
Eligible expenses are those that are
medically necessary and that are
not covered by insurance; these
generally include:
• Deductibles and coinsurance
• Unreimbursed dental care
expenses
• Orthodontic treatment
• Vision care expenses, including
eyeglasses and exams
• Routine physical exams
• Hearing aids and hearing care
expenses
• Prescription drugs
• Over-the-counter medications
for which you have a prescription
• Chiropractor services
• Osteopath services
• Podiatry services
• Medical equipment
• Acupuncture
• Nursing care
• Organ transplants
• Convalescent home expenses for
medical treatment
• Drug treatment center expenses
• Kidney donor expenses
• Institutional care required for a
health condition (not custodial
care only)
• Seeing Eye dog expenses
• Special expenses for physi-
cally and mentally handicapped
children
• Laboratory examinations
and tests
In addition, other health care
expenses considered tax deductible
under Section 213 of the Internal
Revenue Code may be eligible
for reimbursement through your
account (but health insurance
premiums are not eligible for reim-
bursement). However, any health
care expenses you have deducted
or intend to deduct on your income
tax return cannot be submitted for
reimbursement.
Maximum Contributions
You may elect to set aside any
amount in your FSA—Health Care
up to $2,500 a plan year.
Filing Claims
You can be reimbursed from
your account as often as once a
month by filing a claim form with
the necessary substantiation with
the Benefits Section of Human
Resources.
Note: IRS regulations require substantia-
tion of claim.
If you file a claim and it is denied in
whole or in part, you have a right
to appeal the denial. Information
about appealing a denial of benefits
is included in the “Administrative
Information” section of this hand-
book.

115
Leaves of Absence
If you leave work for any reason
for a prolonged period of time, you
should always contact the Benefits
Section of Human Resources to ask
what effect your absence may have
on your participation in this and
other University-sponsored benefit
plans.
• Leave of Absence with Pay If you
are granted a leave of absence
with pay, your participation will
continue, provided your usual
payroll deductions continue. If
you wish to discontinue your
participation, you may do so by
obtaining the necessary forms
from the Benefits Section of
Human Resources or from the
website at www.bu.edu/hr/
home/forms/benefit-forms/.
• Leave of Absence Without Pay
If you are granted a leave of
absence without pay, you may
continue your participation dur-
ing your leave with limitations.
The Benefits Section of Human
Resources will provide you with
the necessary information and
forms to either continue or dis-
continue participation in this
program during an unpaid leave
of absence.
When Your Program
Participation Ends
Your participation in the Flexible
Benefits Program ends the day your
employment with the University ter-
minates. It will also end when your
status as a regular employee ends
or, for the reimbursement accounts,
if you do not re-enroll during the
annual open enrollment period.
At that time you can be reimbursed
for eligible expenses that were
incurred before your date of ter-
mination of employment or other
termination of participation.
Closing Thoughts
The Flexible Benefits Program can be
a valuable tool in your financial plan-
ning. You can realize significant tax
savings by paying for eligible benefit
expenses with before-tax dollars.
Every effort will be made to help
you identify eligible expenses for
reimbursement; however, Boston
University cannot provide you
with legal or tax advice. Also, the
University will not be responsible if
the treatment of a reimbursement
amount is later challenged by the IRS.
The Flexible Benefits Program is
intended to qualify under Section
125 of the Internal Revenue Code
and other applicable Code Sections.
Boston University reserves the right
to modify or terminate the program
at any time (including a change in
the applicable tax laws).

Overview
Other Benefits
118
Y
ou have a variety of other benefits available as an employee
of Boston University. These include:
• Child Care Facilities
• DASH for Health
• Economic Security Planner
• Faculty/Staff Assistance Office
• Family Resources Office
• Fitness & Recreation Center
• Income Solutions
®
• New England Eye Benefit
• Personal Insurance Program
• QuitNet
• Real Estate Services
• Metro Credit Union
These benefits are provided to help you and your family live life to
its fullest, both personally and professionally.
Finally, the University contributes toward additional benefits
that have been established under state and federal statutes.
These statutory benefits include Social Security, Unemployment
Compensation, and Workers’ Compensation.
119
Child Care and Preschool
Education Programs
Boston University offers two child care
and preschool education programs:
• The Boston University Children’s
Center, Inc., has full-time and
part-time programs for children
two to six years old. For addi-
tional information and applica-
tion forms, contact:
The Director
Boston University Children’s
Center, Inc.
32 Harry Agganis Way
Boston, MA 02215
Phone: 617-353-3413
• The Early Childhood Learning
Lab, a nursery school for children
two years and nine months to
five years old, is operated by the
School of Education. Learning Lab
programs run morning sessions,
Monday through Friday. For addi-
tional information and application
forms, contact:
The Director
Early Childhood Learning Lab
Boston University School of
Education
605 Commonwealth Avenue
Boston, MA 02215
Phone: 617-353-3410
Space in both programs is lim-
ited. If you are interested in them,
we encourage you to talk to the
directors as early as possible.
DASH for Health
This program is designed to help
you eat better, exercise better, lose
weight, and lower blood pressure; it
was developed by physicians at BU
and Boston Medical Center.
What is DASH for Health?
DASH for Health is an online nutrition
and weight loss program that is FREE
to all Boston University employees
and up to three of their adult house-
hold members. Its aim is to help you
learn better eating and exercise habits
and it was designed right here at BU
by a team of doctors and nutrition-
ists lead by Dr. Tom Moore, on the
Medical Campus.
New information is provided on the
DASH website twice each week.
Articles cover food, food preparation,
eating out, losing weight, getting fit,
and much more. In addition to pro-
viding new information each week,
you have a web page especially for
you where you can track progress
in areas such as your weight, food
intake, blood pressure, and exercise.
The program has been tested with
several thousand people and there
is good evidence that people who
use the program successfully reduce
their weight, lower their blood pres-
sure, and improve their eating habits.
It’s recommended by the American
Heart Association.
DASH Eating
All nutrition advice is based on the
DASH Diet—a diet with more scien-
tific proof behind it than any other
eating plan. The DASH Diet is a well-
balanced, easy-to-understand way of
eating that gives you lots of choices,
and it is scientifically proven to help
you lose weight and lower blood
pressure and cholesterol levels.
How do I Enroll?
To learn more about DASH for Health,
go to www.bu.edu/hr/benefits/
health-wellness/dash-for-health
and enter your BU username and
Kerberos password. You will see
the link that will connect you to the
DASH for Health website where you
can take a tour of the program and
get more information about enrolling.
Economic Security Planner
Free for Boston University
Employees—Two Versions Available
Traditional financial planning asks
you to do all the hard work. It makes
you set your own saving and life
insurance targets. This puts you at
risk. Set your targets too low and
you’ll under-save and under-insure.
Set them too high and you’ll over-
save and over-insure.
Economic Security Planner
(ESPlanner™), developed by
Boston University Professor
Laurence Kotlikoff and other lead-
ing economists, finds the right
targets. It calculates your family’s
highest sustainable living standard
and the amounts you need to save
and insure to maintain that living
standard through time.
• ESPlannerBASIC—a simpli-
fied on-line version of this
lifetime, financial planning
software. To learn more about
ESPlannerBASIC, go to www.
bu.edu/hr/benefits/finances/
retirement-planning-resources-
tools/esplanner-financial-plan-
ning-tools and enter your BU
login and Kerberos password.
You will press the LOGIN button
on the ESPlannerBASIC website.
Once you create your personal
account, you can return to it
whenever you wish. Your infor-
mation will be kept secure and
confidential.
• ESPlannerPLUS—a detailed
downloadable version of the
Other Benefits

120
software is available at www.
bu.edu/hr/benefits/finances/
retirement-planning-resources-
tools/esplanner-plus-financial-
planning-software.
To learn more about ESPlanner
and examine research studies based
on ESPlanner, please visit www.
esplanner.com.
Faculty & Staff
Assistance Office
The Boston University Faculty &
Staff Assistance Office provides con-
fidential counseling and referral ser-
vices. It is available to you and your
family members if you are experienc-
ing personal, family, or work-related
problems. Services are available
without charge and include:
• Consultation
• Problem assessment
• Short-term psychotherapy
• Referral resource information
If you have a problem and are in
doubt about the wisest course
of action, we encourage you to
contact the program. In response
to your call, a counselor will meet
with you to discuss your prob-
lems and consider solutions. If
additional specialized counseling
proves necessary, a referral will be
made. Inquiries are confidential; no
one will know you have used the
Faculty & Staff Assistance Office
unless you tell them.
For additional information or to
schedule an appointment, call
617-353-5381. Appointments are
generally scheduled between 9 a.m.
and 5 p.m., Monday through Friday.
After-hours appointments may be
arranged upon request.
Family Resources Office
The Family Resources Office
is committed to helping Boston
University faculty and staff become
knowledgeable and informed about
child care and elder care by provid-
ing a resource and referral service.
For further information, contact
the director at 617-353-5954.
Fitness & Recreation Center
The Fitness & Recreation Center
has membership plans and pro-
gramming designed specifically for
faculty and staff. Come work out,
learn a new skill, recreate with your
family, and enjoy over six acres of
world-class fitness and recreation
under one roof, including:
• Faculty/staff locker rooms
and saunas
• Competition and recreation
pools
• 8,000-square-foot fitness center
• Dance theater
• Elevated jogging track
• Racquetball and squash
• Seven courts of gymnasia
• 35-foot climbing wall
• Juice bar and lounge with wire-
less internet access
• Hundreds of recreational classes
(at a significantly reduced rate if
you are a member) in yoga, fit-
ness, dance, martial arts, cycling,
swimming, and much, much
more.
The Fitness & Recreation Center
offers highly competitive member-
ship plans for faculty/staff, as well
as spouses and dependents.
The Fitness & Recreation Center
is located at 915 Commonwealth
Avenue. Contacts: 617-353-2748,
www.bu.edu/fitrec.
Income Solutions
Income Solutions
®
is an income
annuity purchase program. It is part
of the Hueler Companies, which is
a leading technology and research
firm located in Minneapolis,
Minnesota.
How Can Income Solutions Help
You? When you are ready to begin
receiving your retirement income,
an income annuity is one option
you may want to explore. Income
Solutions provides you with the tools
necessary to easily convert all or a
portion of your retirement assets into
an annuity which provides a steady
income stream you cannot outlive.
Since Income Solutions is offered
through Boston University, you are
able to purchase income annuities at
a group discount or wholesale prices
compared to those offered in the
retail marketplace.
An annuity is a long-term contract
between an annuitant and an insur-
ance company in which the annui-
tant receives income payments at
regular intervals from a fixed date
for a specific fixed period of time
and/or until death in return for the
premium that the annuitant pays to
the insurance company.
Use the Annuity Income Calculator
By accessing Income Solutions
through Boston University’s
website, you will be able to
use the income calculator.
After you answer several ques-
tions, estimates for each of the
immediate fixed income annuity
options available through Income
Solutions will be provided along
with a definition of each type.
You may want to try calculating
several scenarios before deter-
mining which best meets your
personal circumstances. Once you
have an idea of what your needs
are and which annuity option(s)

For more information, contact
Liberty Mutual at 1-888-480-4566
or go to www.libertymutual.com/
buemployee.
QuitNet
QuitNet is an Internet-based service
designed to help individual tobacco
users through the quitting process.
Launched as a smoking cessa-
tion service on the Web in 1995,
QuitNet was created by Nathan
Cobb, MD, and further developed at
Boston University School of Public
Health. QuitNet is now managed by
Healthways.
Boston University faculty and staff
and their family members who
register with QuitNet can receive
free stop-smoking medications.
Participants may select from the
Nicoderm Patch, Nicorette Gum,
or Commit Lozenge for convenient
home delivery.
QuitNet members may choose from
the following support services:
• Comprehensive online support
from QuitNet’s website
• Expert support
• Printed guide to quitting
• Quit Tips email support delivered
to your inbox
For more information, log on to
www.bu.edu/hr/benefits/health-
wellness/quitnet and select the
“introduction” link. You will be able
to view screen shots of pages on
the QuitNet website before you join
QuitNet.
If you decide that you want to join
QuitNet, you can enroll yourself or
your family members by going to
www.bu.edu/hr/benefits/health-
wellness/quitnet and clicking on the
“log in” link. You will need to log on
with your BU Kerberos password.
121
may make sense for you, you may
request quotes.
Request Quotes Income Solutions
provides you with a platform in
which you can receive quotes from
a broad group of high-quality insur-
ance companies that participate
in the Income Solutions program.
Every quote request is competi-
tively bid across the participating
insurance companies to ensure
that retirees receive the best avail-
able annuity quotes. All annuity
quotes are provided on equal
terms, ensuring comparison.
There is no cost to you to use
the annuity income calcula-
tor or to request quotes; how-
ever, if you purchase an annuity
through Income Solutions, Hueler
Companies will receive a speci-
fied fee which is disclosed at the
Income Solutions site.
How to Access Income Solutions For
more information, log on to www.
bu.edu/hr/benefits/finances/
retirement-planning-resources-
tools/income-solutions.
You will need to log on with your
BU Kerberos password.
If you have any questions, please
contact the Benefits Section of
Human Resources at hrben
@
bu.edu
or call 617-353-4488 or
617-353-5459.
New England Eye Benefit
BU employees and their family
members receive an enhanced eye
care benefit through New England
Eye (NEE) at the Commonwealth
Avenue and Roslindale full-service
eye clinics.
NEE offers a full range of eye care
services including comprehensive
eye care exams, pediatric and vision
therapy services, optical services,
contact lens and cornea services,
low vision and rehabilitative services,
consultative ophthal mology, and
laser vision correction evaluations.
Features of the benefit:
• 40% discount on eyewear and
competitive pricing on contact
lenses.
New England Eye is the patient care
subsidiary of The New England
College of Optometry.
For more information, contact
New England Eye at 617-262-2020
or visit their website at
www.newenglandeye.org.
Personal Insurance
This program offers a special dis-
count on the cost of automobile
and homeowners insurance for
Massachusetts residents. It is cur-
rently underwritten by Liberty
Mutual. You are eligible to par-
ticipate in the program if you are a
Massachusetts resident, provided
you have not failed to pay an auto-
mobile insurance premium during
the past 12 months. Enrollment is
completely voluntary and is handled
directly by Liberty Mutual.
Coverage includes:
• Automobile coverage through
a group discount plan
• Homeowners and renters
insurance
• Umbrella coverage
• Premium payment by payroll
deduction or monthly home bill-
ing (premium payments are on
an after-tax basis)

If you have any questions, please
contact the Benefits Section of
Human Resources at hrben
@
bu.edu
or call 617-353-4488 or 617-353-
5459.
Real Estate Services
• Assistance with home finding
and selling
• Mortgage services
• Relocation and moving services
For more information, contact the
Real Estate Advantage Program at
1-800-396-0960.
Metro Credit Union
Join 11,000 Boston University
faculty, staff, students, and other
supporters by becoming a mem-
ber of Metro Credit Union (www.
metrocu.org/home/home). As
a member, you have access to
numerous financial services,
including checking accounts, sav-
ings accounts, IRAs, and auto and
home loans. The Credit Union also
provides financial calculators and
other helpful tools.
Metro Credit Union is another
University resource for you and
your family. Employees, retirees,
students, and all family members
are eligible to become a Metro
Credit Union member. And at
Metro Credit Union, you stay a
member for life—even if you retire
or leave Boston University.
For more information, please call
1-877-MYMETRO or visit the Credit
Union’s main branch, located on
the Charles River Campus at 922
Commonwealth Avenue. The Credit
Union also has an office on the
Medical Campus at 710 Albany
Street.
Additional Benefits
In addition to your Boston University
benefits, federal and state laws
require employers to provide
you with certain other benefits.
These statutory benefits include
Social Security, Unemploy ment
Compensation, and Workers’
Compensation.
Boston University pays the
entire cost of Unemployment
Compensation and Workers’
Compensation and also contributes
to the cost of your Social Security
benefits.
Statutory benefits may provide
you and your family with financial
assistance, in addition to University-
sponsored benefits, when you are
injured on the job, become disabled,
retire, or die.
Social Security
The Social Security Act provides a
range of programs to afford you a
basic level of benefits in the event of
your retirement, death, or disability.
Most of these benefits are financed
by payroll taxes.
Your Social Security benefits include:
• Retirement insurance
• Survivors’ insurance
• Disability insurance
• Medicare
• Supplemental security income
Social Security benefits are adjusted
frequently, and the rules and regula-
tions change. You should contact
your local Social Security office to
obtain the latest information about
the benefits to which you may be
entitled.
Unemployment Compensation
The University pays the Common-
wealth of Massachusetts the cost
of your unemployment compensa-
tion. You may be eligible to receive
unemployment compensation ben-
efits if you lose your job through no
fault of your own. Unemployment
compensation is coordinated
through the Massachusetts Division
of Unemployment Assistance,
which determines your eligibility.
Workers’ Compensation
Massachusetts Workers’ Compen-
sation laws prescribe certain
medical, hospital, disability com-
pensation, rehabilitation, and death
benefits to be paid in the event of
injury or death due to work-related
accidents or illnesses. Boston
University pays the full cost of insur-
ance to cover these benefits. You
are automatically covered by this
insurance while you are employed
by the University.
If you are injured while you are at
work, report the injury to your
supervisor immediately. Remember,
minor injuries (which at the time
may seem trivial, but may later
require medical attention) may
also be covered, provided they are
reported when they occur.
Severance Pay Plan
A severance pay plan is available
to eligible staff members. See your
Employee Handbook for further
details.
122

Overview
Administrative Information
124
A
ll of the plans described in the previous sections of this
handbook are sponsored and administered by Boston
University. These plans were designed to provide you with an
outstanding benefits package—one that is comprehensive and
also responsive to the needs of all employees.
This section provides information regarding the administra-
tion of your benefits. It also explains your rights under the
Employee Retirement Income Security Act of 1974 (ERISA).

125
About the Plans
Sponsor for the Plans
All of the plans described in this
handbook are sponsored by the
employer, Boston University,
Boston, Massachusetts.
Boston University’s Employer
Identification Number
For identification purposes, the
Internal Revenue Service has
assigned number 04-2103547 to
Boston University. You will need to
know this number if you write to a
government agency about any of
the plans.
Types of Plans, Plan Numbers,
and Plan Years
In addition to the University’s
Employer Identification Number,
you need to know the following
information:
• Types of Plans The plans
described in this handbook are
characterized by the federal
government as either Defined
Contribution Plans or Welfare
Plans.
• Plan Numbers Boston University
has assigned Plan Numbers to all
of the plans.
• Plan Years The financial records
of all plans are kept on a Plan
Year basis. The Type of Plan,
Plan Number, and Plan Year for
each plan are listed on the fol-
lowing pages.
Administrator for All Plans
The day-to-day administration of
all plans is handled by the Benefits
Section of Human Resources.
However, if you have a question or
a problem that cannot be resolved
by the Benefits Section of Human
Resources, you should contact the
Plan Administrator.
The Plan Administrator for all plans
can be reached by contacting:
Plan Administrator
The Trustees of Boston University
25 Buick Street
Boston, MA 02215
Phone: 617-353-4489
Funding and Administration
of All Plans
Boston University pays the entire
cost of many of the benefit plans
described in this handbook. In some
cases you and the University share
the cost. In others, you pay the
entire cost.
Following is an explanation of how
the plans are funded and who is
responsible for paying benefits:
• Defined Contribution
Plans Contri butions to the
Retirement Plan and the
Supplemental Retirement and
Savings Plan go to the following
investment entities, which hold
the plan’s assets and are respon-
sible for paying benefits from
the participants’ accounts. The
addresses and telephone num-
bers of these offices are:
Fidelity Investments Tax-Exempt
Services Company (Fidelity)
82 Devonshire Street
Boston, MA 02109
Phone: 1-800-343-0860
Teachers Insurance and Annuity
Association (TIAA)
730 Third Avenue
New York, NY 10017
Phone: 1-800-842-2733
College Retirement Equities
Fund (CREF)
730 Third Avenue
New York, NY 10017
Phone: 1-800-842-2733
Administrative Information

126
Name of Plan Type of Plan Plan Number Plan Year
Boston University
Retirement Plan Defined Contribution 002 January 1–December 31
Supplemental Retirement
and Savings Plan Defined Contribution 005 January 1–December 31
Boston University Health Plan Welfare 502 January 1–December 31
Boston University Dental
Health Plan Welfare 703 January 1–December 31
Long-Term Disability Plan Welfare 507 February 1–January 31
Basic Life Insurance Plan Welfare 504 January 1–December 31
Group Supplemental Life
Insurance Plan Welfare 510 January 1–December 31
Travel Accident Insurance Plan Welfare 505 May 1–April 30
Personal and Family
Accident Insurance Plan Welfare 506 January 1–December 31
Supplemental Death
Benefit Plan Welfare 509 July 1–June 30
Tuition Remission Program Welfare 701 January 1–December 31
Flexible Benefits Program Welfare 702 January 1–December 31
Automatic Before-Tax
Health, Dental, and Accident
Insurance
Contributions
Flexible Spending Account—
Dependent Care
Flexible Spending Account—
Health Care January 1–March 15 of following year
Severance Pay Plan Welfare 704 January 1–December 31

127
• Welfare Plans Contributions to
the Health Plan go to the following
providers, who are responsible for
processing claims for benefits. The
addresses and telephone numbers
of these processors are:
Blue Cross Blue Shield of
Massachusetts
Landmark Center
401 Park Drive
Boston, MA 02215
1-800-814-4371
Medco/Express Scripts
100 Parsons Pond Drive
Franklin Lakes, NJ 07417
1-800-230-0508
You pay for your portion of the cost
of your health plan coverage with
before-tax dollars.
Contributions to the Dental Health
Plan are used by the University for
paying plan benefits. The address
and telephone number of the Dental
Health Plan are:
Blue Cross Blue Shield of
Massachusetts
Landmark Center
401 Park Drive
Boston, MA 02215
1-800-814-4371
Contributions to the Basic and
Group Supplemental Life Insurance
Plans go to The Prudential Insurance
Company of America. Basic and
Group Supplemental Life Insurance
benefits are paid by Prudential
through a contract it has with
Boston University. The address and
telephone number of the Prudential
administrative office are:
The Prudential Insurance
Company of America
800 Boylston Street, 14th Floor
Boston, MA 02199
1-800-778-3827
You pay for the cost of your
Group Supplemental Life Insurance
Coverage with after-tax dollars.
Contributions to the Travel Accident
Insurance Plan and the Personal and
Family Accident Insurance Plan go
to The Hartford. Benefits are paid
by The Hartford through a contract
it has with Boston University. The
address and telephone number of
the company’s administrative office
are:
The Hartford
Group Benefits
P.O. Box 2999
Hartford, CT 06104-2999
1-888-747-8819
You pay for the cost of your
Personal and Family Accident
Insurance coverage with before-tax
dollars.
Long-Term Disability Plan benefits
are processed by Liberty Mutual
through a contract it has with the
University. The address and tele-
phone number of Liberty Mutual are:
Liberty Mutual
P.O. Box 1525
Dover, NH 03821
1-800-210-0268, ext. 58535
Contributions to the Dependent
Care and Health Care Flexible
Spending Accounts are credited
to your accounts by the University.
Your contributions to these accounts
are made with pre-tax dollars. The
University is responsible for paying
Flexible Spending Account benefits.
Finally, Accidental Death Benefit,
Severance Pay Plan, and Tuition
Remission Program benefits are paid
out of the general assets of Boston
University.
Agent of Legal Service
The agent for the service of legal
process for all plans is:
University Counsel
125 Bay State Road
Boston, MA 02215
Legal process may be served on the
plan administrator.
Fraudulent Claims
Submission of a claim for benefits
under any of the plans described
in this handbook includes a rep-
resentation that the claim is bona
fide and, to the best knowledge of
the employee, dependent, or other
claimant, proper for payment.
Submission of a fraudulent or know-
ingly false claim by an employee
or an employee’s dependent par-
ticipating in a plan will be grounds
for disciplinary action against the
employee or for termination of
participation by the employee and/
or covered dependent(s) under the
plan.

128
Claims for Benefits/Appealing a
Denial of Claims for Benefits
At the end of each benefit descrip-
tion contained in this handbook,
there is a section that explains how
to apply for benefits. When you
apply for benefits, there are time
periods within which you must
receive a decision on your claim for
benefits. If you or your beneficiary
applies for benefits and either part
or all of the request is denied, you
have the right to appeal that deci-
sion, provided the appeal is made
in accordance with the provisions
of the plan and applicable laws
(e.g., appeals must be filed within
required time periods). Appeals are
generally decided by the provider
of the benefit involved, which is the
insurance carrier or vendor for most
benefits, or the University or its
Plan Administration Committee for
some benefits.
Appeals to Insurance Carriers/
Claims Administrators/Other
Vendors
For the following plans, appeals
regarding benefits or other issues
affecting plan participants or other
persons should be made directly to
the applicable provider under the
Plan:
• The Health Plan
• The Dental Health Plan
• The Basic and Group
Supplemental Life Insurance Plan
• The Travel Accident and
Personal and Family Accident
Insurance Plan
• The Long-Term Disability Plan
Details of claims and appeal proce-
dures may vary, but generally the
following procedures apply:
• If a claim for benefits is either
wholly or partially denied, you
will be notified in writing. The
notice will state the reasons why
the claim was denied and the
deadline for requesting review,
which is different for different
types of plans and/or claims.
• If you wish to appeal, you are
entitled to review all documents
pertaining to your claim free
of charge and may also submit
comments pertaining to your
claim.
• Your appeal of the denial should
be addressed to the carrier as
directed in the denial of benefits
notice.
• The applicable provider will
decide the claims and appeals in
the time and manner required by
law.
• Unless a different time period
applies, claims will be decided
within 90 days (180 days if spe-
cial circumstances apply) and
appeals for denied claims must
be filed within 60 days of denial.
A decision must be made within
60 days (or 120 days if special
circumstances are present and
you are notified).
• There are different time periods
for filing and appealing claims for
the Health Plan, Dental Health
Plan, and Long-Term Disability
Plan. Please refer to the Benefits
Handbook sections for these
plans for the specific time periods.
Claims and Appeals to the
University
For the following plans, appeals
regarding benefits or other issues
affecting plan participants or other
persons should be made to the
University’s Plan Administration
Committee:
• Supplemental Death Benefit
• The Boston University
Retirement Plan
• The Supplemental Retirement
and Savings Plan
• The Flexible Benefits Program
• The Severance Pay Plan
For the Tuition Remission Plan,
appeals regarding benefits or other
issues affecting plan participants
or other persons should be made
to the Office of the Senior Vice
President and General Counsel.
For claims and appeals to the
University’s Plan Administration
Committee, the following proce-
dures will apply:
• If a claim for benefits is either
wholly or partially denied, you
will be notified in writing within
90 days after receipt of your
claim (180 days if special cir-
cumstances apply). The notice
will state:
o the reasons why the claim
was denied,
o the specific references in the
plan document that support
those reasons,
o the information you must pro-
vide to verify your claim and
the reasons why that informa-
tion is necessary,
o the Plan’s review procedures,
including your right to bring
a civil action following an
adverse benefit determination
on review,
o and the deadline for request-
ing review.
• After receiving the notice,
you or your beneficiaries may
request, in writing, a review of
your claim by the University’s
Plan Administration Committee
or Senior Vice President and

129
General Counsel, as applicable,
by submitting an appeal to:
Plan Administration Committee
(or Senior Vice President and
General Counsel), c/o Plan
Administrator, Boston University
Human Resources, 25 Buick
Street, Boston, MA 02215.
• Your appeal of a denied claim
must be submitted within 60
days after your claim has been
denied. You (or your representa-
tive) may review Plan documents
and submit issues and com-
ments orally, in writing, or both.
• The Plan Administration
Committee (or Senior Vice
President and General Counsel)
will conduct a full and fair review
of your claim and appeal, and
notify you of the final decision
regarding your appeal within 60
days (120 days if special circum-
stances apply) after your request
for review is received. The deci-
sion will be in writing and will
include the specific reasons and
the plan references on which the
decision is based.
Appeals may be submitted to the
following carriers:
• The Health Plan
Blue Cross Blue Shield
Member Grievance Program
Blue Cross Blue Shield of
Massachusetts
One Enterprise Drive
Quincy, MA 02171-2126
1-800-814-4371
Medco/Express Scripts Health
Solutions of Irving
Attn: Administrative Reviews
8111 Royal Ridge Parkway
Irving, TX 75063
1-800-230-0508
• The Dental Plan
Blue Cross Blue Shield
Member Grievance Program
Blue Cross Blue Shield of
Massachusetts
One Enterprise Drive
Quincy, MA 02171-2126
1-800-814-4371
• The Group Life Insurance Plan
and the Group Supplemental Life
Insurance Plan
The Prudential Insurance
Company of America
800 Boylston Street, 14th Floor
Boston, MA 02199
1-800-778-3827
• Travel Accident Insurance Plan
and the Personal and Family
Accident Insurance Plans
The Hartford
Group Benefits
P.O. Box 2999
Hartford, CT 06104-2999
1-888-747-8819
• The Long-Term Disability Plan
Liberty Mutual
P.O. Box 1525
Dover, NH 03821
1-800-210-0268, ext. 58535
Documents and Laws Governing
All Plans
The plan descriptions contained in
this handbook were written from the
documents that legally govern how
the plans work.
In the event of any discrepancy
between the plan descriptions in
this handbook and the controlling
contracts or plan documents, the
language in the controlling contracts
or plan documents will govern. If
you would like a copy of any of
these documents, please contact
the Benefits Section of Human
Resources.
The plans are also regulated by
applicable provisions of applicable
laws, which will govern in the event
of any conflict between the law and
the terms of the plans as described
in either the documents or in the
summary plan description.
Equal Opportunity/Affirmative
Action Policy
Since its founding in 1869, Boston
University has been dedicated to
equal opportunity and has opened
its doors to students without regard
to race, sex, creed, or other irrel-
evant criteria. Consistent with this
tradition, it is the policy of Boston
University to promote equal oppor-
tunity in educational programs and
employment through practices
designed to extend opportunities to
all individuals on the basis of indi-
vidual merit and qualifications, and
to help ensure the full realization
of equal opportunity for students,
employees, and applicants for
admission and employment. The
University is committed to main-
taining an environment that is wel-
coming and respectful to all.
Boston University prohibits dis-
crimination against any individual
on the basis of race, color, religion,
sex, age, national origin, physical or
mental disability, sexual orientation,
genetic information, military service,
or because of marital, parental, or
veteran status. This policy extends
to all rights, privileges, programs,
and activities, including admissions,
financial assistance, educational and
athletic programs, housing, employ-
ment, compensation, employee ben-
efits, and the providing of, or access
to, University services or facilities.
Boston University recognizes that
non-discrimination does not ensure
that equal opportunity is a reality.
Accordingly, the University will con-
tinue to take affirmative action to

130
achieve equal opportunity through
recruitment, outreach, and internal
reviews of policies and practices.
The coordination and implementation
of this policy is the responsibility of
the Director of Equal Opportunity.
The officers of the University and all
deans, directors, department heads,
and managers are responsible for
the proper implementation of equal
opportunity and affirmative action
in their respective areas, and they
are expected to exercise leader-
ship toward their achievement. It
is expected that every employee
of Boston University will share this
commitment and cooperate fully in
helping the University meet its equal
opportunity and affirmative action
objectives.
Boston University has developed
detailed procedures, described in
its Complaint Procedures in Cases
of Alleged Unlawful Discrimination
or Harassment (www.bu.edu/eeo/
policies-procedures/complaint), by
which individuals may bring forward
concerns or complaints of discrimi-
nation and harassment. Retaliation
against any individual who brings
forward such a complaint or who
cooperates or assists with an inves-
tigation of such a complaint is both
unlawful and strictly prohibited by
Boston University.
Inquiries regarding this policy or
its application should be addressed
to the Director of Equal Opportunity,
Equal Opportunity Office, 25 Buick
Street, Boston, MA 02215,
617-353-9286.
Amendment or Termin ation
of the Plans
Boston University intends to
continue maintaining the plans
described in this handbook for the
exclusive benefit of its employees.
However, the University reserves the
right to change or discontinue any
of them, and to implement changes
as required by federal, state, or local
laws.
You will be informed of any mate-
rial changes that are made to the
plans. If a plan is terminated, your
rights, on the date of the termina-
tion, would be governed by the pro-
visions of the plan document.
Your Rights Under ERISA
The following Boston University ben-
efit plans are subject to the provisions
of the Employee Retirement Income
Security Act of 1974 (ERISA):
• Health Plan
• Dental Health Plan
• Long-Term Disability Plan
• Basic Life Insurance Plan
• Group Supplemental Life
Insurance Plan
• Travel Accident Insurance Plan
• Personal and Family Accident
Insurance Plan
• Supplemental Death Benefit
• Retirement Plan
• Supplemental Retirement and
Savings Plan
• Flexible Benefits Program
• Severance Pay Plan
ERISA provides the participants in
these plans with certain rights and
protections. The following state-
ment is included here so that you
will be aware of your rights under
the law.
Under ERISA:
• You may examine, without
charge, at the Benefits Section
of Human Resources and at
other specified locations, during
normal business hours, all plan
documents relating to the plans
in which you participate. The
documents that must be available
for your review include insur-
ance contracts, plan and trust
documents, collective bargaining
agreements, and all documents
filed with the U.S. Department of
Labor and available at the Public
Disclosure Room of the Employee
Benefits Security Administration,
for example, detailed annual
reports.
• If you wish, you may request
your own copies of these plan
documents by writing to the
Benefits Section of Human
Resources. You may have to pay
a reasonable charge to cover the
costs of copying.
• You will receive summaries
of the plans’ annual financial
reports each year, free of charge.
The administrator for the plans
is required by law to furnish each
participant with a copy of these
summary annual reports.
• You may request a statement of
your vested benefits under the
Boston University Retirement
Plan and the Supplemental
Retirement and Savings Plan.
This statement will be given to
you free of charge and may be
requested once each year.
• You have a right to receive a
copy of any material change to
a plan within 210 days of the
plan year in which the change
is adopted.

Continue Health and Dental Coverage
You may continue health care or
dental care coverage for yourself,
your spouse, or your dependents if
there is a loss of coverage under the
Health Plan or Dental Health Plan
as a result of a qualifying event. You
or your dependents may have to
pay for such coverage. Review the
applicable section of this handbook
and the documents governing the
Health Plan and Dental Health Plan
on the rules governing your COBRA
continuation coverage rights.
You may reduce or eliminate exclu-
sionary periods of coverage for pre-
existing conditions under the Health
Plan, if you have creditable coverage
from another plan. You should be
provided a certificate of creditable
coverage, free of charge, from your
group health plan or health insur-
ance issuer when you lose coverage
under the Health Plan, when you
become entitled to elect COBRA
continuation coverage, when your
COBRA continuation coverage
ceases, if you request it before los-
ing coverage, or if you request it up
to 24 months after losing coverage.
Without evidence of creditable cov-
erage, you may be subject to a pre-
existing condition exclusion for 12
months (18 months for late enroll-
ees) after your enrollment date in
your coverage.
Plan Fiduciaries
Besides giving you certain rights as
a participant, ERISA places certain
duties upon the people who are
responsible for the management of
the above-mentioned plans. These
people are called “fiduciaries” under
the law, and they have the duty to act
prudently and in your best interests.
Under ERISA, no one may fire you or
discriminate against you to prevent
you from obtaining a plan benefit or
exercising your rights under ERISA.
Enforcing Your Rights
If your claim for a benefit is denied,
in whole or in part, you must receive
a written explanation of the reason
for the denial. You have a right to
obtain copies, without charge, of
documents relating to the decision,
and to appeal any denial all within
certain time schedules.
Under ERISA, there are steps you
can take to enforce your rights. For
instance, if you request materials
from the plan and do not receive
them within 30 days, you may file
suit in a federal court. In such case,
the court may require the Plan
Administrator to provide the materi-
als and pay you up to $110 for each
day’s delay until you receive the
materials, unless the materials were
not sent for reasons beyond the
administrator’s control. If you have
a claim for benefits that is denied
or ignored, in whole or in part, you
may file suit in a state or federal
court. In addition, if you disagree
with a plan’s decision or lack thereof
concerning the qualified status of a
domestic relations order or medical
child support order, you may file suit
in federal court. If it should happen
that plan fiduciaries misuse plan
money, or if you are discriminated
against for asserting your rights, you
may seek assistance from the U.S.
Department of Labor or file suit in a
federal court.
In a lawsuit, the court normally
decides who pays the court costs
and legal fees. If you are success-
ful, the other party might have to
pay. But, if you lose, the court might
order you to pay these costs and
fees, especially if the court finds
your claim to be frivolous.
Assistance with Questions
If you have any questions about
this statement of your rights under
ERISA, contact the Benefits Section
of Human Resources. If you have
any questions about this state-
ment or about your rights under
ERISA, or if you need assistance
in obtaining documents from the
Plan Administrator, you should
contact the nearest area office of
the Employee Benefits Security
Administration, U.S. Department of
Labor, listed in your telephone direc-
tory, or the Division of Technical
Assistance and Inquiries, Employee
Benefits Security Administration,
U.S. Department of Labor, 200
Constitution Avenue, NW,
Washington, DC 20210. You may
also obtain certain publications
about your rights and responsi-
bilities under ERISA by calling the
publications hotline of the Employee
Benefits Security Administration.
A Final Note
This handbook presents a summary
of Boston University’s benefits for
faculty and staff. It is designed as
a quick reference source and is not
intended to cover every point of
policy. In certain instances, the
University may exercise discretion,
with respect to the administration
of the plans described in this hand-
book. For more in-depth informa-
tion, contact the Benefits Section of
Human Resources.
Periodically, the University may
make changes in policy that may
not be reflected immediately in this
handbook.
Again, for complete and up-to-date
information about any policy or ben-
efit, you should contact the Benefits
Section of Human Resources.
Please note: The policies described
in this handbook are not intended
to create an employment contract
between Boston University and its
employees. Therefore, they do not
alter the University’s rights regard-
ing discharges and layoffs.
131
0513 9040040605

Notes

